Perspectives in Prevention of Biofilm for Medical Applications
Abstract
:1. Introduction
2. Issues of Bacterial Biofilm
3. Methods of Prevent Creating of Biofilm Based on Different Authors
3.1. Antibiotics Therapy and Silver Modification
3.2. Surface Modification
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bartoszewicz, M.; Rygiel, A. Biofilm as the basic mechanism of surgical site infection—Prevention methods in local treatment. Pol. Surg. 2006, 8, 171–178. [Google Scholar]
- Percival, S.L.; Malic, S.; Cruz, H.; Williams, D.W. Introduction to Biofilms. In Biofilms and Veterinary Medicine; Springer: New York, NY, USA, 2011; pp. 41–68. [Google Scholar]
- Wolska, K.I.; Markowska, K.; Wypij, M.; Golińska, P.; Dahm, H. Nanocząstki srebra, synteza i biologiczna aktywn-ość. Kosm. 2017, 66, 125–138. [Google Scholar]
- Maciejewska, M.; Bauer, M.; Dawgul, M. Nowoczesne metody zwalczania biofilmu bakteryjnego. Postępy Mikrobiol. 2016, 55, 3–11. [Google Scholar]
- Phillips, P.; Wolcott, R.; Fletcher, J.; Schultz, G. Biofim made easy. Wounds Int. 2010, 1, 1–5. [Google Scholar]
- Strzelec-Nowak, D.; Bogut, A.; Niedźwiadek, J.; Kozioł-Montewka, M.; Sikora, A. Mikrobiologiczna diagnostyka zakażeń implantów stawu biodrowego. Postepy Mikrobiol. 2012, 51, 219–225. [Google Scholar]
- Markowska, K. Antybakteryjne Działanie Nanocząstek Srebra—Wpływ na Strukturę i Funkcje Komórek Bakteryjnych. Ph.D. Thesis, Warsaw University, Warsaw, Poland, 2016. [Google Scholar]
- Wróblewska, M.; Strużycka, I.; Mierzwińska-Nastalska, E. Znaczenie biofilmów w stomatologii. Przegl. Epidemiol. 2015, 69, 879–883. [Google Scholar]
- Huang, Z.; Nazifi, S.; Jafari, P.; Karim, A.; Ghasemi, H. Networked Zwitterionic Durable Antibacterial Surfaces. ACS Appl. Bio. Mater. 2020, 3, 911–919. [Google Scholar] [CrossRef] [PubMed]
- Forum Leczenia Ran. Przełom w Walce z Biofilmem. Available online: http://forumleczeniaran.pl/przelom-w-walce-z-biofilmem/ (accessed on 1 December 2021).
- Bi, Y.; Xia, G.; Shi, C.; Wan, J.; Liu, L.; Chen, Y.; Wu, Y.; Zhang, W.; Zhou, M.; He, H.; et al. Therapeutic strategies against bacterial biofilms. Fundam. Res. 2021, 1, 193–212. [Google Scholar] [CrossRef]
- Szewczyk, M.T.; Cwajda-Białasik, J.; Mościcka, P.; Jawień, A.; Gospodarek, E.; Deptuła, A.; Kózka, M.; Szopiński, J.; Mikucka, A.; Cierzniakowska, K.; et al. Recommendations for the prevention of surgical site infections and use of antibiotic therapy during preoperative nursing care in surgery departments. Pielęgniarstwo Chir. Angiol. 2015, 2, 39–55. [Google Scholar]
- Bratzler, D.W.; Dellinger, E.P.; Olsen, K.M.; Perl, T.M.; Auwaerter, P.G.; Bolon, M.K.; Fish, D.N.; Napolitano, L.M.; Sawyer, R.G.; Slain, D.; et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am. J. Health Pharm. 2013, 70, 195–283. [Google Scholar] [CrossRef] [Green Version]
- Hryniewicz, W.; Kulig, J.; Ozorowski, T. Stosowanie Antybiotyków w Profilaktyce Okołooperacyjnej; National Medicines Institute: Warsaw, Poland, 2011. [Google Scholar]
