Cefiderocol and Sulbactam-Durlobactam against Carbapenem-Resistant Acinetobacter baumannii
Abstract
:1. Introduction
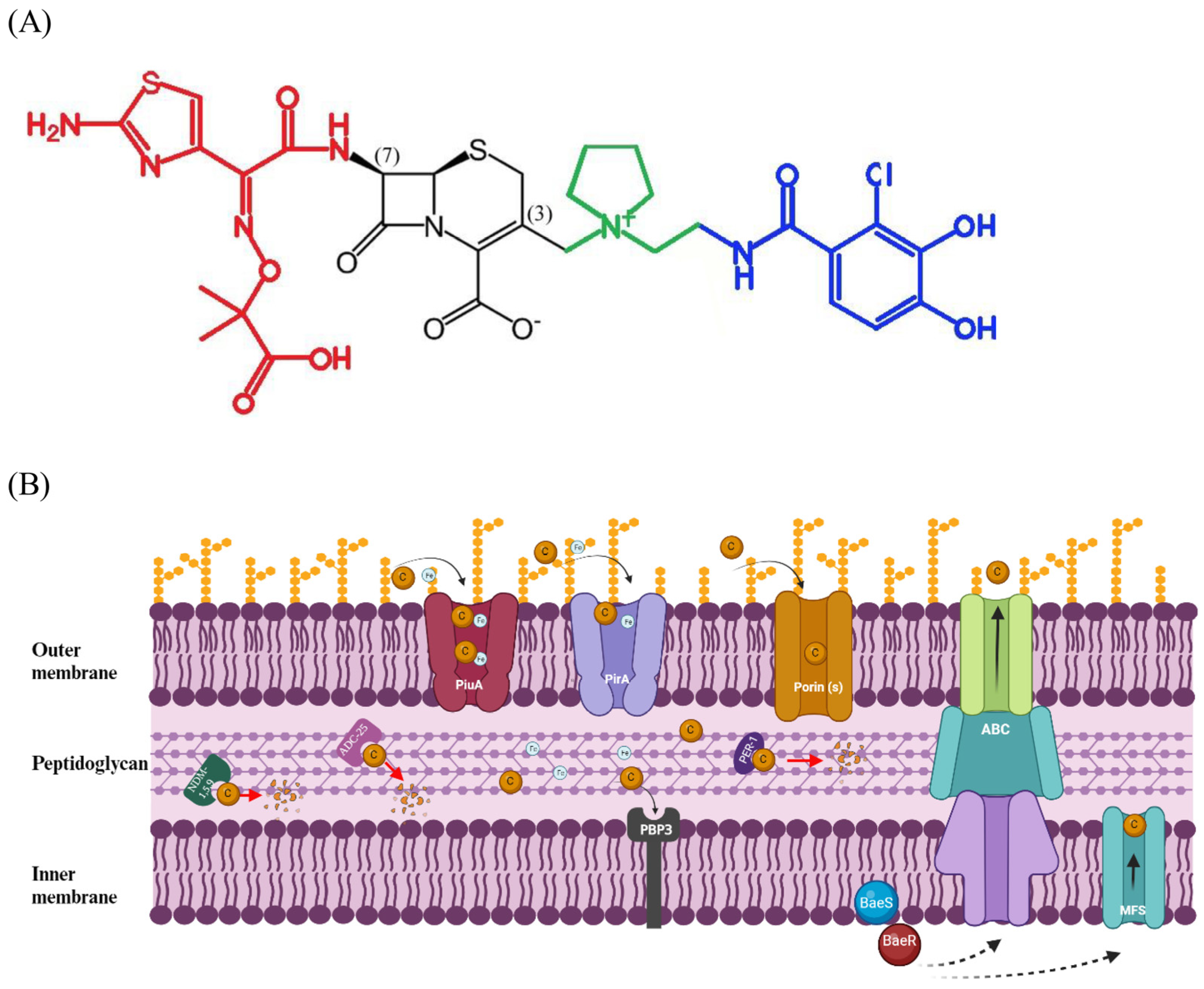
2. Cefiderocol Is a Novel Siderophore Cephalosporin
2.1. Chemical Structure and Pharmacological Data
2.2. In Vitro and In Vivo Activity against CRAB
2.3. Mechanisms of Resistance
2.4. Therapy against CRAB
2.4.1. Studies Evaluating the Clinical Efficacy of FDC
Randomized, Phase III Studies
- APEKS-NP—enrolling patients with nosocomial pneumonia;
- CREDIBLE-CR—focusing on severe infections caused by CR Gram-negatives.
Clinical Studies Comparing the Efficacy of FDC with That of Colistin
Mortality
Mortality Based on Type of Infection
Other Outcomes
Clinical Studies and Case Series Assessing the Efficacy of FDC in Treating CRAB Infections
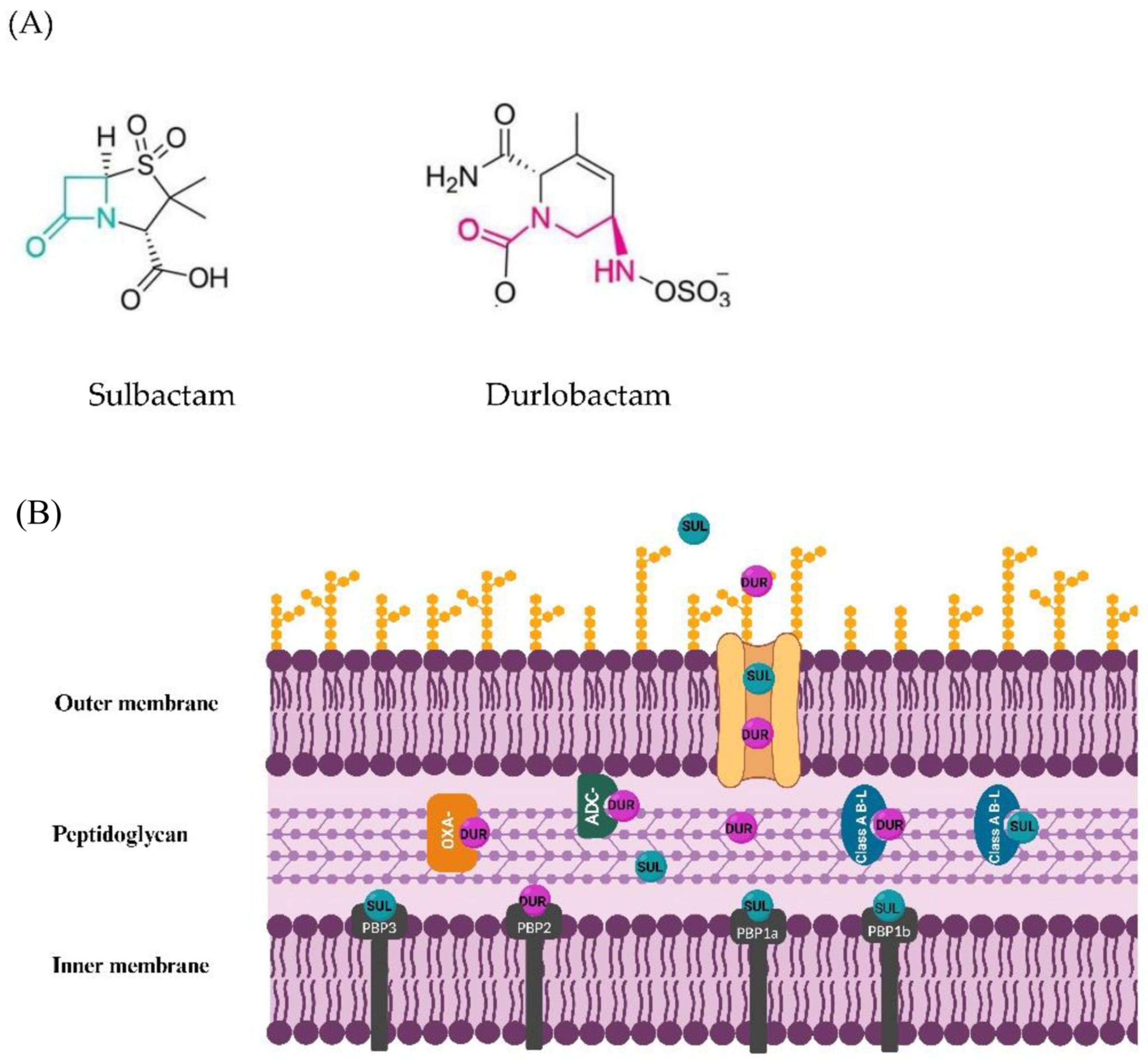
3. Sulbactam-Durlobactam: A Novel Combination of a Beta-Lactamase Inhibitor with Beta-Lactam Activity and a Non-Beta-Lactam/Beta-Lactamase Inhibitor
3.1. Chemical Structure and Pharmacological Data
3.2. In Vitro and In Vivo Activity against CRAB
3.3. Mechanisms of Resistance
3.4. Therapy against CRAB
3.4.1. Clinical Trials Assessing Efficacy and Safety of SUL-DUR
3.4.2. Clinical Studies/Case Reports of SUL-DUR Efficacy in Real Life
4. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zarrilli, R.; Pournaras, S.; Giannouli, M.; Tsakris, A. Global evolution of multidrug-resistant Acinetobacter baumannii clonal lineages. Int. J. Antimicrob. Agents 2013, 41, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.; Nielsen, T.B.; Bonomo, R.A.; Pantapalangkoor, P.; Luna, B.; Spellberg, B. Clinical and pathophysiological overview of Acinetobacter infections: A century of challenges. Clin. Microbiol. Rev. 2017, 30, 409–447. [Google Scholar] [CrossRef] [PubMed]
