Gut Microbiome in the Progression of NAFLD, NASH and Cirrhosis, and Its Connection with Biotics: A Bibliometric Study Using Dimensions Scientific Research Database
Abstract
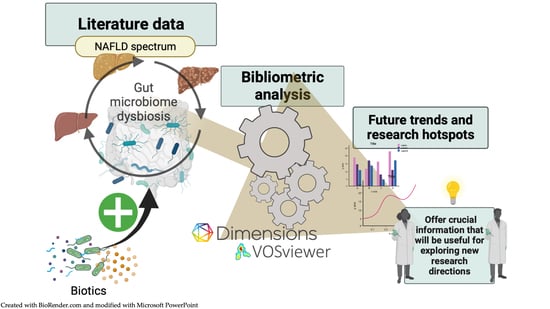
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Publication Trends and Country Productivity/Cooperation
3.2. Institution’s Productivity and Cooperation
3.3. Authors’ Productivity and Cooperation
3.4. Analysis of the Most Cited Journals and Articles
3.5. Analysis of Co-Citation References
3.6. Dynamic Changes in Co-Occurrence Keywords: A Visualization Analysis
4. Discussion
5. Conclusions
- -
- evaluation of risk factors that are associated with the progression of NAFLD, such as obesity and metabolic syndrome;
- -
- pathogenic mechanisms, such as liver inflammation through toll-like receptor activation or alteration of short-chain fatty acid metabolisms, which contribute to NAFLD development and its progression in more severe forms, such as cirrhosis;
- -
- therapy for cirrhosis rough dysbiosis reduction, and research on hepatic encephalopathy, a common consequence of cirrhosis;
- -
- evaluation of diversity, and composition of gut microbiome under NAFLD, and as it varies under NASH and cirrhosis by rRNA gene sequencing, a tool which can also be used for the development of new probiotics and explore into the impact of biotics on the gut microbiome;
- -
- treatments to reduce dysbiosis, almost with probiotics, prebiotics, and synbiotics, and with new probiotics, such as Akkermansia, or FMT, or diet.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thursby, E.; Juge, N. Introduction to the Human Gut Microbiota. Biochem. J. 2017, 474, 1823–1836. [Google Scholar] [CrossRef]
- Bartlomiejczyk, M.A.; Penson, P.; Banach, M. Human Microbiome Project Consortium Structure, Function and Diversity of the Healthy Human Microbiome. Nature 2012, 486, 207–214. [Google Scholar] [CrossRef][Green Version]
- Wang, J.; Chen, W.-D.; Wang, Y.-D. The Relationship between Gut Microbiota and Inflammatory Diseases: The Role of Macrophages. Front. Microbiol. 2020, 11, 1065. [Google Scholar] [CrossRef] [PubMed]
- Pezzino, S.; Sofia, M.; Greco, L.P.; Litrico, G.; Filippello, G.; Sarvà, I.; La Greca, G.; Latteri, S. Microbiome Dysbiosis: A Pathological Mechanism at the Intersection of Obesity and Glaucoma. Int. J. Mol. Sci. 2023, 24, 1166. [Google Scholar] [CrossRef]
- Zhang, H.; Chen, Y.; Wang, Z.; Xie, G.; Liu, M.; Yuan, B.; Chai, H.; Wang, W.; Cheng, P. Implications of Gut Microbiota in Neurodegenerative Diseases. Front. Immunol. 2022, 13, 325. [Google Scholar] [CrossRef]
- Albhaisi, S.A.M.; Bajaj, J.S. The Influence of the Microbiome on NAFLD and NASH. Clin. Liver Dis. 2021, 17, 15–18. [Google Scholar] [CrossRef]
- Kolodziejczyk, A.A.; Zheng, D.; Shibolet, O.; Elinav, E. The Role of the Microbiome in NAFLD and NASH. EMBO Mol. Med. 2019, 11, e9302. [Google Scholar] [CrossRef] [PubMed]
- Solé, C.; Guilly, S.; Silva, K.D.; Llopis, M.; Le-Chatelier, E.; Huelin, P.; Carol, M.; Moreira, R.; Fabrellas, N.; Prada, G.D.; et al. Alterations in Gut Microbiome in Cirrhosis as Assessed by Quantitative Metagenomics: Relationship with Acute-on-Chronic Liver Failure and Prognosis. Gastroenterology 2021, 160, 206–218.e13. [Google Scholar] [CrossRef]
- Byrne, C.D.; Targher, G. NAFLD: A Multisystem Disease. J. Hepatol. 2015, 62, S47–S64. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pezzino, S.; Sofia, M.; Faletra, G.; Mazzone, C.; Litrico, G.; La Greca, G.; Latteri, S. Gut-Liver Axis and Non-Alcoholic Fatty Liver Disease: A Vicious Circle of Dysfunctions Orchestrated by the Gut Microbiome. Biology 2022, 11, 1622. [Google Scholar] [CrossRef]
- Lee, N.Y.; Suk, K.T. The Role of the Gut Microbiome in Liver Cirrhosis Treatment. Int. J. Mol. Sci. 2020, 22, 199. [Google Scholar] [CrossRef]
- Albillos, A.; de Gottardi, A.; Rescigno, M. The Gut-Liver Axis in Liver Disease: Pathophysiological Basis for Therapy. J. Hepatol. 2020, 72, 558–577. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Song, Q.; Zhang, X. The Role of Gut–Liver Axis in Gut Microbiome Dysbiosis Associated NAFLD and NAFLD-HCC. Biomedicines 2022, 10, 524. [Google Scholar] [CrossRef]
- Pandey, K.R.; Naik, S.R.; Vakil, B.V. Probiotics, Prebiotics and Synbiotics—A Review. J. Food. Sci. Technol. 2015, 52, 7577–7587. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Carpi, R.Z.; Barbalho, S.M.; Sloan, K.P.; Laurindo, L.F.; Gonzaga, H.F.; Grippa, P.C.; Zutin, T.L.M.; Girio, R.J.S.; Repetti, C.S.F.; Detregiachi, C.R.P.; et al. The Effects of Probiotics, Prebiotics and Synbiotics in Non-Alcoholic Fat Liver Disease (NAFLD) and Non-Alcoholic Steatohepatitis (NASH): A Systematic Review. Int. J. Mol. Sci. 2022, 23, 8805. [Google Scholar] [CrossRef] [PubMed]