- Wan, Y.Z.; Raman, S.; He, F.; Huang, Y. Surface modification of medical metals by ion implantation of silver and copper. Vacuum 2007, 81, 1114–1118. [Google Scholar] [CrossRef]
- Wojcieszak, D.; Domaradzki, J.; Mazur, M. Influence of Cu and Nb additives on specific surface properties and bio-logical activity of transparent TiO2 thin-film coatings. Polim. Med. 2013, 43, 141–146. [Google Scholar]
- Wojcieszak, D.; Kaczmarek, D.; Adamiak, B.; Domaradzki, J.; Mazur, M.; Jankowska, D.; Gamian, A.; Antosiak, A.; Szponar, B. Wpływ dodatków Cu i Nb na właściwości powierzchni właściwej oraz aktywność bakteriobójczą przezroczystych powłok cien-kowarstwowych TiO2. Polim. Med. 2013, 43, 141–146. [Google Scholar]
- El Habnouni, S.; Lavigne, J.P.; Darcos, V.; Porsio, B.; Garric, X.; Coudane, J.; Nottelet, B. Toward potent antibiofilm degradable medical devices: A generic method for the antibacterial surface modification of polylactide. Acta Biomater. 2013, 9, 7709–7718. [Google Scholar] [CrossRef]
- El Habnouni, S.; Darcos, V.; Garric, X.; Lavigne, J.P.; Nottelet, B.; Coudane, J. Mild methodology for the versatile chemical modification of polylactide surfaces: Original combination of anionic and click chemistry for biomedical applications. Adv. Funct. Mater. 2011, 21, 3321–3330. [Google Scholar] [CrossRef]
- Sintubin, L.; Verstraete, W.; Boon, N. Biologically produced nanosilver: Current state and future perspectives. Bio-Technol. Bioeng. 2012, 109, 2422–2436. [Google Scholar] [CrossRef]
- Lemire, J.A.; Harrison, J.J.; Turner, R.J. Antimicrobial activity of metals: Mechanisms, molecular targets and applications. Nat. Rev. Microbiol. 2013, 11, 371–384. [Google Scholar] [CrossRef]
- Czaplewski, L.; Bax, R.; Clokie, M.; Dawson, M.; Fairhead, H.; Fischetti, V.A.; Foster, S.; Gilmore, B.F.; Hancock, R.E.W.; Harper, D.; et al. Alternatives to antibiotics-a pipeline portfolio review. Lancet Infect. Dis. 2016, 16, 239–251. [Google Scholar] [CrossRef] [Green Version]
- Ziąbka, M.; Mertas, A.; Król, W. Poly(lactide-co-glycolide) composites containing antibacterial silver nanoparticles: In vitro preliminary study. Compos. Theory Pract. 2014, 14, 155–162. [Google Scholar]
- Marambio-Jones, C.; Hoek, E.M.V. A review of the antibacterial effects of silver nanomaterials and potential implications for human health and the environment. J. Nanoparticle Res. 2010, 12, 1531–1551. [Google Scholar] [CrossRef]
- Schierholz, J.M.; Lucas, L.J.; Rump, A.; Pulverer, G. Efficacy of silver-coated medical devices. J. Hosp. Infect. 1998, 40, 257–262. [Google Scholar] [CrossRef]
- Pupka, A.; Skóra, J.; Jańczak, D. Leczenie masywnego zakażenia w chirurgii naczyniowej przy użyciu protezy dakronowej, uszczelnianej kolagenem i impregnowanej solami srebra. Polim. Med. 2003, 23, 41–56. [Google Scholar]
