Geriatric Healthcare Supported by Decision-Making Tools Integrated into Digital Health Solutions
Abstract
1. Introduction
1.1. Comprehensive Geriatric Assessment Boosted by Personalized Digital Health Solutions
1.2. RO-SmartAgeing System and NeuroPredict Platform—Innovative Digital Health Solutions for Enhancing Geriatric Care
2. Literature Review
2.1. Leveraging Digital Health Solutions for the Care of the Elderly
2.2. Opportunities Brought by Decision-Making Tools for Geriatric Care
2.3. Challenges in Decision-Making Tools for Geriatric Care
3. Materials and Methods
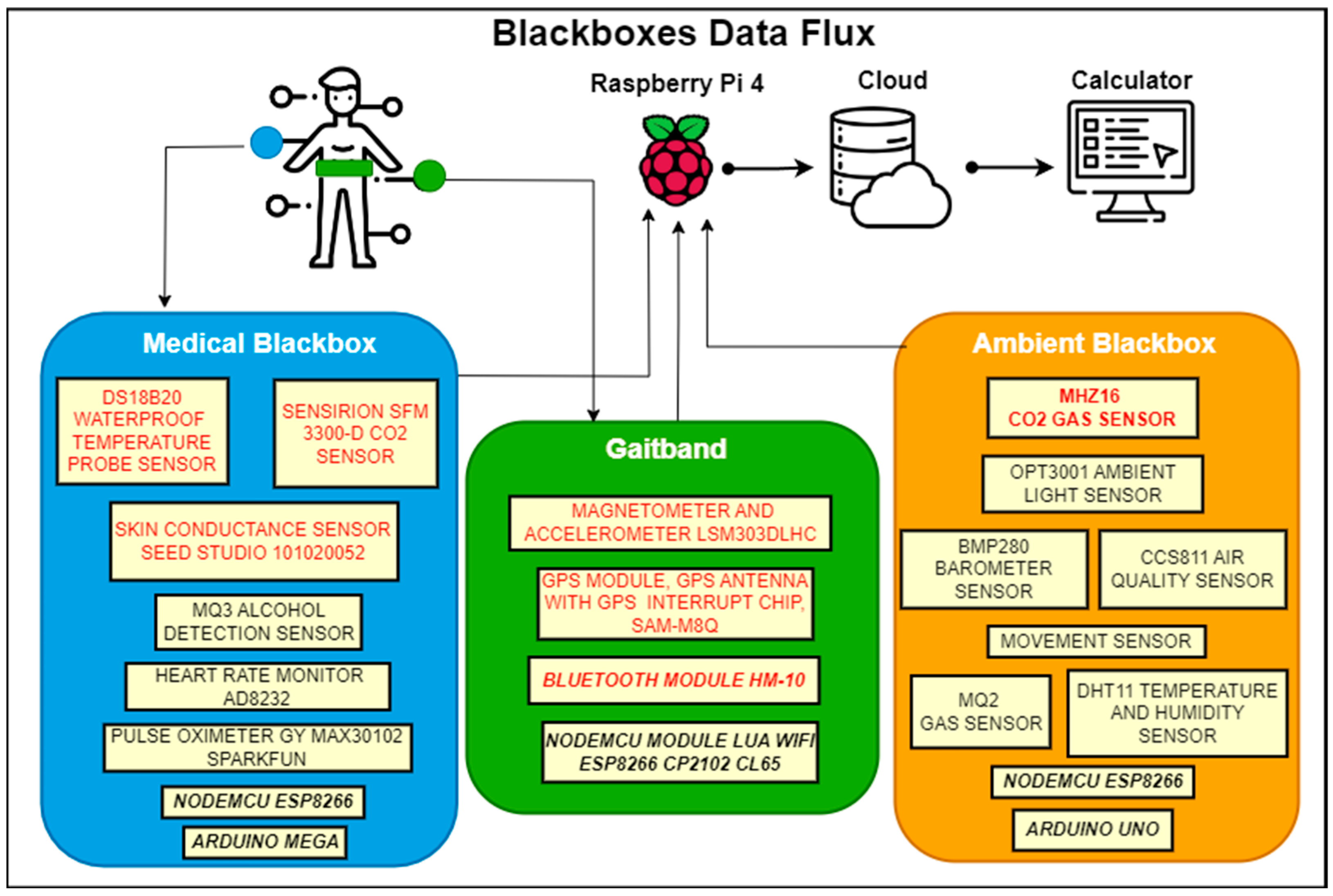
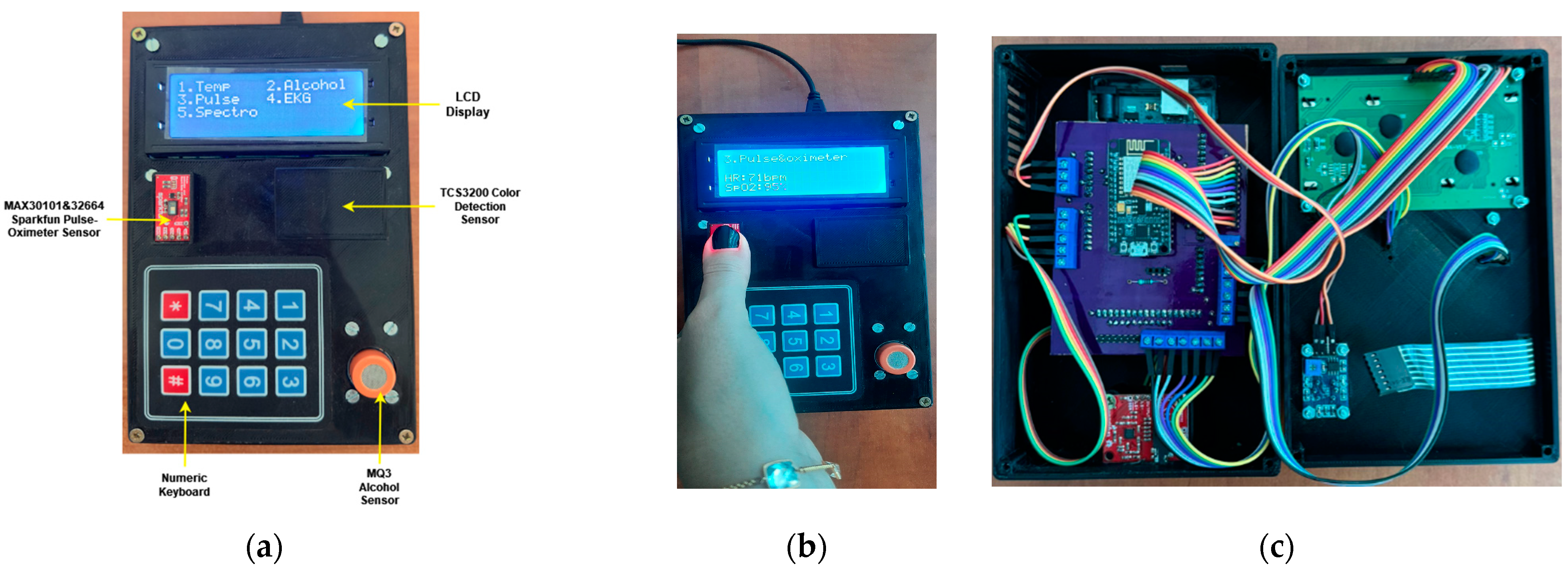
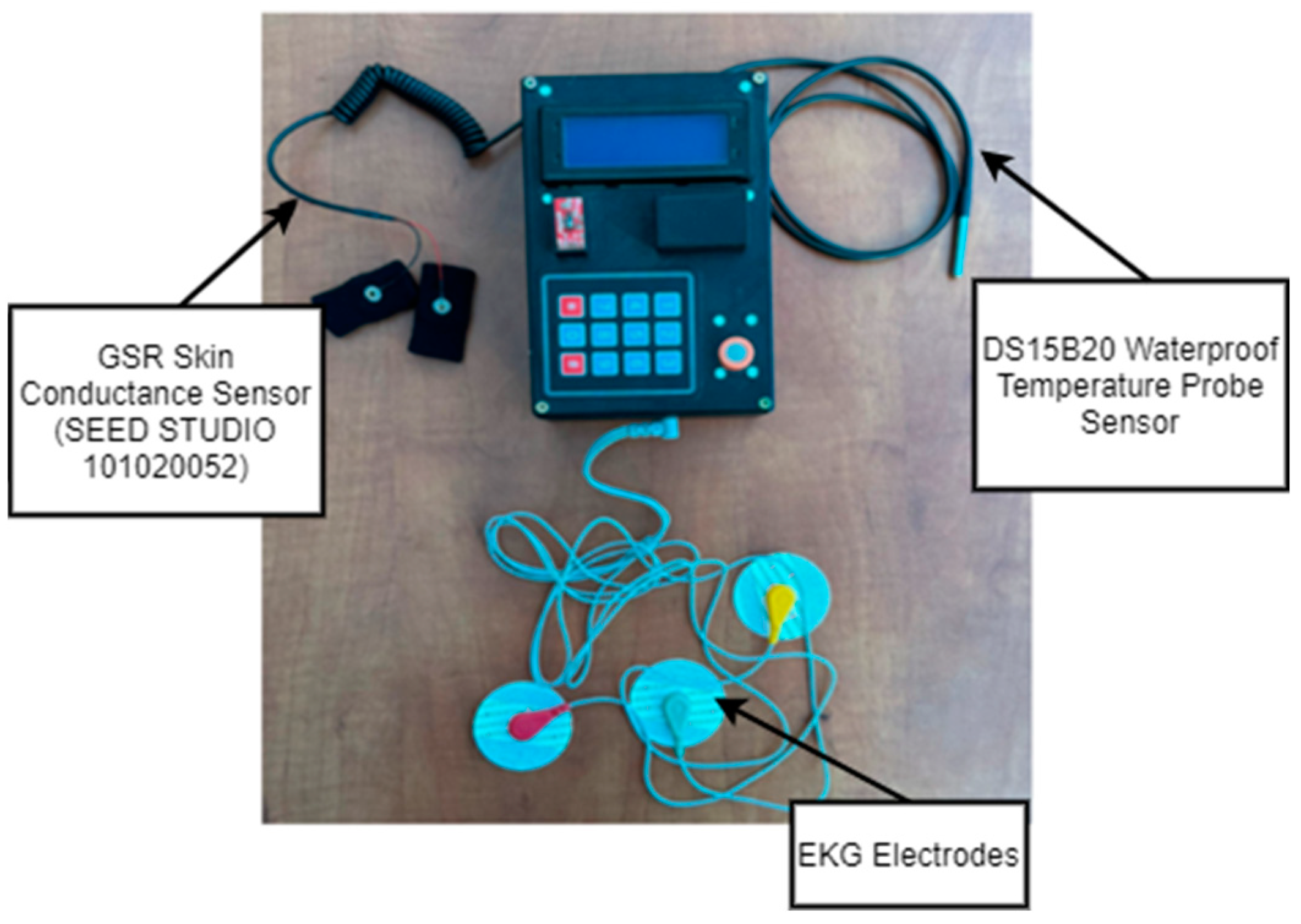
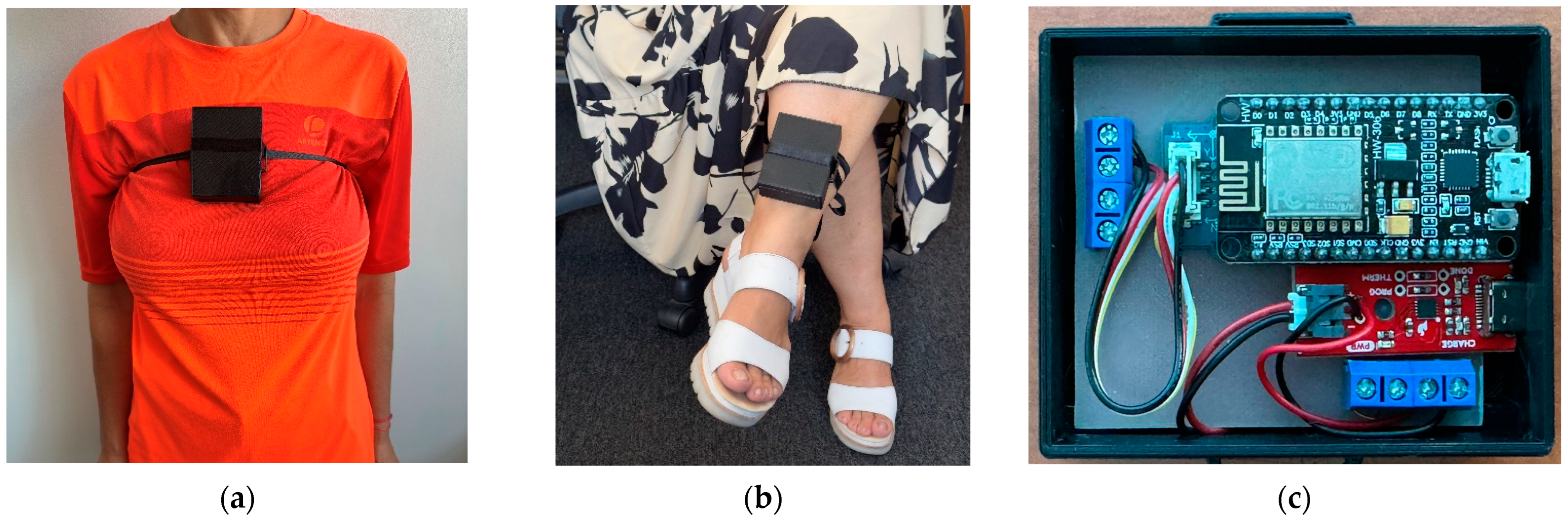
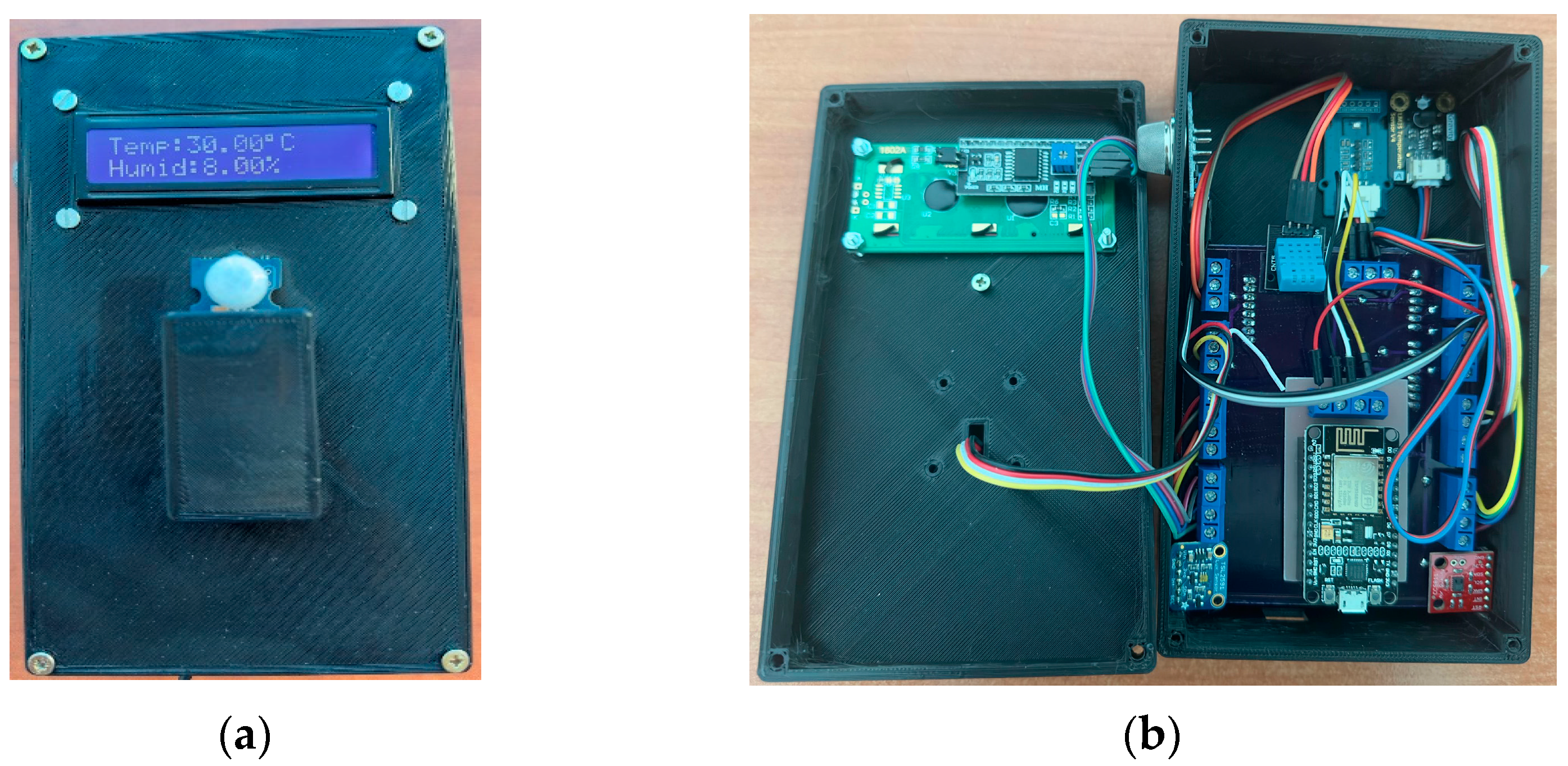
3.1. Design and Development of Genuine Decision-Making Tools within the RO-SmartAgeing System
3.2. Expanding the Functionalities Provided by the Decision-Making Tools within the NeuroPredict Platform
3.3. Data-Driven Decision Support
