Relationship between Risk Perception, Emotion, and Coping Behavior during Public Health Emergencies: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
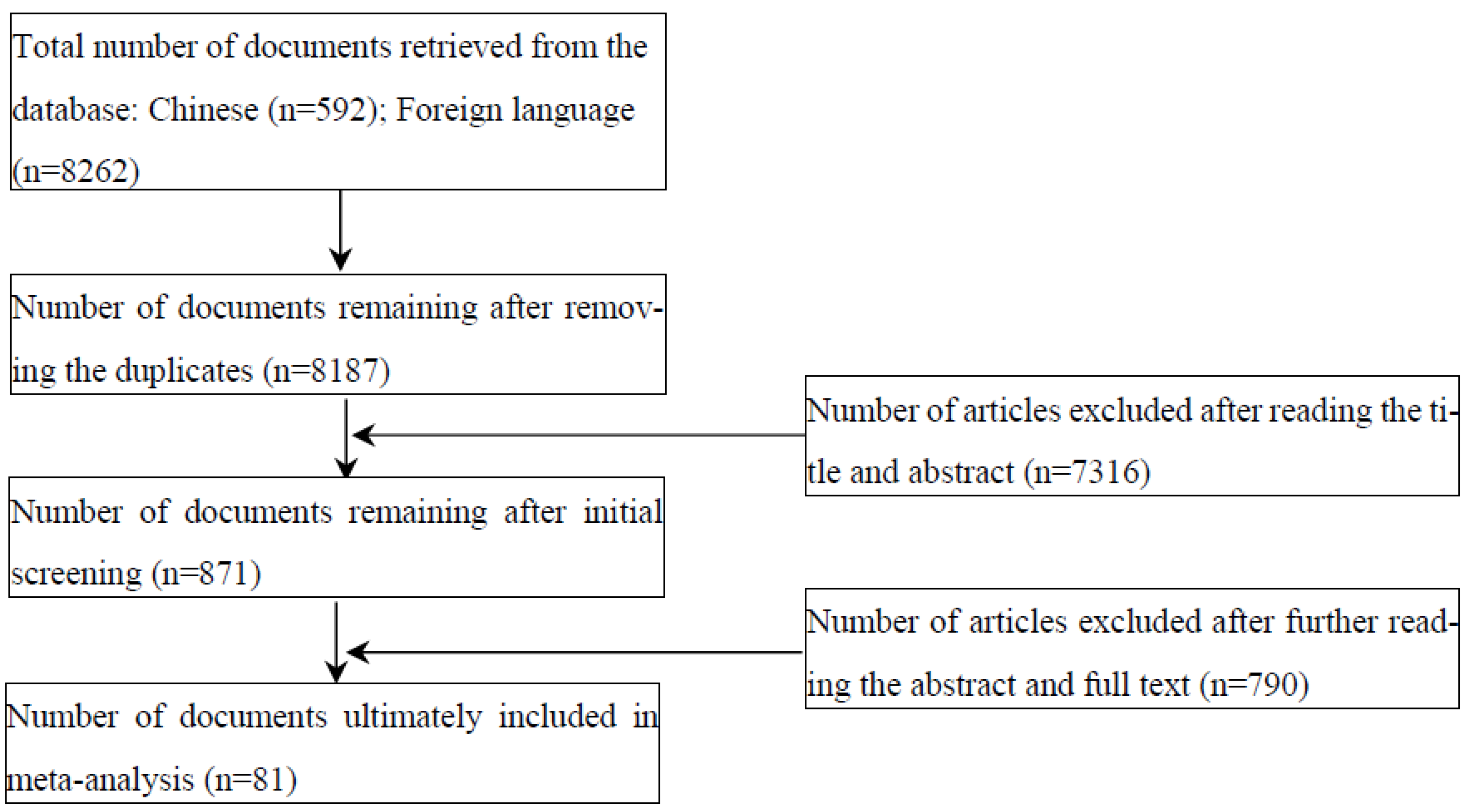
2.1. Identification of Studies
2.2. Inclusion and Exclusion Criteria
2.3. Literature Coding Procedure
2.4. Statistical Analysis
2.5. Data Analysis Procedures
3. Results
3.1. Basic Characteristics of the Included Literature
3.2. Main Effects Test
3.3. Publication Bias Test
3.4. Sensitivity Analyses
4. Discussion
4.1. Theoretical and Practical Implications
4.2. Strengths
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Msemburi, W.; Karlinsky, A.; Knutson, V.; Aleshin-Guendel, S.; Chatterji, S.; Wakefield, J. The WHO Estimates of Excess Mortality Associated with the COVID-19 Pandemic. Nature 2023, 613, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Dawood, F.S.; Iuliano, A.D.; Reed, C.; Meltzer, M.I.; Shay, D.K.; Cheng, P.-Y.; Bandaranayake, D.; Breiman, R.F.; Brooks, W.A.; Buchy, P.; et al. Estimated Global Mortality Associated with the First 12 Months of 2009 Pandemic Influenza A H1N1 Virus Circulation: A Modelling Study. Lancet Infect. Dis. 2012, 12, 687–695. [Google Scholar] [CrossRef] [PubMed]
- Wang, M. Evolution of management of emergency protective materials for mass panic in the context of public health emergencie. Oper. Res. Trans. 2023, 27, 30–42. [Google Scholar]
- Xi, J.; Wang, Y.; Ju, K. Psychological intervention in major public health emergencies from the perspective of positive psychology. J. Cap. Norm. Univ. 2022, 50, 181–187. [Google Scholar]
- Zhao, G.; Wang, Y.G.; Wang, Y.Q.; Cao, R.F.; Fu, S.F. Psychological Crisis Intervention in Disasters: Comment on Psychiatric View. Adv. Psychol. Sci. 2009, 17, 489–494. [Google Scholar]
- Shi, K. Research and Thinking on Socio-psychological Early Warning System of Disaster and Major Events in China. Manag. Rev. 2003, 15, 18–22. [Google Scholar]
- Zhang, N.; Zhang, S.W. Emergent Management Strategies during Public Health Emergency: Perspectives from Behavioral Sciences. J. Comp. Econ. Soc. Syst. 2020, 36, 25–34. [Google Scholar]
- Brug, J.; Oenema, A.; Ferreira, I. Theory, evidence and Intervention Mapping to improve behavior nutrition and physical activity interventions. Int. J. Behav. Nutr. Phy. 2005, 2, 2. [Google Scholar] [CrossRef]
- Brug, J.; Aro, A.R.; Richardus, J.H. Risk Perceptions and Behaviour: Towards Pandemic Control of Emerging Infectious Diseases: International Research on Risk Perception in the Control of Emerging Infectious Diseases. Int. J. Behav. Med. 2009, 16, 3–6. [Google Scholar] [CrossRef]
- Dolan, R.J. Emotion, Cognition, and Behavior. Science 2002, 298, 1191–1194. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behaviour: Reactions and reflections. Psychol. Health 2011, 26, 1113–1127. [Google Scholar] [CrossRef]
- Yıldırım, M.; Geçer, E.; Akgü, Ö. The impacts of vulnerability, perceived risk, and fear on preventive behaviours against COVID-19. Psychol. Health Med. 2021, 26, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Duong, H.T.; Nguyen, H.T. Media exposure and intentions to wear face masks in the early stages of the COVID-19 outbreak: The mediating role of negative emotions and risk perception. Atl. J. Commun. 2021, 30, 467–480. [Google Scholar] [CrossRef]
- Zhang, W.; Li, L.; Mou, J.; Zhang, M.; Cheng, X.; Xia, H. Mediating Effects of Attitudes, Risk Perceptions, and Negative Emotions on Coping Behaviors: Evidence From a Survey of Older Chinese Adults. J. Organ. End User Com. 2022, 34, 1–22. [Google Scholar] [CrossRef]
- Teasdale, E.; Santer, M.; Geraghty, A.W.A.; Little, P.; Yardley, L. Public Perceptions of Non-Pharmaceutical Interventions for Reducing Transmission of Respiratory Infection: Systematic Review and Synthesis of Qualitative Studies. BMC Public Health 2014, 14, 589. [Google Scholar] [CrossRef]
- Parsons, J.E.; Newby, K.V.; French, D.P. Do Interventions Containing Risk Messages Increase Risk Appraisal and the Subsequent Vaccination Intentions and Uptake?—A Systematic Review and Meta-Analysis. Br. J. Health Psychol. 2018, 23, 1084–1110. [Google Scholar] [CrossRef]
- Liu, M.; Zhang, H.; Huang, H. Media Exposure to COVID-19 Information, Risk Perception, Social and Geographical Proximity, and Self-Rated Anxiety in China. BMC Public Health 2020, 20, 1649. [Google Scholar] [CrossRef]
- Mahmood, S.; Hussain, T.; Mahmood, F.; Ahmad, M.; Majeed, A.; Beg, B.M.; Areej, S. Attitude, Perception, and Knowledge of COVID-19 Among General Public in Pakistan. Front. Public Health 2020, 8, 602434. [Google Scholar] [CrossRef]
- Li, J.B.; Yang, A.; Dou, K.; Wang, L.X.; Zhang, M.C.; Lin, X.Q. Chinese public’s knowledge, perceived severity, and perceived controllability of COVID-19 and their associations with emotional and behavioural reactions, social participation, and precautionary behaviour: A national survey. BMC Public Health 2020, 20, 1589. [Google Scholar] [CrossRef]
