System of Project Management at a Medical Hub as an Instrument for Implementation of Open Innovation
Abstract
:1. Introduction
- The formation of a common knowledge base, the exchange of necessary competencies and the ability to offer the market a more attractive product value;
- The distribution of risks between partners;
- The maximization of total revenues due to the emergence of a network synergetic effect (system effect).
2. Literature Review
- The network involves two or more enterprises whose activities are aimed at achieving common goals and solving problems in the long run;
- Partner companies coordinate their functions, but do not combine them.
- A single goal ensures the stability of the network;
- The independent performance of the network participants also allows benefiting from their position in the network structure;
- Pooling the resources and efforts of the network participants takes place on a voluntary basis;
- The functional uniqueness of each member of the network makes it possible to achieve greater success for the entire organization. The presence of several leaders gives the organization stability and flexibility;
- Network organizations are multi-level structures.
- -
- Adaptability and rapid response to changes in the market;
- -
- The ability to concentrate the activities of each participant on the best competencies and unique processes, which allows achieving high quality production and distribution of goods and services;
- -
- Significant reduction of costs and rational allocation;
- -
- The possibility of attracting optimal partners to joint activities within the network, excluding the use of incompetent performers.
3. Materials and Methods
4. Results and Discussion
4.1. Structure of the Medical Hub Business Model
4.2. Structure of the Operational Business Model of the Medical Hub Business Processes
- Level of operations and key abilities;
- Resource level.

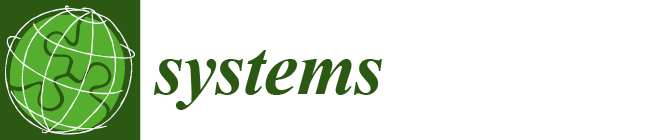
4.3. Project Management System as a Tool for Implementing Strategic Goals of the Medical Hub
- Optimizing a medical hub’s business model may require systems, processes and assets that are quite costly;
- In medicine, project management is used to solve unique and large-scale business problems, but the degree of prevalence of the project approach is still low;
- There is a degree of impenetrability in the medical hub’s business model, which makes it difficult for competitors to reproduce it;
- There are unique resources, such as a brand, an organizational system and a network of partners that have a certain static nature.
4.4. Efficiency Assessment of the Medical Hub Business Model
- Dimension;
- Density;
- Diameter;
- Average degree;
- Centrality measures (centrality by mediation, centrality by degree and centrality by proximity);
- Clustering coefficient;
- Maximum click;
- K-core.
5. Conclusions
- –
- Pay increased attention to optimizing the business model of the medical hub in the field of configuration;
- –
- Update in a timely manner the interface for interaction with suppliers and partners and/or the interface for interaction with external clients, depending on the chosen strategy for the development of the medical hub;
- –
- The quality of medical care can be solved primarily by introducing modern management systems into medical institutions, in particular, a quality management system based on international standards;
- –
- It is necessary to develop management rules and procedures that ensure optimal management of each of the types of projects of the company participating in the medical hub, as well as to obtain a trained project management team with a separate analytical service;
- –
- Each project participant needs to know all the steps to complete the tasks of each sprint, so participants need access to the standard operating procedures of the companies participating in the medical hub so that they can do their job efficiently and reliably.
