A Polymer-Infiltrated Ceramic as Base Adherent in an Experimental Specimen Model to Test the Shear Bond Strength of CAD-CAM Monolithic Ceramics Used in Resin-Bonded Dental Bridges
Abstract
:1. Introduction
2. Research Significance
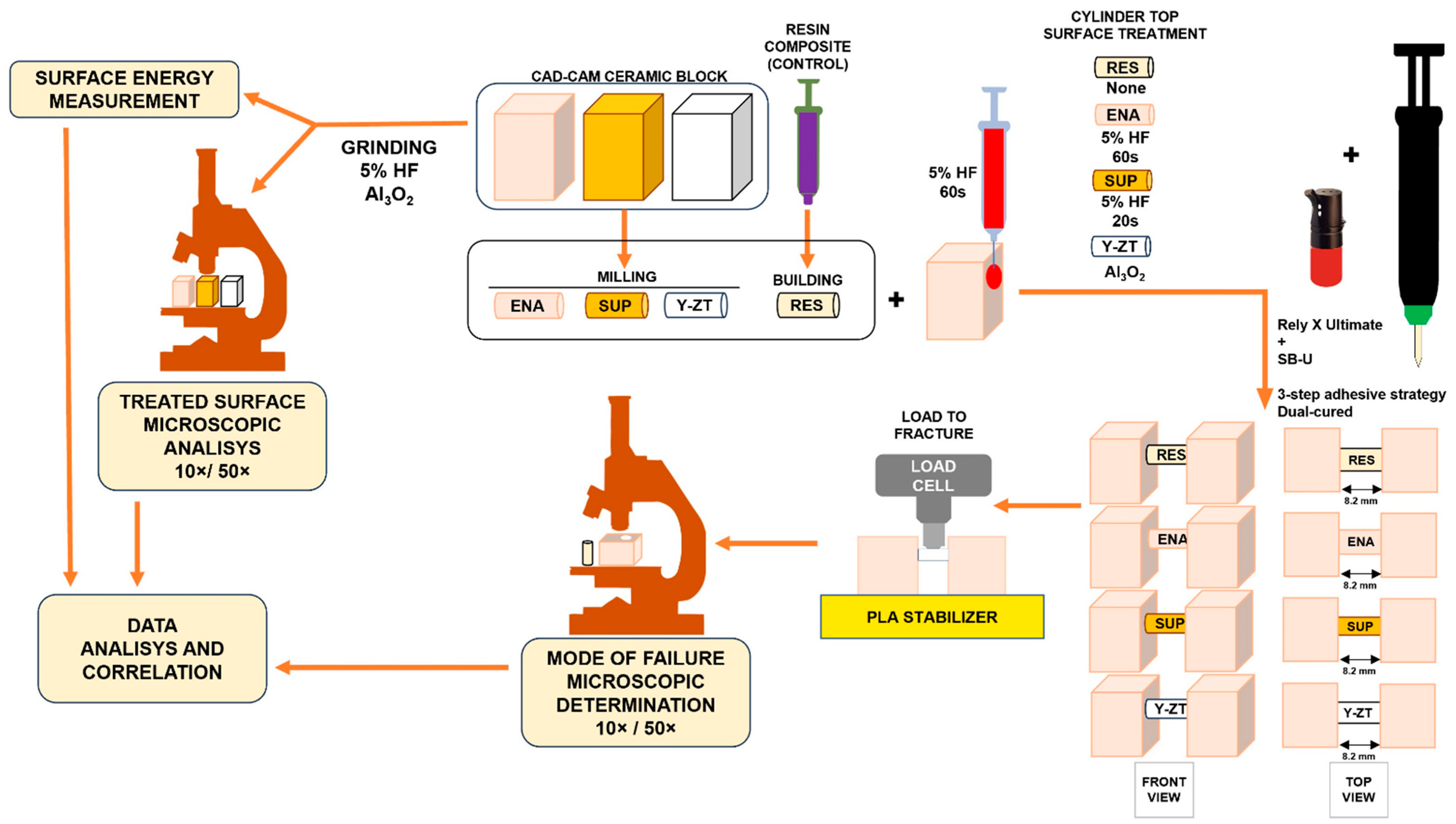
3. Materials and Methods
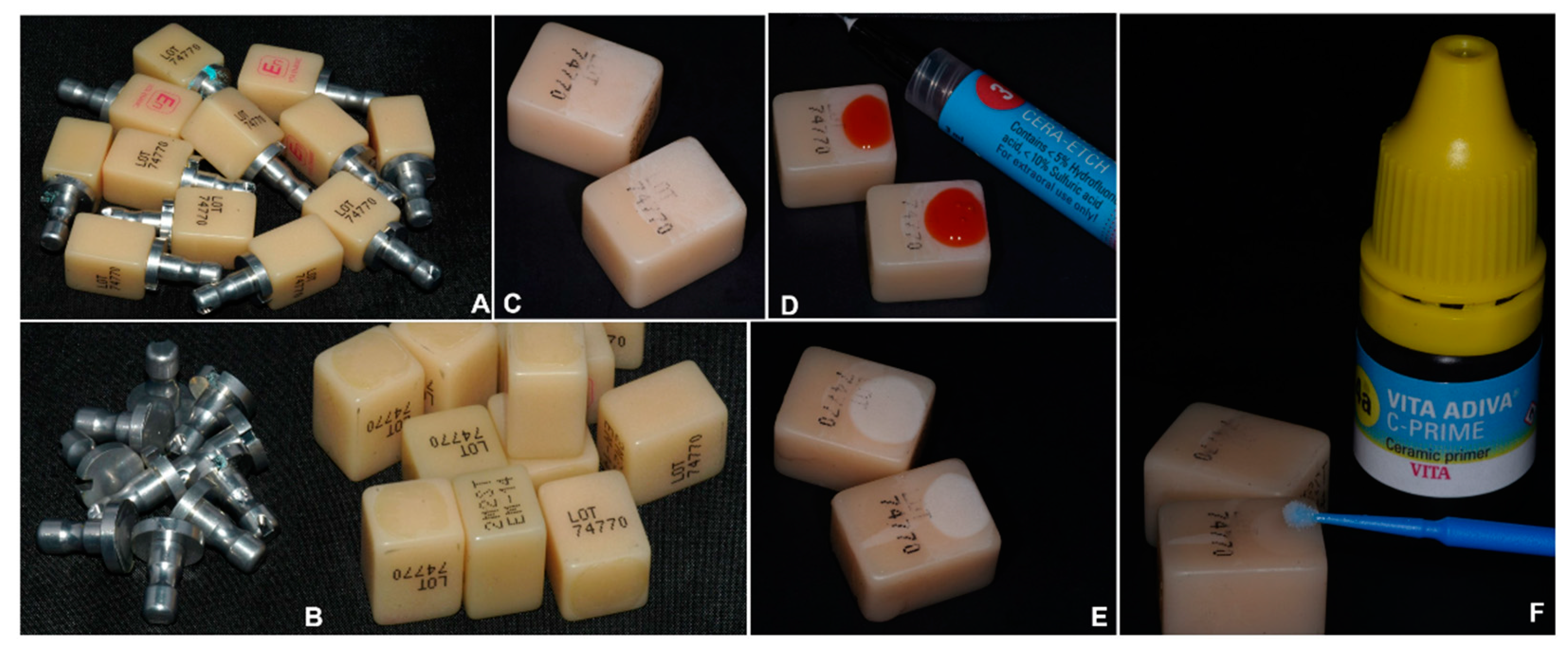
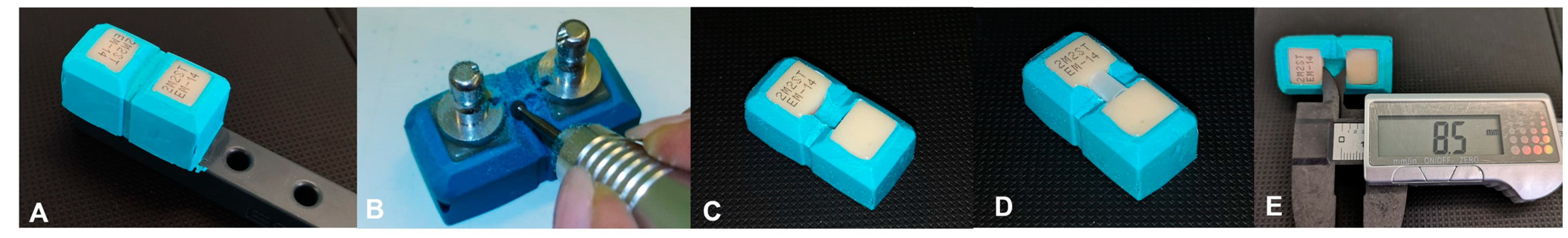
3.1. Preparation of the Bases Adherend
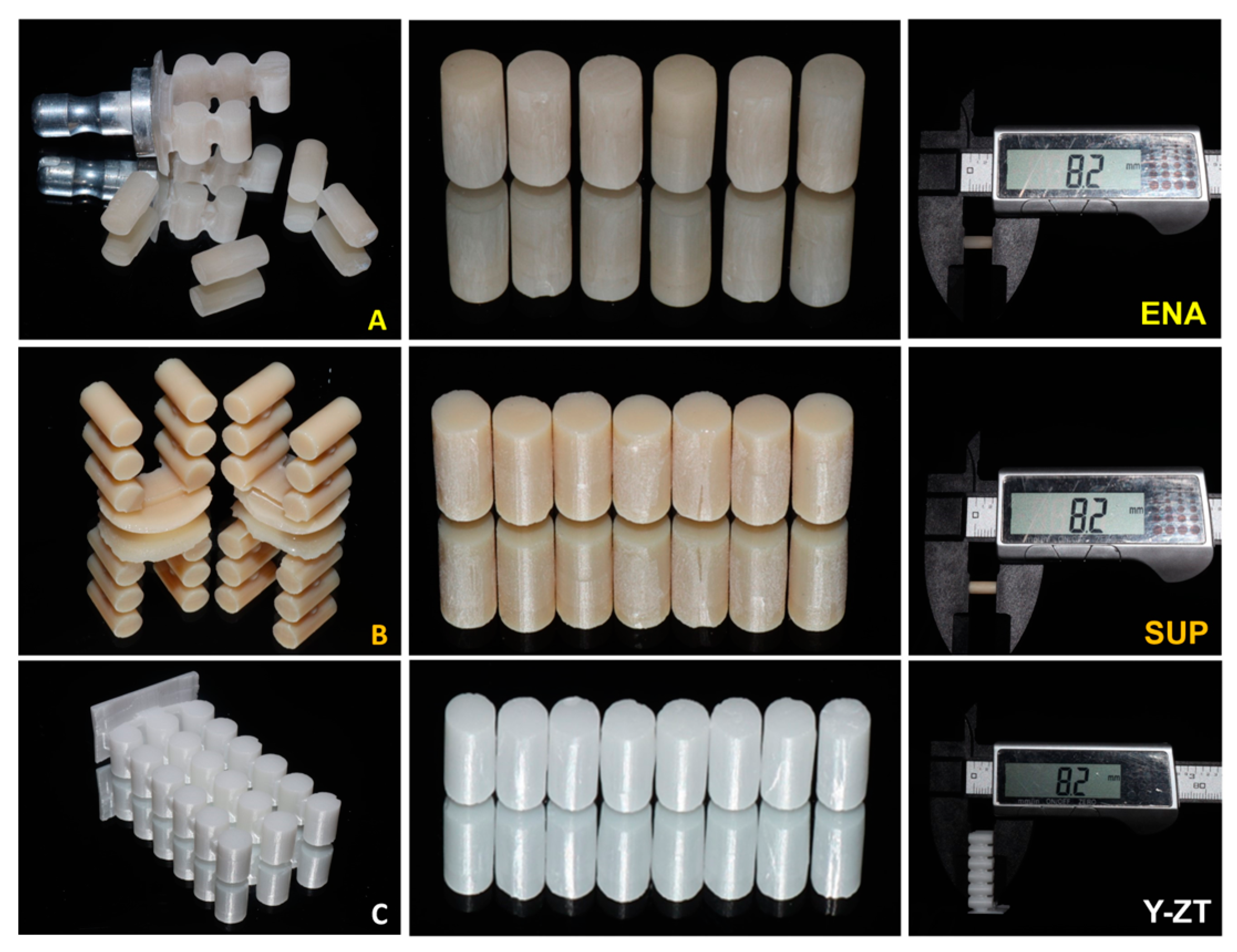
3.2. Preparation of the Cylinders
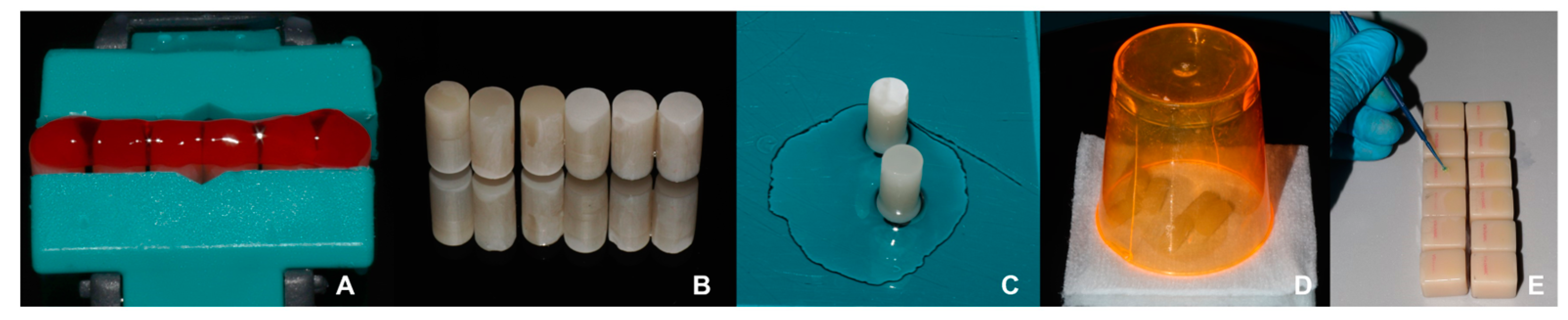
3.3. Specimens Assembling for Shear Strength Test
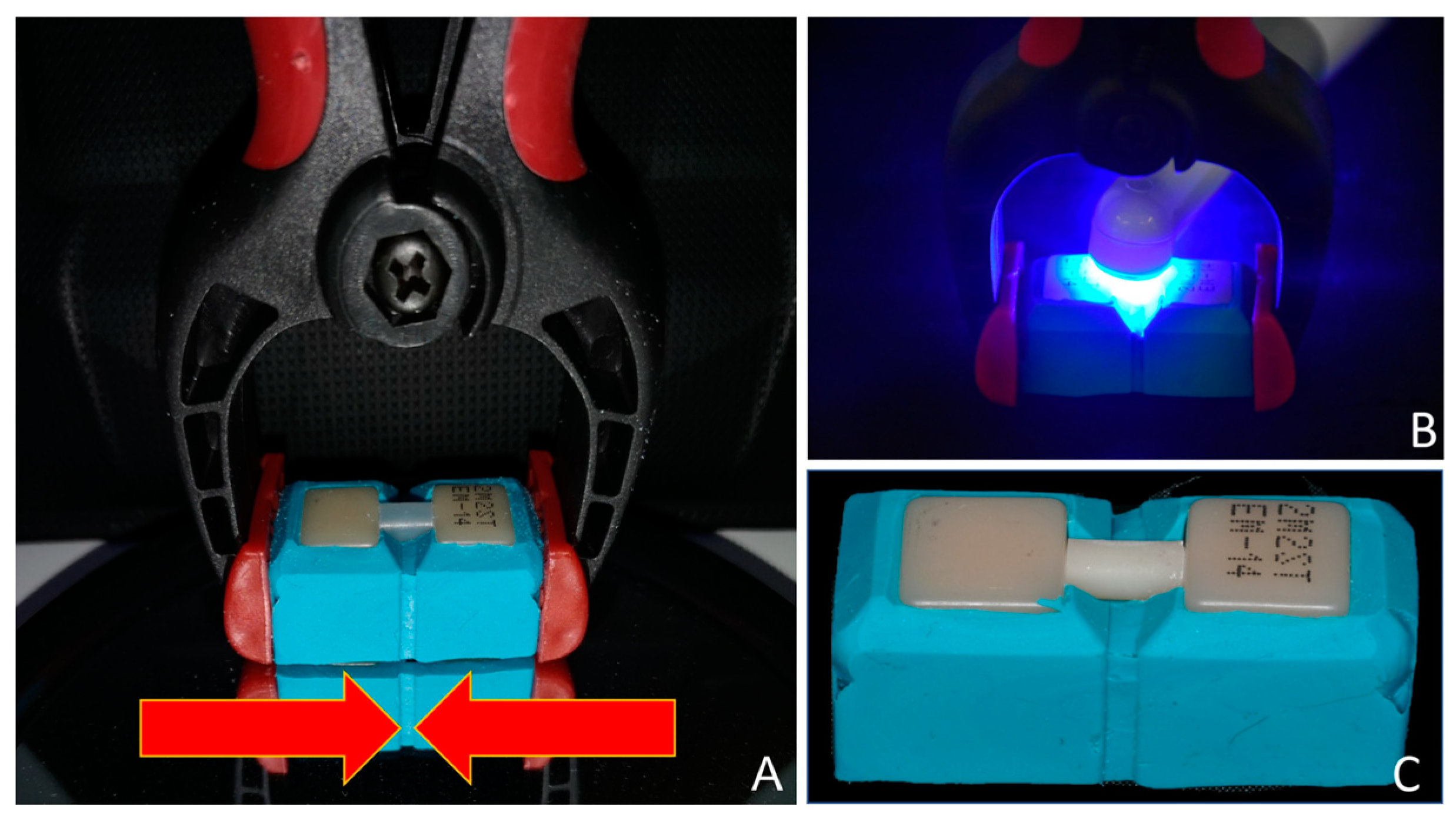
3.4. Mechanical Characterization of Adhesive Joints
3.5. In Vitro RBB Materials Adhesive Joint Mechanical Characterization
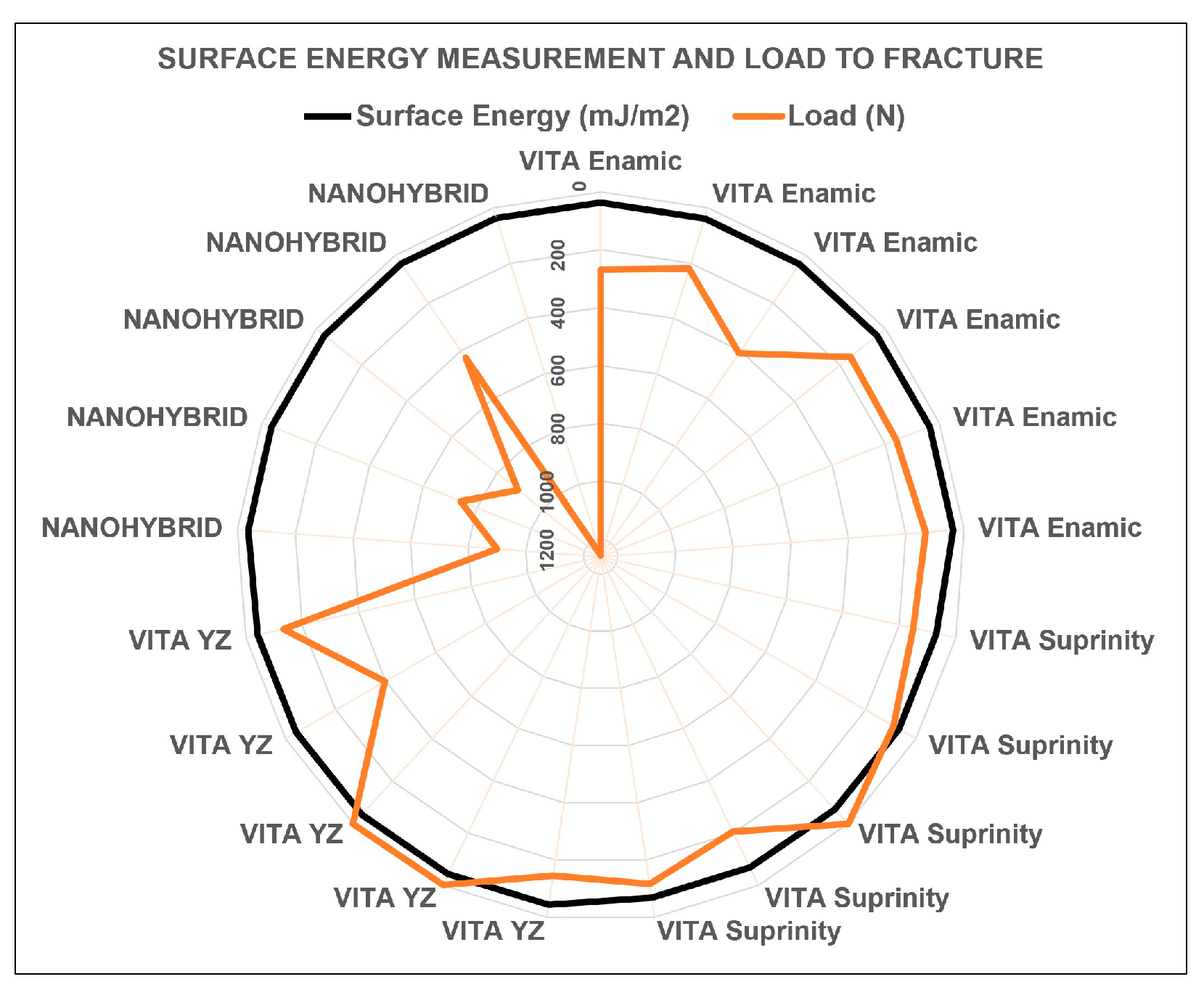
3.6. Surface Energy Measurements
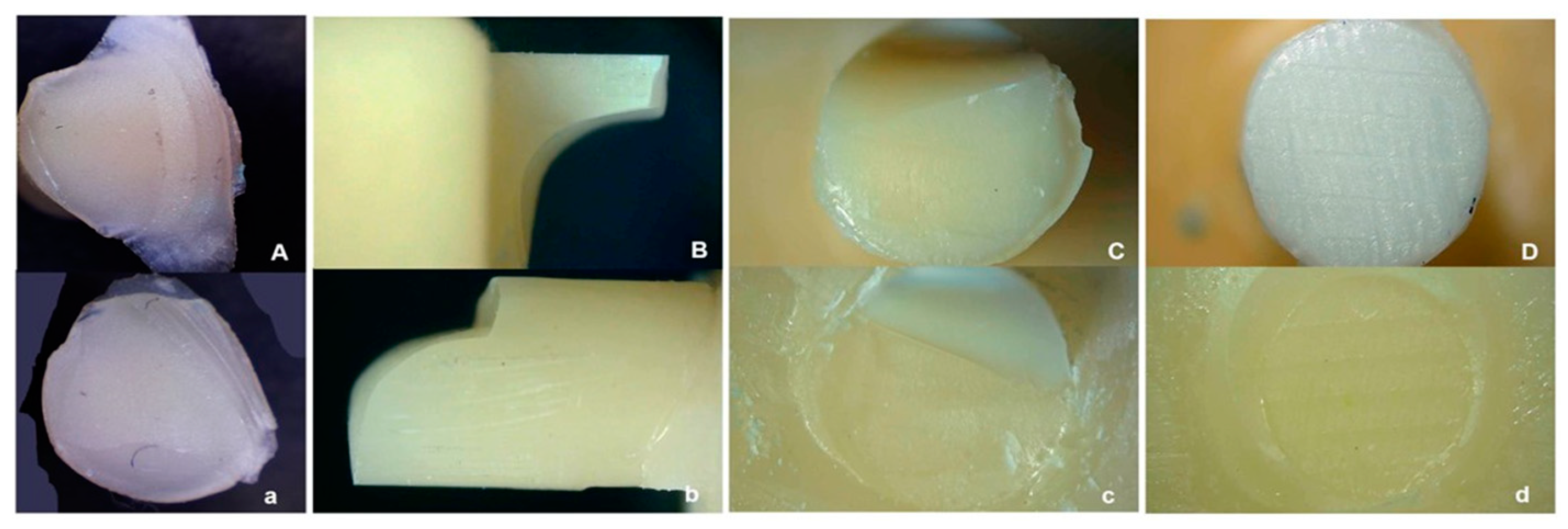
3.7. Adhesive Joint Fractography
3.8. Data Analysis
4. Results
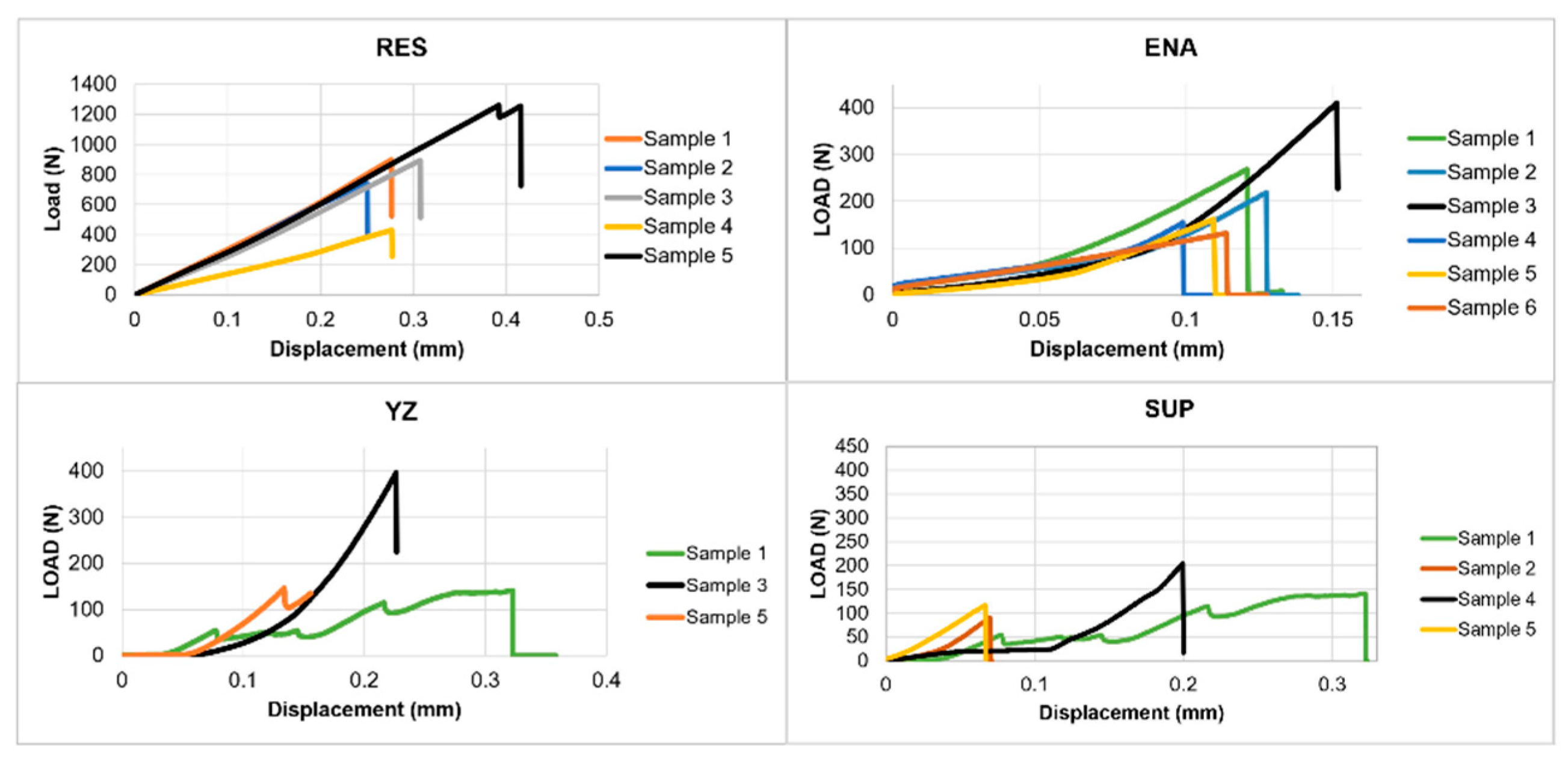
Mechanical Tests
5. Discussion
6. Recommendations for Future Research
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Calheiros-Lobo, M.J.; Carbas, R.; da Silva, L.F.M.; Pinho, T. Impact of in vitro findings on clinical protocols for the adhesion of CAD-CAM blocks: A systematic integrative review and meta-analysis. J. Prosthet. Dent. 2022, S0022-3913(22)00551-0. [Google Scholar] [CrossRef] [PubMed]
- Sulaiman, T.A. Materials in digital dentistry-A review. J. Esthet. Restor. Dent. 2020, 32, 171–181. [Google Scholar] [CrossRef]
- Raszewski, Z.; Brząkalski, D.; Derpeński, Ł.; Jałbrzykowski, M.; Przekop, R.E. Aspects and Principles of Material Connections in Restorative Dentistry-A Comprehensive Review. Materials 2022, 15, 7131. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.R. Clinically relevant approach to failure testing of all-ceramic restorations. J. Prosthet. Dent. 1999, 81, 652–661. [Google Scholar] [CrossRef]
- Rekow, E.D.; Silva, N.R.; Coelho, P.G.; Zhang, Y.; Guess, P.; Thompson, V.P. Performance of dental ceramics: Challenges for improvements. J. Dent. Res. 2011, 90, 937–952. [Google Scholar] [CrossRef] [Green Version]
- Baldi, A.; Carossa, M.; Comba, A.; Alovisi, M.; Femiano, F.; Pasqualini, D.; Berutti, E.; Scotti, N. Wear Behaviour of Polymer-Infiltrated Network Ceramics, Lithium Disilicate and Cubic Zirconia against Enamel in a Bruxism-Simulated Scenario. Biomedicines 2022, 10, 1682. [Google Scholar] [CrossRef] [PubMed]
