Heart Rate Variability during Virtual Reality Activity in Individuals after Hospitalization for COVID-19: A Cross-Sectional Control Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Location
2.2. Inclusion Criteria
2.3. Exclusion Criteria
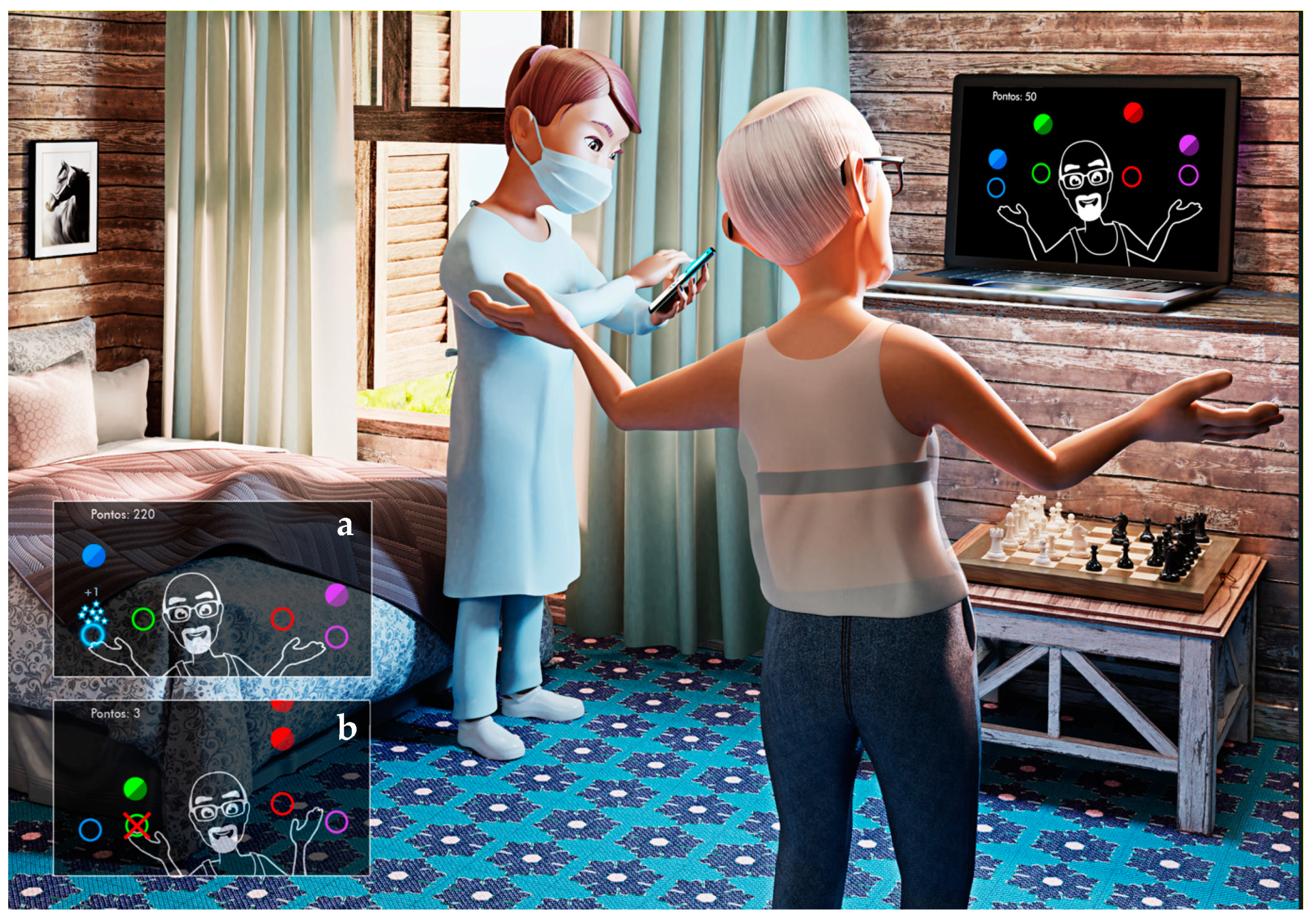
2.4. MoveHero—VR Activity
2.5. Characterization
2.6. Physiological Variables
2.7. Procedures
2.8. Age Groups
2.9. Heart Rate Variability (HRV)
2.10. Data Analysis
3. Results
3.1. Physiological Variables
3.2. Heart Rate Variability
3.2.1. Linear Indices—Time and Frequency Domain
3.2.2. Non-Linear Indices—Symbolic Dynamic Analysis
4. Discussion
4.1. Physiological Variables and HRV before, during, and after the Virtual Reality Game
4.2. Comparison of HRV between Groups and Different Ages
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, T.J.; Chau, B.; Lui, M.D.; Lam, G.-T.; Lin, N.; Humbert, S. Physical Medicine and Rehabilitation and Pulmonary Rehabilitation for COVID-19. Am. J. Phys. Med. Rehabil. 2020, 99, 769–774. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, E.; Lipsitch, M.; Cevik, M. On the Effect of Age on the Transmission of SARS-CoV-2 in Households, Schools, and the Community. J. Infect. Dis. 2020, 223, 362–369. [Google Scholar] [CrossRef] [PubMed]
- How the vagus nerve produces beat-to-beat heart rate variability; experiments in rabbits to mimic in vivo vagal patterns. J. Clin. Transl. Res. 2015, 1, 190–204. [CrossRef]
- Mol, M.B.A.; Strous, M.T.A.; van Osch, F.H.M.; Vogelaar, F.J.; Barten, D.G.; Farchi, M.; Foudraine, N.A.; Gidron, Y. Heart-rate-variability (HRV), predicts outcomes in COVID-19. PLoS ONE 2021, 16, e0258841. [Google Scholar] [CrossRef] [PubMed]
- Silveira, A.C.; Moraes, Í.A.P.; Vidigal, G.P.; Simcsik, A.O.; Rosa, R.M.; Favero, F.M.; Fernandes, S.M.S.; Garner, D.M.; Araújo, L.V.; Massa, M.; et al. Cardiac Autonomic Modulation in Subjects with Amyotrophic Lateral Sclerosis (ALS) during an Upper Limb Virtual Reality Task: A Prospective Control Trial. BioMed Res. Int. 2022, 2022, 4439681. [Google Scholar] [CrossRef]
- Dias, R.M.; Moraes, Í.A.P.; Dantas, M.T.A.P.; Fernani, D.C.G.L.; Fontes, A.M.G.G.; Silveira, A.C.; Barnabé, V.; Fernandes, M.; Martinelli, P.M.; Monteiro, C.B.M.; et al. Influence of Chronic Exposure to Exercise on Heart Rate Variability in Children and Adolescents Affected by Obesity: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 11065. [Google Scholar] [CrossRef]
- Moraes, Í.A.P.; Silva, T.D.; Massetti, T.; Menezes, L.D.C.; Ribeiro, V.F.; Tropiano, L.M.C.C.; Barnabé, V.; Hoshi, R.A.; Monteiro, C.B.M.; Fernandes, M. Fractal correlations and linear analyses of heart rate variability in healthy young people with different levels of physical activity. Cardiol. Young 2019, 29, 1236–1242. [Google Scholar] [CrossRef]
- Imamura, M.; Mirisola, A.R.; de Quadros Ribeiro, F.; De Pretto, L.R.; Alfieri, F.M.; Delgado, V.R.; Battistella, L.R. Rehabilitation of patients after COVID-19 recovery: An experience at the Physical and Rehabilitation Medicine Institute and Lucy Montoro Rehabilitation Institute. Clinics 2021, 76, e2804. [Google Scholar] [CrossRef]