- Kanchanasurakit, S.; Kositamongkol, C.; Lanoi, K.; Nunta, M.; Saetuan, T.; Chaiyakunapruk, N.; Saokaew, S.; Phisalprapa, P. Effects of Synbiotics, Probiotics, and Prebiotics on Liver Enzymes of Patients with Non-Alcoholic Fatty Liver Disease: A Systematic Review and Network Meta-Analysis. Front. Nutr. 2022, 9, 880014. [Google Scholar] [CrossRef] [PubMed]
- Hill, C.; Guarner, F.; Reid, G.; Gibson, G.R.; Merenstein, D.J.; Pot, B.; Morelli, L.; Canani, R.B.; Flint, H.J.; Salminen, S.; et al. Expert Consensus Document. The International Scientific Association for Probiotics and Prebiotics Consensus Statement on the Scope and Appropriate Use of the Term Probiotic. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 506–514. [Google Scholar] [CrossRef][Green Version]
- Bamigbade, G.B.; Subhash, A.J.; Kamal-Eldin, A.; Nyström, L.; Ayyash, M. An Updated Review on Prebiotics: Insights on Potentials of Food Seeds Waste as Source of Potential Prebiotics. Molecules 2022, 27, 5947. [Google Scholar] [CrossRef]
- Xing, W.; Gao, W.; Lv, X.; Zhao, Z.; Mao, G.; Dong, X.; Zhang, Z. The Effects of Supplementation of Probiotics, Prebiotics, or Synbiotics on Patients with Non-Alcoholic Fatty Liver Disease: A Meta-Analysis of Randomized Controlled Trials. Front. Nutr. 2022, 9, 1024678. [Google Scholar] [CrossRef]
- Xu, R.; Wan, Y.; Fang, Q.; Lu, W.; Cai, W. Supplementation with Probiotics Modifies Gut Flora and Attenuates Liver Fat Accumulation in Rat Nonalcoholic Fatty Liver Disease Model. J. Clin. Biochem. Nutr. 2011, 50, 72–77. [Google Scholar] [CrossRef][Green Version]
- Esposito, E.; Iacono, A.; Bianco, G.; Autore, G.; Cuzzocrea, S.; Vajro, P.; Canani, R.B.; Calignano, A.; Raso, G.M.; Meli, R. Probiotics Reduce the Inflammatory Response Induced by a High-Fat Diet in the Liver of Young Rats. J. Nutr. 2009, 139, 905–911. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rodríguez-Pastén, A.; Pérez-Hernández, N.; Añorve-Morga, J.; Jiménez-Alvarado, R.; Cariño-Cortés, R.; Sosa-Lozada, T.; Fernández-Martínez, E. The Activity of Prebiotics and Probiotics in Hepatogastrointestinal Disorders and Diseases Associated with Metabolic Syndrome. Int. J. Mol. Sci. 2022, 23, 7229. [Google Scholar] [CrossRef] [PubMed]
- Sugatani, J.; Osabe, M.; Wada, T.; Yamakawa, K.; Yamazaki, Y.; Takahashi, T.; Ikari, A.; Miwa, M. Comparison of Enzymatically Synthesized Inulin, Resistant Maltodextrin and Clofibrate Effects on Biomarkers of Metabolic Disease in Rats Fed a High-Fat and High-Sucrose (Cafeteria) Diet. Eur. J. Nutr. 2008, 47, 192–200. [Google Scholar] [CrossRef]
- Ma, J.; Zhou, Q.; Li, H. Gut Microbiota and Nonalcoholic Fatty Liver Disease: Insights on Mechanisms and Therapy. Nutrients 2017, 9, 1124. [Google Scholar] [CrossRef][Green Version]
- Megur, A.; Daliri, E.B.-M.; Baltriukienė, D.; Burokas, A. Prebiotics as a Tool for the Prevention and Treatment of Obesity and Diabetes: Classification and Ability to Modulate the Gut Microbiota. Int. J. Mol. Sci. 2022, 23, 6097. [Google Scholar] [CrossRef]
- Tsay, C.J.; Lim, J.K. NASH and the Gut Microbiome: Implications for New Therapies. Clin. Liver Dis. 2022, 19, 97–100. [Google Scholar] [CrossRef]
- Mattace Raso, G.; Simeoli, R.; Iacono, A.; Santoro, A.; Amero, P.; Paciello, O.; Russo, R.; D’Agostino, G.; Di Costanzo, M.; Berni Canani, R.; et al. Effects of a Lactobacillus Paracasei B21060 Based Synbiotic on Steatosis, Insulin Signaling and Toll-like Receptor Expression in Rats Fed a High-Fat Diet. J. Nutr. Biochem. 2014, 25, 81–90. [Google Scholar] [CrossRef]
- Nataraj, B.H.; Ali, S.A.; Behare, P.V.; Yadav, H. Postbiotics-Parabiotics: The New Horizons in Microbial Biotherapy and Functional Foods. Microb. Cell Factories 2020, 19, 168. [Google Scholar] [CrossRef]
- Siciliano, R.A.; Reale, A.; Mazzeo, M.F.; Morandi, S.; Silvetti, T.; Brasca, M. Paraprobiotics: A New Perspective for Functional Foods and Nutraceuticals. Nutrients 2021, 13, 1225. [Google Scholar] [CrossRef] [PubMed]
- Arellano-García, L.; Portillo, M.P.; Martínez, J.A.; Milton-Laskibar, I. Usefulness of Probiotics in the Management of NAFLD: Evidence and Involved Mechanisms of Action from Preclinical and Human Models. Int. J. Mol. Sci. 2022, 23, 3167. [Google Scholar] [CrossRef]
- Niazi, M.K.; Hassan, F. Potential Biotics for Nutritional Improvement of Health via Microbiome-Gut-Brain Axis. Adv. Gut Microb. Res. 2022, 2022, e9976555. [Google Scholar] [CrossRef]
- Mejia, C.; Wu, M.; Zhang, Y.; Kajikawa, Y. Exploring Topics in Bibliometric Research Through Citation Networks and Semantic Analysis. Front. Res. Metr. Anal. 2021, 6, 742311. [Google Scholar] [CrossRef]
- Szomszor, M.; Adams, J.; Fry, R.; Gebert, C.; Pendlebury, D.A.; Potter, R.W.K.; Rogers, G. Interpreting Bibliometric Data. Front. Res. Metr. Anal. 2021, 5, 30. [Google Scholar] [CrossRef]
- Trusted Publisher-Independent Citation Database. Web of Science Group. Available online: https://mjl.clarivate.com/home (accessed on 22 March 2023).
