Abstract
This study analyzes the current status of the digitalization of the Romanian Health System (RHS). Data were collected from 135 active public and private health professionals using an online questionnaire with 102 items. The results of the analysis show that, if the qualification level and the experience of managers are high, seniority in management positions is an essential factor in the adoption of digital technologies, the digitalization of health services increases the efficiency and quality of medical and management services, and the success of the implementation of digital technologies is conditioned by the harmonization of a variety of factors because there are differences between the public and private sectors in terms of the economic efficiency determined by the adoption of digital technologies. There are also differences in the implementation of digital technologies between the national and worldwide levels, there are specific technologies that positively influence managerial performance, and the innovation process is conditioned by the management level. Because Romanian health service managers are updated with new technologies, they can ensure the implementation of digital technologies, considering that economic efficiency and managerial performance are directly related to the level of adoption and the type of technologies implemented.
1. Introduction
The global digital transformation process finds the Romanian Health System (RHS) facing multiple challenges: structural reform, under-financing health, insufficient staff, deficient and outdated infrastructure, a lack of population trust, and many others [1,2].
After the fall of the communist regime in December 1989, RHS experienced a transition from the Semashko model to the Bismark model, with some influences from the Beveridge and Semaschko models [3,4]; the characteristics of these systems can be seen in Table 1.

Table 1.
Comparison of Semashko, Bismarck, and Beveridge models according to provision and funding (source: adapted from [3,4]).
Currently, RHS provides universal health coverage, with public and private providers, family doctors providing primary care, and hospitals and specialized centers providing secondary and tertiary care. The total health expenditure in 2021 was 1663 EUR per capita, representing the lowest rate in the European Union (EU) [1,5].
Romanian patients consider the main problems facing RHS to be the low quality of medical care, the overworking of employees, the cost of access to treatment, bureaucracy, waiting time, or insufficient staff [2]. RHS registers a health index score of 73 out of 100, considering a variety of indicators [6].
Data provided by the National Institute of Statistics show us that 293,710 people make up the medical staff working in 65,942 health units, with the following distribution: 1 family medicine office to an average number of 1823 inhabitants, one pharmacy to 1926 inhabitants, one independent specialized medical office to 1386 inhabitants, one independent dental office to 1165 inhabitants/unit, 351 hospitals and health facilities with more than 100 beds (extensive medical facilities), and 269 with fewer than 50 beds (small medical facilities) [7].
In this work, our goal is to provide a detailed analysis of the current state of digitalization in the Romanian Health System (RHS). Drawing on data from 135 public and private health professionals, collected via a 102-item online questionnaire, we conducted a cross-sectional study to evaluate how digitalization can improve the managerial performance of health services. We believe these findings offer valuable insights and a realistic perspective on the digitalization of the RHS, as reflected in the responses of active health professionals.
This paper is structured according to the following sections: Section 2—regarding concepts such as smart hospital management, digital economy efficiency, digital technologies and innovation processes, or the health information system; Section 3—which describes the study’s objectives and research questions, hypotheses, instruments and investigation tools, the population, and the respondents; and Section 4—analytical, statistical, and descriptive results and hypotheses testing and validation, followed by discussions and conclusions.
2. Related Works
There is a gap in exploring recent innovations in digital health that have not been fully integrated or studied in the specific context of health services management. The topic addressed is particularly important while RHS faces major challenges related to efficiency, accessibility, and quality, and digital technologies offer promising solutions for optimizing these aspects.
2.1. Smart Hospital Management
First, we analyzed the smart hospital (SH) concept, which can be viewed from academic and industrial perspectives. SH is described by a multitude of characteristics that can be grouped into the following broad categories: technology, services, and goals. SH implementation implies setting clear objectives and reaching the maximum potential of smart technology and not just digitalizing the existing environment with partial exploitation of technologies [8].
Building information modeling (BIM) digitally represents the physical and functional characteristics of hospital and health facility buildings, aiding in real-time decision-making for operational parameters [9]. There is a growing need to assess and prioritize the most advantageous BIM applications for facility management [10]. Smart management aims to integrate medical resources, support management decisions, and enhance management efficiency [11].
The smart hospital management (SHM) concept develops proportionally to the emergence of new technologies and knowledge management, and it is an essential component of Healthcare 4.0. SHM is based on integrating several technologies, such as IoT, AI, cyber–physical systems, or management information systems [12].
The smart hospital management system (HMS) represents a solution for streamlining the administrative process and achieving high standards of patient care. The development and implementation of HMS are researchers’ concerns. The system integrates modules that help optimize hospital operations, prioritizing data security and compliance with regulations [13].
In this context, the level of preparation of health service managers in Romania regarding the adoption of digital technologies becomes a concern for us.
2.2. Digital Economy Efficiency
Increasing economic momentum and improving the efficient allocation of resources have a positive role in the speed with which the digital economy (DE) develops. The evolution of the DE in public health applications requires increased attention to quantity and quality. The efficiency of public health services did not experience a significant increase as an effect of DE, even registering a reduction [14]. DE mediates the quality and performance of government regulations, resulting in the digital transformation of public health services. Thus, the ability to respond to public health crises such as the COVID-19 pandemic could be strengthened [15].
The efficiency of public health services through digitalization requires an integrated approach, including improved e-government practices, policies based on innovation and adaptation, efficient management, and significant investments in digital technologies [16].
A Romanian study involving 423 accountants from the healthcare industry shows that digital technologies in Industry 4.0 will enhance healthcare costing processes, requiring adaptation and support from senior accountants for effective implementation [17].
Scalability, limited resources, regulations, and policies characterize the public/state health sector. In comparison, the private sector is characterized by flexibility, the quality of services, innovation, and personalization. The mode of operation, the resources, and the objectives are the fundamental differences between the two sectors.
2.3. Digital Technologies and the Innovation Process
The digitalization of healthcare consists of adopting various approaches, concepts, and technologies. Some have been studied and tested in the last decades, and others are emerging. Some became more than necessary during the pandemic period [18], which must be addressed through the development of clear national health policies, harmonized systems of education, and the continuous training of specialists, especially managers of health units, who should also know the policies of other countries regarding the mobility of medical personnel [19].
The electronic health record (EHR) is a digital document that records and shares a person’s official health data across institutions [20]. Its implementation requires strict policy development and adherence to information management guidelines [21]. Telemedicine enables remote connections between specialists and patients, addressing non-urgent issues without face-to-face consultations [22,23]. As part of the e-health concept, telemedicine’s applications are influenced by social factors, attitudes, and e-health literacy [24,25]. Wearable technologies collect and transmit patient data to healthcare providers for real-time detection, tracking, and monitoring [26,27]. These technologies come in various forms and have diverse potential applications [26].
Artificial intelligence (AI) simulates human intelligence to revolutionize patient care and administrative processes, though its implementation poses ethical and workforce challenges [28,29]. Virtual reality (VR) and augmented reality (AR) offer interactive experiences that improve medical communication and patient outcomes [30,31]. Integrating VR and AR in immersive settings with mixed-reality headsets provides real-time access to critical data for better decision-making [32]. Big Data, generated from various sources, strengthen predictive systems and have amassed 2314 exabytes of information since the Mayo Clinic EHR’s implementation [33,34].
Mobile applications support health monitoring and data collection for healthcare professionals, with significant usage during the pandemic and beyond [35,36]. Blockchain technology ensures the secure exchange and integrity of patient data and clinical trials through cryptographic techniques [37,38]. The Internet of Things (IoT) connects devices and systems via embedded sensors and software, facilitating communication across a three-layer architecture [39,40]. Voice search enhances patient access to medical information, with potential dominance due to its convenience and ease of use [41,42]. Video marketing presents healthcare services dynamically, aiding in patient education and professional training [43]. Social networks enable interactions among healthcare providers, institutions, patients, and the public, becoming essential tools in the digital transformation of healthcare [44,45].
Three-dimensional printing creates three-dimensional objects for clinical care, including implants, prostheses, anatomical models, and medical equipment [46]. Next-generation sequencing (NGS) enables the simultaneous sequencing of billions of DNA fragments, promising future advancements in genomics research with more portable platforms [47]. Nanotechnologies aid in accurate diagnosis through nanorobots that provide images of disease sites within the body [48].
Digital transformation needs a commitment from central decision-makers and health unit managers to promote interoperability and boost digital literacy among healthcare providers and beneficiaries [49]. Assessing patients’ digital literacy is challenging without standardized tools and staff training, particularly for nurses, who frequently interact with patients [50].
Transitioning from traditional to digital medicine is challenging due to infrastructure, financing, and restructuring issues. A major concern is redundancy in human resources across practice levels. A positive attitude toward digital transformation is linked to individuals’ behavioral traits and innovative qualities. Additionally, this attitude positively influences both the personal and social acceptance of digital transformation [51].
Successful innovation in healthcare demands a careful selection of technologies to enhance medical and management performance, highlighting the process’s complexity and need for expertise.
2.4. Health Information System
The Romanian National Health Strategy 2023–2030 highlights digitalization and interoperability as key milestones for modernizing the health information system (HIS) [52]. Effective knowledge and information management heavily rely on strengthening HIS implementation [53]. The three digital transformation priorities are secure access to personal health data across the EU, standardized data infrastructure for personalized medicine, and patient-centered care with digital tools [54].
The quality, accessibility, efficiency, and equity of healthcare can be positively influenced by the adoption of digital technologies, a set of tools that provide opportunities for discovering needs and providing quality care [55]. Opinions on technology adoption rates vary, but healthcare professionals emphasize that technological development should enhance administrative efficiency and practical medical care. They seek centralized control with a patient-centered approach [56].
