Impact of the COVID-19 Pandemic on Epidemiology of Antibiotic Resistance in an Intensive Care Unit (ICU): The Experience of a North-West Italian Center
Abstract
:1. Introduction
2. Materials and Methods
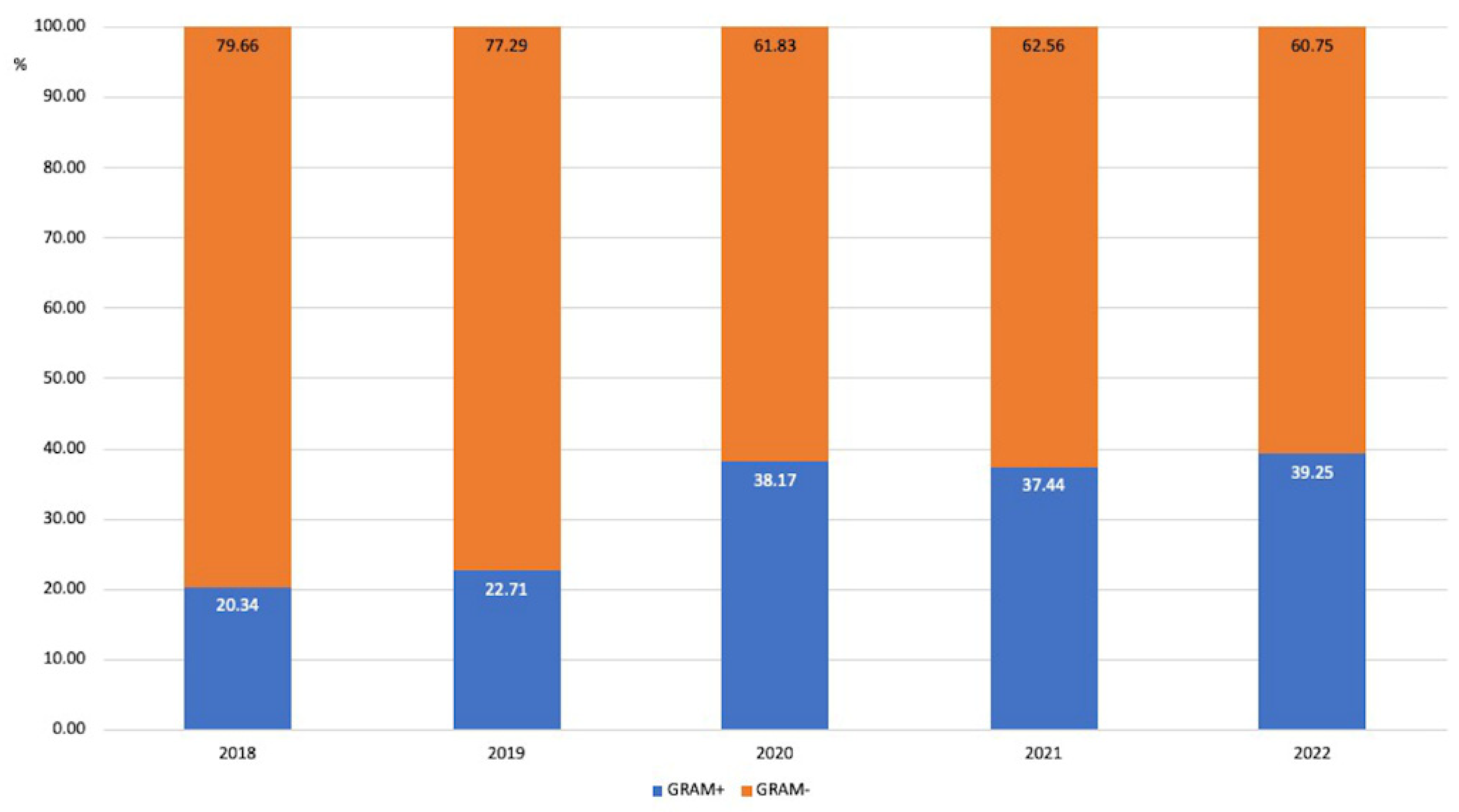
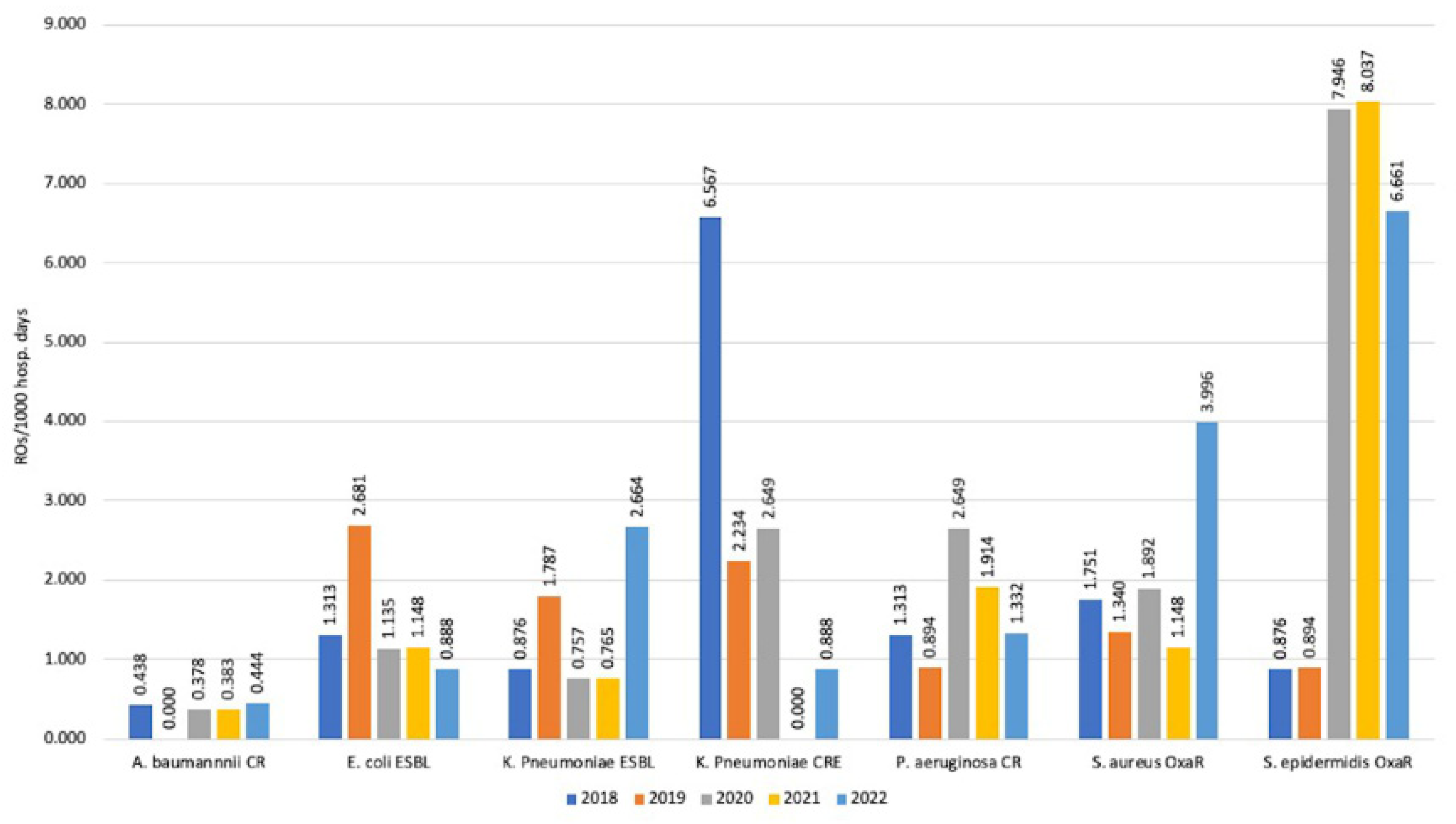
3. Results
3.1. Oxacillin Resistance
3.1.1. S. aureus
3.1.2. Coagulase-Negative Staphylococci (CoNS)
3.2. Carbapenem Resistance (CR)
3.2.1. Enterobacterales
3.2.2. Nonfermenting Gram-Negative Microorganisms
3.2.3. K. pneumoniae
3.3. Extended-Spectrum Beta-Lactamase (ESBL)
Enterobacterales
3.4. Incidence Rates
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sartini, M.; Del Puente, F.; Oliva, M.; Carbone, A.; Blasi Vacca, E.; Parisini, A.; Boni, S.; Bobbio, N.; Feasi, M.; Battistella, A.; et al. Riding the COVID Waves: Clinical Trends, Outcomes, and Remaining Pitfalls of the SARS-CoV-2 Pandemic: An Analysis of Two High-Incidence Periods at a Hospital in Northern Italy. J. Clin. Med. 2021, 10, 5239. [Google Scholar] [CrossRef]
- Giacobbe, D.R.; Battaglini, D.; Ball, L.; Brunetti, I.; Bruzzone, B.; Codda, G.; Crea, F.; De Maria, A.; Dentone, C.; Di Biagio, A.; et al. Bloodstream infections in critically ill patients with COVID-19. Eur. J. Clin. Investig. 2020, 50, e13319. [Google Scholar] [CrossRef]
- Bentivegna, E.; Luciani, M.; Arcari, L.; Santino, I.; Simmaco, M.; Martelletti, P. Reduction of Multidrug-Resistant (MDR) Bacterial Infections during the COVID-19 Pandemic: A Retrospective Study. Int. J. Environ. Res. Public Health 2021, 18, 1003. [Google Scholar] [CrossRef]