- Migliaccio, A.; Bray, J.; Intoccia, M.; Stabile, M.; Scala, G.; Jolley, K.A.; Brisse, S.; Zarrilli, R. Phylogenomics of Acinetobacter species and analysis of antimicrobial resistance genes. Front. Microbiol. 2023, 14, 1264030. [Google Scholar] [CrossRef] [PubMed]
- Dickstein, Y.; Lellouche, J.; Amar, M.B.D.; Schwartz, D.; Nutman, A.; Daitch, V.; Yahav, D.; Leibovici, L.; Skiada, A.; Antoniadou, A.; et al. Treatment outcomes of colistin- and carbapenem-resistant Acinetobacter baumannii infections: An exploratory subgroup analysis of a randomized clinical trial. Clin. Infect. Dis. 2019, 69, 769–776. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Global Priority List of Antibiotic-Resistant Bacteria to Guide Research, Discovery, and Development of New Antibiotics; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- El-Lababidi, R.M.; Rizk, J.G. Cefiderocol: A Siderophore Cephalosporin. Ann. Pharmacother. 2020, 54, 1215–1231. [Google Scholar] [CrossRef] [PubMed]
- Shortridge, D.; Streit, J.M.; Mendes, R.; Castanheira, M. In Vitro Activity of Cefiderocol against U.S. and European Gram-Negative Clinical Isolates Collected in 2020 as Part of the SENTRY Antimicrobial Surveillance Program. Microbiol. Spectr. 2022, 10, e0271221. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, S.; Singley, C.M.; Hoover, J.; Nakamura, R.; Echols, R.; Rittenhouse, S.; Tsuji, M.; Yamano, Y. Efficacy of Cefiderocol against carbapenem-resistant Gram-negative bacilli in immunocompetent-rat respiratory tract infection models recreating human plasma pharmacokinetic. Antimicrob. Agents Chemother. 2017, 61, e00700-17. [Google Scholar] [CrossRef] [PubMed]
- US Food and Drug Administration. Highlights of Prescribing Information: Fetroja (Cefiderocol). 2019. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/209445s000lbl.pdf (accessed on 12 November 2023).
