High and Low Dosage of Vancomycin in Polymethylmethacrylate Cements: Efficacy and Mechanical Properties
Abstract
:1. Introduction
2. Results
2.1. ISO Compression Strength
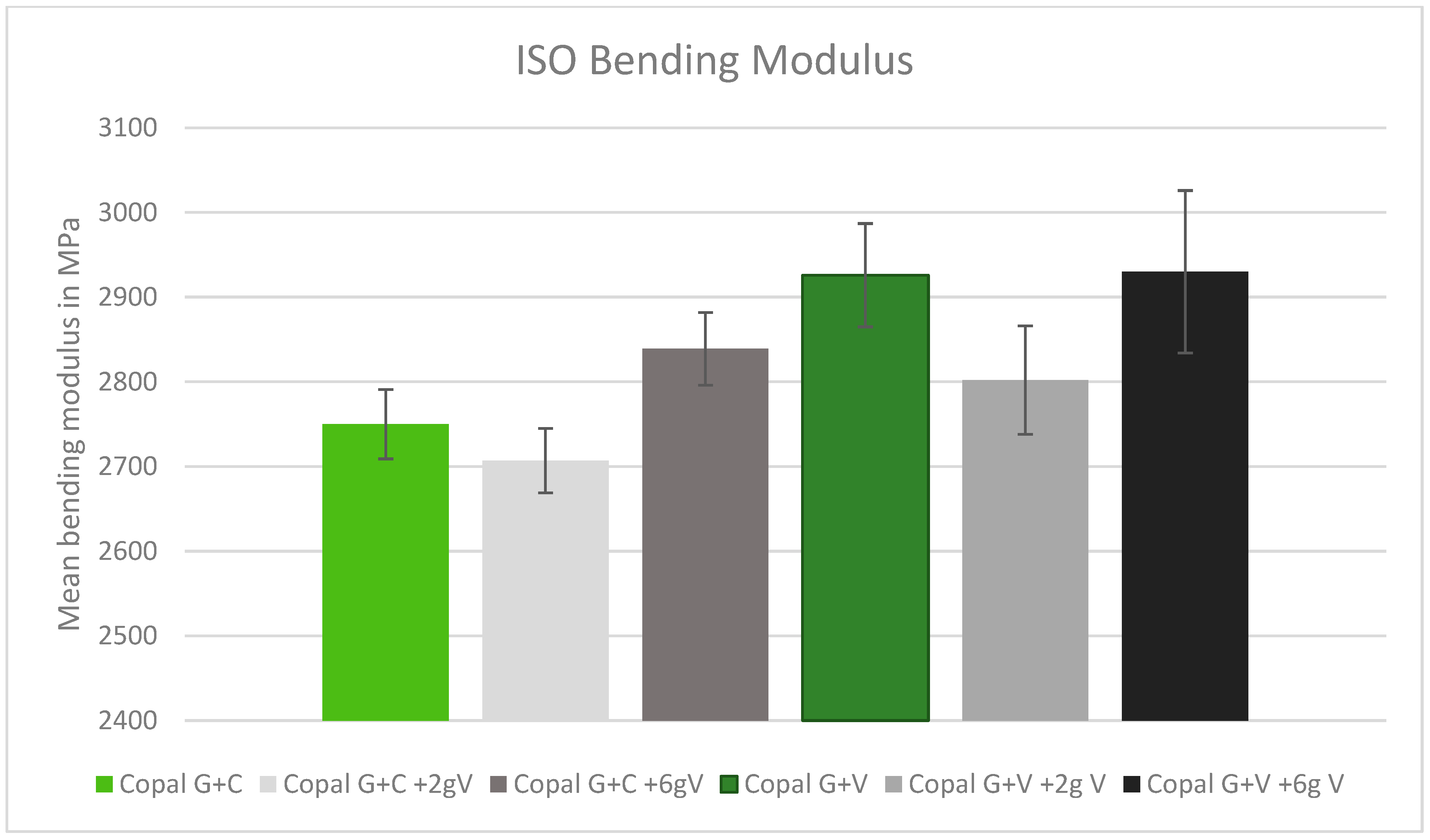
2.2. ISO Bending Modulus
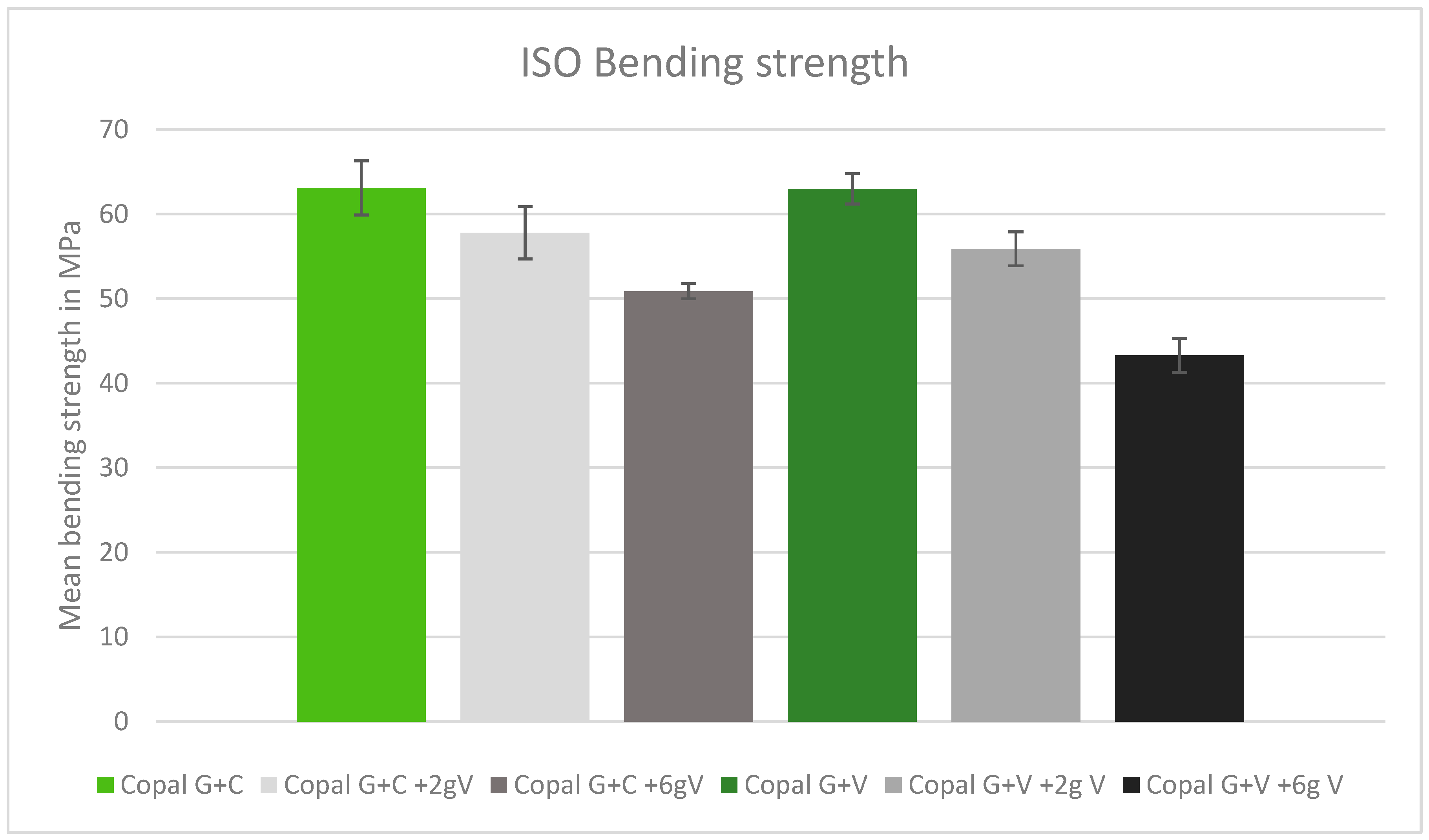
2.3. ISO Bending Strength
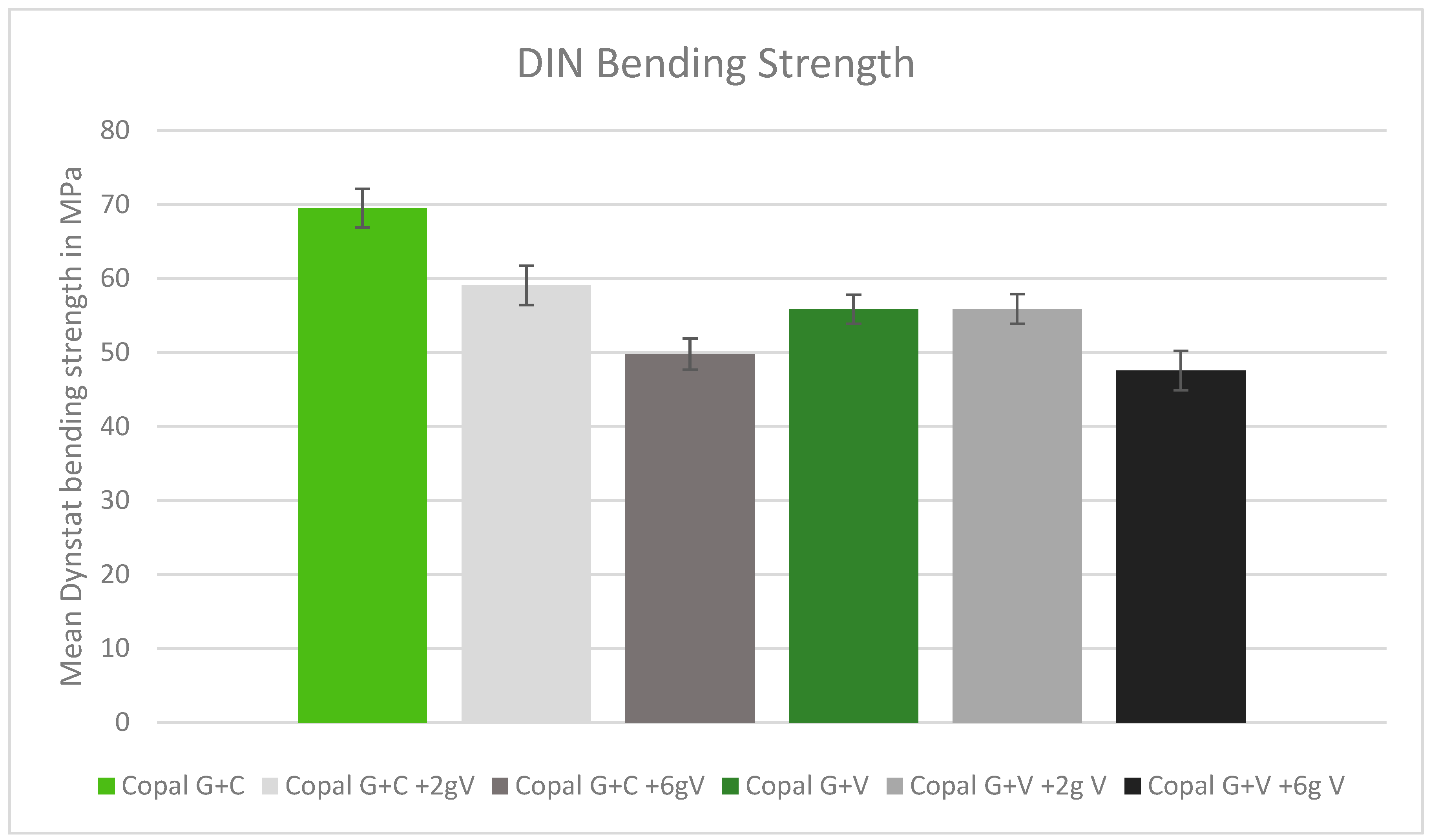
2.4. DIN Bending Strength
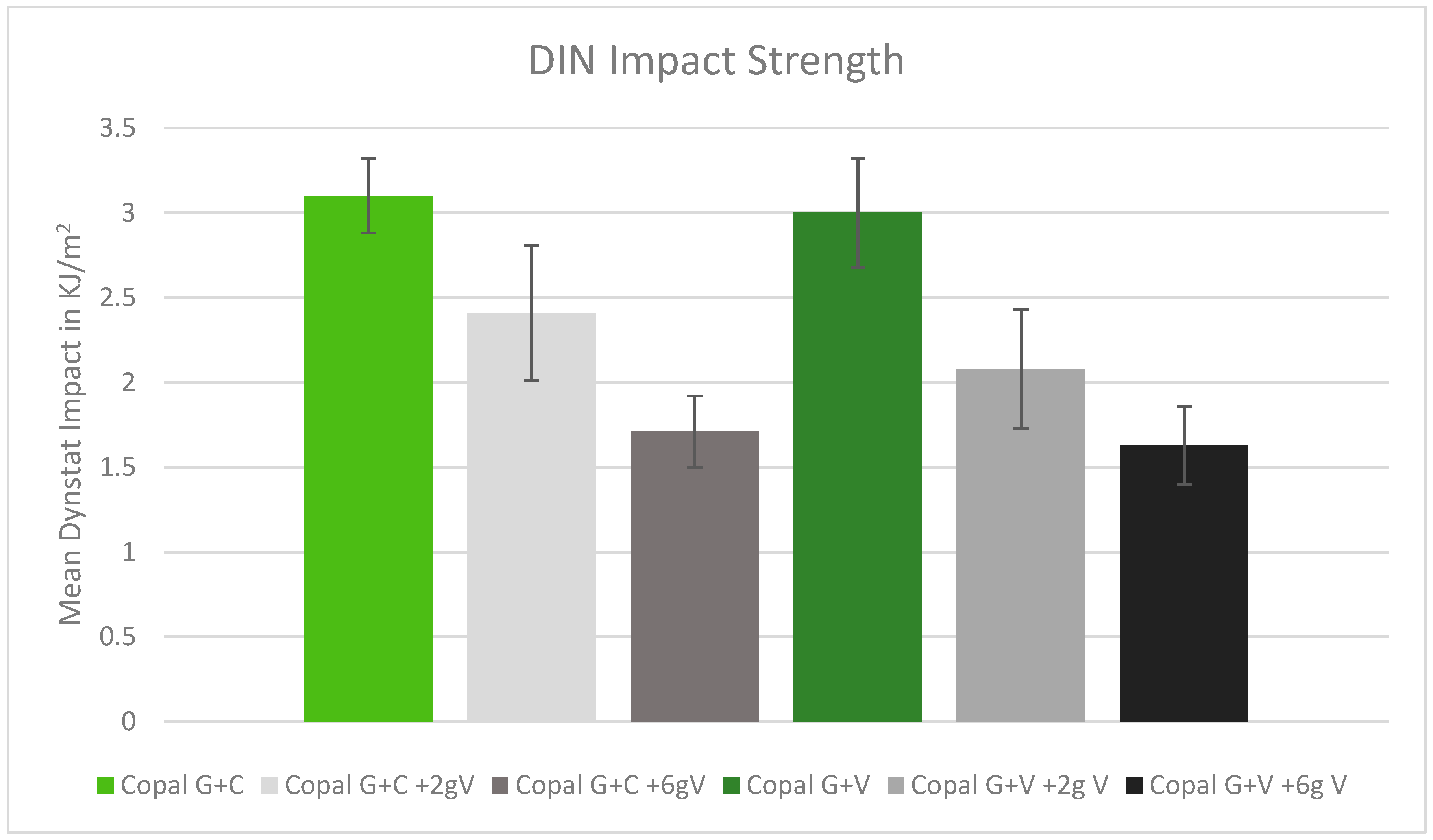
2.5. DIN Impact Strength
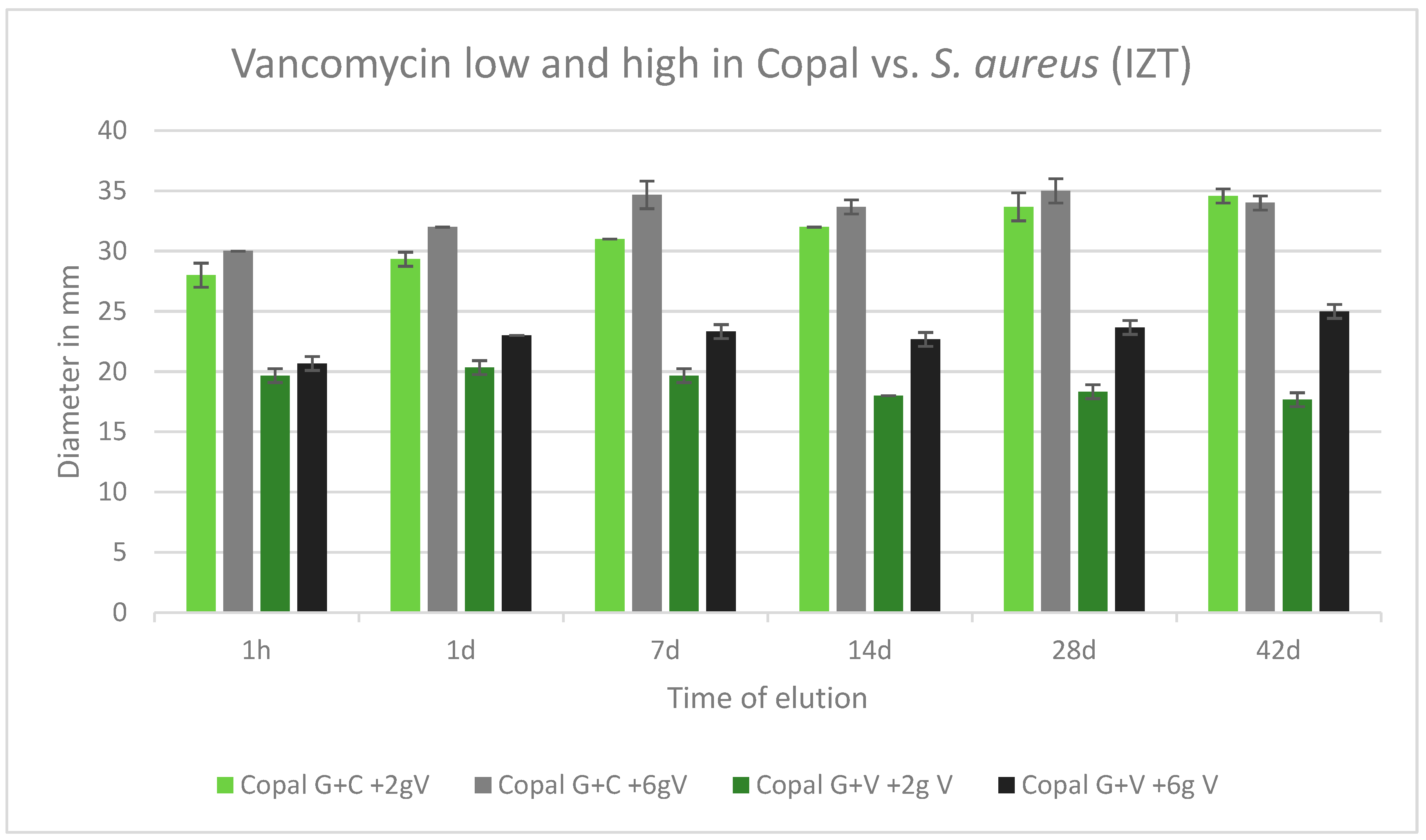
2.6. Efficacy against Staphylococcus aureus
2.7. Efficacy against E. faecalis
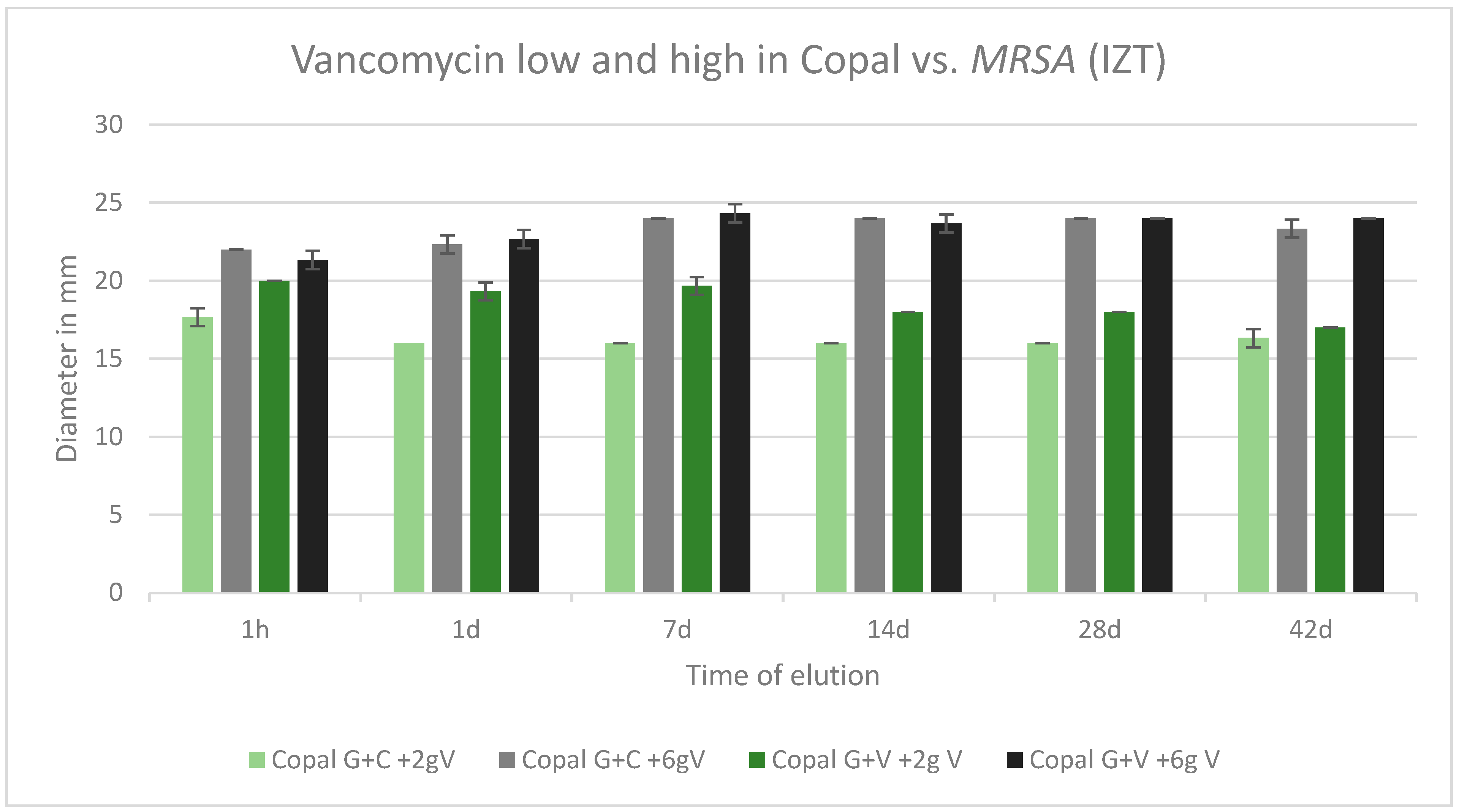
2.8. Efficacy against MRSA
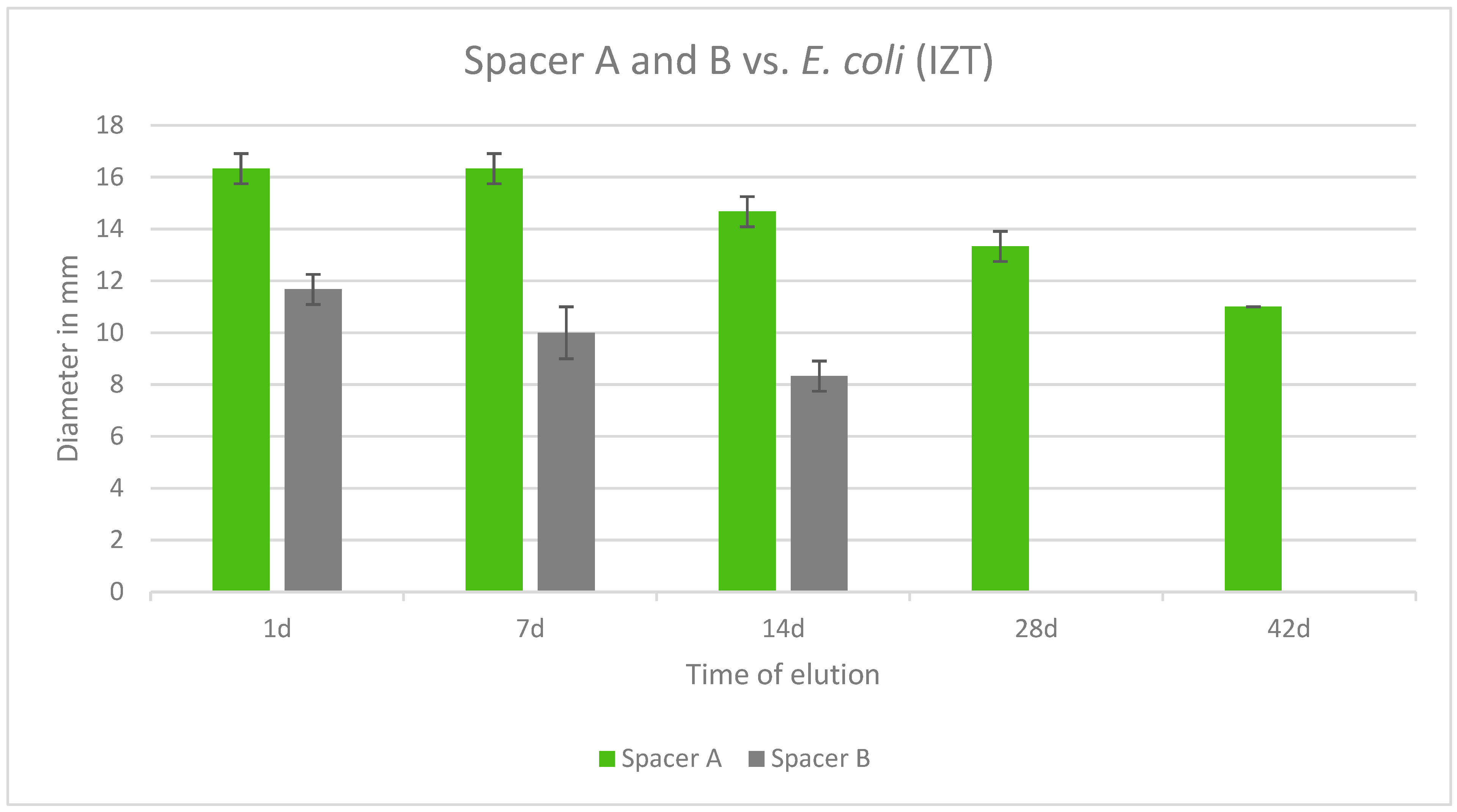
2.9. Prefabricated Spacers with Gentamicin
3. Discussion
3.1. Microbiology
3.2. Biomechanics
4. Methodology
4.1. Mechanical Tests
4.1.1. ISO 5833 Compressive Strength
4.1.2. ISO 5833 Bending Modulus and Bending Strength
4.1.3. DIN Bending and DIN Impact Strength according to DIN 53435
4.2. Spacers
4.3. Microbiological Tests
4.3.1. Preparation
4.3.2. Bacteria Preparation
4.3.3. Spacer Preparation and Eluate Extraction
4.3.4. Inhibition Zone Test
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bhandari, M.; Schemitsch, E.; Jönsson, A.; Zlowodzki, M.; Haidukewych, G.J. Gamma nails revisited: Gamma nails versus compression hip screws in the management of intertrochanteric fractures of the hip: A meta-analysis. J. Orthop. Trauma 2009, 23, 460–464. [Google Scholar] [CrossRef] [PubMed]
- Dainty, J.R.; Smith, T.O.; Clark, E.M.; Whitehouse, M.R.; Price, A.J.; MacGregor, A.J. Trajectories of pain and function in the first five years after total hip and knee arthroplasty: An analysis of patient reported outcome data from the National Joint Registry. Bone Jt. J. 2021, 103-B, 1111–1118. [Google Scholar] [CrossRef]
- Hamilton, D.F.; Giesinger, J.M.; MacDonald, D.J.; Simpson, A.H.R.W.; Howie, C.R.; Giesinger, K. Responsiveness and ceiling effects of the Forgotten Joint Score-12 following total hip arthroplasty. Bone Jt. Res. 2016, 5, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Canovas, F.; Dagneaux, L. Quality of life after total knee arthroplasty. Orthop. Traumatol. Surg. Res. 2018, 104 (Suppl. S1), S41–S46. [Google Scholar] [CrossRef]
- Bozic, K.J.; Kamath, A.F.; Ong, K.; Lau, E.; Kurtz, S.; Chan, V.; Vail, T.P.; Rubash, H.; Berry, D.J. Comparative Epidemiology of Revision Arthroplasty: Failed THA Poses Greater Clinical and Economic Burdens Than Failed TKA. Clin. Orthop. Relat. Res. 2015, 473, 2131–2138. [Google Scholar] [CrossRef] [PubMed]
- Park, J.W.; Won, S.H.; Moon, S.Y.; Lee, Y.K.; Ha, Y.C.; Koo, K.H. Burden and future projection of revision Total hip Arthroplasty in South Korea. BMC Musculoskelet. Disord. 2021, 22, 375. [Google Scholar] [CrossRef] [PubMed]
- Cheng, R.; Krell, E.C.; Chiu, Y.F.; Stimac, J.D.; Heyse, T.J.; Abdel, M.P.; Figgie, M.P.; Blevins, J.L. Survivorship and Clinical Outcomes of Primary Total Knee Arthroplasty Performed in Patients 35 Years of Age and Younger. J. Arthroplast. 2023, 38, 2316–2323.e1. [Google Scholar] [CrossRef]
- Stockwell, K.D.; Gascoyne, T.C.; Singh, M.; Turgeon, T.R. Survivorship of constrained polyethylene inserts in primary total knee replacements. Knee 2020, 27, 1343–1348. [Google Scholar] [CrossRef]
- Schwartz, A.M.; Farley, K.X.; Guild, G.N.; Bradbury, T.L. Projections and Epidemiology of Revision Hip and Knee Arthroplasty in the United States to 2030. J. Arthroplast. 2020, 35, S79–S85. [Google Scholar] [CrossRef]
- Bozic, K.J.; Kurtz, S.M.; Lau, E.; Ong, K.; Chiu, V.; Vail, T.P.; Rubash, H.E.; Berry, D.J. The Epidemiology of Revision Total Knee Arthroplasty in the United States. Clin. Orthop. Relat. Res. 2010, 468, 45–51. [Google Scholar] [CrossRef]
