Characteristics of COVID-19 Inpatients in Rehabilitation Units during the First Pandemic Wave: A Cohort Study from a Large Hospital in Champagne Region
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Study Measurements
2.4. Statistical Analysis
3. Results
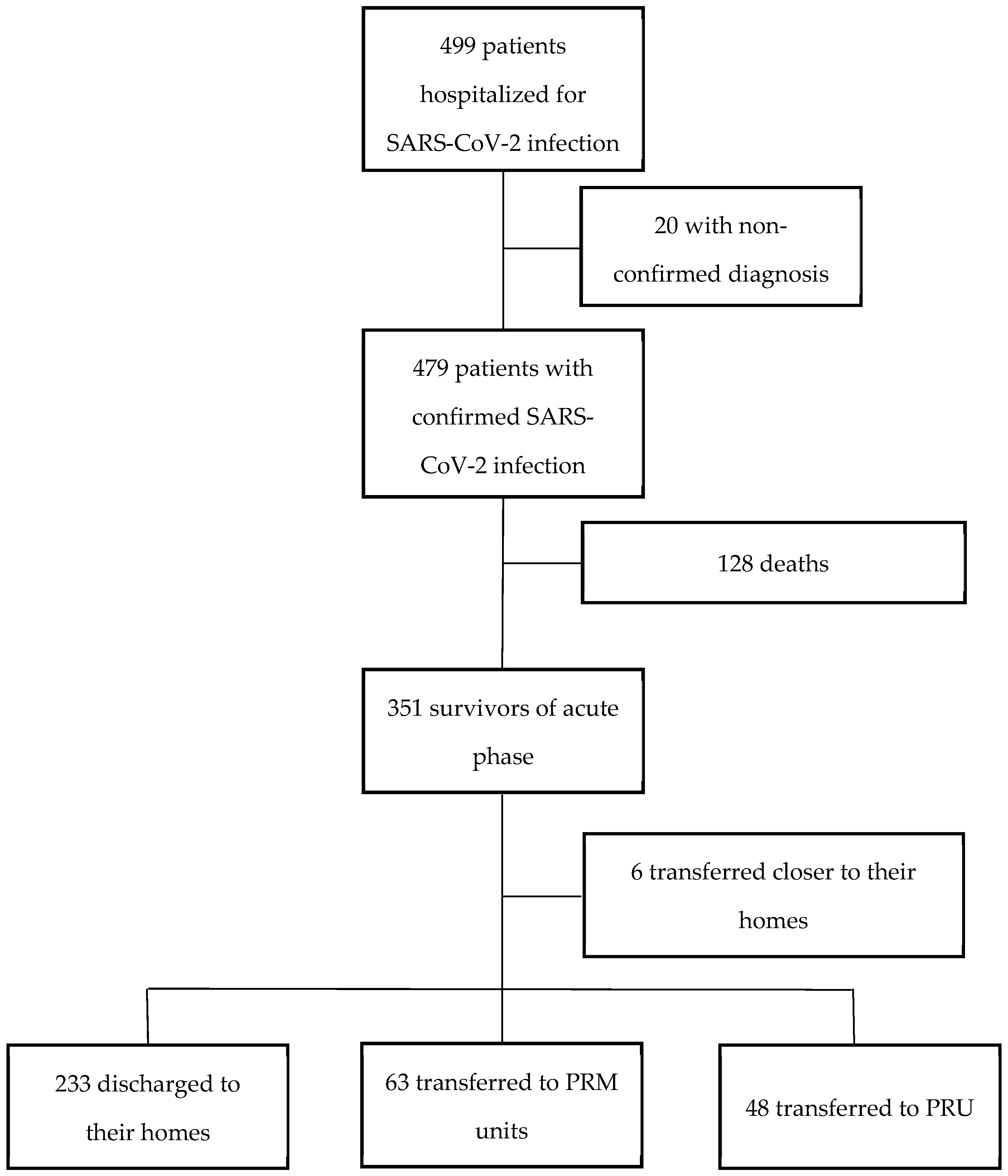
3.1. Population Distribution
3.2. Population Characteristics
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Slim, K.; Boirie, Y. The quintuple penalty of obese patients in the COVID-19 pandemic. Surg. Obes. Relat. Dis. Off. J. Am. Soc. Bariatr. Surg. 2020, 16, 1163–1164. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet Lond. Engl. 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Torres-Ruiz, J.; Pérez-Fragoso, A.; Maravillas-Montero, J.L.; Llorente, L.; Mejía-Domínguez, N.R.; Páez-Franco, J.C.; Romero-Ramírez, S.; Sosa-Hernández, V.A.; Cervantes-Díaz, R.; Absalón-Aguilar, A.; et al. Redefining COVID-19 Severity and Prognosis: The Role of Clinical and Immunobiotypes. Front. Immunol. 2021, 12, 689966. [Google Scholar] [CrossRef]
- Mudatsir, M.; Fajar, J.K.; Wulandari, L.; Soegiarto, G.; Ilmawan, M.; Purnamasari, Y.; Mahdi, B.A.; Jayanto, G.D.; Suhendra, S.; Setianingsih, Y.A.; et al. Predictors of COVID-19 severity: A systematic review and meta-analysis. F1000Res 2021, 9, 1107. [Google Scholar] [CrossRef]
- Emanuel, E.J.; Persad, G.; Upshur, R.; Thome, B.; Parker, M.; Glickman, A.; Zhang, C.; Boyle, C.; Smith, M.; Phillips, J.P. Fair Allocation of Scarce Medical Resources in the Time of Covid-19. N. Engl. J. Med. 2020, 382, 2049–2055. [Google Scholar] [CrossRef]
- Ranney, M.L.; Griffeth, V.; Jha, A.K. Critical Supply Shortages—The Need for Ventilators and Personal Protective Equipment during the Covid-19 Pandemic. N. Engl. J. Med. 2020, 382, e41. [Google Scholar] [CrossRef]
- Tran, B.X.; Vo, L.H.; Phan, H.T.; Pham, H.Q.; Vu, G.T.; Le, H.T.; Latkin, C.A.; Ho, C.S.; Ho, R.C. Mobilizing medical students for COVID-19 responses: Experience of Vietnam. J. Glob. Health 2020, 10, 020319. [Google Scholar] [CrossRef]
- Park, S.; Elliott, J.; Berlin, A.; Hamer-Hunt, J.; Haines, A. Strengthening the UK primary care response to covid-19. BMJ 2020, 370, m3691. [Google Scholar] [CrossRef]
- Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7). Chin. Med. J. (Engl.) 2020, 133, 1087–1095. [CrossRef]
- Salje, H.; Tran Kiem, C.; Lefrancq, N.; Courtejoie, N.; Bosetti, P.; Paireau, J.; Andronico, A.; Hozé, N.; Richet, J.; Dubost, C.-L.; et al. Estimating the burden of SARS-CoV-2 in France. Science 2020, 369, 208–211. [Google Scholar] [CrossRef]
- Chan, K.; Zheng, J.; Mok, Y.W.; Li, Y.; Liu, Y.-N.; Chu, C.; Ip, M.S. SARS: Prognosis, outcome and sequelae. Respirology 2003, 8, S36–S40. [Google Scholar] [CrossRef]
