Co-Existence of Free-Living Amoebae and Potential Human Pathogenic Bacteria Isolated from Rural Household Water Storage Containers
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area
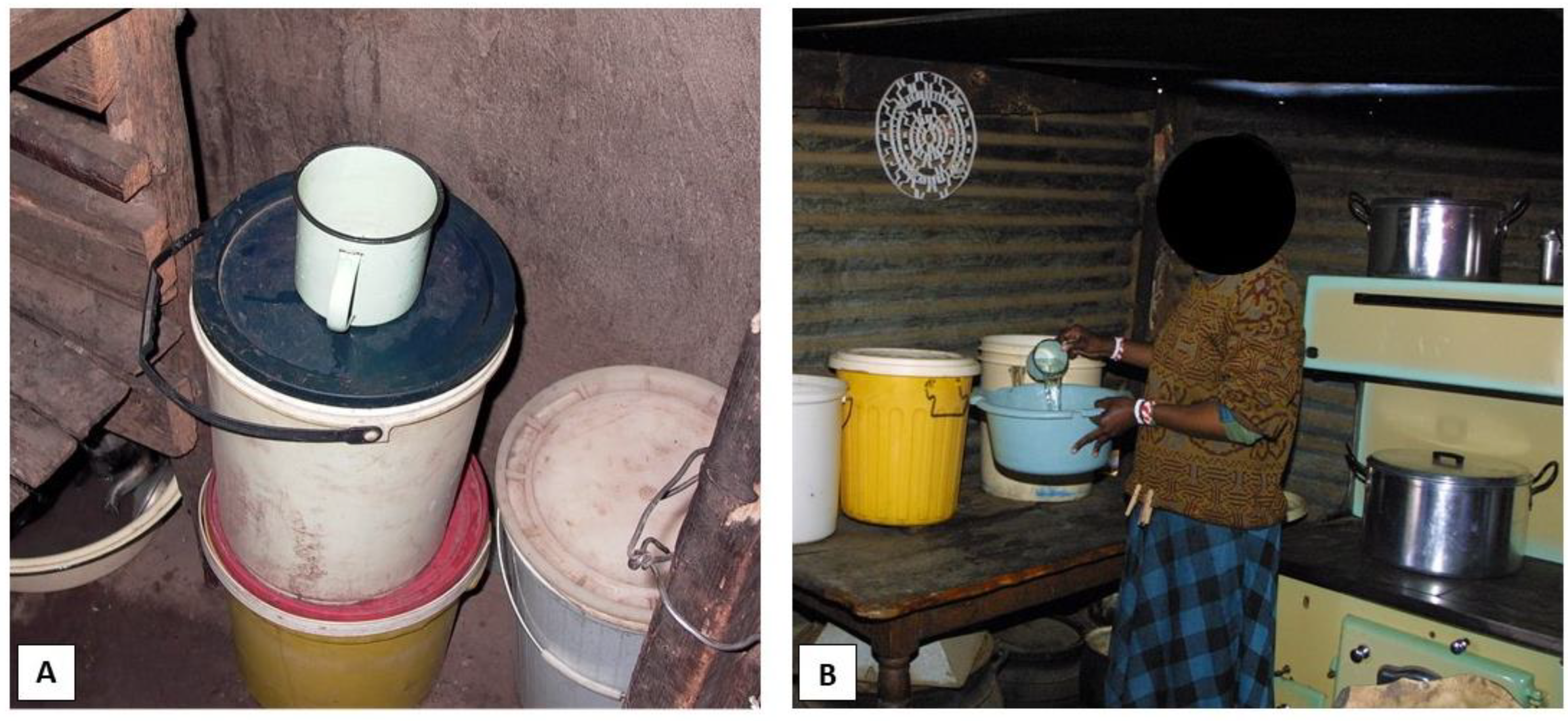
2.2. Sample Collection
2.3. Isolation and Identification of Potential Human Pathogenic Bacteria
2.4. Isolation of FLA from the Water Samples
2.5. Isolation of FLA from the Biofilm Samples
2.6. FLA Identification
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stats SA. General Household Survey. (Report No. P0318). Pretoria, South Africa; 2019. Available online: https://www.statssa.gov.za/publications/P0318/P03182019.pdf (accessed on 8 October 2021).