Other Romanian studies emphasize the importance of digital advancements in enhancing stability, profitability, and efficiency in the banking sector, for example. For organizational management, adopting Industry 4.0 processes is crucial for boosting productivity, innovation, and communication. Additionally, standardization and interoperability are essential for seamless system integration, ensuring that organizations remain competitive in the rapidly evolving digital landscape [57,58,59].
Interoperability is essential to fully realize the potential of digital medicine, as much of today’s medical data is fragmented and incompatible, slowing progress in areas like AI and big data. Standardized, interoperable health data would improve communication, research, and international collaboration, fostering digital innovation. Achieving this demands collaboration between healthcare professionals, researchers, IT specialists, and policymakers. In the long run, creating global standards for interoperability will build a connected digital health infrastructure, turning medical data into valuable insights and enhancing patient care globally [60].
However, an uncoordinated implementation of all the components that make up the HIS can accentuate inequities in healthcare, further disadvantaging individuals or groups with limited resources [61]. The HIS development considers the critical success factors (CSFs), having a prospective orientation in their application and management at different system levels [62].
The full potential of digital health innovations is hindered by inconsistent adoption and sustainability, while increasing cyberattacks make patient data confidentiality a critical challenge, requiring close collaboration between cybersecurity and digital transformation teams [63].
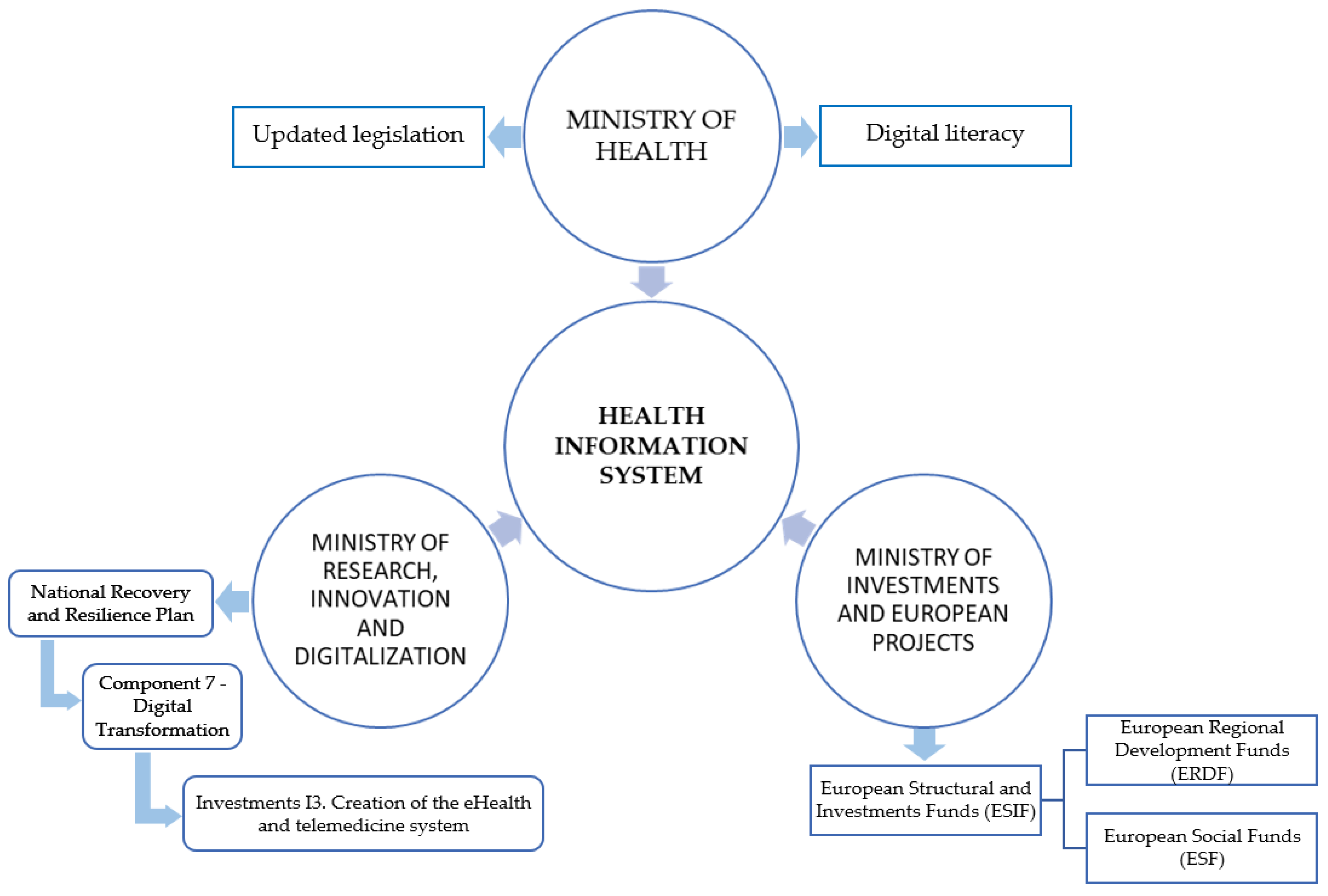
We believe that for the effective implementation of a health information system (HIS) in Romania, the synchronization and harmonization of the actions of the following institutions is crucial, as presented in Figure 1.
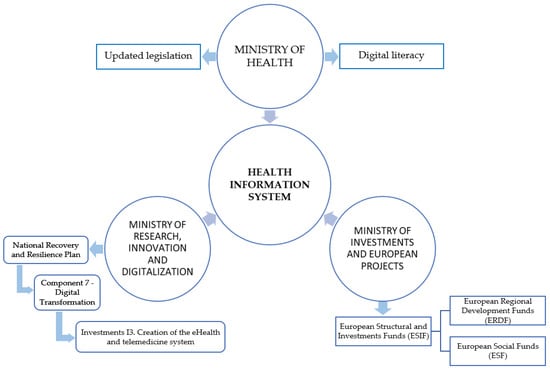
Figure 1.
Factors that ensure the implementation of an efficient health information system in Romania.
3. Methodology
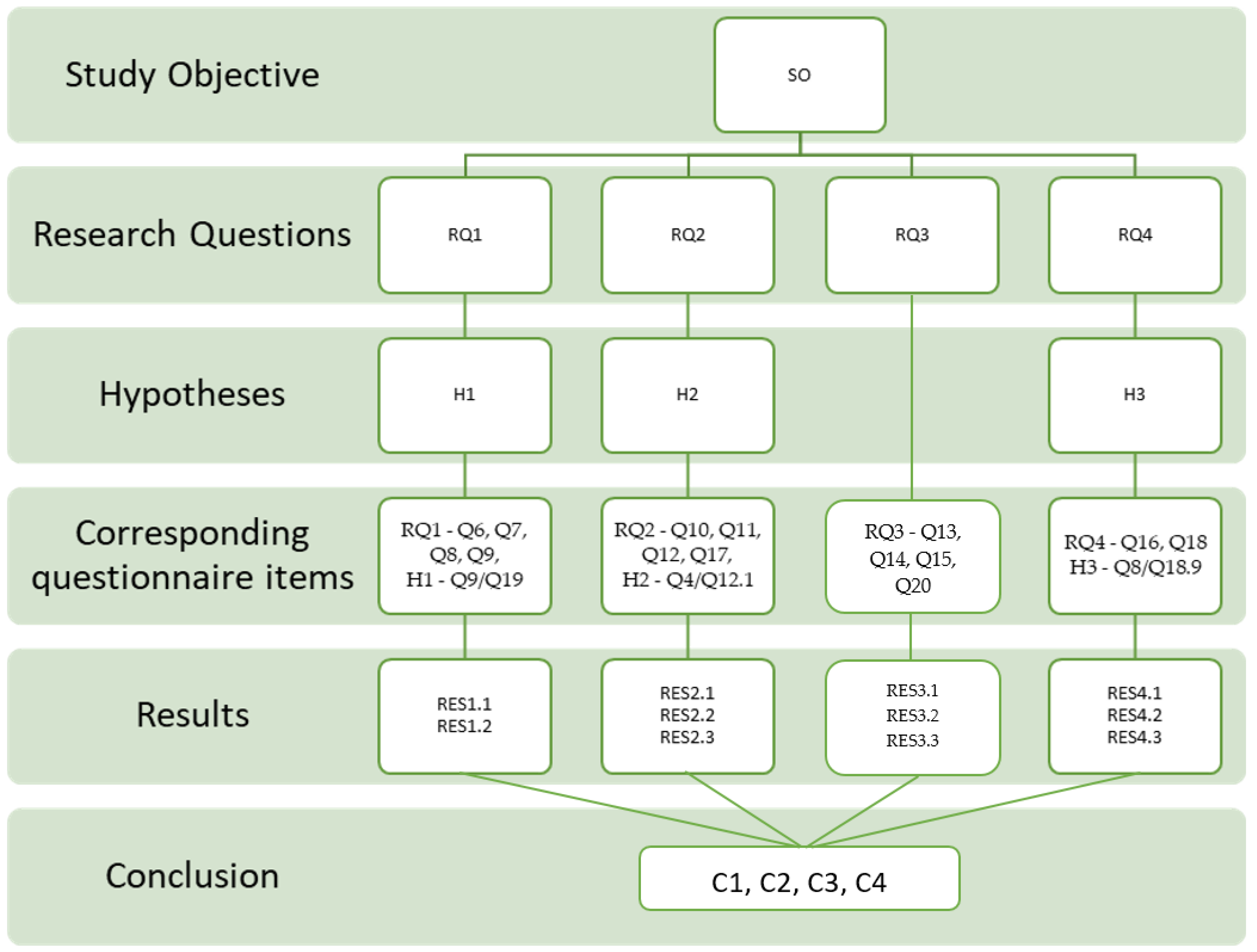
The study was structured following a linear flow, as seen in Figure 2: study objective, research questions, hypotheses, a demonstration intended to support the research questions, questionnaire items corresponding to each question and hypothesis, results, and conclusions.