- Hui, D.S.C.; Wong, K.T.; Antonio, G.E.; Tong, M.; Chan, D.P.; Sung, J.J.Y. Long-term sequelae of SARS: Physical, neuropsychiatric, and quality-of-life assessment. Hong Kong Med. J. Xianggang Yi Xue Za Zhi 2009, 15 (Suppl. S8), 21–23. [Google Scholar]
- Herridge, M.S.; Tansey, C.M.; Matté, A.; Tomlinson, G.; Diaz-Granados, N.; Cooper, A.; Guest, C.B.; Mazer, C.D.; Mehta, S.; Stewart, T.E.; et al. Functional disability 5 years after acute respiratory distress syndrome. N. Engl. J. Med. 2011, 364, 1293–1304. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet Lond. Engl. 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Vanderlind, W.M.; Rabinovitz, B.B.; Miao, I.Y.; Oberlin, L.E.; Bueno-Castellano, C.; Fridman, C.; Jaywant, A.; Kanellopoulos, D. A systematic review of neuropsychological and psychiatric sequalae of COVID-19: Implications for treatment. Curr. Opin. Psychiatry 2021, 34, 420–433. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kumble, S.; Patel, B.; Pruski, A.D.; Azola, A.; Tatini, A.L.; Nadendla, K.; Richards, L.; Keszler, M.S.; Kott, M.; et al. Managing the Rehabilitation Wave: Rehabilitation Services for COVID-19 Survivors. Arch. Phys. Med. Rehabil. 2020, 101, 2243–2249. [Google Scholar] [CrossRef]
- Argenziano, M.G.; Bruce, S.L.; Slater, C.L.; Tiao, J.R.; Baldwin, M.R.; Barr, R.G.; Chang, B.P.; Chau, K.H.; Choi, J.J.; Gavin, N.; et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: Retrospective case series. BMJ 2020, 369, m1996. [Google Scholar] [CrossRef]
- Somani, S.S.; Richter, F.; Fuster, V.; De Freitas, J.K.; Naik, N.; Sigel, K.; Mount Sinai COVID Informatics Center; Bottinger, E.P.; Levin, M.A.; Fayad, Z.; et al. Characterization of Patients Who Return to Hospital Following Discharge from Hospitalization for COVID-19. J. Gen. Intern. Med. 2020, 35, 2838–2844. [Google Scholar] [CrossRef]
- Lavery, A.M.; Preston, L.E.; Ko, J.Y.; Chevinsky, J.R.; DeSisto, C.L.; Pennington, A.F.; Kompaniyets, L.; Datta, S.D.; Click, E.S.; Golden, T.; et al. Characteristics of Hospitalized COVID-19 Patients Discharged and Experiencing Same-Hospital Readmission-United States, March-August 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1695–1699. [Google Scholar] [CrossRef]
- Wiertz, C.M.H.; Vints, W.A.J.; Maas, G.J.C.M.; Rasquin, S.M.C.; van Horn, Y.Y.; Dremmen, M.P.M.; Hemmen, B.; Verbunt, J.A. COVID-19: Patient Characteristics in the First Phase of Postintensive Care Rehabilitation. Arch. Rehabil. Res. Clin. Transl. 2021, 3, 100108. [Google Scholar] [CrossRef] [PubMed]
- Gaudart, J.; Landier, J.; Huiart, L.; Legendre, E.; Lehot, L.; Bendiane, M.K.; Chiche, L.; Petitjean, A.; Mosnier, E.; Kirakoya-Samadoulougou, F.; et al. Factors associated with the spatial heterogeneity of the first wave of COVID-19 in France: A nationwide geo-epidemiological study. Lancet Public Health 2021, 6, e222–e231. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. Lond. Engl. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tuty Kuswardhani, R.A.; Henrina, J.; Pranata, R.; Anthonius Lim, M.; Lawrensia, S.; Suastika, K. Charlson comorbidity index and a composite of poor outcomes in COVID-19 patients: A systematic review and meta-analysis. Diabetes Metab. Syndr. 2020, 14, 2103–2109. [Google Scholar] [CrossRef]