- Liao, Y.; Wang, L.; Liu, F.; Zhou, Y.; Lin, X.; Zhao, Z.; Xu, S.; Tang, D.; Jiao, Y.; Yang, L.; et al. Emerging Trends and Hotspots in Metabolic Dysfunction-Associated Fatty Liver Disease (MAFLD) Research from 2012 to 2021: A Bibliometric Analysis. Front. Endocrinol. 2023, 14, 1078149. [Google Scholar] [CrossRef]
- Li, Y.; Zhou, Y.; Wang, L.; Lin, X.; Mao, M.; Yin, S.; Zhu, L.; Jiao, Y.; Yu, W.; Gao, P.; et al. Emerging Trends and Hotspots in the Links between the Gut Microbiota and MAFLD from 2002 to 2021: A Bibliometric Analysis. Front. Endocrinol. 2022, 13, 990953. [Google Scholar] [CrossRef]
- Yang, S.; Yu, D.; Liu, J.; Qiao, Y.; Gu, S.; Yang, R.; Chai, X.; Wang, W. Global Publication Trends and Research Hotspots of the Gut-Liver Axis in NAFLD: A Bibliometric Analysis. Front. Endocrinol. 2023, 14, 1121540. [Google Scholar] [CrossRef]
- Hook, D.W.; Porter, S.J.; Herzog, C. Dimensions: Building Context for Search and Evaluation. Front. Res. Metr. Anal. 2018, 3, 23. [Google Scholar] [CrossRef][Green Version]
- Resources, D.; Adams, J.; Jones, P.; Porter, S.; Szomszor, M.; Draux, H.; Osipov, I. Dimensions—A Collaborative Approach to Enhancing Research Discovery. Digital Sci. 2018. [Google Scholar] [CrossRef]
- Publications—Dimensions. Available online: https://app.dimensions.ai/discover/publication (accessed on 27 March 2023).
- Van Eck, N.; Waltman, L. Software Survey: VOSviewer, a Computer Program for Bibliometric Mapping. Scientometrics 2010, 84, 523–538. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Marchesi, J.R.; Adams, D.H.; Fava, F.; Hermes, G.D.A.; Hirschfield, G.M.; Hold, G.; Quraishi, M.N.; Kinross, J.; Smidt, H.; Tuohy, K.M.; et al. The Gut Microbiota and Host Health: A New Clinical Frontier. Gut 2015, 65, 330. [Google Scholar] [CrossRef][Green Version]
- Boursier, J.; Mueller, O.; Barret, M.; Machado, M.; Fizanne, L.; Araujo-Perez, F.; Guy, C.D.; Seed, P.C.; Rawls, J.F.; David, L.A.; et al. The Severity of Nonalcoholic Fatty Liver Disease Is Associated with Gut Dysbiosis and Shift in the Metabolic Function of the Gut Microbiota. Hepatology 2016, 63, 764–775. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wiest, R.; Garcia-Tsao, G. Bacterial Translocation (BT) in Cirrhosis. Hepatology 2005, 41, 422–433. [Google Scholar] [CrossRef] [PubMed]
- Leung, C.; Rivera, L.; Furness, J.B.; Angus, P.W. The Role of the Gut Microbiota in NAFLD. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 412–425. [Google Scholar] [CrossRef] [PubMed]
- Plaza-Diaz, J.; Ruiz-Ojeda, F.J.; Gil-Campos, M.; Gil, A. Mechanisms of Action of Probiotics. Adv. Nutr. 2019, 10, s49–s66. [Google Scholar] [CrossRef][Green Version]
- Everard, A.; Cani, P.D. Diabetes, Obesity and Gut Microbiota. Best Pract. Res. Clin. Gastroenterol. 2013, 27, 73–83. [Google Scholar] [CrossRef][Green Version]
- Abu-Shanab, A.; Quigley, E.M.M. The Role of the Gut Microbiota in Nonalcoholic Fatty Liver Disease. Nat. Rev. Gastroenterol. Hepatol. 2010, 7, 691–701. [Google Scholar] [CrossRef] [PubMed]
- Festi, D.; Schiumerini, R.; Eusebi, L.H.; Marasco, G.; Taddia, M.; Colecchia, A. Gut Microbiota and Metabolic Syndrome. World J. Gastroenterol. 2014, 20, 16079–16094. [Google Scholar] [CrossRef]
- Tilg, H.; Cani, P.D.; Mayer, E.A. Gut Microbiome and Liver Diseases. Gut 2016, 65, 2035. [Google Scholar] [CrossRef]
- Bajaj, J.S. Alcohol, Liver Disease and the Gut Microbiota. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 235–246. [Google Scholar] [CrossRef]
- Jie, Z.; Xia, H.; Zhong, S.-L.; Feng, Q.; Li, S.; Liang, S.; Zhong, H.; Liu, Z.; Gao, Y.; Zhao, H.; et al. The Gut Microbiome in Atherosclerotic Cardiovascular Disease. Nat. Commun. 2017, 8, 845. [Google Scholar] [CrossRef][Green Version]
- Li, Z.; Yang, S.; Lin, H.; Huang, J.; Watkins, P.A.; Moser, A.B.; DeSimone, C.; Song, X.; Diehl, A.M. Probiotics and Antibodies to TNF Inhibit Inflammatory Activity and Improve Nonalcoholic Fatty Liver Disease. Hepatology 2003, 37, 343–350. [Google Scholar] [CrossRef]
- Mouzaki, M.; Comelli, E.M.; Arendt, B.M.; Bonengel, J.; Fung, S.K.; Fischer, S.E.; McGilvray, I.D.; Allard, J.P. Intestinal Microbiota in Patients with Nonalcoholic Fatty Liver Disease. Hepatology 2013, 58, 120–127. [Google Scholar] [CrossRef][Green Version]
- Kakiyama, G.; Pandak, W.M.; Gillevet, P.M.; Hylemon, P.B.; Heuman, D.M.; Daita, K.; Takei, H.; Muto, A.; Nittono, H.; Ridlon, J.M.; et al. Modulation of the Fecal Bile Acid Profile by Gut Microbiota in Cirrhosis. J. Hepatol. 2013, 58, 949–955. [Google Scholar] [CrossRef][Green Version]
- Raman, M.; Ahmed, I.; Gillevet, P.M.; Probert, C.S.; Ratcliffe, N.M.; Smith, S.; Greenwood, R.; Sikaroodi, M.; Lam, V.; Crotty, P.; et al. Fecal Microbiome and Volatile Organic Compound Metabolome in Obese Humans with Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2013, 11, 868–875.e1-3. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Duan, Z.P.; Ha, D.K.; Bengmark, S.; Kurtovic, J.; Riordan, S.M. Synbiotic Modulation of Gut Flora: Effect on Minimal Hepatic Encephalopathy in Patients with Cirrhosis. Hepatology 2004, 39, 1441–1449. [Google Scholar] [CrossRef]