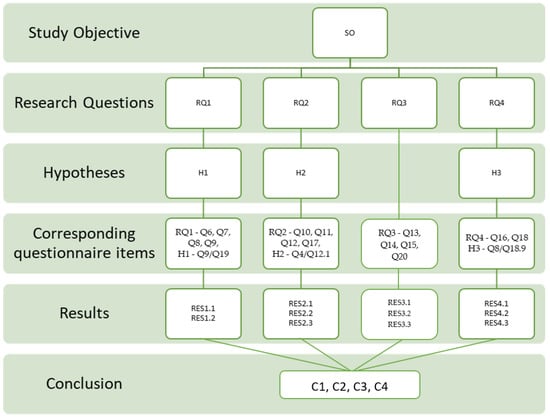
Figure 2.
Conceptual research model.
The questionnaire items (Qs) to which the research questions and hypotheses relate, as shown in the figure above, are as follows: Q4—practice sector, Q6—field of qualification, Q7—level of education, Q8—management level, Q9—seniority in a management position, Q10—opinion on certain statements, Q11—the importance of some factors that condition the implementation of modern technologies, Q12—agreeing with some statements, Q12.1—the economic efficiency and sustainability of a health system increased using digital solutions, Q13–Q14—technologies indicated worldwide, Q15—the level of technology implementation in Romania, Q16—increasing managerial efficiency and productivity based on the integration of technologies, Q17—essential aspects in the digital transformation process, Q18—the influence of some factors on managerial performance, Q18.9—the innovation process, Q19—attendance at conferences and specific technology events, and Q20—the order in which one would implement certain technologies.
We conducted research based on an online questionnaire, collecting data from a single sample at a single time (cross-sectional study) to analyze the current state of RHS digitalization, which facilitates an increase in managerial performance for health services.
3.1. Study Objectives and Research Questions
The objective of this study was to answer the following question: “What is the current status of the Romanian Health System digitalization?” The following four questions were derived from this question, and this study’s objectives represented the answers to them.
Research Question 1 (RQ1).
How receptive are health service managers to adopting digital technologies in their units?
Research Question 2 (RQ2).
What are the opinions and perceptions of specialists regarding different aspects of adopting digital technologies?
Research Question 3 (RQ3).
What digital technologies have specialists indicated to support medical activity worldwide and in Romania?
Research Question 4 (RQ4).
What technologies and factors influence managerial efficiency and performance in health services?
3.2. Hypotheses
We proposed the following hypotheses for this study to support the research questions, taking into account related papers or articles.
Medical and technology conferences are essential for professional development, offering direct exposure to new tools, practices, and theories. They facilitate networking with experts, showcase cutting-edge technologies, and influence decision-making, particularly among senior management, leading to the adoption of new practices and technologies at healthcare institutions [64,65,66]. Therefore, the following hypothesis is proposed:
Hypothesis 1 (H1).
There is a difference in updating with new technologies in a medical institution, measured using the attendance at conferences and technology events, depending on the seniority of the attendant’s management position.
Private healthcare institutions, driven by competition and the need for profitability, often adopt digital solutions more swiftly and invest more heavily in these technologies than public institutions, leading to greater cost efficiency and improved patient outcomes. While facing significant funding and regulatory challenges, public-sector healthcare systems can benefit from digital advancements through strategic partnerships with private entities [67,68]. Therefore, the following hypothesis is proposed:
Hypothesis 2 (H2).
There is a difference in the economic efficiency induced by implementing digital solutions for a healthcare system, depending on the type of property (private or state sector).
The adoption of innovation involves an organization integrating new advancements into its core operations [69]. Making strategic decisions, allocating resources, and fostering a culture of innovation are crucial factors for senior healthcare managers in their perception of successful healthcare technology adoption. Their top-down influence ensures that innovations are prioritized, funded, and implemented effectively, leading to better integration and use of new health technologies [70,71]. Therefore, the following hypothesis is proposed:
Hypothesis 3 (H3).
There is a difference in the perception of the adoption of innovation in a medical institution, depending on the level of the managers.
3.3. Instruments and Investigation Tools
The study was based on a questionnaire that contained 21 questions, with an average completion time of approximately 24 min and the obligation to provide an answer for each of the 102 items (except Q2 regarding the collection of email addresses to provide feedback), determining, in our opinion, a high dropout rate during completion from potential respondents. According to the type of questions and answers, the questionnaire was structured as follows: Q1. Expression of consent to participate—unique answer. Q2. Open-text question (optional)/email—open answer. Q3–Q9. Socio-demographic characteristics—unique answer. Q10–Q18. Questions of opinion and perception—single—Likert scale (numerical intervals and word scales), multiple, open answers. Q19 and Q21. Open-text questions—open, count answers. The questionnaire used the five-value Likert ordinal scale, with the associated categories and ranks: “Very unimportant”/“Not at all”/“Strongly Disagree” (1); “Unimportant”/“To a small extent”/“Disagree” (2); “Neutral” (3); “Important”/“To a great extent”/“Agree” (4); and “Very important”/“Totally”/“Strongly Agree” (5); and numerical scale was also used, in which 1 represents the lowest level, and five is the highest.
We tested the reliability of the main variables using Cronbach’s alpha coefficient, which indicated whether the responses collected from the 135 respondents were consistent between items. The values in Table 2 are above the recommendation of 0.70 [72], and the values of 0.975, 0.963, 0.942, 0.888, and 0.862 demonstrate high internal consistency.

Table 2.
Reliability statistics.
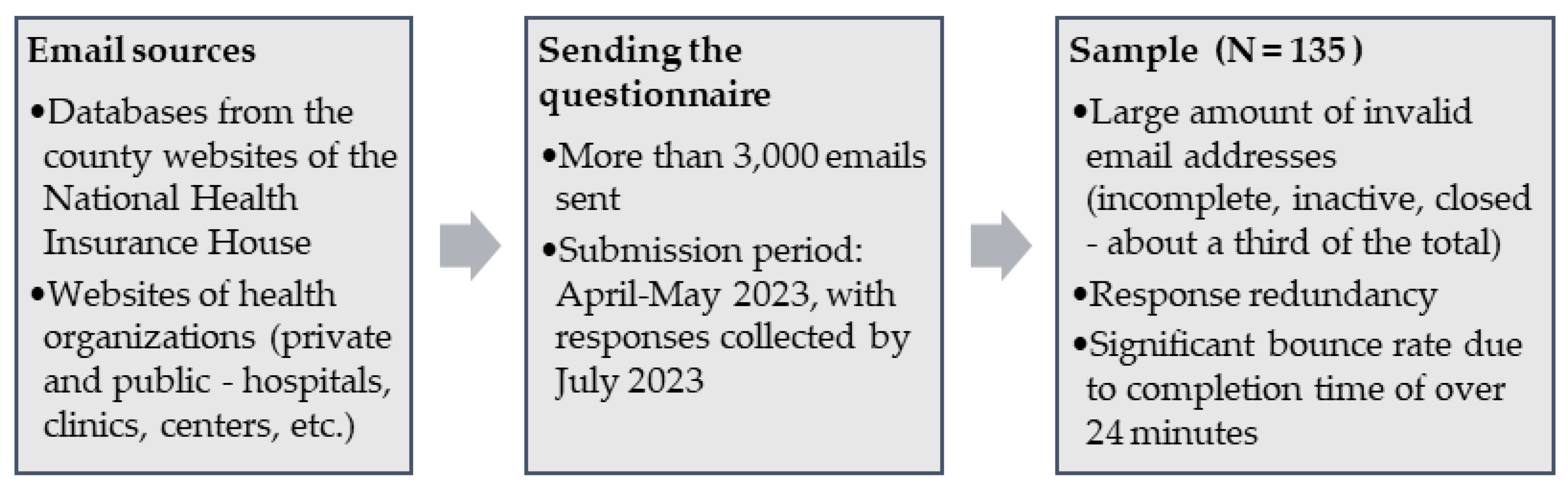
3.4. Population and Sample Respondents
From the perspective of administrative–territorial organization, the following types of units are distinguished in Romania: counties (41 in number), municipalities (urban localities with a more significant number of inhabitants, the most important being the municipality of Bucharest, the capital of the country), cities, communes, and villages [73]. In 2022, the distribution of healthcare facilities was as follows: 54,046 in urban areas and 11,896 in rural areas. Two-thirds of rural healthcare facilities are represented by family medicine offices (35%), respectively, and by pharmacies (32%) [7].
We applied the voluntary sampling technique, usually used in medicine, with respondents being included in the sample only to the extent that they absolutely answered all the questions included in the statistical questionnaire. Data collection is usually a long-term operation, a characteristic feature of research in the medical field [74]. There are 544 hospitals operating in the RHS, each unit having a team of four managers (manager, medical director, economic director, and care director), resulting in a number of 2200 managers. The sample included 135 respondents, a small sample, characteristic of survey research in the medical field compared to other fields [75], which resulted as shown in Figure 3, with a balanced distribution of the development regions [76], as can be seen in Table 3. The 92 managers who provided answers in this study represented 16.9% of the number of hospitals, and the answer of one manager per unit was considered edifying.
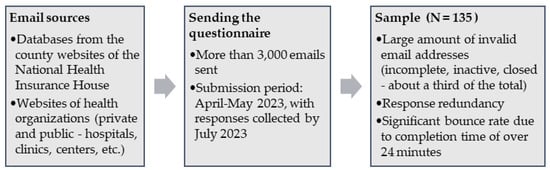
Figure 3.