- Upfill-Brown, A.; Hsiue, P.P.; Sekimura, T.; Shi, B.; Ahlquist, S.A.; Patel, J.N.; Adamson, M.; Stavrakis, A.I. Epidemiology of Revision Total Knee Arthroplasty in the United States, 2012 to 2019. Arthroplast. Today 2022, 15, 188–195.e6. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.M.; Lau, E.; Schmier, J.; Ong, K.L.; Zhao, K.; Parvizi, J. Infection Burden for Hip and Knee Arthroplasty in the United States. J. Arthroplast. 2008, 23, 984–991. [Google Scholar] [CrossRef] [PubMed]
- Koh, C.K.; Zeng, I.; Ravi, S.; Zhu, M.; Vince, K.G.; Young, S.W. Periprosthetic Joint Infection Is the Main Cause of Failure for Modern Knee Arthroplasty: An Analysis of 11,134 Knees. Clin. Orthop. Relat. Res. 2017, 475, 2194–2201. [Google Scholar] [CrossRef] [PubMed]
- Premkumar, A.; Kolin, D.A.; Farley, K.X.; Wilson, J.M.; McLawhorn, A.S.; Cross, M.B.; Sculco, P.K. Projected Economic Burden of Periprosthetic Joint Infection of the Hip and Knee in the United States. J. Arthroplast. 2021, 36, 1484–1489.e3. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, T.; Alijanipour, P.; Parvizi, J. The management of an infected total knee arthroplasty. Bone Jt. J. 2015, 97-B, 20–29. [Google Scholar] [CrossRef]
- Wongworawat, M.D. Clinical Faceoff: One- Versus Two-Stage Exchange Arthroplasty for Prosthetic Joint Infections. Clin. Orthop. Relat. Res. 2013, 471, 1750. [Google Scholar] [CrossRef] [PubMed]
- Duncan, S.T.; Schwarzkopf, R.; Seyler, T.M.; Landy, D.C. The Practice Patterns of American Association of Hip and Knee Surgeons for the Management of Chronic Periprosthetic Joint Infection After Total Knee Arthroplasty. J. Arthroplast. 2023, 38, 2441–2446. [Google Scholar] [CrossRef]
- Cui, Q.; Mihalko, W.M.; Shields, J.S.; Ries, M.; Saleh, K.J. Antibiotic-impregnated cement spacers for the treatment of infection associated with total hip or knee arthroplasty. J. Bone Jt. Surg. Am 2007, 89, 871–882. [Google Scholar] [CrossRef]
- Springer, B.D.; Lee, G.C.; Osmon, D.; Haidukewych, G.J.; Hanssen, A.D.; Jacofsky, D.J. Systemic safety of high-dose antibiotic-loaded cement spacers after resection of an infected total knee arthroplasty. Clin. Orthop. Relat. Res. 2004, 427, 47–51. [Google Scholar] [CrossRef]
- Kuzyk, P.R.T.; Dhotar, H.S.; Sternheim, A.; Gross, A.E.; Safir, O.; Backstein, D. Two-stage Revision Arthroplasty for Management of Chronic Periprosthetic Hip and Knee Infection: Techniques, Controversies, and Outcomes. JAAOS J. Am. Acad. Orthop. Surg. 2014, 22, 153. [Google Scholar] [CrossRef]
- Osmon, D.R.; Berbari, E.F.; Berendt, A.R.; Lew, D.; Zimmerli, W.; Steckelberg, J.M.; Rao, N.; Hanssen, A.; Wilson, W.R. Executive Summary: Diagnosis and Management of Prosthetic Joint Infection: Clinical Practice Guidelines by the Infectious Diseases Society of Americaa. Clin. Infect. Dis. 2013, 56, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, P.H.; Chang, Y.H.; Chen, S.H.; Ueng, S.W.N.; Shih, C.H. High concentration and bioactivity of vancomycin and aztreonam eluted from Simplex cement spacers in two-stage revision of infected hip implants: A study of 46 patients at an average follow-up of 107 days. J. Orthop. Res. 2006, 24, 1615–1621. [Google Scholar] [CrossRef] [PubMed]
- Mühlberg, E.; Umstätter, F.; Kleist, C.; Domhan, C.; Mier, W.; Uhl, P. Renaissance of vancomycin: Approaches for breaking antibiotic resistance in multidrug-resistant bacteria. Can. J. Microbiol. 2020, 66, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Bruniera, F.R.; Ferreira, F.M.; Saviolli, L.R.M.; Bacci, M.R.; Feder, D.; da Luz Gonçalves Pedreira, M.; Peterlini, M.A.S.; Azzalis, L.A.; Junqueira, V.B.C.; Fonseca, F.L.A. The use of vancomycin with its therapeutic and adverse effects: A review. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 694–700. [Google Scholar]