- Shapiro, A.B.; Moussa, S.H.; McLeod, S.M.; Durand-Réville, T.; Miller, A.A. Durlobactam, a New Diazabicyclooctane β-Lactamase Inhibitor for the Treatment of Acinetobacter Infections in Combination With Sulbactam. Front. Microbiol. 2021, 12, 709974. [Google Scholar] [CrossRef]
- Karlowsky, J.A.; Hackel, M.A.; McLeod, S.M.; Miller, A.A. In Vitro Activity of Sulbactam-Durlobactam against Global Isolates of Acinetobacter baumannii-calcoaceticus Complex Collected from 2016 to 2021. Antimicrob. Agents Chemother. 2022, 66, e0078122. [Google Scholar] [CrossRef]
- Petropoulou, D.; Siopi, M.; Vourli, S.; Pournaras, S. Activity of Sulbactam-Durlobactam and Comparators Against a National Collection of Carbapenem-Resistant Acinetobacter baumannii Isolates from Greece. Front. Cell. Infect. Microbiol. 2022, 11, 814530. [Google Scholar] [CrossRef]
- Findlay, J.; Poirel, L.; Bouvier, M.; Nordmann, P. In vitro activity of sulbactam-durlobactam against carbapenem-resistant Acinetobacter baumannii and mechanisms of resistance. J. Glob. Antimicrob. Resist. 2022, 30, 445–450. [Google Scholar] [CrossRef]
- O’donnell, J.P.; Bhavnani, S.M. The Pharmacokinetics/Pharmacodynamic Relationship of Durlobactam in Combination With Sulbactam in In Vitro and In Vivo Infection Model Systems Versus Acinetobacter baumannii-calcoaceticus Complex. Clin. Infect. Dis. 2023, 76 (Suppl. 2), S202–S209. [Google Scholar] [CrossRef] [PubMed]
- Papp-Wallace, K.M.; McLeod, S.M.; A Miller, A. Durlobactam, a Broad-Spectrum Serine β-lactamase Inhibitor, Restores Sulbactam Activity Against Acinetobacter Species. Clin. Infect. Dis. 2023, 76 (Suppl. 2), S194–S201. [Google Scholar] [CrossRef] [PubMed]
- Keam, S.J. Sulbactam/Durlobactam: First Approval. Drugs 2023, 83, 1245–1252. [Google Scholar] [CrossRef] [PubMed]
- Malik, S.; Kaminski, M.; Landman, D.; Quale, J. Cefiderocol resistance in Acinetobacter baumannii: Roles of β-lactamases, siderophore receptors, and penicillin binding protein 3. Antimicrob. Agents Chemother. 2020, 64, e01221-20. [Google Scholar] [CrossRef] [PubMed]
- Asrat, H.; Samaroo-Campbell, J.; Ata, S.; Quale, J. Contribution of Iron-Transport Systems and β-Lactamases to Cefiderocol Resistance in Clinical Isolates of Acinetobacter baumannii Endemic to New York City. Antimicrob. Agents Chemother. 2023, 67, e0023423. [Google Scholar] [CrossRef] [PubMed]
- Moynié, L.; Luscher, A.; Rolo, D.; Pletzer, D.; Tortajada, A.; Weingart, H.; Braun, Y.; Page, M.G.P.; Naismith, J.H.; Köhler, T. Structure and Function of the PiuA and PirA Siderophore-Drug Receptors from Pseudomonas aeruginosa and Acinetobacter baumannii. Antimicrob. Agents Chemother. 2017, 61, e02531-16. [Google Scholar] [CrossRef]
- Ito, A.; Nishikawa, T.; Matsumoto, S.; Yoshizawa, H.; Sato, T.; Nakamura, R.; Tsuji, M.; Yamano, Y. Siderophore Cephalosporin Cefiderocol Utilizes Ferric Iron Transporter Systems for Antibacterial Activity against Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2016, 60, 7396–7401. [Google Scholar] [CrossRef]
- Hackel, M.A.; Tsuji, M.; Yamano, Y.; Echols, R.; Karlowsky, J.A.; Sahm, D.F. In Vitro Activity of the Siderophore Cephalosporin, Cefiderocol, against Carbapenem-Nonsusceptible and Multidrug-Resistant Isolates of Gram-Negative Bacilli Collected Worldwide in 2014 to 2016. Antimicrob. Agents Chemother. 2018, 62, e01968-17. [Google Scholar] [CrossRef]
- Zhanel, G.G.; Golden, A.R.; Zelenitsky, S.; Wiebe, K.; Lawrence, C.K.; Adam, H.J.; Idowu, T.; Domalaon, R.; Schweizer, F.; Zhanel, M.A.; et al. Cefiderocol: A siderophore cephalosporin with activity against carbapenem- resistant and multidrug-resistant Gram-negative bacilli. Drugs 2019, 79, 271–289. [Google Scholar] [CrossRef]
- EUCAST Disk Diffusion Manual v 11.0 (2 January 2023). Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Disk_test_documents/2022_manuals/Cefiderocol_disk_diffusion_training.pdf (accessed on 10 November 2023).
- Hackel, M.A.; Tsuji, M.; Yamano, Y.; Echols, R.; Karlowsky, J.A.; Sahm, D.F. Reproducibility of broth microdilution MICs for the novel siderophore cephalosporin, cefiderocol, determined using iron-depleted cation-adjusted Mueller-Hinton broth. Diagn. Microbiol. Infect. Dis. 2019, 94, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing M100 S, 33rd ed; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2023. [Google Scholar]
- Liu, Y.; Ding, L.; Han, R.; Zeng, L.; Li, J.; Guo, Y.; Hu, F. Assessment of cefiderocol disk diffusion versus broth microdilution results when tested against Acinetobacter baumannii complex clinical isolates. Microbiol. Spectr. 2023, 11, e0535522. [Google Scholar] [CrossRef] [PubMed]
- Jeannot, K.; Gaillot, S.; Triponney, P.; Portets, S.; Pourchet, V.; Fournier, D.; Potron, A. Performance of the Disc Diffusion Method, MTS Gradient Tests and Two Commercially Available Microdilution Tests for the Determination of Cefiderocol Susceptibility in Acinetobacter spp. Microorganisms 2023, 11, 1971. [Google Scholar] [CrossRef] [PubMed]
- Raro, O.H.F.; Bouvier, M.; Kerbol, A.; Decousser, J.-W.; Poirel, L.; Nordmann, P. Rapid detection of cefiderocol susceptibility/resistance in Acinetobacter baumannii. Eur. J. Clin. Microbiol. Infect. Dis. 2023, 42, 1511–1518. [Google Scholar] [CrossRef] [PubMed]
- Gill, C.M.; Santini, D.; Takemura, M.; Longshaw, C.; Yamano, Y.; Echols, R.; Nicolau, D.P. In vivo efficacy & resistance prevention of cefiderocol in combination with ceftazidime/avibactam, ampicillin/sulbactam or meropenem using human-simulated regimens versus Acinetobacter baumannii. J. Antimicrob. Chemother. 2023, 78, 983–990. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Chang, Y.; Xu, Q.; Zhang, W.; Huang, Z.; Zhang, L.; Weng, S.; Leptihn, S.; Jiang, Y.; Yu, Y.; et al. Mutation in the two-component regulator BaeSR mediates cefiderocol resistance and enhances virulence in Acinetobacter baumannii. mSystems 2023, 8, e0129122. [Google Scholar] [CrossRef] [PubMed]