- –
- Avoiding losses from the provision of services of inadequate quality, the share of which in the health care system is, according to a number of experts, 30–60%;
- –
- Application of the process approach at the initial stage of the implementation of the project management system will allow you to look at the medical organization from the outside and clearly define the responsibility, authority, resources, information and management communications. This approach does not reject the existing management system, but determines ways to improve it and gradually transition to a process management system;
- –
- Thanks to the many built-in self-improvement mechanisms (internal audits, management analysis, feedback from consumers, etc.), the implementation of a project management system will ensure timely changes in the system in response to changes in the external and internal environment, as well as continuous improvement in the activities of a medical organization;
- –
- The involvement of personnel in project management activities enables the medical organization to more effectively use the abilities, knowledge, skills and abilities of its employees;
- –
- When building a project management system within the framework of a medical hub, the costs of a medical organization are reduced, mainly due to streamlining activities, eliminating unnecessary or inefficient processes and external and internal losses caused by defects and inconsistencies;
- –
- An effective project management system within the medical hub also reduces management costs.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dubois, A. Organizing Industrial Activities Across Firm Boundaries; Routledge: London, UK, 1998. [Google Scholar] [CrossRef]
- Stamps, J.; Lipnack, J. The Age of the Network: Organizing Principles for the 21st Century; Omneo, Oliver Wight Publications: Essex, UK, 1994. [Google Scholar]
- Webster, F.E. The Changing Role of Marketing in the Corporation. J. Mark. 1992, 56, 1–17. [Google Scholar] [CrossRef]
- Hakansson, H. Evolution Processes in Industrial Networks; Industrial Networks; A New View of Reality; Routledge: London, UK, 1999. [Google Scholar]
- Sheresheva, M.Y. Forms of Network Interaction of Companies; Higher School of Economics Publ.: Moscow, Russia, 2010. [Google Scholar]
- Atkinson, R. Project management: Cost, time and quality, two best guesses and a phenomenon, its time to accept other success criteria. Int. J. Proj. Manag. 1999, 17, 337–342. [Google Scholar] [CrossRef]
- Cooke-Davis, T. Project Success. In The Wiley Guide to Managing Projects; Morris, P., Pinto, G., Eds.; Wiley: Hoboken, NJ, USA, 2004; pp. 99–122. [Google Scholar]
- Ellmann, S. Management of complex projects: Invisible structures, coordination and recommendations for management. In Proceedings of the 22nd IPMA World Congress, Rome, Italy, 9–11 November 2008; pp. 12–32. [Google Scholar]