- Koo, K.H.; Yang, J.W.; Cho, S.H.; Song, H.-R.; Park, H.-B.; Ha, Y.-C.; Chang, J.-D.; Kim, S.-Y.; Kim, Y.-H. Impregnation of vancomycin, gentamicin, and cefotaxime in a cement spacer for two-stage cementless reconstruction in infected total hip arthroplasty. J. Arthroplast. 2001, 16, 882–892. [Google Scholar] [CrossRef]
- Lawrie, C.M.; Jo, S.; Barrack, T.; Roper, S.; Wright, R.W.; Nunley, R.M.; Barrack, R.L. Local delivery of tobramycin and vancomycin in primary total knee arthroplasty achieves minimum inhibitory concentrations for common bacteria causing acute prosthetic joint infection. Bone Jt. J. 2020, 102-B, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Urena, E.O.; Tande, A.J.; Osmon, D.R.; Berbari, E.F. Diagnosis of Prosthetic Joint Infection: Cultures, Biomarker and Criteria. Infect. Dis. Clin. North Am. 2017, 31, 219–235. [Google Scholar] [CrossRef]
- Iarikov, D.; Demian, H.; Rubin, D.; Alexander, J.; Nambiar, S. Choice and doses of antibacterial agents for cement spacers in treatment of prosthetic joint infections: Review of published studies. Clin. Infect. Dis. 2012, 55, 1474–1480. [Google Scholar] [CrossRef]
- James, A.; Larson, T. Acute renal failure after high-dose antibiotic bone cement: Case report and review of the literature. Ren. Fail. 2015, 37, 1061–1066. [Google Scholar] [CrossRef]
- Hanssen, A.D.; Spangehl, M.J. Practical Applications of Antibiotic-Loaded Bone Cement for Treatment of Infected Joint Replacements. Clin. Orthop. Relat. Res. 2004, 427, 79. [Google Scholar] [CrossRef]
- Jiranek, W.A.; Hanssen, A.D.; Greenwald, A.S. Antibiotic-loaded bone cement for infection prophylaxis in total joint replacement. J. Bone Jt. Surg. Am 2006, 88, 2487–2500. [Google Scholar] [CrossRef] [PubMed]
- Corró, S.; Vicente, M.; Rodríguez-Pardo, D.; Pigrau, C.; Lung, M.; Corona, P.S. Vancomycin-Gentamicin Prefabricated Spacers in 2-Stage Revision Arthroplasty for Chronic Hip and Knee Periprosthetic Joint Infection: Insights Into Reimplantation Microbiology and Outcomes. J. Arthroplast. 2020, 35, 247–254. [Google Scholar] [CrossRef]
- Warwick, H.S.; Tan, T.L.; Rangwalla, K.; Shau, D.N.; Barry, J.J.; Hansen, E.N. Effect of Antibiotic Spacer Dosing on Treatment Success in Two-Stage Exchange for Periprosthetic Joint Infection. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2024, 8, e23.00103. [Google Scholar] [CrossRef] [PubMed]
- Moore, A.J.; Wylde, V.; Whitehouse, M.R.; Beswick, A.D.; Walsh, N.E.; Jameson, C.; Blom, A.W. Development of evidence-based guidelines for the treatment and management of periprosthetic hip infection. Bone Jt. 2023, 4, 226–231. [Google Scholar] [CrossRef]
- Lenguerrerand, E.; Whitehouse, M.R.; Beswick, A.D.; Kunutsor, S.K.; Porter, M.; Blom, A.W. Risk factors associated with revision of prosthetic joint infection after hip replacement: A prospective observational study. Lancet Infect. Dis. 2018, 18, 1004–1014. [Google Scholar] [CrossRef]
- Li, C.; Renz, N.; Trampuz, A.; Ojeda-Thies, C. Twenty common errors in the diagnosis and treatment of periprosthetic joint infection. Int. Orthop. 2020, 44, 3–14. [Google Scholar] [CrossRef]
- Osmon, D. Microbiology and antimicrobial challenges of periprosthetic joint infection. J. Am. Acad. Orthop. Surg. 2017, 25 (Suppl. S1), S17–S19. [Google Scholar] [CrossRef] [PubMed]
- Frank, B.; Simon, S.; Aichmair, A.; Dominkus, M.; Hofstaetter, J. Clinical impact of microbiology results in two-stage revision arthroplasty with spacer exchange. Arch. Orthop. Trauma Surg. 2023, 143, 4741–4754. [Google Scholar] [CrossRef]
