An Efficient Disinfectant, Composite Material {SLS@[Zn3(CitH)2]} as Ingredient for Development of Sterilized and Non Infectious Contact Lens
Abstract
:1. Introduction
2. Results
2.1. General Aspects
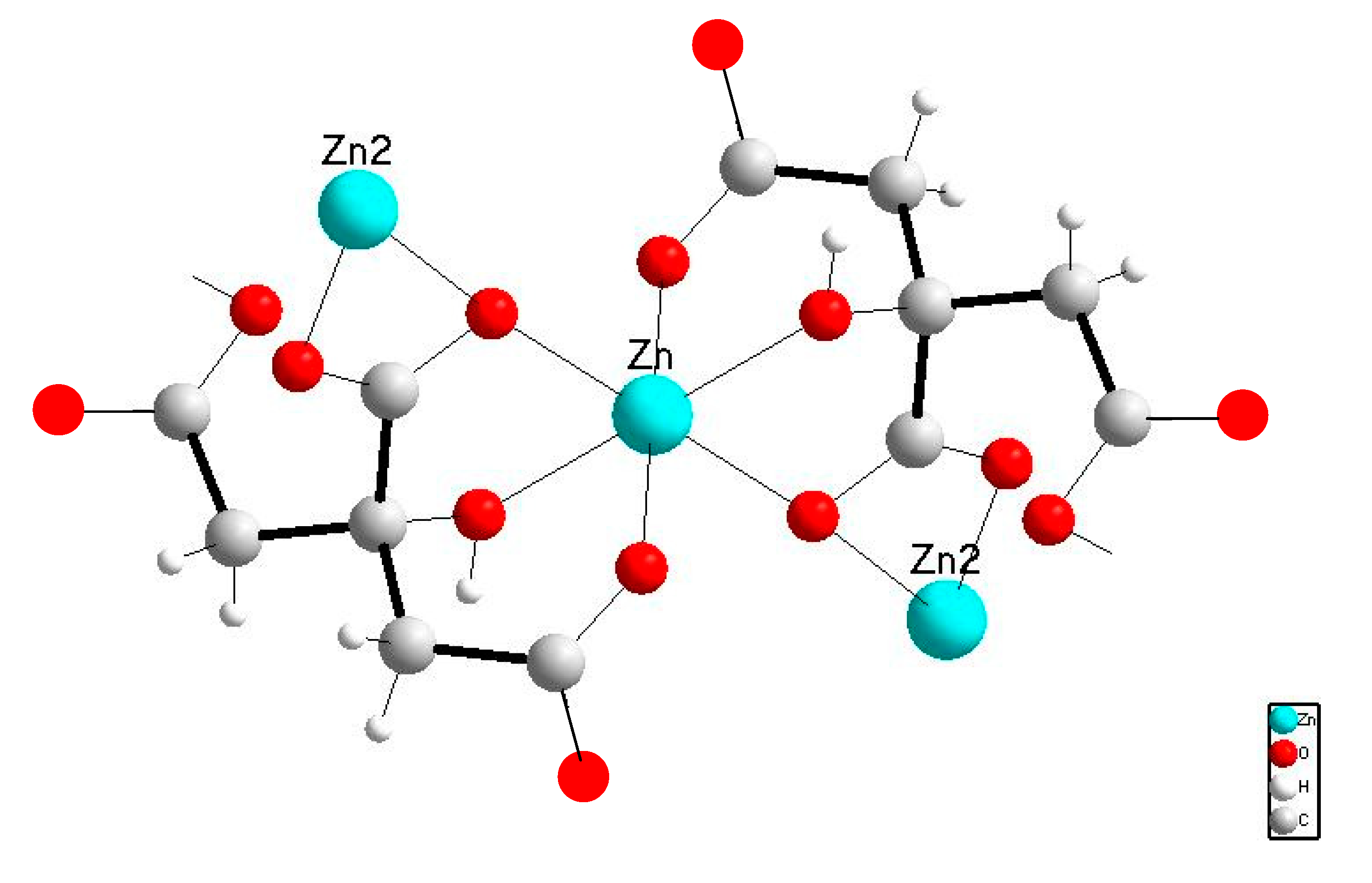
2.2. Characterization of 1
2.2.1. Solid State Studies
2.2.2. Solution Studies
2.3. Preparation and Characterization of Micelle
2.3.1. Solid State Studies
Vibrational Spectroscopy
Thermo Gravimetric Analysis of the Composite 2
2.3.2. Solution Studies
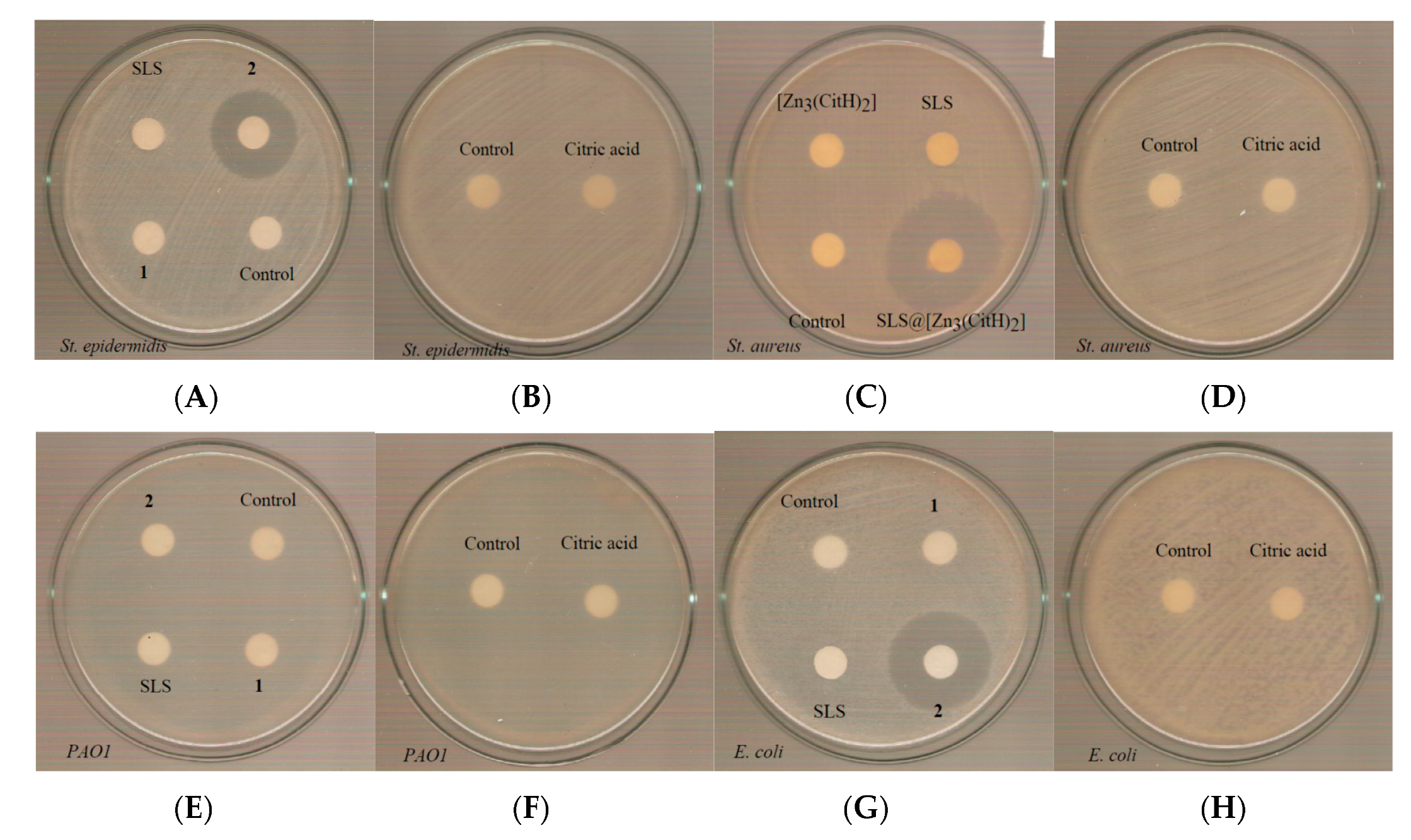
2.4. Biological Studies
3. Conclusions
4. Materials and Methods
Biological Studies
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Taube, M.-A.; del Mar Cendra, M.; Elsahn, A.; Christodoulides, M.; Hossain, P. Pattern recognition receptors in microbial keratitis. Eye 2015, 29, 1399–1415. [Google Scholar] [CrossRef] [Green Version]
- Stapleton, F.; Carnt, N. Contact lens-related microbial keratitis: How have epidemiology and genetics helped us with pathogenesis and prophylaxis. Eye 2012, 26, 185–193. [Google Scholar] [CrossRef]
- Teweldemedhin, M.; Gebreyesus, H.; HailuAtsbaha, A.; Weldegebreal Asgedom, S.; Saravanan, M. Bacterial profile of ocular infections: A systematic review. BMC Ophthalmol. 2017, 17, 212. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, A.B.; Nixon, A.D.; Rueff, E.M. Contact lens associated microbial keratitis: Practical considerations for the optometrist. Clin. Optom. 2016, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Yepes, N.; Lee, S.B.; Hill, V.; Ashenhurst, M.; Saunders, P.P.; Slomovic, A.R. Infectious keratitis after overnight orthokeratology in Canada. Cornea 2005, 24, 857–860. [Google Scholar] [CrossRef] [PubMed]
- Tseng, C.H.; Fong, C.F.; Chen, W.L.; Hou, Y.C.; Wang, I.J.; Hu, F.R. Overnight orthokeratology-associated microbial keratitis. Cornea 2005, 24, 778–782. [Google Scholar] [CrossRef]
- Keay, L.; Stapleton, F.; Schein, O. Epidemiology of contact lens-related inflammation and microbial keratitis: A 20-year perspective. Eye Contact Lens. 2007, 33, 346–353. [Google Scholar] [CrossRef]
- Lee, D.; Cho, S.; Sung-Park, H.; Kwon, I. Ocular drug delivery through pHEMA-Hydrogel contact lenses co-loaded with lipophilic vitamins. Sci. Rep. 2016, 6, 34194. [Google Scholar] [CrossRef]