- Cheng, C.; Espanha, R. Association of Sina-microblog Use with Knowledge, Attitude and Practices Towards COVID-19 Control in China. Open Access J. Public Health 2021, 4, 7. [Google Scholar]
- Lyu, X.; Hu, J.; Xu, X.; Xianyu, Y.; Dong, W. Factors influencing risk perception and nosocomial infection prevention practices of frontline nurses during the COVID-19 pandemic. BMC Nurs. 2021, 20, 78. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.P.; Shi, K. Comparative Study on Risk Perception and Coping Behavior of Beijing Residents During SARS Period. Chin. J. Clin. Psychol. 2004, 12, 293–295+298. [Google Scholar]
- Kim, Y.; Zhong, W.; Jehn, M.; Walsh, L. Public Risk Perceptions and Preventive Behaviors During the 2009 H1N1 Influenza Pandemic. Disaster Med. Public 2015, 9, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.N.; Zhang, Y.C.; Wu, R.K.; Li, B.; Li, C.W.; Yu, B.T.; Zhang, Y.L. A study of self-precaution against the background of the COVID-19 pandemic from the perspective of risk perception attitude theory and social support. BMC Public Health 2021, 21, 1527. [Google Scholar] [CrossRef]
- Levkovich, I.; Shinan-Altman, S. The Impact of Gender on Emotional Reactions, Perceived Susceptibility and Perceived Knowledge about COVID-19 among the Israeli Public. Int. Health 2021, 13, 555–561. [Google Scholar] [CrossRef]
- Shen, F.; Min, C.; Lu, Y.; Chu, Y. The Effect of Cognition and Affect on Preventive Behaviors during the COVID-19 Pandemic: A Cross-Sectional Study in China. BMC Public Health 2021, 21, 722. [Google Scholar] [CrossRef]
- Hedges, L.V.; Vevea, J.L. Fixed- and Random-Effects Models in Meta-Analysis. Psychol. Methods 1998, 3, 486–504. [Google Scholar] [CrossRef]
- Rupinski, M.T.; Dunlap, W.P. Approximating Pearson product-moment correlations from Kendall’s tau and Spearman’s rho. Educ. Psychol. Meas. 1996, 56, 419–429. [Google Scholar] [CrossRef]
- Huedo-Medina, T.B.; Sánchez-Meca, J.; Marín-Martínez, F.; Botella, J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index. Psychol. Methods 2006, 11, 193–206. [Google Scholar] [CrossRef]
- Lipsey, M.W.; Wilson, D.B. The way in which intervention studies have “personality” and why it is important to meta-analysis. Eval. Health Prof. 2001, 24, 236–254. [Google Scholar]
- Yıldırım, M.; Güler, A. COVID-19 severity, self-efficacy, knowledge, preventive behaviors, and mental health in Turkey. Death Stud. 2022, 46, 979–986. [Google Scholar] [CrossRef]
- Song, E.; Lee, J.E.; Kwon, S. Effect of Public Empathy with Infection-Control Guidelines on Infection-Prevention Attitudes and Behaviors: Based on the Case of COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 13408. [Google Scholar] [CrossRef] [PubMed]
- Alijanzadeh, M.; Ahorsu, D.K.; Alimoradi, Z.; Mahmoudi, N.; Griffiths, M.D.; Lin, C.Y.; Liu, H.K.; Pakpour, A.H. Fear of COVID-19 and Trust in the Healthcare System Mediates the Association between Individual’s Risk Perception and Preventive COVID-19 Behaviours among Iranians. Int. J. Environ. Res. Public Health 2021, 18, 12146. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.; Chen, J.; Chow, K.M.; Law, B.M.H.; Chan, D.N.S.; So, W.K.W.; Leung, A.W.Y.; Chan, C.W.H. Knowledge, Attitudes and Practices Towards COVID-19 Amongst Ethnic Minorities in Hong Kong. Int. J. Environ. Res. Public Health 2020, 17, 7878. [Google Scholar] [CrossRef] [PubMed]
- Mirakzadeh, A.A.; Karamian, F.; Khosravi, E.; Parvin, F. Analysis of Preventive Behaviors of Rural Tourism Hosts in the Face of COVID-19 Pandemic: Application of Health Belief Model. Front. Public Health 2021, 9, 793173. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Rao, N.; Han, B. Pathways Improving Compliance with Preventive Behaviors during the Remission Period of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 3512. [Google Scholar] [CrossRef] [PubMed]
- Mihelič, A.; Jelovčan, L.; Prislan, K. Internal and external drivers for compliance with the COVID-19 preventive measures in Slovenia: The view from general deterrence and protection motivation. PLoS ONE 2021, 16, e0259675. [Google Scholar] [CrossRef] [PubMed]
- Shabu, S.A.; M-Amin, K.; Mahmood, K.I.; Shabila, N.P. Risk Perception and Behavioral Response to COVID-19: A Survey of University Students and Staff in the Iraqi Kurdistan Region. Soc. Work Public Health 2021, 36, 474–485. [Google Scholar] [CrossRef]
- Rayani, M.; Rayani, S.; Najafi-Sharjabad, F. COVID-19-related knowledge, risk perception, information seeking, and adherence to preventive behaviors among undergraduate students, southern Iran. Environ. Sci. Pollut. Res. 2021, 28, 59953–59962. [Google Scholar] [CrossRef]
- Alagili, D.E.; Bamashmous, M. The Health Belief Model as an explanatory framework for COVID-19 prevention practices. J. Infect. Public Health 2021, 14, 1398–1403. [Google Scholar] [CrossRef]
- Yazdanpanah, M.; Abadi, B.; Komendantova, N.; Zobeidi, T.; Sieber, S. Some at Risk for COVID-19 Are Reluctant to Take Precautions, but Others Are Not: A Case From Rural in Southern Iran. Front. Public Health 2020, 8, 562300. [Google Scholar] [CrossRef] [PubMed]
