Comparison of Radiographic Outcomes Assessed via the Radiographic Union Scale for Tibial Fractures and Alkaline Phosphatase Levels during the Tibial Healing Process: A Series of Case Reports
Abstract
Simple Summary
Abstract
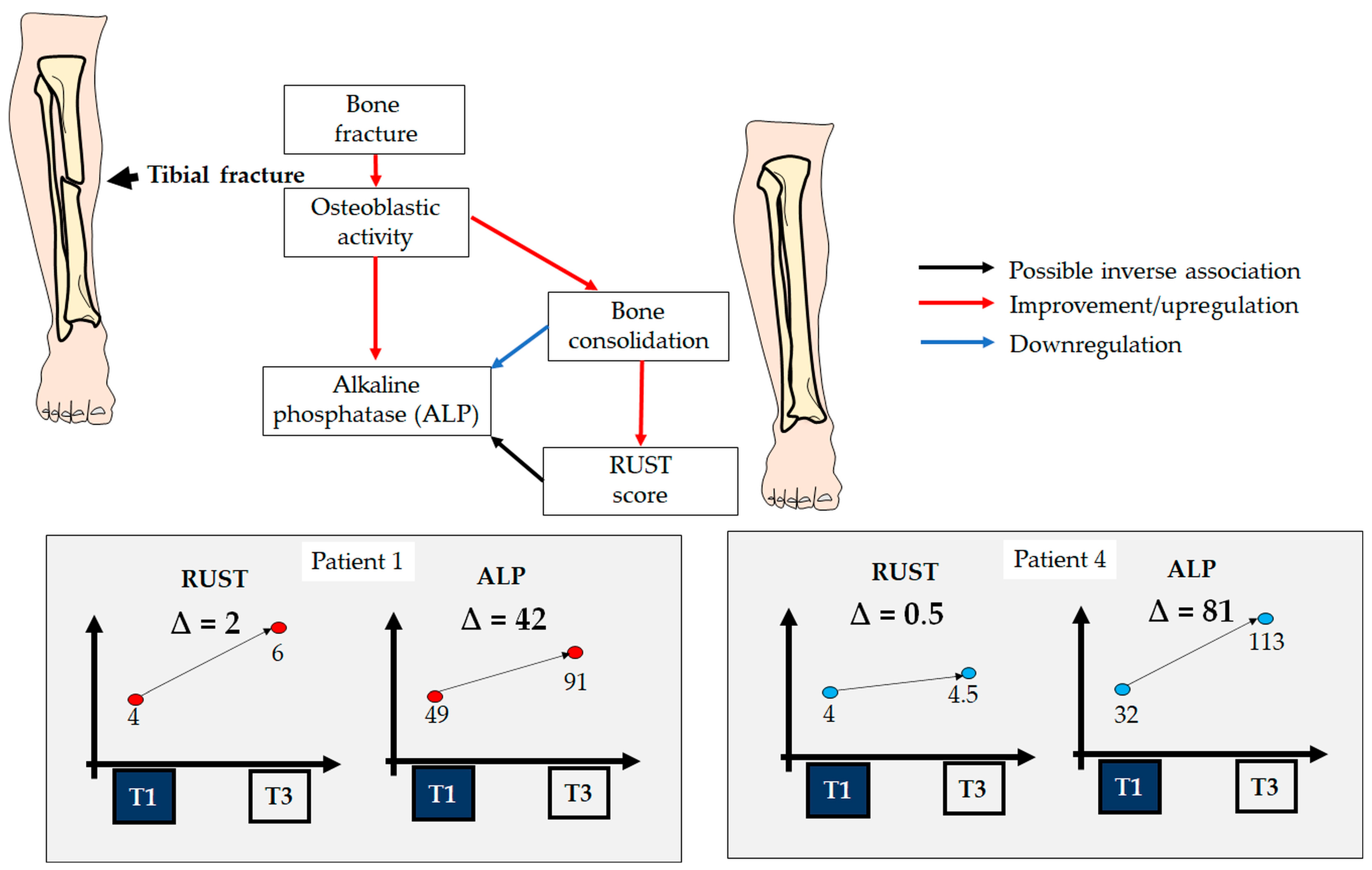
1. Introduction
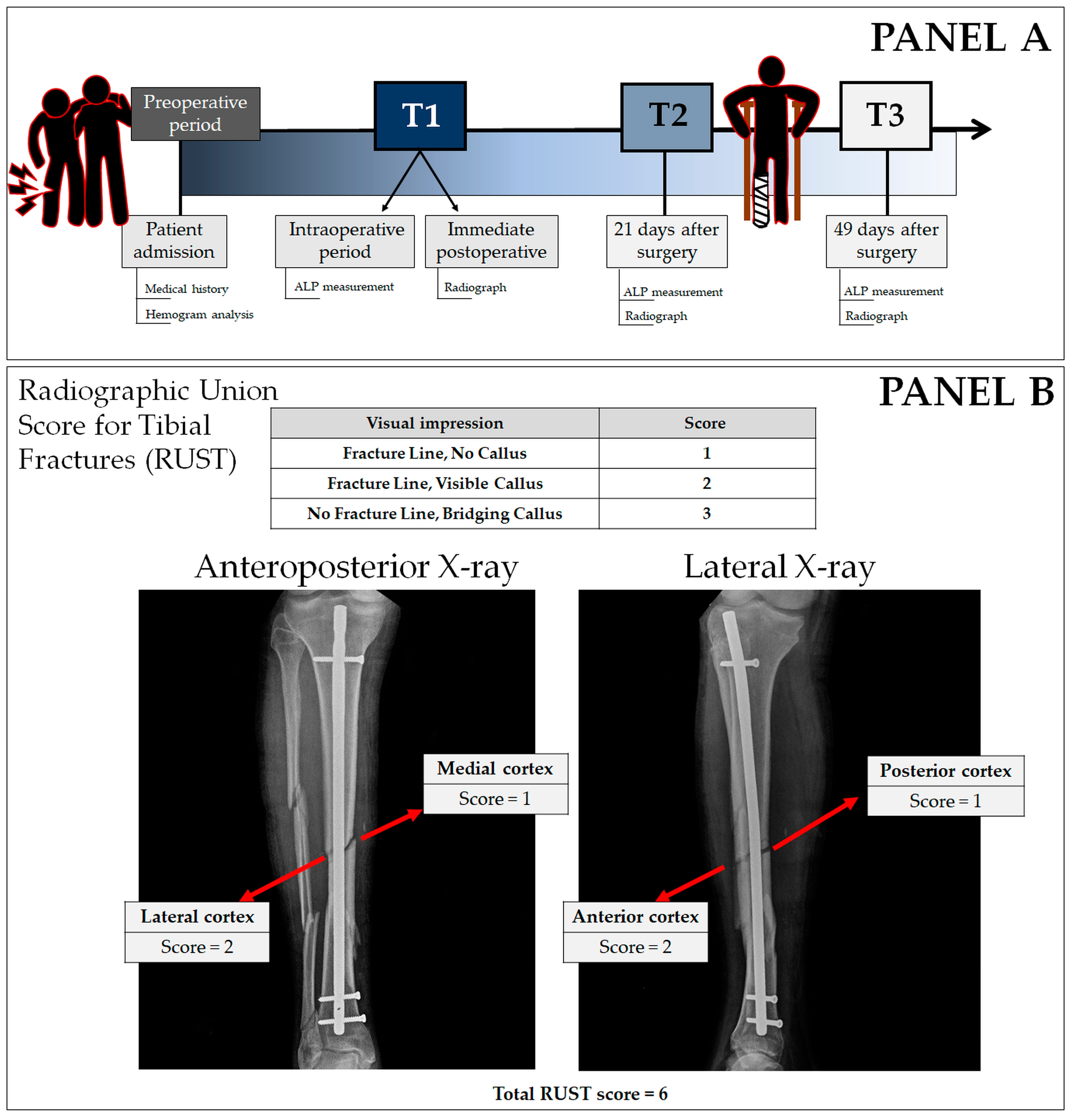
2. Materials and Methods
2.1. Case Series
2.2. Tibial Reamed Intramedullary Nailing Surgery
2.3. X-ray
2.4. Radiographic Union Scale for Tibial Fractures
2.5. Alkaline Phosphatase Measurement
2.6. Statistical Analysis
3. Results
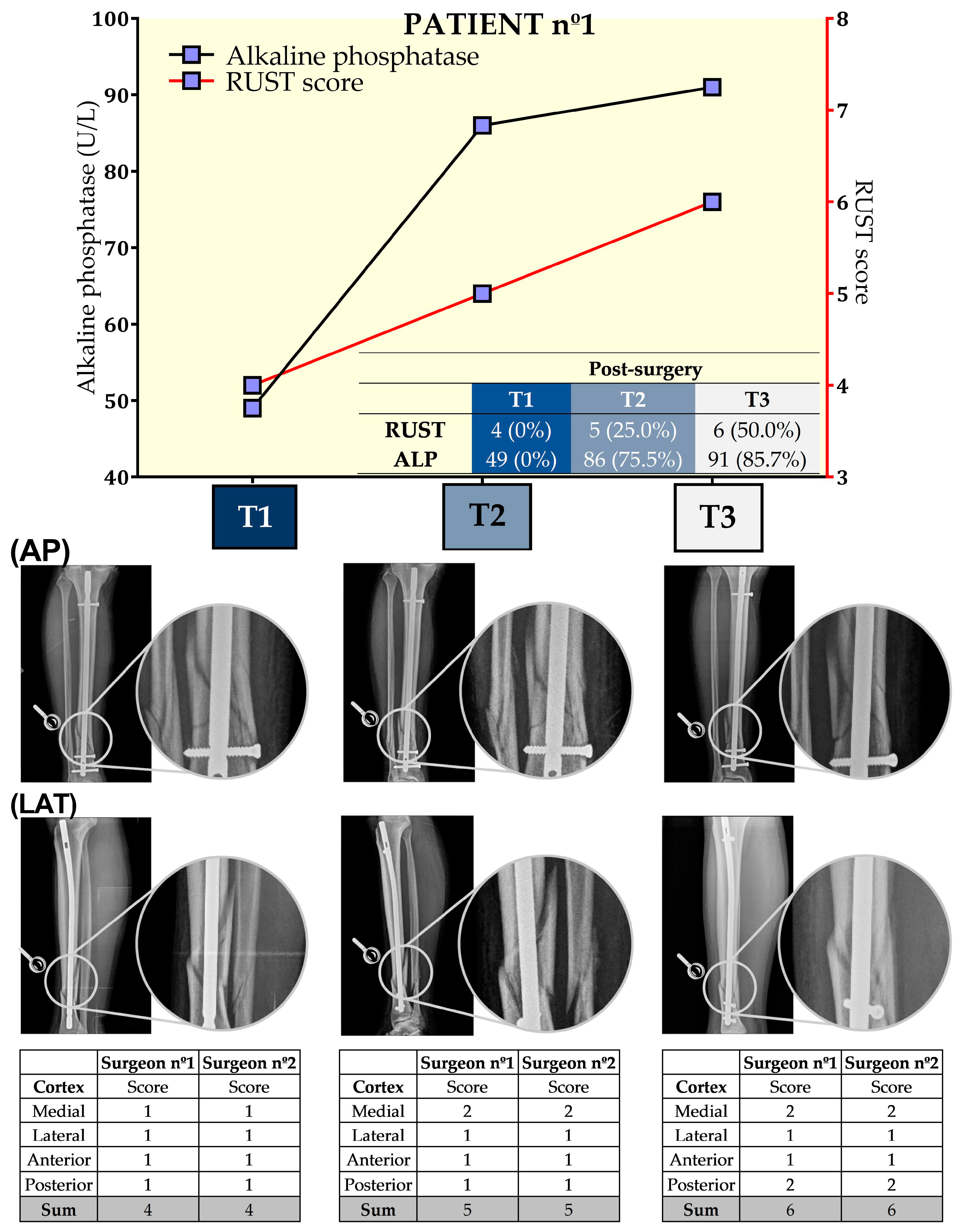
3.1. Patient nº1
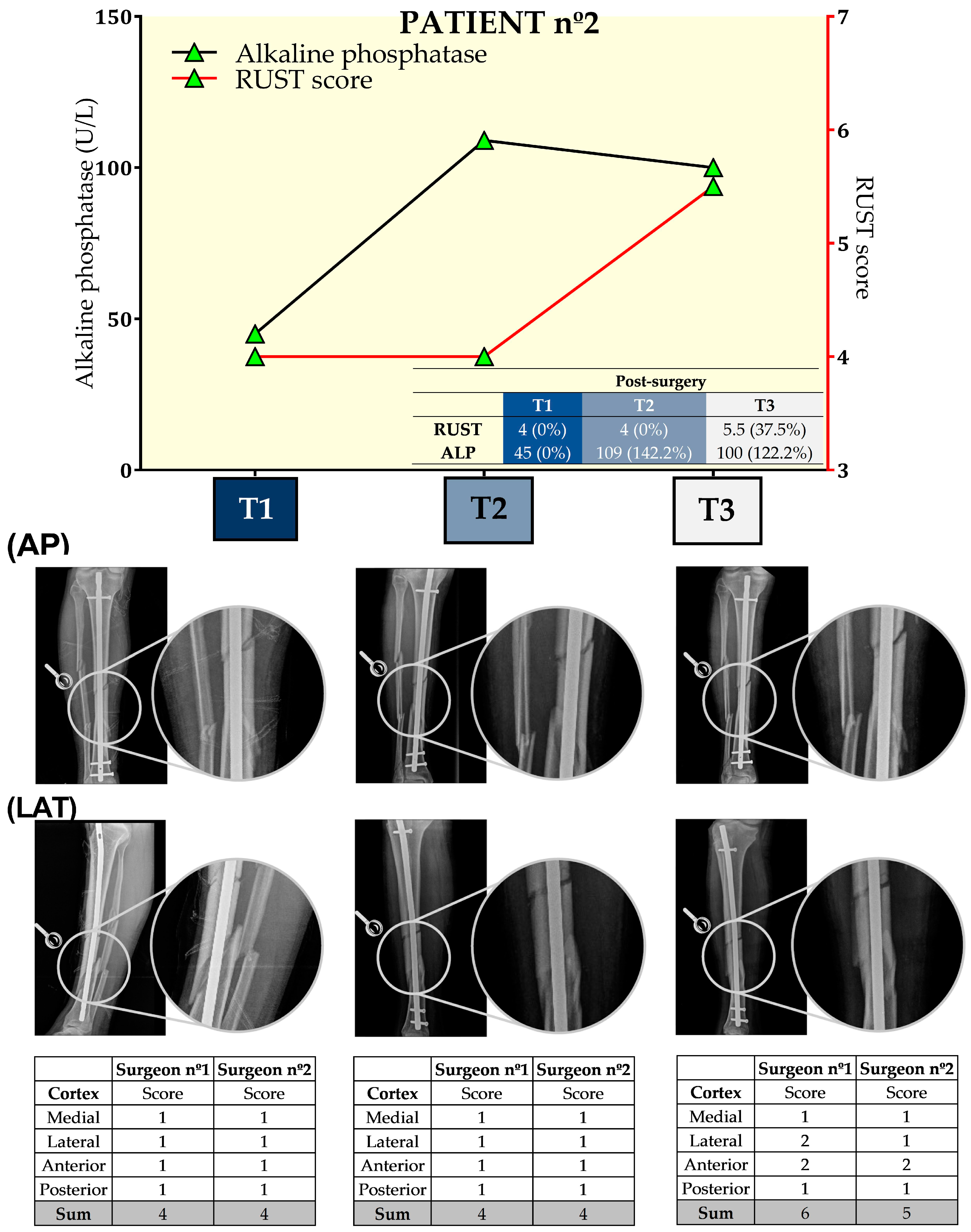