- Grigoletto, I.; Cavalheri, V.; de Lima, F.F.; Ramos, E.M.C. Recovery after COVID-19: The potential role of pulmonary rehabilitation. Braz. J. Phys. Ther. 2020, 24, 463–464. [Google Scholar] [CrossRef]
- Smondack, P.; Gravier, F.; Prieur, G.; Repel, A.; Muir, J.-F.; Cuvelier, A.; Combret, Y.; Medrinal, C.; Bonnevie, T. Physiotherapy and COVID-19. From Intensive Care Unit to Home Care–An Overview of International Guidelines. Revue Des Maladies Respiratoires 2020, 37, 811–822. [Google Scholar] [CrossRef]
- Lew, H.L.; Oh-Park, M.; Cifu, D.X. The War on COVID-19 Pandemic: Role of Rehabilitation Professionals and Hospitals. Am. J. Phys. Med. Rehabil. 2020, 99, 571–572. [Google Scholar] [CrossRef] [PubMed]
- Bond, S.; Laddu, D.R.; Ozemek, C.; Lavie, C.J.; Arena, R. Exergaming and Virtual Reality for Health: Implications for Cardiac Rehabilitation. Curr. Probl. Cardiol. 2021, 46, 100472. [Google Scholar] [CrossRef]
- García-Bravo, S.; Cuesta-Gómez, A.; Campuzano-Ruiz, R.; López-Navas, M.J.; Domínguez-Paniagua, J.; Araújo-Narváez, A.; Barreñada-Copete, E.; García-Bravo, C.; Flórez-García, M.T.; Botas-Rodríguez, J.; et al. Virtual reality and video games in cardiac rehabilitation programs. A systematic review. Disabil. Rehabil. 2021, 43, 448–457. [Google Scholar] [CrossRef] [PubMed]
- Cuesta-Gómez, A.; Sánchez-Herrera-Baeza, P.; Oña-Simbaña, E.D.; Martínez-Medina, A.; Ortiz-Comino, C.; Balaguer-Bernaldo-De-Quirós, C.; Jardón-Huete, A.; Cano-De-La-Cuerda, R. Effects of virtual reality associated with serious games for upper limb rehabilitation in patients with multiple sclerosis: Randomized controlled trial. J. Neuroeng. Rehabil. 2020, 17, 90. [Google Scholar] [CrossRef] [PubMed]
- da Silva, T.D.; de Oliveira, P.M.; Dionizio, J.B.; de Santana, A.P.; Bahadori, S.; Dias, E.D.; Ribeiro, C.M.; de Andrade Gomes, R.; Ferreira, M.; Ferreira, C.; et al. Comparison Between Conventional Intervention and Non-immersive Virtual Reality in the Rehabilitation of Individuals in an Inpatient Unit for the Treatment of COVID-19: A Study Protocol for a Randomized Controlled Crossover Trial. Front. Psychol. 2021, 12, 622618. [Google Scholar] [CrossRef] [PubMed]
- Ostrowska, P.M.; Śliwiński, M.; Studnicki, R.; Hansdorfer-Korzon, R. Telerehabilitation of Post-Stroke Patients as a Therapeutic Solution in the Era of the COVID-19 Pandemic. Healthcare 2021, 9, 654. [Google Scholar] [CrossRef]
- Groenveld, T.; Achttien, R.; Smits, M.; de Vries, M.; van Heerde, R.; Staal, B.; van Goor, H. COVID Rehab Group Feasibility of Virtual Reality Exercises at Home for Post–COVID-19 Condition: Cohort Study. JMIR Rehabil. Assist. Technol. 2022, 9, e36836. [Google Scholar] [CrossRef]
- Marzaleh, M.A.; Peyravi, M.; Azhdari, N.; Bahaadinbeigy, K.; Sharifian, R.; Samad-Soltani, T.; Sarpourian, F. Virtual reality applications for rehabilitation of COVID-19 patients: A systematic review. Health Sci. Rep. 2022, 5, e853. [Google Scholar] [CrossRef]