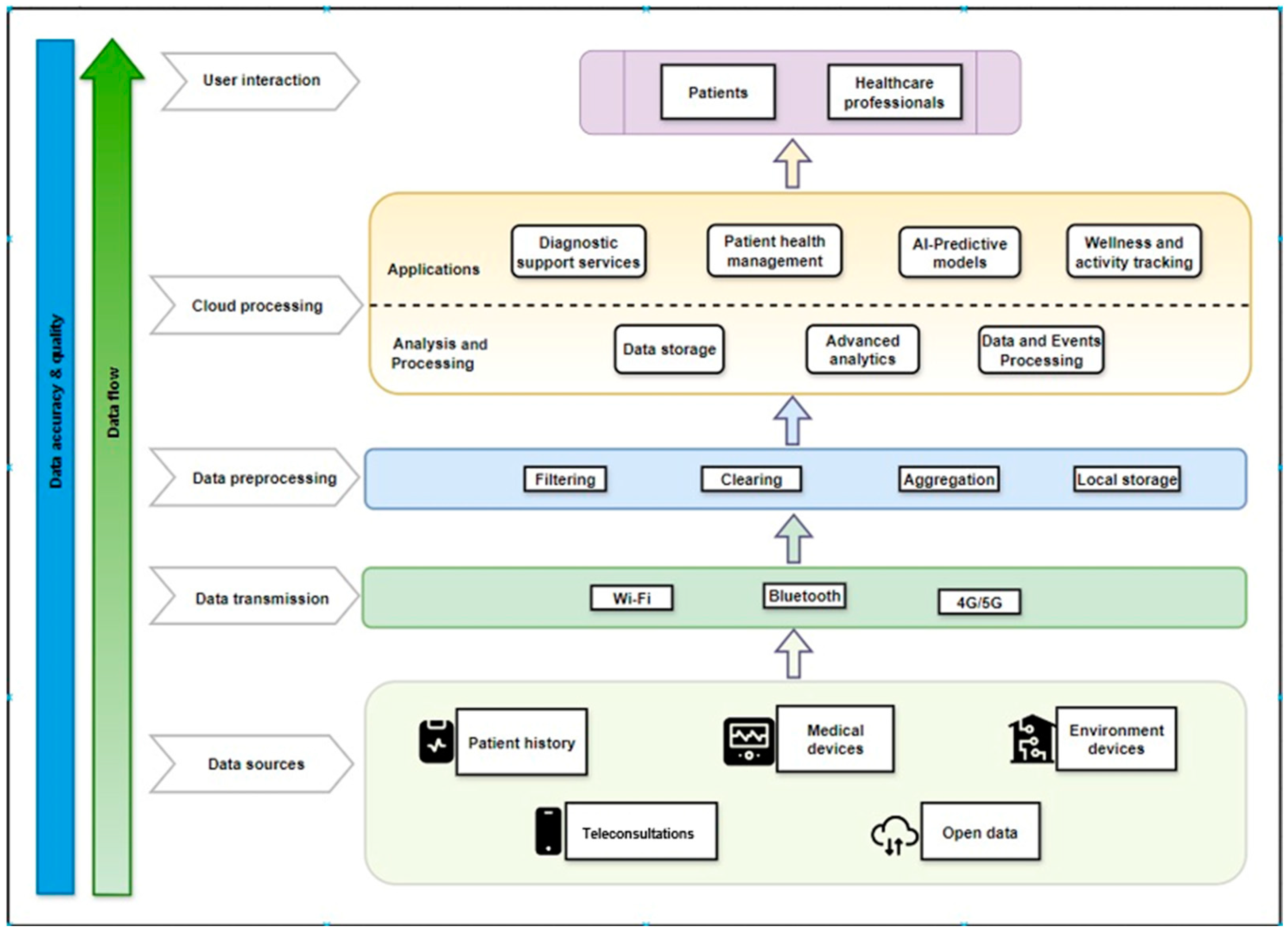
- Complex health parameters: To achieve comprehensive monitoring, multiple health parameters must be tracked concurrently, such as blood glucose levels, vital signs, dietary patterns, physical activity, and other pertinent biomarkers. A more comprehensive and nuanced picture of a person’s health is provided by the integration of data from many sources [85]. This integrated approach not only facilitates personalized healthcare but also supports the proactive management of chronic conditions prevalent in elderly populations, thereby improving overall health outcomes and quality of life. In geriatric healthcare, where holistic assessment and personalized interventions are paramount, leveraging comprehensive health data enables data-driven decision-support systems to analyze complex health patterns over time. This capability empowers healthcare providers to tailor care plans specifically to the evolving needs of elderly patients, ensuring timely interventions and optimizing treatment efficacy.
