Wearable Technology and Visual Reality Application for Healthcare Systems
Abstract
1. Introduction
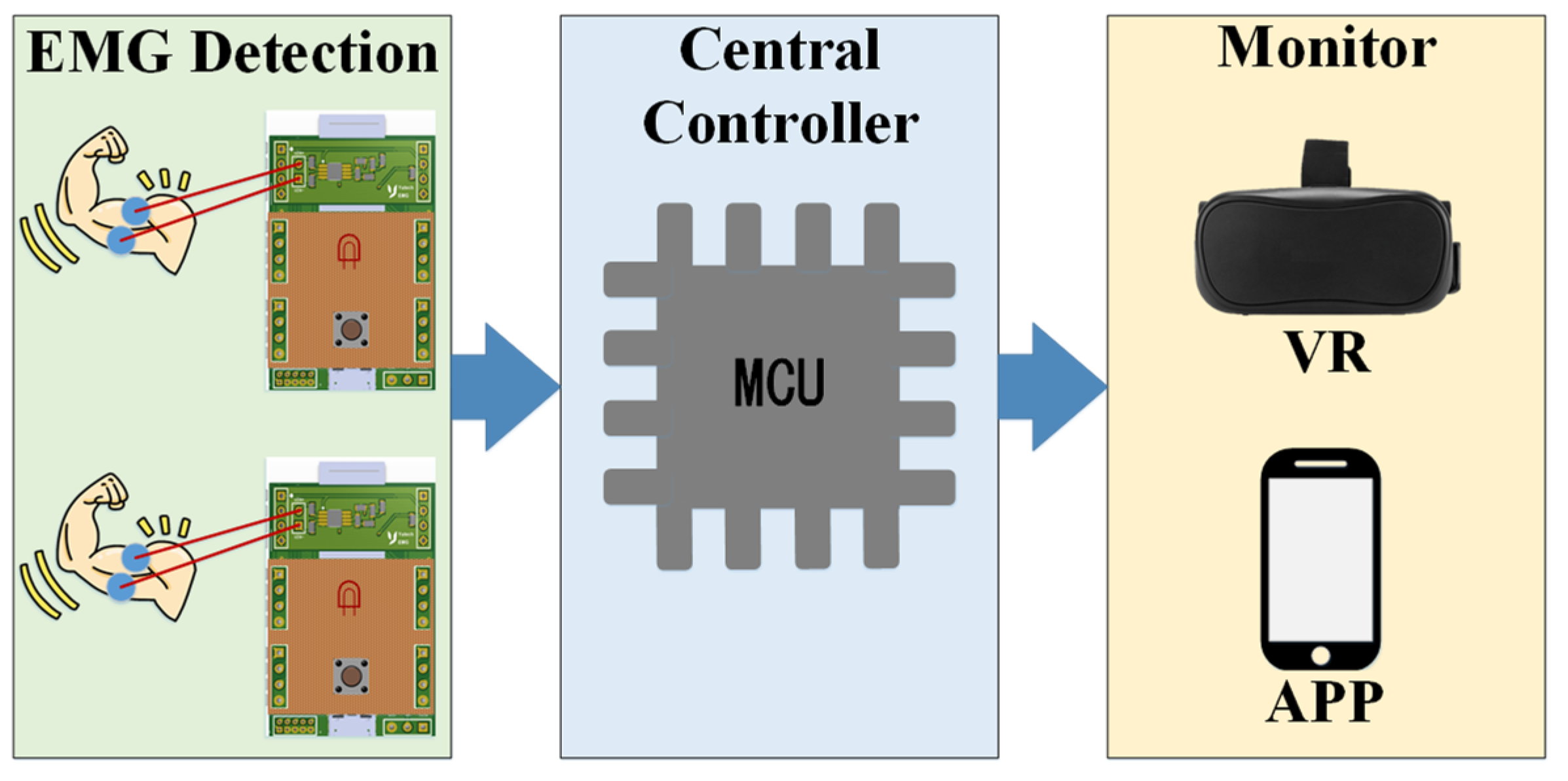
2. System Architecture
Hardware Architecture
3. EMG Peak Detection
3.1. System Flow
3.2. Algorithm
| Algorithm 1: S & C Algorithm. |
| Input: |
| Y(n) |
| Output: |
| 1: slope = 0 |
| 2: initial_slope_maxi = 0 |
| 3: for i: = 1 to 500 do |
| 4: if i ≥ 3 then |
| 5: slope = −2 × Y(i − 2) − Y(i − 1) + Y(i + 1) + 2 × Y(i + 2) |
| 6: if slope > initial_slope_maxi then |
| 7: initial_slope_maxi = slope |
| 8: end if |
| 9: end if |
| 10: end for |
| 11: maxi = initial_slope_maxi |
| Algorithm 2: ASM S & C Algorithm. |
| Input: |
| Y(n) |
| Output: |
| 1: initial_value = avg(sum(Y(1:n))) × (λ + 1) |
| 2: slope = 0 |
| 3: initial_slope_maxi = 0 |
| 4: count = 0 |
| 5: en = 0 |
| 6: for i:= 1 to length(Y) do |
| 7: if I ≥ 3 && Y(i) > initial_value then |
| 8: initial_slope_maxi = −2 × Y(I — 2)−Y(I — 1)+Y(I + 1)+2 × Y(I + 2) |
| 9: count = count + i |
| 10: break |
| 11: end if |
| 12: end for |
| 13: for i:= count to length(Y) do |
| 14: slope = −2 × Y(I — 2) — Y(I — 1) + Y(I + 1) + 2 × Y(I + 2) |
| 15: if slope > initial_slope_maxi then |
| 16: en = 1 |
| 17: end if |
| 18: if en == 1 then |
| 19: if slope < initial_slope_maxi then |
| 20: initial_slope_maxi = old_slope |
| 21: break |
| 22: end if |
| 23: end if |
| 24: end for |
| 25: maxi = initial_slope_maxi |
4. Experimental Results
4.1. Electromyography
4.2. Virtual Reality
4.3. The App
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Spanò, E.; Pascoli, S.D.; Iannaccone, G. Low-Power Wearable ECG Monitoring System for Multiple-Patient Remote Monitoring. IEEE Sensors J. 2016, 16, 5452–5462. [Google Scholar] [CrossRef]
- Satija, U.; Ramkumar, B.; Manikandan, M.S. Real-Time Signal Quality-Aware ECG Telemetry System for IoT-Based Health Care Monitoring. IEEE IoT J. 2017, 4, 815–823. [Google Scholar] [CrossRef]
- Borulkar, N.; Pandey, P.; Davda, C.; Chettiar, J. Drowsiness Detection and Monitoring the Sleeping Pattern using Brainwaves Technology and IoT. In Proceedings of the 2018 2nd International Conference on I-SMAC, Palladam, India, 30–31 August 2018; pp. 703–706. [Google Scholar]
- Daoud, H.; Williams, P.; Bayoumi, M. IoT based Efficient Epileptic Seizure Prediction System Using Deep Learning. In Proceedings of the 2020 IEEE 6th World Forum on IoT (WF-IoT), New Orleans, LA, USA, 2–16 June 2020; pp. 1–6. [Google Scholar]