- Vibhuti; Kumar, N.; Kataria, C. Efficacy assessment of virtual reality therapy for neuromotor rehabilitation in home environment: A systematic review. Disabil. Rehabil. Assist. Technol. 2021, 1–21. [Google Scholar] [CrossRef]
- Dębska, M.; Polechoński, J.; Mynarski, A.; Polechoński, P. Enjoyment and Intensity of Physical Activity in Immersive Virtual Reality Performed on Innovative Training Devices in Compliance with Recommendations for Health. Int. J. Environ. Res. Public Health 2019, 16, 3673. [Google Scholar] [CrossRef]
- Dimbwadyo-Terrer, I.; Trincado-Alonso, F.; de los Reyes-Guzmán, A.; Aznar, M.A.; Alcubilla, C.; Pérez-Nombela, S.; del Ama-Espinosa, A.; Polonio-López, B.; Gil-Agudo, Á. Upper limb rehabilitation after spinal cord injury: A treatment based on a data glove and an immersive virtual reality environment. Disabil. Rehabil. Assist. Technol. 2016, 11, 462–467. [Google Scholar] [CrossRef] [PubMed]
- de Mello Monteiro, C.B.; Massetti, T.; da Silva, T.D.; van der Kamp, J.; de Abreu, L.C.; Leone, C.; Savelsbergh, G.J. Transfer of motor learning from virtual to natural environments in individuals with cerebral palsy. Res. Dev. Disabil. 2014, 35, 2430–2437. [Google Scholar] [CrossRef] [PubMed]
- de Mello Monteiro, C.B.; da Silva, T.D.; de Abreu, L.C.; Fregni, F.; de Araujo, L.V.; Ferreira, F.H.I.B.; Leone, C. Short-term motor learning through non-immersive virtual reality task in individuals with down syndrome. BMC Neurol. 2017, 17, 71. [Google Scholar] [CrossRef]
- Dias, E.D.; de Menezes, L.D.C.; da Silva, T.D.; da Silva, N.M.; Vidal, P.R.; Brondane, B.R.; Padula, N.; Gaspar, R.C.; Santos, S.; Auricchio, J.R.; et al. Comparison of cardiac autonomic modulation of athletes and non-athletes individuals with spinal cord injury at rest and during a non-immersive virtual reality task. Spinal Cord 2021, 59, 1294–1300. [Google Scholar] [CrossRef] [PubMed]
- Sammito, S.; Böckelmann, I. Reference values for time- and frequency-domain heart rate variability measures. Heart Rhythm. 2016, 13, 1309–1316. [Google Scholar] [CrossRef] [PubMed]
- Marin, B.G.; Aghagoli, G.; Lavine, K.; Yang, L.; Siff, E.J.; Chiang, S.S.; Salazar-Mather, T.P.; Dumenco, L.; Savaria, M.C.; Aung, S.N.; et al. Predictors of COVID -19 severity: A literature review. Rev. Med. Virol. 2021, 31, 1–10. [Google Scholar] [CrossRef]
- Kang, S.-J.; Jung, S.I. Age-Related Morbidity and Mortality among Patients with COVID-19. Infect. Chemother. 2020, 52, 154–164. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef]
- Da Silva, T.D.; Fontes, A.M.G.G.; De Oliveira-Furlan, B.S.; Roque, T.T.; Lima, A.I.I.; De Souza, B.M.M.; Alberissi, C.A.D.O.; Silveira, A.C.; De Moraes, Í.A.P.; Collett, J.; et al. Effect of Combined Therapy of Virtual Reality and Transcranial Direct Current Stimulation in Children and Adolescents with Cerebral Palsy: A Study Protocol for a Triple-Blinded Randomized Controlled Crossover Trial. Front. Neurol. 2020, 11, 953. [Google Scholar] [CrossRef]