- Clarke, A. A practical use of key success factors to improve the effectiveness of project management. Int. J. Proj. Manag. 1999, 17, 139–145. [Google Scholar] [CrossRef]
- Brown, S.L.; Eisenhardt, K.M. Product Development: Past Research, Present Findings, and Future Directions. Acad. Manag. Rev. 1995, 20, 343–378. [Google Scholar] [CrossRef]
- Väänänen, M. Communication in high technology product development projects. In Project Personnel’s Viewpoint for Improvement; Juvenes Print; University of Oulu: Oulu, Finland, 2010; Volume C364, p. 210. [Google Scholar]
- Fliaster, A.; Schloderer, F. Dyadic ties among employees: Empirical analysis of creative performance and efficiency. Hum. Relat. 2010, 63, 1513–1540. [Google Scholar] [CrossRef]
- Müller, R.; Jugdev, K. Critical success factors in projects: Pinto, Slevin, and Prescott—The elucidation of project success. Int. J. Manag. Proj. Bus. 2012, 5, 757–775. [Google Scholar] [CrossRef]
- Spalek, S. Critical success factors in project management. To fail or not to fail, that is the question! In Proceedings of the Global Congress 2005—EMEA, Edinburgh, Scotland, 23–25 May 2005; Project Management Institute: Newtown Square, PA, USA, 2005. [Google Scholar]
- Mead, S.P. Using social network analysis to visualize project teams. Proj. Manag. J. 2001, 32, 32–38. [Google Scholar] [CrossRef]
- Toomey, L. Social Networks and Project Management Performance: How Do Social Networks Contribute to Project Management Performance? In Proceedings of the Research and Education Conference, Limerick, Ireland, 15–18 July 2012; Project Management Institute: Newtown Square, PA, USA, 2012. [Google Scholar]
- Ballinger, G.; Craig, E.; Cross, R.; Gray, P. A Stitch in Time Saves Nine: Leveraging Networks to Reduce the Costs of Turnover. Calif. Manag. Rev. 2011, 53, 111–133. [Google Scholar] [CrossRef] [Green Version]
- Chinowsky, P.; Diekmann, J.; Galotti, V. Social network model of construction. J. Constr. Eng. Manag. 2008, 134, 799–804. [Google Scholar] [CrossRef]
- Durland, M.; Fredericks, K. An Introduction to Social Network Analysis. New Dir. Eval. 2006, 2005, 5–13. [Google Scholar] [CrossRef]
- Plokhov, D.V.; Nikulchev, E.V.; Titov, S.; Osipov, I.V. Methodology for assessing the impact of social communications on the effectiveness of an innovative project. Cloud Sci. 2016, 3, 444–487. [Google Scholar]
- Hossain, L.; Wu, A. Communications network centrality correlates to organizational coordination. Int. J. Proj. Manag. 2009, 27, 795–811. [Google Scholar] [CrossRef]
- Pekericli, M.K.; Akinci, B.; Karaesmen, I. Modeling information dependencies in construction project network organizations. In Proceedings of the Fourth Joint International Symposium on Information Technology in civil Engineering, Nashville, TN, USA, 15–16 November 2003; pp. 1–13. [Google Scholar]