- Del Chierico, F.; Nobili, V.; Vernocchi, P.; Russo, A.; De Stefanis, C.; Gnani, D.; Furlanello, C.; Zandonà, A.; Paci, P.; Capuani, G.; et al. Gut Microbiota Profiling of Pediatric Nonalcoholic Fatty Liver Disease and Obese Patients Unveiled by an Integrated Meta-omics-based Approach. Hepatology 2017, 65, 451–464. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bajaj, J.S.; Hylemon, P.B.; Ridlon, J.M.; Heuman, D.M.; Daita, K.; White, M.B.; Monteith, P.; Noble, N.A.; Sikaroodi, M.; Gillevet, P.M. Colonic Mucosal Microbiome Differs from Stool Microbiome in Cirrhosis and Hepatic Encephalopathy and Is Linked to Cognition and Inflammation. AJP Gastroint. Liver Physiol. 2012, 303, g675–g685. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Wu, N.; Wang, X.; Chi, Y.; Zhang, Y.; Qiu, X.; Hu, Y.; Li, J.; Liu, Y. Dysbiosis Gut Microbiota Associated with Inflammation and Impaired Mucosal Immune Function in Intestine of Humans with Non-Alcoholic Fatty Liver Disease. Sci. Rep. 2015, 5, 8096. [Google Scholar] [CrossRef][Green Version]
- Zhu, L.; Baker, S.S.; Gill, C.; Liu, W.; Alkhouri, R.; Baker, R.D.; Gill, S.R. Characterization of Gut Microbiomes in Nonalcoholic Steatohepatitis (NASH) Patients: A Connection between Endogenous Alcohol and NASH. Hepatology 2013, 57, 601–609. [Google Scholar] [CrossRef]
- Turnbaugh, P.J.; Ley, R.E.; Mahowald, M.A.; Magrini, V.; Mardis, E.R.; Gordon, J.I. An Obesity-Associated Gut Microbiome with Increased Capacity for Energy Harvest. Nature 2006, 444, 1027–1031. [Google Scholar] [CrossRef]
- Godoy-Matos, A.F.; Silva Júnior, W.S.; Valerio, C.M. NAFLD as a Continuum: From Obesity to Metabolic Syndrome and Diabetes. Diabetol. Metab. Syndr. 2020, 12, 60. [Google Scholar] [CrossRef] [PubMed]
- da Cruz, N.S.; Pasquarelli-do-Nascimento, G.; Oliveira, A.C.P.E.; Magalhães, K.G. Inflammasome-Mediated Cytokines: A Key Connection between Obesity-Associated NASH and Liver Cancer Progression. Biomedicines 2022, 10, 2344. [Google Scholar] [CrossRef] [PubMed]
- Miele, L.; Valenza, V.; La Torre, G.; Montalto, M.; Cammarota, G.; Ricci, R.; Mascianà, R.; Forgione, A.; Gabrieli, M.L.; Perotti, G.; et al. Increased Intestinal Permeability and Tight Junction Alterations in Nonalcoholic Fatty Liver Disease. Hepatology 2009, 49, 1877–1887. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, J.S.; Heuman, D.M.; Hylemon, P.B.; Sanyal, A.J.; White, M.B.; Monteith, P.; Noble, N.A.; Unser, A.B.; Daita, K.; Fisher, A.R.; et al. Altered Profile of Human Gut Microbiome Is Associated with Cirrhosis and Its Complications. J. Hepatol. 2014, 60, 940–947. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bäckhed, F.; Ding, H.; Wang, T.; Hooper, L.V.; Koh, G.Y.; Nagy, A.; Semenkovich, C.F.; Gordon, J.I. The Gut Microbiota as an Environmental Factor That Regulates Fat Storage. Proc. Natl. Acad. Sci. USA 2004, 101, 15718–15723. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, Y.; Yang, F.; Lu, H.; Wang, B.; Chen, Y.; Lei, D.; Wang, Y.; Zhu, B.; Li, L. Characterization of Fecal Microbial Communities in Patients with Liver Cirrhosis. Hepatology 2011, 54, 562–572. [Google Scholar] [CrossRef]
- Cani, P.D.; Amar, J.; Iglesias, M.A.; Poggi, M.; Knauf, C.; Bastelica, D.; Neyrinck, A.M.; Fava, F.; Tuohy, K.M.; Chabo, C.; et al. Metabolic Endotoxemia Initiates Obesity and Insulin Resistance. Diabetes 2007, 56, 1761–1772. [Google Scholar] [CrossRef][Green Version]
- Qin, N.; Yang, F.; Li, A.; Prifti, E.; Chen, Y.; Shao, L.; Guo, J.; Le Chatelier, E.; Yao, J.; Wu, L.; et al. Alterations of the Human Gut Microbiome in Liver Cirrhosis. Nature 2014, 513, 59–64. [Google Scholar] [CrossRef]
- Kastl, A.J.; Terry, N.A.; Wu, G.D.; Albenberg, L.G. The Structure and Function of the Human Small Intestinal Microbiota: Current Understanding and Future Directions. Cell. Mol. Gastroenterol. Hepatol. 2020, 9, 33–45. [Google Scholar] [CrossRef][Green Version]
- Guo, L.; Yang, K.; Zhou, P.; Yong, W. Gut Microbiota in Obesity and Nonalcoholic Fatty Liver Disease. Surg. Pract. Sci. 2021, 5, 100030. [Google Scholar] [CrossRef]
- Pouwels, S.; Sakran, N.; Graham, Y.; Leal, A.; Pintar, T.; Yang, W.; Kassir, R.; Singhal, R.; Mahawar, K.; Ramnarain, D. Non-Alcoholic Fatty Liver Disease (NAFLD): A Review of Pathophysiology, Clinical Management and Effects of Weight Loss. BMC Endocr. Disord. 2022, 22, 63. [Google Scholar] [CrossRef]
- Muscogiuri, G.; Cantone, E.; Cassarano, S.; Tuccinardi, D.; Barrea, L.; Savastano, S.; Colao, A. Gut Microbiota: A New Path to Treat Obesity. Int. J. Obes. Suppl. 2019, 9, 10–19. [Google Scholar] [CrossRef]
- Divella, R.; Mazzocca, A.; Daniele, A.; Sabbà, C.; Paradiso, A. Obesity, Nonalcoholic Fatty Liver Disease and Adipocytokines Network in Promotion of Cancer. Int. J. Biol. Sci. 2019, 15, 610–616. [Google Scholar] [CrossRef][Green Version]
- Magne, F.; Gotteland, M.; Gauthier, L.; Zazueta, A.; Pesoa, S.; Navarrete, P.; Balamurugan, R. The Firmicutes/Bacteroidetes Ratio: A Relevant Marker of Gut Dysbiosis in Obese Patients? Nutrients 2020, 12, 1474. [Google Scholar] [CrossRef]
- Wang, B.; Jiang, X.; Cao, M.; Ge, J.; Bao, Q.; Tang, L.; Chen, Y.; Li, L. Altered Fecal Microbiota Correlates with Liver Biochemistry in Nonobese Patients with Non-Alcoholic Fatty Liver Disease. Sci. Rep. 2016, 6, 32002. [Google Scholar] [CrossRef]