3.2. Patient nº2
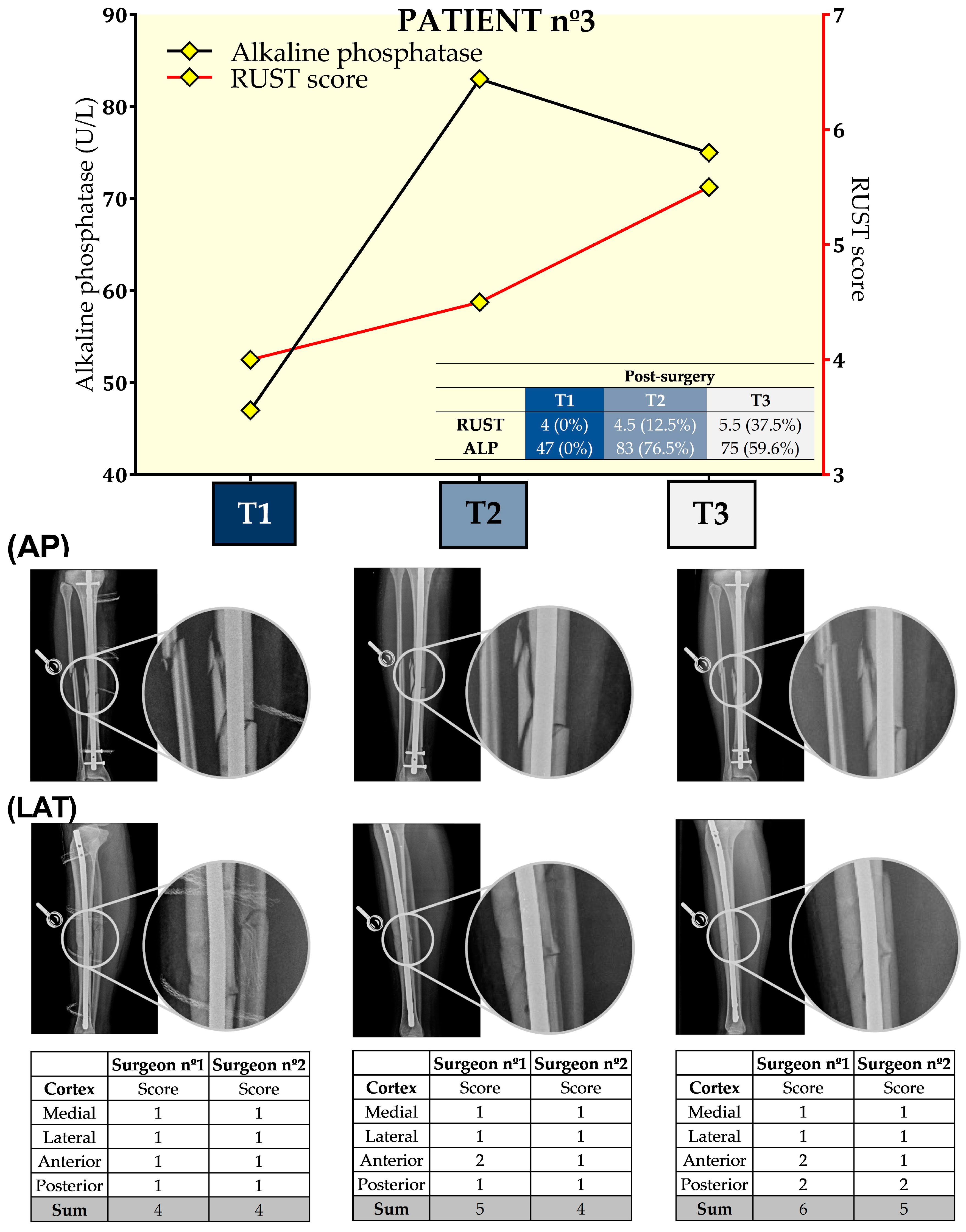
3.3. Patient nº3
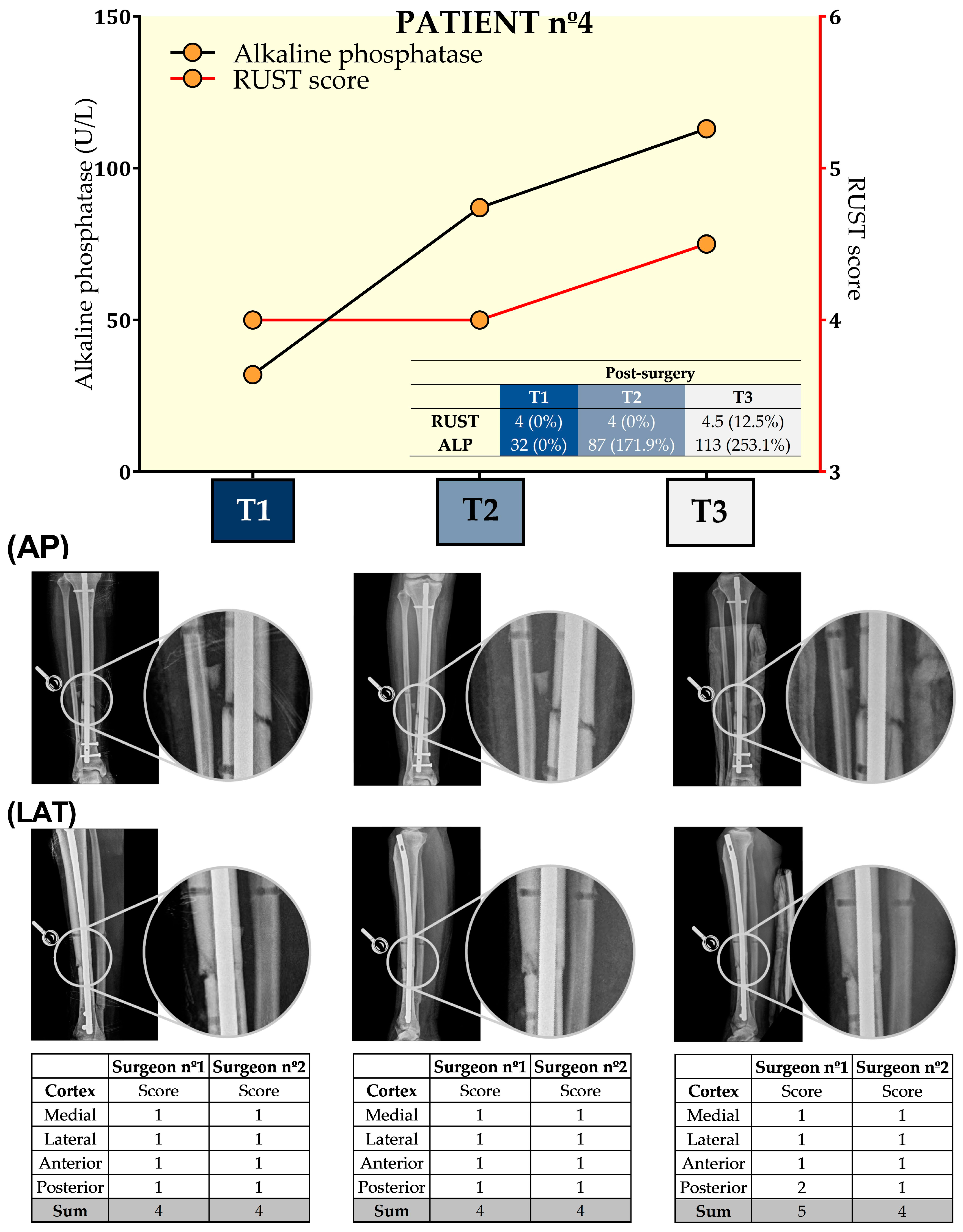
3.4. Patient nº4
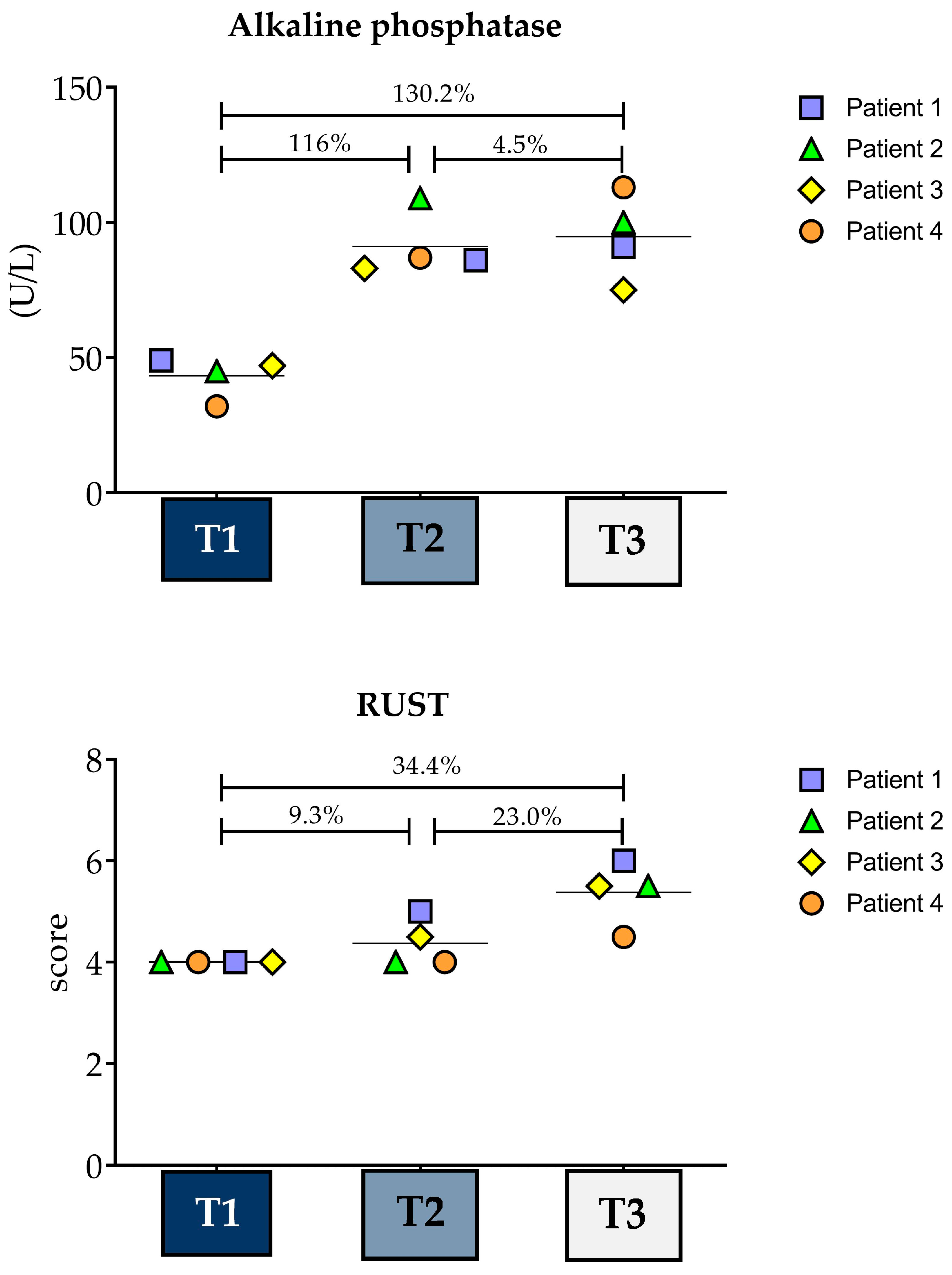
3.5. Variance Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wennergren, D.; Bergdahl, C.; Ekelund, J.; Juto, H.; Sundfeldt, M.; Möller, M. Epidemiology and incidence of tibia fractures in the Swedish Fracture Register. Injury 2018, 49, 2068–2074. [Google Scholar] [CrossRef] [PubMed]
- Clement, N.D.; Beauchamp, N.J.F.; Duckworth, A.D.; McQueen, M.M.; Court-Brown, C.M. The outcome of tibial diaphyseal fractures in the elderly. Bone Jt. J. 2013, 95, 1255–1262. [Google Scholar] [CrossRef] [PubMed]