- Slavik, I.; Oliveira, K.R.; Cheung, P.B.; Uhl, W. Water quality aspects related to domestic drinking water storage tanks and consideration in current standards and guidelines throughout the world—A review. J. Water Health 2020, 18, 439–463. [Google Scholar] [CrossRef]
- Jagals, P.; Grabow, W.O.K.; Williams, E. The effect of supplied water quality on human health in an urban development with limited basic -subsistence facilities. Water SA 1997, 23, 373–378. [Google Scholar]
- Momba, M.N.B.; Notshe, T.L. The effect of long storage and household containers on the microbiological quality of drinking water in rural communities of South Africa. J. Water Supply Res. Technol. 2003, 52, 67–76. [Google Scholar] [CrossRef]
- Potgieter, N.; Mudau, L.S.; Maluleke, F.R.S. The microbiological quality of ground water sources used by rural communities in the Limpopo Province, South Africa. Water Sci. Technol. 2006, 54, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Esterhuizen, L.; Fossey, A.; Potgieter, E. Groundwater quality on dairy farms in central South Africa. Water SA 2015, 41, 194–198. [Google Scholar] [CrossRef]
- Costerton, J.W.; Lewandowski, Z.; Caldwell, D.E.; Korber, D.R.; Lappin-Scott, H.M. Microbial Biofilms. Annu. Rev. Microbiol. 1995, 49, 711–742. [Google Scholar] [CrossRef] [PubMed]
- Berlanga Herranz, M.; Guerrero, R. Living together in biofilms: The microbial cell factory and its biotechnological implications. Microbial Cell Factories 2016, 15, 165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Budeli, P.; Moropeng, R.C.; Mpenyana-Monyatsi, L.; Momba, M.N.B. Inhibition of biofilm formation on the surface of water storage containers using biosand zeolite silver-impregnated clay granular and silver impregnated porous pot filtration systems. PLoS ONE 2018, 13, e0194715. [Google Scholar] [CrossRef] [Green Version]
- Barbeau, J.; Buhler, T. Biofilms augment the number of free-living amoebae in dental unit waterlines. Res. Microbiol. 2001, 152, 753–760. [Google Scholar] [CrossRef]
- Costerton, J.W.; Stewart, P.S.; Greenberg, E.P. Bacterial biofilms: A common cause of persistent infections. Science 1999, 284, 1318–1322. [Google Scholar] [CrossRef] [Green Version]
- Arndt, H.; Schmidt-Denter, K.; Auer, B.; Weitere, M. Protozoans and Biofilms. In Fossil and Recent Biofilms; Krumbein, W.E., Paterson, D.M., Zavarzin, G.A., Eds.; Kluwer Academic Publishing: Dordrecht, The Netherlands, 2003; pp. 173–189. [Google Scholar]
- Jackson, S.M.; Jones, E.B.G. Interactions within biofilms: The disruption of biofilm structure by protozoa. Kieler Meeresforsch. Sonderh. 1991, 8, 264–268. [Google Scholar]
- Murcott, S. Implementation, Critical Factors and Challenges to Scale-Up of Household Drinking Water Treatment and Safe Storage Systems. In Background Paper on Household Water Treatment and Safe Storage (HWTS) for the Electronic Conference. USAID/Hygiene Improvement Project (HIP). 2006. Available online: http://hip.fhi360.org/file/6114/20060501-HWTS-Murcott.pdf (accessed on 8 October 2021).