- Decker, C.; Hanley, N.; Czajkowski, M.; Morrison, T.A.; Keyyu, J.; Munishi, L.; Lankester, F.; Cleaveland, S. Predicting uptake of a malignant catarrhal fever vaccine by pastoralists in northern Tanzania: Opportunities for improving livelihoods and ecosystem health. Ecol. Econ. 2021, 190, 107189. [Google Scholar] [CrossRef]
- Pryke, S.D. Towards a social network theory of project governance. Constr. Manag. Econ. 2005, 23, 927–939. [Google Scholar] [CrossRef]
- Shlyakhto, E.; Ilin, I.; Iliashenko, O.; Karaptan, D.; Tick, A. Digital Platforms as a Key Factor of the Medical Organizations Activities Development. Lect. Notes Netw. Syst. 2022, 387, 327–343. [Google Scholar] [CrossRef]
- Ilin, I.V.; Levina, A.I.; Dubgorn, A.S.; Abran, A. Investment models for enterprise architecture (EA) and IT architecture projects within the open innovation concept. J. Open Innov. Technol. Mark. Complex. 2021, 7, 69. [Google Scholar] [CrossRef]
- Kliem, R.L.; Ludin, I.S.; Robertso, K.L. Project Management Methodology: A Practical Guide for the Next Millennium; CRC Press: New York, NY, USA, 1997; pp. 86–98. [Google Scholar]
- Ilin, I.; Levina, A.; Frolov, K. Innovative Ecosystem Model of Vaccine Lifecycle Management. J. Open Innov. Technol. Mark. Complex. 2022, 8, 5–10. [Google Scholar] [CrossRef]
- Ilin, I.; Levina, A.; Iliashenko, V. Innovation Hub and Its IT Support: Architecture Model. Lect. Notes Inf. Syst. Organ. 2022, 53, 49–67. [Google Scholar] [CrossRef]
- Cross, R.; Rebele, R.; Grant, A. Collaborative Overload. Harv. Bus. Rev. 2016, 94, 74–79. [Google Scholar]
- Jarrett, S.; Wilmansyah, T.; Bramanti, Y.; Alitamsar, H.; Alamsyah, D.; Krishnamurthy, K.R.; Yang, L.; Pagliusi, S. The role of manufacturers in the implementation of global traceability standards in the supply chain to combat vaccine counterfeiting and enhance safety monitoring. Vaccine 2020, 38, 8318–8325. [Google Scholar] [CrossRef]
- Krackhardt, D.; Hanson, J.R. Informal networks: The company behind the charts. Harv. Bus. Rev. 1993, 71, 104–111. [Google Scholar] [PubMed]
- Otte, E.; Rousseau, R. Social network analysis: A powerful strategy, also for the information sciences. J. Inf. Sci. 2002, 28, 441–453. [Google Scholar] [CrossRef]
- Ilin, I.V.; Koposov, V.I.; Levina, A.I. Model of asset portfolio improvement in structured investment products. Life Sci. J. 2014, 11, 265–269. [Google Scholar] [CrossRef]
- Titov, S.A. The study of the relationship between the structure of intra-project communications and the effectiveness of innovative projects using the analysis of social networks. Cloud Sci. 2014, 1, 665–695. [Google Scholar]