- Martins, F.P.A.; Massetti, T.; Crocetta, T.B.; Lopes, P.B.; da Silva, A.A.; Figueiredo, E.F.; de Abreu, L.C.; da Silva, T.D.; de Mello Monteiro, C.B. Analysis of motor performance in individuals with cerebral palsy using a non-immersive virtual reality task—A pilot study. Neuropsychiatr. Dis. Treat. 2019, 15, 417–428. [Google Scholar] [CrossRef]
- Moraes, Í.A.P.; Lima, J.A.; Silva, N.M.; Simcsik, A.O.; Silveira, A.C.; Menezes, L.D.C.; Araújo, L.V.; Crocetta, T.B.; Voos, M.C.; Tonks, J.; et al. Effect of Longitudinal Practice in Real and Virtual Environments on Motor Performance, Physical Activity and Enjoyment in People with Autism Spectrum Disorder: A Prospective Randomized Crossover Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 14668. [Google Scholar] [CrossRef] [PubMed]
- Schefold, J.C.; Wollersheim, T.; Grunow, J.J.; Luedi, M.M.; Z’Graggen, W.J.; Weber-Carstens, S. Muscular weakness and muscle wasting in the critically ill. J. Cachex-Sarcopenia Muscle 2020, 11, 1399–1412. [Google Scholar] [CrossRef] [PubMed]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ 2008, 337, a1655. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Novak, S.; Johnson, J.; Greenwood, R. Barthel revisited: Making guidelines work. Clin. Rehabil. 1996, 10, 128–134. [Google Scholar] [CrossRef]
- Houlden, H.; Edwards, M.; McNeil, J.; Greenwood, R. Use of the Barthel Index and the Functional Independence Measure during early inpatient rehabilitation after single incident brain injury. Clin. Rehabil. 2006, 20, 153–159. [Google Scholar] [CrossRef]
- Catai, A.M.; Pastre, C.M.; de Godoy, M.F.; da Silva, E.; Takahashi, A.C.D.M.; Vanderlei, L.C.M. Heart rate variability: Are you using it properly? Standardisation checklist of procedures. Braz. J. Phys. Ther. 2019, 24, 91–102. [Google Scholar] [CrossRef]
- Giles, D.; Draper, N.; Neil, W. Validity of the Polar V800 heart rate monitor to measure RR intervals at rest. Eur. J. Appl. Physiol. 2015, 116, 563–571. [Google Scholar] [CrossRef]
- Perrotta, A.S.; Jeklin, A.T.; Hives, B.A.; Meanwell, L.E.; Warburton, D.E. Validity of the Elite HRV Smartphone Application for Examining Heart Rate Variability in a Field-Based Setting. J. Strength Cond. Res. 2017, 31, 2296–2302. [Google Scholar] [CrossRef]
- Vanderlei, L.C.M.; Pastre, C.M.; Hoshi, R.A.; de Carvalho, T.D.; de Godoy, M.F. Basic Notions of Heart Rate Variability and Its Clinical Applicability. Braz. J. Cardiovasc. Surg. 2009, 24, 205–217. [Google Scholar] [CrossRef]
- Chen, Y.; Klein, S.L.; Garibaldi, B.T.; Li, H.; Wu, C.; Osevala, N.M.; Li, T.; Margolick, J.B.; Pawelec, G.; Leng, S.X. Aging in COVID-19: Vulnerability, immunity and intervention. Ageing Res. Rev. 2020, 65, 101205. [Google Scholar] [CrossRef] [PubMed]