- Levy, K.; Nelson, K.L.; Hubbard, A.; Eisenberg, J.N. Following the water: A controlled study of drinking water storage in northern coastal Ecuador. Environ. Health Perspect. 2008, 116, 1533–1540. [Google Scholar] [CrossRef] [PubMed]
- Jagals, P.; Jagals, C.; Bokako, T. The effect of container-biofilm on the microbiological quality of water used from plastic household containers. J. Water Health 2003, 1, 101–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van der Merwe, V.; Duvenage, S.; Korsten, L. Comparison of biofilm formation and water quality when water from different sources was stored in large commercial water storage tanks. J. Water Health 2013, 11, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Lantagne, D.; Clasen, T. Point-of-use water treatment in emergency response. Waterlines 2012, 31, 30–52. [Google Scholar] [CrossRef] [Green Version]
- Oloruntoba, E.O.; Babalola, T.F.; Morakinyo, O.M.; Mumuni, A. Effects of improved storage containers on the bacteriological quality of household drinking water in low-income urban communities in Ibadan, Nigeria. Water Supply 2016, 16, 378–387. [Google Scholar] [CrossRef]
- McGuinness, S.L.; O’Toole, J.; Barker, S.F.; Forbes, A.B.; Boving, T.B.; Giriyan, A.; Patil, K.; D’Souza, F.; Vhaval, R.; Cheng, A.C.; et al. Household Water Storage Management, Hygiene Practices, and Associated Drinking Water Quality in Rural India. Environ. Sci. Technol. 2020, 54, 4963–4973. [Google Scholar] [CrossRef]
- Soliman, M.Y.; van Halem, D.; Medema, G. Virus removal by ceramic pot filter disks: Effect of biofilm growth and surface cleaning. Int. J. Hyg. Environ. Health 2019, 224, 113438. [Google Scholar] [CrossRef]
- Momba, M.N.; Kaleni, P. Regrowth and survival of indicator microorganisms on the surfaces of household containers used for the storage of drinking water in rural communities of South Africa. Water Res. 2002, 36, 3023–3028. [Google Scholar] [CrossRef]
- Momba, M.N.B.; Mnqumevu, B.V. Detection of Faecal Coliforms and Heterotrophic Plate Count Bacteria Attached to Household Containers during the Storage of Drinking Groundwater in Rural Communities. In Proceedings of the WISA 2000 Biennial Conference, Sun City, South Africa, 28 May–1 June 2000; pp. 21–28. Available online: https://wisa.org.za (accessed on 20 October 2021).
- Wright, J.; Gundry, S.; Conroy, R.M. Household drinking water in developing countries: A systematic review of microbiological contamination between source and point-of-use. Trop. Med. Int. Health 2004, 9, 106–117. [Google Scholar] [CrossRef] [Green Version]
- Taravaud, A.; Ali, M.; Lafosse, B.; Nicolas, V.; Féliers, C.; Thibert, S.; Lévi, Y.; Loiseau, P.; Pomel, S. Enrichment of free-living amoebae in biofilms developed at upper water levels in drinking water storage towers: An inter- and intra-seasonal study. Sci. Total. Environ. 2018, 633, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Stockman, L.J.; Wright, C.J.; Visvesvara, G.S.; Fields, B.S.; Beach, M.J. Prevalence of Acanthamoeba spp. and other free-living amoebae in household water, Ohio, USA—1990–1992. Parasitol. Res. 2010, 108, 621–627. [Google Scholar] [CrossRef]
- Rohr, U.; Weber, S.; Michel, R.; Selenka, F.; Wilhelm, M. Comparison of Free-Living Amoebae in Hot Water Systems of Hospitals with Isolates from Moist Sanitary Areas by Identifying Genera and Determining Temperature Tolerance. Appl. Environ. Microbiol. 1998, 64, 1822–1824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muchesa, P.; Barnard, T.G.; Bartie, C. The prevalence of free-living amoebae in a South African hospital water distribution system. S. Afr. J. Sci. 2015, 111, 1–3. [Google Scholar] [CrossRef]
- Muchesa, P.; Leifels, M.; Jurzik, L.; Hoorzook, K.B.; Barnard, T.G.; Bartie, C. Coexistence of free-living amoebae and bacteria in selected South African hospital water distribution systems. Parasitol. Res. 2016, 116, 155–165. [Google Scholar] [CrossRef] [PubMed]