- Guth, J.F.; Stawarczyk, B.; Edelhoff, D.; Liebermann, A. Zirconia and its novel compositions: What do clinicians need to know? Quintessence Int. 2019, 50, 512–520. [Google Scholar] [CrossRef]
- Fung, L.; Brisebois, P. Implementing Digital Dentistry into Your Esthetic Dental Practice. Dent. Clin. N. Am. 2020, 64, 645–657. [Google Scholar] [CrossRef]
- Watanabe, H.; Fellows, C.; An, H. Digital Technologies for Restorative Dentistry. Dent. Clin. N. Am. 2022, 66, 567–590. [Google Scholar] [CrossRef]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.S.; Jiang, H.B. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M. Factors affecting flexural strength of 3D-printed resins: A systematic review. J. Prosthodont. 2023, 32, 96–110. [Google Scholar] [CrossRef]
- Mazza, L.C.; Lemos, C.A.A.; Pesqueira, A.A.; Pellizzer, E.P. Survival and complications of monolithic ceramic for tooth-supported fixed dental prostheses: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, 128, 566–574. [Google Scholar] [CrossRef]
- Leitão, C.; Fernandes, G.V.O.; Azevedo, L.P.P.; Araújo, F.M.; Donato, H.; Correia, A.R.M. Clinical performance of monolithic CAD/CAM tooth-supported zirconia restorations: Systematic review and meta-analysis. J. Prosthodont. Res. 2022, 66, 374–384. [Google Scholar] [CrossRef] [PubMed]
- Leung, G.K.; Wong, A.W.; Chu, C.H.; Yu, O.Y. Update on Dental Luting Materials. Dent. J. 2022, 10, 208. [Google Scholar] [CrossRef] [PubMed]
- Manuja, N.; Nagpal, R.; Pandit, I. Dental adhesion: Mechanism, techniques and durability. J. Clin. Pediatr. Dent. 2012, 36, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Junior, L.; Baroudi, K.; Barroso, L.; Miranda, M.; Vitti, R.; Brandt, W. Bond strength of self-adhesive resin cement to dentin using different adhesion protocols. J. Clin. Exp. Dent. 2022, 14, e35–e39. [Google Scholar] [CrossRef] [PubMed]
- Van Meerbeek, B.; De Munck, J.; Yoshida, Y.; Inoue, S.; Vargas, M.; Vijay, P.; Van Landuyt, K.; Lambrechts, P.; Vanherle, G. Adhesion to enamel and dentin: Current status and future challenges. Oper. Dent. 2003, 28, 215–235. [Google Scholar]
- Tosun, B.; Yanıkoğlu, N. Evaluation of the effects of different surface modification methods on the bond strength of high-performance polymers and resin matrix ceramics. Clin. Oral Investig. 2022, 26, 3781–3790. [Google Scholar] [CrossRef]
- da Silva, M.A.; Vitti, R.P.; Sinhoreti, M.A.; Consani, R.L.; Silva-Junior, J.G.; Tonholo, J. Effect of alcoholic beverages on surface roughness and microhardness of dental composites. Dent. Mater. J. 2016, 35, 621–626. [Google Scholar] [CrossRef] [Green Version]