- Milionis, I.; Banti, C.N.; Sainis, I.; Raptopoulou, C.P.; Psycharis, V.; Kourkoumelis, N.; Hadjikakou, S.K. Silver ciprofloxacin (CIPAG): A successful combination of antibiotics in inorganic-organic hybrid for the development of novel formulations based on chemically modified commercially available antibiotics. J. Biol. Inorg. Chem. 2018, 23, 705–723. [Google Scholar] [CrossRef]
- Pasquet, J.; Chevalier, Y.; Pelletier, J.; Couval, E.; Bouvier, D.; Bolzinger, M.-A. The contribution of zinc ions to the antimicrobial activity of zinc oxide. Colloids Surf. A Physicochem. Eng. Asp. 2014, 457, 263–274. [Google Scholar] [CrossRef]
- Papadimitriou, A.; Ketikidis, I.; Stathopoulou, M.K.; Banti, C.N.; Papachristodoulou, C.; Zoumpoulakis, L.; Agathopoulos, S.; Vagenas, G.V.; Hadjikakou, S.K. Innovative material containing the natural product curcumin, with enhanced antimicrobial properties for active packaging. Mater. Sci. Eng. C Mater. Biol. Appl. 2018, 84, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Supuran, C.T. Inhibition of bacterial carbonic anhydrases and zinc proteases: From orphan targets to innovative new antibiotic drugs. Curr. Med. Chem. 2012, 19, 831–844. [Google Scholar] [CrossRef] [PubMed]
- Homzová, K.; Győryová, K.; Hudecová, D.; Koman, M.; Melník, M.; Kovářová, J. Synthesis, thermal, spectral, and biological properties of zinc(II) 4-aminobenzoate complexes. J. Therm. Anal. Calorim. 2017, 129, 1065–1082. [Google Scholar] [CrossRef]
- Zelenák, V.; Györyová, K.; Mlynarcík, D. Antibacterial and antifungal activity of Zinc(II) carboxylates with/without n-donor organic ligands. Met. Based Drugs 2002, 8, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Urdaneta, S.; Wigdahl, B.; Neely, E.B.; Berlin, C.M.; Schengrund, C.L.; Lin, H.M.; Howett, M.K. Inactivation of HIV-1 in breast milk by treatment with the alkyl sulfate microbicide sodium dodecyl sulfate (SDS). Retrovirology 2005, 2, 28. [Google Scholar] [CrossRef]
- Guan, A.; Li, Z.; Phillips, K.S. The effects of non-ionic polymeric surfactants on the cleaning of biofouled hydrogel materials. Biofouling 2015, 31, 689–697. [Google Scholar] [CrossRef]
