Shoulder Surgery Postoperative Immobilization: An International Survey of Shoulder Surgeons
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Arthroscopic Bankart Repair (ABR)
3.2. Latarjet
3.3. ARCR (Tears < 3 cm)
3.4. ARCR Cuff (Tears > 3 cm)
3.5. aTSA
3.6. rTSA with Subscapularis Repair
3.7. rTSA without Subscapularis Repair
3.8. Isolated Biceps Tenodesis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jain, N.B.; Higgins, L.D.; Losina, E.; Collins, J.; Blazar, P.E.; Katz, J.N. Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet. Disord. 2014, 15, 4. [Google Scholar] [CrossRef] [PubMed]
- Craig, R.S.; Lane, J.C.E.; Carr, A.J.; Furniss, D.; Collins, G.S.; Rees, J.L. Serious adverse events and lifetime risk of reoperation after elective shoulder replacement: Population based cohort study using hospital episode statistics for England. BMJ (Clin. Res. Ed.) 2019, 364, l298. [Google Scholar] [CrossRef] [PubMed]
- Vidal, C.; Lira, M.J.; de Marinis, R.; Liendo, R.; Contreras, J.J. Increasing incidence of rotator cuff surgery: A nationwide registry study in Chile. BMC Musculoskelet. Disord. 2021, 22, 1052. [Google Scholar] [CrossRef] [PubMed]
- MacDermid, J.C.; Bryant, D.; Holtby, R.; Razmjou, H.; Faber, K.; Balyk, R.; Boorman, R.; Sheps, D.; McCormack, R.; Athwal, G.; et al. Arthroscopic Versus Mini-open Rotator Cuff Repair: A Randomized Trial and Meta-analysis. Am. J. Sport. Med. 2021, 49, 3184–3195. [Google Scholar] [CrossRef]
- Wong, I.; Sparavalo, S.; King, J.P.; Coady, C.M. Bridging Allograft Reconstruction Is Superior to Maximal Repair for the Treatment of Chronic, Massive Rotator Cuff Tears: Results of a Prospective, Randomized Controlled Trial. Am. J. Sport. Med. 2021, 49, 3173–3183. [Google Scholar] [CrossRef] [PubMed]
- Lapner, P.; Li, A.; Pollock, J.W.; Zhang, T.; McIlquham, K.; McRae, S.; MacDonald, P. A Multicenter Randomized Controlled Trial Comparing Single-Row With Double-Row Fixation in Arthroscopic Rotator Cuff Repair: Long-Term Follow-up. Am. J. Sport. Med. 2021, 49, 3021–3029. [Google Scholar] [CrossRef]
- Yapp, L.Z.; Nicholson, J.A.; Robinson, C.M. Primary Arthroscopic Stabilization for a First-Time Anterior Dislocation of the Shoulder: Long-Term Follow-up of a Randomized, Double-Blinded Trial. J. Bone Jt. Surg. Am. 2020, 102, 460–467. [Google Scholar] [CrossRef]
