Abstract
In the past decade, Internet of Things (IoT) technologies have become more and more pervasive, allowing the development of Ambient Intelligence and Context Awareness applications. While the smart home is the chosen scenario for such technologies, a variety of environments could potentially benefit from the synergies between IoT and digital applications. Among them, the clinical waiting rooms is an environment facing several challenges, particularly after the COVID-19 pandemic. Clinical waiting rooms are crowded places associated with stress and anxiety, often linked to patients’ idling time. Nonetheless, the rise of IoT-enabled telehealth has focused attention on the possibility of changing the functions of clinical waiting rooms. In this work, we conducted a systematic literature review to identify the existing solutions for “smart waiting rooms”. The review process started with 278 works, and it identified 16 papers relevant to the topic of smart clinical waiting rooms. Moreover, the results of this review underlined that waiting rooms are a neglected research area that could take advantage of IoT and Artificial Intelligence (AI) technologies to enhance patients’ experience and support the diagnostic process. Leveraging the research directions identified in the review process, this work proposes a “Smart Waiting Room” that exploits virtual reality (VR), AI, and IoT technologies to support the diagnostic process (via a cognitive assessment) and the personalization of the patient’s context—taking into account the features of the physical environment. The prototypical smart waiting room constitutes an example of the potentialities of novel technologies applied to healthcare and can contribute to shaping the future of clinical waiting rooms.
1. Introduction
The diffusion of Internet of Things (IoT) technologies greatly enhanced the possibility for smart homes to deliver personalized solutions according to users’ preferences and needs [1]. IoT-enabled smart homes can support dwellers in the management of energy consumption and the adoption of energy-saving behaviors; they can support indoor comfort settings (also tailored to user’s preferences); and they can also monitor and provide for those users who are not completely independent and are characterized by special needs. To date, IoT-enabled smart homes can enhance dwellers’ quality of life, foster older adults’ independent living, and anticipate users’ needs.
Although smart homes have to face a significant number of challenges to get to market (e.g., social challenges related to individual monitoring and privacy; technological challenges concerning data management between the smart home, healthcare providers, and third-party applications; challenges related to personal data security, leakage, and external attacks) [1], disciplines such as Ambient Intelligence, Artificial Intelligence (AI), and Context Awareness—fueled by advancements in IoT technologies—further evolved the paradigm of smart homes into the “smart environment”, i.e., a physical space in which smart devices continuously work for occupants’ comfort and well-being [2]. In such a context, any human-built environment could be enhanced by physical and digital technologies devoted to occupants’ monitoring and comfort.
However, while the scientific literature on smart homes has thrived in the past two decades (see, for instance, the meta-reviews dedicated to different smart-home-related functions [3,4,5]), far fewer studies have been devoted to smart environments outside the domestic walls. Among them, waiting rooms are particular environments characterized by the co-presence of several individuals “forced” to occupy a room while waiting for a service or information. In particular, clinical waiting rooms—i.e., waiting rooms designed to accommodate patients or their caregivers in the General Practice (GP) medical office, hospitals, and Emergency Rooms (ERs)—exist in all countries and are characterized by the same issues and challenges.
The most known and common issue in waiting rooms is the patients’ perceived inactivity during the waiting time. Waiting times are strongly related to patients’ overall satisfaction [6], to the point that increased waits negatively impact patients’ willingness to return to a structure for a service [7]. They also impact the perceived level of care (i.e., longer waits are associated with a lower quality of the received care) [8]; moreover, longer waiting times are also associated in some cases with patients’ clinical deterioration [9]. Finally, studies conducted in the 1990s illustrate that the waiting room’s physical environment can play a pivotal role in both customer satisfaction [10] and perceived quality of care [11]. To these issues, each patient’s specific needs and peculiarities may somehow impact his/her perception of waits and care.
For several years, researchers have investigated how to reduce waiting times from several perspectives and also how to intervene to make waiting times more productive [12]. However, several countries’ national health systems are currently stressed as a consequence of the recent COVID-19 pandemic, which resulted in clinicians having to visit more patients [13] and in care pathways being revisited to include primary, short-term, and long-term care [14]. While healthcare systems are undergoing significant changes, patients may have to face longer waits due to overloads to clinics, hospitals, and General Practices—due to delayed essential clinical care [15] and backlogs [16].