- De Moura-Tonello, S.C.G.; Carvalho, V.; De Godoy, M.F.; Porta, A.; Leal, Â.M.d.O.; Bocchi, E.A.; Catai, A.M. Evaluation of Cardiac Autonomic Modulation Using Symbolic Dynamics after Cardiac Transplantation. Braz. J. Cardiovasc. Surg. 2019, 34, 572–580. [Google Scholar] [CrossRef] [PubMed]
- Dias, R.M.; Hoshi, R.A.; Vanderlei, L.C.M.; Monteiro, C.B.d.M.; Alvarez, M.P.B.; Crocetta, T.B.; Grossklauss, L.F.; Fernani, D.C.G.L.; Dantas, M.T.A.P.; Martins, F.P.A.; et al. Influence of Different Types of Corticosteroids on Heart Rate Variability of Individuals with Duchenne Muscular Dystrophy—A Pilot Cross Sectional Study. Life 2021, 11, 752. [Google Scholar] [CrossRef] [PubMed]
- Porta, A.; Tobaldini, E.; Guzzetti, S.; Furlan, R.; Montano, N.; Gnecchi-Ruscone, T. Assessment of cardiac autonomic modulation during graded head-up tilt by symbolic analysis of heart rate variability. Am. J. Physiol. Circ. Physiol. 2007, 293, H702–H708. [Google Scholar] [CrossRef] [PubMed]
- Molina, G.E.; Fontana, K.E.; Porto, L.G.G.; Junqueira, L.F. Post-exercise heart-rate recovery correlates to resting heart-rate variability in healthy men. Clin. Auton. Res. 2016, 26, 415–421. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Gottlieb, J.; Capetian, P.; Hamsen, U.; Janssens, U.; Karagiannidis, C.; Kluge, S.; Nothacker, M.; Roiter, S.; Volk, T.; Worth, H.; et al. German S3 Guideline: Oxygen Therapy in the Acute Care of Adult Patients. Respiration 2021, 101, 214–252. [Google Scholar] [CrossRef]
- De Carvalho, T.; Milani, M.; Ferraz, A.S.; Da Silveira, A.D.; Herdy, A.H.; Hossri, C.A.C.; e Silva, C.G.S.; de Araújo, C.G.S.; Rocco, E.A.; Teixeira, J.A.C.; et al. Diretriz Brasileira de Reabilitação Cardiovascular—2020. Arq. Bras. De Cardiol. 2020, 114, 943–987. [Google Scholar] [CrossRef]
- Haykowsky, M.J.; Timmons, M.P.; Kruger, C.; McNeely, M.; Taylor, D.A.; Clark, A.M. Meta-Analysis of Aerobic Interval Training on Exercise Capacity and Systolic Function in Patients with Heart Failure and Reduced Ejection Fractions. Am. J. Cardiol. 2013, 111, 1466–1469. [Google Scholar] [CrossRef] [PubMed]
- Mediano, M.F.F.; Mendes, F.d.S.N.S.; Pinto, V.L.M.; da Silva, G.M.S.; da Silva, P.S.; Carneiro, F.M.; Sangenis, L.H.C.; Saraiva, R.M.; Xavier, S.S.; do Brasil, P.E.A.A.; et al. Cardiac rehabilitation program in patients with Chagas heart failure: A single-arm pilot study. Rev. Da Soc. Bras. De Med. Trop. 2016, 49, 319–328. [Google Scholar] [CrossRef]
- Monteiro, C.B.D.M.; Dawes, H.; Deutsch, J.E. Editorial: Virtual Reality for Sensorimotor Rehabilitation of Neurological Health Conditions Across the Lifespan. Front. Neurol. 2021, 12, 1985. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, M.P.B.; da Silva, T.D.; Favero, F.M.; Valenti, V.E.; Raimundo, R.D.; Vanderlei, L.C.M.; Garner, D.M.; de Mello Monteiro, C.B. Autonomic Modulation in Duchenne Muscular Dystrophy during a Computer Task: A Prospective Control Trial. PLoS ONE 2017, 12, e0169633. [Google Scholar] [CrossRef] [PubMed]
- Qian, J.; McDonough, D.J.; Gao, Z. The Effectiveness of Virtual Reality Exercise on Individual’s Physiological, Psychological and Rehabilitative Outcomes: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 4133. [Google Scholar] [CrossRef]