- Nace, J.; Chen, Z.; Bains, S.; Kahan, M.; Gilson, G.; Mont, M.; Delanois, R. 1.5-stage versus 2-stage exchange total hip arthroplasty for chronic periprosthetic joint infections: A comparison of survivorships, reinfections, and patient-reported outcomes. J. Arthroplast. 2023, 38, S235–S241. [Google Scholar] [CrossRef]
- Tarabichi, S.; Chen, A.; Higuera, C.; Parvizi, J.; Polkowski, G. 2022 American association of hip and knee surgeons symposium: Periprosthetic joint infection. J. Arthroplast. 2023, 38, S45–S49. [Google Scholar] [CrossRef]
- Abdel, M.P.; Barreira, P.; Battenberg, A.; Berry, D.J.; Blevins, K.; Font-Vizcarra, L.; Frommelt, L.; Goswami, K.; Greiner, J.; Janz, V.; et al. Hip and Knee Section, Treatment, Two-Stage Exchange Spacer-Related: Proceedings of International Consensus on Orthopedic Infections. J. Arthroplast. 2019, 34 (Suppl. S2), S427–S438. [Google Scholar] [CrossRef]
- Chen, Y.C.; Lin, Y.C.; Chang, C.H.; Lee, S.H.; Chang, Y. Risk factors for treatment failure in patients who have knee periprosthetic joint infection treated with two-stage exchange arthroplasty as well as their fate. J. Arthroplast. 2023, 38, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Akgün, D.; Perka, C.; Trampuz, A.; Renz, N. Outcome of hip and knee periprosthetic joint infections caused ba pathogens resistant to biofilm-active antibiotics: Results from a prospective cohort study. Arch. Orthop. Trauma Surg. 2018, 138, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Young, B.C.; Dudareva, M.; Vicentine, M.; Hotchen, A.; Ferguson, J.; McNally, M. Microbial persistence, replacement and local antimicrobial therapy in recurrent bone and joint infection. Antibiotics 2023, 12, 708. [Google Scholar] [CrossRef]
- Dombrowski, M.; Wilson, A.; Wawrose, R.; O’Malley, M.; Urish, K.; Klatt, B. A low percentage of patients satisfy typical indications for single-stage exchange arthroplasty for chronic periprosthetic joint infection. Clin. Orthop. Relat. Res. 2020, 478, 1780–1786. [Google Scholar] [CrossRef]
- Thakrar, R.; Horriat, S.; Kayani, B.; Haddad, F. Indications fo a single-stage exchange arthroplasty for chronic prosthetic joint infection: A systematic review. Bone Jt. J. 2019, 101-B, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Grammatopoulos, G.; Bolduc, M.; Atkins, B.; Kendrick, B.; McLardy-Smith, P.; Murray, D.; Gundle, R.; Taylor, A. Functional outcome of debridement, antibiotics and implant retention in periprosthetic joint infection involving the hip: A case control study. Bone Jt. J. 2017, 99-B, 614–622. [Google Scholar] [CrossRef] [PubMed]
- Krizsan, G.; Sallai, I.; Veres, D.; Prinz, G.; Szeker, D.; Skaliczki, G. Rifampicin resistance and risk factors associated with significantly lower recovery rates after two-stage revision in patients with prosthetic joint infection. J. Glob. Antimicrob. Resist. 2022, 30, 231–236. [Google Scholar] [CrossRef]
- Lazarinis, S.; Hailer, N.; Järhult, J.; Brüggemann, A. Incidence of rifampicin resistance in periprosthetic joint infection: A single-centre cohort study on 238 patients. Antibiotics 2023, 12, 1499. [Google Scholar] [CrossRef]
- Gao, Z.; Du, Y.; Piao, S.; Sun, J.; Li, X.; Zhou, Y. Comparison between the Staphylococci aureus and coagulase-negative staphylococci infected total joint arthroplasty treated by two-stage revision: A retrospective study with two year minimum follow-up. J. Orthop. Sci. 2019, 24, 109–115. [Google Scholar] [CrossRef]