- Kinney, E.V.; Bandyk, D.F.; Seabrook, G.A.; Kelly, H.M.; Towne, J.B. Antibiotic-bonded PTFE vascular grafts: The effect of silver antibiotic on bioactivity following implantation. J. Surg. Res. 1991, 50, 430–435. [Google Scholar] [CrossRef]
- Darxouiche, R.O. Anti-infective efficacy of silver-coated medical prostheses. Clin. Infect. Dis. 1999, 29, 1371–1377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Novali, C. Omoinnesti vascolari: Strategia e tattica operatoria. Ann. Ital. Chir. 2001, 72, 2. [Google Scholar]
- Goëau-Brissonnièrc, O.A.; Fabre, D.; Leflon-Guibout, V.; Di Centa, I.; Nicolas-Chanoine, M.H.; Coggia, M. Comparison of the resistance to infection of rifampin-bonded gelatin-sealed and silver/collagen-coated polyester prostheses. J. Vasc. Surg. 2002, 35, 1260–1263. [Google Scholar] [CrossRef] [Green Version]
- Shah, S.R.; Kasper, F.K.; Mikos, A.G. Perspectives on the prevention and treatment of infection for orthopedic tissue engineering applications. In Proceedings of the 9th World Biomaterials Congress: Innovative Biomaterials and Crossing Frontiers I Biomaterials and Regenerative Medicine, Chengdu, China, 1–5 June 2012. [Google Scholar]
- Raczkowska, J.; Stetsyshyn, Y.; Awsiuk, K.; Brzychczy-Włoch, M.; Gosiewski, T.; Jany, B.; Lishchynskyi, O.; Shymborska, Y.; Nastyshyn, S.; Bernasik, A.; et al. “Command” surfaces with thermo-switchable antibacterial activity. Mater. Sci. Eng. C. 2019, 103, 109806. [Google Scholar] [CrossRef] [PubMed]
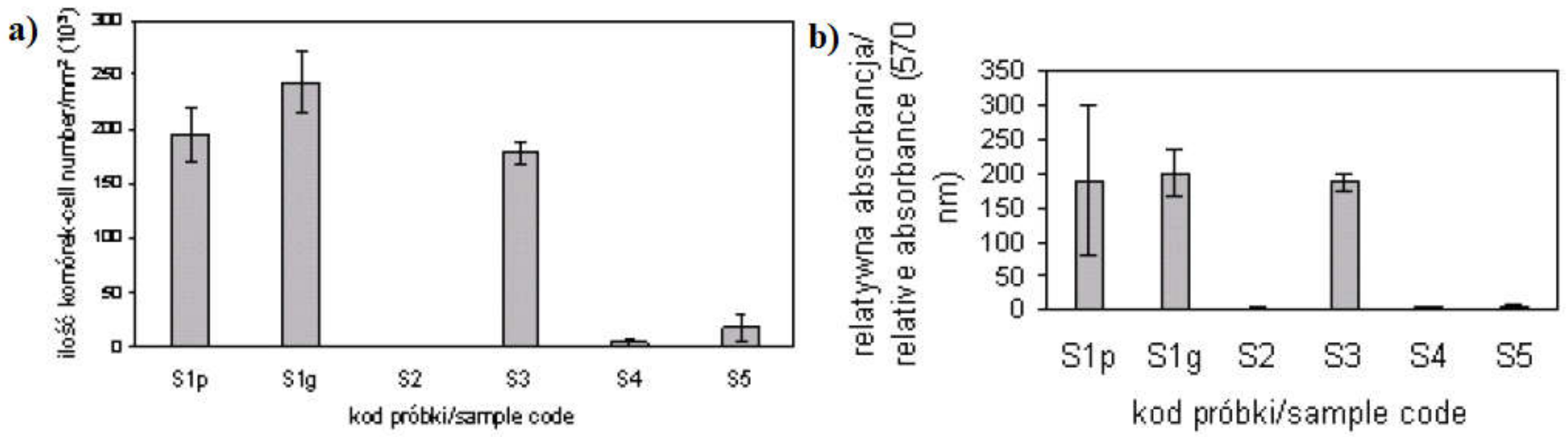
- Sowińska, A.; Zajączkowska, A.; Cukrowska, B.; Wierzchoń, T.; Sobiecki, R.; Czarnowska, E. The effect of TiN on formed biofilm and cel behaviour in vitro. Eng. Biomater. 2004, 38–43, 120–123. [Google Scholar]
- Majkowska-Marzec, B.; Mazurowska, J.; Bartmański, M.; Rogala-Wielgus, D. Modyfikacja powierzchni stopu Ti13Nb13Zr z wykorzystaniem nanorurek węglowych. In Proceedings of the I Nationwide Scientific Conference on IMPLANTS, Gdańsk, Poland, 28 June 2018. [Google Scholar]
- Thukkaram, M.; Sitaram, S.; Kannaiyan, S.K.; Subbiahdoss, G. Antibacterial Efficacy of Iron-Oxide Nanoparticles against Biofilms on Different Biomaterial Surfaces. Int. J. Biomater. 2014, 2014, 716080. [Google Scholar] [CrossRef] [Green Version]
- Bartoszewicz, M.; Rygiel, A.; Krzemiński, M.; Przondo-Mordarska, A. Penetracja wybranego antybiotyku i antyseptyku w biofilmie tworzonym na stalowych wszczepach stosowanych w ortopedii. Ortop. Traumatol. Rehabil. 2007, 9, 310–318. [Google Scholar]
- Lisoń, J.; Taratuta, A.; Paszenda, Z.; Dyner, M.; Basiaga, M. A study on the physicochemical properties of surface modified Ti13Nb13Zr alloy for skeletal implants. Acta Bioeng. Biomech. 2021, 24, 1. [Google Scholar]
- Belcarz, A.; Bieniaś, J.; Surowska, B.; Ginalska, G. Adhesion of Staphylococcus epidermidis cells on Ti6Al4V titanium alloy surfaces modified by bioceramic layers. Eng. Biomater. 2009, 12, 244–246. [Google Scholar]
- Reśliński, A.; Dabrowiecki, S. Evaluation of the effect of glucose on Staphylococcus aureus and Escherichia coli bio-film formation on the surface of polypropylene mesh. Med. Dosw. Mikrobiol. 2013, 65, 19–26. [Google Scholar]
