Cholestatic Pruritus in Children: Conventional Therapies and Beyond
Abstract
:Simple Summary
Abstract
1. Introduction
2. Itch Pathogenesis
3. Management of Cholestatic Pruritus in Children
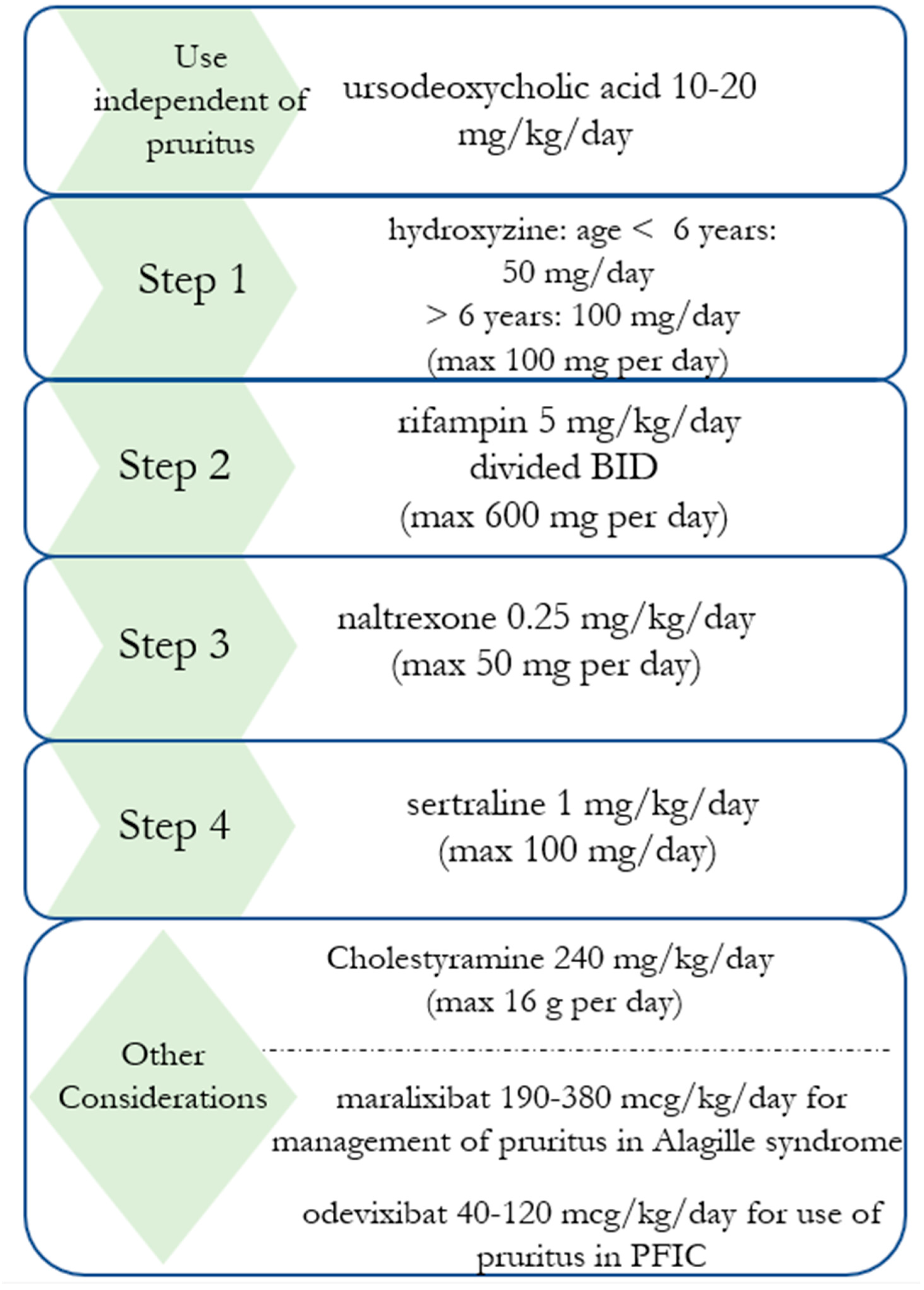
3.1. Ursodeoxycholic Acid
3.2. Bile Acid Binding Resins
3.3. Antihistamines
3.4. Rifampin
3.5. Opioid Antagonists
3.6. Selective Serotonin Reuptake Inhibitors
3.7. Ileal Bile Acid Transport (IBAT) Inhibitors
3.8. Surgical Management
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Khalaf, R.; Phen, C.; Karjoo, S.; Wilsey, M. Cholestasis beyond the Neonatal and Infancy Periods. Pediatr. Gastroenterol. Hepatol. Nutr. 2016, 19, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Bergasa, N.; Schiff, E. The Management of Chronic Pruritus of Cholestasis. Adv. Hepatol. 2009, 5, 550–552. [Google Scholar]
- Thébaut, A.; Habes, D.; Gottrand, F.; Rivet, C.; Cohen, J.; Debray, D.; Jacquemin, E.; Gonzales, E. Sertraline as an Additional Treatment for Cholestatic Pruritus in Children. J. Craniofacial Surg. 2017, 64, 431–435. [Google Scholar] [CrossRef]
- Kamath, B.M.; Abetz-Webb, L.; Kennedy, C.; Hepburn, B.; Gauthier, M.; Johnson, N.; Medendorp, S.; Dorenbaum, A.; Todorova, L.; Shneider, B.L. Development of a Novel Tool to Assess the Impact of Itching in Pediatric Cholestasis. Patient 2018, 11, 69–82. [Google Scholar] [CrossRef]
- Mighiu, C.; O’hara, S.; Grazzi, E.F.; Murray, K.F.; Schattenberg, J.M.; Ventura, E.; Karakaidos, M.; Taylor, A.; Brrang, H.; Dhawan, A.; et al. Impact of progressive familial intrahepatic cholestasis on caregivers: Caregiver-reported outcomes from the multinational PICTURE study. Orphanet J. Rare Dis. 2022, 17, 32. [Google Scholar] [CrossRef]
- Patel, S.P.; Vasavda, C.; Ho, B.; Meixiong, J.; Dong, X.; Kwatra, S.G. Cholestatic pruritus: Emerging mechanisms and therapeutics. J. Am. Acad. Dermatol. 2019, 81, 1371–1378. [Google Scholar] [CrossRef]
- Baker, A.; Kerkar, N.; Todorova, L.; Kamath, B.M.; Houwen, R.H. Systematic review of progressive familial intrahepatic cholestasis. Clin. Res. Hepatol. Gastroenterol. 2019, 43, 20–36. [Google Scholar] [CrossRef] [PubMed]
- Kamath, B.M.; Baker, A.; Houwen, R.; Todorova, L.; Kerkar, N. Systematic Review: The Epidemiology, Natural History, and Burden of Alagille Syndrome. J. Pediatr. Gastroenterol. Nutr. 2018, 67, 148–156. [Google Scholar] [CrossRef]
- Singham, J.; Schaeffer, D.; Yoshida, E.; Scudamore, C. Choledochal cysts: Analysis of disease pattern and optimal treatment in adult and paediatric patients. HPB 2007, 9, 383–387. [Google Scholar] [CrossRef]
- Swain, M.G. Pruritus in Primary Sclerosing Cholangitis: New Insights into Cause and Treatment. In Primary Sclerosing Cholangitis; Forman, L., Ed.; Springer: Cham, Switzerland, 2017. [Google Scholar] [CrossRef]