- Bhowmick, S.; Kundu, P.K.; Mandal, D.D. IoT Assisted Real Time PPG Monitoring System for Health Care Application. In Proceedings of the IEEE Second International Conference on Control, Measurement and Instrumentation (CMI), Kolkata, India, 8–10 January 2021; pp. 122–127. [Google Scholar]
- Huang, Q.; Wang, W.; Zhang, Q. Your Glasses Know Your Diet: Dietary Monitoring Using Electromyography Sensors. IEEE IoT J. 2017, 4, 705–712. [Google Scholar] [CrossRef]
- Marjani, M.; Nasaruddin, F.; Gani, A.; Karim, A.; Hashem, I.A.T.; Siddiqa, A.; Yaqoob, I. Big IoT Data Analytics: Architecture, Opportunities, and Open Research Challenges. IEEE Access 2017, 5, 5247–5261. [Google Scholar]
- Cai, H.; Xu, B.; Jiang, L.; Vasilakos, A.V. IoT-Based Big Data Storage Systems in Cloud Computing: Perspectives and Challenges. IEEE IoT J. 2017, 4, 75–87. [Google Scholar] [CrossRef]
- Sitzmann, V.; Serrano, A.; Pavel, A.; Agrawala, M.; Gutierrez, D.; Masia, B.; Wetzstein, G. Saliency in VR: How Do People Explore Virtual Environments? IEEE Trans. Vis. Comput. Graph. 2018, 24, 1633–1642. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Xie, Z.; Yu, Y.; Lee, J.; Vazquez-Guardado, A.; Luan, H.; Ruban, J.; Ning, X.; Akhtar, A.; Li, D. Skin-integrated wireless haptic interfaces for virtual and augmented reality. Nature 2019, 575, 473–479. [Google Scholar] [CrossRef] [PubMed]
- Ozkan, H.; Ozhan, O.; Karadana, Y.; Gulcu, M.; Macit, S.; Husain, F. A Portable Wearable Tele-ECG Monitoring System. IEEE Trans. Instrum. Meas. 2020, 69, 173–182. [Google Scholar] [CrossRef]
- Ensina, L.A.; Lee, H.D.; Takaki, W.S.R.; Maciejewski, N.A.R.; Spolaôr, N.; Wu, F.C. Heuristics-based Responsiveness Evaluation of a Telemedicine Computational Web System. IEEE Latin Am. Trans. 2019, 17, 444–452. [Google Scholar] [CrossRef]
- Narukiyo, S.; Tanaka, Y.; Aoyama, T.; Shiokawa, M. Scope of human manipulability sharing with VR device and EMG sensor for online motion analysis. In Proceedings of the IEEE/SICE International Symposium on System Integration (SII), Iwaki, Japan, 11–14 January 2021; pp. 831–832. [Google Scholar]
- Wen, F.; Zhang, Z.; He, T. AI enabled sign language recognition and VR space bidirectional communication using triboelectric smart glove. Nat. Commun. 2021, 12, 5378. [Google Scholar] [CrossRef] [PubMed]