- Grasselli, G.; Scaravilli, V.; Mangioni, D.; Scudeller, L.; Alagna, L.; Bartoletti, M.; Bellani, G.; Biagioni, E.; Bonfanti, P.; Bottino, N.; et al. Hospital-Acquired Infections in Critically Ill Patients With COVID-19. Chest 2021, 160, 454–465. [Google Scholar] [CrossRef]
- Cusumano, J.A.; Dupper, A.C.; Malik, Y.; Gavioli, E.M.; Banga, J.; Berbel Caban, A.; Nadkarni, D.; Obla, A.; Vasa, C.V.; Mazo, D.; et al. Staphylococcus aureus Bacteremia in Patients Infected With COVID-19: A Case Series. Open Forum Infect. Dis. 2020, 7, ofaa518. [Google Scholar] [CrossRef]
- Conway Morris, A.; Kohler, K.; De Corte, T.; Ercole, A.; De Grooth, H.J.; Elbers, P.W.G.; Povoa, P.; Morais, R.; Koulenti, D.; Jog, S.; et al. COVID investigators Co-infection and ICU-acquired infection in COIVD-19 ICU patients: A secondary analysis of the UNITE-COVID data set. Crit. Care 2022, 26, 236. [Google Scholar] [CrossRef]
- Langford, B.J.; So, M.; Leung, V.; Raybardhan, S.; Lo, J.; Kan, T.; Leung, F.; Westwood, D.; Daneman, N.; MacFadden, D.R.; et al. Predictors and microbiology of respiratory and bloodstream bacterial infection in patients with COVID-19: Living rapid review update and meta-regression. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2022, 28, 491–501. [Google Scholar] [CrossRef]