- Gallimore, B.; Gagnon, R.F.; Subang, R.; Richards, G.K. Natural history of chronic Staphylococcus epidermidis foreign body infection in a mouse model. J. Infect. Dis. 1991, 164, 1220–1223. [Google Scholar] [CrossRef]
- Engelsman, A.F.; van der Mei, H.C.; Busscher, H.J.; Ploeg, R.J. Morphological aspects of surgical meshes as a risk factor for bacterial colonization. Br. J. Surg. 2008, 95, 1051–1059. [Google Scholar] [CrossRef]
- Engelsman, A.F.; van Dam, G.M.; van der Mei, H.C.; Busscher, H.J.; Ploeg, R.J. In vivo evaluation of bacterial infection involving morphologically different surgical meshes. Ann. Surg. 2010, 251, 133–137. [Google Scholar] [CrossRef]
- Karakeçili, A.G.; Gümüşderelioglu, M. Comparison of bacterial and tissue cell initial adhesion on hydrophilic/hydrophobic biomaterials. J. Biomater. Sci. Polym. Ed. 2002, 13, 185–196. [Google Scholar] [CrossRef]
- Kiremitci-Gumusderelioglu, M.; Pesmen, A. Microbial adhesion to ionogenic PHEMA, PU and PP implants. Biomaterials 1996, 17, 443–449. [Google Scholar] [CrossRef]
- Dickson, J.S.; Koohmaraie, M. Cell surface charge characteristics and their relationship to bacterial attachment to meat surfaces. Appl. Environ. Microbiol. 1989, 55, 832–836. [Google Scholar] [CrossRef] [Green Version]
- Cerca, N.; Pier, G.B.; Vilanova, M.; Oliveira, R.; Azeredo, J. Quantitative analysis of adhesion and biofilm formation on hydrophilic and hydrophobic surfaces of clinical isolates of Staphylococcus epidermidis. Res. Microbiol. 2005, 156, 506–514. [Google Scholar] [CrossRef] [Green Version]
- Gungor, B.; Esen, S.; Gök, A.; Yılmaz, H.; Malazgirt, Z.; Leblebicioğlu, H. Comparison of the adherence of E.Coli and S. Aureus to ten different prosthetic mesh grafts: In vitro experimental study. Indian J. Surg. 2010, 72, 226–231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bellón, J.M.; G-Honduvilla, N.; Jurado, F.; Carranza, A.; Buján, J. In vitro interaction of bacteria with polypropylene/ePTFE prostheses. Biomater. 2001, 22, 2021–2024. [Google Scholar] [CrossRef]
- Łukomska-Szymańska, M.; Cajdler, M.; Klimek, L.; Sokołowski, J. Evaluation of bacterial adhesion to nanocrystal-line diamond coated cobalt-chromium dental alloy. Dent. Med. Probl. 2009, 46, 424–430. [Google Scholar]
- Basiaga, M.; Walke, W.; Staszuk, M.; Kajzer, W.; Kajzer, A.; Nowińska, K. Influence of ALD process parameters on the physical and chemical properties of the surface of vascular stents. Arch. Civ. Mech. 2017, 17, 32–42. [Google Scholar] [CrossRef]
- Pupka, A.; Barć, P.; Kałuża, G.; Dawiskiba, T.; Szyber, P. Ocena wgajania dakronowej protezy naczyniowej impregnowanej solami srebra i uszczelnianej kolagenem w leczeniu zakażeń w chirurgii naczyniowej. Inż. Biomater. 2003, 6, 18–20. [Google Scholar]
- Pupka, A.; Abrahamów, A.; Szyber, P. Biomateriały i materiał tkankowy w leczeniu zakażeń protez naczyniowych. Polim. Med. 2005, 35, 41–47. [Google Scholar]