- Sugiarto, T.; Hsu, C.-L.; Sun, C.-T.; Hsu, W.-C.; Ye, S.-H.; Lu, K.-T. Surface EMG vs. High-Density EMG: Tradeoff Between Performance and Usability for Head Orientation Prediction in VR Application. IEEE Access 2021, 9, 45418–45427. [Google Scholar] [CrossRef]
- Pancholi, S.; Jain, P.; Varghese, A.; Joshi, A.M. A Novel Time-Domain based Feature for EMG-PR Prosthetic and Rehabilitation Application. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 5084–5087. [Google Scholar]
- Raurale, S.A.; McAllister, J.; Rincón, J.M.D. EMG Biometric Systems Based on Different Wrist-Hand Movements. IEEE Access 2021, 9, 12256–12266. [Google Scholar] [CrossRef]
- Wang, C.-Y.; Chang, R.C.-H.; Lin, C.-H.; Su, S.-H. Fatigue Detection System Using Enhanced So and Chan Method. In Proceedings of the 2018 IEEE International Conference on Consumer Electronics-Taiwan (ICCE-TW), Taichung, Taiwan, 19–21 May 2018; pp. 1–2. [Google Scholar]
- Lee, C.; Choi, W.; Kwak, M.; Kim, S.; Hwang, H. Impact of electrolyte density on synaptic characteristics of oxygen-based ionic synaptic transistor. Small 2021, 17, 2103543. [Google Scholar] [CrossRef]
- Nikam, R.D.; Lee, J.; Choi, W.; Banerjee, W.; Kwak, M.; Yadav, M.; Hwang, H. Ionic Sieving Through One-Atom-Thick 2D Material Enables Analog Nonvolatile Memory for Neuromorphic Computing. Adv. Electron. Mater. 2021, 17, 2100142. [Google Scholar] [CrossRef]
- Friesen, G.M.; Jannett, T.C.; Jadallah, M.A.; Yates, S.L.; Quint, S.R.; Nagle, H.T. A Comparison of the Noise Sensitivity of Nine QRS Detection Algorithms. IEEE Trans. Biomed. Eng. 1990, 37, 85–98. [Google Scholar] [CrossRef] [PubMed]
- So, H.H.; Chan, K.L. Development of QRS Detection Method for Real-time Ambulatory Cardiac Monitor. In Proceedings of the 19th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 30 October–2 November 1997; pp. 289–292. [Google Scholar]
- Tan, K.F.; Chan, K.L.; Choi, K. Detection of the QRS Complex, P Wave and T Wave in Electrocardiogram. In Proceedings of the 2000 First International Conference Advances in Medical Signal and Information Processing, Bristol, UK, 4–6 September 2000; pp. 41–47. [Google Scholar]
- Lin, K.-H.; Wu, J.-H. Low-Cost High-Accuracy QRS Detection for Body Area Network Applications. J. Med. Biol. Eng. 2016, 36, 810–819. [Google Scholar] [CrossRef]
- Chiu, C.-C.; Lin, T.-H.; Liau, B.-Y. Using Correlation Coefficient in ECG Waveform for Arrhythmia Detection. Biomed. Eng. Appl. Basis Commun. 2005, 17, 147–152. [Google Scholar] [CrossRef][Green Version]