- Eichhorn, S.; Koller, V.; Schreiber, U.; Mendoza, A.; Krane, M.; Lange, R. Development of an Exergame for individual rehabilitation of patients with cardiovascular diseases. Australas. Phys. Eng. Sci. Med. 2013, 36, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Vieira, Á.; Melo, C.; Machado, J.; Gabriel, J. Virtual reality exercise on a home-based phase III cardiac rehabilitation program, effect on executive function, quality of life and depression, anxiety and stress: A randomized controlled trial. Disabil. Rehabil. Assist. Technol. 2017, 13, 112–123. [Google Scholar] [CrossRef] [PubMed]
- García-Bravo, S.; Cano-de-la-Cuerda, R.; Domínguez-Paniagua, J.; Campuzano-Ruiz, R.; Barreñada-Copete, E.; López-Navas, M.J.; Araujo-Narváez, A.; García-Bravo, C.; Florez-Garcia, M.; Botas-Rodríguez, J.; et al. Effects of Virtual Reality on Cardiac Rehabilitation Programs for Ischemic Heart Disease: A Randomized Pilot Clinical Trial. Int. J. Environ. Res. Public Health 2020, 17, 8472. [Google Scholar] [CrossRef] [PubMed]
- Szczepańska-Gieracha, J.; Jóźwik, S.; Cieślik, B.; Mazurek, J.; Gajda, R. Immersive Virtual Reality Therapy as a Support for Cardiac Rehabilitation: A Pilot Randomized-Controlled Trial. Cyberpsychol. Behav. Soc. Netw. 2021, 24, 543–549. [Google Scholar] [CrossRef]
- Bashir, Z.; Misquith, C.; Shahab, A.; Has, P.; Bukhari, S. The impact of Virtual Reality on Anxiety and Functional Capacity in Cardiac Rehabilitation: A Systematic Review and Meta-analysis. Curr. Probl. Cardiol. 2023, 48, 101628. [Google Scholar] [CrossRef]
- van der Kruk, S.R.; Zielinski, R.; MacDougall, H.; Hughes-Barton, D.; Gunn, K.M. Virtual reality as a patient education tool in healthcare: A scoping review. Patient Educ. Couns. 2022, 105, 1928–1942. [Google Scholar] [CrossRef]
- Shah, B.; Kunal, S.; Bansal, A.; Jain, J.; Poundrik, S.; Shetty, M.K.; Batra, V.; Chaturvedi, V.; Yusuf, J.; Mukhopadhyay, S.; et al. Heart rate variability as a marker of cardiovascular dysautonomia in post-COVID-19 syndrome using artificial intelligence. Indian Pacing Electrophysiol. J. 2022, 22, 70–76. [Google Scholar] [CrossRef]
- Perseguini, N.M.; Takahashi, A.C.M.; Rebelatto, J.R.; Silva, E.; Borghi-Silva, A.; Porta, A.; Montano, N.; Catai, A.M. Spectral and symbolic analysis of the effect of gender and postural change on cardiac autonomic modulation in healthy elderly subjects. Braz. J. Med. Biol. Res. 2011, 44, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Jokinen, V.; Tapanainen, J.M.; Seppänen, T.; Huikuri, H.V. Temporal changes and prognostic significance of measures of heart rate dynamics after acute myocardial infarction in the beta-blocking era. Am. J. Cardiol. 2003, 92, 907–912. [Google Scholar] [CrossRef] [PubMed]