- McGinley, A.; Pearse, R.M. A national early warning score for acutely ill patients. BMJ 2012, 345, e5310. [Google Scholar] [CrossRef]
- Décision d’admission des patients en unités de réanimation et unités de soins critiques dans un contexte d’épidémie à Covid-19. Société Fr. D’Anesthésie Réanimation. Available online: https://sfar.org/decision-dadmission-des-patients-en-unites-de-reanimation-et-unites-de-soins-critiques-dans-un-contexte-depidemie-a-covid-19/ (accessed on 15 May 2022).
- Katz, S.; Ford, A.B.; Moskowitz, R.W.; Jackson, B.A.; Jaffe, M.W. Studies of illness in the aged. the index of adl: A standardized measure of biological and psychosocial function. JAMA 1963, 185, 914–919. [Google Scholar] [CrossRef]
- Halpin, S.J.; McIvor, C.; Whyatt, G.; Adams, A.; Harvey, O.; McLean, L.; Walshaw, C.; Kemp, S.; Corrado, J.; Singh, R.; et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J. Med. Virol. 2021, 93, 1013–1022. [Google Scholar] [CrossRef]
- Nakayama, L.F.; Urias, M.G.; Gonçalves, A.S.; Ribeiro, R.A.; Macruz, T.d.A.; Pardo, R.B. Post-discharge follow-up of patients with COVID-19: A Brazilian experience. SAGE Open Med. 2022, 10, 20503121221096600. [Google Scholar] [CrossRef]
- Fugazzaro, S.; Denti, M.; Mainini, C.; Accogli, M.A.; Bedogni, G.; Ghizzoni, D.; Bertolini, A.; Esseroukh, O.; Gualdi, C.; Schiavi, M.; et al. Sex differences and rehabilitation needs after hospital discharge for COVID-19: An Italian cross-sectional study. BMJ Open 2022, 12, e055308. [Google Scholar] [CrossRef]
- Daunter, A.K.; Bowman, A.; Danko, J.; Claflin, E.S.; Kratz, A.L. Functional decline in hospitalized patients with COVID-19 in the early months of the pandemic. PM R 2022, 14, 198–201. [Google Scholar] [CrossRef]
- Mehlhorn, J.; Freytag, A.; Schmidt, K.; Brunkhorst, F.M.; Graf, J.; Troitzsch, U.; Schlattmann, P.; Wensing, M.; Gensichen, J. Rehabilitation interventions for postintensive care syndrome: A systematic review. Crit. Care Med. 2014, 42, 1263–1271. [Google Scholar] [CrossRef]
- Mijnarends, D.M.; Koster, A.; Schols, J.M.G.A.; Meijers, J.M.M.; Halfens, R.J.G.; Gudnason, V.; Eiriksdottir, G.; Siggeirsdottir, K.; Sigurdsson, S.; Jónsson, P.V.; et al. Physical activity and incidence of sarcopenia: The population-based AGES-Reykjavik Study. Age Ageing 2016, 45, 614–620. [Google Scholar] [CrossRef] [Green Version]