- Fathian-Dastgerdi, Z.; Khoshgoftar, M.; Tavakoli, B.; Jaleh, M. Factors associated with preventive behaviors of COVID-19 among adolescents: Applying the health belief model. Res. Soc. Admin. Pharm. 2021, 17, 1786–1790. [Google Scholar] [CrossRef] [PubMed]
- Iorfa, S.K.; Ottu, I.F.A.; Oguntayo, R.; Ayandele, O.; Kolawole, S.O.; Gandi, J.C.; Dangiwa, A.L.; Olapegba, P.O. COVID-19 Knowledge, Risk Perception, and Precautionary Behavior Among Nigerians: A Moderated Mediation Approach. Front. Psychol. 2020, 11, 566773. [Google Scholar] [CrossRef] [PubMed]
- Ezati Rad, R.; Mohseni, S.; Kamalzadeh Takhti, H.; Hassani Azad, M.; Shahabi, N.; Aghamolaei, T.; Norozian, F. Application of the protection motivation theory for predicting COVID-19 preventive behaviors in Hormozgan, Iran: A cross-sectional study. BMC Public Health 2021, 21, 466. [Google Scholar] [CrossRef] [PubMed]
- Tajeri Moghadam, M.; Zobeidi, T.; Sieber, S.; Löhr, K. Investigating the Adoption of Precautionary Behaviors Among Young Rural Adults in South Iran During COVID-19. Front. Public Health 2022, 10, 787929. [Google Scholar] [CrossRef]
- Xie, K.; Liang, B.; Dulebenets, M.A.; Mei, Y. The Impact of Risk Perception on Social Distancing during the COVID-19 Pandemic in China. Int. J. Environ. Res. Public Health 2020, 17, 6256. [Google Scholar] [CrossRef]
- Pilch, I.; Wardawy, P.; Probierz, E. The predictors of adaptive and maladaptive coping behavior during the COVID-19 pandemic: The Protection Motivation Theory and the Big Five personality traits. PLoS ONE 2021, 16, e0258606. [Google Scholar] [CrossRef]
- Jadil, Y.; Ouzir, M. Exploring the predictors of health-protective behavior during the COVID-19 pandemic: A multi-country comparison. Environ. Res. 2021, 199, 111376. [Google Scholar] [CrossRef]
- Rabin, C.; Dutra, S. Predicting engagement in behaviors to reduce the spread of COVID-19: The roles of the health belief model and political party affiliation. Psychol. Health Med. 2022, 27, 379–388. [Google Scholar] [CrossRef]
- Batra, K.; Urankar, Y.; Batra, R.; Gomes, A.F.; Kaurani, P. Knowledge, Protective Behaviors and Risk Perception of COVID-19 among Dental Students in India: A Cross-Sectional Analysis. Healthcare 2021, 9, 574. [Google Scholar] [CrossRef]
- Shi, G.; Zhong, X.; He, W.; Liu, H.; Liu, X.; Ma, M. Factors influencing protective behavior in the post-COVID-19 period in China: A cross-sectional study. Environ. Health Prev. Med. 2021, 26, 95. [Google Scholar] [CrossRef] [PubMed]
- Karimy, M.; Bastami, F.; Sharifat, R.; Heydarabadi, A.B.; Hatamzadeh, N.; Pakpour, A.H.; Cheraghian, B.; Zamani-Alavijeh, F.; Jasemzadeh, M.; Araban, M. Factors related to preventive COVID-19 behaviors using health belief model among general population: A cross-sectional study in Iran. BMC Public Health 2021, 21, 1934. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.S.; Jeon, M.J.; Lim, M.H. A study on knowledge of influenza A(H1N1) and preventive behavior in the midst of the spread of the flu. J. Korean Soc. Dent. Hyg. 2010, 10, 567–576. [Google Scholar]
- Choi, J.S.; Kim, K.M. Infection-control knowledge, attitude, practice, and risk perception of occupational exposure to Zika virus among nursing students in Korea: A cross-sectional survey. J. Infect. Public Health 2018, 11, 840–844. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Wang, Q.; Chen, H.L.; Jiang, Y.H. Relationship between Risk Perception and Unintentional/Intentional Rumor Spread Behavior during The COVID-19 Pneumonia Outbreak in China: The Mediating Role of Negative Emotion. Chin. J. Clin. Psychol. 2020, 28, 734–738. [Google Scholar]
- Tang, X.M.; Lai, S.Q. Research on the Online Health Rumor Forwarding in Public Health and Safety Incidents—The Interaction of Perceived Risk and Information Credibility. J. Intell. 2021, 40, 101–107. [Google Scholar]
- Alhaimer, R. The health belief model: Evaluating governmental public health messages on social media aimed at preventing a COVID-19 epidemic in Kuwait. Cogent. Bus. Manag. 2022, 9, 2031682. [Google Scholar] [CrossRef]
- Mehanna, A.; Elhadi, Y.A.M.; Lucero-Prisno Iii, D.E. Public willingness to adhere to COVID-19 precautionary measures in Sudan: An application of the Health Belief Model. Pan Afr. Med. J. 2021, 39, 135. [Google Scholar] [CrossRef]
- Arceo, E.; Jurado, J.E.; Cortez, L.A.; Sibug, N.; Sarmiento, G.L.; Lawingco, A.C.; Carbungco, C.; Tiongco, R.E. Understanding COVID-19 preventive behavior: An application of the health belief model in the Philippine setting. J. Educ. Health Promot. 2021, 10, 228. [Google Scholar]
- Bagherzadeh, M.; Salehi, L.; Mahmoodi, Z. Investigating preventive health behaviors against COVID-19 in elementary school students’ parents: A cross-sectional study from Tehran—Capital of Iran. J. Educ. Health Promot. 2021, 10, 435. [Google Scholar]