- Huikuri, H.V.; Mäkikallio, T.H.; Perkiömäki, J. Measurement of heart rate variability by methods based on nonlinear dynamics. J. Electrocardiol. 2003, 36, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Godoy, M.F.; Takakura, I.T.; Correa, P.R. The Relevance of Nonlinear Dynamic Analysis (Chaos Theory) to Predict Morbidity and Mortality in Patients Undergoing Surgical Myocardial Revascularization. Arqu Ciênc Saúde 2005, 12, 161–171. [Google Scholar]
- Scheff, J.D.; Griffel, B.; Corbett, S.A.; Calvano, S.E.; Androulakis, I.P. On heart rate variability and autonomic activity in homeostasis and in systemic inflammation. Math. Biosci. 2014, 252, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Soliński, M.; Pawlak, A.; Petelczyc, M.; Buchner, T.; Aftyka, J.; Gil, R.; Król, Z.J.; Żebrowski, J.J. Heart rate variability comparison between young males after 4–6 weeks from the end of SARS-CoV-2 infection and controls. Sci. Rep. 2022, 12, 8832. [Google Scholar] [CrossRef]
- Erdal, Y.; Atalar, A.C.; Gunes, T.; Okluoglu, T.; Yavuz, N.; Emre, U. Autonomic dysfunction in patients with COVID-19. Acta Neurol. Belg. 2022, 122, 885–891. [Google Scholar] [CrossRef]
- Medrinal, C.; Prieur, G.; Bonnevie, T.; Gravier, F.-E.; Mayard, D.; Desmalles, E.; Smondack, P.; Lamia, B.; Combret, Y.; Fossat, G. Muscle weakness, functional capacities and recovery for COVID-19 ICU survivors. BMC Anesthesiol. 2021, 21, 64. [Google Scholar] [CrossRef]
- Pícoli, T.D.S.; De Figueiredo, L.L.; Patrizzi, L.J. Sarcopenia e envelhecimento. Fisioter. Em Mov. 2011, 24, 455–462. [Google Scholar] [CrossRef]
- Piotrowicz, K.; Gąsowski, J.; Michel, J.-P.; Veronese, N. Post-COVID-19 acute sarcopenia: Physiopathology and management. Aging Clin. Exp. Res. 2021, 33, 2887–2898. [Google Scholar] [CrossRef]
- Bezerra, K.M.G.; Berto, C.M.; Da Silva, F.A.A.; Silva, L.M.d.S.; Marques, A.P.D.O. Impacto da obesidade na mortalidade de idosos com COVID-19. Rev. Bras. De Ciências Do Envelhec. Hum. 2020, 17. [Google Scholar] [CrossRef]
- Freire, A.P.C.F.; Lira, F.S.; Morano, A.E.V.A.; Pereira, T.; Coelho-E-Silva, M.-J.; Caseiro, A.; Christofaro, D.G.D.; Júnior, O.M.; Dorneles, G.P.; Minuzzi, L.G.; et al. Role of Body Mass and Physical Activity in Autonomic Function Modulation on Post-COVID-19 Condition: An Observational Subanalysis of Fit-COVID Study. Int. J. Environ. Res. Public Health 2022, 19, 2457. [Google Scholar] [CrossRef] [PubMed]




| Variables | 25–40 yo | 41–60 yo | 61–80 yo | |||
|---|---|---|---|---|---|---|
| Control | Post-COVID | Control | Post-COVID | Control | Post-COVID | |
| n = 14 | n = 12 | n = 18 | n = 18 | n = 13 | n = 19 | |
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |
| Age | 34.2 ± 5.2 | 33.9 ± 4.6 | 52.3 ± 5.6 | 51.5 ± 6.0 | 69.3 ± 6.7 | 68.8 ± 5.6 |
| BMI | 25.4 ± 4.7 | 28.7 ± 3.2 | 25.6 ± 3.5 | 30.2 ± 4.73 * | 27.4 ± 4.9 | 33.5 ± 5.7 * |
| MRC | 60.0 ± 0.0 | 60.0 ± 0.0 | 59.9 ± 0.5 | 56.4 ± 14.1 | 59.8 ± 0.5 | 48.2 ± 22.1 * |
| Barthel index | 100.0 ± 0.0 | 100.0 ± 0.0 | 100.0 ± 0.0 | 99.2 ± 3.5 | 100.0 ± 0.0 | 95.5 ± 14.0 |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Sex | ||||||