- Sypniewska-Kawka, D.; Paszyńska, E. The possibilities of using nanotechnology in dentistry. Dent. Forum 2016, 44, 53–58. [Google Scholar]
- Boryło, P.; Matus, K.; Lukaszkowicz, K.; Kubacki, J.; Balin, K.; Basiaga, M.; Szindler, M.; Mikuła, J. The influence of atomic layer deposition process temperature on ZnO thin film structure. Appl. Surf. Sci. 2019, 474, 177–186. [Google Scholar] [CrossRef]
- Das Neves, P.B.; Agnelli, J.A.; Kurachi, C.; de Souza, C.W. Addition of silver nanoparticles to composite resin: Effect on physical and bactericidal properties in vitro. Braz. Dent. J. 2014, 25, 141–145. [Google Scholar] [CrossRef] [Green Version]
- Li, F.; Weir, M.D.; Fouad, A.F.; Xu, H.H. Effect of salivary pellicle on antibacterial activity of novel antibacterial dental adhesives using a dental plaque microcosm biofilm model. Dent. Mater. 2014, 30, 182–191. [Google Scholar] [CrossRef] [Green Version]
- Esteban, J.; Gomez-Barrena, E.; Cordero, J.; Martín-de-Hijas, N.Z.; Kinnari, T.J.; Fernandez-Roblas, R. Evaluation of quantitative analysis of cultures from sonicated retrieved orthopedic implants in diagnosis of orthopedic infection. J. Clin. Microbiol. 2008, 46, 488–492. [Google Scholar] [CrossRef] [Green Version]
- Gallo, J.; Holinka, M.; Moucha, C.S. Antibacterial surface treatment for orthopaedic implants. Int. J. Mol. Sci. 2014, 15, 13849–13880. [Google Scholar] [CrossRef] [Green Version]
- Holinka, J.; Bauer, L.; Hirschl, A.M.; Graninger, W.; Windhager, R.; Presterl, E. Sonication cultures of explanted components as an add-on test to routinely conducted microbiological diagnostics improve pathogen detection. J. Orthop. Res. 2011, 29, 617–622. [Google Scholar] [CrossRef]
- Monsen, T.; Lövgren, E.; Widerström, M.; Wallinder, L. In vitro effect of ultrasound on bacteria and suggested pro-tocol for sonication and diagnosis of prosthetic infections. J. Clin. Microbiol. 2009, 47, 2496–2501. [Google Scholar] [CrossRef] [Green Version]
- Parvizi, J.; Zmistowski, B.; Berbari, E.F.; Bauer, T.W.; Springer, B.D.; Della Valle, C.J.; Garvin, K.L.; Mont, M.A.; Wongworawat, M.D.; Zalavras, C.G. New definition for periprosthetic joint infection: From the Workgroup of the Musculoskeletal Infection Society. J. Arthroplast. 2011, 469, 2992–2994. [Google Scholar] [CrossRef] [Green Version]
- Pokrowiecki, R.; Szaraniec, B.; Chłopek, J.; Zaleska, M. Recent trends in surface modification of the titanium bio-materials used for endoosseus dental implants. Eng. Biomater. 2014, 17, 2–10. [Google Scholar]
- Puckett, S.D.; Taylor, E.; Raimondo, T.; Webster, T.J. The relationship between the nanostructure of titanium surfaces and bacterial attachment. Biomater. 2010, 31, 706–713. [Google Scholar] [CrossRef]
- Whitehead, K.A.; Colligon, J.; Verran, J. Retention of microbial cells in substratum surface features of micrometer and sub-micrometer dimensions. Colloids Surf. B Biointerfaces 2005, 41, 129–138. [Google Scholar] [CrossRef]