- Awad, M.M.; Alqahtani, H.; Al-Mudahi, A.; Murayshed, M.S.; Alrahlah, A.; Bhandi, S.H. Adhesive Bonding to Computer-aided Design/Computer-aided Manufacturing Esthetic Dental Materials: An Overview. J. Contemp. Dent. Pract. 2017, 18, 622–626. [Google Scholar] [CrossRef]
- Skorulska, A.; Piszko, P.; Rybak, Z.; Szymonowicz, M.; Dobrzyński, M. Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry—Application, Mechanical Characteristics and Comparison. Materials 2021, 14, 1592. [Google Scholar] [CrossRef] [PubMed]
- Palacios, T.; Tarancón, S.; Pastor, J.Y. On the Mechanical Properties of Hybrid Dental Materials for CAD/CAM Restorations. Polymers 2022, 14, 3252. [Google Scholar] [CrossRef] [PubMed]
- Eldafrawy, M.; Ebroin, M.G.; Gailly, P.A.; Nguyen, J.F.; Sadoun, M.J.; Mainjot, A.K. Bonding to CAD-CAM Composites: An Interfacial Fracture Toughness Approach. J. Dent. Res. 2018, 97, 60–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- da Silva, P.; Martinelli-Lobo, C.M.; Bottino, M.A.; Melo, R.M.; Valandro, L.F. Bond strength between a polymer-infiltrated ceramic network and a composite for repair: Effect of several ceramic surface treatments. Braz. Oral Res. 2018, 32, e28. [Google Scholar] [CrossRef] [Green Version]
- Vita-Zahnfabrik. Vita Suprinity® PC—Working Instructions; VITA Zahnfabrik: Bad Säckingen, Germany, 2019. [Google Scholar]
- Zarone, F.; Ruggiero, G.; Leone, R.; Breschi, L.; Leuci, S.; Sorrentino, R. Zirconia-reinforced lithium silicate (ZLS) mechanical and biological properties: A literature review. J. Dent. 2021, 109, 103661. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.J.; Lawson, N.C.; McLaren, E.E.; Nejat, A.H.; Burgess, J.O. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J. Prosthet. Dent. 2018, 120, 132–137. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Keul, C.; Eichberger, M.; Figge, D.; Edelhoff, D.; Lumkemann, N. Three generations of zirconia: From veneered to monolithic. Part I. Quintessence Int. 2017, 48, 369–380. [Google Scholar] [CrossRef]
- Fathy, S.M.; Al-Zordk, W.; Grawish, M.E.; Swain, M.V. Flexural strength and translucency characterization of aesthetic monolithic zirconia and relevance to clinical indications: A systematic review. Dent. Mater. 2021, 37, 711–730. [Google Scholar] [CrossRef]