- Hägg, S.; Jylhävä, J.; Wang, Y.; Xu, H.; Metzner, C.; Annetorp, M.; Garcia-Ptacek, S.; Khedri, M.; Boström, A.-M.; Kadir, A.; et al. Age, Frailty, and Comorbidity as Prognostic Factors for Short-Term Outcomes in Patients With Coronavirus Disease 2019 in Geriatric Care. J. Am. Med. Dir. Assoc. 2020, 21, 1555–1559.e2. [Google Scholar] [CrossRef]
- Imazio, M.; Klingel, K.; Kindermann, I.; Brucato, A.; De Rosa, F.G.; Adler, Y.; De Ferrari, G.M. COVID-19 pandemic and troponin: Indirect myocardial injury, myocardial inflammation or myocarditis? Heart Br. Card. Soc. 2020, 106, 1127–1131. [Google Scholar] [CrossRef]
- Lin, L.; Wang, X.; Ren, J.; Sun, Y.; Yu, R.; Li, K.; Zheng, L.; Yang, J. Risk factors and prognosis for COVID-19-induced acute kidney injury: A meta-analysis. BMJ Open 2020, 10, e042573. [Google Scholar] [CrossRef] [PubMed]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Carda, S.; Invernizzi, M.; Bavikatte, G.; Bensmaïl, D.; Bianchi, F.; Deltombe, T.; Draulans, N.; Esquenazi, A.; Francisco, G.E.; Gross, R.; et al. The role of physical and rehabilitation medicine in the COVID-19 pandemic: The clinician’s view. Ann. Phys. Rehabil. Med. 2020, 63, 554–556. [Google Scholar] [CrossRef]
- Ahmad, M.; Kim, K.; Indorato, D.; Petrenko, I.; Diaz, K.; Rotatori, F.; Salhany, R.; Lakhi, N. Post-COVID Care Center to Address Rehabilitation Needs in COVID-19 Survivors: A Model of Care. Am. J. Med. Qual. Off. J. Am. Coll. Med. Qual. 2022, 37, 266–271. [Google Scholar] [CrossRef]
- Lew, H.L.; Oh-Park, M.; Cifu, D.X. The War on COVID-19 Pandemic: Role of Rehabilitation Professionals and Hospitals. Am. J. Phys. Med. Rehabil. 2020, 99, 571–572. [Google Scholar] [CrossRef]
- World Health Organization, Regional Office for Europe. Strengthening the Health System Response to COVID-19: Technical Guidance #1: Maintaining the Delivery of Essential Health Care Services While Mobilizing the Health Workforce for the COVID-19 Response, 18 April 2020; World Health Organization, Regional Office for Europe: Geneva, Switzerland, 2020. [Google Scholar]
- Alemanno, F.; Houdayer, E.; Parma, A.; Spina, A.; Del Forno, A.; Scatolini, A.; Angelone, S.; Brugliera, L.; Tettamanti, A.; Beretta, L.; et al. COVID-19 cognitive deficits after respiratory assistance in the subacute phase: A COVID-rehabilitation unit experience. PLoS ONE 2021, 16, e0246590. [Google Scholar] [CrossRef]
- van den Borst, B.; Peters, J.B.; Brink, M.; Schoon, Y.; Bleeker-Rovers, C.P.; Schers, H.; van Hees, H.W.H.; van Helvoort, H.; van den Boogaard, M.; van der Hoeven, H.; et al. Comprehensive health assessment three months after recovery from acute COVID-19. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2020. [Google Scholar] [CrossRef]
- Zhou, H.; Lu, S.; Chen, J.; Wei, N.; Wang, D.; Lyu, H.; Shi, C.; Hu, S. The landscape of cognitive function in recovered COVID-19 patients. J. Psychiatr. Res. 2020, 129, 98–102. [Google Scholar] [CrossRef]