- Zhang, Y.; Young, L.S. A Study on the Factors Influencing the Intention to Continue COVID-19 Preventive Behavior: Focusing on the Health Belief Model (HBM), Media/interpersonal Information Exposure, Negative Emotions, and Interdependent Self-construal. J. Speech Media Commun. Res. 2021, 20, 315–348. [Google Scholar] [CrossRef]
- Grano, C.; Singh, S.C.; Di, P.A. Predictors of protective behaviours during the Italian COVID-19 pandemic: An application of protection motivation theory. Psychol. Health 2022, 37, 1584–1604. [Google Scholar] [CrossRef] [PubMed]
- Kurnia, A.D.; Masruroh, N.L.; Melizza, N.; Rofi’i, A.Y. Factors associated with preventive behaviors of COVID-19 among Indonesian nursing students: Application of Health Belief Model. Russ. Open Med. J. 2021, 10, e0201. [Google Scholar] [CrossRef]
- Kim, S.J.; Kim, E.Y.; Yang, H.R.; Chae, Y.J. Gyeongnam Inhabitants’ Effects of COVID-19 Infection Prevention Behavior: Focus on Anxiety and Health Belief. J. Korean Public Health Nurs. 2021, 35, 19–32. [Google Scholar]
- DeDonno, M.A.; Longo, J.; Levy, X.; Morris, J.D. Perceived Susceptibility and Severity of COVID-19 on Prevention Practices, Early in the Pandemic in the State of Florida. J. Community Health 2022, 47, 627–634. [Google Scholar] [CrossRef]
- Song, H.S.; Bang, S.H.; Shim, G.S.; Kim, E.M. An Analysis of COVID-19 Prevention Behaviors between Firefighters and Maritime Police Officers. J. Korea Soc. Comput. Inf. 2021, 26, 213–220. [Google Scholar]
- Magano, J.; Vidal, D.G.; Sousa, H.F.P.e.; Dinis, M.A.P.; Leite, Â. Psychological Factors Explaining Perceived Impact of COVID-19 on Travel. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 1120–1133. [Google Scholar] [CrossRef]
- Idrees, M.; Asif, M.; Ghazal, S. Effect of Risk Perceptions, Fear and myths about COVID-19 infection susceptibility on Protective behaviors in Pakistan. Asean J. Psychiatr. 2022, 23, 1–8. [Google Scholar]
- Elsayed, E.A. Impact of COVID-19 risk perception on compliance with preventive measures among adult Egyptians. Med. Sci. 2022, 26, ms65e1826. [Google Scholar] [CrossRef]
- Feng, Y.; Tong, Q. Exploring the Mediating Role of Situation Awareness and Crisis Emotions Between Social Media Use and COVID-19 Protective Behaviors: Cross-Sectional Study. Front. Public Health. 2022, 10, 793033. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhou, R. Promoting social distancing and preventing panic buying during the epidemic of COVID-19: The contributions of people’s psychological and behavioural factors. J. Public Health 2023, 31, 187–201. [Google Scholar] [CrossRef] [PubMed]
- Güngör, A.; Brahim Sarı, H.; Asıcı, E. Health Anxiety in the Early Phase of COVID-19 Outbreak in Turkey: Investigation of Predictive Variables. Ansiedad Estrés 2021, 27, 74–80. [Google Scholar] [CrossRef]
- Das, D.; Pal, S. Do Socio-Demographic and Corona Reassurance-Seeking Behaviour Predict Corona Anxiety?—A study among Indian population. Asia-Pac. J. Health Manag. 2021, 16, 86–93. [Google Scholar] [CrossRef]
- Jouybari, T.A.; Hatamzadeh, N.; Fattahi, M.; Gharibnavaz, H.; Khashij, S.; Mahboubi, M. Cognitive Determinants of Influenza Preventive Behaviors among Students: An Application of the Health Belief Model (HBM). Int. J. Pediatr. 2018, 6, 7833–7841. [Google Scholar]
- Sadeghi, R.; Khanjani, N.; Naghibzadeh-Tahami, A.; Kakolaki, Z.K. Education of Iranian Pregnant Women About Prevention of Influenza A. Int. J. Women’s Health Reprod. Sci. 2017, 6, 321–327. [Google Scholar] [CrossRef]
- Zhang, Y.; Yang, H.; Cheng, P.; Luqman, A. Predicting consumers’ intention to consume poultry during an H7N9 emergency: An extension of the theory of planned behavior model. Hum. Ecol. Risk Assess. 2020, 26, 190–211. [Google Scholar] [CrossRef]
- Gutiérrez-Doña, B.; Renner, B.; Reuter, T.; Giese, H.; Schubring, D. Health Behavior Education, e-research and a (H1N1) Influenza (Swine Flu): Bridging the Gap between Intentions and Health Behavior Change. Procedia-Soc. Behav. Sci. 2012, 46, 2782–2795. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.Y.; Tang, C.S.K. Practice of habitual and volitional health behaviors to prevent severe acute respiratory syndrome among Chinese adolescents in Hong Kong. J. Adolesc. Health 2005, 36, 193–200. [Google Scholar] [CrossRef]
- Karademas, E.C.; Bati, A.; Karkania, V.; Georgiou, V.; Sofokleous, S. The association between Pandemic Influenza A (H1N1) public perceptions and reactions: A prospective study. J. Health Psychol. 2013, 18, 419–428. [Google Scholar] [CrossRef]
- Li, P.P.; Zhong, F. A Study on the Correlation Between Media Usage Frequency and Audiences’ Risk Perception, Emotion and Behavior. Front. Psychol. 2022, 12, 822300. [Google Scholar] [CrossRef]
- Bults, M.; Beaujean, D.; Wijkmans, C.; Richardus, J.H.; Voeten, H. Q fever in the Netherlands: Public perceptions and behavioral responses in three different epidemiological regions: A follow-up study. BMC Public Health 2014, 14, 263. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Choi, J.S. Middle East respiratory syndrome-related knowledge, preventive behaviours and risk perception among nursing students during outbreak. J. Clin. Nurs. 2016, 25, 2542–2549. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.M.; Kim, J.Y. Predictors of Respiratory Infection Prevention Behavoirs of Nursing College Students. J. Korea Acad.-Ind. Cooper. Soc. 2022, 23, 134–145. [Google Scholar]