- Vij, M.; Rela, M. Biliary atresia: Pathology, etiology and pathogenesis. Futur. Sci. OA 2020, 6, FSO466. [Google Scholar] [CrossRef]
- Kremer, A.E. What are new treatment concepts in systemic itch? Exp. Dermatol. 2019, 28, 1485–1492. [Google Scholar] [CrossRef] [PubMed]
- Kremer, A.E.; Martens, J.J.W.W.; Kulik, W.; Ruëff, F.; Kuiper, E.M.M.; van Buuren, H.R.; van Erpecum, K.J.; Kondrackiene, J.; Prieto, J.; Rust, C.; et al. Lysophosphatidic acid is a potential mediator of cholestatic pruritus. Gastroenterology 2010, 139, 1008–1018.e1. [Google Scholar] [CrossRef] [PubMed]
- Meixiong, J.; Vasavda, C.; Green, D.; Zheng, Q.; Qi, L.; Kwatra, S.G.; Hamilton, J.P.; Snyder, S.H.; Dong, X. Identification of a bilirubin receptor that may mediate a component of cholestatic itch. Elife 2019, 8, e44116. [Google Scholar] [CrossRef] [PubMed]
- Bishop, G.H. The skin as an organ of senses with special reference to the itching sensation. J. Invest. Dermatol. 1948, 11, 143–154. [Google Scholar] [CrossRef]
- Lewis, T.; Zotterman, Y. Vascular reactions of the skin to injury: Part VIII. The resistance of the human skin to constant currents, in relation to injury and vascular response. J. Physiol. 1927, 62, 280–288. [Google Scholar] [CrossRef]
- Davidson, S.; Moser, H.; Giesler, G. Ascending Pathways for Itch. In Itch: Mechanisms and Treatment; National Library of Medicine: Bethesda, MD, USA, 2014. [Google Scholar]
- Dong, X.; Dong, X. Peripheral and Central Mechanisms of Itch. Neuron 2018, 98, 482–494. [Google Scholar] [CrossRef]
- Meixiong, J.; Dong, X. Mas-Related G Protein–Coupled Receptors and the Biology of Itch Sensation. Annu. Rev. Genet. 2017, 51, 103–121. [Google Scholar] [CrossRef]
- Shimada, S.G.; LaMotte, R.H. Behavioral differentiation between itch and pain in mouse. Pain 2008, 139, 681–687. [Google Scholar] [CrossRef]
- Liu, Q.; Tang, Z.; Surdenikova, L.; Kim, S.; Patel, K.N.; Kim, A.; Ru, F.; Guan, Y.; Weng, H.-J.; Geng, Y.; et al. Sensory neuron-specific GPCR Mrgprs are itch receptors mediating chloroquine-induced pruritus. Cell 2009, 139, 1353–1365. [Google Scholar] [CrossRef]
- Han, L.; Ma, C.; Liu, Q.; Weng, H.-J.; Cui, Y.; Tang, Z.; Kim, Y.; Nie, H.; Qu, L.; Patel, K.N.; et al. A subpopulation of nociceptors specifically linked to itch. Nat. Neurosci. 2012, 16, 174–182. [Google Scholar] [CrossRef]
- Usoskin, D.; Furlan, A.; Islam, S.; Abdo, H.; Lönnerberg, P.; Lou, D.; Hjerling-Leffler, J.; Haeggström, J.; Kharchenko, O.; Kharchenko, P.V.; et al. Unbiased classification of sensory neuron types by large-scale single-cell RNA sequencing. Nat. Neurosci. 2015, 18, 145–153. [Google Scholar] [CrossRef]
- Kupari, J.; Usoskin, D.; Parisien, M.; Lou, D.; Hu, Y.; Fatt, M.; Lönnerberg, P.; Spångberg, M.; Eriksson, B.; Barkas, N.; et al. Single cell transcriptomics of primate sensory neurons identifies cell types associated with chronic pain. Nat. Commun. 2021, 12, 1510. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.Q.; von Buchholtz, L.J.; Reker, A.N.; Ryba, N.J.; Davidson, S. Single-nucleus transcriptomic analysis of human dorsal root ganglion neurons. Elife 2021, 10, e71752. [Google Scholar] [CrossRef]