- Li, H.; Ni, M.; Li, X.; Zhang, Q.; Li, X.; Chen, J. Two-stage revisions for culture-negative infected total knee arthroplasties: A five-year outcome in comparison with one-stage and two-stage revisions for culture-positive cases. J. Orthop. Sci. 2017, 22, 306–312. [Google Scholar] [CrossRef]
- Maden, C.; Jaibaji, M.; Konan, S.; Zagra, L.; Borella, M.; Harvey, A.; Volpin, A. The outcomes of surgical mangement of failed two-stage revision knee arthroplasty. Acta Biomed. 2021, 92, e2021197. [Google Scholar]
- Hipfl, C.; Mooij, W.; Perka, C.; Hardt, S.; Wassilew, G. Unexpected low-grade infections in revision hip arthroplasty for aseptic loosening. Bone Jt. J. 2021, 103-B, 1070–1077. [Google Scholar] [CrossRef]
- Kozaily, E.; Tan, T.L.; Yacovelli, S.; Anis, H.; Higuera, C.; Piuzzi, N.S.; Parvizi, J. Interim spacer exchange for treatment of periprosthetic joint infection: Almost half the patients subsequently fail. J. Arthroplast. 2022, 37, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Steadman, W.; Chapman, P.; Schuetz, M.; Schmutz, B.; Trampuz, A.; Tetsworth, K. Local antibiotic delivery options in periprosthetic joint infection. Antibiotics 2023, 12, 752. [Google Scholar] [CrossRef] [PubMed]
- Hansen, E.; Kühn, K.D. (Eds.) Essentials of Cemented Knee Arthroplasty; Springer: Berlin/Heidelberg, Germany, 2022; ISBN 978-3-662-63112-6/978-3-662-63115-7/978-3-662-63113-3. [Google Scholar] [CrossRef]
- Kühn, K.D.; Lieb, E.; Berberich, C. PMMA bone cement: What is the role of local antibiotics. In Matrise Orthopaedic, Proceeding of N°243, Commission Paritaire 1218T86410; Heraeus: Lyon, France, 2016; pp. 12–18. ISSN 1148 2362. [Google Scholar]
- Gbejuade, H.O.; Lovering, A.M.; Webb, J.C. The role of microbial biofilms in prosthetic joint infections. Acta Orthop. 2015, 86, 147–158. [Google Scholar] [CrossRef] [PubMed]
- Winkler, T.; Stuhlert, M.G.; Lieb, E.; Müller, M.; von Roth, P.; Preininger, B.; Trampuz, A.; Perka, C.F. Outcome of short versus long interval in two-stage exchange for periprosthetic joint infection: A prospective cohort study. Arch. Orthop. Trauma Surg. 2019, 139, 295–303. [Google Scholar] [CrossRef]
- Lunz, A.; Schonhoff, M.; Omlor, G.; Knappe, K.; Bangert, Y.; Lehner, B.; Renkawitz, T.; Jaeger, S. Enhanced antibiotic release from bone cement spacers utilizing dual antibiotic loading with elevated vancomycin concentrations in two-stage revision for periprosthetic joint infection. Int. Orthop. 2023, 47, 2655–2661. [Google Scholar] [CrossRef]
- Kaplan, S.S.; Heine, R.P.; Simmons, R.L. Defensins impair phagocytic killing by neutrophils in biomaterial-related infection. Infect. Immun. 1999, 67, 1640–1645. [Google Scholar] [CrossRef]
- Sousa, R.; Serrano, P.; Gomes Dias, J.; Oliveira, J.C.; Oliveira, A. Improving the accuracy of synovial fluid analysis in the diagnosis of prosthetic joint infection with simple and inexpensive biomarkers. Bone Jt. J. 2017, 99-B, 351–357. [Google Scholar] [CrossRef]
- Ma, C.Y.; Lu, Y.D.; Bell, K.L.; Wang, J.W.; Ko, J.Y.; Wang, C.J.; Kuo, F.C. Predictors of treatment failure after 2-stage reimplantation for infected total knee arthroplasty: A 2- to 10-year follow-up. J. Arthroplast. 2018, 33, 2234–2239. [Google Scholar] [CrossRef]
- Tan, T.L.; Goswami, K.; Fillingham, Y.A.; Shohat, N.; Rondon, A.J.; Parvizi, J. Defining treatment success after 2-stage exchange arthroplasty for periprosthetic joint infection. J. Arthroplast. 2018, 33, 3541–3546. [Google Scholar] [CrossRef]
- Goumenos, S.; Hardt, S.; Kontogeorgakos, V.; Trampuz, A.; Perka, C.; Meller, S. Success rate after 2-stage spacer-free total hip arthroplasty exchange and risk factors for reinfection: A prospective cohort study of 187 patients. J. Arthroplast. 2024. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Lieb, E.; Hanstein, T.; Schuerings, M.; Trampuz, A.; Perka, C. Reduction of treatment duration in periprosthetic infection with a fast-track concept is economically not feasible. Z. Orthop. Unf. 2015, 153, 618–623. [Google Scholar]