- Pereira, G.K.R.; Guilardi, L.F.; Dapieve, K.S.; Kleverlaan, C.J.; Rippe, M.P.; Valandro, L.F. Mechanical reliability, fatigue strength and survival analysis of new polycrystalline translucent zirconia ceramics for monolithic restorations. J. Mech. Behav. Biomed. Mater. 2018, 85, 57–65. [Google Scholar] [CrossRef]
- Zhang, Y.; Lawn, B.R. Evaluating dental zirconia. Dent. Mater. 2019, 35, 15–23. [Google Scholar] [CrossRef]
- Bilir, H.; Yuzbasioglu, E.; Sayar, G.; Kilinc, D.D.; Bag, H.G.G.; Özcan, M. CAD/CAM single-retainer monolithic zirconia ceramic resin-bonded fixed partial dentures bonded with two different resin cements: Up to 40 months clinical results of a randomized-controlled pilot study. J. Esthet. Restor. Dent. 2022, 34, 1122–1131. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, K. Effect of 10-Methacryloyloxydecyl Dihydrogen Phosphate Concentrations in Primers on Bonding Resin Cements to Zirconia. J. Prosthodont. 2021, 30, 356–362. [Google Scholar] [CrossRef]
- Heboyan, A.; Vardanyan, A.; Karobari, M.I.; Marya, A.; Avagyan, T.; Tebyaniyan, H.; Mustafa, M.; Rokaya, D.; Avetisyan, A. Dental Luting Cements: An Updated Comprehensive Review. Molecules 2023, 28, 1619. [Google Scholar] [CrossRef]
- Marshall, S.J.; Bayne, S.C.; Baier, R.; Tomsia, A.P.; Marshall, G.W. A review of adhesion science. Dent. Mater. 2010, 26, e11–e16. [Google Scholar] [CrossRef]
- Calheiros-Lobo, M.J.; Vieira, T.; Carbas, R.; da Silva, L.F.M.; Pinho, T. Effectiveness of Self-Adhesive Resin Luting Cement in CAD-CAM Blocks—A Systematic Review and Meta-Analysis. Materials 2023, 16, 2996. [Google Scholar] [CrossRef]
- von Fraunhofer, J.A. Adhesion and cohesion. Int. J. Dent. 2012, 2012, 951324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lima, R.B.W.; Silva, A.F.; da Rosa, W.L.O.; Piva, E.; Duarte, R.M.; De Souza, G.M. Bonding Efficacy of Universal Resin Adhesives to Zirconia Substrates: Systematic Review and Meta-Analysis. J. Adhes. Dent. 2023, 25, 51–62. [Google Scholar] [CrossRef] [PubMed]
- Fathy, H.; Hamama, H.H.; El-Wassefy, N.; Mahmoud, S.H. Effect of different surface treatments on resin-matrix CAD/CAM ceramics bonding to dentin: In vitro study. BMC Oral. Health 2022, 22, 635. [Google Scholar] [CrossRef]
- Peumans, M.; Valjakova, E.B.; De Munck, J.; Mishevska, C.B.; Van Meerbeek, B. Bonding Effectiveness of Luting Composites to Different CAD/CAM Materials. J. Adhes. Dent. 2016, 18, 289–302. [Google Scholar] [CrossRef] [Green Version]