- United Nations Environment Programme (UNEP). SIDS initial assessment report. Sodium dodecyl sulfate (CAS No. 151-21-3). In Screening Information Data Sheet (SIDS) for High Volume Chemicals; UNEP, OECD, UN, IRPTC, Eds.; United Nations: Geneva, Switzerland, 1997; Volume 4, Part 2; pp. 1–39. [Google Scholar]
- Zilberman, M.; Kraitzer, A.; Grinberg, O.; Elsner, J.J. Drug-eluting medical implants. In Handbook of Experimental Pharmacology; Springer: Berlin/Heidelberg, Germany, 2010; Volume 197, pp. 299–341. [Google Scholar]
- Sainis, I.; Banti, C.N.; Owczarzak, A.M.; Kyros, L.; Kourkoumelis, N.; Kubicki, M.; Hadjikakou, S.K. New antibacterial, non-genotoxic materials, derived from the functionalization of the anti-thyroid drug methimazole with silver ions. J. Inorg. Biochem. 2016, 160, 114–124. [Google Scholar] [CrossRef]
- Kyros, L.; Banti, C.N.; Kourkoumelis, N.; Kubicki, M.; Sainis, I.; Hadjikakou, S.K. Synthesis, characterization, and binding properties towards CT-DNA and lipoxygenase of mixed-ligand silver(I) complexes with 2-mercaptothiazole and its derivatives and triphenylphosphine. J. Biol. Inorg. Chem. 2014, 19, 449–464. [Google Scholar] [CrossRef]
- Stathopoulou, M.-E.K.; Banti, C.N.; Kourkoumelis, N.; Hatzidimitriou, A.G.; Kalampounias, A.G.; Hadjikakou, S.K. Silver complex of salicylic acid and its hydrogel-cream in wound healing chemotherapy. J. Inorg. Biochem. 2018, 181, 41–55. [Google Scholar] [CrossRef]
- Giertsen, E.; Scheie, A.A.; Rölla, G. Plaque inhibition by a combination of zinc citrate and sodium lauryl sulfate. Caries Res. 1989, 23, 278–283. [Google Scholar] [CrossRef]
- Che, P.; Fang, D.; Zhang, D.; Feng, J.; Wang, J.; Hu, N.I.; Meng, J. Hydrothermal synthesis and crystal structure of a new two dimensional zinc citrate complex. J. Coord. Chem. 2005, 58, 1581–1588. [Google Scholar] [CrossRef]
- Abdellah, M.A.; Hadjikakou, S.K.; Hadjiliadis, N.; Kubicki, M.; Bakas, T.; Kourkoumelis, N.; Simos, Y.V.; Karkabounas, S.; Barsan, M.M.; Butler, I.S. Synthesis, characterization, and biological studies of organotin(IV) derivatives with o- or p-hydroxybenzoic acids. Bioinorg. Chem. Appl. 2009, 2009, 542979. [Google Scholar] [CrossRef]
- Wang, L.; Chen, H.; He, Y.-E.; Li, Y.; Li, M.; Li, X. Long chain olefin hydroformylation in biphasic catalytic system—How the reaction is accelerated. Appl. Catal. A 2003, 242, 85–88. [Google Scholar] [CrossRef]