- Campoccia, D.; Montanaro, L.; Agheli, H.; Sutherland, D.S.; Pirini, V.; Donati, M.E.; Arciola, C.R. Study of Staphylococcus aureus adhesion on a novel nanostructured surface by chemiluminometry. Int. J. Artif. Organs. 2006, 29, 622–629. [Google Scholar] [CrossRef]
- Díaz, C.; Schilardi, P.L.; Salvarezza, R.C.; De Mele, M.F.L. Nano/microscale order affects the early stages of biofilm formation on metal surfaces. Langmuir 2007, 23, 11206–11210. [Google Scholar] [CrossRef]
- Harris, L.G.; Mead, L.; Müller-Oberländer, E.; Richards, R.G. Bacteria and cell cytocompatibility studies on coated medical grade titanium surfaces. J. Biomed. Mater. Res. A. 2006, 78, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Maddikeri, R.R.; Tosatti, S.; Schuler, M.; Chessari, S.; Textor, M.; Richards, R.G.; Harris, L.G. Reduced medical infection related bacterial strains adhesion on bioactive RGD modified titanium surfaces: A first step toward cell selective surfaces. J. Biomed. Mater. Res. A. 2008, 84, 425–435. [Google Scholar] [CrossRef] [PubMed]
- Price, J.S.; Tencer, A.F.; Arm, D.M.; Bohach, G.A. Controlled release of antibiotics from coated orthopedic implants. J. Biomed. Mater. Res. 1996, 30, 281–286. [Google Scholar] [CrossRef]
- Lucke, M.; Schmidmaier, G.; Sadoni, S.; Wildemann, B.; Schiller, R.; Haas, N.P.; Raschke, M. Gentamicin coating of metallic implants reduces implant-related osteomyelitis in rats. Bone 2003, 32, 521–531. [Google Scholar] [CrossRef]
- Nałęcz, M. Biocybernetyka i Inżynieria Biomedyczna 2000; EXIT: Warsaw, Poland, 2003. [Google Scholar]
- Oleszkiewicz, A.; Korzekwa, K.; Bugia-Płoskońska, G. Nanocząsteczki w biologii i medycynie. Lab. Med. 2008, 5, 30–33. [Google Scholar]
- Cho, K.H.; Park, J.E.; Osaka, T.; Park, S.G. The study of antimicrobial activity and preservative effects of nanosilver ingredient. Electrochim. Acta. 2005, 51, 956–960. [Google Scholar] [CrossRef]
- Zalas-Wiecek, P.; Gospodarek, E.; Piecyk, K. Adhezja pałeczek Escherichia coli do cewników moczowych [Adhesion of Escherichia coli rods to urological catheters]. Med. Dosw. Mikrobiol. 2009, 61, 335–341. [Google Scholar]
- Paduch, D.; Niedzielski, J. Materiały biomedyczne: Część II: Ocena przyczepności pałeczki okrężnicy do materiałów biomedycznych w oryginalnym dynamicznym układzie przepływowym. Chir. Pol. 2005, 7, 252–256. [Google Scholar]
- Wolska, K.; Jakubczak, A. Wykrywanie biofilmu Pseudomonas aeruginosa na biomateriałach medycznych [Detection of Pseudomonas aeruginosa biofilm on medical biomaterials]. Med. Dosw. Mikrobiol. 2003, 55, 371–378. [Google Scholar]
- Rózalska, B.; Sadowska, B.; Wieckowska, M.; Rudnicka, W. Wykrywanie biofilmu bakteryjnego na biomateriałach medycznych [Detection of bacterial biofilm on medical biomaterials]. Med. Dosw. Mikrobiol. 1998, 50, 115–122. [Google Scholar]