- Barutcigil, K.; Barutcigil, Ç.; Kul, E.; Özarslan, M.M.; Buyukkaplan, U.S. Effect of Different Surface Treatments on Bond Strength of Resin Cement to a CAD/CAM Restorative Material. J. Prosthodont. 2019, 28, 71–78. [Google Scholar] [CrossRef]
- Fidalgo-Pereira, R.; Carpio, D.; Torres, O.; Carvalho, O.; Silva, F.; Henriques, B.; Özcan, M.; Souza, J.C.M. The influence of inorganic fillers on the light transmission through resin-matrix composites during the light-curing procedure: An integrative review. Clin. Oral. Investig. 2022, 26, 5575–5594. [Google Scholar] [CrossRef]
- Diemer, F.; Stark, H.; Helfgen, E.H.; Enkling, N.; Probstmeier, R.; Winter, J.; Kraus, D. In vitro cytotoxicity of different dental resin-cements on human cell lines. J. Mater. Sci. Mater. Med. 2021, 32, 4. [Google Scholar] [CrossRef]
- Lopes-Rocha, L.; Ribeiro-Gonçalves, L.; Henriques, B.; Özcan, M.; Tiritan, M.E.; Souza, J.C.M. An integrative review on the toxicity of Bisphenol A (BPA) released from resin composites used in dentistry. J. Biomed. Mater. Res. B Appl. Biomater. 2021, 109, 1942–1952. [Google Scholar] [CrossRef]
- Barutcigil, K.; Dundar, A.; Batmaz, S.G.; Yildirim, K.; Barutcugil, C. Do resin-based composite CAD/CAM blocks release monomers? Clin. Oral. Investig. 2021, 25, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Hilgemberg, B.; Siqueira, F.S.F.; Cardenas, A.F.M.; Ribeiro, J.L.; Dávila-Sánchez, A.; Sauro, S.; Loguercio, A.D.; Arrais, C.A.G. Effect of Bonding Protocols on the Performance of Luting Agents Applied to CAD-CAM Composites. Materials 2022, 15, 4. [Google Scholar] [CrossRef] [PubMed]
- Anuntasainont, M.; Po-Ngam, N.; Lührs, A.K.; Neoh, S.P.; Pongprueksa, P. Fracture resistance of CAD/CAM blocks cemented on dentin using different cementation strategies. J. Prosthodont. Res. 2023, JPR_D_22_00196. [Google Scholar] [CrossRef] [PubMed]
- Stylianou, A.; Liu, P.R.; O’Neal, S.J.; Essig, M.E. Restoring Congenitally Missing Maxillary Lateral Incisors Using Zirconia-Based Resin Bonded Prostheses. J. Esthet. Restor. Dent. 2016, 28, 8–17. [Google Scholar] [CrossRef]
- Narwani, S.; Yadav, N.S.; Hazari, P.; Saxena, V.; Alzahrani, A.H.; Alamoudi, A.; Zidane, B.; Albar, N.H.M.; Robaian, A.; Kishnani, S.; et al. Comparison of Tensile Bond Strength of Fixed-Fixed Versus Cantilever Single- and Double-Abutted Resin-Bonded Bridges Dental Prosthesis. Materials 2022, 15, 5744. [Google Scholar] [CrossRef]