Sampling frame.

Table 3.
Socio-demographic characteristics of the sample.
We considered the sample significant, given the high weight regarding characteristics such as the field of education, level of studies, and level and length in the management function.
By level of education (Q7), we included bachelor’s and master’s graduates (36%), postgraduate studies (41%), doctoral and postdoctoral studies (19%), and others (4%); 85% of the respondents had medicine as their qualification field, the others being graduates of economics, law, or other fields (Q6).
According to the management level (Q8) at which the respondents were currently active, we distinguished between the following categories: top managers (31%), mid-level and operational managers (37%), and 32% who did not hold a management position. Seventy-one percent of the respondents stated that they had at least five years of experience in a management position (Q9).
From the perspective of the practice sector (Q4), half of the respondents worked exclusively in the private sector, and the other half in the state (46% of them also practiced in the private sector). The following types of services (Q5) in which the respondents worked were distinguished: hospital, family medicine office, polyclinic, specialized medical office, dental clinic, health and rehabilitation center, home medical care, pharmacy, medical laboratory, IT specialist, medical technology, and infrastructure provider.
4. Results
The results were collected using the Microsoft Forms platform, through which we generated the questionnaire and collected the responses from the respondents. The average completion time was long because the questionnaire was set with the obligation to answer for all items, with only sending the final email to submit the responses being optional. In our opinion, this aspect certainly generated an appreciable dropout rate from the respondents during the completion.
4.1. RQ1. How Receptive Are Health Service Managers to Adopting Digital Technologies in Their Units?
We rated the sample as very valuable, considering the following significant results: Q6—medical graduates (85%), Q7—postgraduate/doctoral/postdoctoral studies (60%), Q8—top/middle level/first-line management (69%), and Q9—more than ten years as a manager (55%). These percentages are relevant to outlining the training level of the Romanian health service manager in the context of digitalization.
Hypothesis 1.
”There is a difference in updating with new technologies in a medical institution, measured by the attendance at conferences and technology events, depending on the seniority of the management position of the attendant.”
We used the one-way ANOVA (Table 3) and Tukey’s post hoc test (Table 4) to test whether there were statistical differences between the means of the groups corresponding to the independent variable “Seniority in the management position”/Q9 regarding the “Attendance in conferences and specific technology events”/Q19 (dependent variable). The scores corresponding to the dependent variable were given by the number of attendances expressed in numerical responses.

Table 4.
One-way ANOVA results.
In Table 4, we notice that the significance value is 0.038 (less than the chosen significance level of α = 0.05); therefore, there was a statistically significant difference between the means of the groups. We applied Tukey’s post hoc test to discover which specific groups differed. Table 5 shows us that there was a significant difference in terms of attendance at conferences and technological events between the groups “Non-management position” (N = 25) and “More than 10 years of experience” (N = 74), p = 0.042. There were no statistically significant differences between the experienced groups ”Under 5 years of experience” (N = 16), ”Between 5.1 and 10 years of experience” (N = 20), and “More than 10 years of experience”.

Table 5.
Post hoc test results.
The results obtained from the statistical analyses confirmed Hypothesis 1. The seniority of the respondents in management positions at medical institutions significantly influenced their updates using new technologies, an essential aspect of the field’s digital transformation.
Results
RES1.1. The managers within Romanian health services had the following characteristics: medical graduates with postgraduate, doctoral, or postdoctoral studies, in most cases, and more than five years of experience in a management position.
This profile indicates a high level of qualification and expertise in the medical field, combined with management skills, suggesting a solid background in the health system’s clinical and administrative aspects. This clinical experience was complemented by a detailed knowledge of the rules and regulations of the health sector, allowing for the efficient and compliant management of the operational aspects of a medical institution. The profile also reflects significant management expertise, demonstrating the ability to coordinate multidisciplinary teams, develop strategies to improve medical services, and optimize available resources in order to ensure a high level of quality care.
RES1.2. The seniority of respondents in management positions at medical institutions significantly influenced their updates using new technologies, an important aspect of the field’s digital transformation.
This suggests that experienced managers are probably more open to innovation and the implementation of modern technologies, thereby contributing to the modernization of the institutions they lead. They bring not only deep knowledge accumulated throughout their careers but also a clear understanding of the need to integrate advanced technological solutions to remain competitive and efficient in the current context of the healthcare system. Experienced managers can identify and capitalize on opportunities to implement new technologies, such as patient management information systems, telemedicine, artificial intelligence for diagnosis and treatment, and next-generation medical devices, optimizing workflows, reducing medical errors, and improving the quality of care for patients. Their openness to innovation enables the creation of work environments that encourage continuous professional development and the adoption of best practices, fostering an organizational culture where employees are motivated to embrace change and adapt quickly to new technologies and leading to higher operational efficiency and increased patient satisfaction.
4.2. RQ2. What Are the Opinions and Perceptions of Specialists Regarding Different Aspects of Adopting Digital Technologies?
Through Q10 and Q12, we wanted to find out the respondents’ opinions on certain statements and were significant in using “Agree” and “Strongly Agree” in favor of these statements, as follows: the difference between the type of health services (78%), the difference between the level of education (87%), the difference between state and private involvement (72%), the difference between geographical locations (72%), and levels of implementation (62%). Respondents’ opinions were significant in choosing “Agree” and “Strongly Agree” in favor of these statements: increasing economic efficiency and sustainability (86%), improving the quality of treatment results (85%), reducing waiting times, increasing the population’s access to health care and improving patient safety (70%), and increasing the performance of medical staff (79%).
Through Q11, we wanted to find out the importance of specific factors in the RHS digitalization process. Respondents’ opinions were significant in choosing “Important” and “Very important” in favor of these statements, as follows: the proactive attitude of relevant ministries (88%), updated legislation (91%), the quality of national infrastructure (89%), the existence of dedicated funding sources (95%), and decision-making capacity at the level of health facilities (93%).
Through Q17, we intended to learn the extent to which the respondents considered some aspects essential in the digital transformation process. Respondents’ opinions were significant in choosing “To a great extent” and “Totally” in favor of these statements, as follows: the exchange of good practices between health systems (86%), promoting technical specifications and common standards for digital health tools and exchange formats (81%), establishing an effective national strategy (90%), and the existence of a coordinating institution with a clear national mandate (67%).
Hypothesis 2.
“There is a difference in the economic efficiency induced by implementing digital solutions for a healthcare system depending on the type of property (private or state sector).”
We used the independent-sample t-test to test whether there were statistical differences between the means of the groups corresponding to the independent variable “Practice sector” (“Private” (N = 68) and “State” (N = 36)) regarding the “Economic efficiency and sustainability of a health system increased by the digital solutions” (dependent variable). The scores corresponding to the dependent variable were obtained using the associated ranks of the ordinal scale from 1 to 5 (where 1 is the lowest level, and 5 is the highest level).
Table 6 provides descriptive statistics for the two groups compared, including the mean and standard deviation, and Table 7 provides the results of the independent-sample t-test.

Table 6.
Group statistics.

Table 7.
Independent-sample t-test results.
The p-value of Levene’s Test (Sig.) was 0.215, higher than the chosen significance level (α = 0.05), which means the null hypothesis was not rejected. Therefore, we followed the line “Equal variances assumed” for the t-test results.
The 68 respondents who expressed themselves regarding the economic efficiency and sustainability of a health system (M = 4.43, SD = 0.759) compared to the 36 respondents from the control group (M = 4.00, SD = 1.069) recorded appreciably higher scores, t(102) = 2.357, p = 0.020.
According to the results obtained from the statistical analyses, we concluded that Hypothesis 2 was confirmed. The type of practice sector of the medical institution of a respondent (private/state) significantly influenced the economic efficiency and sustainability of the health system induced by adopting digital solutions, an important aspect of the field’s digital transformation.
Results
RES2.1. Specialists consider that adopting digital technologies increases the efficiency and quality of medical and administrative work by eliminating manual form filling, and the manager’s training area can be an advantage for implementing new technologies.
The training of managers in the medical field is a significant advantage for the implementation of new technologies because these managers are better equipped to integrate digital solutions, facilitating a more efficient and accurate work process. Medical education gives them a deep understanding of the clinical and operational needs of healthcare facilities, enabling them to correctly identify the areas where technology can bring the greatest benefits. These managers can evaluate and select the technologies that best meet the needs of patients and healthcare staff, from data management systems to advanced equipment and telemedicine applications. Their clinical knowledge enables the improved diagnosis, treatment, and monitoring of patients, as well as the optimization of administrative and logistical processes.
RES2.2. Specialists believe the following actions are necessary for the healthcare system: the establishment of an effective national strategy, the existence of dedicated funding sources, updated legislation, the proactive attitude of relevant ministries, the scheme of best practices between health systems, or the promotion of technical specifications and common standards for digital health tools and exchange formats.
These measures are essential to creating a favorable framework for the development and implementation of digital technologies in the health field, and an effective national strategy is paramount to ensuring a clear direction in their adoption, including clear objectives, action plans, and a well-defined timetable. Dedicated funding sources are vital to support these initiatives, providing the necessary resources for digital infrastructure, staff training, and the purchase of modern equipment. Up-to-date legislation is crucial in creating a regulatory environment that supports digital innovation, addressing data protection, cyber security, and the interoperability of digital systems. The proactive attitude of the relevant ministries is essential to drive these changes through policies that encourage the adoption of new technologies. The exchange of best practices between health systems can accelerate the adoption of successful solutions, and the promotion of technical specifications and common standards for digital health tools ensures their compatibility and efficiency. The integration of these measures in a coherent and well-coordinated framework will contribute decisively to the digital transformation of the health system, improving the quality of medical services and operational efficiency.