- Poirel, L.; Sadek, M.; Nordmann, P. Contribution of PER-type and NDM-type b-lactamases to Cefiderocol resistance in Acinetobacter baumannii. Antimicrob. Agents Chemother. 2021, 65, e00877-21. [Google Scholar] [CrossRef]
- Liu, X.; Lei, T.; Yang, Y.; Zhang, L.; Liu, H.; Leptihn, S.; Yu, Y.; Hua, X. Structural Basis of PER-1-Mediated Cefiderocol Resistance and Synergistic Inhibition of PER-1 by Cefiderocol in Combination with Avibactam or Durlobactam in Acinetobacter baumannii. Antimicrob. Agents Chemother. 2022, 66, e0082822. [Google Scholar] [CrossRef]
- Stracquadanio, S.; Bonomo, C.; Marino, A.; Bongiorno, D.; Privitera, G.F.; Bivona, D.A.; Mirabile, A.; Bonacci, P.G.; Stefani, S. Acinetobacter baumannii and Cefiderocol, between Cidality and Adaptability. Microbiol. Spectr. 2022, 10, e0234722. [Google Scholar] [CrossRef]
- Longshaw, C.; Henriksen, A.S.; Dressel, D.; Malysa, M.; Silvestri, C.; Takemura, M.; Yamano, Y.; Baba, T.; Slover, C.M. Heteroresistance to cefiderocol in carbapenem-resistant Acinetobacter baumannii in the CREDIBLE-CR study was not linked to clinical outcomes: A post hoc analysis. Microbiol. Spectr. 2023, 15, e0237123. [Google Scholar] [CrossRef]
- Choby, J.E.; Ozturk, T.; Satola, S.W.; Jacob, J.T.; Weiss, D.S. Does cefiderocol heteroresistance explain the discrepancy between the APEKS-NP and CREDIBLE-CR clinical trial results? Lancet Microbe 2021, 2, e648–e649. [Google Scholar] [CrossRef] [PubMed]
- Wunderink, R.G.; Matsunaga, Y.; Ariyasu, M.; Clevenbergh, P.; Echols, R.; Kaye, K.S.; Kollef, M.; Menon, A.; Pogue, J.M.; Shorr, A.F.; et al. Cefiderocol versus high-dose, extended-infusion meropenem for the treatment of Gram-negative nosocomial pneumonia (APEKS-NP): A randomised, double-blind, phase 3, non-inferiority trial. Lancet Infect. Dis. 2020, 21, 213–225. [Google Scholar] [CrossRef] [PubMed]
- Bassetti, M.; Echols, R.; Matsunaga, Y.; Ariyasu, M.; Doi, Y.; Ferrer, R.; Lodise, T.P.; Naas, T.; Niki, Y.; Paterson, D.L.; et al. Efficacy and safety of cefiderocol or best available therapy for the treatment of serious infections caused by carbapenem-resistant Gram-negative bacteria (CREDIBLE-CR): A randomised, open-label, multicentre, pathogen-focused, descriptive, phase 3 trial. Lancet Infect. Dis. 2021, 21, 226–240. [Google Scholar] [CrossRef] [PubMed]
- Paul, M.; Daikos, G.L.; Durante-Mangoni, E.; Yahav, D.; Carmeli, Y.; Benattar, Y.D.; Skiada, A.; Andini, R.; Eliakim-Raz, N.; Nutman, A.; et al. Colistin alone versus colistin plus meropenem for treatment of severe infections caused by carbapenem-resistant Gram-negative bacteria: An open-label, randomised controlled trial. Lancet Infect. Dis. 2018, 18, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Durante-Mangoni, E.; Signoriello, G.; Andini, R.; Mattei, A.; De Cristoforo, M.; Murino, P.; Bassetti, M.; Malacarne, P.; Petrosillo, N.; Galdieri, N.; et al. Colistin and rifampicin compared with colistin alone for the treatment of serious infections due to extensively drug-resistant Acinetobacter baumannii: A multicenter, randomized clinical trial. Clin. Infect. Dis. 2013, 57, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Sirijatuphat, R.; Thamlikitkul, V. Preliminary Study of Colistin versus Colistin plus Fosfomycin for Treatment of Carbapenem-Resistant Acinetobacter baumannii Infections. Antimicrob. Agents Chemother. 2014, 58, 5598–5601. [Google Scholar] [CrossRef] [PubMed]
- Kaye, K.S.; Marchaim, D.; Thamlikitkul, V.; Carmeli, Y.; Chiu, C.-H.; Daikos, G.; Dhar, S.; Durante-Mangoni, E.; Gikas, A.; Kotanidou, A.; et al. Colistin Monotherapy versus Combination Therapy for Carbapenem-Resistant Organisms. NEJM Évid. 2023, 2, EVIDoa2200131. [Google Scholar] [CrossRef]
- Ho, Y.; Hu, F.; Lee, P. The Advantages and Challenges of Using Real-World Data for Patient Care. Clin. Transl. Sci. 2020, 13, 4–7. [Google Scholar] [CrossRef]
- Falcone, M.; Tiseo, G.; Leonildi, A.; Della Sala, L.; Vecchione, A.; Barnini, S.; Farcomeni, A.; Menichetti, F. Cefiderocol- Compared to Colistin-Based Regimens for the Treatment of Severe Infections Caused by Carbapenem-Resistant Acinetobacter baumannii. Antimicrob. Agents Chemother. 2022, 66, e0214221. [Google Scholar] [CrossRef]
- Russo, A.; Bruni, A.; Gullì, S.; Borrazzo, C.; Quirino, A.; Lionello, R.; Serapide, F.; Garofalo, E.; Serraino, R.; Romeo, F.; et al. Efficacy of cefiderocol- vs colistin-containing regimen for treatment of bacteraemic ventilator-associated pneumonia caused by carbapenem-resistant Acinetobacter baumannii in patients with COVID-19. Int. J. Antimicrob. Agents 2023, 62, 106825. [Google Scholar] [CrossRef]
- Russo, A.; Bruni, A.; Gullì, S.; Borrazzo, C.; Quirino, A.; Lionello, R.; Torti, C. Effectiveness of First-Line Therapy with Old and Novel Antibiotics in Ventilator-Associated Pneumonia Caused by Carbapenem-Resistant Acinetobacter baumannii: A Real Life, Prospective, Observational, Single-Center Study. Antibiotics 2023, 12, 1048. [Google Scholar] [CrossRef]
- Mazzitelli, M.; Gregori, D.; Sasset, L.; Trevenzoli, M.; Scaglione, V.; Lo Menzo, S.; Marinello, S.; Mengato, D.; Venturini, F.; Tiberio, I.; et al. Cefiderocol -Based versus Colistin-Based Regimens for Severe Carbapenem-Resistant Acinetobacter baumannii Infections: A Propensity Score-Weighted, Retrospective Cohort Study during the First Two Years of the COVID-19 Pandemic. Microorganisms 2023, 11, 984. [Google Scholar] [CrossRef] [PubMed]