- Winch, G.; Usmani, A.; Edkins, F. Towards total project quality: A gap analysis approach. Constr. Manag. Econ. 1998, 16, 193–207. [Google Scholar] [CrossRef]
- Lock, D. Project Management, 9th ed.; Gower Publishing Limited: Aldershot, UK, 2007; pp. 67–78. [Google Scholar]
- Ghosh, S.; Forrest, D.; Di Netta, T.; Wolfe, B.; Lambertet, D.C. Enhance PMBOK® by Comparing it with P2M, ICB, PRINCE2, APM and Scrum Project Management Standards. PM World Today 2012, 14, 1–77. [Google Scholar]
- Hossain, L. Effect of organisational position and network centrality on project coordination. Int. J. Proj. Manag. 2009, 27, 680–689. [Google Scholar] [CrossRef]
- Ilin, I.; Iliashenko, V.M.; Dubgorn, A.; Esser, M. Critical Factors and Challenges of Healthcare Digital Transformation. In Studies on Entrepreneurship, Structural Change and Industrial Dynamics; Springer: Berlin/Heidelberg, Germany, 2022; pp. 205–220. [Google Scholar]
- Chaddock, C. The external malleolar sign. Interstate Med. J. 1911, 18, 1026–1038. [Google Scholar]
- Osterwalder, A.; Pigneur, Y.; Bernarda, G.; Smith, A. Value Proposition Design: How to Create Products and Services Customers Want; Wiley & Sons, Inc.: Hoboken, NJ, USA, 2015; p. 320. [Google Scholar]
- Osterwalder, A.; Pigneur, Y. Business Model Generation: A Handbook for Visionaries, Game Changers, and Challengers; Wiley & Sons, Inc.: Hoboken, NJ, USA, 2013; p. 288. [Google Scholar]
- Hamel, G.; Prahalad, C.; Thomas, H.; O’Neal, D. Strategic Flexibility; Piter Publishing House: Saint-Petersburg, Russia, 2005; p. 384. [Google Scholar]
- Koptelov, A. Management of Business Processes in Russia. Available online: https://koptelov.info/kniga-upravlenie-biznes-protsessami/ (accessed on 15 January 2023).
- Repin, V. Process Approach to Management. In Modeling of Business Processes; Mann-Ivanov-Ferber: Moscow, Russia, 2013; p. 544. [Google Scholar]




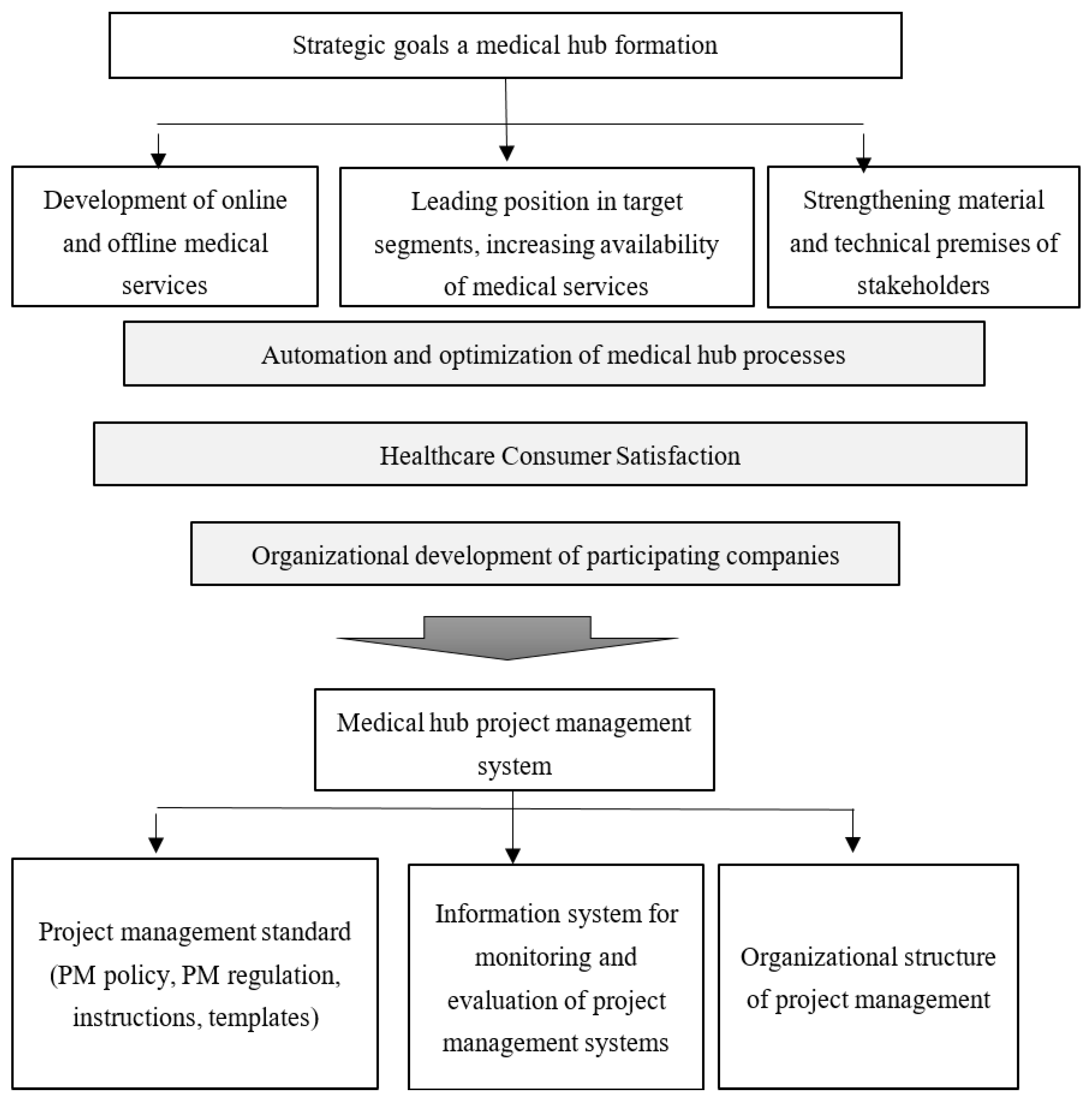



| Number of Vertices | Average Degree | Density | Centrality by Degree | Centrality by Proximity | Centrality by Mediation | Max. Click | Diameter | Clustering of Networks | K-Cores | |
|---|---|---|---|---|---|---|---|---|---|---|
| G1 | 14 | 3.285714 | 0.252747 | 0.153846 | 0.236272 | 0.149244 | 3 | 4 | 0.316667 | 2 |
| G2 | 18 | 2.666687 | 0.156863 | 0.154412 | 0.236166 | 0.265552 | 3 | 7 | 0.137037 | 3 |
| G3 | 11 | 7.090909 | 0.709091 | 0.233333 | 0.297580 | 0.033937 | 5 | 2 | 0.695455 | 5 |
| G4 | 10 | 2.800000 | 0.311111 | 0.722222 | 0.707302 | 0.515432 | 3 | 3 | 0.541657 | 2 |
| G5 | 11 | 3.454545 | 0.345455 | 0.188889 | 0.235913 | 0.160926 | 3 | 3 | 0.266667 | 2 |
| G6 | 12 | 2.833333 | 0.257578 | 0.236364 | 0.334830 | 0.274380 | 3 | 4 | 0.211111 | 2 |
| G7 | 10 | 3.200000 | 0.355558 | 0.250000 | 0.281675 | 0.249486 | 3 | 3 | 0.250000 | 2 |
| G8 | 16 | 3.333333 | 0.238085 | 0.919780 | 0.236433 | 0.161041 | 3 | 4 | 0.164444 | 2 |