- Jonsson, E.; Ekholm, C.; Salomonsson, B.; Demir, Y.; Olerud, P. Reverse total shoulder arthroplasty provides better shoulder function than hemiarthroplasty for displaced 3- and 4-part proximal humeral fractures in patients aged 70 years or older: A multicenter randomized controlled trial. J. Shoulder Elb. Surg. 2021, 30, 994–1006. [Google Scholar] [CrossRef]
- Bandara, U.; An, V.V.G.; Imani, S.; Nandapalan, H.; Sivakumar, B.S. Rehabilitation protocols following rotator cuff repair: A meta-analysis of current evidence. ANZ J. Surg. 2021, 91, 2773–2779. [Google Scholar] [CrossRef]
- Chan, K.; MacDermid, J.C.; Hoppe, D.J.; Ayeni, O.R.; Bhandari, M.; Foote, C.J.; Athwal, G.S. Delayed versus early motion after arthroscopic rotator cuff repair: A meta-analysis. J. Shoulder Elb. Surg. 2014, 23, 1631–1639. [Google Scholar] [CrossRef]
- Arndt, J.; Clavert, P.; Mielcarek, P.; Bouchaib, J.; Meyer, N.; Kempf, J.F. Immediate passive motion versus immobilization after endoscopic supraspinatus tendon repair: A prospective randomized study. Orthop. Traumatol. Surg. Res. OTSR 2012, 98, S131–S138. [Google Scholar] [CrossRef] [PubMed]
- Klintberg, I.H.; Gunnarsson, A.C.; Svantesson, U.; Styf, J.; Karlsson, J. Early loading in physiotherapy treatment after full-thickness rotator cuff repair: A prospective randomized pilot-study with a two-year follow-up. Clin. Rehabil. 2009, 23, 622–638. [Google Scholar] [CrossRef]
- Abtahi, A.M.; Granger, E.K.; Tashjian, R.Z. Factors affecting healing after arthroscopic rotator cuff repair. World J. Orthop. 2015, 6, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Chung, S.W.; Kim, J.Y.; Ok, J.H.; Park, I.; Oh, J.H. Is early passive motion exercise necessary after arthroscopic rotator cuff repair? Am. J. Sport. Med. 2012, 40, 815–821. [Google Scholar] [CrossRef] [PubMed]
- Denard, P.J.; Lädermann, A.; Burkhart, S.S. Prevention and management of stiffness after arthroscopic rotator cuff repair: Systematic review and implications for rotator cuff healing. Arthroscopy 2011, 27, 842–848. [Google Scholar] [CrossRef] [PubMed]
- Hsu, J.E.; Horneff, J.G.; Gee, A.O. Immobilization After Rotator Cuff Repair: What Evidence Do We Have Now? Orthop. Clin. N. Am. 2016, 47, 169–177. [Google Scholar] [CrossRef]
- Sharareh, B.; Edwards, T.B.; Shah, A.; Shybut, T. Variation in technique and postoperative management of the Latarjet procedure among orthopedic surgeons. J. Shoulder Elb. Surg. 2021, 30, e157–e164. [Google Scholar] [CrossRef] [PubMed]
- Steinmetz, R.G.; Guth, J.J.; Matava, M.J.; Brophy, R.H.; Smith, M.V. Return to Play Following Non-Surgical Management of Superior Labrum Anterior-Posterior Tears: A Systematic Review. J. Shoulder Elb. Surg. 2022, 31, 1323–1333. [Google Scholar] [CrossRef]