- Browner, B.; Levine, A.; Trafton, P. Skeletal Trauma: Fractures, Dislocations, Ligamentous Injuries; W.B.S.C. Ltd.: Philadelphia, PA, USA, 2003. [Google Scholar]
- Iqbal, S.; Saeed, H.S.; Aslam, B.; Fayyaz, I. Tibial diaphyseal fractures; evaluation of management treated by pop cast versus intramedullary nailing in terms of time of union. Prof. Med. J. 2017, 24, 1336–1341. [Google Scholar]
- Siddique, A.; Pirwani, M.A.; Lal, K.; Rehman, A. Reamed versus unreamed interlocking nailing for fracture shaft of tibia. Pak. J. Surg. 2009, 25, 53–57. [Google Scholar]
- Kruppa, C.G.; Hoffmann, M.F.; Sietsema, D.L.; Mulder, M.B.; Jones, C.B. Outcomes After Intramedullary Nailing of Distal Tibial Fractures. J. Orthop. Trauma 2015, 29, e309–e315. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.A.; Swiontkowski, M.; Bhandari, M.; Walter, S.D.; Schemitsch, E.H.; Sanders, D.; Tornetta, P., III. Reaming Does Not Affect Functional Outcomes After Open and Closed Tibial Shaft Fractures: The Results of a Randomized Controlled Trial. J. Orthop. Trauma 2016, 30, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Filho, F.A.S.d.A.; Cotias, R.B.; Azi, M.L.; Teixeira, A.A.d.A. Reliability of the radiographic union scale in tibial fractures (RUST). Rev. Bras. Ortop. 2017, 52, 35–39. [Google Scholar]
- Bell, A.; Templeman, D.; Weinlein, J.C. Nonunion of the Femur and Tibia: An Update. Orthop. Clin. N. Am. 2016, 47, 365–375. [Google Scholar] [CrossRef] [PubMed]
- FDA (Food and Drug Administration). Guidance Document for Industry and CDRH Staff for the Preparation of Investigational Device Exemptions and Premarket Approval Applications for Bone Growth Stimulator Devices; 1998; pp. 23292–23293. Available online: https://www.federalregister.gov/documents/1998/04/28/98-11158/guidance-document-for-industry-and-cdrh-staff-for-the-preparation-of-investigational-device (accessed on 8 April 2024).