- Meixiong, J.; Vasavda, C.; Snyder, S.H.; Dong, X. MRGPRX4 is a G protein-coupled receptor activated by bile acids that may contribute to cholestatic pruritus. Proc. Natl. Acad. Sci. USA 2019, 116, 10525–10530. [Google Scholar] [CrossRef] [PubMed]
- Alemi, F.; Kwon, E.; Poole, D.P.; Lieu, T.; Lyo, V.; Cattaruzza, F.; Cevikbas, F.; Steinhoff, M.; Nassini, R.; Materazzi, S.; et al. The TGR5 receptor mediates bile acid–induced itch and analgesia. J. Clin. Investig. 2013, 123, 1513–1530. [Google Scholar] [CrossRef] [PubMed]
- Lieu, T.; Jayaweera, G.; Zhao, P.; Poole, D.P.; Jensen, D.; Grace, M.; McIntyre, P.; Bron, R.; Wilson, Y.M.; Krappitz, M.; et al. The Bile Acid Receptor TGR5 Activates the TRPA1 Channel to Induce Itch in Mice. Gastroenterology 2014, 147, 1417–1428. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Zhao, T.; Liu, S.; Wu, Q.; Johnson, O.; Wu, Z.; Zhuang, Z.; Shi, Y.; Peng, L.; He, R.; et al. MRGPRX4 is a bile acid receptor for human cholestatic itch. Elife 2019, 8, e48431. [Google Scholar] [CrossRef]
- Kremer, A.E.; Beuers, U.; Oude-Elferink, R.P.J.; Pusl, T. Pathogenesis and treatment of pruritus in cholestasis. Drugs 2008, 68, 2163–2182. [Google Scholar] [CrossRef] [PubMed]
- Kremer, A.E.; van Dijk, R.; Leckie, P.; Schaap, F.G.; Kuiper, E.M.; Mettang, T.; Reiners, K.S.; Raap, U.; van Buuren, H.R.; van Erpecum, K.J.; et al. Serum autotaxin is increased in pruritus of cholestasis, but not of other origin, and responds to therapeutic interventions. Hepatology 2012, 56, 1391–1400. [Google Scholar] [CrossRef]
- Kittaka, H.; Uchida, K.; Fukuta, N.; Tominaga, M. Lysophosphatidic acid-induced itch is mediated by signalling of LPA5 receptor, phospholipase D and TRPA1/TRPV1. J. Physiol. 2017, 595, 2681–2698. [Google Scholar] [CrossRef]
- Düll, M.M.; Kremer, A.E. Newer Approaches to the Management of Pruritus in Cholestatic Liver Disease. Curr. Hepatol. Rep. 2020, 19, 86–95. [Google Scholar] [CrossRef]
- Does, A.V.; Levy, C.; Yosipovitch, G. Cholestatic Itch: Our Current Understanding of Pathophysiology and Treatments. Am. J. Clin. Dermatol. 2022, 23, 647–659. [Google Scholar] [CrossRef] [PubMed]
- Bunchorntavakul, C.; Reddy, K.R. Pruritus in Chronic Cholestatic Liver Disease. Clin. Liver Dis. 2012, 16, 331–346. [Google Scholar] [CrossRef] [PubMed]
- Product Information: ATARAX(R) Oral Tablet, Oral Syrup, Hydroxyzine Hydrochloride Oral Tablet, Oral Syrup; Pfizer Roerig: New York, NY, USA, 2001.
- Sikand, P.; Dong, X.; LaMotte, R.H. BAM8–22 Peptide Produces Itch and Nociceptive Sensations in Humans Independent of Histamine Release. J. Neurosci. 2011, 31, 7563–7567. [Google Scholar] [CrossRef]