- Kuiper, M.W.; Wullings, B.A.; Akkermans, A.D.L.; Beumer, R.R.; Van der Kooij, D. Intracellular Proliferation of Legionella pneumophila in Hartmanella vermiformis in Aquatic Biofilms Grown on Plasticized Polyvinyl Chloride. Appl. Environ. Microbiol. 2004, 70, 6826–6833. [Google Scholar] [CrossRef] [Green Version]
- van der Kooij, D.; Veenendaal, H.R.; Scheffer, W.J. Biofilm formation and multiplication of Legionella in a model warm water system with pipes of copper, stainless steel and cross-linked polyethylene. Water Res. 2005, 39, 2789–2798. [Google Scholar] [CrossRef]
- Lau, H.Y.; Ashbolt, N.J. The role of biofilms and protozoa in Legionella pathogenesis: Implications for drinking water. J. Appl. Microbiol. 2009, 107, 368–378. [Google Scholar] [CrossRef]
- Muchesa, P.; Lelfels, M.; Jurzik, L.; Barnard, T.G.; Bartle, C. Detection of amoeba-associated Legionella pneumophila in hospital water networks of Johannesburg. South. Afr. J. Infect. Dis. 2018, 33, 72–75. [Google Scholar] [CrossRef]
- Shaheen, M.; Scott, C.; Ashbolt, N.J. Long-term persistence of infectious Legionella with free-living amoebae in drinking water biofilms. Int. J. Hyg. Environ. Health 2019, 222, 678–686. [Google Scholar] [CrossRef]
- Greub, G.; Raoult, D. Microorganisms Resistant to Free-Living Amoebae. Clin. Microbiol. Rev. 2004, 17, 413–433. [Google Scholar] [CrossRef] [Green Version]
- International Union against Tuberculosis and Lung Disease. Technical guide for sputum examination for tuberculosis by direct microscopy. Bull. Int. Union Tuberc. Lung Dis. 1978, 2, 4–16. [Google Scholar]
- Frank, J.A.; Reich, C.I.; Sharma, S.; Weisbaum, J.S.; Wilson, B.A.; Olsen, G.J. Critical evaluation of two primers commonly used for amplification of bacterial 16S rRNA genes. Appl. Environ. Microbiol. 2008, 74, 2461–2470. [Google Scholar] [CrossRef] [Green Version]
- Fredriksson, N.J.; Hermansson, M.; Wilén, B.-M. The Choice of PCR Primers Has Great Impact on Assessments of Bacterial Community Diversity and Dynamics in a Wastewater Treatment Plant. PLoS ONE 2013, 8, e76431. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.S.; Ball, N.W.; Beck, L.A.; de Lisle, G.W.; Skuce, R.A.; Neill, S.D. Determination of the etiology of presumptive feline leprosy by 16S rRNA gene analysis. J. Clin. Microbiol. 1997, 35, 2464–2467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miyamoto, H.; Yamamoto, H.; Arima, K.; Fujii, J.; Maruta, K.; Izu, K.; Shiomori, T.; Yoshida, S. Development of a new semi-nested PCR method for detection of Legionella species and its application to surveillance of legionellae in hospital cooling tower water. Appl. Environ. Microbiol. 1997, 63, 2489–2494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altschul, S.F.; Madden, T.L.; Schäffer, A.A.; Zhang, J.; Zhang, Z.; Miller, W.; Lipman, D.J. Gapped BLAST and PSI-BLAST: A new generation of protein database search programs. Nucleic Acids Res. 1997, 25, 3389–3402. [Google Scholar] [CrossRef] [Green Version]
- Thomas, V.; Herrera-Rimann, K.; Blanc, D.S.; Greub, G. Biodiversity of amoebae and amoebae-resisting bacteria in a hospital water network. Appl. Environ. Microbiol. 2006, 72, 2428–2438. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schroeder, J.M.; Booton, G.C.; Hay, J.; Niszl, I.A.; Seal, D.V.; Markus, M.B.; Fuerst, P.A.; Byers, T.J. Use of Subgenic 18S Ribosomal DNA PCR and Sequencing for Genus and Genotype Identification of Acanthamoebae from Humans with Keratitis and from Sewage Sludge. J. Clin. Microbiol. 2001, 39, 1903–1911. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schilde, C.; Schaap, P. The Amoebozoa. Methods Mol. Biol. 2013, 983. [Google Scholar] [CrossRef] [Green Version]
- Denoncourt, A.M.; Paquet, V.E.; Charette, S.J. Potential role of bacteria packaging by protozoa in the persistence and transmission of pathogenic bacteria. Front. Microbiol. 2014, 5, 240. [Google Scholar] [CrossRef] [Green Version]
- WHO. Combating Waterborne Disease at the Household Level: The International Network to Promote Household Water Treatment and Safe Storage; World Health Organization: Geneva, Switzerland, 2007; Available online: http://www.who.int/household_water/advocacy/combating_disease.pdf (accessed on 8 October 2021).