- Montrucchio, G.; Corcione, S.; Lupia, T.; Shbaklo, N.; Olivieri, C.; Poggioli, M.; Pagni, A.; Colombo, D.; Roasio, A.; Bosso, S.; et al. The Burden of Carbapenem-Resistant Acinetobacter baumannii in ICU COVID-19 Patients: A Regional Experience. J. Clin. Med. 2022, 11, 5208. [Google Scholar] [CrossRef]
- Kinross, P.; Gagliotti, C.; Merk, H.; Plachouras, D.; Monnet, D.L.; Högberg, L.D.; EARS-Net Study Group; EARS-Net Study Group Participants. Large increase in bloodstream infections with carbapenem-resistant Acinetobacter species during the first 2 years of the COVID-19 pandemic, EU/EEA, 2020 and 2021. Euro Surveill. Bull. Eur. Sur Les Mal. Transm. = Eur. Commun. Dis. Bull. 2022, 27, 2200845. [Google Scholar] [CrossRef]
- Buetti, N.; Tabah, A.; Loiodice, A.; Ruckly, S.; Aslan, A.T.; Montrucchio, G.; Cortegiani, A.; Saltoglu, N.; Kayaaslan, B.; Aksoy, F.; et al. Different epidemiology of bloodstream infections in COVID-19 compared to non-COVID-19 critically ill patients: A descriptive analysis of the Eurobact II study. Crit. Care 2022, 26, 319. [Google Scholar] [CrossRef]
- Petazzoni, G.; Bellinzona, G.; Merla, C.; Corbella, M.; Monzillo, V.; Samuelsen, Ø.; Corander, J.; Sassera, D.; Gaiarsa, S.; Cambieri, P. The COVID-19 Pandemic Sparked Off a Large-Scale Outbreak of Carbapenem-Resistant Acinetobacter baumannii from the Endemic Strains at an Italian Hospital. Microbiol. Spectr. 2023, 11, e0450522. [Google Scholar] [CrossRef]
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 13.0, 2023. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_13.0_Breakpoint_Tables.pdf (accessed on 7 March 2023).