- Real-time data synthesis: When connected to a DHS like the RO-SmartAgeing system or the NeuroPredict platform, decision-making tools facilitate the synthesis of health data in real-time, giving healthcare professionals fast access to the most recent information. By leveraging real-time data synthesis, healthcare providers can implement timely adjustments to treatment plans, ensuring optimal care strategies tailored to the evolving health needs of elderly patients, thus enhancing their health management experience, and reducing healthcare costs associated with preventable complications. This capability exemplifies the transformative impact of DHS in geriatric care, where proactive monitoring and real-time insights enable data-driven decision support to enhance clinical outcomes and patient satisfaction.
- Interconnected medical devices: Integration is the process of efficiently integrating different medical devices into DHS to build a networked environment. The total effectiveness of disease care is improved by this interconnection [86], which offers a more thorough picture of the patient’s health evolution. This interconnectedness is crucial in facilitating data-driven decision-making processes that empower healthcare professionals to intervene proactively, anticipate health deterioration, and optimize treatment strategies specifically tailored to the complex healthcare needs of elderly patients, thereby promoting personalized care and improving health outcomes.
- Predictive analytics: Predictive modeling is made possible by DHS’ advanced analytics, in conjunction with extensive monitoring. Predictive analytics can foresee potential challenges or deviances from the intended health evolution by examining patterns and trends in health data across time [87]. In geriatric healthcare, predictive analytics play a crucial role in enhancing data-driven decision-support systems, enabling proactive management of chronic conditions and personalized care planning based on predictive insights derived from comprehensive health data.
- Patient engagement and empowerment: By giving patients direct access to their health data, smart monitoring environments integrated with DHS encourage patient involvement ([25]. Enhanced patient engagement fosters a collaborative healthcare environment in which elderly patients become active partners in their care journey, leading to improved adherence to treatment regimens, better health outcomes, and increased satisfaction with healthcare services, ultimately promoting a patient-centered approach to geriatric care.
- Customized treatment plans: Treatment plans that are both individualized and data-driven may be created due to the integration of comprehensive health data within DHS. Tailored medical care approaches enhance patient compliance and lead to better results. DHS that support customized treatment plans based on comprehensive health data enable data-driven decision-support systems to optimize care delivery and enhance treatment efficacy for elderly patients, highlighting the critical role of these treatment plans in modern geriatric healthcare practices.
- Secure data management: Robust data security measures are necessary inside DHS, given their monitoring capacity, in order to protect sensitive health information [88]. To guarantee patient privacy and comply with healthcare standards, secure data transmission and storage, as well as access constraints, should be given top priority in smart environments. DHS that prioritize secure data management enhance patient trust and healthcare-provider confidence in the usage of DHS for comprehensive health monitoring and data-driven decision support, thereby promoting sustainable and patient-centric geriatric healthcare practices.
4. Results
5. Discussion
- The Medical Blackbox might encounter limitations in sensor performance and reliability that can be impacted by external factors such as electromagnetic interference and calibration inaccuracies, leading to inappropriate decision-making support. While its design is user-friendly, the interface’s four-row LCD display may pose challenges for senior users, especially those with visual impairments. Real-time data transmission may be disrupted in places with limited internet connectivity, influencing the timely availability of key health data.
- The Gaitband’s performance varies based on its placement on the body. While chest placement enhances accuracy, it may cause discomfort, whereas ankle placement might result in false positives, particularly in sitting-down circumstances. The device’s three-axis accelerometer and gyroscope may occasionally fail to correctly make distinctions between real falls and other movement disturbances, leading to possible errors and needless alerts. The fall-detection algorithm’s periodic posture assessments may even generate false alarms if non-fall situations are incorrectly classified as falls, making for unnecessary anxieties.
- The Ambient Blackbox’s environmental sensors may face calibration errors or deviations from the norm, compromising data accuracy. Data transmission may be hampered by breaks in wireless connectivity or communication difficulties with the NodeMCU, affecting the promptness of monitoring and response. Although the device requires minimal user engagement once installed, initial setup and configuration may be difficult for certain senior users or their caretakers, which would require simple instructions and easy setup procedures.
6. Conclusions
- Integrating these devices with forthcoming technology can considerably improve their performance. For example, integrating advanced machine-learning algorithms and AI might increase the accuracy of data analysis and prediction capabilities, allowing for more accurate and useful insights into patient health.
- Increasing the number of physiological and environmental parameters monitored by devices can provide a more complete assessment of a patient’s health. Integrating sensors that collect additional health metrics or ambient factors might improve the identification of possible concerns and enable tailored solutions.
- Improving user experience and device security is critical. For instance, with regard to the Gaitband, this would entail refining its design for greater comfort during extended usage and lowering the number of errors that occur.
- Validation and testing in real-world situations are vital for addressing the changing demands of older patients and healthcare professionals.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- United Nations Department of Economic and Social Affairs Population Division. World Population to Reach 8 Billion on 15 November 2022; United Nations Department of Economic and Social Affairs: New York, NY, USA, 2023. [Google Scholar]
- Schippinger, W. Comprehensive Geriatric Assessment. Wiener Med. Wochenschr. 2022, 172, 122–125. [Google Scholar] [CrossRef] [PubMed]
- Jiao, W.; Chang, A.; Ho, M.; Lu, Q.; Liu, M.T.; Schulz, P.J. Predicting and Empowering Health for Generation Z by Comparing Health Information Seeking and Digital Health Literacy: Cross-Sectional Questionnaire Study. J. Med. Internet Res. 2023, 25, e47595. [Google Scholar] [CrossRef] [PubMed]
- Sak, G.; Rothenfluh, F.; Schulz, P.J. Assessing the Predictive Power of Psychological Empowerment and Health Literacy for Older Patients’ Participation in Health Care: A Cross-Sectional Population-Based Study. BMC Geriatr. 2017, 17, 59. [Google Scholar] [CrossRef]
- Glover, C.M.; Stewart, C.C.; Yu, L.; Wilson, R.S.; Lamar, M.; Bennett, D.A.; Boyle, P.A. Psychological Well-Being Relates to Healthcare and Financial Decision Making in a Study of Predominantly White Older Adults. J. Appl. Gerontol. 2023, 42, 1770–1780. [Google Scholar] [CrossRef]
- Parker, S.G.; Mccue, P.; Phelps, K.; Mccleod, A.; Arora, S.; Nockels, K.; Kennedy, S.; Roberts, H.; Conroy, S. What Is Comprehensive Geriatric Assessment (CGA)? An Umbrella Review. Age Ageing 2018, 47, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Elsawy, B.; Higgins, K.E. The Geriatric Assessment. Am. Fam. Physician 2011, 83, 48–56. [Google Scholar]
- Wu, X.; Freeman, S.; Miyagi, M.; Park, U.; Nomura, K.; Ebihara, S. Comprehensive Geriatric Assessment in the Era of Telemedicine. Geriatr. Gerontol. Int. 2024, 24, 67–73. [Google Scholar] [CrossRef]