- Rando, E.; Cutuli, S.L.; Sangiorgi, F.; Tanzarella, E.S.; Giovannenze, F.; De Angelis, G.; Murri, R.; Antonelli, M.; Fantoni, M.; De Pascale, G. Cefiderocol-containing regimens for the treatment of carbapenem-resistant A. baumannii ventilator-associated pneumonia: A propensity-weighted cohort study. JAC-Antimicrobial Resist. 2023, 5, dlad085. [Google Scholar] [CrossRef] [PubMed]
- Pascale, R.; Pascale, R.; Pasquini, Z.; Pasquini, Z.; Bartoletti, M.; Bartoletti, M.; Caiazzo, L.; Caiazzo, L.; Fornaro, G.; Fornaro, G.; et al. Cefiderocol treatment for carbapenem-resistant Acinetobacter baumannii infection in the ICU during the COVID-19 pandemic: A multicentre cohort study. JAC-Antimicrobial Resist. 2021, 3, dlab174. [Google Scholar] [CrossRef] [PubMed]
- Bavaro, D.F.; Papagni, R.; Belati, A.; Diella, L.; De Luca, A.; Brindicci, G.; De Gennaro, N.; Di Gennaro, F.; Romanelli, F.; Stolfa, S.; et al. Cefiderocol Versus Colistin for the Treatment of Carbapenem-Resistant Acinetobacter baumannii Complex Bloodstream Infections: A Retrospective, Propensity-Score Adjusted, Monocentric Cohort Study. Infect. Dis. Ther. 2023, 12, 2147–2163. [Google Scholar] [CrossRef] [PubMed]
- Calò, F.; Onorato, L.; De Luca, I.; Macera, M.; Monari, C.; Durante-Mangoni, E.; Massa, A.; Gentile, I.; Di Caprio, G.; Pagliano, P.; et al. Outcome of patients with carbapenem-resistant Acinetobacter baumannii infections treated with cefiderocol: A multicenter observational study. J. Infect. Public Health 2023, 16, 1485–1491. [Google Scholar] [CrossRef] [PubMed]
- Giannella, M.; Verardi, S.; Karas, A.; Hadi, H.A.; Dupont, H.; Soriano, A.; Henriksen, A.S.; Cooper, A.; Falcone, M.; Viale, P.; et al. Carbapenem-Resistant Acinetobacter spp Infection in Critically Ill Patients with Limited Treatment Options: A Descriptive Study of Cefiderocol Therapy During the COVID-19 Pandemic. Open Forum Infect. Dis. 2023, 10, ofad329. [Google Scholar] [CrossRef]
- Piccica, M.; Spinicci, M.; Botta, A.; Bianco, V.; Lagi, F.; Graziani, L.; Faragona, A.; Parrella, R.; Giani, T.; Bartolini, A.; et al. Cefiderocol use for the treatment of infections by carbapenem-resistant Gram-negative bacteria: An Italian multicentre real-life experience. J. Antimicrob. Chemother. 2023, 78, 2752–2761. [Google Scholar] [CrossRef]
- Inchai, J.; Pothirat, C.; Bumroongkit, C.; Limsukon, A.; Khositsakulchai, W.; Liwsrisakun, C. Prognostic factors associated with mortality of drug-resistant Acinetobacter baumannii ventilator-associated pneumonia. J. Intensiv. Care 2015, 3, 9. [Google Scholar] [CrossRef]
- Silva, D.; Lima, C.; Magalhães, V.; Baltazar, L.; Peres, N.; Caligiorne, R.; Moura, A.; Fereguetti, T.; Martins, J.; Rabelo, L.; et al. Fungal and bacterial coinfections increase mortality of severely ill COVID-19 patients. J. Hosp. Infect. 2021, 113, 145–154. [Google Scholar] [CrossRef]
- Ballouz, T.; Aridi, J.; Afif, C.; Irani, J.; Lakis, C.; Nasreddine, R.; Azar, E. Risk Factors, Clinical Presentation, and Outcome of Acinetobacter baumannii Bacteremia. Front. Cell. Infect. Microbiol. 2017, 7, 156. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.M.; Kim, C.-J.; Kim, S.E.; Park, K.-H.; Bae, J.Y.; Choi, H.J.; Jung, Y.; Lee, S.S.; Choe, P.G.; Park, W.B.; et al. Risk factors for early mortality in patients with carbapenem-resistant Acinetobacter baumannii bacteraemia. J. Glob. Antimicrob. Resist. 2022, 31, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Palermo, G.; Medaglia, A.A.; Pipitò, L.; Rubino, R.; Costantini, M.; Accomando, S.; Giammanco, G.M.; Cascio, A. Cefiderocol Efficacy in a Real-Life Setting: Single-Centre Retrospective Study. Antibiotics 2023, 12, 746. [Google Scholar] [CrossRef] [PubMed]
- Durante-Mangoni, E.; Andini, R.; Signoriello, S.; Cavezza, G.; Murino, P.; Buono, S.; De Cristofaro, M.; Taglialatela, C.; Bassetti, M.; Malacarne, P.; et al. Acute kidney injury during colistin therapy: A prospective study in patients with extensively-drug resistant Acinetobacter baumannii infections. Clin. Microbiol. Infect. 2016, 22, 984–989. [Google Scholar] [CrossRef] [PubMed]
- Wagenlehner, F.; Lucenteforte, E.; Pea, F.; Soriano, A.; Tavoschi, L.; Steele, V.R.; Henriksen, A.S.; Longshaw, C.; Manissero, D.; Pecini, R.; et al. Systematic review on estimated rates of nephrotoxicity and neurotoxicity in patients treated with polymyxins. Clin. Microbiol. Infect. 2021, 27, 671–686. [Google Scholar] [CrossRef] [PubMed]
- Falcone, M.; Tiseo, G.; Nicastro, M.; Leonildi, A.; Vecchione, A.; Casella, C.; Forfori, F.; Malacarne, P.; Guarracino, F.; Barnini, S.; et al. Cefiderocol as Rescue Therapy for Acinetobacter baumannii and Other Carbapenem-resistant Gram-negative Infections in Intensive Care Unit Patients. Clin. Infect. Dis. 2021, 72, 2021–2024. [Google Scholar] [CrossRef] [PubMed]
- Bavaro, D.F.; Belati, A.; Diella, L.; Stufano, M.; Romanelli, F.; Scalone, L.; Saracino, A. Cefiderocol-Based Combination Therapy for “Difficult-to-Treat” Gram-Negative Severe Infections: Real-Life Case Series and Future Perspectives. Antibiotics 2021, 10, 652. [Google Scholar] [CrossRef]
- Corcione, S.; De Benedetto, I.; Pinna, S.M.; Vita, D.; Lupia, T.; Montrucchio, G.; Brazzi, L.; De Rosa, F.G. Cefiderocol use in Gram negative infections with limited therapeutic options: Is combination therapy the key? J. Infect. Public Health 2022, 15, 975–979. [Google Scholar] [CrossRef]
- Gavaghan, V.; Miller, J.L.; Dela-Pena, J. Case series of cefiderocol for salvage therapy in carbapenem-resistant Gram-negative infections. Infection 2023, 51, 475–482. [Google Scholar] [CrossRef]