- Borges, J.; Byrne, M. Investigating COVID-19 risk perception and preventive behaviours in third-level students in Ireland. Acta Psychol. 2022, 224, 103535. [Google Scholar] [CrossRef] [PubMed]
- Kwak, S.J.; Kim, N.Y. Media Dependence of Nursing Students on COVID-19-Related Infection Prevention Behavior: Mediating Effect of Risk Perception. Korean J. Adul. Nurs. 2021, 33, 630–638. [Google Scholar] [CrossRef]
- Kim, H.; Cheon, E.Y.; Yoo, J.H. A Study on the Relationship between Knowledge, Risk Perception, Preventive Health Behavior from Coronavirus disease-2019 in Nursing Students. J. Korea Acad.-Ind. Cooper. Soc. 2021, 22, 246–254. [Google Scholar]
- Lee, S.J.; Jin, X.; Lee, S. Factors Influencing COVID-19 Preventive Behaviors in Nursing Students: Knowledge, Risk Perception, Anxiety, and Depression. J. Korean Biol. Nurs. Sci. 2021, 23, 110–118. [Google Scholar] [CrossRef]
- Donizzetti, A.R.; Lagacé, M. COVID-19 and the Elderly’s Mental Illness: The Role of Risk Perception, Social Isolation, Loneliness and Ageism. Int. J. Environ. Res. Public Health 2022, 19, 4513. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.R.; Choi, E.Y.; Park, S.Y.; Kim, E.A. Factors Influencing Preventive Behavior against Coronavirus Disease 2019 (COVID-19) among Medically Inclined College Students. J. Korean Acad. Fund Nurs. 2020, 27, 428–437. [Google Scholar] [CrossRef]
- Kyung, L.H.; Kang, N.G.; Kim, S.H.; Kim, M.S.; Nam, Y.N.; Noh, S.H.; Lee, H.D.; Jung, D.U.; Joo, S.H.; Choi, S.R. Effect of nursing students’ knowledge of COVID-19 and risk perception on COVID-19 prevention behavior. J. Ind. Converg. 2021, 19, 29–137. [Google Scholar]
- Jeon, S.W.; Han, S.J. Factors Influencing Hospital Nurses’ COVID-19 Prevention Behaviors. J. Korea Converg. Soc. 2021, 12, 583–594. [Google Scholar]
- Zancu, S.A.; Măirean, C.; Diaconu-Gherasim, L.R. The longitudinal relation between time perspective and preventive behaviors during the COVID-19 pandemic: The mediating role of risk perception. Curr. Psychol. 2022, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Fu, H.; Wang, B. The Effect of Risk Perception on Anxiety in Emerging Adulthood Under the Local Outbreak of COVID-19: A Conditional Process Analysis. Front. Psychol. 2022, 13, 759510. [Google Scholar] [CrossRef] [PubMed]
- Jeong, Y.J.; Park, J.H.; Kim, H.S. Effects of Information Literacy, Risk Perception and Crisis Communication Related to COVID-19 on Preventive Behaviors of Nursing Students in Clinical Practice. J. Converge. Inf. Technol. 2022, 12, 66–74. [Google Scholar]
- Kim, Y.; Yoon, T.; Sohn, A. Effects of COVID-19 knowledge, risk perception, subjective norms, and perceived behavioral control on preventive action intentions and preventive action practices in college students. Korean J. Educ. Health Promot. 2021, 38, 25–36. [Google Scholar] [CrossRef]
- Jeon, E.B.; Baek, E.M.; Cho, S.I.; Jeong, Y. The Impact of Fear and Perception of Infection Risk on Depression among Service Workers during COVID-19. Korean J. Occup. Health Nurs. 2022, 31, 1–10. [Google Scholar]
- Park, M.; Chai, S. The Effects of COVID-19 Risk Information Seeking and Processing on its Preventive Behaviors and Information Sharing. J. Inf. Technol. Serv. 2020, 19, 65–81. [Google Scholar]
- Park, J.H.; Kim, J.H.; Lee, H.J.; Kang, P. The Relationship of Anxiety, Risk Perception, Literacy, and Compliance of Preventive Behaviors during COVID-19 Pandemic in Nursing Students. J. Korean Appl. Sci. Technol. 2021, 38, 48–59. [Google Scholar]
- Lee, C.K.; Jung, E.K.; Kang, S.E.; Petrick, J.F.; Park, Y.N. Impact of perception of COVID-19 on NPI, job satisfaction, and customer orientation: Highlighting three types of NPIs for the airline industry. J. Air Transp. Manag. 2022, 100, 102191. [Google Scholar] [CrossRef]
- Lee, H.; Park, J.; Kim, J.; Kang, P. Factors Influencing University Students’ Infection Prevention Behaviors Compliance in the Early Stage of COVID-19. J. Korean Soc. Sch. Health 2021, 34, 190–199. [Google Scholar]
- Li, X.J.; Liu, Q.L. An Extended Model of Risk Transmission from the Perspective of Media Credibility—Based on the National Survey of COVID-19. Mod. Commun. 2021, 43, 33–40. [Google Scholar]
- Zhang, R.J.; Jiang, T.T.; Li, N. The negative psychology for the public in Zhejiang province during the epidemic of human H7N9 avian influenza. Chin. J. Prev. Med. 2015, 49, 1073–1079. [Google Scholar]