- Gkaniatsou, E.I.; Banti, C.N.; Kourkoumelis, N.; Skoulika, S.; Manoli, M.; Tasiopoulos, A.J.; Hadjikakou, S.K. Novel mixed metal Ag(I)-Sb(III)-metallotherapeutics of the NSAIDs, aspirin and salicylic acid: Enhancement of their solubility and bioactivity by using the surfactant CTAB. J. Inorg. Chem. 2015, 150, 108–119. [Google Scholar] [CrossRef]
- Rub, M.A.; Naqvi, A.Z. Micellization of mixtures of amphiphilic drugs and cationic surfactants: A detailed study. Colloids Surf. B Biointerfaces 2012, 92, 16–24. [Google Scholar]
- Goldshleger, N.F.; Chernyak, A.V.; Kalashnikov, I.P.; Baulin, V.E.; Tsivadze, A.Y. Magnesium Octa (benzo-15-crown-5) phthalocyaninate in the Sodium Dodecyl Sulfate Solutions: A Study Using Electron and 1 H NMR Spectroscopy. Russ. J. Gen. Chem. 2012, 82, 856–865. [Google Scholar] [CrossRef]
- Capone, S.; de Robertis, A.; de Stefano, C.; Sammartano, S. Formation and stability of zinc(II) and cadmium(II) citrate complexes in aqueous solution at various temperatures. Talanta 1986, 33, 763–767. [Google Scholar] [CrossRef]
- Wiegand, I.; Hilpert, K.; Hancock, R.E.W. Agar and broth dilution methods to determine the minimal inhibitory concentration (MIC) of antimicrobial substances. Nat. Protoc. 2008, 3, 163–175. [Google Scholar] [CrossRef]
- Kostenko, V.; Ceri, H.; Martinuzzi, R.J. Increased tolerance of Staphylococcus aureus to vancomycin in Viscous media. FEMS Immunol. Med. Microbiol. 2007, 51, 277–288. [Google Scholar] [CrossRef]
- Motyl, M.; Dorso, K.; Barrett, J.; Giacobbe, R. Basic microbiological techniques used in antibacterial drug discovery. Curr. Protoc. Pharmacol. 2006, 31, 13A-3. [Google Scholar]
- Matuschek, E.; Brown, D.F.J.; Kahlmeter, G. Development of the EUCAST disk diffusion antimicrobial susceptibility testing method and its implementation in routine microbiology laboratories. Clin. Microbiol. Infect. 2014, 20, o255–o266. [Google Scholar] [CrossRef] [PubMed]
- Wayne, P.A.; Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing; approved standard, 25th Informational Supplement, CLSI document M100-S25; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2015. [Google Scholar]
- Doroshenko, N.; Rimmer, S.; Hoskins, R.; Garg, P.; Swift, T.; Spencer, H.L.M.; Lord, R.M.; Katsikogianni, M.; Pownall, D.; MacNeil, S.; et al. Antibiotic functionalised polymers reduce bacterial biofilm and bioburden in a simulated infection of the cornea. Biomater. Sci. 2018, 6, 2101–2109. [Google Scholar] [CrossRef] [Green Version]