- Masri, B.A.; Duncan, C.P.; Beauchamp, C.P. Long-term elution of antibiotics from bone-cement: An in vivo study using the prosthesis of antibiotic-loaded acrylic cement (PROSTALAC) system. J. Arthroplast. 1998, 13, 331–338. [Google Scholar] [CrossRef]
- Atıcı, T.; Şahin, N.; Çavun, S.; Özakin, C.; Kaleli, T. Antibiotic release and antibacterial efficacy in cement spacers and cement beads impregnated with different techniques: In Vitro study. Eklem Hastalik. Cerrahisi 2018, 29, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Bertazzoni Minelli, E.; Benini, A.; Magnan, B.; Bartolozzi, P. Release of gentamicin and vancomycin from temporary human hip spacers in two-stage revision of infected arthroplasty. J. Antimicrob. Chemother. 2004, 53, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.; Chen, W.C.; Hsieh, P.H.; Chen, D.W.; Lee, M.S.; Shih, H.-N.; Ueng, S.W.N. In vitro activities of daptomycin-, vancomycin-, and teicoplanin-loaded polymethylmethacrylate against methicillin-susceptible, methicillin-resistant, and vancomycin-intermediate strains of Staphylococcus aureus. Antimicrob. Agents Chemother. 2011, 55, 5480–5484. [Google Scholar] [CrossRef]
- Paz, E.; Sanz-Ruiz, P.; Abenojar, J.; Vaquero-Martín, J.; Forriol, F.; Del Real, J.C. Evaluation of Elution and Mechanical Properties of High-Dose Antibiotic-Loaded Bone Cement: Comparative “In Vitro” Study of the Influence of Vancomycin and Cefazolin. J. Arthroplast. 2015, 30, 1423–1429. [Google Scholar] [CrossRef]
- Edelstein, A.I.; Okroj, K.T.; Rogers, T.; Della Valle, C.J.; Sporer, S.M. Nephrotoxicity After the Treatment of Periprosthetic Joint Infection With Antibiotic-Loaded Cement Spacers. J. Arthroplast. 2018, 33, 2225–2229. [Google Scholar] [CrossRef]
- Kuechle, D.K.; Landon, G.C.; Musher, D.M.; Noble, P.C. Elution of vancomycin, daptomycin, and amikacin from acrylic bone cement. Clin. Orthop. Relat. Res. 1991, 264, 302–308. [Google Scholar] [CrossRef]
- Amin, T.J.; Lamping, J.W.; Hendricks, K.J.; McIff, T.E. Increasing the elution of vancomycin from high-dose antibiotic-loaded bone cement: A novel preparation technique. J. Bone Jt. Surg. Am 2012, 94, 1946–1951. [Google Scholar] [CrossRef]
- Fink, B.; Vogt, S.; Reinsch, M.; Büchner, H. Sufficient release of antibiotic by a spacer 6 weeks after implantation in two-stage revision of infected hip prostheses. Clin. Orthop. Relat. Res. 2011, 469, 3141–3147. [Google Scholar] [CrossRef]
- Wang, J.S.; Toksvig-Larsen, S.; Müller-Wille, P.; Franźen, H. Is there any difference between vacuum mixing systems in reducing bone cement porosity? J. Biomed. Mater. Res. 1996, 33, 115–119. [Google Scholar] [CrossRef]
- Kühn, K.-D. PMMA Cements Are We Aware What We Are Using; Springer: Berlin/Heidelberg, Germany, 2014; ISBN 13 978-3-642-41535-7. [Google Scholar] [CrossRef]
- Stevens, C.M.; Tetsworth, K.D.; Calhoun, J.H.; Mader, J.T. An articulated antibiotic spacer used for infected total knee arthroplasty: A comparative in vitro elution study of Simplex and Palacos bone cements. J. Orthop. Res. 2005, 23, 27–33. [Google Scholar] [CrossRef]
- Lee, S.H.; Tai, C.L.; Chen, S.Y.; Chang, C.H.; Chang, Y.H.; Hsieh, P.H. Elution and Mechanical Strength of Vancomycin-Loaded Bone Cement: In Vitro Study of the Influence of Brand Combination. PLoS ONE 2016, 11, e0166545. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, D.; Kodali, P.; Dipersio, J.; Acus, R.; Askew, M. In vitro analysis of antifungal impregnated polymethylmethacrylate bone cement. Clin. Orthop. Relat. Res. 2002, 403, 228–231. [Google Scholar] [CrossRef]