RES2.3. The type of practice sector of the medical institution of a respondent (private/state) significantly influenced the economic efficiency and sustainability of a health system induced by adopting digital solutions, an important aspect of the field’s digital transformation.
The institutional context is crucial in the implementation of digital technologies, as the private and public sectors have different resources and motivations that influence the integration and sustainability of digital solutions. Private institutions benefit from easier access to funds and flexibility in adopting new technologies, motivated by market competition that forces them to be at the forefront of digital transformations in order to attract patients and improve service quality. In contrast, the public sector faces budgetary and bureaucratic constraints that can delay the implementation of digital technologies, but it has the advantage of being able to implement uniform policies and standards at scale, facilitating interoperability and data exchange between entities in the health system. The public sector can also access government funding and grants for digitalization, providing a solid foundation for the development and implementation of advanced technologies. Thus, the type of sector significantly influences the economic efficiency and sustainability of digital solutions in the health system, determining their long-term success.
4.3. RQ3. What Digital Technologies Have Specialists Indicated Support Medical Activity Worldwide and in Romania?
Through Q13 and Q14, we wanted to identify the most applied technologies worldwide, as indicated by specialists in the field of medical care. Respondents could provide multiple answers, choosing any of 25 items. These technologies were telemedicine (93%), electronic health records/EHRs (89%), portable devices/wearables (81%), custom mobile apps (74%), and nanotechnologies (56%).
Q15 concerns the level of digital technologies’ implementation with which the respondents worked. The respondents’ opinions were significant in choosing “To a small extent” and “Not at all,” as follows: EHR (40%), telemedicine (31%), and custom mobile apps (20%).
Q20 concerns the order in which the respondents would implement digital technologies in their own units, and the results were as follows: first choice—telemedicine (56%), second choice—AI (24%), third choice—Big Data, and fourth and fifth choices—VR and AR (33%).
Results
RES3.1. The most applied technologies worldwide indicated by specialists are (in descending order) telemedicine, electronic medical records, portable devices, personalized mobile applications, and nanotechnologies.
These technologies are implemented in descending order of applicability, indicating a clear trend towards digitalization and personalization in health services, with telemedicine and electronic medical records at the top of the list due to the significant benefits they bring in improving access to health services and efficiency in information management patients.
RES3.2. In Romania, electronic medical records, telemedicine, and personalized mobile applications are considered the most used technologies, but in a much lower proportion than worldwide.
Although the recognition of the importance of digital technologies in health is evident, their adoption remains limited due to insufficient infrastructure, limited financial resources, and cultural resistance to change. For example, telemedicine has become crucial during the COVID-19 pandemic, enabling remote medical consultations, reducing the risk of infections, and removing geographical barriers, especially for patients in rural areas.
RES3.3. Most specialists state that Romanian health services implement digital technologies shallowly.
This perception highlights that, although digitalization initiatives exist, they are sporadic and insufficient to significantly transform the healthcare system. Obstacles to the adoption of digital technologies include the lack of a coherent national strategy, the underfunding of the health sector, and deficiencies in the training of medical staff in the use of new technologies.
4.4. RQ4: What Technologies and Factors Influence Managerial Efficiency and Performance in Health Services?
Question 16 looks at the extent to which the integration of technologies would increase the efficiency and productivity of health service managers. Respondents’ opinions were significant in choosing “To a great extent” and “Totally” in favor of these statements, as follows: VR and AR (46%), AI/ML (47%), Big Data (58%), portable technology (60%), and mobile applications at work (65%).
Question 18 sought to measure the respondents’ opinions of the influence of certain factors on managerial performance, with most items registering high values. Respondents’ opinions were significant in selecting fourth- and fifth-level responses in favor of these factors, as follows: infrastructure (72%), technical resources and medical technologies (76%), information resources (79%), material endowment (78%), financial resources (78%), human resources (79%), management processes and leadership (76%), strategic planning process (72%), innovation process (70%), the quality of medical services (81%), employee satisfaction (79%), and patient satisfaction (81%).
Attendance at conferences and specific technology events between 2019 and 2023 (Q19), measured by the number of instances of participation, is presented as follows: 40 respondents (including 38 managers) had fewer than five instances of participation, 7 respondents (including 4 managers) had between 6 and 10 instances of participation, and 10 respondents (including 8 managers) had more than 11 instances of participation.
Hypothesis 3.
“There is a difference in perception of the adoption of innovation in a medical institution depending on the level of the managers.”
We used the independent-sample t-test to test whether there were statistical differences between the means of the groups “Non-managerial employees” (N = 43) and “Top Management” (N = 42) regarding the perception of the “Innovation Process” as a factor of influence for managerial performance. The scores corresponding to the dependent variable “Innovation Process” were obtained using the numerical scale from 1 to 5 (where 1 is the lowest level, and 5 is the highest level).
Table 8 provides descriptive statistics for the two groups compared, including the mean and standard deviation, and Table 9 provides the results of the independent-samples t-test.

Table 8.
Group statistics.

Table 9.
Independent-sample t-test results.
The p-value of Levene’s Test (Sig.) was 0.025, less than the chosen significance level of α = 0.05), which means the null hypothesis was rejected. Therefore, we followed the line “Equal variances not assumed” for the t-test results.
The 42 respondents who expressed themselves regarding the innovation process (M = 4.26, SD = 0.939) compared to the 43 respondents from the control group (M = 3.70, SD = 1.301) recorded appreciably higher scores, t(76.455) = 2.297, p = 0.024.
The results obtained from the statistical analyses confirmed Hypothesis 1. The management level significantly influenced the perception of the innovation process as a factor of influence for managerial performance, which is particularly important in the context of digital transformation in the field.
Results
RES4.1. The technologies that influence managerial efficiency, according to the respondents, in descending order, are mobile applications at work, portable technology, Big Data, artificial intelligence/machine learning, virtual reality, and augmented reality.
These technologies improve management processes by facilitating quick access to information, automating tasks, and analyzing data for informed decision-making, thereby creating interactive and personalized work environments. Mobile apps allow managers and employees to share critical information efficiently, regardless of location, increasing flexibility and quick response to issues. Wearable technology provides real-time data on employee performance and working conditions, optimizing resources and improving workplace health and safety. Big Data and artificial intelligence/machine learning are essential for analyzing large volumes of data, identifying patterns and trends, predicting outcomes, and optimizing operations, helping managers make more informed strategic decisions. Virtual reality and augmented reality are revolutionizing training and meetings by providing interactive learning experiences and realistic simulations, improving employee skills and process efficiency. Thus, these integrated technologies not only automate and simplify managerial tasks but also create an innovative and adaptable work environment to meet an organization’s needs.
RES4.2. The most important factors in increasing the managerial performance role are patient satisfaction, the quality of medical services, information resources, employee satisfaction, and human resources.
These factors highlight the importance of a holistic approach to health management, in which the focus is not only on internal processes and operational efficiency but also on the experience and satisfaction of all parties involved, including patients and medical staff.
RES4.3. The management level and the perception of managerial performance significantly influenced the innovation process, which is particularly important in the context of digital transformation in the field.
Effective management, which recognizes the importance and potential of emerging technologies, can stimulate innovation and facilitate the adoption of new digital solutions, transforming the way healthcare services are delivered. Well-informed management, open to change, can create an organizational culture that values innovation and embraces new technologies. In addition, management that understands managerial performance and its impact on innovation can implement strategies that encourage the development and testing of innovative solutions, which is essential for overcoming internal resistance and accelerating the integration of emerging technologies into clinical and administrative processes. Such visionary management can significantly improve the quality and efficiency of healthcare services, ensuring sustainability and competitiveness in the ever-evolving digital landscape.
The results indicate that the RHS is encountering a significant challenge in implementing digital technologies. To succeed in this endeavor, it must consider various conditions, and relevant institutions must address the digital transformation process in an integrated manner.
The last question (Q21), with an open-text response, asked respondents to rank from 1 to 3 (with 1 being the first choice) the countries/health systems in which they would like to exercise their profession/position as a manager of healthcare services from the perspective of digital transformation in the field. Because another challenge for the RHS, which has been important for the RHS for more than 30 years, is the migration of medical personnel, we also investigated this challenge. France was the first choice (18%, total of choices = 118) and the second choice (17%, total of choices = 100), and Great Britain was the third choice (16%, total of choices = 104).
For Romanian medical personnel, the decision to migrate abroad is motivated by several factors: practicing one’s profession in the best possible conditions and, implicitly, for career development, due to the curiosity to try something new or start a career in another country, specific to professionals at the beginning of their career, and based on the social environment as a whole [69].
5. Discussion
A series of challenges can be identified in the Romanian healthcare system, such as the outdated infrastructure and the lack of hospital construction, the migration of doctors to other countries, the underfunding of healthcare, recovery, and resilience after the crisis caused by the COVID-19 pandemic, structural reforms, the aging of the population, or the confidence of the population [1,2,8,77,78,79]. Facing a significant increase in the elderly population, efforts in rethinking the medical and social care system based on the integration of digital technologies must consider the specific needs of this category, factors such as accessibility, comfort with technologies, or socio-demographic features [80].
Specialists who provided answers in this study believed the field of education and management experience (87%) represent conditions for the rapid implementation of digital technologies. Specialized educational institutions must adapt their curricula in order to train medical staff to use new technologies. Currently, the National Institute of Health Services Management is the only official institution that offers such courses, though they last only a few weeks [81].
Based on the opinions and perceptions of managers and staff in the health field, dedicated funding sources (95%) are the most important condition for implementing digital technologies. Another condition reported by health specialists is establishing an effective national strategy (90%). Competent institutions have already taken some steps in this regard.