- Kelley, T.D.; Clegg, S.; Rodenhouse, P.; Hinz, J.; Busconi, B.D. Functional Rehabilitation and Return to Play After Arthroscopic Surgical Stabilization for Anterior Shoulder Instability. Sport. Health 2021, 14, 19417381211062852. [Google Scholar] [CrossRef]
- McIsaac, W.; Lalani, A.; Silveira, A.; Chepeha, J.; Luciak-Corea, C.; Beaupre, L. Rehabilitation after arthroscopic Bankart repair: A systematic scoping review identifying important evidence gaps. Physiotherapy 2022, 114, 68–76. [Google Scholar] [CrossRef]
- Paterson, W.H.; Throckmorton, T.W.; Koester, M.; Azar, F.M.; Kuhn, J.E. Position and duration of immobilization after primary anterior shoulder dislocation: A systematic review and meta-analysis of the literature. J. Bone Jt. Surg. Am. 2010, 92, 2924–2933. [Google Scholar] [CrossRef] [PubMed]
- Sheps, D.M.; Silveira, A.; Beaupre, L.; Styles-Tripp, F.; Balyk, R.; Lalani, A.; Glasgow, R.; Bergman, J.; Bouliane, M. Early Active Motion Versus Sling Immobilization After Arthroscopic Rotator Cuff Repair: A Randomized Controlled Trial. Arthroscopy 2019, 35, 749–760.e742. [Google Scholar] [CrossRef]
- Tirefort, J.; Schwitzguebel, A.J.; Collin, P.; Nowak, A.; Plomb-Holmes, C.; Lädermann, A. Postoperative Mobilization After Superior Rotator Cuff Repair: Sling Versus No Sling: A Randomized Prospective Study. J. Bone Jt. Surg. Am. 2019, 101, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Whelan, D.B.; Kletke, S.N.; Schemitsch, G.; Chahal, J. Immobilization in External Rotation Versus Internal Rotation After Primary Anterior Shoulder Dislocation: A Meta-analysis of Randomized Controlled Trials. Am. J. Sport. Med. 2016, 44, 521–532. [Google Scholar] [CrossRef]
- Belk, J.W.; Wharton, B.R.; Houck, D.A.; Bravman, J.T.; Kraeutler, M.J.; Mayer, B.; Noonan, T.J.; Seidl, A.J.; Frank, R.M.; McCarty, E.C. Shoulder Stabilization Versus Immobilization for First-Time Anterior Shoulder Dislocation: A Systematic Review and Meta-analysis of Level 1 Randomized Controlled Trials. Am. J. Sport. Med. 2022, 3635465211065403. [Google Scholar] [CrossRef]
- Boland, K.; Smith, C.; Bond, H.; Briggs, S.; Walton, J. Current concepts in the rehabilitation of rotator cuff related disorders. J. Clin. Orthop. Trauma 2021, 18, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Handoll, H.H.; Hanchard, N.C.; Goodchild, L.; Feary, J. Conservative management following closed reduction of traumatic anterior dislocation of the shoulder. Cochrane Database Syst. Rev. 2006, Cd004962. [Google Scholar] [CrossRef]