- Fouquet, V.; Lachard, F.; Abdel-Gawad, S.; Dursun, E.; Attal, J.P.; François, P. Shear Bond Strength of a Direct Resin Composite to CAD-CAM Composite Blocks: Relative Contribution of Micromechanical and Chemical Block Surface Treatment. Materials 2022, 15, 5018. [Google Scholar] [CrossRef]
- Farah, S.; Anderson, D.G.; Langer, R. Physical and mechanical properties of PLA, and their functions in widespread applications—A comprehensive review. Adv. Drug Deliv. Rev. 2016, 107, 367–392. [Google Scholar] [CrossRef] [Green Version]
- Quigley, N.P.; Loo, D.S.S.; Choy, C.; Ha, W.N. Clinical efficacy of methods for bonding to zirconia: A systematic review. J. Prosthet. Dent. 2020, 125, 231–240. [Google Scholar] [CrossRef]
- Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Marginal and internal fit of CAD-CAM inlay/onlay restorations: A systematic review of in vitro studies. J. Prosthet. Dent. 2019, 121, 590–597.e593. [Google Scholar] [CrossRef] [PubMed]
- Papadiochou, S.; Pissiotis, A.L. Marginal adaptation and CAD-CAM technology: A systematic review of restorative material and fabrication techniques. J. Prosthet. Dent. 2018, 119, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Vita-Zahnfabrik. VITA ENAMIC®—Technical and Scientific Documentation; VITA Zahnfabrik: Bad Säckingen, Germany, 2019. [Google Scholar]
- Vita-Zahnfabrik. Vita YZ®—Solutions; VITA Zahnfabrik: Bad Säckingen, Germany, 2019. [Google Scholar]
- Yano, H.T.; Ikeda, H.; Nagamatsu, Y.; Masaki, C.; Hosokawa, R.; Shimizu, H. Correlation between microstructure of CAD/CAM composites and the silanization effect on adhesive bonding. J. Mech. Behav. Biomed. Mater. 2020, 101, 103441. [Google Scholar] [CrossRef] [PubMed]
- Calheiros-Lobo, M.J.; Carbas, R.; da Silva, L.F.M.; Pinho, T. Effect of the Modulation of the Adhesive Interface between a CAD-CAM Hybrid Ceramic adherend and Three Luting Cements on Shear Bond Strength: In Vitro Study. J. Adhes. Dent. 2023, 16, 2996. [Google Scholar]
- Al-Wahadni, A.; Dkmak, M.S.F.; Almohammed, S.; Hatamleh, M.M.; Tabanjah, A.A. Fracture strength of anterior cantilever resin bonded fixed partial dentures fabricated from high translucency zirconia with different intaglio surface treatments. J. Prosthodont. 2023; Epub ahead of print. [Google Scholar] [CrossRef]
- Mutlu-Sağesen, H.L.E.; Sağesen, E.A.; Özcan, M. Bibliometric analysis of zirconia publications between 1980 and 2021: Global productivity and publication trends. J. Prosthodont. Res. 2023; Online ahead of print. [Google Scholar] [CrossRef]








| Material | Name | Code | Composition | Manufacturer |