- Bajenaru, O.-L.; Nuță, C.-R.; Gabriela-Cristina, C.; Sanziana-Georgeta, M.; Herghelegiu, A.M.; Ovidiu, P.N.; Prada, G.-I. Risk Factors for Cerebrovacular Disease in the Elderly. Abstracts of the 19th Congress of the European Geriatric Medicine Society. Eur. Geriatr. Med. 2023, 14 (Suppl. S1), S1–S387. [Google Scholar] [CrossRef]
- Băjenaru, O.-L.; Cătălina, N.; Prada, G.-I.; Herghelegiu, A.M. Movement Disorders in Older People. Rom. J. Gerontol. Geriatr. 2022, 11, 36. [Google Scholar]
- Scuteri, A. Comprehensive Geriatric Assessment (CGA) in Patients with DM. J. Gerontol. Geriatr. 2021, 69, 258–261. [Google Scholar] [CrossRef]
- Briede-Westermeyer, J.C.; Radici Fraga, P.G.; Schilling-Norman, M.J.; Pérez-Villalobos, C. Identifying the Needs of Older Adults Associated with Daily Activities: A Qualitative Study. Int. J. Environ. Res. Public Health 2023, 20, 4257. [Google Scholar] [CrossRef] [PubMed]
- Băjenaru, L.; Marinescu, I.A.; Dobre, C.; Drăghici, R.; Herghelegiu, A.M.; Rusu, A. Identifying the Needs of Older People for Personalized Assistive Solutions in Romanian Healthcare System. Stud. Inform. Control 2020, 29, 363–372. [Google Scholar] [CrossRef]
- Fallahzadeh, R.; Rokni, S.A.; Ghasemzadeh, H.; Soto-Perez-de-Celis, E.; Shahrokni, A. Digital Health for Geriatric Oncology. JCO Clin. Cancer Inform. 2018, 2, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Monge, J.; Ribeiro, G.; Raimundo, A.; Postolache, O.; Santos, J. AI-Based Smart Sensing and AR for Gait Rehabilitation Assessment. Information 2023, 14, 355. [Google Scholar] [CrossRef]
- Mei, Y.; Xu, X.; Li, X. Encouraging Patient Engagement Behaviors from the Perspective of Functional Quality. Int. J. Environ. Res. Public Health 2020, 17, 8613. [Google Scholar] [CrossRef]
- Jimenez, J.; del Rio, A.; Berman, A.N.; Grande, M. Personalizing Digital Health: Adapting Health Technology Systems to Meet the Needs of Different Older Populations. Healthcare 2023, 11, 2140. [Google Scholar] [CrossRef]
- Miranda, R.; Oliveira, M.D.; Nicola, P.; Baptista, F.M.; Albuquerque, I. Towards A Framework for Implementing Remote Patient Monitoring From an Integrated Care Perspective: A Scoping Review. Int. J. Health Policy Manag. 2023, 12, 1–13. [Google Scholar] [CrossRef]
- Abdulmalek, S.; Nasir, A.; Jabbar, W.A.; Almuhaya, M.A.M.; Bairagi, A.K.; Khan, M.A.-M.; Kee, S.-H. IoT-Based Healthcare-Monitoring System towards Improving Quality of Life: A Review. Healthcare 2022, 10, 1993. [Google Scholar] [CrossRef]
- Morag, I.; Kedmi-Shahar, E.; Arad, D. Remote Communications between Patients and General Practitioners: Do Patients Choose the Most Effective Communication Routes? Int. J. Environ. Res. Public Health 2023, 20, 7188. [Google Scholar] [CrossRef]
- Melnykova, N.; Shakhovska, N.; Gregus, M.; Melnykov, V.; Zakharchuk, M.; Vovk, O. Data-Driven Analytics for Personalized Medical Decision Making. Mathematics 2020, 8, 1211. [Google Scholar] [CrossRef]
- Portz, J.D.; Ford, K.L.; Doyon, K.; Bekelman, D.B.; Boxer, R.S.; Kutner, J.S.; Czaja, S.; Bull, S. Using Grounded Theory to Inform the Human-Centered Design of Digital Health in Geriatric Palliative Care. J. Pain Symptom. Manag. 2020, 60, 1181–1192.e1. [Google Scholar] [CrossRef]
- Depp, C.; Vahia, I.; Fortuna, K.L.; Ajilore, O.A. DIGITAL TOOLS IN GEROPSYCHIATRY: FROM RESEARCH TO PATIENT CARE. Am. J. Geriatr. Psychiatry 2019, 27, S30. [Google Scholar] [CrossRef]
- Molinari-Ulate, M.; Mahmoudi, A.; Parra-Vidales, E.; Muñoz-Sánchez, J.L.; Franco-Martín, M.A.; van der Roest, H.G. Digital Health Technologies Supporting the Application of Comprehensive Geriatric Assessments in Long-Term Care Settings or Community Care: A Systematic Review. Digit Health 2023, 9, 20552076231191008. [Google Scholar] [CrossRef] [PubMed]
- Syed-Abdul, S.; Li, Y.-C. Empowering Patients and Transforming Healthcare in the Post-COVID-19 Era: The Role of Digital and Wearable Technologies. J. Pers. Med. 2023, 13, 722. [Google Scholar] [CrossRef] [PubMed]
- LaMonica, H.M.; Davenport, T.A.; Roberts, A.E.; Hickie, I.B. Understanding Technology Preferences and Requirements for Health Information Technologies Designed to Improve and Maintain the Mental Health and Well-Being of Older Adults: Participatory Design Study. JMIR Aging 2021, 4, e21461. [Google Scholar] [CrossRef] [PubMed]
- Bhyat, R.; Hagens, S.; Bryski, K.; Kohlmaier, J.F. Digital Health Value Realization Through Active Change Efforts. Front. Public Health 2021, 9, 741424. [Google Scholar] [CrossRef]
- Ianculescu, M.; Alexandru, A.; Pop, F. Critical Analysis and Evaluation of Current Digital Healthcare Solutions. In Proceedings of the 23nd International Conference on Control Systems and Computer Science (23rd CSCS 2021), Bucharest, Romania, 26–28 May 2021; pp. 482–488. [Google Scholar]
- Coman, L.-I.; Ianculescu, M.; Paraschiv, E.-A.; Alexandru, A.; Bădărău, I.-A. Smart Solutions for Diet-Related Disease Management: Connected Care, Remote Health Monitoring Systems, and Integrated Insights for Advanced Evaluation. Appl. Sci. 2024, 14, 2351. [Google Scholar] [CrossRef]
- Ianculescu, M.; Paraschiv, E.-A.; Alexandru, A. Addressing Mild Cognitive Impairment and Boosting Wellness for the Elderly through Personalized Remote Monitoring. Healthcare 2022, 10, 1214. [Google Scholar] [CrossRef]
- Paraschiv, E.-A.; Ianculescu, M.; Alexandru, A.; Bica, O. Internet of Things (IoT)—Based Healthcare Monitoring Systems for Assisting Neurodegenerative Patients in Healthcare Environment. In Proceedings of the 39th International Business Information Management Conference (39th IBIMA): Innovation Management and Education Excellence and through Vision 2025: From Regional Development Sustainability to Global Economic Growth, Granada, Spain, 30 May 2022; pp. 16411–16420. [Google Scholar]
- Ianculescu, M.; Nicolau, D.N.; Alexandru, A. Ensuring the Completeness and Accuracy of Data in a Customizable Remote Health Monitoring System. In Proceedings of the 2022 14th International Conference on Electronics, Computers and Artificial Intelligence (ECAI), Matsue, Japan, 30 June 2022; IEEE: New York, NY, USA, 2022; pp. 1–6. [Google Scholar]
- Ianculescu, M.; Alexandru, A.; Pop, F. Data Management in a Microservice Architecture of a Remote Patient Monitoring Application. In Proceedings of the International Business Information Management Conference (IBIMA) “Innovation Management and Sustainable Economic Development in the Era of Global Pandemic”, Seville, Spain, 23 November 2021; pp. 5743–5753. [Google Scholar]
- Ianculescu, M.; Alexandru, A.; Giura, I.-E.; Vasilevschi, A.-M. Delivering Improved Care through Remote Health Monitoring Systems by Using Microservices. In Case Study: Fall Detection Encompassed into Connected Care. In Proceedings of the 2023 24th International Conference on Control Systems and Computer Science (CSCS), Bucharest, Romania, 24–26 May 2023; IEEE: New York, NY, USA, 2023; pp. 598–605. [Google Scholar]
- Molinari Ulate, M.; Mahmoudi, A.; Parra−Vidales, E.; Muñoz−Sánchez, J.; van der Roest, H.G.; Franco-Martín, M.A. 410—A Systematic Review on Digital Health Interventions (DHIs) Supporting the Administration of Comprehensive Geriatric Assessments (CGAs) Use in Long-Term and Home Care Settings. Int. Psychogeriatr. 2021, 33, 35. [Google Scholar] [CrossRef]
- Mac Eochagain, C.; Senac, N.M.G.; Cavanagh, M.; Roy, M.; Ciccone, A.S.; Contreras, B.; Testa, G.D.; Velasco, R.; Marinho, J.; Serrano, A.G.; et al. Digital Health in Geriatric Oncology: A Young International Society of Geriatric Oncology Review. J. Geriatr. Oncol. 2023, 14, 101649. [Google Scholar] [CrossRef]
- Stara, V.; Soraci, L.; Takano, E.; Kondo, I.; Möller, J.; Maranesi, E.; Luzi, R.; Riccardi, G.R.; Browne, R.; Dacunha, S.; et al. Intrinsic Capacity and Active and Healthy Aging Domains Supported by Personalized Digital Coaching: Survey Study Among Geriatricians in Europe and Japan on EHealth Opportunities for Older Adults. J. Med. Internet Res. 2023, 25, e41035. [Google Scholar] [CrossRef]
- Bajenaru, O.-L.; Custura, A.-M. Enhanced Framework for an Elderly-Centred Platform: Big Data in Monitoring the Health Status. In Proceedings of the 2019 22nd International Conference on Control Systems and Computer Science (CSCS), Bucharest, Romania, 28–30 May 2019; pp. 643–648. [Google Scholar]
- Ianculescu, M.; Gavrila, V.; Petrache, C.; Tirlea, C. Improving the Elderly’s Fall Management through Innovative Personalized Remote Monitoring Solution. In Proceedings of the 2021 International Conference on e-Health and Bioengineering (EHB), Iasi, Romania, 18 November 2021; IEEE: New York, NY, USA, 2021; pp. 1–4. [Google Scholar]