- Mintz, E.D.; Reiff, F.M.; Tauxe, R.V. Safe water treatment and storage in the home. A practical new strategy to prevent waterborne disease. JAMA 1995, 273, 948–953. [Google Scholar] [CrossRef] [PubMed]
- Trevett, A.F.; Carter, R.C.; Tyrrel, S. Water quality deterioration: A study of household drinking water quality in rural Honduras. Int. J. Environ. Health Res. 2004, 14, 273–283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oswald, W.E.; Bern, C.; Cabrera, L.; Lescano, A.; Gilman, R.H.; Calderon, M.M. Fecal Contamination of Drinking Water within Peri-Urban Households, Lima, Peru. Am. J. Trop. Med. Hyg. 2007, 77, 699–704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adane, M.; Mengistie, B.; Medhin, G.; Kloos, H.; Mulat, W. Piped water supply interruptions and acute diarrhea among under-five children in Addis Ababa slums, Ethiopia: A matched case-control study. PLoS ONE 2017, 12, e0181516. [Google Scholar] [CrossRef] [Green Version]
- Odiyo, J.O.; Mathoni, M.M.; Makungo, R. Health Risks and Potential Sources of Contamination of Groundwater Used by Public Schools in Vhuronga 1, Limpopo Province, South Africa. Int. J. Environ. Res. Public Health 2020, 17, 6912. [Google Scholar] [CrossRef]
- Schafer, C.A.; Mihelcic, J.R. Effect of storage tank material and maintenance on domestic water quality. J. Am. Water Works Assoc. 2012, 104, E521–E529. [Google Scholar] [CrossRef]
- Akuffo, I.; Cobbina, S.J.; Alhassan, E.H.; Nkoom, M. Assessment of the quality of water before and after storage in the Nyankpala Community of the Tolon-Kumbungu District, Ghana. Int. J. Scient. Technol. Res. 2013, 2, 221–227. [Google Scholar]
- Pagnier, I.; Valles, C.; Raoult, D.; La Scola, B. Isolation of Vermamoeba vermiformis and associated bacteria in hospital water. Microb. Pathog. 2015, 80, 14–20. [Google Scholar] [CrossRef]
- Javanmard, E.; Niyyati, M.; Lorenzo-Morales, J.; Lasjerdi, Z.; Behniafar, H.; Mirjalali, H. Molecular identification of waterborne free living amoebae (Acanthamoeba, Naegleria and Vermamoeba) isolated from municipal drinking water and environmental sources, Semnan province, north half of Iran. Exp. Parasitol. 2017, 183, 240–244. [Google Scholar] [CrossRef]
- Mulec, J.; Dietersdorfer, E.; Üstüntürk-Onan, M.; Walochnik, J. Acanthamoeba and other free-living amoebae in bat guano, an extreme habitat. Parasitol. Res. 2015, 115, 1375–1383. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo-Morales, J.; Martínez-Carretero, E.; Batista, N.; Álvarez-Marín, J.; Bahaya, Y.; Walochnik, J.; Valladares, B. Early diagnosis of amoebic keratitis due to a mixed infection with Acanthamoeba and Hartmannella. Parasitol. Res. 2007, 102, 167–169. [Google Scholar] [CrossRef]
- Cabello-Vílchez, A.M.; Mena, R.; Zuñiga, J.; Cermeño, P.; Martín-Navarro, C.M.; González, A.C.; Arencibia, A.L.; Reyes-Batlle, M.; Piñero, J.; Valladares, B.; et al. Endosymbiotic Mycobacterium chelonae in a Vermamoeba vermiformis strain isolated from the nasal mucosa of an HIV patient in Lima, Peru. Exp. Parasitol. 2014, 145, S127–S130. [Google Scholar] [CrossRef] [PubMed]
- Walochnik, J.; Scheikl, U.; Haller-Schober, E. Twenty Years of Acanthamoeba Diagnostics in Austria. J. Eukaryot. Microbiol. 2014, 62, 3–11. [Google Scholar] [CrossRef] [Green Version]