|---|---|---|---|---|
| CAD-CAM Ceramics | VITA Enamic | ENA | 86% feldspar ceramic: SiO2 58%–63%, Al2O3 20%–23%, Na2O9–11%, K2O4–6% by weight, 14% polymer by weight: TEGDMA, UDMA | VITA Zahnfabrik, Bad Säckingen, Germany |
| VITA Suprinity | SUP | Zirconium oxide 8–12, silicon dioxide 56%–64%, lithium oxide 15%–21%, various > 10% by weight | VITA Zahnfabrik, Bad Säckingen, Germany | |
| VITA 3Y-TPZ | Y-ZT | Zirconia reinforced with 3% Yitria | VITA Zahnfabrik, Bad Säckingen, Germany | |
| Resin-matrix restorative composite | PROCLINIC EXPERT Nano Hybrid composite | RES | 22.5% weight, multifunctional methacrylic ester; 77.5% weight, inorganic filler (40 nm–1.5 microns). | SDI Limited, Burnston, AUS |
| Resin-matrix composite cement | RelyX Ultimate | RU | MDP phosphate monomer, dimethacrylate resins, HEMA, Vitrebond™ copolymer filler, ethanol, water, initiators, silane | 3M Oral Care, St. Paul, MN, USA |
| Etching agent | VITA ADIVA Cera Etch | HF5 | Hydrofluoric acid 5% | VITA Zahnfabrik, Bad Säck ingen, Germany |
| Ceramic primer | Monobond Plus | MB | 50%–100% ethanol, disulfit methacrylate, ≤2.5% phosphoric acid di methacrylate, ≤2.5% 3-trimethoxysilylpropyl methacrylate | Ivoclar Vivadent AG, Schaan, Liechtenstein |
| VITA ADIVA C Primer | CP | Solution of methacrylsilanes in ethanol | VITA Zahnfabrik, Bad Säck ingen, Germany | |
| Adhesive system | Scotchbond Universal adhesive | SB-U | MDP, Bis-GMA, phosphate monomer, dimethacrylate resins, HEMA, methacrylate-modified polyalkenoic acid copolymer, filler, ethanol, water, initiators, silane-treated silica | 3M Oral Care, St. Paul, MN, USA |
| Groups | Failure Load | Shear Stress | ||||
|---|---|---|---|---|---|---|
| n | Mean (N) | SD (N) | Mean (MPa) | SD (MPa) | ||
| Resin-matrix Composite | 5 | 843.07 | 299.82 | 69.10 | 24.58 | |
| Rely X Ultimate | VITA Enamic | 6 | 224.27 | 103.82 | 18.38 | 8.51 |
| VITA Suprinity | 5 | 139.56 | 48.99 | 11.44 | 4.02 | |
| VITA Y-ZT | 5 | 225.40 | 147.88 | 18.48 | 12.12 | |
| GROUP | Type of Failure | |||||||
|---|---|---|---|---|---|---|---|---|
| Interface 1 | Interface 2 | Base 1 | Base 2 | Cylinder | MIX | |||
| AD | C | AD | C | C | C | C | ||
| VITA Enamic | x | x | x | |||||
| VITA Enamic | x | |||||||
| VITA Enamic | x | |||||||
| VITA Enamic | x | |||||||
| VITA Enamic | x | x | x | |||||
| VITA Enamic | x | |||||||
| Interface 1 | Interface 2 | Base 1 | Base 2 | Cylinder | ||||
| AD | C | AD | C | C | C | C | ||