Romania ranks last in the Digital Economy and Society Index (DESI) 2020 among EU member states, considering the following variables: human capital, connectivity, the integration of digital technology, and digital public services. To address these deficiencies, the contribution for the digital domain within Romania’s Recovery and Resilience Plan is 5.97 billion EUR, with 1.817 billion EUR allocated to Component 7 (Digital Transformation) [82]. According to Decision (EU) 2022/2481, the National Action Plan on the Digital Decade for Romania 2030 was developed as a strategic document in digital transformation. As part of Measure 4—the creation of the e-health and telemedicine system, with a proposed completion in 2025, the allocated budget is 400 million EUR [83]. Within Component 7—Digital Transformation, specific investment I3.2—Digitalization of institutions with attributions in the health field subordinated to the Ministry of Health, a budget of 21.5 million EUR was allocated for the 41 County Public Health Directorates (including that of the municipality of Bucharest), with a maximum value of 0.5 million EUR/project, giving equal chances to each county [84,85]. For specific investment I3.3—Investments in IT systems and digital infrastructure of public health units, the Ministry of Health allocated a budget of 100 million EUR [86].
Another condition indicated by specialists was a proactive attitude at relevant ministries (88%). In this sense, the Ministry of Health is fair in distributing funds at the national level for digitalizing health services from a geographical point of view. The digitalization process’s effectiveness is also achieved by avoiding the gap between territorial administrative units, thus guaranteeing the access of all people to digitized services.
Another condition reported by specialists in this study is updated legislation (91%). The Romanian Government approved a decision establishing the services that qualify as telemedicine services, the 51 specialties in which telemedicine services can be provided, and the conditions for the organization and operation of telemedicine, respectively, the modalities of providing telemedicine services [87]. In this idea, 131 emergency reception units and emergency reception departments operating in hospitals in county-seat municipalities, other municipalities, and cities will be equipped with telemedicine equipment—a World Bank project worth 1.3 million EUR [88].
Most specialists consider that, due to its decentralized decision-making power, the private medical sector implements modern technologies more effectively than the state sector (72%). For example, the private health network Regina Maria implemented the most complex telemedicine solution in Romania, the Virtual Clinic, in just ten days, together with Microsoft, during the onset of the COVID-19 pandemic [89].
Specialists consider the quality of national infrastructure (89%) to be an important condition for implementing new technologies. If, since the fall of the communist regime in Romania, only one hospital was built “from scratch”, with an investment of 68 million EUR [90], the situation has seen a positive change via the allocation of funding of almost 1.23 billion EUR for the continuation of investments in regional emergency hospitals that will be built in Iași, Cluj-Napoca, and Craiova [91]. The project has a total value of about 1.6 billion EUR, and it creates more than 6000 full-time jobs [92].
The construction of regional hospitals offers solutions for many of the problems faced by the Romanian Health System, which were also revealed by the respondents in the study, such as new infrastructure with integrated digital technologies, providing quality care via multi-disciplinary teams, reducing the phenomenon of the migration of professionals to other countries, moving to smart management, and interoperability. The start of investments in the implementation of telemedicine and the updating of the corresponding legislation, the digitalization of health services, or the construction of new, high-capacity hospitals shows that the Romanian Health System is taking important steps in the global context of digital transformation of the health field.
Limitations of the study—The research method and instrument presented risks in collecting answers, and the obligation to complete all items determined a high degree of abandonment, which reduced the volume of the sample. The redundancy of potential respondents, the lack of a database with managers’ emails and not those of their institutions, and the impossibility of measuring the impact of the adoption of digital technologies on managerial performance, due both to the lack of standardized items in the research instrument and to the low level of technology implementation, were also limitations.
6. Conclusions
The process of digital transformation in the field of healthcare is in full swing worldwide, entering an irreversible path, so it is essential to have an integrated approach for these institutions in the implementation of new technologies, making the management process more efficient, increasing the quality of health services, and providing access to medical care for as many people as possible.
The analysis of the digital transformation process in healthcare in Romania reveals that it has implications in several important directions: technological, professional, educational, social, and administrative. As a result of testing the hypotheses corresponding to the research questions, we draw the following conclusions:
C1. Romanian health service managers have the qualifications and experience needed to facilitate the rapid adoption of digital technologies.
C2. There are differences in opinions and perceptions between specialists from the state sector and those from the private sector regarding the conditions for implementing digital technologies in the health system, especially at the level of health units.
C3. Specialists from Romanian health services are updated on the level of implementation of digital technologies, signaling significant differences between the level of implementation in the Romanian Health System and the worldwide level.
C4. According to health specialists, the integration of digital technologies in the health system increases the efficiency and performance of health services management in Romania.
The major contribution of this paper consists of the results obtained and interpreted by us, based on data obtained from active health professionals and processed using specific statistical methods, showing the respondents’ views on the current state of RHS digitalization from multiple perspectives on the process. This research could represent an important benchmark for other research involving the institutions at the government level.
Finally, we consider digital transformation to require an integrated systems approach based on exchanges of best practices worldwide to raise awareness among the population about the benefits of integrating digital technologies in healthcare facilities.
Author Contributions
Conceptualization, N.R. and E.E.; methodology, E.E.; software, N.R. and E.E.; validation, N.R.; formal analysis, E.E.; investigation, N.R.; resources, N.R. and E.E.; data curation, N.R.; writing—original draft preparation, N.R.; writing—review and editing, N.R. and E.E.; visualization, N.R.; supervision, E.E.; project administration, N.R. and E.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Regarding the Institutional Review Board Statement, ethical review and approval of this study was non-interventional, and the confidentiality of the respondents was maintained through the responses being completely anonymous, and only aggregated data are presented. The study was conducted according to the guidelines of the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in this study are included in the article; further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- State of Health in the EU, România. Profilul de Țară din 2023. Available online: https://health.ec.europa.eu/system/files/2024-01/2023_chp_ro_romanian.pdf (accessed on 2 April 2024).
- Arpad, L. Românii Își Exprimă Nemulțumirea Față de Sistemul Sanitar din Țară. Available online: https://www.ipsos.com/ro-ro/romanii-isi-exprima-nemultumirea-fata-de-sistemul-sanitar-din-tara (accessed on 2 April 2024).
- Miron, A. O radiografie a sistemului de sănătate din România. Rev. Științe Politice Polis 2020, 8, 201–212. Available online: https://revistapolis.ro/o-radiografie-a-sistemului-de-sanatate-din-romania/ (accessed on 2 April 2024).
- Mihalache, I.C.; Apetroi (Răcoare), F.C. The Evolution of the Financing of Health Services in Romania, from the Semashko Model to the Bismarck Model. Rev. Econ. Bus. Stud. 2020, 13, 137–147. [Google Scholar] [CrossRef]
- Petre, I.; Barna, F.; Gurgus, D.; Tomescu, L.C.; Apostol, A.; Petre, I.; Furau, C.; Năchescu, M.L.; Bordianu, A. Analysis of the Healthcare System in Romania: A Brief Review. Healthcare 2023, 11, 2069. [Google Scholar] [CrossRef] [PubMed]
- Vankar, P. Health Ranking of European Countries in 2023, by Health Index Score. Available online: https://www.statista.com/statistics/1376355/health-index-of-countries-in-europe/ (accessed on 2 April 2024).
- Institutul Național de Statistică. Comunicat de Presă Nr 167/3 Iulie 2023. Activitatea Rețelei Sanitare și de Ocrotire a Sănătății în Anul 2022. Available online: https://insse.ro/cms/ro/tags/comunicat-activitati-unitati-sanitare (accessed on 3 April 2024).
- Rajaei, O.; Khayami, S.R.; Rezaei, M.S. Smart hospital definition: Academic and industrial perspective. Int. J. Med. Inform. 2024, 182, 105304. [Google Scholar] [CrossRef] [PubMed]
- How BIM and Smart Building Technology Can Transform Healthcare. Available online: https://www.linkedin.com/pulse/how-bim-smart-building-technology-can-transform-earnest-j-morgan-6saqe/ (accessed on 7 April 2024).
- Chen, J.K.C.; Ho, H.-H. Asset Resource Optimization Solution for Smart Hospital Facilities and Energy Management through an Interpretive Structural Model. Buildings 2023, 13, 3064. [Google Scholar] [CrossRef]
- Zhang, G.-W.; Gong, M.; Li, H.-J.; Wang, S.; Gong, D.-X. The “Trinity” smart hospital construction policy promotes the development of hospitals and health management in China. Front. Public Health 2023, 11, 1219407. [Google Scholar] [CrossRef]
- Lin, C.-L.; Chen, J.K.C.; Ho, H.-H. BIM for Smart Hospital Management during COVID-19 Using MCDM. Sustainability 2021, 13, 6181. [Google Scholar] [CrossRef]
- Gaikwad, G.; Chaitanya, V.M.; Rohit, K.; Sunakshi, P. Smart Hospital Management System: Streamlining Healthcare Operations with SQL Integration. J. Trends Comput. Sci. Smart Technol. 2024, 6, 112–124. [Google Scholar] [CrossRef]
- Zhao, X.; Wu, S.; Yan, B.; Liu, B. New evidence on the real role of digital economy in influencing public health efficiency. Sci. Rep. 2024, 14, 7190. [Google Scholar] [CrossRef]
- Lyu, Y.; Peng, Y.; Liu, H.; Hwang, J.-J. Impact of Digital Economy on the Provision Efficiency for Public Health Services: Empirical Study of 31 Provinces in China. Int. J. Environ. Res. Public Health 2022, 19, 5978. [Google Scholar] [CrossRef]
- Kwilinski, A.; Szczepanska-Woszczyna, K.; Lyulyov, O.; Pimonenko, T. Digital Public Services: Catalysts for Healthcare Efficiency. J. Open Innov. Technol. Mark. Complex. 2024, 10, 100319. [Google Scholar] [CrossRef]
- Vărzaru, A.A. Assessing Digital Transformation of Cost Accounting Tools in Healthcare. Int. J. Environ. Res. Public Health 2022, 19, 15572. [Google Scholar] [CrossRef] [PubMed]
- Senbekov, M.; Saliev, T.; Bukeyeva, Z.; Almabayeva, A.; Zhanaliyeva, M.; Aitenova, N.; Toishibekov, Y.; Fakhradiyev, I. The Recent Progress and Applications of Digital Technologies in Healthcare: A Review. Int. J. Telemed. Appl. 2020, 2020, 8830200. [Google Scholar] [CrossRef] [PubMed]
- Biancuzzi, H.; Dal Mas, F.; Bidoli, C.; Pegoraro, V.; Zantedeschi, M.; Negro, P.A.; Campostrini, S.; Cobianchi, L. Economic and Performance Evaluation of E-Health before and after the Pandemic Era: A Literature Review and Future Perspectives. Int. J. Environ. Res. Public Health 2023, 20, 4038. [Google Scholar] [CrossRef] [PubMed]
- Electronic Health Record (EHR). Available online: https://www.techtarget.com/searchhealthit/definition/electronic-health-record-EHR (accessed on 3 April 2024).