- Smoke, S.M.; Brophy, A.; Reveron, S.; Iovleva, A.; Kline, E.G.; Marano, M.; Miller, L.P.; Shields, R.K. Evolution and Transmission of Cefiderocol-Resistant Acinetobacter baumannii during an Outbreak in the Burn Intensive Care Unit. Clin. Infect. Dis. 2023, 76, e1261–e1265. [Google Scholar] [CrossRef]
- Wicky, P.-H.; Poiraud, J.; Alves, M.; Patrier, J.; D’humières, C.; Lê, M.; Kramer, L.; de Montmollin, É.; Massias, L.; Armand-Lefèvre, L.; et al. Cefiderocol Treatment for Severe Infections due to Difficult-to-Treat-Resistant Non-Fermentative Gram-Negative Bacilli in ICU Patients: A Case Series and Narrative Literature Review. Antibiotics 2023, 12, 991. [Google Scholar] [CrossRef] [PubMed]
- Karruli, A.; Massa, A.; Andini, R.; Marrazzo, T.; Ruocco, G.; Zampino, R.; Durante-Mangoni, E. Clinical efficacy and safety of cefiderocol for resistant Gram-negative infections: A real-life, single-centre experience. Int. J. Antimicrob. Agents 2023, 61, 106723. [Google Scholar] [CrossRef] [PubMed]
- Takemura, M.; Yamano, Y.; Matsunaga, Y.; Ariyasu, M.; Echols, R.; Nagata, T.D. 1266. Characterization of Shifts in Minimum Inhibitory Concentrations During Treatment with Cefiderocol or Comparators in the Phase 3 CREDIBLE-CR and APEKS-NP Studies. Open Forum Infect. Dis. 2020, 7, S649–S650. [Google Scholar] [CrossRef]
- E Choby, J.; Ozturk, T.; Satola, S.W.; Jacob, J.T.; Weiss, D.S. Widespread cefiderocol heteroresistance in carbapenem-resistant Gram-negative pathogens. Lancet Infect. Dis. 2021, 21, 597–598. [Google Scholar] [CrossRef] [PubMed]
- Karakonstantis, S.; Rousaki, M.; Kritsotakis, E.I. Cefiderocol: Systematic Review of Mechanisms of Resistance, Heteroresistance and In Vivo Emergence of Resistance. Antibiotics 2022, 11, 723. [Google Scholar] [CrossRef] [PubMed]
- Tamma, P.D.; Aitken, S.L.; Bonomo, R.A.; Mathers, A.J.; van Duin, D.; Clancy, C.J. Infectious Diseases Society of America 2023 Guidance on the Treatment of Antimicrobial Resistant Gram-Negative Infections. Clin Infect Dis. 2023, ciad428. [Google Scholar] [CrossRef] [PubMed]
- Oliva, A.; Ceccarelli, G.; De Angelis, M.; Sacco, F.; Miele, M.C.; Mastroianni, C.M.; Venditti, M. Cefiderocol for compassionate use in the treatment of complicated infections caused by extensively and pan-resistant Acinetobacter baumannii. J. Glob. Antimicrob. Resist. 2020, 23, 292–296. [Google Scholar] [CrossRef]
- Dagher, M.; Ruffin, F.; Marshall, S.; Taracila, M.; A Bonomo, R.; Reilly, R.; Fowler, V.G.; Thaden, J.T. Case Report: Successful Rescue Therapy of Extensively Drug-Resistant Acinetobacter baumannii Osteomyelitis with Cefiderocol. Open Forum Infect. Dis. 2020, 7, ofaa150. [Google Scholar] [CrossRef]
- Mabayoje, A.D.; NicFhogartaigh, C.; Cherian, B.P.; Tan, M.G.M.; Wareham, D.W. Compassionate use of cefiderocol for carbapenem-resistant Acinetobacter baumannii prosthetic joint infection. JAC-Antimicrobial Resist. 2021, 3, dlab109. [Google Scholar] [CrossRef]
- Kufel, W.D.; Abouelhassan, Y.; Steele, J.M.; Gutierrez, R.L.; Perwez, T.; Bourdages, G.; Nicolau, D.P. Plasma and cerebrospinal fluid concentrations of cefiderocol during successful treatment of carbapenem-resistant Acinetobacter baumannii meningitis. J. Antimicrob. Chemother. 2022, 77, 2737–2741. [Google Scholar] [CrossRef]
- Durand-Reville, T.F.; Guler, S.; Comita-Prevoir, J.; Chen, B.; Bifulco, N.; Huynh, H.; Lahiri, S.; Shapiro, A.B.; McLeod, S.M.; Carter, N.M.; et al. ETX2514 is a broad-spectrum b-lactamase inhibitor for the treatment of drug-resistant Gram-negative bacteria including Acinetobacter baumannii. Nat. Microbiol. 2017, 2, 17104. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, A.B. Kinetics of SUL hydrolysis by β-lactamases, and kinetics of β-lactamase inhibition by Sulbactam. Antimicrob. Agents Chemother. 2017, 61, e01612-17. [Google Scholar] [CrossRef] [PubMed]
- FDA Approves New Treatment for Pneumonia Caused by Certain Difficult-to-Treat Bacteria. News Release. 23 May 2023. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-new-treatment-pneumonia-caused-certain-difficult-treat-bacteria (accessed on 12 November 2023).
- Seifert, H.; Müller, C.; Stefanik, D.; Higgins, P.G.; Miller, A.; Kresken, M. In vitro activity of sulbactam/durlobactam against global isolates of carbapenem-resistant Acinetobacter baumannii. J. Antimicrob. Chemother. 2020, 75, 2616–2621. [Google Scholar] [CrossRef] [PubMed]
- McLeod, S.M.; Shapiro, A.B.; Moussa, S.H.; Johnstone, M.; McLaughlin, R.E.; de Jonge, B.L.M.; Miller, A.A. Frequency and mechanism of spontaneous resistance to SUL combined with the novel β-lactamase inhibitor ETX2514 in clinical isolates of Acinetobacter baumannii. Antimicrob. Agents Chemother. 2018, 62, e01576-17. [Google Scholar] [CrossRef] [PubMed]
- Kaye, K.S.; Kaye, K.S.; Shorr, A.F.; Shorr, A.F.; Wunderink, R.G.; Wunderink, R.G.; Du, B.; Du, B.; E Poirier, G.; E Poirier, G.; et al. Efficacy and safety of sulbactam–durlobactam versus colistin for the treatment of patients with serious infections caused by Acinetobacter baumannii–calcoaceticus complex: A multicentre, randomised, active-controlled, phase 3, non-inferiority clinical trial (ATTACK). Lancet Infect. Dis. 2023, 23, 1072–1084. [Google Scholar] [CrossRef] [PubMed]
- Zaidan, N.; Hornak, J.P.; Reynoso, D. Extensively Drug-Resistant Acinetobacter baumannii Nosocomial Pneumonia Successfully Treated with a Novel Antibiotic Combination. Antimicrob. Agents Chemother. 2021, 65, e0092421. [Google Scholar] [CrossRef] [PubMed]