- Ahmadabadi, H.Y.; Yu, K.; Kizhakkedathu, J.N. Surface modification approaches for prevention of implant associated infec-tions. Colloids Surf. B Biointerfaces 2020, 193, 111116. [Google Scholar] [CrossRef]
- Geddes, A. Infection in the twenty-first century: Predictions and postulates. J. Antimicrob. Chemother. 2000, 46, 873–877. [Google Scholar] [CrossRef] [Green Version]
- Bryers, J.D. Medical biofilms. Biotechnol. Bioeng. 2008, 100, 1–18. [Google Scholar] [CrossRef]
- Poirel, L.; Karim, A.; Mercat, A.; Le Thomas, I.; Vahaboglu, H.; Richard, C.; Nordmann, P. Extended-spectrum beta-lactamase-producing strain of Acinetobacter baumannii isolated from a patient in France. J. Antimicrob. Chemother. 1999, 43, 157–158. [Google Scholar] [CrossRef]
- Schierholz, J.M.; Beuth, J. Implant infections: A haven for opportunistic bacteria. J. Hosp. Infect. 2001, 49, 87–93. [Google Scholar] [CrossRef]
- Høiby, N.; Ciofu, O.; Johansen, H.K.; Song, Z.J.; Moser, C.; Jensen, P.Ø.; Molin, S.; Givskov, M.; Tolker-Nielsen, T.; Bjarnsholt, T. The clinical impact of bacterial biofilms. Int. J. Oral Sci. 2011, 3, 55–65. [Google Scholar] [CrossRef] [Green Version]
- Jensen, P.Ø.; Bjarnsholt, T.; Phipps, R.; Rasmussen, T.B.; Calum, H.; Christoffersen, L.; Moser, C.; Williams, P.; Pressler, T.; Givskov, M.; et al. Rapid necrotic killing of polymorphonuclear leukocytes is caused by quorum-sensing-controlled production of rhamnolipid by Pseudomonas aeruginosa. Microbiology 2007, 153, 1329–1338. [Google Scholar] [CrossRef] [Green Version]
- Bjarnsholt, T.; Jensen, P.Ø.; Burmølle, M.; Hentzer, M.; Haagensen, J.A.J.; Hougen, H.P.; Calum, H.; Madsen, K.G.; Moser, C.; Molin, S.; et al. Pseudomonas aeruginosa tolerance to tobramycin, hydrogen peroxide and polymorphonuclear leukocytes is quorum-sensing dependent. Microbiology 2005, 151, 373–383. [Google Scholar] [CrossRef] [Green Version]
- Lin, Y.S.; Vidic, R.D.; Stout, J.E.; Yu, V.L. Negative effect of high pH on biocidal efficacy of copper and silver ions in controlling Legionella pneumophila. Appl. Environ. Microbiol. 2002, 68, 2711–2715. [Google Scholar] [CrossRef] [Green Version]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lisoń, J.; Taratuta, A.; Paszenda, Z.; Szindler, M.; Basiaga, M. Perspectives in Prevention of Biofilm for Medical Applications. Coatings 2022, 12, 197. https://doi.org/10.3390/coatings12020197
Lisoń J, Taratuta A, Paszenda Z, Szindler M, Basiaga M. Perspectives in Prevention of Biofilm for Medical Applications. Coatings. 2022; 12(2):197. https://doi.org/10.3390/coatings12020197
Chicago/Turabian StyleLisoń, Julia, Anna Taratuta, Zbigniew Paszenda, Magdalena Szindler, and Marcin Basiaga. 2022. "Perspectives in Prevention of Biofilm for Medical Applications" Coatings 12, no. 2: 197. https://doi.org/10.3390/coatings12020197
APA StyleLisoń, J., Taratuta, A., Paszenda, Z., Szindler, M., & Basiaga, M. (2022). Perspectives in Prevention of Biofilm for Medical Applications. Coatings, 12(2), 197. https://doi.org/10.3390/coatings12020197