- Townsend, L.; Dowds, J.; O’Brien, K.; Sheill, G.; Dyer, A.H.; O’Kelly, B.; Hynes, J.P.; Mooney, A.; Dunne, J.; Ni Cheallaigh, C.; et al. Persistent Poor Health after COVID-19 Is Not Associated with Respiratory Complications or Initial Disease Severity. Ann. Am. Thorac. Soc. 2021, 18, 997–1003. [Google Scholar] [CrossRef] [PubMed]
- Katzenschlager, S.; Zimmer, A.J.; Gottschalk, C.; Grafeneder, J.; Schmitz, S.; Kraker, S.; Ganslmeier, M.; Muth, A.; Seitel, A.; Maier-Hein, L.; et al. Can we predict the severe course of COVID-19—A systematic review and meta-analysis of indicators of clinical outcome? PLoS ONE 2021, 16, e0255154. [Google Scholar] [CrossRef]
- Lam Wai Shun, P.; Bottari, C.; Dubé, S.; Grondin, M.; Swaine, B. Factors influencing clinicians’ referral or admission decisions for post-acute stroke or traumatic brain injury rehabilitation: A scoping review. PM R 2021. Online Version of Record before inclusion in an issue. [Google Scholar] [CrossRef]
- Petrilli, C.M.; Jones, S.A.; Yang, J.; Rajagopalan, H.; O’Donnell, L.; Chernyak, Y.; Tobin, K.A.; Cerfolio, R.J.; Francois, F.; Horwitz, L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 2020, 369, m1966. [Google Scholar] [CrossRef]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet Lond. Engl. 2013, 381, 752–762. [Google Scholar] [CrossRef] [Green Version]
| Characteristic | Home (A) n = 233 | PRM Units (B) n = 63 | p Value (A) vs. (B) | PRU (C) n = 48 | p Value (B) vs. (C) | |||
|---|---|---|---|---|---|---|---|---|
| Women (n, %) | 120 | (51.5%) | 28 | (44.4%) | 0.320 | 22 | (45.8%) | 0.884 |
| Age, years (median, [Q1–Q3]) | 67 | [53–79] | 72 | [68–81] | 0.001 | 82 | [72.8–85] | 0.002 |
| BMI Kg/m2 ‡ (median, [Q1–Q3]) | 29 | [25–32] | 27 | [23–32.2] | 0.293 | 24 | [22–28] | 0.010 |
| BMI ≥ 30 Kg/m2 ‡ (n, %) | 13 | (5.6%) | 4 | (6.3%) | 0.999 | 0 | (0.0%) | 0.129 |
| Current smokers * (n, %) | 14 | (6.0%) | 3 | (4.8%) | 0.572 | 1 | (2.1%) | 0.999 |
| Arterial hypertension (n, %) | 117 | (50.2%) | 38 | (60.3%) | 0.572 | 29 | (60.4%) | 0.885 |
| Diabetes (n, %) | 54 | (23.2%) | 21 | (33.3%) | 0.253 | 11 | (22.9%) | 0.197 |
| Chronic respiratory disease (n, %) | 40 | (17.2%) | 14 | (22.2%) | 0.610 | 10 | (20.8%) | 0.810 |
| Renal failure requiring RRT (n, %) | 14 | (6.0%) | 3 | (4.8%) | 0.769 | 4 | (8.7%) | 0.697 |
| Charlson score (median, [Q1–Q3]) | 1 | [0–2] | 1 | [0–3] | 0.586 | 2 | [1–4] | 0.093 |
| At risk of severe form of disease (n, %) | 194 | (83.3%) | 59 | (93.65%) | 0.038 | 46 | (95.8%) | 0.697 |
| Home (A) n = 233 | PRM Units (B) n = 63 | p Value (A) vs. (B) | PRU (C) n = 48 | p Value (B) vs. (C) | ||||
|---|---|---|---|---|---|---|---|---|
| Clinical presentation | ||||||||
| Severe clinical presentation (n, %) | 60 | (25.8%) | 22 | (34.9%) | 0.149 | 13 | (27.1%) | 0.379 |
| Early warning score † (median, [Q1–Q3]) | 6 | [3–8] | 7 | [4–9] | 0.091 | 8 | [5–10] | 0.343 |