- Kariyawasam, R.M.; Julien, D.A.; Jelinski, D.C.; Larose, S.L.; Rennert-May, E.; Conly, J.M.; Dingle, T.C.; Chen, J.Z.; Tyrrell, G.J.; Ronksley, P.E.; et al. Antimicrobial resistance (AMR) in COVID-19 patients: A systematic review and meta-analysis (November 2019-June 2021). Antimicrob. Resist. Infect. Control 2022, 11, 45. [Google Scholar] [CrossRef]
- Langford, B.J.; Soucy, J.R.; Leung, V.; So, M.; Kwan, A.T.H.; Portnoff, J.S.; Bertagnolio, S.; Raybardhan, S.; MacFadden, D.R.; Daneman, N. Antibiotic resistance associated with the COVID-19 pandemic: A systematic review and meta-analysis. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2023, 29, 302–309. [Google Scholar] [CrossRef]
- Abubakar, U.; Al-Anazi, M.; Alanazi, Z.; Rodríguez-Baño, J. Impact of COVID-19 pandemic on multidrug resistant gram positive and gram negative pathogens: A systematic review. J. Infect. Public Health 2023, 16, 320–331. [Google Scholar] [CrossRef]
- Segala, F.V.; Pafundi, P.C.; Masciocchi, C.; Fiori, B.; Taddei, E.; Antenucci, L.; De Angelis, G.; Guerriero, S.; Pastorino, R.; Damiani, A.; et al. Incidence of bloodstream infections due to multidrug-resistant pathogens in ordinary wards and intensive care units before and during the COVID-19 pandemic: A real-life, retrospective observational study. Infection 2023, advance online publication, 1–9. [Google Scholar] [CrossRef]
- Punjabi, C.D.; Madaline, T.; Gendlina, I.; Chen, V.; Nori, P.; Pirofski, L.A. Prevalence of methicillin-resistant Staphylococcus aureus (MRSA) in respiratory cultures and diagnostic performance of the MRSA nasal polymerase chain reaction (PCR) in patients hospitalized with coronavirus disease 2019 (COVID-19) pneumonia. Infect. Control Hosp. Epidemiol. 2021, 42, 1156–1158. [Google Scholar] [CrossRef]
- Perez, S.; Innes, G.K.; Walters, M.S.; Mehr, J.; Arias, J.; Greeley, R.; Chew, D. Increase in Hospital-Acquired Carbapenem-Resistant Acinetobacter baumannii Infection and Colonization in an Acute Care Hospital During a Surge in COVID-19 Admissions—New Jersey, February-July 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1827–1831. [Google Scholar] [CrossRef]
- Temperoni, C.; Caiazzo, L.; Barchiesi, F. High Prevalence of Antibiotic Resistance among Opportunistic Pathogens Isolated from Patients with COVID-19 under Mechanical Ventilation: Results of a Single-Center Study. Antibiotics 2021, 10, 1080. [Google Scholar] [CrossRef]
- Gajic, I.; Jovicevic, M.; Popadic, V.; Trudic, A.; Kabic, J.; Kekic, D.; Ilic, A.; Klasnja, S.; Hadnadjev, M.; Popadic, D.J.; et al. The emergence of multi-drug-resistant bacteria causing healthcare-associated infections in COVID-19 patients: A retrospective multi-centre study. J. Hosp. Infect. 2023, 137, 1–7. [Google Scholar] [CrossRef]
- Tiri, B.; Sensi, E.; Marsiliani, V.; Cantarini, M.; Priante, G.; Vernelli, C.; Martella, L.A.; Costantini, M.; Mariottini, A.; Andreani, P.; et al. Antimicrobial Stewardship Program, COVID-19, and Infection Control: Spread of Carbapenem-Resistant Klebsiella Pneumoniae Colonization in ICU COVID-19 Patients. What Did Not Work? J. Clin. Med. 2020, 9, 2744. [Google Scholar] [CrossRef]