- O’Halloran, K.; Coale, M.; Costales, T.; Zerhusen, T.; Castillo, R.C.; Nascone, J.W.; O’Toole, R.V. Will My Tibial Fracture Heal? Predicting Nonunion at the Time of Definitive Fixation Based on Commonly Available Variables. Clin. Orthop. Relat. Res. 2016, 474, 1385–1395. [Google Scholar] [CrossRef]
- Wildemann, B.; Ignatius, A.; Leung, F.; Taitsman, L.A.; Smith, R.M.; Pesántez, R.; Stoddart, M.J.; Richards, R.G.; Jupiter, J.B. Non-union bone fractures. Nat. Rev. Dis. Primers 2021, 7, 57. [Google Scholar] [CrossRef]
- Salih, S.; Dennison, M.G.; Blakey, C.; Chan, D.; McGregor-Riley, J.C.; Royston, S.L.; Gowlett, S.; Moore, D. The callus fracture sign: A radiological predictor of progression to hypertrophic non-union in diaphyseal tibial fractures. Strateg. Trauma Limb Reconstr. 2015, 10, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.S.; Kazam, J.J.; Fufa, D.; Bartolotta, R.J. Radiologic evaluation of fracture healing. Skelet. Radiol. 2019, 48, 349–361. [Google Scholar] [CrossRef] [PubMed]
- McCloskey, E.V.; Spector, T.D.; Eyres, K.S.; Fern, E.D.; O’Rourke, N.; Vasikaran, S.; Kanis, J.A. The assessment of vertebral deformity: A method for use in population studies and clinical trials. Osteoporos. Int. 1993, 3, 138–147. [Google Scholar] [CrossRef]
- Whelan, D.B.M.; Bhandari, M.M.; Stephen, D.M.; Kreder, H.M.; McKee, M.D.M.; Zdero, R.; Schemitsch, E.H.M. Development of the radiographic union score for tibial fractures for the assessment of tibial fracture healing after intramedullary fixation. J. Trauma 2010, 68, 629–632. [Google Scholar] [CrossRef]
- Kooistra, B.W.; Dijkman, B.G.; Busse, J.W.; Sprague, S.; Schemitsch, E.H.; Bhandari, M. The radiographic union scale in tibial fractures: Reliability and validity. J. Orthop. Trauma 2010, 24 (Suppl. 1), S81–S86. [Google Scholar] [CrossRef]
- Leow, J.M.; Clement, N.D.; Tawonsawatruk, T.; Simpson, C.J.; Simpson AH, R.W. The radiographic union scale in tibial (RUST) fractures: Reliability of the outcome measure at an independent centre. Bone Jt. Res. 2016, 5, 116–121. [Google Scholar] [CrossRef]
- Hunter, L.W.; Shiekh, F.A.; Pisimisis, G.T.; Kim, S.-H.; Edeh, S.N.; Miller, V.M.; Lieske, J.C. Key role of alkaline phosphatase in the development of human-derived nanoparticles in vitro. Acta Biomater. 2011, 7, 1339–1345. [Google Scholar] [CrossRef]
- Sharma, U.; Pal, D.; Prasad, R. Alkaline phosphatase: An overview. Indian J. Clin. Biochem. 2014, 29, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Shu, J.; Tan, A.; Li, Y.; Huang, H.; Yang, J. The correlation between serum total alkaline phosphatase and bone mineral density in young adults. BMC Musculoskelet. Disord. 2022, 23, 467. [Google Scholar]
- Ajai, S.; Sabir, A.; Mahdi, A.A.; Srivastava, R.N. Evaluation of Serum Alkaline Phosphatase as a Biomarker of Healing Process Progression of Simple Diaphyseal Fractures in Adult Patients. Int. Res. J. Biol. Sci. 2013, 2, 40–43. [Google Scholar]
- Freitas, G.N.P.; Pinho, R.C.; Pereira, V.M.; Antonini, C.E.; Oliveira, A. Diaphysial fracture of the tibia: Osteosynthesis with medullary nail by Lottes. Rev. Bras. Ortop. 1993, 28, 597–601. [Google Scholar]