- Gensthaler, L.; Felsenreich, D.M.; Jedamzik, J.; Eichelter, J.; Nixdorf, L.; Bichler, C.; Krebs, M.; Itariu, B.; Langer, F.B.; Prager, G. Trends of Overweight and Obesity in Male Adolescents: Prevalence, Socioeconomic Status, and Impact on Cardiovascular Risk in a Central European Country. Obes. Surg. 2022, 32, 1024–1033. [Google Scholar] [CrossRef]
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. PharmacoEconomics 2015, 33, 673–689. [Google Scholar] [CrossRef]
- Lin, X.; Li, H. Obesity: Epidemiology, Pathophysiology, and Therapeutics. Front. Endocrinol. 2021, 12, 706978. [Google Scholar] [CrossRef]
- Park, J.H.; Moon, J.H.; Kim, H.J.; Kong, M.H.; Oh, Y.H. Sedentary Lifestyle: Overview of Updated Evidence of Potential Health Risks. Korean J. Fam. Med. 2020, 41, 365–373. [Google Scholar] [CrossRef]
- Cunningham, M.; Azcarate-Peril, M.A.; Barnard, A.; Benoit, V.; Grimaldi, R.; Guyonnet, D.; Holscher, H.D.; Hunter, K.; Manurung, S.; Obis, D.; et al. Shaping the Future of Probiotics and Prebiotics. Trends Microbiol. 2021, 29, 667–685. [Google Scholar] [CrossRef]
- Selvamani, S.; Mehta, V.; Ali El Enshasy, H.; Thevarajoo, S.; El Adawi, H.; Zeini, I.; Pham, K.; Varzakas, T.; Abomoelak, B. Efficacy of Probiotics-Based Interventions as Therapy for Inflammatory Bowel Disease: A Recent Update. Saudi J. Biol. Sci. 2022, 29, 3546–3567. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Niu, Z.; Zou, M.; Liu, S.; Wang, M.; Gu, X.; Lu, H.; Tian, H.; Jha, R. Probiotics, Prebiotics, and Synbiotics Regulate the Intestinal Microbiota Differentially and Restore the Relative Abundance of Specific Gut Microorganisms. J. Dairy Sci. 2020, 103, 5816–5829. [Google Scholar] [CrossRef] [PubMed]
- Castillo, V.; Figueroa, F.; González-Pizarro, K.; Jopia, P.; Ibacache-Quiroga, C. Probiotics and Prebiotics as a Strategy for Non-Alcoholic Fatty Liver Disease, a Narrative Review. Foods 2021, 10, 1719. [Google Scholar] [CrossRef] [PubMed]
- Sangouni, A.A.; Ghavamzadeh, S. A Review of Synbiotic Efficacy in Non-Alcoholic Fatty Liver Disease as a Therapeutic Approach. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2917–2922. [Google Scholar] [CrossRef]
- Eslamparast, T.; Poustchi, H.; Zamani, F.; Sharafkhah, M.; Malekzadeh, R.; Hekmatdoost, A. Synbiotic Supplementation in Nonalcoholic Fatty Liver Disease: A Randomized, Double-Blind, Placebo-Controlled Pilot Study. Am. J. Clin. Nutr. 2014, 99, 535–542. [Google Scholar] [CrossRef][Green Version]
- Nova, E.; Gómez-Martinez, S.; González-Soltero, R. The Influence of Dietary Factors on the Gut Microbiota. Microorganisms 2022, 10, 1368. [Google Scholar] [CrossRef]
- Tokuhara, D. Role of the Gut Microbiota in Regulating Non-Alcoholic Fatty Liver Disease in Children and Adolescents. Front. Nutr. 2021, 8, 700058. [Google Scholar] [CrossRef]
- Fukui, H. Role of Gut Dysbiosis in Liver Diseases: What Have We Learned So Far? Diseases 2019, 7, 58. [Google Scholar] [CrossRef][Green Version]
- Tsai, M.-C.; Liu, Y.-Y.; Lin, C.-C.; Wang, C.-C.; Wu, Y.-J.; Yong, C.-C.; Chen, K.-D.; Chuah, S.-K.; Yao, C.-C.; Huang, P.-Y.; et al. Gut Microbiota Dysbiosis in Patients with Biopsy-Proven Nonalcoholic Fatty Liver Disease: A Cross-Sectional Study in Taiwan. Nutrients 2020, 12, 820. [Google Scholar] [CrossRef][Green Version]
- Hydes, T.J.; Ravi, S.; Loomba, R.; Gray, M.E. Evidence-Based Clinical Advice for Nutrition and Dietary Weight Loss Strategies for the Management of NAFLD and NASH. Clin. Mol. Hepatol. 2020, 26, 383–400. [Google Scholar] [CrossRef]
- van den Hoek, A.M.; de Jong, J.C.B.C.; Worms, N.; van Nieuwkoop, A.; Voskuilen, M.; Menke, A.L.; Lek, S.; Caspers, M.P.M.; Verschuren, L.; Kleemann, R. Diet and Exercise Reduce Pre-Existing NASH and Fibrosis and Have Additional Beneficial Effects on the Vasculature, Adipose Tissue and Skeletal Muscle via Organ-Crosstalk. Metabolism 2021, 124, 154873. [Google Scholar] [CrossRef]
- Plaza-Díaz, J.; Solis-Urra, P.; Aragón-Vela, J.; Rodríguez-Rodríguez, F.; Olivares-Arancibia, J.; Álvarez-Mercado, A.I. Insights into the Impact of Microbiota in the Treatment of NAFLD/NASH and Its Potential as a Biomarker for Prognosis and Diagnosis. Biomedicines 2021, 9, 145. [Google Scholar] [CrossRef]
- Luci, C.; Bourinet, M.; Leclère, P.S.; Anty, R.; Gual, P. Chronic Inflammation in Non-Alcoholic Steatohepatitis: Molecular Mechanisms and Therapeutic Strategies. Front. Endocrinol. 2020, 11, 597648. [Google Scholar] [CrossRef]
- Yu, J.; Zhu, C.; Wang, X.; Kim, K.; Bartolome, A.; Dongiovanni, P.; Yates, K.P.; Valenti, L.; Carrer, M.; Sadowski, T.; et al. Hepatocyte TLR4 Triggers Inter-Hepatocyte Jagged1/Notch Signaling to Determine NASH-Induced Fibrosis. Sci. Transl. Med. 2021, 13, eabe1692. [Google Scholar] [CrossRef] [PubMed]
- Miura, K.; Ishioka, M.; Minami, S.; Horie, Y.; Ohshima, S.; Goto, T.; Ohnishi, H. Toll-like Receptor 4 on Macrophage Promotes the Development of Steatohepatitis-Related Hepatocellular Carcinoma in Mice. J. Biol. Chem. 2016, 291, 11504–11517. [Google Scholar] [CrossRef][Green Version]
- Miura, K.; Kodama, Y.; Inokuchi, S.; Schnabl, B.; Aoyama, T.; Ohnishi, H.; Olefsky, J.M.; Brenner, D.A.; Seki, E. Toll-Like Receptor 9 Promotes Steatohepatitis by Induction of Interleukin-1β in Mice. Gastroenterology 2010, 139, 323–334.e7. [Google Scholar] [CrossRef][Green Version]
- Villena, J.; Kitazawa, H. Modulation of Intestinal TLR4-Inflammatory Signaling Pathways by Probiotic Microorganisms: Lessons Learned from Lactobacillus Jensenii TL2937. Front. Immunol. 2014, 4, 512. [Google Scholar] [CrossRef][Green Version]