- Holger, D.J.; Coyne, A.J.K.; Zhao, J.J.; Sandhu, A.; Salimnia, H.; Rybak, M.J. Novel Combination Therapy for Extensively Drug-Resistant Acinetobacter baumannii Necrotizing Pneumonia Complicated by Empyema: A Case Report. Open Forum Infect. Dis. 2022, 9, ofac092. [Google Scholar] [CrossRef]
- Tiseo, G.; Giordano, C.; Leonildi, A.; Riccardi, N.; Galfo, V.; Limongi, F.; Nicastro, M.; Barnini, S.; Falcone, M. Salvage therapy with sulbactam/durlobactam against cefiderocol-resistant Acinetobacter baumannii in a critically ill burn patient: Clinical challenges and molecular characterization. JAC-Antimicrobial Resist. 2023, 5, dlad078. [Google Scholar] [CrossRef]
- Durante-Mangoni, E.; Utili, R.; Zarrilli, R. Combination therapy in severe Acinetobacter baumannii infections: An update on the evidence to date. Futur. Microbiol. 2014, 9, 773–789. [Google Scholar] [CrossRef]
| Types of Infections | Outcomes | |||||||
|---|---|---|---|---|---|---|---|---|
| Clinical Cure at TOC | Clinical Failure at TOC | Microbiological Eradication at TOC | Microbiological Persistence at TOC | |||||
| FDC | BAT | FDC | BAT | FDC | BAT | FDC | BAT | |
| Nosocomial pneumonia | 20 (50) | 10 (53) | 16 (40) | 6 (32) | 9 (23) | 4 (21) | 8 (20) | 7 (37) |
| Bloodstream infections | 10 (43) | 6 (43) | 9 (39) | 7 (50) | 7 (30) | 4 (29) | 3 (13) | 2 (14) |
| Complicated urinary tract infections | 12 (71) | 3 (60) | 2 (12) | 1 (20) | 9 (53) | 1 (20) | 5 (29) | 1 (20) |
| Overall | 42 (53) | 19 (50) | 27 (34) | 14 (37) | 25 (31) | 9 (24) | 16 (20) | 10 (26) |
| Author | Study Design | Site of Infection and Pathogens | No. of Patients | Treatment | Clinical Outcome and Adverse Event (AKI) | Microbiological Outcome | Mortality |
|---|---|---|---|---|---|---|---|
| Falcone et al. [43] | Single-center observational retrospective study | CRAB: BSI 63.7% VAP 28.5% Other sites 8.1% | 124 | FDC 47 (37.9%): 15 (31.9%) monotherapy 32 (69.1%) combination | Clinical cure-NA | Microbiological failure FDC 17.4% Colistin 6.8% | All infections 30-day mortality FDC 34% Colistin 55.8% BSI 14-day mortality: FDC 7.4% Colistin 42.3% 30-day mortality: FDC 25.9% Colistin 57.7% VAP no difference [Septic shock, SOFA score associated with mortality] |
| colistin-based regimens 77 (62.1%): 12 (15.6%) monotherapy 55 (84.4%) combination | Adverse event FDC 2.1% Colistin 21.1% | ||||||
| Russo et al. [44] | Single-center, retrospective, observational study | VAP and bacteremia due to CRAB in COVID-19 in ICU | 73 | FDC 19 (26%) 100% in combination | NA | Microbiological clearance higher in survivors | FDC regimen and FDC+ fosfomycin associated with survival compared to colistin |
| colistin-based regimen 54 (74%) 12 (22.2%) monotherapy 32 (77.8%) combination | |||||||
| Dalfino et al. [45] | Single-center prospective observational study | VAP due to CRAB in COVID-19 and non-COVID-19 | 90 | FDC 40 patients 19 (47.5%) monotherapy 21 (52.5%) + fosfomycin | Clinical failure FDC 25% Colistin 48% | Microbiological failure FDC 30% Colistin 60% | 14-day mortality FDC 10% Colistin 38% |
| colistin 50 patients all combination Inhaled colistin in both groups | AKI FDC 45% Colistin 47% | ||||||
| Mazzitelli et al. [46] | Single-center, retrospective, observational study | CRAB: BSI 53 (47.7%) VAP 58 (52.3%) | 111 | FDC 60 patients 50% monotherapy | Clinical cure FDC 73% Colistin 67% FDC Monotherapy 76.7% Combination 70% | Microbiological eradication FDC 43% Colistin 41% FDC Monotherapy 50% Combination 36.7% | Death FDC 51% Colistin 37% FDC Monotherapy 33.3% Combination 53.3% |
| colistin 51 patients all combination | AKI FDC 10% Colistin 25.5% | ||||||
| Pascale et al. [48] | Multi-center retrospective observational | CRAB BSI 58% LRTI 41% | 107 | FDC 42 patients monotherapy all cases | Clinical cure 14 days FDC 40% Colistin 36% | Microbiological cure 14 days FDC 28% Colistin 21% | 28-day mortality FDC 55% Colistin 58% (High SOFA score risk factor for mortality) |
| colistin 65 patients 82% combination | AKI FDC 9.5% Colistin 9.2% | ||||||
| Rando et al. [47] | Single-center, prospective, observational | CRAB VAP | 121 | 55 FDC monotherapy 21.8% 66 other | Clinical cure-NA | Microbiological failure FDC 53% Other 31% | 28-day mortality FDC 44% Other 67% (mortality higher in septic shock and higher SOFA score) |
| AKI FDC 9.1% Other 17% | |||||||
| Bavaro et al. [49] | Single-center, retrospective, observational | CRAB-BSI | 118 | −43 FDC combination 63% | Clinical cure FDC 60.5% Colistin 41.3% | NA | 30-day all-cause mortality FDC 40% Colistin 59% |
| −75 colistin combination 96% | Adverse event FDC 2% Colistin 16% |
| Study | Study Design | Type Of Infection and Pathogens | Patients | Clinical Outcome and Adverse Events | Microbiological Outcome | Mortality |
|---|---|---|---|---|---|---|
| Clinical studies | ||||||
| Palermo et al. [57] | Single-center, retrospective observational | CR GN For CRAB: BSI 48.4% HAP 41.9% SSTI 25.8% cIAIs 19.3% cUTI 9.7% Other 12.8% | 41 total patients: 31 CRAB | CRAB: Clinical cure at EOT 64.5% Adverse events 4.9% | CRAB: Microbiological eradication at EOT 80.6% | CRAB: 30-day mortality 35.5% VAP 61.5% BSI 46.7% |
| Calò et al. [50] | Multi-center, retrospective/prospective, observational study | CRAB All types of infections (mostly): BSI 45% Respiratory 40% | 38 patients | Clinical failure at EOT 32.5% Monotherapy 27.6% Combination 45.5% (non-significant) Adverse event none | Microbiological failure at EOT 10% Monotherapy 13.8% Combination 0 (non-significant) | 30-day mortality 47.5% Monotherapy: 48.3% Combination 45.5% |