- Spinsante, S.; Poli, A.; Mongay Batalla, J.; Krawiec, P.; Dobre, C.; Bǎjenaru, L.; Mavromoustakis, C.X.; Costantinou, C.S.; Molan, G.; Herghelegiu, A.M.; et al. Clinically-Validated Technologies for Assisted Living: The VINCI Project. J. Ambient Intell. Humaniz. Comput. 2023, 14, 2095–2116. [Google Scholar] [CrossRef]
- Alruwaili, M.M.; Shaban, M.; Elsayed Ramadan, O.M. Digital Health Interventions for Promoting Healthy Aging: A Systematic Review of Adoption Patterns, Efficacy, and User Experience. Sustainability 2023, 15, 16503. [Google Scholar] [CrossRef]
- Bãjenaru, L.; Balog, A.; Tomescu, M.; Drãghici, R. Satisfaction of Older Adults with Health Applications: VINCI Case Study. In Proceedings of the 2023 24th International Conference on Control Systems and Computer Science (CSCS), Bucharest, Romania, 24–26 May 2023; IEEE: New York, NY, USA, 2023; pp. 606–612. [Google Scholar]
- Bajenaru, L.; Dobre, C.; Ciobanu, R.-I.; Balog, A. Patient Profile Using Ontologies in an Older Adults Monitoring IoT-Based Platform. In Proceedings of the 2019 7th E-Health and Bioengineering Conference EHB, Iasi, Romania, 21–23 November 2019. [Google Scholar]
- Agarwal, A.; Pradhan, S. Review on Health And Quality of Life of Elderly People: A Meta-Analysis from The Medical and Health Sciences. J. Angiother. 2023, 7, 1–10. [Google Scholar] [CrossRef]
- Bajenaru, L.; Marinescu, I.A.; Dobre, C.; Prada, G.I.; Constantinou, C.S. Towards the Development of a Personalized Healthcare Solution for Elderly: From User Needs to System Specifications. In Proceedings of the 2020 12th International Conference on Electronics, Computers and Artificial Intelligence (ECAI), Bucharest, Romania, 25–27 June 2020; IEEE: New York, NY, USA, 2020; pp. 1–6. [Google Scholar]
- Clarfield, A.M.; Dwolatzky, T. Age and Ageing During the COVID-19 Pandemic; Challenges to Public Health and to the Health of the Public. Front. Public Health 2021, 9, 655831. [Google Scholar] [CrossRef]
- Paiva, J.O.V.; Andrade, R.M.C.; de Oliveira, P.A.M.; Duarte, P.; Santos, I.S.; de, P.; Evangelista, A.L.; Theophilo, R.L.; de Andrade, L.O.M.; de HC Barreto, I.C. Mobile Applications for Elderly Healthcare: A Systematic Mapping. PLoS ONE 2020, 15, e0236091. [Google Scholar] [CrossRef]
- Dobre, C.; Băjenaru, L.; Drăghici, R.; Prada, G.-I.; Balog, A.; Herghelegiu, A.M. Sustainable Health-Related Quality of Life in Older Adults as Supported by the VINCI Technology. Sensors 2023, 23, 2287. [Google Scholar] [CrossRef]
- Papachristou, N.; Kartsidis, P.; Anagnostopoulou, A.; Marshall-McKenna, R.; Kotronoulas, G.; Collantes, G.; Valdivieso, B.; Santaballa, A.; Conde-Moreno, A.J.; Domenech, J.R.; et al. A Smart Digital Health Platform to Enable Monitoring of Quality of Life and Frailty in Older Patients with Cancer: A Mixed-Methods, Feasibility Study Protocol. Semin. Oncol. Nurs. 2023, 39, 151437. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, K.; Nazarzadeh, M.; Pinho-Gomes, A.C.; Woodward, M.; Salimi-Khorshidi, G.; Ohkuma, T.; Fitzpatrick, R.; Tarassenko, L.; Denis, M.; Cleland, J. Home Monitoring with Technology-Supported Management in Chronic Heart Failure: A Randomised Trial. Heart 2020, 106, 1573–1578. [Google Scholar] [CrossRef]
- W Miller, T. Digital Health Transformed for Elderly Care Through the Metaverse. Int. J. Clin. Stud. Med. Case Rep. 2023, 27, 4. [Google Scholar] [CrossRef]
- Vasiljev, V.; Juraga, D.; Rukavina, T.; Bilajac, L.; Marinović Glavić, M.; Raat, H. Improving Health Outcomes of Patients with Myocardial Infarction with Value Based Methodology. Eur. J. Public Health 2023, 33, ckad160-1218. [Google Scholar] [CrossRef]
- Askenäs, L.; Campos, J.; Aidemark, J.; Boström, M. Integrated Care for Elderly Living at Home—A Case Description of IoT and Big Data Possibilities. Int. J. Integr. Care 2021, 20, 30. [Google Scholar] [CrossRef]
- Ejaz, M.; Kumar, T.; Kovacevic, I.; Ylianttila, M.; Harjula, E. Health-BlockEdge: Blockchain-Edge Framework for Reliable Low-Latency Digital Healthcare Applications. Sensors 2021, 21, 2502. [Google Scholar] [CrossRef]
- Cevallos, N.; Ramadhani, W.A.; Lindgren, J.; Bell, B.; Martinez-Cosio, M.; Harvey, T.E.; Nanda, U.; Mustata Wilson, G. (St)Aging in Place: Information and Communication Technologies for a Health-Centered Agile Dwelling Unit. Front. Public Health 2023, 11, 1057689. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.-H.; Hsu, W.-S. Integrating Artificial Intelligence and Wearable IoT System in Long-Term Care Environments. Sensors 2023, 23, 5913. [Google Scholar] [CrossRef]
- Lu, Y. A Knowledge-Driven Decision Support System for Remote Medical Management. Math. Biosci. Eng. 2022, 20, 2732–2749. [Google Scholar] [CrossRef] [PubMed]
- Brunzini, A.; Caragiuli, M.; Massera, C.; Mandolini, M. Healthy Ageing: A Decision-Support Algorithm for the Patient-Specific Assignment of ICT Devices and Services. Sensors 2023, 23, 1836. [Google Scholar] [CrossRef]
- Javadi-Pashaki, N.; Ghazanfari, M.J.; Karkhah, S. Machine Learning for Geriatric Clinical Care: Opportunities and Challenges. Ann. Geriatr. Med. Res. 2021, 25, 137–138. [Google Scholar] [CrossRef]
- Lapp, L.; Egan, K.; McCann, L.; Mackenzie, M.; Wales, A.; Maguire, R. Decision Support Tools in Adult Long-Term Care Facilities: Scoping Review. J. Med. Internet Res. 2022, 24, e39681. [Google Scholar] [CrossRef]
- Seljelid, B.; Varsi, C.; Solberg Nes, L.; Stenehjem, A.-E.; Bollerslev, J.; Børøsund, E. Content and System Development of a Digital Patient-Provider Communication Tool to Support Shared Decision Making in Chronic Health Care: InvolveMe. BMC Med. Inform. Decis. Mak. 2020, 20, 46. [Google Scholar] [CrossRef]
- Optimus Digital-MQ-2. Available online: https://www.optimusdigital.ro/ro/senzori-de-gaze/107-modul-senzor-gas-mq-2.html (accessed on 1 July 2024).
- Simagnoterc. Available online: https://www.sigmanortec.ro/Mod-ul-Senzor-ECG-EKG-AD8232-Kit-p141487101?gad_source=1 (accessed on 1 July 2024).
- Optimus Digital-MAX30102. Available online: https://www.optimusdigital.ro/ro/senzori-altele/12530-modul-senzor-pulsoximetru-max30102.html (accessed on 1 July 2024).
- Optimus Digital-DS18B20. Available online: https://www.optimusdigital.ro/ro/senzori/1465-senzor-de-temperatura-ds18b20-to-92.html?srsltid=AfmBOooQb8TPQ9ITe41QB6ecCbee5xns1bwR447bmMl4JOVeg6F6W5Ut (accessed on 20 August 2024).
- Optimus Digital-TCS230. Available online: https://www.optimusdigital.ro/ro/senzori-senzori-optici/111-modul-senzor-de-culoare-tcs230.html?gad_source=1&gclid=CjwKCAjw5qC2BhB8EiwAvqa41qj_zE74DzeP-aBcoZG2CMAwXc_UvgYLwoh3s0_Xybk8QnnHwMmy8xoCc90QAvD_BwE (accessed on 20 August 2024).
- Paraschiv, E.-A.; Ianculescu, M.; Petrache, M.-C. Building an Optimized Remote Healthcare Monitoring Scenario in Order to Alleviate the Pressure of COVID-19 Pandemic. Rev. Rom. Inform. Autom. 2021, 31, 83–96. [Google Scholar] [CrossRef]
- Optimus Digital-Accelerometru. Available online: https://www.optimusdigital.ro/ro/senzori-senzori-inertiali/11458-accelerometru-6dof-lsm303d.html?srsltid=AfmBOoo-bUr_ZGraIu0OsOBaqSv_1p020TO4drsOK7VPevuHLkmQweLDr (accessed on 1 July 2024).
- Ampul-Modul WiFi ESP8266. Available online: https://ampul.eu/ro/casa-inteligenta/2642-modul-wifi-esp8266-esp-12f-cu-baza-ch340?gad_source=1&gclid=CjwKCAjwuMC2BhA7EiwAmJKRrA3uCFVoddcgPZ0dgM_keFEfBzv7A6deOX7hT4HzOjXEuyYH3qUUmxoCSwIQAvD_BwE (accessed on 28 August 2024).
- Optimus Digital-DHT11. Available online: https://www.optimusdigital.ro/ro/senzori-senzori-de-tempera-tu-ra/99-senzor-de-temperatura-si-si-umiditate-dht11.html?gad_source=1&gclid=CjwKCAjwzIK1BhAuEiwAHQmU3kZSYuLM3MtqzPvFpwKzXQES9Q1mfQX5aHxQo8bl9lbHtaw-gOJ3l0RoCEecQAvD_BwE (accessed on 1 July 2024).
- Optimus Digital-BMP280. Available online: https://www.optimusdigital.ro/ro/senzori-senzori-de-presiune/12417-modul-senzor-de-presiune-barometric-hw-611-ep-280.html?gad_source=1&gclid=CjwKCAjwzIK1BhAuEi-wAHQmU3oBzsc0mMRaf3IDRTlkk_XVXj5kfthOMio5Z_3_iPeOGrKi7KoBibRoCCXUQAvD_BwE (accessed on 1 July 2024).
- Cleste.Ro-Senzor Temperatura. Available online: https://cleste.ro/modul-senzor-temperatura-dfr0023.html (accessed on 1 July 2024).
- Optimus Digital-TSL2591. Available online: https://www.optimusdigital.ro/ro/senzori-senzori-optici/3351-senzor-de-lumina-digital-adafruit-tsl2591.html?srsltid=AfmBOop68ZwS2otTVbtEgRedzedVscB7lbeJqSBnMeKrwBmnqg86heTa (accessed on 1 July 2024).