- Ayandele, O.; Ramos-Vera, C.A.; Iorfa, S.K.; Chovwen, C.O.; Olapegba, P.O. Exploring the Complex Pathways between the Fear of COVID-19 and Preventive Health Behavior among Nigerians: Mediation and Moderation Analyses. Am. J. Trop. Med. Hyg. 2021, 105, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Zickfeld, J.H.; Schubert, T.W.; Herting, A.K.; Grahe, J.; Faasse, K. Correlates of Health-Protective Behavior During the Initial Days of the COVID-19 Outbreak in Norway. Front. Psychol. 2020, 11, 564083. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, S.H.; Yu, R.H. Compliance of home quarantine protection and its effect on anxiety degree during the epidemic outbreak period of COVID-19. Chin. J. Control 2020, 19, 404–410. [Google Scholar]
- Zeidi, I.M.; Zeidi, B.M. Knowledge, Attitude, Fear, and Practice towards Coronavirus Disease-2019 Preventive Measures among Iranian Dentists. Iran. Red. Crescent. Me. 2021, 23, e778. [Google Scholar]
- Rosenthal, R. The file drawer problem and tolerance for null results. Psychol. Bull. 1979, 86, 638–641. [Google Scholar] [CrossRef]
- Egger, M.; Davey, S.G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ-Clin. Res. Ed. 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef]
- Patsopoulos, N.A.; Evangelou, E.; Ioannidis, J.P.A. Sensitivity of between-study heterogeneity in meta-analysis: Proposed metrics and empirical evaluation. Int. J. Epidemiol. 2008, 37, 1148–1157. [Google Scholar] [CrossRef]
- Shekriladze, I.; Javakhishvili, N.; Chkhaidze, N. Culture Related Factors May Shape Coping During Pandemics. Front. Psychol. 2021, 12, 634078. [Google Scholar] [CrossRef]
- Cho, H.; Lee, J.-S. The Influence of Self-Efficacy, Subjective Norms, and Risk Perception on Behavioral Intentions Related to the H1N1 Flu Pandemic: A Comparison between Korea and the US. Asian J. Soc. Psychol. 2015, 18, 311–324. [Google Scholar] [CrossRef]
- Kowalczyk, O.; Roszkowski, K.; Montane, X.; Pawliszak, W.; Tylkowski, B.; Bajek, A. Religion and Faith Perception in a Pandemic of COVID-19. J. Relig. Health 2020, 59, 2671–2677. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.M.; Stockman, J.K. Fear of COVID-19 and Prevention Behaviors: Cross-Lagged Panel Analysis. JMIR Form. Res. 2022, 6, e35730. [Google Scholar] [CrossRef] [PubMed]
- Cipolletta, S.; Andreghetti, G.R.; Mioni, G. Risk Perception towards COVID-19: A Systematic Review and Qualitative Synthesis. Int. J. Environ. Res. Public Health 2022, 19, 4649. [Google Scholar] [CrossRef]
- Fuentes, A.; Peterson, J.V. Social Media and Public Perception as Core Aspect of Public Health: The Cautionary Case of @realdonaldtrump and COVID-19. PLoS ONE 2021, 16, e0251179. [Google Scholar] [CrossRef]
- Abbas, J.; Wang, D.; Su, Z.; Ziapour, A. The Role of Social Media in the Advent of COVID-19 Pandemic: Crisis Management, Mental Health Challenges and Implications. Risk Manag. Healthc. Policy 2021, 14, 1917–1932. [Google Scholar] [CrossRef]
- Liu, Y.; Luo, D. The use of social media in public health emergencies and its impact on college students’ health behavior. New Media Res. 2021, 7, 19–24. [Google Scholar]
- Liu, F.; Chen, X.; Yuan, L. The relationship between risk perception and negative coping behaviors in public crisis events: Analysis of a moderated mediation model. Psychol. Mon. 2021, 16, 7–9+70. [Google Scholar]
- Mesquita, C.T.; Oliveira, A.; Seixas, F.L.; Paes, A. Infodemia, Fake News and Medicine: Science and The Quest for Truth. Int. J. Cardiovasc. Sci. 2020, 33, 203–205. [Google Scholar] [CrossRef]
- Zhang, L.; Li, H.; Chen, K. Effective Risk Communication for Public Health Emergency: Reflection on the COVID-19 (2019-NCoV) Outbreak in Wuhan, China. Healthcare 2020, 8, 64. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.D.; Zhang, A.H.; Feng, X.Q. Research progress on risk perception, emotion and behavior of the public under major emergencies. Chin. Nurs. Res. 2022, 36, 1803–1809. [Google Scholar]
- Brewer, N.T.; Chapman, G.B.; Gibbons, F.X.; Gerrard, M.; McCaul, K.D.; Weinstein, N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2007, 26, 136–145. [Google Scholar] [CrossRef] [PubMed]







| No. | Study Code No. | Location | Sample Size | Event | Subjects |
|---|---|---|---|---|---|
| 1 | Yildirim 2022 [31] | Turkey | 3190 | COVID-19 | The general public |
| 2 | Song 2021 [32] | Republic of Korea | 211 | COVID-19 | The general public |
| 3 | Alijanzadeh 2021 [33] | Iran | 3652 | COVID-19 | The general public |
| 4 | Wong 2020 [34] | China | 352 | COVID-19 | Hong Kong South Asians |
| 5 | Mirakzadeh2021 [35] | Iran | 80 | COVID-19 | Rural tourism operators |
| 6 | Wang 2021 [24] | China | 429 | COVID-19 | The general public |
| 7 | Levkovich 2021 [25] | Israel | 482 | COVID-19 | The general public |
| 8 | Wang 2021 [36] | China | 200 | COVID-19 | The general public |
| 9 | Mihelic 2021 [37] | Slovenia | 394 | COVID-19 | The general public |
| 10 | Shabu 2021 [38] | Iraq | 976 | COVID-19 | University teachers and students |
| 11 | Rayani 2021 [39] | Iran | 319 | COVID-19 | general student population |
| 12 | Alagili 2021 [40] | Saudi Arabia | 1027 | COVID-19 | The general public |
| 13 | Yazdanpanah 2020 [41] | Iran | 305 | COVID-19 | Rural youth |
| 14 | Fathian-Dastgerdi 2021 [42] | Iran | 797 | COVID-19 | Teenagers |