- Marschall, H.; Wagner, M.; Zollner, G.; Fickert, P.; Diczfalusy, U.; Gumhold, J.; Silbert, D.; Fuchsbichler, A.; Benthin, L.; Grundström, R.; et al. Complementary stimulation of hepatobiliary transport and detoxification systems by rifampicin and ursodeoxycholic acid in humans. Gastroenterology 2005, 129, 476–485. [Google Scholar] [CrossRef]
- Cies, J.J.; Giamalis, J.N. Treatment of cholestatic pruritus in children. Am. J. Health Pharm. 2007, 64, 1157–1162. [Google Scholar] [CrossRef]
- Khurana, S.; Singh, P. Rifampin is safe for treatment of pruritus due to chronic cholestasis: A meta-analysis of prospective randomized-controlled trials. Liver Int. 2006, 26, 943–948. [Google Scholar] [CrossRef]
- Geenes, V.; Chambers, J.; Khurana, R.; Shemer, E.W.; Sia, W.; Mandair, D.; Elias, E.; Marschall, H.-U.; Hague, W.; Williamson, C. Rifampicin in the treatment of severe intrahepatic cholestasis of pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 189, 59–63. [Google Scholar] [CrossRef]
- Bergasa, N.V. The pruritus of cholestasis: From bile acids to opiate agonists: Relevant after all these years. Med. Hypotheses 2018, 110, 86–89. [Google Scholar] [CrossRef]
- Chang, Y.; Golkar, L. The Use of Naltrexone in the Management of Severe Generalized Pruritus in Biliary Atresia: Report of a Case. Pediatr. Dermatol. 2008, 25, 403–404. [Google Scholar] [CrossRef]
- Tandon, P.; Rowe, B.H.; VanderMeer, B.; Bain, V.G. The Efficacy and Safety of Bile Acid Binding Agents, Opioid Antagonists, or Rifampin in the Treatment of Cholestasis-Associated Pruritus. Am. J. Gastroenterol. 2007, 102, 1528–1536. [Google Scholar] [CrossRef] [PubMed]
- Kamath, B.M.; Stein, P.; Houwen, R.H.J.; Verkade, H.J. Potential of ileal bile acid transporter inhibition as a therapeutic target in Alagille syndrome and progressive familial intrahepatic cholestasis. Liver Int. 2020, 40, 1812–1822. [Google Scholar] [CrossRef]
- Gonzales, E.; Hardikar, W.; Stormon, M.; Baker, A.; Hierro, L.; Gliwicz, D.; Lacaille, F.; Lachaux, A.; Sturm, E.; Setchell, K.D.R.; et al. Efficacy and safety of maralixibat treatment in patients with Alagille syndrome and cholestatic pruritus (ICONIC): A randomised phase 2 study. Lancet 2021, 398, 1581–1592. [Google Scholar] [CrossRef] [PubMed]
- Loomes, K.M.; Squires, R.H.; Kelly, D.; Rajwal, S.; Soufi, N.; Lachaux, A.; Jankowska, I.; Mack, C.; Setchell, K.D.R.; Karthikeyan, P.; et al. Maralixibat for the treatment of PFIC: Long-term, IBAT inhibition in an open-label, Phase 2 study. Hepatol. Commun. 2022, 6, 2379–2390. [Google Scholar] [CrossRef] [PubMed]
- Lemoine, C.; Superina, R. Surgical diversion of enterohepatic circulation in pediatric cholestasis. Semin. Pediatr. Surg. 2020, 29, 150946. [Google Scholar] [CrossRef] [PubMed]