- Morais, A.; Siqueira, A. Posicionamento Radiográfico. 2016. Available online: https://integrada.minhabiblioteca.com.br/#/books/9788527730297/ (accessed on 8 April 2024).
- Macri, F.; Marques, L.F.; Backer, R.C.; Santos, M.J.; Belangero, W.D. Validation of a standardised gait score to predict the healing of tibial fractures. J. Bone Jt. Surg. Br. 2012, 94, 544–548. [Google Scholar] [CrossRef]
- Roy, A.V. Rapid method for determining alkaline phosphatase activity in serum with thymolphthalein monophosphate. Clin. Chem. 1970, 16, 431–436. [Google Scholar] [CrossRef]
- Chaudhary, D.S.; Solanki, J.J.; Verma, T.; Chavali, V.H. Monitoring the Progress of Treatment in Fracture Non-Union: The Role of Alkaline Phosphatase and Ultrasonography. Rev. Bras. Ortop. 2021, 56, 796–803. [Google Scholar]
- Oni, O.O.; Mahabir, J.; Iqbal, S.; Gregg, P. Serum osteocalcin and total alkaline phosphatase levels as prognostic indicators in tibial shaft fractures. Injury 1989, 20, 37–38. [Google Scholar] [CrossRef]
- Bowles, S.A.; Kurdy, N.; Davis, A.M.; France, M.W. Changes in Serum Bone-Specific Alkaline Phosphatase following Tibial Fracture. Ann. Clin. Biochem. 1997, 34, 690–691. [Google Scholar] [CrossRef] [PubMed]
- Magnusson, P.; Sharp, C.A.; Farley, J.R. Different distributions of human bone alkaline phosphatase isoforms in serum and bone tissue extracts. Clin. Chim. Acta 2002, 325, 59–70. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Result | 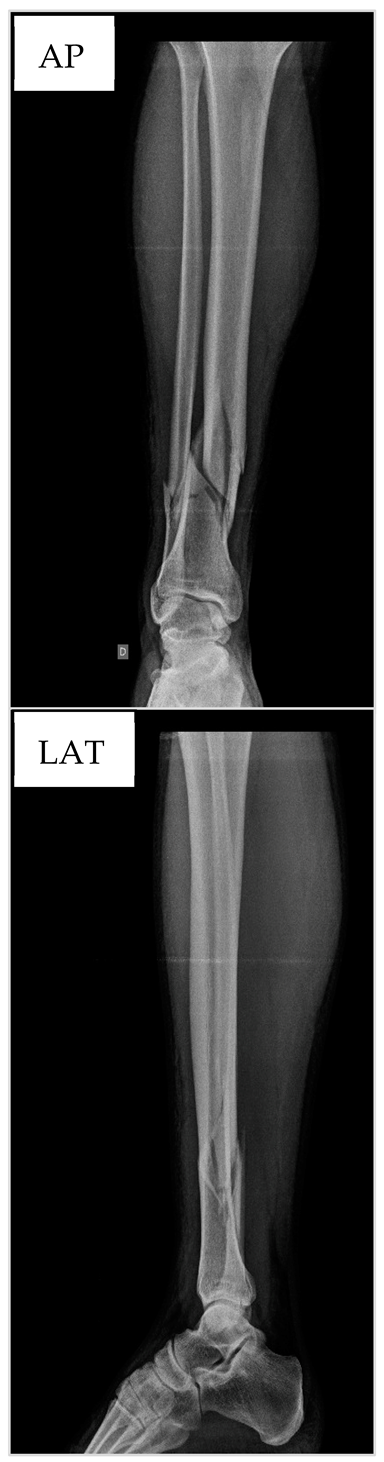 |
| Body mass (kg) | 82 | |
| Height (m) | 170 | |
| BMI (kg/m2) | 28.3 | |
| RBC (106/µL) | 4.6 | |
| Hemoglobin (g/dL) | 13.2 | |
| Hematocrit (%) | 39.2 | |
| MCV (fL) | 85.2 | |
| MCH (pg) | 28.7 | |
| MCHC (106/µL) | 33.7 | |
| RDW (%) | 13.6 | |
| WBC (109/µL) | 8400 | |
| Promyelocytes (%) | 0 | |
| Myelocytes (%) | 0 | |
| Metamyelocytes (%) | 0 | |
| Band cells (%) | 0 | |
| Segregated cells (%) | 72 | |
| Neutrophils (%) | 72 | |
| Eosinophils (%) | 1 | |
| Basophils (%) | 0 | |
| Typical lymphocytes (%) | 18 | |
| Atypical lymphocytes (%) | 0 | |
| Monocytes (%) | 9 | |
| Blasts (%) | 0 | |
| Platelets (109/L) | 211.000 | |
| MPV (fL) | 8.7 |
| Parameter | Result | 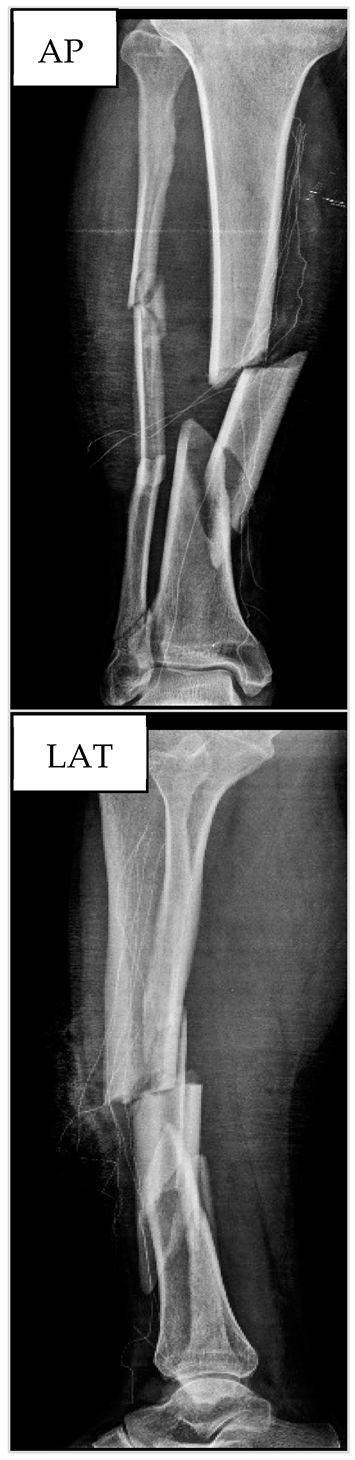 |
| Body mass (kg) | 82.0 | |
| Height (m) | 1.75 | |
| BMI (kg/m2) | 26.7 | |
| RBC (106/µL) | 3.93 | |
| Hemoglobin (g/dL) | 12.5 | |
| Hematocrit (%) | 37.1 | |
| MCV (fL) | 94.4 | |
| MCH (pg) | 31.8 | |
| MCHC (106/µL) | 33.7 | |
| RDW (%) | 11.5 | |
| WBC (109/µL) | 9.700 | |
| Promyelocytes (%) | 0 | |
| Myelocytes (%) | 0 | |
| Metamyelocytes (%) | 0 | |
| Band cells (%) | 0 | |
| Segregated cells (%) | 73 | |
| Neutrophils (%) | 73 | |
| Eosinophils (%) | 1 | |
| Basophils (%) | 0 | |
| Typical lymphocytes (%) | 21 | |
| Atypical lymphocytes (%) | 0 | |
| Monocytes (%) | 5 | |
| Blasts (%) | 0 | |
| Platelets (109/L) | 165.000 | |
| MPV (fL) | 10.5 |
| Parameter | Result | 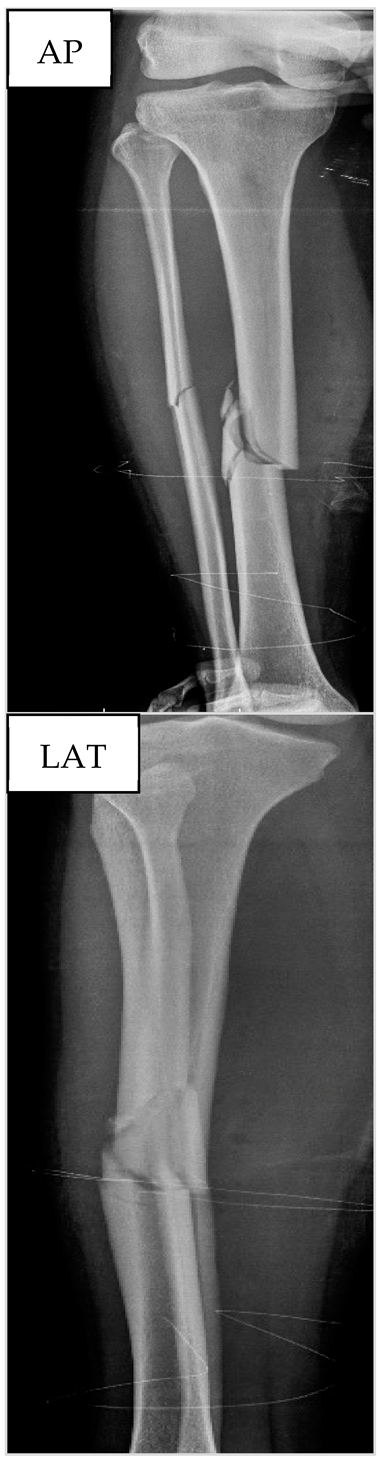 |
| Body mass (kg) | 63.0 | |
| Height (m) | 1.61 | |
| BMI (kg/m2) | 24.3 | |