| 15 | Iorfa 2020 [43] | Nigeria | 890 | COVID-19 | The general public |
| 16 | Iorfa2 2020 [43] | Nigeria | 664 | COVID-19 | The general public |
| 17 | Rad 2021 [44] | Iran | 2032 | COVID-19 | The general public |
| 18 | Shen 2021 [26] | China | 3000 | COVID-19 | The general public |
| 19 | Moghadam 2022 [45] | Iran | 305 | COVID-19 | Rural adults |
| 20 | Xie 2020 [46] | China | 317 | COVID-19 | The general public |
| 21 | Yildirim2 2021 [12] | Turkey | 4536 | COVID-19 | The general public |
| 22 | Pilch 2021 [47] | Poland | 397 | COVID-19 | The general public |
| 23 | Jadil 2021 [48] | Morocco | 215 | COVID-19 | The general public |
| T | Jadil2 2021 [48] | India | 229 | COVID-19 | The general public |
| 25 | Rabin 2022 [49] | America | 186 | COVID-19 | The general public |
| 26 | Batra 2021 [50] | India | 381 | COVID-19 | Medical students |
| 27 | Shi 2021 [51] | China | 2830 | COVID-19 | The general public |
| 28 | Karimy 2021 [52] | Iran | 1090 | COVID-19 | The general public |
| 29 | Cui 2010 [53] | Republic of Korea | 484 | H1N1 | Medical students |
| 30 | Choi 2018 [54] | Republic of Korea | 249 | ZIKA | Medical students |
| 31 | Hu 2020 [55] | China | 1063 | COVID-19 | The general public |
| 32 | Tang 2021 [56] | China | 627 | Public health events | The general public |
| 33 | Alhaimer 2022 [57] | Kuwait | 746 | COVID-19 | The general public |
| 34 | Mehanna 2021 [58] | Sudan | 680 | COVID-19 | The general public |
| 35 | Arceo 2021 [59] | The Philippines | 304 | COVID-19 | The general public |
| 36 | Liu 2021 [13] | America | 590 | COVID-19 | The general public |
| 37 | Bagherzadeh 2021 [60] | Iran | 660 | COVID-19 | Parents of primary school students |
| 38 | Zhang 2021 [61] | Republic of Korea | 299 | COVID-19 | The general public |
| 39 | Grano 2022 [62] | Italy | 309 | COVID-19 | The general public |
| 40 | Grano2 2022 [62] | Italy | 237 | COVID-19 | The general public |
| 41 | Kurnia 2021 [63] | Indonesia | 112 | COVID-19 | Nursing students |
| 42 | Kim 2021 [64] | Republic of Korea | 186 | COVID-19 | The general public |
| 43 | DeDonno 2022 [65] | America | 719 | COVID-19 | The general public |
| 44 | Suk 2021 [66] | Republic of Korea | 300 | COVID-19 | Firemen and marine police |
| 45 | Magano 2021 [67] | Portugal | 1122 | COVID-19 | The general public |
| 46 | Idrees 2022 [68] | Pakistan | 440 | COVID-19 | The general public |
| 47 | Elsayed 2022 [69] | Egypt | 582 | COVID-19 | The general public |
| 48 | Feng 2022 [70] | China | 632 | COVID-19 | The general public |
| 49 | Zhang2 2021 [71] | China | 192 | COVID-19 | The general public |
| 50 | Gungor 2021 [72] | Turkey | 1473 | COVID-19 | The general public |
| 51 | Das 2021 [73] | India | 550 | COVID-19 | The general public |
| 52 | Jouybari 2018 [74] | Iran | 300 | influenza | High school students |
| 53 | Sadeghi 2018 [75] | Iran | 400 | H1N1 | Pregnant women |
| 54 | Zhang3 2020 [76] | China | 710 | H7N9 | The general public |
| 55 | Gutierrez-Dona 2012 [77] | Costa Rica | 428 | H1N1 | The general public |
| 56 | Gutierrez-Dona2 2012 [77] | Costa Rica | 97 | H1N1 | The general public |
| 57 | Wong2 2005 [78] | Hong Kong, China | 1537 | SARS | The general public |
| 58 | Karademas 2013 [79] | Greece | 273 | H1N1 | The general public |
| 59 | Karademas2 2013 [79] | Greece | 273 | H1N1 | The general public |
| 60 | Li 2022 [80] | China | 306 | COVID-19 | The general public |
| 61 | Bults 2014 [81] | Netherlands | 1249 | Q Fever | The general public |
| 62 | Kim2 2016 [82] | Republic of Korea | 249 | MERS | Nursing students |
| 63 | Park 2022 [83] | Republic of Korea | 193 | respiratory tract infection | Nursing students |
| 64 | Borges 2022 [84] | Ireland | 364 | COVID-19 | College students |
| 65 | Kwak 2021 [85] | Republic of Korea | 159 | COVID-19 | Nursing students |
| 66 | Haejin 2021 [86] | Republic of Korea | 291 | COVID-19 | Nursing students |
| 67 | Lee 2021 [87] | Republic of Korea | 222 | COVID-19 | Nursing students |
| 68 | Donizzetti 2022 [88] | Italy | 1301 | COVID-19 | Old people |
| 69 | Haeran 2020 [89] | Republic of Korea | 400 | COVID-19 | Medically inclined college students |
| 70 | Kyung 2021 [90] | Republic of Korea | 184 | COVID-19 | Nursing students |
| 71 | Jeon 2021 [91] | Republic of Korea | 200 | COVID-19 | Nurses |
| 72 | Zancu 2022 [92] | Romania | 634 | COVID-19 | College students |
| 73 | Fu 2022 [93] | China | 522 | COVID-19 | Youths |
| 74 | Jeong 2022 [94] | Republic of Korea | 187 | COVID-19 | Nursing students |
| 75 | Kim3 2021 [95] | Republic of Korea | 500 | COVID-19 | College students |
| 76 | Jeon2 2022 [96] | Republic of Korea | 237 | COVID-19 | Service workers |
| 77 | Minjung 2020 [97] | Republic of Korea | 412 | COVID-19 | Adults |
| 78 | Park2 2021 [98] | Republic of Korea | 241 | COVID-19 | Nursing students |
| 79 | Lee2 2022 [99] | Republic of Korea | 371 | COVID-19 | Aircraft crews |
| 80 | Lee 2021 [100] | Republic of Korea | 261 | COVID-19 | College students |
| 81 | Li 2021 [101] | China | 802 | COVID-19 | The general public |