- Rigaku, M.S. CrystalClear; Rigaku/MSC Inc.: The Woodlands, TX, USA, 2005. [Google Scholar]








| Compound | Gram-Positive | Gram-Negative | ||
|---|---|---|---|---|
| St. epidermidis | St. aureus | PAO1 | E. coli | |
| MIC (μΜ) | ||||
| 1 | 119.2 ± 18.1 | 183.3 ± 31.4 | >250 | >250 |
| 2 | 11.7 ± 2.1 | 8.5 ± 0.3 | 228.5 ± 4.6 | 14.9 ± 0.4 |
| SLS | 49.7 ± 0.4 | 42.9 ± 6.2 | >250 | 39.8 ± 0.6 |
| CitH4 | >250 | >250 | >250 | >250 |
| MBC (μΜ) | ||||
| 1 | 201.7 | >250 | >250 | >250 |
| 2 | 13.4 | 12 | >250 | >250 |
| SLS | 100 | 60 | >250 | >250 |
| CitH4 | >250 | >250 | >250 | >250 |
| MBC/MIC | ||||
| 1 | 1.69 | ND | ND | ND |
| 2 | 1.15 | 1.41 | ND | ND |
| SLS | 2.01 | 1.40 | ND | ND |
| CitH4 | ND | ND | ND | ND |
| IZ (mm) | ||||
| 1 | ND | ND | ND | ND |
| 2 | 23.0 ± 2.0 | 30.5 ± 5.4 | ND | 26.5 ± 1.3 |
| SLS | ND | ND | ND | ND |
| CitH4 | ND | ND | ND | ND |
| 3 | 14.0 ± 2.8 | 17.0 ± 1.4 | ND | ND |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karetsi, V.A.; Banti, C.N.; Kourkoumelis, N.; Papachristodoulou, C.; Stalikas, C.D.; Raptopoulou, C.P.; Psycharis, V.; Zoumpoulakis, P.; Mavromoustakos, T.; Sainis, I.; et al. An Efficient Disinfectant, Composite Material {SLS@[Zn3(CitH)2]} as Ingredient for Development of Sterilized and Non Infectious Contact Lens. Antibiotics 2019, 8, 213. https://doi.org/10.3390/antibiotics8040213
Karetsi VA, Banti CN, Kourkoumelis N, Papachristodoulou C, Stalikas CD, Raptopoulou CP, Psycharis V, Zoumpoulakis P, Mavromoustakos T, Sainis I, et al. An Efficient Disinfectant, Composite Material {SLS@[Zn3(CitH)2]} as Ingredient for Development of Sterilized and Non Infectious Contact Lens. Antibiotics. 2019; 8(4):213. https://doi.org/10.3390/antibiotics8040213
Chicago/Turabian StyleKaretsi, V.A., C.N. Banti, N. Kourkoumelis, C. Papachristodoulou, C.D. Stalikas, C.P. Raptopoulou, V. Psycharis, P. Zoumpoulakis, T. Mavromoustakos, I. Sainis, and et al. 2019. "An Efficient Disinfectant, Composite Material {SLS@[Zn3(CitH)2]} as Ingredient for Development of Sterilized and Non Infectious Contact Lens" Antibiotics 8, no. 4: 213. https://doi.org/10.3390/antibiotics8040213