- Park, E.-J.; Lee, Y.-S.; Kim, S.M.; Park, G.-S.; Lee, Y.H.; Jeong, D.Y.; Kang, J.; Lee, H.-J. Beneficial Effects of Lactobacillus Plantarum Strains on Non-Alcoholic Fatty Liver Disease in High Fat/High Fructose Diet-Fed Rats. Nutrients 2020, 12, 542. [Google Scholar] [CrossRef][Green Version]
- Okubo, H.; Sakoda, H.; Kushiyama, A.; Fujishiro, M.; Nakatsu, Y.; Fukushima, T.; Matsunaga, Y.; Kamata, H.; Asahara, T.; Yoshida, Y.; et al. Lactobacillus Casei Strain Shirota Protects against Nonalcoholic Steatohepatitis Development in a Rodent Model. Am. J. Physiol.-Gastroint. Liver Physiol. 2013, 305, G911–G918. [Google Scholar] [CrossRef]
- Marsano, L.S.; Mendez, C.; Hill, D.; Barve, S.; Mcclain, C.J. Diagnosis and Treatment of Alcoholic Liver Disease and Its Complications. Alcohol Res. Health 2003, 27, 247–256. [Google Scholar]
- Bajaj, J.S. The Role of Microbiota in Hepatic Encephalopathy. Gut Microbes 2014, 5, 397–403. [Google Scholar] [CrossRef][Green Version]
- Luo, M.; Xin, R.-J.; Hu, F.-R.; Yao, L.; Hu, S.-J.; Bai, F.-H. Role of Gut Microbiota in the Pathogenesis and Therapeutics of Minimal Hepatic Encephalopathy via the Gut-Liver-Brain Axis. World J. Gastroenterol. 2023, 29, 144–156. [Google Scholar] [CrossRef]
- Woo, P.C.Y.; Lau, S.K.P.; Teng, J.L.L.; Tse, H.; Yuen, K.-Y. Then and Now: Use of 16S RDNA Gene Sequencing for Bacterial Identification and Discovery of Novel Bacteria in Clinical Microbiology Laboratories. Clin. Microbiol. Infect. 2008, 14, 908–934. [Google Scholar] [CrossRef][Green Version]
- Almonacid, D.E.; Kraal, L.; Ossandon, F.J.; Budovskaya, Y.V.; Cardenas, J.P.; Bik, E.M.; Goddard, A.D.; Richman, J.; Apte, Z.S. 16S RRNA Gene Sequencing and Healthy Reference Ranges for 28 Clinically Relevant Microbial Taxa from the Human Gut Microbiome. PLoS ONE 2017, 12, e0176555. [Google Scholar] [CrossRef][Green Version]
- Xu, Y.; Xie, Z.; Wang, H.; Shen, Z.; Guo, Y.; Gao, Y.; Chen, X.; Wu, Q.; Li, X.; Wang, K. Bacterial Diversity of Intestinal Microbiota in Patients with Substance Use Disorders Revealed by 16S RRNA Gene Deep Sequencing. Sci. Rep. 2017, 7, 3628. [Google Scholar] [CrossRef][Green Version]
- Cheng, D.; Xie, M.Z. A Review of a Potential and Promising Probiotic Candidate-Akkermansia Muciniphila. J. Appl. Microbiol. 2021, 130, 1813–1822. [Google Scholar] [CrossRef]
- Zhang, T.; Li, Q.; Cheng, L.; Buch, H.; Zhang, F. Akkermansia Muciniphila Is a Promising Probiotic. Microb. Biotechnol. 2019, 12, 1109–1125. [Google Scholar] [CrossRef][Green Version]
- Deng, L.; Ou, Z.; Huang, D.; Li, C.; Lu, Z.; Liu, W.; Wu, F.; Nong, C.; Gao, J.; Peng, Y. Diverse Effects of Different Akkermansia Muciniphila Genotypes on Brown Adipose Tissue Inflammation and Whitening in a High-Fat-Diet Murine Model. Microb. Pathogen. 2020, 147, 104353. [Google Scholar] [CrossRef]
- Depommier, C.; Everard, A.; Druart, C.; Plovier, H.; Van Hul, M.; Vieira-Silva, S.; Falony, G.; Raes, J.; Maiter, D.; Delzenne, N.M.; et al. Supplementation with Akkermansia Muciniphila in Overweight and Obese Human Volunteers: A Proof-of-Concept Exploratory Study. Nat. Med. 2019, 25, 1096–1103. [Google Scholar] [CrossRef]
- Plovier, H.; Everard, A.; Druart, C.; Depommier, C.; Van Hul, M.; Geurts, L.; Chilloux, J.; Ottman, N.; Duparc, T.; Lichtenstein, L.; et al. A Purified Membrane Protein from Akkermansia Muciniphila or the Pasteurized Bacterium Improves Metabolism in Obese and Diabetic Mice. Nat. Med. 2017, 23, 107–113. [Google Scholar] [CrossRef][Green Version]
- Baxter, N.T.; Schmidt, A.W.; Venkataraman, A.; Kim, K.S.; Waldron, C.; Schmidt, T.M. Dynamics of Human Gut Microbiota and Short-Chain Fatty Acids in Response to Dietary Interventions with Three Fermentable Fibers. mBio 2019, 10, e02566-18. [Google Scholar] [CrossRef][Green Version]
- Ríos-Covián, D.; Ruas-Madiedo, P.; Margolles, A.; Gueimonde, M.; de los Reyes-Gavilán, C.G.; Salazar, N. Intestinal Short Chain Fatty Acids and Their Link with Diet and Human Health. Front. Microbiol. 2016, 7, 185. [Google Scholar] [CrossRef][Green Version]
- Schönfeld, P.; Wojtczak, L. Short- and Medium-Chain Fatty Acids in Energy Metabolism: The Cellular Perspective. J. Lipid Res. 2016, 57, 943–954. [Google Scholar] [CrossRef][Green Version]
- Gao, F.; Lv, Y.-W.; Long, J.; Chen, J.-M.; He, J.; Ruan, X.-Z.; Zhu, H. Butyrate Improves the Metabolic Disorder and Gut Microbiome Dysbiosis in Mice Induced by a High-Fat Diet. Front. Pharmacol. 2019, 10, 1040. [Google Scholar] [CrossRef][Green Version]
- Rau, M.; Rehman, A.; Dittrich, M.; Groen, A.K.; Hermanns, H.M.; Seyfried, F.; Beyersdorf, N.; Dandekar, T.; Rosenstiel, P.; Geier, A. Fecal SCFAs and SCFA-Producing Bacteria in Gut Microbiome of Human NAFLD as a Putative Link to Systemic T-Cell Activation and Advanced Disease. United Eur. Gastroenterol. J. 2018, 6, 1496–1507. [Google Scholar] [CrossRef]
- Zhou, D.; Fan, J.-G. Microbial Metabolites in Non-Alcoholic Fatty Liver Disease. World J. Gastroenterol. 2019, 25, 2019–2028. [Google Scholar] [CrossRef]
- de Groot, P.F.; Frissen, M.N.; de Clercq, N.C.; Nieuwdorp, M. Fecal Microbiota Transplantation in Metabolic Syndrome: History, Present and Future. Gut Microbes 2017, 8, 253–267. [Google Scholar] [CrossRef][Green Version]