- Doheny, E.P.; Goulding, C.; Flood, M.W.; Mcmanus, L.; Lowery, M.M. Feature-Based Evaluation of a Wearable Surface EMG Sensor against Laboratory Standard EMG During Force-Varying and Fatiguing Contractions. IEEE Sensors J. 2020, 20, 2757–2765. [Google Scholar] [CrossRef]
- Merletti, R.; Lloyd, D.G.; Besier, T.F.; Fernandez, J.W.; Farina, D. Electromyography-Driven Modeling for Simulating Subject-Specific Movement at the Neuromusculoskeletal Level. In Surface Electromyography: Physiology, Engineering, and Applications; John Wiley& Sons, Inc.: Hoboken, NJ, USA, 2016; pp. 247–272. [Google Scholar]
- Francisc, D.S.; Flávio, D.S.; Alexandre, C.A.C. Classification of Hand Movements from EMG Signals for People with Motor Disabilities. IEEE Latin Am. Trans. 2020, 18, 2019–2026. [Google Scholar] [CrossRef]


















| Refrence | Algorithm | Complexity | Equipment |
|---|---|---|---|
| Sugiarto [15] | CNN | High | Delsys Trigno IMU |
| Pancholi [16] | LDA | High | I7 core |
| Raurale [17] | Subsequently classified | Medium | ARM Cortex A-53 |
| Wang [18] | Enhanced So and Chan | Low | FPGA |
| Our propose | ASM S&C | Low | nRF52840 |
| System Requirement | Equipment |
|---|---|
| Biomedical Development Platform | TriAnswer (Tri-BLE, Tri-EMG) |
| Central controller | Arduino UNO |
| Monitor | Virtual reality HTC-VIVE Cosmos Android Smartphones |
| Algorithm | SP (Data) | EP (Data) | MP (Data) | Accuracy (%) |
|---|---|---|---|---|
| ACD | 132 | 31 | 22 | 71.35 |
| S & C [22] | 154 | 54 | 0 | 74.08 |
| ASM S & C | 154 | 9 | 0 | 95.06 |
| Event | Time |
|---|---|
| EMG image update | 30 (s) |
| Hardware sampling | 3.3 (ms) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, K.-H.; Peng, B.-X. Wearable Technology and Visual Reality Application for Healthcare Systems. Electronics 2022, 11, 178. https://doi.org/10.3390/electronics11020178
Lin K-H, Peng B-X. Wearable Technology and Visual Reality Application for Healthcare Systems. Electronics. 2022; 11(2):178. https://doi.org/10.3390/electronics11020178
Chicago/Turabian StyleLin, Kuang-Hao, and Bo-Xun Peng. 2022. "Wearable Technology and Visual Reality Application for Healthcare Systems" Electronics 11, no. 2: 178. https://doi.org/10.3390/electronics11020178
APA StyleLin, K.-H., & Peng, B.-X. (2022). Wearable Technology and Visual Reality Application for Healthcare Systems. Electronics, 11(2), 178. https://doi.org/10.3390/electronics11020178