- Optimus Digital-CCS811. Available online: https://www.optimusdigital.ro/ro/senzori-de-gaze/4865-mod-ul-senzor-calitate-aer-sgp30-voc-i-eco2-adafruit.html?gad_source=1&gclid=CjwKCAjwzIK1BhAuEiwAHQmU3nYrvcKQCph6ymFtxSWrTG46sjuYE-spQgnRX5Aj0xPjqDX2BP6JHtBoCXQ4QAvD_BwE (accessed on 1 July 2024).
- Optimus Digital-MQ2. Available online: https://www.optimusdigital.ro/ro/senzori-de-gaze/1126-mod-ul-senzor-de-gaz-mq-5.html?gad_source=1&gclid=CjwKCAjwzIK1BhAuEiwAHQmU3qjEwXE-AcEe1IbTQpHAleHCfEbxmAGnJ6XoVz1ggHZrgfYvaNOJoYRoC6QcQAvD_BwE (accessed on 1 July 2024).
- Optimus Digital-PIR. Available online: https://www.optimusdigital.ro/ro/senzori-senzori-pir/1498-senzor-pir-in-miniatura-hc-sr505.html?gad_source=1&gclid=CjwKCAjwzIK1BhAuEiwAHQmU3sox2tb23bTKtjI-uJVZnBSgFK-pAVxDI1Wt7dyc-p3qA72ZlGmBOZxoCjWkQAvD_BwE (accessed on 1 July 2024).
- Elena-Anca, P.; Ovidiu, B.; Cristian, P.; Ianculescu, M. IoT-Based Ambient Parameters Monitoring Device for in-Home Elderly Care. In Proceedings of the 2021 23rd International Conference on Control Systems and Computer Science (CSCS), Bucharest, Romania, 26–28 May 2021; IEEE: New York, NY, USA, 2021; pp. 495–500. [Google Scholar]
- Ardusop. Available online: https://ardushop.ro/ro/home/1300-senzor-sonda-temperatura-impermeabil-ds18b20-dsb18b20.html?gad_source=1 (accessed on 31 May 2024).
- Farnell-SFM3300-D. Available online: https://ro.farnell.com/sensiri-on/sfm3300-d/airflow-sen-sor-i2c-digital-1-1bar/dp/3804265?cjdata=MXxZfDB8WXww&gross_price=true&CMP=AFC-CJ-SK-8280252&source=CJ&cjevent=a9cfc9fa47b011ef835c3a3a0a18b8f9 (accessed on 31 May 2024).
- Distrelec. Available online: https://www.distrelec.ro/ro/gsr-sensor-seeed-studio-101020052/p/30069834 (accessed on 31 May 2024).
- Elecbee. Available online: https://www.elecbee.com/en-25698-GY-511-LSM303DLHC-E-Compass-3-Axis-Magnetometer-And-3-Axis-Accelerometer-Module (accessed on 31 May 2024).
- Robofun. Available online: https://www.robofun.ro/spark-fun-gps-breakout-chip-anten-na-sam-m10q-qwiic.html?gad_source=1 (accessed on 31 May 2024).
- Cel. Available online: https://www.cel.ro/modul-serial-cu-bluetooth-hm10-oky3375-1-pMiEyNDwrMg-l/?gad_source=1 (accessed on 31 May 2024).
- Farnell-MZ-16. Available online: https://www.fruugo.ro/-z16-0-5000ppm-carbon-diox-ide-sensor-module-air-quali-ty-co2-detection-support-uart-pwm-output/p-303750812-680792104?language=en&ac=KelkooCSS&asc=pmax&gad_source=1 (accessed on 31 May 2024).
- Zhang, Z.; Amegbor, P.M.; Sabel, C.E. Assessing the Current Integration of Multiple Personalised Wearable Sensors for Environment and Health Monitoring. Sensors 2021, 21, 7693. [Google Scholar] [CrossRef] [PubMed]
- Nourse, R.; Dingler, T.; Kelly, J.; Kwasnicka, D.; Maddison, R. The Role of a Smart Health Ecosystem in Transforming the Management of Chronic Health Conditions. J. Med. Internet Res. 2023, 25, e44265. [Google Scholar] [CrossRef] [PubMed]
- Badawy, M.; Ramadan, N.; Hefny, H.A. Healthcare Predictive Analytics Using Machine Learning and Deep Learning Techniques: A Survey. J. Electr. Syst. Inf. Technol. 2023, 10, 40. [Google Scholar] [CrossRef]
- Dirin, A.; Oliver, I.; Laine, T.H. A Security Framework for Increasing Data and Device Integrity in Internet of Things Systems. Sensors 2023, 23, 7532. [Google Scholar] [CrossRef]


| Application/System | Key Attributes | Disadvantages/Shortcomings | Advantages of Brought by RO-SmartAgeing System and NeuroPredict Platform |
|---|---|---|---|
| Telehealth Platforms [24,35] | Enhance healthcare access, support continuous monitoring, and improve CGAs by enhancing data availability. | Lack of integration with advanced decision-making tools, limited data analysis capabilities. | Offer more comprehensive real-time monitoring and advanced decision-making tools. |
| Mobile Health Applications [47] | Support continuous monitoring, enable early detection of health issues, and improve communication between patients and providers. | Often limited in scope, focusing on specific health metrics without integration into broader healthcare systems. | Provide a more holistic approach, integrating various health metrics and offering predictive analytics. |
| Wearable Devices [52] | Monitor vital signs and physical activities and enable remote health oversight. | Limited to specific functions (e.g., heart rate and steps), may not provide comprehensive health insights. | Integrate data from wearables into a larger system that supports complex decision-making. |
| IoT Systems [44] | Support active lifestyles, enhance sensory experiences, promote social interaction, and deliver continuous remote monitoring. | Potentially complex to manage, may not offer real-time predictive analytics. | Streamline data from IoT devices into actionable insights for proactive healthcare management. |
| vINCI System [40,48] | Integrates devices like smart insoles, depth cameras, smartwatches, and a mobile application for continuous monitoring and early detection. | Might lack integration with broader healthcare systems and advanced predictive analytics. | Offer a more integrated approach with advanced analytics and real-time decision-making capabilities. |
| LifeChamps Digital Platform [49] | Integrates AI and big-data analytics for predictive modeling and supports continuous health monitoring and functional assessment for older cancer patients. | Focuses on a specific patient group (older cancer patients), which may limit broader applicability. | Are designed to cater to a wider range of geriatric and neurodegenerative conditions with broader system integration. |
| Metaverse [51] | Provides a virtual environment for elderly patients to access healthcare information and engage in educational activities. | Primarily educational, may not offer direct health monitoring or real-time data integration. | Focus on real-time health monitoring and data-driven decision-making rather than purely educational experiences. |
| Agile Dwelling Units (AgDUs) [55] | Integrate ICTs to provide personalized, sustainable solutions for independent living, adapting to older adults’ needs throughout the patient’s lifespan. | May lack advanced health monitoring and decision-making capabilities. | Integrate environmental monitoring with health data analysis for comprehensive management of the care of elderly patients. |
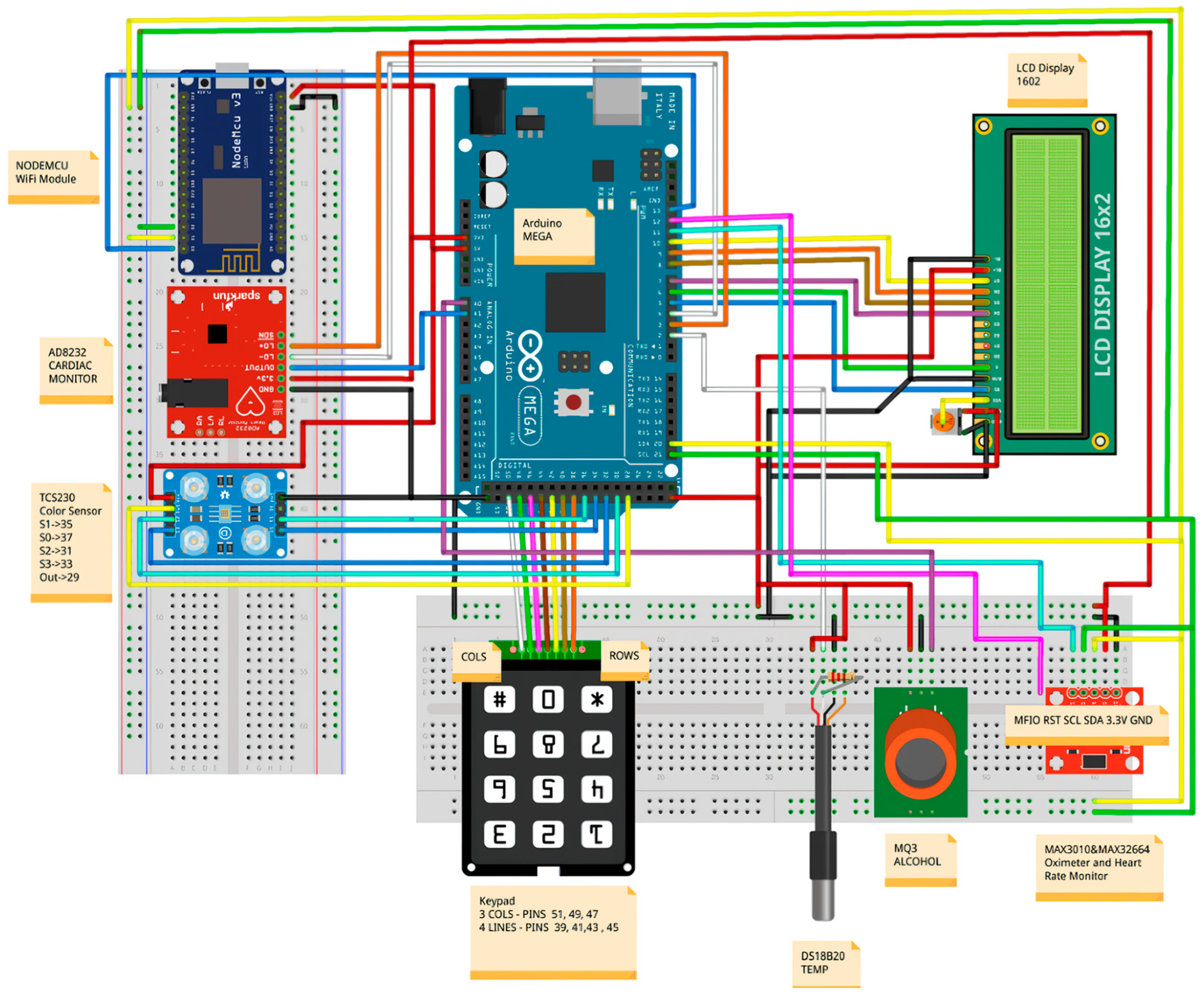
| Sensor Type | Function | Key Specification | Technical Details |
|---|---|---|---|
| Alcohol Gas Sensor (MQ-2) [62] | Measures alcohol concentration in breath | Detection range: 10–1000 ppm ethanol; Operating voltage: 5 V; Response time: Typically within 10 s | Measurement principle: Uses a semiconductor sensor that changes resistance in the presence of ethanol; Components: MQ-2 sensor element, heater, and sensitive layer; Sensitivity: Detects various gases, including alcohol, methane, and propane |
| EKG Sensor (AD8232) [63] | Monitors electrical activity of the heart | Signal output: Analog; Operating voltage: 3.3 V to 5 V; Bandwidth: 0.5 to 40 Hz; Noise rejection: High | Measurement principle: Extracts and amplifies the small electrical signals generated by the heart; Components: AD8232 IC, electrodes, amplification circuit; Signal conditioning: Includes filtering for noise and motion artifact removal |
| Pulse Oximeter Sensor (MAX30102) [64] | Measures blood oxygen saturation and heart rate | SpO2 range: 70–100%; Heart rate range: 30–240 bpm; Operating voltage: 1.8 V to 3.3 V; Data rate: Up to 1 kHz | Measurement principle: Photoplethysmography uses LEDs to emit light and photodetectors to measure the absorption of light by blood; Components: Internal LEDs (red and infrared), photodetectors, low-noise electronics; Ambient light rejection: Designed to minimize interference from external light sources |