- Vaughn, B.P.; Rank, K.M.; Khoruts, A. Fecal Microbiota Transplantation: Current Status in Treatment of GI and Liver Disease. Clin. Gastroenterol. Hepatol. 2019, 17, 353–361. [Google Scholar] [CrossRef]
- Bloom, P.P.; Tapper, E.B.; Young, V.B.; Lok, A.S. Microbiome Therapeutics for Hepatic Encephalopathy. J. Hepatol. 2021, 75, 1452–1464. [Google Scholar] [CrossRef]
- Wang, L.; Cao, Z.-M.; Zhang, L.-L.; Li, J.; Lv, W. The Role of Gut Microbiota in Some Liver Diseases: From an Immunological Perspective. Front. Immunol. 2022, 13, 923599. [Google Scholar] [CrossRef]
- Abenavoli, L.; Maurizi, V.; Rinninella, E.; Tack, J.; Di Berardino, A.; Santori, P.; Rasetti, C.; Procopio, A.C.; Boccuto, L.; Scarpellini, E. Fecal Microbiota Transplantation in NAFLD Treatment. Medicina 2022, 58, 1559. [Google Scholar] [CrossRef] [PubMed]
- Witjes, J.J.; Smits, L.P.; Pekmez, C.T.; Prodan, A.; Meijnikman, A.S.; Troelstra, M.A.; Bouter, K.E.C.; Herrema, H.; Levin, E.; Holleboom, A.G.; et al. Donor Fecal Microbiota Transplantation Alters Gut Microbiota and Metabolites in Obese Individuals with Steatohepatitis. Hepatol. Commun. 2020, 4, 1578–1590. [Google Scholar] [CrossRef] [PubMed]










| Name | Organization, Country | Publications | Citations | Citations (Mean) |
|---|---|---|---|---|
| Jasmohan Singh Bajaj | Virginia Commonwealth University, United States | 25 | 2375 | 95 |
| Patrick Martin Gillevet | George Mason University, United States | 15 | 1932 | 128.8 |
| Masoumeh Sikaroodi | George Mason University, United States | 15 | 1932 | 128.8 |
| Ki Tae Suk | Hallym University, Republic of Korea | 12 | 260 | 21.67 |
| Lanjuan Li | Zhejiang University, China | 12 | 635 | 52.92 |
| Andrew C. Fagan | Virginia Commonwealth University, United States | 11 | 153 | 13.91 |
| Nathalie Maria Delzenne | Université Catholique de Louvain, Belgium | 11 | 702 | 63.82 |
| Bernd G. Schnabl | University of California, San Diego, United States | 10 | 385 | 38.5 |
| Michael Fuchs | Virginia Commonwealth University, United States | 10 | 877 | 87.7 |
| Ludovico Montebianco Abenavoli | Magna Graecia University, Italy | 9 | 332 | 36.89 |
| Phillip B. Hylemon | Virginia Commonwealth University, United States | 8 | 1347 | 168.38 |
| María Victoria García-Mediavilla | Centro de Investigación Biomédica en Red de Enfermedades Hepáticas y Digestivas, Spain | 8 | 462 | 57.75 |
| Carlos Guarner | Hospital de Sant Pau, Spain | 8 | 711 | 88.88 |
| Hitoshi Yoshiji | Nara Medical University, Japan | 8 | 290 | 36.25 |
| Esther Nistal | University of Leon, Spain | 8 | 462 | 57.75 |
| Hideto Kawaratani | Nara Medical University, Japan | 8 | 291 | 36.38 |
| Antonio Gasbarrini | Catholic University of the Sacred Heart, Italy | 8 | 534 | 66.75 |
| Lorenza Putignani | Bambino Gesù Children’s Hospital, Italy | 8 | 896 | 112 |
| Hiroshi Fukui | Nara Medical University, Japan | 8 | 513 | 64.13 |
| Sonia Sánchez-Campos | Centro de Investigación Biomédica en Red de Enfermedades Hepáticas y Digestivas, Spain | 8 | 462 | 57.75 |
| Journal | Documents | Journal | Citations |
|---|---|---|---|
| Nutrients | 33 | Hepatology | 4552 |
| International Journal of Molecular Sciences | 29 | Journal of Hepatology | 2348 |
| World Journal of Gastroenterology | 27 | World Journal of Gastroenterology | 2279 |
| Frontiers in Microbiology | 20 | Gut | 2002 |
| Food & Function | 20 | Scientific Reports | 1437 |
| Journal of Hepatology | 20 | Gastroenterology | 1178 |
| Scientific Reports | 18 | Alimentary Pharmacology & Therapeutics | 894 |
| Gut Microbes | 17 | Nutrients | 799 |
| Hepatology | 15 | AJP Gastrointestinal and Liver Physiology | 756 |
| Liver International | 15 | PLoS ONE | 755 |
| The Journal of Nutritional Biochemistry | 13 | Frontiers in Microbiology | 728 |
| World Journal of Hepatology | 12 | International Journal of Molecular Sciences | 723 |
| Molecular Nutrition & Food Research | 12 | The Journal of Nutritional Biochemistry | 683 |
| Gastroenterology | 12 | Clinical Gastroenterology and Hepatology | 667 |
| Frontiers in Cellular and Infection Microbiology | 11 | Liver International | 599 |
| PLoS ONE | 10 | Journal of Clinical Gastroenterology | 598 |
| Frontiers in Nutrition | 10 | Food & Function | 530 |
| Alimentary Pharmacology & Therapeutics | 10 | Molecular Nutrition & Food Research | 454 |
| AJP Gastrointestinal and Liver Physiology | 10 | Digestive Diseases and Sciences | 450 |
| Biomedicine & Pharmacotherapy | 10 | Gut Microbes | 439 |
| Reviews | |||||
| Title | Source Title | PubYear | Authors | Times Cited | Ref |
| The gut microbiota and host health: a new clinical frontier | Gut | 2015 | Marchesi, Julian R | 1436 | [42] |
| Bacterial translocation (BT) in cirrhosis | Hepatology | 2005 | Wiest, Reiner | 569 | [44] |
| The role of the gut microbiota in NAFLD | Nature Reviews Gastroenterology & Hepatology | 2016 | Leung, Christopher | 561 | [45] |
| The gut-liver axis in liver disease: pathophysiological basis for therapy | Journal of Hepatology | 2019 | Albillos, Agustín | 546 | [12] |
| Mechanisms of action of probiotics | Advances in Nutrition | 2019 | Plaza-Diaz, Julio | 446 | [46] |
| Diabetes, obesity and gut microbiota | Best Practice & Research Clinical Gastroenterology | 2013 | Everard, Amandine | 421 | [47] |