Nevertheless, the COVID-19 pandemic acted as an eye-opener for the adoption of telehealth and digital technologies in healthcare, proving that IoT and smart technologies can significantly support diagnosis and visit delivery in some cases [17]. Hence, considering the current advancements in smart environments and the IoT, it is plausible to assume that patients’ waits in clinical waiting rooms could be somehow “enhanced” or tailored. In particular, it is known that there are a few intervention areas that can be tackled in waiting, e.g., reducing the amount of unoccupied time during the waiting [10], reducing anxiety during wait times [18], and reducing the uncertainty in waiting (try to motivate the amount of time spent waiting by patients) [10].
Therefore, this work aims to investigate the role of smart technologies in clinical waiting rooms. By adopting a systematic literature review approach, this article tries to answer the following Research Questions (RQs):
- RQ1: what is the purpose of the proposed smart waiting room?
- RQ2: what category (or categories) of patients does the identified solution address?
- RQ3: what technologies do the identified solutions adopt?
- RQ4: in which clinical contexts (ER, hospital, GP office, etc.) are the identified solutions adopted?
The literature review contributes to the research on smart waiting rooms, an under-explored topic, while identifying the main trends adopted or investigated by researchers.
The remainder of this paper is organized as follows: Section 2 presents the methodology adopted for the literature review. Section 3 illustrates the quantitative results of the review process, while Section 4 discusses them in light of the RQs identified above and attempts to draft some possible research directions. Section 5 describes a proposal for a smart waiting room and its components. Section 6 summarizes the main outcomes of this paper and illustrates future works to be conducted on the proposed smart waiting room.
2. Review Methodology
To answer the four RQs presented in the Introduction, this article adopts the systematic literature review using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) approach [19]. This approach enables the identification of relevant scientific works in the domains of interest following a transparent step-by-step method. This article reviews scientific papers limited to conference proceedings, book chapters, and journal articles published between 2000 and 2024, focusing solely on English-language publications.
2.1. Database and Queries
The databases queried for this review were Clarivate ISI Web of Science, PubMed, Scopus, and ProQuest. Since all databases enable queries using logical operators and are accessible online, they were selected as eligible for the scope of this review. In particular, the queries performed were:
- Q1: “smart” AND “waiting room”;
- Q2: “techn*” AND “waiting room”;
- Q3: “virtual” AND “waiting room”;
- Q4: “smart” AND “foyer”.
Such strings were searched in the title, abstract, and authors’ keywords of the records, limiting the search to conference proceedings papers, journal articles, and book chapters published between 2000 and 2024 (to include those works accepted for publication in 2023 but expected to be published in the following year). The range of publication years selected corresponds to the years when researchers started to investigate smart environments that enabled (or combined) Ambient Intelligence, Context Awareness, or Artificial Intelligence techniques. The database search was conducted in July 2023 and updated in November 2023.
2.2. Article Retrieval and Selection Process
Following the PRISMA methodology, the works pertaining to the RQs were identified by selecting relevant articles from the records retrieved after the database search. The process is represented in Figure 1 in detail.
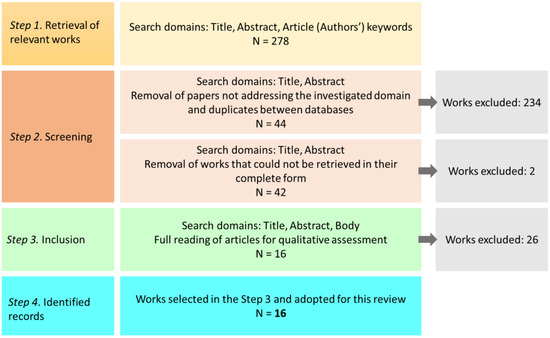
Figure 1.
The PRISMA flow diagram adopted in this review to retrieve, screen, include, and identify the relevant articles.
- Retrieval of the works: In this step, the search retrieved 278 works. Taking into account the specific RQs, the search was limited to subject areas: computer science, engineering, medicine, social sciences, and decision sciences.