- Wadowsky, R.M.; Butler, L.J.; Cook, M.K.; Verma, S.M.; A Paul, M.; Fields, B.S.; Keleti, G.; Sykora, J.L.; Yee, R.B. Growth-supporting activity for Legionella pneumophila in tap water cultures and implication of hartmannellid amoebae as growth factors. Appl. Environ. Microbiol. 1988, 54, 2677–2682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delafont, V.; Rodier, M.-H.; Maisonneuve, E.; Cateau, E. Vermamoeba vermiformis: A Free-Living Amoeba of Interest. Microb. Ecol. 2018, 76, 991–1001. [Google Scholar] [CrossRef] [PubMed]
- Cateau, E.; Delafont, V.; Hechard, Y.; Rodier, M.H. Free-living amoebae: What part do they play in healthcare-associated infections? J. Hospital Infec. 2014, 87, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.A. Acanthamoeba: Biology and increasing importance in human health. FEMS Microbiol. Rev. 2006, 30, 564–595. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maciver, S.K.; Asif, M.; Simmen, M.W.; Lorenzo-Morales, J. A systematic analysis of Acanthamoeba genotype frequency correlated with source and pathogenicity: T4 is confirmed as a pathogen-rich genotype. Eur. J. Protistol. 2013, 49, 217–221. [Google Scholar] [CrossRef]
- Arnalich-Montiel, F.; Lumbreras-Fernández, B.; Martín-Navarro, C.M.; Valladares, B.; Lopez-Velez, R.; Morcillo-Laiz, R.; Lorenzo-Morales, J. Influence of Acanthamoeba Genotype on Clinical Course and Outcomes for Patients with Acanthamoeba Keratitis in Spain. J. Clin. Microbiol. 2014, 52, 1213–1216. [Google Scholar] [CrossRef] [Green Version]
- Siddiqui, R.; Khan, N.A. War of the microbial worlds: Who is the beneficiary in Acanthamoeba–bacterial interactions? Exp. Parasitol. 2012, 130, 311–313. [Google Scholar] [CrossRef] [PubMed]
- Neff, R.J. Purification, Axenic Cultivation, and Description of a Soil Amoeba, Acanthamoeba sp. J. Protozool. 1957, 4, 176–182. [Google Scholar] [CrossRef]
- Page, F.C. Platyamoeba stenopodia n. g., n. sp., a freshwater amoeba. J. Protozool. 1969, 16, 437–441. [Google Scholar] [CrossRef] [PubMed]
- Geisen, S.; Weinert, J.; Kudryavtsev, A.; Glotova, A.; Bonkowski, M.; Smirnov, A. Two new species of the genus Stenamoeba (Discosea, Longamoebia): Cytoplasmic MTOC is present in one more amoebae lineage. Eur. J. Protistol. 2014, 50, 153–165. [Google Scholar] [CrossRef] [PubMed]
- Van Wichelen, J.; D’Hondt, S.; Claeys, M.; Vyverman, W.; Berney, C.; Bass, D.; Vanormelingen, P. A Hotspot of Amoebae Diversity: 8 New Naked Amoebae Associated with the Planktonic Bloom-forming Cyanobacterium Microcystis. Acta Protozool. 2015, 55, 61–87. [Google Scholar]
- O'Kelly, C.J.; Peglar, M.T.; Black, M.; Sawyer, T.K.; Nerad, T.A. Korotnevella hemistylolepis N. Sp. and Korotnevella monacantholepis N. Sp. (Paramoebidae), Two New Scale-covered Mesohaline Amoebae. J. Eukaryot. Microbiol. 2001, 48, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Michel, R.; Smirnov, A. The genus Flamella Schaeffer, 1926 (lobosea, gymnamoebia), with description of two new species. Eur. J. Protistol. 1999, 35, 403–410. [Google Scholar] [CrossRef]
- Rodríguez-Zaragoza, S. Ecology of free-living amoebae. Crit. Rev. Microbiol. 1994, 20, 225–241. [Google Scholar] [CrossRef] [PubMed]
- Marshall, M.M.; Naumovitz, D.; Ortega, Y.; Sterling, C.R. Waterborne protozoan pathogens. Clin. Microbiol. Rev. 1997, 10, 67–85. [Google Scholar] [CrossRef]