| Oxygen therapy at admission (n, %) | 89 | (38.2%) | 30 | (47.6%) | 0.060 | 23 | (47.9%) | 0.782 |
| Breathing rate (median, [Q1–Q3]) | 22 | [18–26] | 20 | [17.8–28] | 0.779 | 20 | [18–25.8] | 0.875 |
| Pulmonary embolism (n, %) | 10 | (4.3%) | 4 | (6.3%) | 0.509 | 3 | (6.2%) | 0.999 |
| Biology during acute infection | ||||||||
| Leukocytes, G/L (median, [Q1–Q3]) | 6.9 | [4.9–9] | 6.55 | [4.8–8.2] | 0.250 | 6 | [3.8–9.8] | 0.999 |
| Lymphocytes < 1.5 G/L (n, %) | 179 | (76.8%) | 53 | (84.1%) | 0.09 | 35 | (72.9%) | 0.22 |
| GFR < 60 mL/min/kg (n, %) | 56 | (24%) | 24 | (38.1%) | 0.03 | 18 | (37.5%) | 0.98 |
| Albuminemia, g/L ₮ (median, [Q1–Q3]) | 35 | [31–38] | 33 | [30.8–36] | 0.072 | 30 | [26–37] | 0.121 |
| CRP mg/L (median, [Q1–Q3]) | 61.6 | [22.5–120] | 90,3 | [30.4–157] | 0.096 | 37.7 | [14.2–91.4] | 0.032 |
| Troponin, ng/L ¥ (median, [Q1–Q3]) | 13.8 | [6.2–34.8] | 19,4 | [13.9–29.6] | 0.030 | 32 | [16.4–92.4] | 0.012 |
| Treatments | ||||||||
| Need for ICU admission (n, %) | 29 | (12.4%) | 27 | (42.9%) | <0.0001 | 9 | (18.7%) | 0.007 |
| Antibiotic therapy (n, %) | 217 | (93.1%) | 62 | (98.4%) | 0.135 | 45 | (93.7%) | 0.314 |
| Corticosteroid therapy (n, %) | 122 | (52.4%) | 41 | (65.1%) | 0.077 | 27 | (56.2%) | 0.344 |
| Anticoagulant therapy (n, %) | 219 | (94.0%) | 62 | (98.4%) | 0.207 | 45 | (93.7%) | 0.314 |
| Length of stay, days (median, [Q1–Q3]) | 8 | [5–14] | 15 | [10–32.5] | <0.0001 | 15.5 | [10.2–29.0] | 0.847 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rapin, A.; Noujaim, P.-J.; Taiar, R.; Carazo-Mendez, S.; Deslee, G.; Jolly, D.; Boyer, F.C. Characteristics of COVID-19 Inpatients in Rehabilitation Units during the First Pandemic Wave: A Cohort Study from a Large Hospital in Champagne Region. Biology 2022, 11, 937. https://doi.org/10.3390/biology11060937
Rapin A, Noujaim P-J, Taiar R, Carazo-Mendez S, Deslee G, Jolly D, Boyer FC. Characteristics of COVID-19 Inpatients in Rehabilitation Units during the First Pandemic Wave: A Cohort Study from a Large Hospital in Champagne Region. Biology. 2022; 11(6):937. https://doi.org/10.3390/biology11060937
Chicago/Turabian StyleRapin, Amandine, Peter-Joe Noujaim, Redha Taiar, Sandy Carazo-Mendez, Gaetan Deslee, Damien Jolly, and François Constant Boyer. 2022. "Characteristics of COVID-19 Inpatients in Rehabilitation Units during the First Pandemic Wave: A Cohort Study from a Large Hospital in Champagne Region" Biology 11, no. 6: 937. https://doi.org/10.3390/biology11060937
APA StyleRapin, A., Noujaim, P.-J., Taiar, R., Carazo-Mendez, S., Deslee, G., Jolly, D., & Boyer, F. C. (2022). Characteristics of COVID-19 Inpatients in Rehabilitation Units during the First Pandemic Wave: A Cohort Study from a Large Hospital in Champagne Region. Biology, 11(6), 937. https://doi.org/10.3390/biology11060937