- O’Keeffe, C.; Baird, A.W.; Nolan, N.; McCormick, P.A. Cholestatic pruritus—The role of cutaneous mast cells and nerves. Aliment. Pharmacol. Ther. 2004, 19, 1293–1300. [Google Scholar] [CrossRef]
- Ghent, C.N.; Bloomer, J.R.; Klatskin, G. Elevations in skin tissue levels of bile acids in human cholestasis: Relation to serum levels and to pruritus. Gastroenterology 1977, 73, 1125–1130. [Google Scholar] [CrossRef]
- Bartholomew, T.C.; Summerfield, J.A.; Billing, B.H.; Lawson, A.M.; Setchell, K.D.R. Bile Acid Profiles of Human Serum and Skin Interstitial Fluid and Their Relationship to Pruritus Studied by Gas Chromatography–Mass Spectrometry. Clin. Sci. 1982, 63, 65–73. [Google Scholar] [CrossRef]
- Nakano, S.; Osaka, S.; Sabu, Y.; Minowa, K.; Hirai, S.; Kondou, H.; Kimura, T.; Azuma, Y.; Watanabe, S.; Inui, A.; et al. Effect of food on the pharmacokinetics and therapeutic efficacy of 4-phenylbutyrate in progressive familial intrahepatic cholestasis. Sci. Rep. 2019, 9, 17075. [Google Scholar] [CrossRef]
- Malatack, J.J.; Doyle, D. A Drug Regimen for Progressive Familial Cholestasis Type 2. Pediatrics 2018, 141, e20163877. [Google Scholar] [CrossRef]
- Naoi, S.; Hayashi, H.; Inoue, T.; Tanikawa, K.; Igarashi, K.; Nagasaka, H.; Kage, M.; Takikawa, H.; Sugiyama, Y.; Inui, A.; et al. Improved Liver Function and Relieved Pruritus after 4-Phenylbutyrate Therapy in a Patient with Progressive Familial Intrahepatic Cholestasis Type 2. J. Pediatr. 2014, 164, 1219–1227.e1213. [Google Scholar] [CrossRef]
- Hasegawa, Y.; Hayashi, H.; Naoi, S.; Kondou, H.; Bessho, K.; Igarashi, K.; Hanada, K.; Nakao, K.; Kimura, T.; Konishi, A.; et al. Intractable itch relieved by 4-phenylbutyrate therapy in patients with progressive familial intrahepatic cholestasis type 1. Orphanet J. Rare Dis. 2014, 9, 89. [Google Scholar] [CrossRef] [PubMed]
- Cazzagon, N.; Floreani, A. Primary biliary cholangitis: Treatment. Curr. Opin. Gastroenterol. 2021, 37, 99–104. [Google Scholar] [CrossRef] [PubMed]
- De Vries, E.; Bolier, R.; Goet, J.; Parés, A.; Verbeek, J.; de Vree, M.; Drenth, J.; van Erpecum, K.; van Nieuwkerk, K.; van der Heide, F.; et al. Fibrates for Itch (FITCH) in Fibrosing Cholangiopathies: A Double-Blind, Randomized, Placebo-Controlled Trial. Gastroenterology 2021, 160, 734–743.e6. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodrigo, M.; Dong, X.; Chien, D.; Karnsakul, W. Cholestatic Pruritus in Children: Conventional Therapies and Beyond. Biology 2023, 12, 756. https://doi.org/10.3390/biology12050756
Rodrigo M, Dong X, Chien D, Karnsakul W. Cholestatic Pruritus in Children: Conventional Therapies and Beyond. Biology. 2023; 12(5):756. https://doi.org/10.3390/biology12050756
Chicago/Turabian StyleRodrigo, Minna, Xinzhong Dong, Daphne Chien, and Wikrom Karnsakul. 2023. "Cholestatic Pruritus in Children: Conventional Therapies and Beyond" Biology 12, no. 5: 756. https://doi.org/10.3390/biology12050756