- Loret, J.; Greub, G. Free-living amoebae: Biological by-passes in water treatment. Int. J. Hyg. Environ. Health 2010, 213, 167–175. [Google Scholar] [CrossRef]
- Matz, C.; Kjelleberg, S. Off the hook—How bacteria survive protozoan grazing. Trends Microbiol. 2005, 13, 302–307. [Google Scholar] [CrossRef]
- Molmeret, M.; Horn, M.; Wagner, M.; Santic, M.; Kwaik, Y.A. Amoebae as Training Grounds for Intracellular Bacterial Pathogens. Appl. Environ. Microbiol. 2005, 71, 20–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Winiecka-Krusnell, J.; Linder, E. Bacterial infections of free living amebae. Res. Microbiol. 2001, 152, 613–619. [Google Scholar] [CrossRef]
- Thomas, V.; McDonnel, G.; Denyer, S.P.; Maillard, J.-Y. Free-living amoebae and their intracellular pathogenic microorganisms: Risk for water quality. FEMS Microbiol. Rev. 2010, 34, 231–259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lowe, C.; Willey, B.; O’Shaughnessy, A.; Lee, W.; Lum, M.; Pike, K.; Larocque, C.; Dedier, H.; Dales, L.; Moore, C.; et al. Outbreak of Extended-Spectrum β-Lactamase–producing Klebsiella oxytoca Infections Associated with Contaminated Handwashing Sinks1. Emerg. Infect. Dis. 2012, 18, 1242–1247. [Google Scholar] [CrossRef] [PubMed]
- Brooke, J.S. Stenotrophomonas maltophilia: And Emerging Global Opportunistic Pathogen. Clin. Microbiol. Rev. 2012, 25, 2–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murugaiyan, J.; Krueger, K.; Roesler, U.; Weinreich, J.; Schierack, P. Assessment of species and antimicrobial resistance among Enterobacteriaceae isolated from mallard duck faeces. Environ. Monit. Assess. 2015, 187, 127. [Google Scholar] [CrossRef]
- Ross, A.J. Mycobacterium salmoniphilum sp. nov. from salmonoid fishes. Am. Rev. Resp. Dis. 1960, 81, 241–250. [Google Scholar]
- Sikorski, J.; Stackebrandt, E.; Wackernagel, W. Pseudomonas kilonensis sp. nov., a bacterium isolated from agricultural soil. Int. J. Syst. Evol. Microbiol. 2001, 51, 1549–1555. [Google Scholar] [CrossRef] [Green Version]
- Kwon, S.W.; Kim, J.S.; Park, I.C.; Yoon, S.H.; Park, D.H.; Lim, C.K.; Go, S.J. Pseudomonas koreensis sp. nov., Pseudomonas umsongensis sp. nov. and Pseudomonas jinjuensis sp. nov., novel species from farm soils in Korea. Int. J. Syst. Evol. Microbiol. 2003, 53, 21–27. [Google Scholar] [CrossRef] [Green Version]
- Yu, H.S.; Jeong, H.J.; Hong, Y.C.; Seol, S.Y.; Chung, D.I.; Kong, H.H. Natural occurrence of Mycobacterium as an endosymbiont of Acanthamoeba isolated from a contact lens storage case. Korean J. Parasitol. 2007, 45, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Krishna Prasad, B.N.; Gupta, S.K. Preliminary report on the engulfment and retention of mycobacteria by trophozoites of axenically grown Acanthamoeba castellanii Douglas, 1930. Curr. Sci. 1978, 47, 245–247. [Google Scholar]

| Presumptive Identification of FLA Types | Water in Storage Container (n = 398) | Biofilm in Storage Container (n = 392) |
|---|---|---|
| Trophozoites | Acanthamoeba cysts | Round cysts |
| 26.9% (107/398) | 89.2% (355/398) | 32.2% (128/398) |
| 13.8% (54/392) | 79.6% (312/392) | 48.5% (190/392) |
| FLA Type | Water (n = 42) | Biofilm (n = 34) |
|---|---|---|
| Trophozoites (n = 42) | 28 | 13 |
| Presumptive Acanthamoeba (n = 43) | 14 | 21 |