- Grubhofer, F.; Gerber, C.; Meyer, D.C.; Wieser, K.; Ernstbrunner, L.; Catanzaro, S.; Bouaicha, S. Compliance with wearing an abduction brace after arthroscopic rotator cuff repair: A prospective, sensor-controlled study. Prosthet. Orthot. Int. 2019, 43, 440–446. [Google Scholar] [CrossRef]
- Lädermann, A.; Denard, P.J.; Tirefort, J.; Collin, P.; Nowak, A.; Schwitzguebel, A.J. Subscapularis- and deltoid-sparing vs traditional deltopectoral approach in reverse shoulder arthroplasty: A prospective case-control study. J. Orthop. Surg. Res. 2017, 12, 112. [Google Scholar] [CrossRef]
- Goetti, P.; Martinho, T.; Seurot, A.; Bothorel, H.; Läderman, A. Is there a benefit of sling immobilization after open Latarjet surgery for anterior shoulder instability? A randomized control trial. Rev. De Chir. Orthopédique Et Traumatol. 2022, 108, S257–S258. [Google Scholar] [CrossRef]








| Survey Question |
|---|
| 1. What country do you practice in? |
| 2. If you practice in the United States, what region? |
| 3. How many years have you been in practice? |
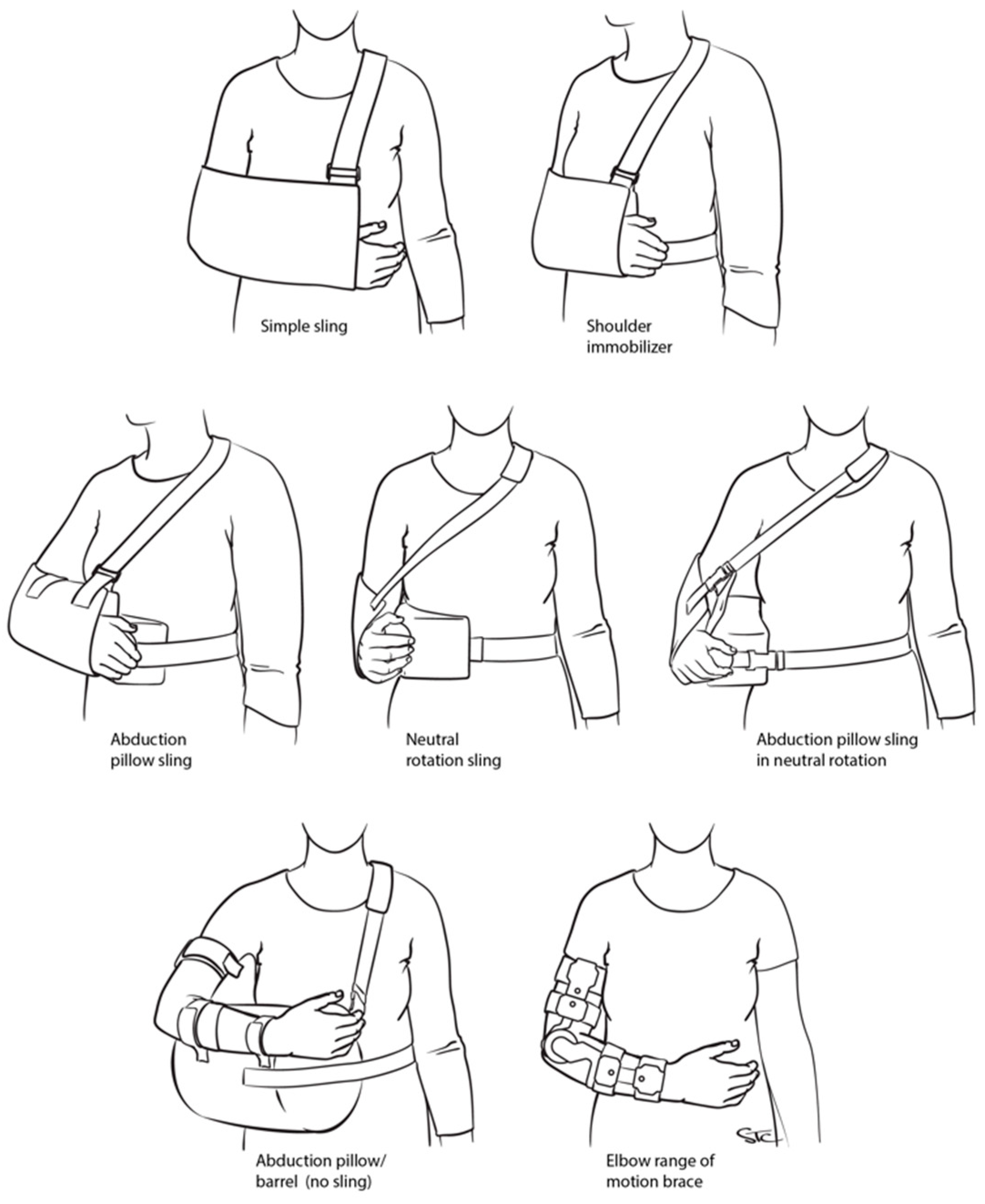
| 4. Following arthroscopic Bankart repair- which shoulder immobilization technique a do you use? |
| 5. For how long do they wear this? |
| 6. Following arthroscopic superior rotator cuff repair < 3 cm- which shoulder immobilization technique a do you use? |
| 7. For how long do they wear this? |
| 8. Following arthroscopic superior rotator cuff repair > 3 cm- which shoulder immobilization technique a do you use? |
| 9. For how long do they wear this? |
| 10. Following a Latarjet procedure- which shoulder immobilization technique a do you use? |
| 11. For how long do they wear this? |
| 12. Following an anatomic total shoulder arthroplasty- which shoulder immobilization technique a do you use? |
| 13. For how long do they wear this? |
| 14. Following a reverse shoulder arthroplasty WITH subscapularis repair- which shoulder immobilization technique a do you use? |
| 15. For how long do they wear this? |
| 16. Following a reverse shoulder arthroplasty WITHOUT subscapularis repair- which shoulder immobilization technique a do you use? |
| 17. For how long do they wear this? |
| 18. Following an isolated arthroscopic or open biceps tenodesis (no cuff repair)- which shoulder immobilization technique a do you use? |