| The role of the gut microbiota in nonalcoholic fatty liver disease | Nature Reviews Gastroenterology & Hepatology | 2010 | Abu-Shanab, Ahmed | 377 | [48] |
| Gut microbiota and metabolic syndrome | World Journal of Gastroenterology, | 2014 | Festi, Davide | 349 | [49] |
| Gut microbiome and liver diseases | Gut | 2016 | Tilg, Herbert | 322 | [50] |
| Alcohol, liver disease and the gut microbiota | Nature Reviews Gastroenterology & Hepatology | 2019 | Bajaj, Jasmohan S | 299 | [51] |
| Original articles | |||||
| Title | Source Title | PubYear | Authors | Times Cited | Ref |
| The severity of nonalcoholic fatty liver disease is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota | Hepatology | 2016 | Boursier, Jérôme | 807 | [43] |
| The gut microbiome in atherosclerotic cardiovascular disease | Nature Communications | 2017 | Jie, Zhuye | 784 | [52] |
| Probiotics and antibodies to TNF inhibit inflammatory activity and improve nonalcoholic fatty liver disease | Hepatology | 2003 | Li, Zhiping | 747 | [53] |
| Intestinal microbiota in patients with nonalcoholic fatty liver disease | Hepatology | 2013 | Mouzaki, Marialena | 540 | [54] |
| Modulation of the fecal bile acid profile by gut microbiota in cirrhosis | Journal of Hepatology | 2013 | Kakiyama, Genta Ridlon | 530 | [55] |
| Fecal microbiome and volatile organic compound metabolome in obese humans with nonalcoholic fatty liver disease | Clinical Gastroenterology and Hepatology | 2013 | Raman, Maitreyi | 495 | [56] |
| Synbiotic modulation of gut flora: Effect on minimal hepatic encephalopathy in patients with cirrhosis | Hepatology | 2004 | Liu, Qing | 493 | [57] |
| Gut microbiota profiling of pediatric nonalcoholic fatty liver disease and obese patients unveiled by an integrated meta-omics-based approach | Hepatology | 2016 | Del Chierico, Federica | 424 | [58] |
| Colonic mucosal microbiome differs from stool microbiome in cirrhosis and hepatic encephalopathy and is linked to cognition and inflammation | AJP Gastrointestinal and Liver Physiology | 2012 | Bajaj, Jasmohan S | 397 | [59] |
| Dysbiosis gut microbiota associated with inflammation and impaired mucosal immune function in intestine of humans with non-alcoholic fatty liver disease | Scientific Reports | 2015 | Jiang, Weiwei | 387 | [60] |
| Title | First Author | Citations | Journal | Year | Ref |
|---|---|---|---|---|---|
| Characterization of gut microbiomes in nonalcoholic steatohepatitis (NASH) patients: a connection between endogenous alcohol and NASH | Zou, L. | 207 | Hepatology | 2013 | [61] |
| An obesity-associated gut microbiome with increased capacity for energy harvest | Turnbaugh, P.J. | 143 | Nature | 2006 | [62] |
| The severity of nonalcoholic fatty liver disease is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota | Boursier, J. | 135 | Hepatology | 2016 | [43] |
| Increased intestinal permeability and tight junction alterations in nonalcoholic fatty liver disease | Miele, L. | 129 | Hepatology | 2009 | [65] |
| Altered profile of human gut microbiome is associated with cirrhosis and its complications | Bajaj, J.S. | 115 | Journal of Hepatology | 2013 | [66] |
| The gut microbiota as an environmental factor that regulates fat storage | Bäckhed, F. | 113 | PNAS USA | 2004 | [67] |
| Characterization of fecal microbial communities in patients with liver cirrhosis | Chen, Y. | 110 | Hepatology | 2011 | [68] |
| Metabolic endotoxemia initiates obesity and insulin resistance | Cani, P.D. | 109 | Diabetes | 2007 | [69] |
| Alterations of the human gut microbiome in liver cirrhosis | Qin, N. | 108 | Nature | 2014 | [70] |
| Intestinal microbiota in patients with nonalcoholic fatty liver disease | Mouzaki, M. | 100 | Hepatology | 2013 | [54] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pezzino, S.; Sofia, M.; Mazzone, C.; Castorina, S.; Puleo, S.; Barchitta, M.; Agodi, A.; Gallo, L.; La Greca, G.; Latteri, S. Gut Microbiome in the Progression of NAFLD, NASH and Cirrhosis, and Its Connection with Biotics: A Bibliometric Study Using Dimensions Scientific Research Database. Biology 2023, 12, 662. https://doi.org/10.3390/biology12050662
Pezzino S, Sofia M, Mazzone C, Castorina S, Puleo S, Barchitta M, Agodi A, Gallo L, La Greca G, Latteri S. Gut Microbiome in the Progression of NAFLD, NASH and Cirrhosis, and Its Connection with Biotics: A Bibliometric Study Using Dimensions Scientific Research Database. Biology. 2023; 12(5):662. https://doi.org/10.3390/biology12050662
Chicago/Turabian StylePezzino, Salvatore, Maria Sofia, Chiara Mazzone, Sergio Castorina, Stefano Puleo, Martina Barchitta, Antonella Agodi, Luisa Gallo, Gaetano La Greca, and Saverio Latteri. 2023. "Gut Microbiome in the Progression of NAFLD, NASH and Cirrhosis, and Its Connection with Biotics: A Bibliometric Study Using Dimensions Scientific Research Database" Biology 12, no. 5: 662. https://doi.org/10.3390/biology12050662
APA StylePezzino, S., Sofia, M., Mazzone, C., Castorina, S., Puleo, S., Barchitta, M., Agodi, A., Gallo, L., La Greca, G., & Latteri, S. (2023). Gut Microbiome in the Progression of NAFLD, NASH and Cirrhosis, and Its Connection with Biotics: A Bibliometric Study Using Dimensions Scientific Research Database. Biology, 12(5), 662. https://doi.org/10.3390/biology12050662