- Kühn, K.D. (Ed.) Management of periprosthetic joint infection. In A Global Perspective on Diagnosis, Treatment Options, Prevention Strategies and Their Economic Impact; Springer: Berlin/Heidelberg, Germany; New York, NY, USA, 2018; ISBN 978-3-662-54469-3. [Google Scholar] [CrossRef]
- Osmanski-Zenk, K.; Klinder, A.; Rimke, C.; Wirtz, D.C.; Lohmann, C.H.; Haas, H.; Kladny, B.; Mittelmeier, W. Evaluation of the standard procedure for treatment of periprosthetic joint infections of total knee and hip arthroplasty: A comparison of the 2015 and 2020 census in total joint replacement centres in Germany. BMC Musculoskelet. Disord. 2021, 22, 791–800. [Google Scholar] [CrossRef]
- Flurin, L.; Greenwood-Quaintance, K.; Patel, R. Microbiology of polymicrobial joint infection. Diagn. Microbiol. Infect. Dis. 2019, 94, 255–259. [Google Scholar] [CrossRef]
- Penner, M.J.; Masri, B.A.; Duncan, C.P. Elution characteristics of vancomycin and tobramycin combined in acrylic bone-cement. J. Arthroplast. 1996, 11, 939–944. [Google Scholar] [CrossRef]
- Slane, J.; Gietman, B.; Squire, M. Antibiotic elution from acrylic bone cement loaded with high doses of tobramycin and vancomycin. J. Orthop. Res. 2018, 36, 1078–1085. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, P.H.; Chen, L.H.; Chen, C.H.; Lee, M.S.; Yang, W.E.; Shih, C.H. Two-stage revision hip arthroplasty for infection with a custom-made, antibiotic-loaded, cement prosthesis as an interim spacer. J. Trauma 2004, 56, 1247–1252. [Google Scholar] [CrossRef] [PubMed]
- Dovas, S.; Liakopoulos, V.; Papatheodorou, L.; Chronopoulou, I.; Papavasiliou, V.; Atmatzidis, E.; Giannopoulou, M.; Eleftheriadis, T.; Simopoulou, T.; Karachalios, T.; et al. Acute renal failure after antibiotic-impregnated bone cement treatment of an infected total knee arthroplasty. Clin. Nephrol. 2008, 69, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Patrick, B.N.; Rivey, M.P.; Allington, D.R. Acute renal failure associated with vancomycin- and tobramycin-laden cement in total hip arthroplasty. Ann. Pharmacother. 2006, 40, 2037–2042. [Google Scholar] [CrossRef]
- Luu, A.; Syed, F.; Raman, G.; Bhalla, A.; Muldoon, E.; Hadley, S.; Smith, E.; Rao, M. Two-stage arthroplasty for prosthetic joint infection: A systematic review of acute kidney injury, systemic toxicity and infection control. J. Arthroplast. 2013, 28, 1490–1498.e1. [Google Scholar] [CrossRef]
- Geller, J.A.; Cunn, G.; Herschmiller, T.; Murtaugh, T.; Chen, A. Acute Kidney Injury After First-Stage Joint Revision for Infection: Risk Factors and the Impact of Antibiotic Dosing. J. Arthroplast. 2017, 32, 3120–3125. [Google Scholar] [CrossRef]
- Chaudhry, Y.P.; LaGreca, M.; Hayes, H.; Papadelis, E.; Rao, S.S.; Amin, R. Acute kidney injury in the context of staged revision arthroplasty and the use of antibiotic-laden cement spacers: A systematic review. J. Orthop. Surg. Res. 2023, 18, 340. [Google Scholar] [CrossRef]
- Lautenschlager, E.P.; Jacobs, J.J.; Marshall, G.W.; Meyer, P.R. Mechanical properties of bone cements containing large doses of antibiotic powders. J. Biomed. Mater. Res. 1976, 10, 929–938. [Google Scholar] [CrossRef] [PubMed]