| 19. For how long do they wear this? |
| Practice Location | N (%) |
|---|---|
| United States | 273 (54.7%) |
| Midwest | 62 (23%) |
| Northeast | 77 (28%) |
| South | 73 (27%) |
| West | 59 (22%) |
| Europe | 226 (45.3%) |
| Eastern | 12 (5%) |
| Northern | 36 (16%) |
| Southern | 60 (27%) |
| Western | 118 (52%) |
| USA | Europe | |||||
|---|---|---|---|---|---|---|
| N | % | N | % | p-Value | Post-Hoc Test | |
| Abduction Pillow Sling | 167 | 62% | 34 | 15% | <0.001 | <0.001 |
| Neutral + Abduction | 1 | 0% | 2 | 1% | >0.999 | |
| Neutral Rotation Sling | 4 | 1% | 7 | 3% | >0.999 | |
| No Sling | 2 | 1% | 1 | 0% | >0.999 | |
| Shoulder Immobilizer | 12 | 4% | 11 | 5% | >0.999 | |
| Simple Sling | 84 | 31% | 163 | 74% | <0.001 | |
| Other | 0 | 0% | 2 | 0% | >0.999 | |
| USA | Europe | |||||
|---|---|---|---|---|---|---|
| N | % | N | % | p-Value | Post-Hoc Test | |
| Abduction Pillow Sling | 137 | 53% | 26 | 12% | <0.001 | <0.001 |
| Mayo | 0 | 0% | 1 | 0% | >0.999 | |
| Neutral + Abduction | 0 | 0% | 1 | 0% | >0.999 | |
| Neutral Rotation Sling | 2 | 1% | 6 | 3% | 0.832 | |
| No Sling | 1 | 0% | 9 | 4% | 0.044 | |
| Shoulder Immobilizer | 5 | 2% | 5 | 2% | >0.999 | |
| Simple Sling | 115 | 44% | 173 | 78% | <0.001 | |
| Sling if Pain | 0 | 0% | 1 | 0% | >0.999 | |
| USA | Europe | |||||
|---|---|---|---|---|---|---|
| N | % | N | % | p-Value | Post-Hoc Test | |
| Ab Pillow No Sling | 1 | 0% | 1 | 0% | <0.001 | >0.999 |
| Abduction Pillow Sling | 216 | 80% | 108 | 42% | <0.001 | |
| Mayo | 0 | 0% | 1 | 0% | >0.999 | |
| Neutral Rotation Sling | 2 | 1% | 4 | 2% | >0.999 | |
| No Sling | 1 | 0% | 5 | 2% | 0.805 | |
| Shoulder Immobilizer | 5 | 2% | 9 | 3% | >0.999 | |
| Simple Sling | 45 | 17% | 130 | 50% | <0.001 | |
| USA | Europe | |||||
|---|---|---|---|---|---|---|
| N | % | N | % | p-Value | Post-Hoc Test | |
| Abduction Pillow Sling | 227 | 84% | 136 | 61% | <0.001 | <0.001 |
| Neutral + Abduction | 0 | 0% | 1 | 0% | >0.999 | |
| Neutral Rotation Sling | 3 | 1% | 1 | 0% | >0.999 | |
| No Sling | 2 | 1% | 2 | 1% | >0.999 | |
| Shoulder Immobilized/Simple Sling | 1 | 0% | 0 | 0% | >0.999 | |
| Shoulder Immobilizer | 3 | 1% | 7 | 3% | >0.999 | |
| Simple Sling | 35 | 13% | 77 | 34% | <0.001 | |
| USA | Europe | |||||
|---|---|---|---|---|---|---|
| N | % | N | % | p-Value | Post-Hoc Test | |
| Abduction Pillow Sling | 132 | 50% | 47 | 21% | <0.001 | <0.001 |
| External Rotation Brace | 0 | 0% | 1 | 0% | >0.999 | |
| Mayo | 0 | 0% | 1 | 0% | >0.999 | |