| G9 | 14 | 4.000000 | 0.307692 | 0.179407 | 0.246911 | 0.123356 | 3 | 4 | 0.264266 | 3 |
| G10 | 9 | 5.777778 | 0.722222 | 0.357143 | 0.494589 | 0.080580 | 5 | 2 | 0.761905 | 4 |
| G11 | 10 | 3.400000 | 0.377778 | 0.666666 | 0.182893 | 0.189300 | 3 | 4 | 0.220000 | 3 |
| G12 | 10 | 3.090909 | 0.309091 | 0.233333 | 0.238305 | 0.179830 | 3 | 4 | 0.324242 | 2 |
| G13 | 11 | 3.636361 | 0.363636 | 0.288889 | 0.325007 | 0.134630 | 3 | 3 | 0.318182 | 3 |
| G14 | 12 | 3.83333 | 0.348485 | 0.345455 | 0.390876 | 0.231405 | 4 | 3 | 0.600000 | 3 |
| G15 | 13 | 4.153846 | 0.346154 | 0.181818 | 0.191651 | 0.102553 | 4 | 4 | 0.330769 | 3 |
| G16 | 13 | 3.500000 | 0.318182 | 0.381818 | 0.422747 | 0.273719 | 3 | 4 | 0.298810 | 3 |
| G17 | 8 | 4.133333 | 0.295238 | 0.318601 | 0.407802 | 0.242487 | 4 | 4 | 0.243651 | 3 |
| G18 | 15 | 2.750000 | 0.395827 | 0.238095 | 0.288357 | 0.319728 | 3 | 3 | 0.291667 | 2 |
| G19 | 17 | 4.588235 | 0.286765 | 0.241667 | 0.196923 | 0.149053 | 4 | 4 | 0.327731 | 3 |
| G20 | 13 | 3.384615 | 0.282051 | 0.159091 | 0.242684 | 0.173632 | 3 | 4 | 0.269231 | 3 |
| Number of Vertices | Average Degree | Density | Centrality by Degree | Centrality by Proximity | Centrality by Mediation | Max. Click | Diameter | Network Clustering | K-Cores | |
|---|---|---|---|---|---|---|---|---|---|---|
| Budget | 0.29 | −0.25 | −0.28 | 0.26 | 0.25 | 0.17 | −0.26 | −0.019 | 0.0078 | −0.37 |
| Deadlines | −0.23 | 0.57 | 0.54 | −0.43 | −0.3 | –0.7 | 0.45 | −0.28 | 0.34 | 0.42 |
| Customer satisfaction | 0.39 | −0.53 | −0.51 | −0.12 | −0.11 | 0.36 | −0.38 | 0.48 | −0.44 | −0.27 |
| Communication level | −0.074 | 0.14 | 0.026 | −0.17 | −0.062 | –0.011 | 0.16 | 0.11 | −0.067 | 0.19 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ilin, I.; Voronova, O.; Pavlov, D.; Kochkarov, A.; Tick, A.; Khusainov, B. System of Project Management at a Medical Hub as an Instrument for Implementation of Open Innovation. Systems 2023, 11, 182. https://doi.org/10.3390/systems11040182
Ilin I, Voronova O, Pavlov D, Kochkarov A, Tick A, Khusainov B. System of Project Management at a Medical Hub as an Instrument for Implementation of Open Innovation. Systems. 2023; 11(4):182. https://doi.org/10.3390/systems11040182
Chicago/Turabian StyleIlin, Igor, Olga Voronova, Dmitriy Pavlov, Azret Kochkarov, Andrea Tick, and Bulat Khusainov. 2023. "System of Project Management at a Medical Hub as an Instrument for Implementation of Open Innovation" Systems 11, no. 4: 182. https://doi.org/10.3390/systems11040182
APA StyleIlin, I., Voronova, O., Pavlov, D., Kochkarov, A., Tick, A., & Khusainov, B. (2023). System of Project Management at a Medical Hub as an Instrument for Implementation of Open Innovation. Systems, 11(4), 182. https://doi.org/10.3390/systems11040182