- Lemenand, O.; Coeffic, T.; Thibaut, S.; Colomb Cotinat, M.; Caillon, J.; Birgand, G.; Clinical Laboratories of PRIMO Network. Nantes, France. Decreasing proportion of extended-spectrum beta-lactamase among E. coli infections during the COVID-19 pandemic in France. J. Infect. 2021, 83, 664–670. [Google Scholar] [CrossRef] [PubMed]




| All (Number of Patients = 791) | Non-ROs (Number of Patients = 730) | ROs (Number of Patients = 180) | |
|---|---|---|---|
| Age (years) | |||
| Mean ± SD | 68.63 ± 13.61 | 68.64 ± 13.94 | 68.56 ± 12.06 |
| Median | 71 | 71 | 69 |
| Gender | |||
| Female | 181 (39.78%) | 158 (42.36%) | 23 (28.05%) |
| Male | 274 (60.22%) | 215 (57.64%) | 59 (71.95%) |
| Number of isolates | 1021 | 801 | 220 |
| Year | BRA/BAL | Blood Culture | CVC- Blood Culture | Urine | Others |
|---|---|---|---|---|---|
| 2018 | 105 (62.88%) | 14 (8.38%) | 7 (4.19%) | 28 (16.77%) | 13 (7.78%) |
| 2019 | 121 (57.90%) | 17 (8.13%) | 7 (3.35%) | 43 (20.57%) | 21 (10.05%) |
| 2020 | 152 (66.08%) | 14 (6.09%) | 16 (6.96%) | 37 (16.09%) | 11 (4.78%) |
| 2021 | 126 (58.60%) | 19 (8.84%) | 15 (6.98%) | 36 (16.74%) | 19 (8.84%) |
| 2022 | 97 (48.50%) | 28 (14.00%) | 8 (4.00%) | 38 (19.00%) | 29 (14.50%) |
| Non-ROs (%) | ROs (%) | Patients (N) | |
|---|---|---|---|
| 2018 | 142 (80.23) | 35 (19.77) | 375 |
| 2019 | 199 (86.90) | 30 (13.10) | 371 |
| 2020 | 179 (74.27) | 62 (25.73) | 337 |
| 2021 | 174 (79.45) | 45 (20.55) | 309 |
| 2022 | 165 (77.10) | 49 (22.90) | 287 |
| Non-ROs/1000 pt Days | ROs/1000 pt Days | Hospitalization Days | |
|---|---|---|---|
| 2018 | 62.172 | 15.324 | 2284 |
| 2019 | 88.919 | 13.405 | 2238 |
| 2020 | 67.726 | 23.458 | 2643 |
| 2021 | 66.590 | 17.222 | 2613 |
| 2022 | 73.268 | 21.758 | 2252 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parisini, A.; Boni, S.; Vacca, E.B.; Bobbio, N.; Del Puente, F.; Feasi, M.; Prinapori, R.; Lattuada, M.; Sartini, M.; Cristina, M.L.; et al. Impact of the COVID-19 Pandemic on Epidemiology of Antibiotic Resistance in an Intensive Care Unit (ICU): The Experience of a North-West Italian Center. Antibiotics 2023, 12, 1278. https://doi.org/10.3390/antibiotics12081278
Parisini A, Boni S, Vacca EB, Bobbio N, Del Puente F, Feasi M, Prinapori R, Lattuada M, Sartini M, Cristina ML, et al. Impact of the COVID-19 Pandemic on Epidemiology of Antibiotic Resistance in an Intensive Care Unit (ICU): The Experience of a North-West Italian Center. Antibiotics. 2023; 12(8):1278. https://doi.org/10.3390/antibiotics12081278
Chicago/Turabian StyleParisini, Andrea, Silvia Boni, Elisabetta Blasi Vacca, Nicoletta Bobbio, Filippo Del Puente, Marcello Feasi, Roberta Prinapori, Marco Lattuada, Marina Sartini, Maria Luisa Cristina, and et al. 2023. "Impact of the COVID-19 Pandemic on Epidemiology of Antibiotic Resistance in an Intensive Care Unit (ICU): The Experience of a North-West Italian Center" Antibiotics 12, no. 8: 1278. https://doi.org/10.3390/antibiotics12081278
APA StyleParisini, A., Boni, S., Vacca, E. B., Bobbio, N., Del Puente, F., Feasi, M., Prinapori, R., Lattuada, M., Sartini, M., Cristina, M. L., Usiglio, D., & Pontali, E. (2023). Impact of the COVID-19 Pandemic on Epidemiology of Antibiotic Resistance in an Intensive Care Unit (ICU): The Experience of a North-West Italian Center. Antibiotics, 12(8), 1278. https://doi.org/10.3390/antibiotics12081278