| Male | 6 (42.9) | 5 (41.7) | 6 (33.3) | 8 (44.4) | 8 (61.5) | 10 (52.6) |
| Female | 8 (57.1) | 7 (58.3) | 12 (66.7) | 10 (55.6) | 5 (38.5) | 9 (47.8) |
| Comorbidities | ||||||
| Systemic arterial hypertension | 0 (0.0) | 2 (16.7) | 0 (0.0) | 2 (11.1) | 8 (61.5) | 15 (78.9) |
| Diabetes mellitus | 0 (0.0) | 0 (0.0) | 4 (22.2) | 1 (5.6) | 1 (7.7) | 8 (42.1) * |
| Congestive heart failure | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (11.1) | 2 (15.4) | 1 (5.3) |
| Habits | ||||||
| Smoker | 0 (0.0) | 0 (0.0) | 1 (5.6) | 2 (11.1) | 1 (7.7) | 0 (0.0) |
| PA pre-pandemic | 3 (21.4) | 4 (33.3) | 3 (16.7) | 4 (22.2) | 4 (30.8) | 5 (26.3) |
| PA during pandemic | 3 (21.4) | 1 (8.3) | 1 (5.6) | 3 (16.7) | 1 (7.7) | 0 (0.0) |
| Medications | ||||||
| Antihypertensive | 0 (0.0) | 1 (8.3) | 5 (27.8) | 3 (16.7) | 9 (69.2) | 10 (52.6) |
| Hospitalization for COVID | Mean ± SD or n (%) | Mean ± SD or n (%) | Mean ± SD or n (%) | |||
| Time (days) | - | 10.7 ± 10.2 | - | 10.4 ± 12.3 | - | 20.2 ± 19.4 |
| Received sedative | - | 4 (33.3) | - | 3 (16.7) | - | 8 (42.1) |
| Received chloroquine | - | 7 (58.3) | - | 7 (38.9) | - | 6 (31.6) |
| Oxygen catheter | - | 10 (83.3) | - | 14 (77.8) | - | 15 (78.9) |
| Non-rebreathing oxygen mask | - | 0 (0.0) | - | 4 (22.2) | - | 2 (10.5) |
| High-flow nasal cannula oxygen | - | 0 (0.0) | - | 1 (5.6) | - | 4 (21.1) |
| Non-invasive ventilation | - | 1 (8.3) | - | 2 (11.1) | - | 11 (57.9) § |
| Invasive mechanical ventilation | - | 1 (8.3) | - | 1 (5.6) | - | 6 (31.6) |
| Oxygen after hospitalization | - | 0 (0.0) | - | 0 (0.0) | - | 6 (31.6) § |
| Post-hospitalization rehabilitation | - | 6 (50.0) § | - | 10 (55.6) | - | 17 (89.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ribeiro, C.M.; Gomes, R.d.A.; Monteiro, C.B.d.M.; Dias, R.M.; Simcsik, A.O.; Araújo, L.V.d.; Maia, L.C.P.; Oliveira, A.P.d.; Freitas, B.L.d.; Dawes, H.; et al. Heart Rate Variability during Virtual Reality Activity in Individuals after Hospitalization for COVID-19: A Cross-Sectional Control Study. Electronics 2023, 12, 1925. https://doi.org/10.3390/electronics12081925
Ribeiro CM, Gomes RdA, Monteiro CBdM, Dias RM, Simcsik AO, Araújo LVd, Maia LCP, Oliveira APd, Freitas BLd, Dawes H, et al. Heart Rate Variability during Virtual Reality Activity in Individuals after Hospitalization for COVID-19: A Cross-Sectional Control Study. Electronics. 2023; 12(8):1925. https://doi.org/10.3390/electronics12081925
Chicago/Turabian StyleRibeiro, Cinthia Mucci, Renata de Andrade Gomes, Carlos Bandeira de Mello Monteiro, Rodrigo Martins Dias, Amanda Orasmo Simcsik, Luciano Vieira de Araújo, Laura Cristina Pereira Maia, Adriana Paulino de Oliveira, Bruna Leal de Freitas, Helen Dawes, and et al. 2023. "Heart Rate Variability during Virtual Reality Activity in Individuals after Hospitalization for COVID-19: A Cross-Sectional Control Study" Electronics 12, no. 8: 1925. https://doi.org/10.3390/electronics12081925