| RBC (106/µL) | 4.37 | |
| Hemoglobin (g/dL) | 12.8 | |
| Hematocrit (%) | 37.1 | |
| MCV (fL) | 84.9 | |
| MCH (pg) | 29.3 | |
| MCHC (106/µL) | 34.5 | |
| RDW (%) | 13 | |
| WBC (109/µL) | 9.400 | |
| Promyelocytes (%) | 0 | |
| Myelocytes (%) | 0 | |
| Metamyelocytes (%) | 0 | |
| Band cells (%) | 0 | |
| Segregated cells (%) | 71 | |
| Neutrophils (%) | 71 | |
| Eosinophils (%) | 1 | |
| Basophils (%) | 0 | |
| Typical lymphocytes (%) | 22 | |
| Atypical lymphocytes (%) | 0 | |
| Monocytes (%) | 6 | |
| Blasts (%) | 0 | |
| Platelets (109/L) | 265.000 | |
| MPV (fL) | 9.4 |
| Parameter | Result | 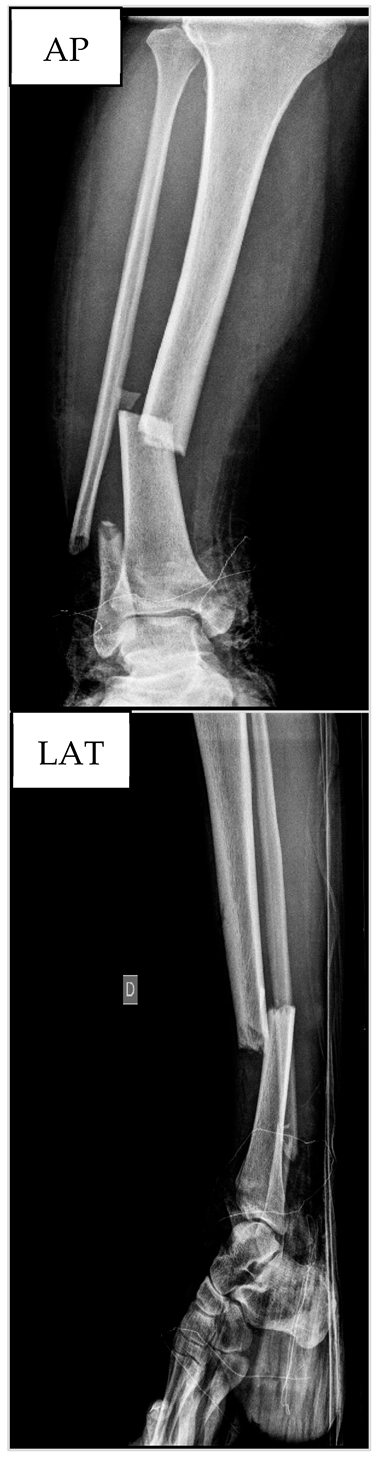 |
| Body mass (kg) | 74.0 | |
| Height (m) | 1.68 | |
| BMI (kg/m2) | 26.2 | |
| RBC (106/µL) | 2.37 | |
| Hemoglobin (g/dL) | 7.2 | |
| Hematocrit (%) | 22.1 | |
| MCV (fL) | 93.2 | |
| MCH (pg) | 30.4 | |
| MCHC (106/µL) | 32.6 | |
| RDW (%) | 12.7 | |
| WBC (109/µL) | 15.100 | |
| Promyelocytes (%) | 0 | |
| Myelocytes (%) | 0 | |
| Metamyelocytes (%) | 0 | |
| Band cells (%) | 3 | |
| Segregated cells (%) | 69 | |
| Neutrophils (%) | 72 | |
| Eosinophils (%) | 0 | |
| Basophils (%) | 0 | |
| Typical lymphocytes (%) | 21 | |
| Atypical lymphocytes (%) | 0 | |
| Monocytes (%) | 7 | |
| Blasts (%) | 0 | |
| Platelets (109/L) | 446.000 | |
| MPV (fL) | 7.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ninomiya, A.F.; Bertolucci, V.; Kaneko, L.O.; Nonose, N.; Abreu, L.d.L.; Harfuch, G.R.; dos Reis, I.G.M.; Scariot, P.P.M.; Messias, L.H.D. Comparison of Radiographic Outcomes Assessed via the Radiographic Union Scale for Tibial Fractures and Alkaline Phosphatase Levels during the Tibial Healing Process: A Series of Case Reports. Biology 2024, 13, 407. https://doi.org/10.3390/biology13060407
Ninomiya AF, Bertolucci V, Kaneko LO, Nonose N, Abreu LdL, Harfuch GR, dos Reis IGM, Scariot PPM, Messias LHD. Comparison of Radiographic Outcomes Assessed via the Radiographic Union Scale for Tibial Fractures and Alkaline Phosphatase Levels during the Tibial Healing Process: A Series of Case Reports. Biology. 2024; 13(6):407. https://doi.org/10.3390/biology13060407
Chicago/Turabian StyleNinomiya, André Felipe, Vanessa Bertolucci, Luisa Oliveira Kaneko, Nilson Nonose, Luiza di Loreto Abreu, Gabriel Rodrigues Harfuch, Ivan Gustavo Masselli dos Reis, Pedro Paulo Menezes Scariot, and Leonardo Henrique Dalcheco Messias. 2024. "Comparison of Radiographic Outcomes Assessed via the Radiographic Union Scale for Tibial Fractures and Alkaline Phosphatase Levels during the Tibial Healing Process: A Series of Case Reports" Biology 13, no. 6: 407. https://doi.org/10.3390/biology13060407
APA StyleNinomiya, A. F., Bertolucci, V., Kaneko, L. O., Nonose, N., Abreu, L. d. L., Harfuch, G. R., dos Reis, I. G. M., Scariot, P. P. M., & Messias, L. H. D. (2024). Comparison of Radiographic Outcomes Assessed via the Radiographic Union Scale for Tibial Fractures and Alkaline Phosphatase Levels during the Tibial Healing Process: A Series of Case Reports. Biology, 13(6), 407. https://doi.org/10.3390/biology13060407