| 82 | Zhang 2015 [102] | China | 2709 | H7N9 | The general public |
| 83 | Ayandele 2021 [103] | Nigeria | 172 | COVID-19 | The general public |
| 84 | Janis 2020 [104] | Norway | 4338 | COVID-19 | The general public |
| 85 | Li 2020 [105] | China | 454 | COVID-19 | The general public |
| 86 | Zeidi 2021 [106] | Iran | 340 | COVID-19 | Dentists |
| Variable | Example of Measurement Items | |
|---|---|---|
| Fear | “It makes me uncomfortable to think about coronavirus-19”, “I am afraid that someone in my family may get sick from the coronavirus”, “I am frightened because of COVID-19”, “I feel fearful about COVID-19”, etc. | |
| Anxiety | “I feel calm and can sit still easily”, “I feel that everything is all right and nothing bad will happen”, etc. | |
| Risk Perception | Perceived Severity | “I think this new coronavirus is very serious”, “I think the new coronavirus poses a serious threat to public health”,” I think this new coronavirus is very powerful”, etc. |
| Perceived Susceptibility | “I am at risk for novel coronavirus”, “My family/friends are likely to have novel coronavirus”, “People around me are likely to have novel coronavirus”, etc. | |
| Coping Behavior | “I avoided going to places outside the home where there were other people”, “Regularly and thoroughly clean your hands with an alcohol-based hand rub or wash them with soap and water”, “How often do you perform the following preventive measures?”, etc. | |
| Relationships | Number of Studies | Sample Size | Overall Effect | p-Value | Heterogeneity Test | I2 (%) | 95% CI | |||
|---|---|---|---|---|---|---|---|---|---|---|
| QB | df | P | Lower Limit | Upper Limit | ||||||
| Risk Perception–Behavior | 28 | 20,273 | 0.189 | 0.000 | 636.986 | 27 | 0.000 | 95.8 | 0.121 | 0.256 |
| Perceived Susceptibility–Behavior | 41 | 25,951 | 0.207 | 0.000 | 1475.235 | 40 | 0.000 | 97.3 | 0.133 | 0.279 |
| Perceived Severity–Behavior | 34 | 19,395 | 0.296 | 0.000 | 643.657 | 33 | 0.000 | 94.9 | 0.237 | 0.354 |
| Risk Perception–Fear | 8 | 11,384 | 0.481 | 0.000 | 643.961 | 7 | 0.000 | 98.9 | 0.327 | 0.610 |
| Risk Perception– Anxiety | 10 | 8897 | 0.338 | 0.000 | 388.233 | 9 | 0.000 | 97.7 | 0.208 | 0.457 |
| Fear– Behavior | 11 | 19,711 | 0.239 | 0.002 | 1083.559 | 10 | 0.000 | 99.1 | 0.089 | 0.377 |
| Anxiety– Behavior | 9 | 6086 | 0.122 | 0.254 | 456.461 | 8 | 0.000 | 98.3 | −0.088 | 0.321 |
| Relationships | k | Fail- Safe Number | Begg’s Test | Egger’s Test | |||||
|---|---|---|---|---|---|---|---|---|---|
| Tau | Z | P | Intercept | SE | 95% CI | P | |||
| Risk Perception–Behavior | 28 | 3626 | 0.000 | 0.000 | 1.000 | 1.987 | 1.935 | [−1.991, 5.965] | 0.314 |
| Perceived Susceptibility–Behavior | 41 | 8805 | 0.141 | 1.303 | 0.193 | 0.220 | 2.110 | [−4.048, 4.487] | 0.918 |
| Perceived Severity–Behavior | 34 | 2049 | 0.094 | 0.786 | 0.432 | 3.198 | 1.810 | [−0.489, 6.886] | 0.087 |
| Risk Perception– Fear | 8 | 4468 | 0.107 | 0.371 | 0.711 | 15.377 | 7.803 | [−3.717, 34.471] | 0.096 |
| Risk Perception– Anxiety | 10 | 2029 | 0.044 | 0.179 | 0.858 | 11.154 | 4.817 | [0.047, 22.262] | 0.049 |
| Fear– Behavior | 11 | 2592 | 0.000 | 0.000 | 1.000 | −2.067 | 6.830 | [−17.517, 13.382] | 0.769 |
| Anxiety– Behavior | 9 | 289 | −0.139 | 0.521 | 0.602 | −1.389 | 5.616 | [−14.667, 11.890] | 0.812 |
| Relationships | Main Effect | 95% CI | Leave-One-Out | ||
|---|---|---|---|---|---|
| Lower Limit | Upper Limit | Min | Max | ||
| Risk Perception–Behavior | 0.192 | 0.121 | 0.256 | 0.180 | 0.208 |
| Perceived Susceptibility–Behavior | 0.207 | 0.133 | 0.279 | 0.191 | 0.218 |
| Perceived Severity–Behavior | 0.296 | 0.237 | 0.354 | 0.284 | 0.305 |
| Risk Perception–Fear | 0.481 | 0.327 | 0.610 | 0.452 | 0.528 |
| Risk Perception–Anxiety | 0.338 | 0.208 | 0.457 | 0.299 | 0.372 |
| Fear–Behavior | 0.239 | 0.089 | 0.377 | 0.186 | 0.278 |
| Anxiety–Behavior | 0.122 | −0.088 | 0.321 | 0.039 | 0.163 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, Y.; Jiang, Y.; Zhang, W.; Zhu, Y. Relationship between Risk Perception, Emotion, and Coping Behavior during Public Health Emergencies: A Systematic Review and Meta-Analysis. Systems 2023, 11, 181. https://doi.org/10.3390/systems11040181
Zhao Y, Jiang Y, Zhang W, Zhu Y. Relationship between Risk Perception, Emotion, and Coping Behavior during Public Health Emergencies: A Systematic Review and Meta-Analysis. Systems. 2023; 11(4):181. https://doi.org/10.3390/systems11040181
Chicago/Turabian StyleZhao, Yuxia, Yicen Jiang, Wei Zhang, and Yanchun Zhu. 2023. "Relationship between Risk Perception, Emotion, and Coping Behavior during Public Health Emergencies: A Systematic Review and Meta-Analysis" Systems 11, no. 4: 181. https://doi.org/10.3390/systems11040181
APA StyleZhao, Y., Jiang, Y., Zhang, W., & Zhu, Y. (2023). Relationship between Risk Perception, Emotion, and Coping Behavior during Public Health Emergencies: A Systematic Review and Meta-Analysis. Systems, 11(4), 181. https://doi.org/10.3390/systems11040181