| Neutral Rotation Sling | 3 | 1% | 5 | 2% | >0.999 | |
| No Sling | 11 | 4% | 7 | 3% | >0.999 | |
| Shoulder Immobilizer | 10 | 4% | 8 | 4% | >0.999 | |
| Simple Sling | 109 | 41% | 154 | 69% | <0.001 | |
| USA | Europe | |||||
|---|---|---|---|---|---|---|
| N | % | N | % | p-Value | Post-Hoc Test | |
| Abduction Pillow Sling | 155 | 61% | 48 | 22% | <0.001 | <0.001 |
| External Rotation Brace | 0 | 0% | 1 | 0% | >0.999 | |
| Mayo | 0 | 0% | 1 | 0% | >0.999 | |
| Neutral Rotation Sling | 2 | 1% | 4 | 2% | >0.999 | |
| No Sling | 3 | 1% | 6 | 3% | >0.999 | |
| Shoulder Immobilizer | 7 | 3% | 5 | 2% | >0.999 | |
| Simple Sling | 89 | 35% | 153 | 70% | <0.001 | |
| USA | Europe | |||||
|---|---|---|---|---|---|---|
| N | % | N | % | p-Value | Post-Hoc Test | |
| Abduction Pillow Sling | 148 | 57% | 37 | 17% | <0.001 | <0.001 |
| Neutral Rotation Sling | 2 | 1% | 3 | 1% | >0.999 | |
| No Sling | 2 | 1% | 20 | 9% | <0.001 | |
| Shoulder Immobilizer | 6 | 2% | 0 | 0% | 0.150 | |
| Simple Sling | 100 | 39% | 161 | 73% | <0.001 | |
| USA | Europe | |||||
|---|---|---|---|---|---|---|
| Sling | N | % | N | % | p-Value | Post-Hoc Test |
| Abduction Pillow Sling | 49 | 18% | 16 | 7% | <0.001 | 0.002 |
| Elbow ROM Brace | 1 | 0% | 0 | 0% | >0.999 | |
| Neutral Rotation Sling | 1 | 0% | 2 | 1% | >0.999 | |
| No Sling | 10 | 4% | 19 | 9% | 0.192 | |
| Shoulder Immobilizer | 3 | 1% | 3 | 1% | >0.999 | |
| Simple Sling | 209 | 77% | 183 | 82% | 0.899 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Freehill, M.T.; Murray, I.R.; Calvo, E.; Lädermann, A.; Srikumaran, U. Shoulder Surgery Postoperative Immobilization: An International Survey of Shoulder Surgeons. Biology 2023, 12, 291. https://doi.org/10.3390/biology12020291
Freehill MT, Murray IR, Calvo E, Lädermann A, Srikumaran U. Shoulder Surgery Postoperative Immobilization: An International Survey of Shoulder Surgeons. Biology. 2023; 12(2):291. https://doi.org/10.3390/biology12020291
Chicago/Turabian StyleFreehill, Michael T., Iain R. Murray, Emilio Calvo, Alexandre Lädermann, and Uma Srikumaran. 2023. "Shoulder Surgery Postoperative Immobilization: An International Survey of Shoulder Surgeons" Biology 12, no. 2: 291. https://doi.org/10.3390/biology12020291
APA StyleFreehill, M. T., Murray, I. R., Calvo, E., Lädermann, A., & Srikumaran, U. (2023). Shoulder Surgery Postoperative Immobilization: An International Survey of Shoulder Surgeons. Biology, 12(2), 291. https://doi.org/10.3390/biology12020291