| Primer Set Used | Water in Storage Container (n = 42) | Biofilm in Storage Container (n = 34) |
|---|---|---|
| Ami6F1, Ami6F2, Ami9R (FLA) [42] | 38.1% (16/42) | 20.6% (7/34) |
| JDP1, JDP2 (Acanthamoeba spp.) [44] | 14.3% (6/42) | 11.8% (4/34) |
| FLA Types Isolated | Total nr of FLA Isolated (n) | FLA Isolated form Stored Water | FLA Isolated from Biofilm |
|---|---|---|---|
| Amoebozoa spp. | 5 | 3 | 2 |
| Acanthamoeba spp. | 5 | 3 | 2 |
| Genotype T3 | 1 | 1 | 0 |
| Genotype T4 | 5 | 3 | 1 |
| Genotype T15 | 1 | 1 | 0 |
| Genotype T16 | 4 | 2 | 2 |
| Flamella spp. | 2 | 2 | 0 |
| F. fluviatalis | 1 | 1 | 0 |
| Korotnevella spp. | |||
| Korotnevella hemistylolepis | 1 | 0 | 1 |
| Lobosea spp. | 1 | 1 | 0 |
| Stenamoeba spp. | 2 | 2 | 0 |
| S. berchidia | 1 | 0 | 1 |
| Vermamoeba spp. | |||
| V. vermiformis | 20 | 16 | 4 |
| Vexillifera spp. | |||
| V. westveldii | 1 | 1 | 0 |
| Total | 50 | 36 | 14 |
| Potential Human Pathogen Bacteria Isolated | ||
|---|---|---|
| Pseudomonas spp.: Pseudomonas fluorescens Pseudomonas geniculata Pseudomonas kilonensis Pseudomonas koreensis Pseudomonas poae Pseudomonas tremae Pseudomonas vancouverensis Pseudomonas poae/tolaasii Pseudomonas putida | Arthobacter spp.: Arthrobacter nicotinovorans | Mycobacterium spp.: Mycobacterium chlorophenolicum Mycobacterium chubuense Mycobacterium elephantis Mycobacterium fallax Mycobacterium farcinogenes Mycobacterium florentinum Mycobacterium gilvum Mycobacterium intermedium Mycobacterium llatzerense Mycobacterium noviomagense Mycobacterium pallens Mycobacterium poriferae Mycobacterium psychrotolerans Mycobacterium rhodesiae Mycobacterium salmoniphilum Mycobacterium smegmatis Mycobacterium tokaiense Mycobacterium triplex |
| Caulobacter spp.: Caulobacter segnis | ||
| Klebsiella spp.: Klebsiella oxytoca Klebsiella variicola | ||
| Enterobacter spp.: Enterobacter amnigenus Enterobacter asburiae Enterobacter cancerogenus Enterobacter kobei Enterobacter ludwigii | Paenibacillus spp.: Paenibacillus validus | |
| Pragia spp.: Pragia fontium | Microbacterium spp.: Microbacterium spp. Microbacterium oxydans Microbacterium paraoxydans | |
| Achromobacter spp.: Achromobacter insolitus Achromobacter marplatensis Achromobacter spanius | Rhodococcus spp.: Rhodococcus erythropolis | |
| Sarratia spp.: Serratia ureilytica | ||
| Stenotrophomonas spp.: Stenotrophomonas maltophilia | ||
| Mixed bacterial spp.: Alcaligenes faecalis and Achromobacter marplatensis | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Potgieter, N.; van der Loo, C.; Barnard, T.G. Co-Existence of Free-Living Amoebae and Potential Human Pathogenic Bacteria Isolated from Rural Household Water Storage Containers. Biology 2021, 10, 1228. https://doi.org/10.3390/biology10121228
Potgieter N, van der Loo C, Barnard TG. Co-Existence of Free-Living Amoebae and Potential Human Pathogenic Bacteria Isolated from Rural Household Water Storage Containers. Biology. 2021; 10(12):1228. https://doi.org/10.3390/biology10121228
Chicago/Turabian StylePotgieter, Natasha, Clarissa van der Loo, and Tobias George Barnard. 2021. "Co-Existence of Free-Living Amoebae and Potential Human Pathogenic Bacteria Isolated from Rural Household Water Storage Containers" Biology 10, no. 12: 1228. https://doi.org/10.3390/biology10121228