- Humez, M.; Domann, E.; Thormann, K.M.; Fölsch, C.; Strathausen, R.; Vogt, S.; Alt, V.; Kühn, K.D. Daptomycin-Impregnated PMMA Cement against Vancomycin-Resistant Germs: Dosage, Handling, Elution, Mechanical Stability, and Effectiveness. Antibiotics 2023, 12, 1567. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Krampitz, B.; Steiner, J.; Trampuz, A.; Kühn, K.D. Voriconazole Admixed with PMMA-Impact on Mechanical Properties and Efficacy. Antibiotics 2023, 12, 848. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brock, H.S.; Moodie, P.G.; Hendricks, K.J.; McIff, T.E. Compression strength and porosity of single-antibiotic cement vacuum-mixed with vancomycin. J. Arthroplast. 2010, 25, 990–997. [Google Scholar] [CrossRef]
- Duncan, C.P.; Masri, B.A. The role of antibiotic-loaded cement in the treatment of an infection after a hip replacement. Instr. Course Lect. 1995, 44, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Lunz, A.; Knappe, K.; Omlor, G.W.; Schonhoff, M.; Renkawitz, T.; Jaeger, S. Mechanical strength of antibiotic-loaded PMMA spacers in two-stage revision surgery. BMC Musculoskelet. Disord. 2022, 23, 945. [Google Scholar] [CrossRef]
- Heraeus Medical (2024). Available online: https://www.heraeus-medical.com/de/healthcare-professionals/products/copal-gc/ (accessed on 14 August 2024).
- Ensing, G.T.; van Horn, J.R.; van der Mei, H.C.; Busscher, H.J.; Neut, D. Copal bone cement is more effective in preventing biofilm formation than Palacos R-G. Clin. Orthop. Relat. Res. 2008, 466, 1492–1498. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Labmayr, M.; Lerchbaumer, M.H.; Kühn, K.D.; Kittinger, C.; Amerstorfer, F.; Leithner, A.; Glehr, M. Comparison of elution characteristics and mechanical properties of acrylic bone cements with and without superficial vancomycin coating (SVC) in the late phase of polymerization. Orthop. Traumatol. Surg. Res. 2021, 107, 102908. [Google Scholar] [CrossRef] [PubMed]
- Heraeus Medical (2024). Available online: https://www.heraeus-medical.com/de/healthcare-professionals/products/copal-gv/ (accessed on 14 August 2024).
- ISO 5833; Implants for Surgery—Acrylic Resin Cements. International Organization for Standardization (ISO): Geneva, Switzerland, 2002.
- DIN 53435; Testing of Plastics—Bending Test and Impact Test on Dynstat Test Specimens. German Institute for Standardization (DIN): Berlin, Germany, 2018.




| Cement/Spacer | Antibiotics | Tested Strains | |
|---|---|---|---|
| Copal G + C | 2 g Vancomycin added manually | S. aureus | ATCC 29213 |
| E. faecalis | ATCC 29212 | ||
| MRSA | ATCC 43300 | ||
| Copal G + C | 6 g Vancomycin added manually | S. aureus | ATCC 29213 |
| E. faecalis | ATCC 29212 | ||
| MRSA | ATCC 43300 | ||
| Copal G + V | 2 g Vancomycin added manually | S. aureus | ATCC 29213 |
| E. faecalis | ATCC 29212 | ||
| MRSA | ATCC 43300 | ||
| Copal G + V | 6 g Vancomycin added manually | S. aureus | ATCC 29213 |
| E. faecalis | ATCC 29212 | ||
| MRSA | ATCC 43300 | ||
| Copal Spacer | S. aureus | ATCC 29213 | |
| E. coli | ATCC 25922 | ||
| Tecres spacer | S. aureus | ATCC 29213 | |
| E. coli | ATCC 25922 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwong, J.W.; Abramowicz, M.; Kühn, K.D.; Foelsch, C.; Hansen, E.N. High and Low Dosage of Vancomycin in Polymethylmethacrylate Cements: Efficacy and Mechanical Properties. Antibiotics 2024, 13, 818. https://doi.org/10.3390/antibiotics13090818
Kwong JW, Abramowicz M, Kühn KD, Foelsch C, Hansen EN. High and Low Dosage of Vancomycin in Polymethylmethacrylate Cements: Efficacy and Mechanical Properties. Antibiotics. 2024; 13(9):818. https://doi.org/10.3390/antibiotics13090818
Chicago/Turabian StyleKwong, Jeffrey W., Michael Abramowicz, Klaus Dieter Kühn, Christian Foelsch, and Erik N. Hansen. 2024. "High and Low Dosage of Vancomycin in Polymethylmethacrylate Cements: Efficacy and Mechanical Properties" Antibiotics 13, no. 9: 818. https://doi.org/10.3390/antibiotics13090818