| Temperature Sensor (DS18B20) [65] | Measures ambient temperature (inside the Medical Blackbox) | Temperature range: −55 °C to +125 °C; Accuracy: ±0.5 °C (from −10 °C to +85 °C); Operating voltage: 3.0 V to 5.5 V | Measurement principle: Uses a digital sensor to provide temperature readings; Components: DS18B20 sensor chip, one-wire digital interface; Resolution: Programmable 9- to 12-bit precision |
| Color Detection Sensor (TCS230) [66] | Detects changes in color on urine test strips to analyze biochemical parameters | Detection range: Full-spectrum color detection; Operating voltage: 2.7 V to 5.5 V; Output: Frequency proportional to the color intensity | Measurement principle: Uses an array of photodiodes and filters to detect RGB color values, converting them to a frequency signal; Components: TCS230 sensor element, RGB LEDs, photodiodes, and an internal oscillator; Application: Suitable for monitoring biochemical parameters in urine via colorimetric analyses on test strips |
| Sensor Type | Function | Key Specification | Technical Details |
|---|---|---|---|
| Accelerometer (LSM303D, 6-axis) [68] | Measures acceleration and orientation | Measurement range: ±2 g, ±4 g, ±8 g, ±16 g; Operating voltage: 2.5 V to 3.6 V; Interface: I2C | Measurement principle: Detects acceleration in three axes and magnetic fields in two axes; Components: Micro-electro-mechanical systems accelerometer and magnetometer; Sensitivity: High precision for motion and orientation tracking |
| Gyroscope (LSM303D, 6-axis) [68] | Measures angular velocity and rotational movement | Measurement range: ±250°/s to ±2000°/s (combined with accelerometer); Operating voltage: 2.5 V to 3.6 V; Interface: I2C | Measurement principle: Detects rotational changes around three axes; Components: Integrated with the accelerometer in the LSM303D; Sensitivity: Precision in rotational motion detection |
| Wi-Fi Module (Espressif NodeMCU 8266) [69] | Facilitates wireless data transmission | Operating voltage: 3.3 V; Interface: I2C, UART; Data rate: Up to 80 Mbps | Measurement principle: Provides wireless connectivity for data transfer to the cloud; Components: Wi-Fi transceiver module; Sensitivity: Reliable connection for real-time data transmission |
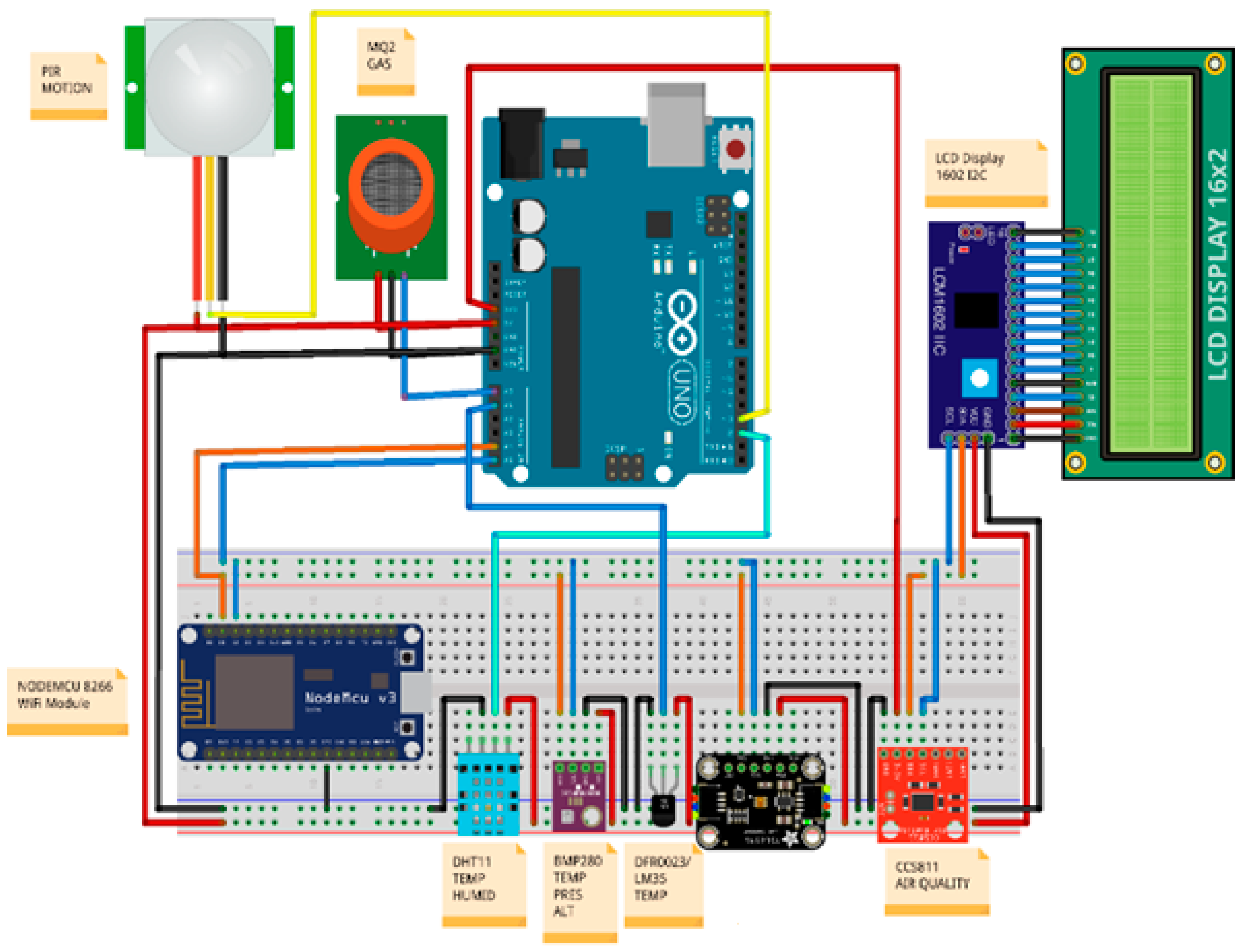
| Sensor Type | Function | Key Specification | Technical Details |
|---|---|---|---|
| Temperature and Humidity Sensor (DHT11) [70] | Measures ambient temperature and humidity | Measurement range: 0–50 °C, 20–80% RH; Operating voltage: 3.3 V–5 V | Measurement principle: Uses a digital sensor with a humidity-sensitive component and a temperature sensor; Components: DHT11 sensor element; Accuracy: ±1 °C for temperature, ±5% RH for humidity |
| Temperature and Pressure Sensor (BMP280) [71] | Measures ambient temperature and atmospheric pressure | Measurement range: 300–1100 hPa; Operating voltage: 1.8 V–3.6 V | Measurement principle: Uses piezoelectric technology to measure pressure and temperature; Components: BMP280 sensor element; Accuracy: ±1 hPa for pressure, ±1 °C for temperature |
| Temperature Sensor (LM35) [72] | Measures ambient temperature | Measurement range: −55 °C–150 °C; Operating voltage: 4 V–30 V | Measurement principle: Produces a linear voltage output that is directly proportional to temperature; Components: LM35 sensor element; Accuracy: ±0.5 °C |
| Light Sensor (TSL2591) [73] | Measures light intensity | Measurement range: 0–88,000 lux; Operating voltage: 3.3 V | Measurement principle: Uses photometric technology to measure light intensity; Components: TSL2591 sensor element; Accuracy: ±20 lux |
| Air Quality Sensor (CCS811) [74] | Measures CO2 concentration and volatile organic compounds | Measurement range: 400–8192 ppm CO2; Operating voltage: 3.3 V | Measurement principle: Detects CO2 levels and volatile organic compounds using a metal oxide sensor; Components: CCS811 sensor element; Accuracy: ±50 ppm for CO2 |
| Gas Sensor (MQ2) [75] | Detects presence of gases (CH4, CO) and smoke | Measurement range: 10–1000 ppm; Operating voltage: 5 V | Measurement principle: Uses a semiconductor sensor that changes resistance in the presence of gases; Components: MQ2 sensor element, heater, and sensitive layer; Sensitivity: Detects alcohol, methane, and propane |
| Motion Sensor (PIR) [76] | Detects motion in the environment | Detection range: 1–7 m; Operating voltage: 5 V | Measurement principle: Uses passive infrared technology to detect motion; Components: PIR sensor element; Sensitivity: Adjustable to detect movement within different ranges |
| Decision-Making Tool | Newly Added Sensor | Main Characteristics | Enhanced Decision-Making Capabilities |
|---|---|---|---|
| Medical Blackbox | Waterproof Temperature-Probe Sensor (DS18B20) [78] | Measures temperature in a range of −20 to 105 °C under various environmental circumstances | Provides information necessary for monitoring body temperature fluctuations that can be suggestive of infections or other health disorders, and is especially important in managing neurological diseases in cases where the regulation of temperature may be affected. |
| Medical Blackbox | Sensirion CO2 Sensor (SFM3300-D) [79]. | Measures air and gas flow with high precision and a digital interface | Improves the capacity to monitor respiratory function and air quality, which is significant for people with neurological diseases like PD, where respiratory problems are widespread. Accurate CO2 measurements enable immediate action and care improvements. |
| Medical Blackbox | Galvanic Skin Response Sensor [80] | Measures galvanic skin response, indicating physiological or emotional activity levels by changes in skin conductivity | Assesses stress and psychological alterations that might impact cognitive performance and general well-being in individuals with neurodegenerative diseases. Addressing these characteristics enables better management of symptoms associated with emotional or psychological stress. |
| Gaitband | Accelerometer (6-Axis) and Magnetometer (GY-511 LSM303DLHC) [81] | Provides extensive movement and orientation data by combining accelerometer and magnetometer measurements | Improves gait and posture monitoring, which is vital for early identification and continuing evaluation of neurodegenerative disorders such as PD disease or AD, as motor symptoms and postural instability are prominent. |
| Gaitband | GPS Module (SAM-M10Q) [82] | High-accuracy GPS module supplied with a u-blox SAM-M8Q GPS receiver for accurate location and navigation information | Supports tracking, including outdoor activities, patient mobility, and spatial orientation, which is essential for patients with cognitive decline or movement disorders. It facilitates safeguarding and assistance by identifying differences from usual movement patterns or potential wandering. |
| Gaitband | Bluetooth Module (HM-10) [83] | Supports Bluetooth Low Energy 4.0 for efficient and low-power communication | Improves real-time data synchronization across devices and allows for easy integration into the health management system. For neurodegenerative patients, this enables constant monitoring and rapid adaptations according to the data gathered, thereby enhancing geriatric and neurodegenerative care management. |
| Ambient Blackbox | Gas Sensor (MH-Z16) [84] | Measures CO2 concentrations up to 50,000 ppm, useful for assessing air quality | Enables the monitoring of environmental conditions that impact respiratory health, which is important for the management of neurological diseases with respiratory consequences. Enhanced air-quality data allow the creation of a safe and healthy living environment for patients who are at risk. |
| Feature | RO-SmartAgeing System Decision-Making Tools (Medical Blackbox, Gaitband, Ambient Blackbox) | NeuroPredict Platform Decision-Making Tools (Medical Blackbox, Gaitband, Ambient Blackbox) |