- Alnashmi, M.; Salman, A.; AlHumaidi, H.; Yunis, M.; Al-Enezi, N. Exploring the Health Information Management System of Kuwait: Lessons and Opportunities. Appl. Syst. Innov. 2022, 5, 25. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef]
- What Is Telemedicine? Available online: https://www.news-medical.net/health/What-is-Telemedicine.aspx (accessed on 3 April 2024).
- Fonda, F.; Galazzi, A.; Chiappinotto, S.; Justi, L.; Frydensberg, M.S.; Boesen, R.L.; Macur, M.; Reig, E.A.; Espaulella, E.R.; Palese, A. Healthcare System Digital Transformation across Four European Countries: A Multiple-Case Study. Healthcare 2024, 12, 16. [Google Scholar] [CrossRef]
- Jang, M. Why Do People Use Telemedicine Apps in the Post-COVID-19 Era? Expanded TAM with E-Health Literacy and Social Influence. Informatics 2023, 10, 85. [Google Scholar] [CrossRef]
- Schroer, A. 13 Examples of Wearable Technology in Healthcare and Wearable Medical Devices. Available online: https://builtin.com/articles/wearable-technology-in-healthcare (accessed on 3 April 2024).
- Nasiri, S.; Khosravani, M.R. Progress and challenges in fabrication of wearable sensors for health monitoring. Sens. Actuators A Phys. 2020, 312, 112105. [Google Scholar] [CrossRef]
- What Is Artificial Intelligence (AI)? Available online: https://www.ibm.com/topics/artificial-intelligence (accessed on 4 April 2024).
- Davenport, T.; Kalakota, R. The potential for artificial intelligence in healthcare. Future Healthc. J. 2019, 6, 94–98. [Google Scholar] [CrossRef]
- Understanding Virtual Reality and Augmented Reality. Available online: https://edu.gcfglobal.org/en/thenow/understanding-virtual-reality-and-augmented-reality/1/?_x_tr_hist=true (accessed on 4 April 2024).
- Aliwi, I.; Schot, V.; Carrabba, M.; Duong, P.; Shievano, S.; Caputo, M.; Wray, J.; de Vecchi, A.; Biglino, G. The Role of Immersive Virtual Reality and Augmented Reality in Medical Communication: A Scoping Review. J Patient Exp. 2023, 27, 23743735231171562. [Google Scholar] [CrossRef] [PubMed]
- Mutabazi, P. How Augmented Reality (AR) and Virtual Reality (VR) Are Transforming the Healthcare Sector. Available online: https://www.linkedin.com/pulse/how-augmented-realityar-virtual-realityvr-healthcare-sector-mutabazi/ (accessed on 4 April 2024).
- Dash, S.; Shakyawar, S.K.; Sharma, M.; Kaushik, S. Big data in healthcare: Management, analysis and future prospects. J. Big Data 2019, 6, 54. [Google Scholar] [CrossRef]
- Big Data in Healthcare: Transforming Patient Experience and Access. Available online: https://populi.ai/big-data-in-healthcare-transforming-patient-experience-and-access/ (accessed on 4 April 2024).
- Pires, I.M.; Marques, G.; Garcia, N.M.; Flórez-Revuelta, F.; Ponciano, V.; Oniani, S. A Research on the Classification and Applicability of the Mobile Health Applications. J. Pers. Med. 2020, 10, 11. [Google Scholar] [CrossRef] [PubMed]
- Wylie, L. Health App Revenue and Usage Statistics. 2024. Available online: https://www.businessofapps.com/data/health-app-market/ (accessed on 4 April 2024).
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R.; Rab, S. Blockchain technology applications in healthcare: An overview. Int. J. Intell. Netw. 2021, 2, 130–139. [Google Scholar] [CrossRef]
- Blockchain: Opportunities for Health Care. Available online: https://www2.deloitte.com/us/en/pages/public-sector/articles/blockchain-opportunities-for-health-care.html (accessed on 4 April 2024).
- Ce Este IoT? Available online: https://www.oracle.com/ro/internet-of-things/what-is-iot/ (accessed on 5 April 2024).
- Razdan, S.; Sharma, S. Internet of Medical Things (IoMT): Overview, Emerging Technologies, and Case Studies. IETE Tech. Rev. 2022, 39, 775–788. [Google Scholar] [CrossRef]
- Voice Search Could Improve Healthcare for Patients and Providers Alike. Available online: https://www.mdconnectinc.com/medical-marketing-insights/medical-marketing-insights/voice-search-improve-healthcare-patients-providers (accessed on 6 April 2024).
- Voice Search and SEO For Healthcare Practices. Available online: https://www.sequencehealth.com/blog/voice-search-and-seo-for-healthcare-practices (accessed on 5 April 2024).
- The Value of Video Marketing in Healthcare. Available online: https://levohealth.com/the-value-of-video-marketing-in-healthcare/ (accessed on 5 April 2024).
- Pianese, T.; Belfiore, P. Exploring the Social Networks’ Use in the Health-Care Industry: A Multi-Level Analysis. Int. J. Environ. Res. Public Health 2021, 18, 7295. [Google Scholar] [CrossRef]
- Future of Social Networks in Healthcare: Revolutionizing the Industry. Available online: https://www.quantumog.com/post/future-of-social-networks-in-healthcare (accessed on 7 April 2024).
- Powell, M. How 3D Printing Is Impacting the Medical Field. Available online: https://www.med-technews.com/medtech-insights/medtech-materials-and-assembly-insights/how-3d-printing-is-impacting-the-medical-field/ (accessed on 7 April 2024).
- Satam, H.; Joshi, K.; Mangrolia, U.; Waghoo, S.; Zaidi, G.; Rawool, S.; Thakare, R.P.; Banday, S.; Mishra, A.K.; Das, G.; et al. Next-Generation Sequencing Technology: Current Trends and Advancements. Biology 2023, 12, 997. [Google Scholar] [CrossRef]
- Three Ways Nanotechnology Is Changing the Healthcare Industry. Available online: https://www.forbes.com/sites/forbestechcouncil/2022/07/20/three-ways-nanotechnology-is-changing-the-healthcare-industry/ (accessed on 7 April 2024).
- Teixeira, L.; Cardoso, I.; Oliveira e Sá, J.; Madeira, F. Are Health Information Systems Ready for the Digital Transformation in Portugal? Challenges and Future Perspectives. Healthcare 2023, 11, 712. [Google Scholar] [CrossRef]
- Dijkman, E.M.; ter Brake, W.W.M.; Drossaert, C.H.C.; Doggen, C.J.M. Assessment Tools for Measuring Health Literacy and Digital Health Literacy in a Hospital Setting: A Scoping Review. Healthcare 2024, 12, 11. [Google Scholar] [CrossRef]
- Rusu, B.; Sandu, C.B.; Avasilcai, S.; David, I. Acceptance of Digital Transformation: Evidence from Romania. Sustainability 2023, 15, 15268. [Google Scholar] [CrossRef]
- Strategia Națională de Sănătate 2023–2030. Available online: https://ms.ro/media/documents/Anexa_1_-_SNS.pdf (accessed on 3 April 2024).
- Epizitone, A.; Moyane, S.P.; Agbehadji, I.E. A Systematic Literature Review of Health Information Systems for Healthcare. Healthcare 2023, 11, 959. [Google Scholar] [CrossRef] [PubMed]
- Shaping Europe’s Digital Future. Available online: https://digital-strategy.ec.europa.eu/en/policies/ehealth (accessed on 3 April 2024).