| Giannella et al. [51] | Multi-center, retrospective observational study | Acinetobacter spp: Respiratory 65.3% BSI 26.5% Other 8.2% | 147 patients 146 A. baumannii 1 other Acinetobacter | Resolution of infection 39.5% Improved symptoms 12.2% Failure 38.1% Clinical success: BSI 52.2%-75% Respiratory 45.8% Monotherapy 61.2% Combination 49% Adverse event 4.8% | NA | 28-day mortality Overall 51% Monotherapy 53.1% Combination 40.8% Survival: septic shock 24.3% Without Septic shock 60.7% |
| Piccica et al. [52] | Multi-center, retrospective observational | CR GN LRTI 57% IAI 9.2% UTI 8.5% BSI 13.4% ABSSSI 6.3% OTHERS 2.1% | 142 patients: 70 monotherapy 72 combination (89 A. baumannii) | Clinical cure-NA AKI 38% | Microbiological eradication All pathogens 48.9% Monotherapy 45.8% Combination 52.3% | Survived All pathogens 36.6% Monotherapy 32.9% Combination 40.3% Mortality higher in septic shock (Survival in A. baumannii 62.9%) |
| CASE SERIES | ||||||
| Bavaro et al. [61] | Case series | XDR GN For CRAB: BSI 70% BSI+ VAP 10% VAP 10% Perihepatic abscess 10% | 13 patients: CRAB in 10 | CRAB: Clinical cure 70% No adverse event | CRAB: Microbiological eradication 100% | CRAB: Mortality 30% |
| Corcione et al. [62] | Case series | CR GN VAP + BSI 61.2% BSI 16.7% VAP 11.1% Other 11.1% | 18 patients: CRAB in 16: 4 monotherapy 11 combination | All pathogens: Clinical cure 66.7% Monotherapy 75% Combination 64.29% No serious adverse event | All pathogens: Microbiological failure 22.2% Monotherapy 25% Combination 21.43% | All pathogens: 30-day mortality 27.8% Monotherapy 25% Combination 28.57% |
| Gavaghan et al. [63] | Case series | CR GN For CRAB: Pneumonia 10 UTI 1 Pneumonia + BSI 2 Wound + BSI 1 | 24 patients: A. baumannii in 14 | CRAB: Clinical success 35.7% No adverse event | NA | CRAB: Mortality 42.8% 62% of isolates susceptible to FDC |
| Falcone et al. [60] | Case series | CR GN For CRAB: 6 patients BSI 2 patients VAP | 10 patients A. baumannii in 8: 7 Monotherapy 1 Combination | CRAB: Clinical success 62.5% No severe adverse event | CRAB: Microbiological failure 25% | CRAB: Mortality 12.5% |
| Wicky et al. [65] | Case series | DTR GN For CRAB: Mostly VAP | 16 patients CRAB in 9: 1 Monotherapy 8 Combination | CRAB: Clinical cure 77.8% Adverse events 66.6% 66.7% (mostly) encephalopathy | CRAB: Death 22.2% | |
| Smoke et al. [64] | Case series | CRAB burn patients 5 BSI 4 BSI/VAP 1 VAP 1 VAT | 11 patients: 3 Combination | Clinical cure 36% (FDC resistance 60% of tested isolates) | Microbiological failure 90 days 88% of 8 patients who completed initial treatment | Mortality 27.3% |
| Case Report | Patient | Comorbidities and History Prior to A. baumannii Isolation | A. baumannii Isolations and Clinical Characteristics | Prior Treatment Failure for A. baumannii Infection | Treatment Success | MIC | Outcome |
|---|---|---|---|---|---|---|---|
| Zaidan et al. [81] | 55-year-old female | Comorbidities: Diabetes mellitus hypertension gastric bypass for obesity History prior to A. baumannii isolation: COVID-19 pneumonia with RF, mechanical ventilation → clinical improvement, extubation | During hospitalization, after improvement of COVID-19 pneumonia: → refractory hypoxia, intubation, vasopressor support → respiratory culture PDR A. baumannii Wild-type P. aeruginosa | Empiric meropenem+vancomycin After AST results meropenem + ampicillin/SUL | SUL-DUR 2 gr q6h + FDC 2 gr q8h | SUL-DUR 4 mg/L FDC 0.5 mg/L | Improvement after 72 h 14-day course treatment → tracheostomy- → discharged long-term care facility → discharged home |
| Holger et al. [82] | 50-year-old male | Pulmonary embolism + infarction → intubation, thoracotomy, partial decortication | Bronchoalveolar lavage A. baumannii meropenem S → thoracotomy, RLL resection (abscess), decortication → Pleural tissue A. baumannii I to colistin → 45 days later, persistence of A. baumannii which developed resistance to FDC, eravacycline | Empiric piperacillin/tazobactam + vancomycin After AST results meropenem tigecycline colistin + meropenem FDC eravacycline FDC + tigecycline | SUL-DUR 2 gr q8 + meropenem 1 gr q6 | SUL-DUR MIC 8 mg/L alone 4 mg/L with meropenem | 13-day treatment Clinical cure Discharged home |
| Tiseo et al. [83] | Young female | Burn injury 45% of total body surface area → intubated | Central line BSI CRAB R to FDC, S to colistin → skin lesion CRAB + CR P. aeruginosa → BAL: CRAB R to FDC and colistin + CR P. aeruginosa | Colistin + tigecycline | SUL-DUR + colistin (for P. aeruginosa) | SUL-DUR MIC 1.5 mg/L | 12-day regimen Clinical improvement Microbiological eradication of CRAB Alive at 30 days |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karruli, A.; Migliaccio, A.; Pournaras, S.; Durante-Mangoni, E.; Zarrilli, R. Cefiderocol and Sulbactam-Durlobactam against Carbapenem-Resistant Acinetobacter baumannii. Antibiotics 2023, 12, 1729. https://doi.org/10.3390/antibiotics12121729
Karruli A, Migliaccio A, Pournaras S, Durante-Mangoni E, Zarrilli R. Cefiderocol and Sulbactam-Durlobactam against Carbapenem-Resistant Acinetobacter baumannii. Antibiotics. 2023; 12(12):1729. https://doi.org/10.3390/antibiotics12121729
Chicago/Turabian StyleKarruli, Arta, Antonella Migliaccio, Spyros Pournaras, Emanuele Durante-Mangoni, and Raffaele Zarrilli. 2023. "Cefiderocol and Sulbactam-Durlobactam against Carbapenem-Resistant Acinetobacter baumannii" Antibiotics 12, no. 12: 1729. https://doi.org/10.3390/antibiotics12121729
APA StyleKarruli, A., Migliaccio, A., Pournaras, S., Durante-Mangoni, E., & Zarrilli, R. (2023). Cefiderocol and Sulbactam-Durlobactam against Carbapenem-Resistant Acinetobacter baumannii. Antibiotics, 12(12), 1729. https://doi.org/10.3390/antibiotics12121729