| VITA Suprinity | x | x | x | |||||
| VITA Suprinity | x | x | x | |||||
| VITA Suprinity | x | x | ||||||
| VITA Suprinity | x | x | x | |||||
| VITA Suprinity | x | |||||||
| Interface 1 | Interface 2 | Base 1 | Base 2 | Cylinder | ||||
| AD | C | AD | C | C | C | C | ||
| VITA Y-ZT | x | |||||||
| VITA Y-ZT | x | |||||||
| VITA Y-ZT | x | |||||||
| VITA Y-ZT | x | |||||||
| VITA Y-ZT | x | |||||||
| Interface 1 | Interface 2 | Base 1 | Base 2 | Cylinder | ||||
| AD | C | AD | C | C | C | C | ||
| Nanohybrid Resin | x | x | x | |||||
| Nanohybrid Resin | x | |||||||
| Nanohybrid Resin | x | x | x | |||||
| Nanohybrid Resin | x | |||||||
| Nanohybrid Resin | x | |||||||
| Only Grinding | |||
|---|---|---|---|
| ENAMIC | SUPRINITY | Y-ZT | |
| Contact angle (°) | 0.0 | 0.0 | 0.0 |
| 45.9–41.0 | 21.5–21.6 | 37.5–38.2 | |
| 773–72.7 | 44.0–39.0 | 58.0–57.2 | |
| Surface Energy (mJ/m2) | 37.2 | 54.5 | 44.1 |
| HF 5% conditioning—60 s | |||
| ENAMIC | SUPRINITY | Y-ZT | |
| Contact angle (°) | 0.0 | 0.0 | 0.0 |
| 23.6–22.8 | 0.0 | 50.1–48.6 | |
| 86.6–85.3 | 0.0 | 57.4–54.6 | |
| Surface Energy (mJ/m2) | 37.2 | 68.6 | 43.2 |
| Sandblasting AL2O3 50 µm | |||
| ENAMIC | SUPRINITY | Y-ZT | |
| Contact angle (°) | 0.0 | 0.0 | 0.0 |
| 15.0–9.0 | 0.0 | 44.0–42.5 | |
| 60.7–55 | 0.0 | 60.0–59.0 | |
| Surface Energy (mJ/m2) | 46.9 | 68.6 | 42.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calheiros-Lobo, M.J.; Calheiros-Lobo, J.M.; Carbas, R.; da Silva, L.F.M.; Pinho, T. A Polymer-Infiltrated Ceramic as Base Adherent in an Experimental Specimen Model to Test the Shear Bond Strength of CAD-CAM Monolithic Ceramics Used in Resin-Bonded Dental Bridges. Coatings 2023, 13, 1218. https://doi.org/10.3390/coatings13071218
Calheiros-Lobo MJ, Calheiros-Lobo JM, Carbas R, da Silva LFM, Pinho T. A Polymer-Infiltrated Ceramic as Base Adherent in an Experimental Specimen Model to Test the Shear Bond Strength of CAD-CAM Monolithic Ceramics Used in Resin-Bonded Dental Bridges. Coatings. 2023; 13(7):1218. https://doi.org/10.3390/coatings13071218
Chicago/Turabian StyleCalheiros-Lobo, Maria João, João Mário Calheiros-Lobo, Ricardo Carbas, Lucas F. M. da Silva, and Teresa Pinho. 2023. "A Polymer-Infiltrated Ceramic as Base Adherent in an Experimental Specimen Model to Test the Shear Bond Strength of CAD-CAM Monolithic Ceramics Used in Resin-Bonded Dental Bridges" Coatings 13, no. 7: 1218. https://doi.org/10.3390/coatings13071218