- Horgan, D.; Hackett, J.; Westphalen, C.B.; Kalra, D.; Richer, E.; Romao, M.; Andreu, A.L.; Lal, J.A.; Bernini, C.; Tumiene, B.; et al. Digitalisation and COVID-19: The Perfect Storm. Biomed. Hub. 2020, 17, 1341–1363. [Google Scholar] [CrossRef] [PubMed]
- Svensson, A.; Gustavsson, L.; Svenningsson, I.; Karlsson, C.; Karlsson, T. Healthcare professionals learning when implementing a digital artefact identifying patients’ cognitive impairment. J. Workplace Learn. 2023, 35, 490–505. [Google Scholar] [CrossRef]
- Ionașcu, A.E.; Gheorghiu, G.; Spătariu, E.C.; Munteanu, I.; Grigorescu, A.; Dănilă, A. Unraveling Digital Transformation in Banking: Evidence from Romania. Systems 2023, 11, 534. [Google Scholar] [CrossRef]
- Căpușneanu, S.; Mateș, D.; Tűrkeș, M.C.; Barbu, C.-M.; Staraș, A.-I.; Topor, D.I.; Stoenică, L.; Fűlöp, M.T. The Impact of Force Factors on the Benefits of Digital Transformation in Romania. Appl. Sci. 2021, 11, 2365. [Google Scholar] [CrossRef]
- Barbu, M.; Vevera, A.V.; Barbu, D.C. Standardization and Interoperability—Key Elements of Digital Transformation. In Digital Transformation. Intelligent Systems Reference Library; Cioca, L.I., Ivascu, L., Filip, F.G., Doina, B., Eds.; Springer: Cham, Switzerland, 2024; Volume 253. [Google Scholar] [CrossRef]
- Lehne, M.; Sass, J.; Essenwanger, A.; Schepers, J.; Thun, S. Why digital medicine depends on interoperability. NPJ Digit. Med. 2019, 2, 79. [Google Scholar] [CrossRef]
- Brewer, L.C.; Fortuna, K.L.; Jones, C.; Walker, R.; Hayes, S.N.; Patten, C.A.; Cooper, L.A. Back to the Future: Achieving Health Equity Through Health Informatics and Digital Health. JMIR Mhealth Uhealth 2020, 8, e14512. [Google Scholar] [CrossRef]
- Aggestam, L.; van Laere, J.; Svensson, A. How to Apply and Manage Critical Success Factors in Healthcare Information Systems Development? Systems 2023, 11, 469. [Google Scholar] [CrossRef]
- Ţiţan, E.; Manea, D.I.; Mihai, M.; Ionescu, C.D. Digital transformation in healthcare. The need for medical technologies. Rev. Romana Econ. 2023, 56. Available online: http://www.revecon.ro/articles/2023-1/2023-1-2.pdf (accessed on 10 September 2024).
- Peck, C.; McCall, M.; McLaren, B.; Rotem, T. Continuing medical education and continuing professional development: International comparisons. BMJ 2000, 320, 432–435. [Google Scholar] [CrossRef]
- Continuing Your Professional Development as a Doctor. Available online: https://www.bmj.com/careers/article/continuing-your-professional-development-as-a-doctor (accessed on 26 July 2024).
- What Is the Purpose of Medical Conferences? Available online: https://within3.com/blog/purpose-of-medical-conferences (accessed on 26 July 2024).
- Filc, D.; Rasooly, A.; Davidovitch, N. From public vs. private to public/private mix in healthcare: Lessons from the Israeli and the Spanish cases. Isr. J. Health Policy Res. 2020, 9, 31. [Google Scholar] [CrossRef] [PubMed]
- Understanding Public and Private Health Care. Available online: https://www.cma.ca/our-focus/public-and-private-health-care/understanding-public-and-private-health-care (accessed on 26 July 2024).
- Kumpf, B.; Proud, E. The Adoption of Innovation. In Stanford Social Innovation Review; Stanford Center on Philanthropy and Civil Society: Stanford, CA USA, 2022. [Google Scholar] [CrossRef]
- Turner, S.; D’Lima, D.; Hudson, E.; Morris, S.; Sheringham, J.; Swart, N.; Fulop, N.J. Evidence use in decision-making on introducing innovations: A systematic scoping review with stakeholder feedback. Implement. Sci. 2017, 12, 145. [Google Scholar] [CrossRef] [PubMed]
- Norton, P.T.; Rodriguez, H.P.; Shortell, S.M.; Lewis, V.A. Organizational influences on healthcare system adoption and use of advanced health information technology capabilities. Am. J. Manag. Care 2019, 25, e21–e25. [Google Scholar] [PubMed]
- Sekaran, U. Data Analysis and Interpretation. In Research Methods for Business; Wiley and Sons: New York, NY, USA, 2008; p. 311. [Google Scholar]
- Organizarea Administrativ-Teritorială. Available online: https://arges.insse.ro/produse-si-servicii/statistici-judetene/organizarea-administrativ-teritoriala/ (accessed on 6 April 2024).
- Andrei, T. Tehnici nealeatoare de esantionare utilizate în practica statistica. Rev. Inform. Econ. 2021, nr. 2 (18)/2001. [Google Scholar]
- Barbu, A.; Testul Fisher F cu Valori Semnificative mici în Eşantioane de Volum Redus. Romanian Statistical Review. 2011. Available online: https://www.revistadestatistica.ro/Articole/2011/A5ro_rrs%204_2011.pdf (accessed on 7 April 2024).
- Legea Nr. 315 din 28 Iunie 2004 Privind Dezvoltarea Regională în România. Available online: https://legislatie.just.ro/Public/DetaliiDocument/53040 (accessed on 6 April 2024).
- Raport de Țară România. Available online: https://cstor.eu/pillarsofhealth/2022/11/5731a67d-pillars-of-health_raport-tara_romania-_romanian_november-2022.pdf (accessed on 8 April 2024).
- În România s-au Construit Doar 4 Spitale de Stat în Ultimii 32 de Ani. Întârzierile au Fost Mari. Available online: https://newsweek.ro/sanatate/in-romania-s-au-construit-doar-4-spitale-in-ultimii-32-de-ani-autoritatile-promit-inca-25-in-4-ani (accessed on 8 April 2024).
- Planul Național de Redresare și Reziliență al României: Situația cea mai Recentă. Available online: https://www.europarl.europa.eu/thinktank/ro/document/EPRS_BRI(2022)733641 (accessed on 8 April 2024).
- Jimenez, J.; del Rio, A.; Berman, A.N.; Grande, M. Personalizing Digital Health: Adapting Health Technology Systems to Meet the Needs of Different Older Populations. Healthcare 2023, 11, 2140. [Google Scholar] [CrossRef]
- Cursuri de Management Servicii de Sănătate Susținute de INMSS. Available online: https://inmss.ro/cursuri-management/ (accessed on 8 April 2024).
- Indicele Economiei și Societății Digitale (DESI) 2022 România. Available online: https://ec.europa.eu/newsroom/dae/redirection/document/88717 (accessed on 8 April 2024).
- Planul Național de Acțiune Privind Deceniul Digital Pentru România 2030. Available online: https://www.mcid.gov.ro/wp-content/uploads/2024/04/Plan-national-de-actiune-roadmap-pentru-publicare.pdf (accessed on 9 April 2024).
- Fisa Proiect PNRR C7. I3.2—Digitalizarea Instituțiilor Sanitare din Subordinea MS. Available online: https://www.fonduri-structurale.ro/fisa-proiect/23/planul-national-de-redresare-si-rezilienta/661/pnrr-c7-i3-2-digitalizarea-institutiilor-sanitare-din-subordinea-ms (accessed on 10 April 2024).
- Lista Obiectivelor de Investiţii Aprobate pentru Finanţare prin PNRR. Direcţiile de Sănătate Publică Judeţene (Inclusiv cea a Municipiului Bucureşti). Available online: https://ms.ro/media/documents/Lista_obiective_aprobate_pentru__finantare____PNRR___Digitalizare___DSP.pdf (accessed on 10 April 2024).
- Componenta 7—Transformare Digitală. Investitia Specifică: I3.3—Investiții în Sistemele Informatice și în Infrastructura Digitală a Unităților Sanitare Publice. Available online: https://ms.ro/ro/de-interes/apeluri-pnrr-c12-sanatate/componenta-7-transformare-digital%C4%83-investitia-specific%C4%83-i33-investi%C8%9Bii-%C3%AEn-sistemele-informatice-%C8%99i-%C3%AEn-infrastructura-digital%C4%83-a-unit%C4%83%C8%9Bilor-sanitare-publice/ (accessed on 10 April 2024).
- Hotărârea de Guvern Nr. 1133/2022 Privind Aprobarea Normelor Metodologice de Punere în Aplicare a Prevederilor Ordonanţei de Urgenţă a Guvernului Nr. 196/2020 pentru Modificarea şi Completarea Legii nr. 95/2006 Privind Reforma în Domeniul Sănătăţii. Available online: https://legislatie.just.ro/Public/DetaliiDocument/259367 (accessed on 3 April 2024).
- Unitățile de Primire Urgențe (UPU) vor fi Dotate cu Echipamente de Telemedicină de Ultimă Generație. Available online: https://www.ms.ro/ro/centrul-de-presa/unit%C4%83%C8%9Bile-de-primire-urgen%C8%9Be-upu-vor-fi-dotate-cu-echipamente-de-telemedicin%C4%83-de-ultim%C4%83-genera%C8%9Bie/ (accessed on 9 April 2024).
- Medicina Digitală Atinge un Nou Record în România: 1 Milion de Programări Online. Available online: https://www.reginamaria.ro/stiri/medicina-digitala-atinge-un-nou-record-romania-1-milion-de-programari-online (accessed on 10 April 2024).
- Cum Arata Primul Spital Construit de la Zero de Statul Roman in Ultimii 30 de Ani. Available online: https://www.wall-street.ro/articol/Social/244355/foto-cum-arata-primul-spital-construit-de-la-zero-de-statul-roman-in-ultimii-30-de-ani.html#gref (accessed on 10 April 2024).
- Lista Proiectelor Selectate la Finanțare—Apel PS/170/PS_P4/OP4/RSO4.5/PS_P4_RSO4.5_A8. Available online: https://mfe.gov.ro/wp-content/uploads/2023/05/398676f62db77b73a4086c29bdebce3a.pdf (accessed on 9 April 2024).
- A Quick Trip to the Hospital. Available online: https://www.eib.org/en/stories/romania-regional-hospitals (accessed on 10 April 2024).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).