|---|---|---|
| Number of Sensors and Technology | 15 | 17, of which 5 are new and 1 is improved |
| Physiological Parameters in Medical Blackbox | EKG, heart rate, alcohol concentration in breath, blood oxygen saturation, heart rate, spectrogram, internal temperature | EKG, heart rate, alcohol concentration in breath, blood oxygen saturation, body temperature, air and gas flow, galvanic skin response |
| Environmental Parameters in Ambient Blackbox | Ambient temperature, humidity, atmospheric pressure, light intensity, CO2 concentration and volatile organic compounds, presence of gases (CH4, CO) or smoke, motion in the environment | Ambient temperature, humidity, atmospheric pressure, light intensity, volatile organic compounds, presence of gases (CH4, CO) or smoke, motion in the environment, improved measurement of CO2 concentrations |
| Motion Parameters in Gaitband | Acceleration, orientation, angular velocity, rotational movement | Improved detection of acceleration, orientation, angular velocity, and rotational movement due to the 6-axis accelerometer with enhanced sensitivity for fall detection, GPS |
| Gaitband Response Time | Immediate fall-detection response | Improved algorithm reduces false alarms and enhances response time (currently under development) |
| Monitoring Interval | Continuous monitoring, with periodic manual checks | Continuous with adaptive intervals based on patient condition |
| Fall-Detection Sensitivity | Moderate, with occasional false positives | Improved fall-detection accuracy due to enhanced algorithm, sensors and technology (currently under development) |
| Battery Life | Gaitband: 48 h (504060 battery) | Gaitband: 50 h (103450 battery) |
| Wireless Connectivity | Wi-Fi connectivity | Bluetooth 4.0, Wi-Fi connectivity |
| Data Storage and Security | Secure storage with basic encryption | Advanced security protocols, with additional data protection features (currently under development) |
| Physical Dimensions | Compact and portable, suitable for elderly users | Slightly reduced size for easier wearability and handling |
| Material Used for 3D Printing the Devices | Polylactic acid—unprotected environmentally friendly material, with rapid degradation | Polylactic acid with an extra layer to ensure minimal environmental impact with slower degradation |
| Potential for Using Collected Data for Customized Decision-Making Support | Tailored to geriatric health profiles | Enhanced personalization, with cognitive and environmental factors associated with PD, AD, and MS |
| Aspect Evaluated | Feedback Summary | Comments | Enhancements in NeuroPredict Platform |
|---|---|---|---|
| Ease of use | Generally intuitive, but varied feedback depending on the tester’s role. Healthcare providers found it efficient, while elderly testers struggled with the small display on the Medical Blackbox. | Medical Blackbox: The 4-row LCD screen was noted as being challenging for elderly users with visual impairments. Healthcare providers suggested a more prominent and clear display. | Medical Blackbox: Plans to introduce a larger, high-contrast display with voice-assisted navigation (currently under development) |
| Sensor accuracy | Accurate in most conditions, but discrepancies were noted by testers simulating patient roles, particularly in fall detection with the Gaitband. | Gaitband: Improved fall-detection sensitivity was observed by healthcare providers, but false positives were reported by those in patient roles, especially in dynamic environments. | Gaitband: Enhanced algorithms and sensors are being integrated to reduce false positives and increase accuracy levels across different conditions (currently under development) |
| System responsiveness | Immediate response in most cases; however, technical support testers noticed a slight delay in data transmission in low-connectivity environments. | Ambient Blackbox: Responsiveness was satisfactory, but Wi-Fi interruptions affected real-time data availability, particularly in more complex testing scenarios. | Ambient Blackbox: Implementation of a dual-connectivity option (Wi-Fi and Bluetooth) to ensure a more reliable transmission of data |
| Overall user experience | Positive overall, but testers in prolonged usage scenarios suggested improvements in battery life and connectivity. | Gaitband: Healthcare providers appreciated the extended monitoring capabilities, while users simulating patients suggested the need for better battery performance for continuous use. | Gaitband: Battery-life improvements are being made, along with enhanced connectivity options to assure consistent performance |
| Setup and configuration | Straightforward for tech-savvy users, challenging for elderly users or those less familiar with technology. | All decision-making tools: Elderly testers found the setup process complex, while technical support testers suggested a more streamlined and intuitive configuration process. | All decision-making tools: Development of a simplified, step-by-step setup guide with visual aids and a more intuitive interface is planned |
| Comfort during use | Generally comfortable, though testers in patient roles found the Gaitband’s chest placement slightly restrictive. | Gaitband: Elderly users noted the chest placement as being somewhat uncomfortable during prolonged use. Healthcare providers suggested alternative placements or adjustments for increased comfort. | Gaitband: Redesigns are underway to offer alternative placements and designs which are more ergonomic for enhanced comfort. |
| Device durability and build quality | Robust and durable, but concerns were raised about long-term wear and tear, particularly by testers simulating active patient roles. | All Tools: The materials used were praised for their durability by healthcare providers, but testers in active roles expressed concerns about the sensors’ longevity and the casing’s ability to withstand daily wear. | All Tools: Ongoing material improvements aim to increase durability while maintaining lightweight and user-friendly designs. |
| Environmental impact of materials | Positive feedback overall, with elderly testers appreciating the eco-friendly materials, but concerns about rapid degradation were noted by those in technical roles. | All Tools: The use of polylactic acid was appreciated for its environmental benefits, though technical testers raised issues regarding its durability and rate of degradation. | All Tools: An improved material composition that balances environmental responsibility with longevity is being developed. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Băjenaru, O.L.; Băjenaru, L.; Ianculescu, M.; Constantin, V.-Ș.; Gușatu, A.-M.; Nuță, C.R. Geriatric Healthcare Supported by Decision-Making Tools Integrated into Digital Health Solutions. Electronics 2024, 13, 3440. https://doi.org/10.3390/electronics13173440
Băjenaru OL, Băjenaru L, Ianculescu M, Constantin V-Ș, Gușatu A-M, Nuță CR. Geriatric Healthcare Supported by Decision-Making Tools Integrated into Digital Health Solutions. Electronics. 2024; 13(17):3440. https://doi.org/10.3390/electronics13173440
Chicago/Turabian StyleBăjenaru, Ovidiu Lucian, Lidia Băjenaru, Marilena Ianculescu, Victor-Ștefan Constantin, Andreea-Maria Gușatu, and Cătălina Raluca Nuță. 2024. "Geriatric Healthcare Supported by Decision-Making Tools Integrated into Digital Health Solutions" Electronics 13, no. 17: 3440. https://doi.org/10.3390/electronics13173440
APA StyleBăjenaru, O. L., Băjenaru, L., Ianculescu, M., Constantin, V.-Ș., Gușatu, A.-M., & Nuță, C. R. (2024). Geriatric Healthcare Supported by Decision-Making Tools Integrated into Digital Health Solutions. Electronics, 13(17), 3440. https://doi.org/10.3390/electronics13173440