- Screening: The retrieved works’ abstracts, titles, and authors’ keywords were scrutinized to provide a preliminary qualitative evaluation, assessing whether or not the retrieved works addressed the domain underlying the four RQs. In this step, duplicate works were also identified and removed. A total of 213 papers were found not to meet the criteria (i.e., they did not address clinical waiting rooms, or they did not rely on any technology). In comparison, 21 papers were duplicated among the different databases. The number of papers identified as relevant was 44. Finally, the 44 works were accessed in their complete form, resulting in 2 papers being removed due to their inaccessibility.
- Inclusion: The 42 papers identified in the previous step were carefully read by three of the authors of this review to assess their adherence to the RQs identified in the Introduction. At the end of this step, 26 papers were found unsuitable to answer any of the RQs.
- Identified records: the number of papers included in this review was 16.
3. Results
This section presents the results of the review process illustrated in Section 2. The presentation of bibliometric results is devoted to presenting the temporal and geographical distribution of articles and the type of articles. The presentation of results related to the articles’ content (content analysis) aims to answer the RQs raised in the Introduction. The results are discussed and commented on in Section 4.
3.1. Biliometric Results
3.1.1. Temporal Distribution and Type of Articles by Year
The temporal distribution of the 16 identified works and their type are presented in Figure 2. This figure indicates the relevance of the works retrieved only from 2009, with peaks in 2019, 2022, and 2023 (three works per year). The list of identified works consists of four conference proceedings papers (CP) and 12 journal articles (JA). No book chapters were found within the identified works.
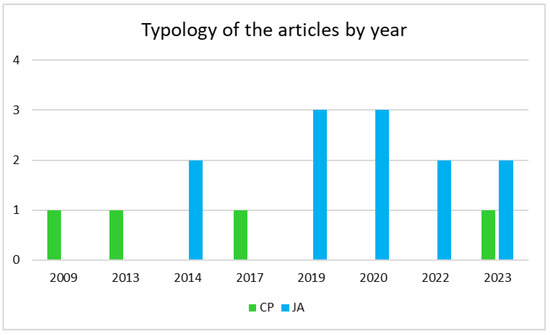
Figure 2.
The distribution of articles by year, grouped by their types (CP: conference proceeding; JA: journal article).
3.1.2. Geographical Distribution of the Authors
An analysis of the geographical distribution of the works was performed to observe in which countries the topic of smart waiting rooms has been investigated. In particular, the author(s)’ affiliation(s) at the time of paper publication was considered (the same author appearing with the same affiliation in two different works was considered once; the same authors with different affiliations contributing to two different papers were considered twice). Table 1 reports the geographical distribution of authors by country (grouped by continent).

Table 1.
Geographical distributions of the authors of the identified records.
The United States of America registered the highest number of authors (47), making North America the continent with the highest number of unique authors (52). Europe accounted for 24 authors, while Asia and Oceania registered 7 authors. Finally, contributions from Africa amounted to four. It is interesting to observe that there is no contribution from South American countries and that only two works are written by authors from different countries: the study of [20] is authored by African and Asian authors, while [21] sees authors from two different European countries.
3.2. Content Analysis
Following the RQs identified in Section 1, it is possible to cluster the retrieved articles to identify their aim(s) towards the waiting activity (RQ1), the type(s) of patients that could benefit from such a smart solution (RQ2), in which type(s) of clinical waiting room they are deployed (RQ3), and the set of technologies required to operate them (RQ4). The quantitative results gathered in this subsection are discussed in the following section.
3.2.1. Purposes of the Smart Waiting Rooms
To provide an answer to RQ1, it is necessary to cluster the included papers according to the type(s) of aims the smart waiting rooms are developed to tackle. Taking into account the issues related to waiting depicted in the Introduction, three clusters have been identified:
- (A)
- Waiting enhancement: the solutions address the problem of shortening or optimizing the waiting times or produce some effects on the waiting patients (e.g., reduce anxiety, provide them with more information about the medical procedures they are going to experience, inform them of some particular aspects of a disease);
- (B)
- Pre-visit data acquisition: the solutions are devoted to exploiting the waiting time in the waiting rooms to acquire physiological or psychological measurements from patients; the acquired data are necessary for the subsequent visit;
- (C)
- Assessment and diagnosis: waiting times are exploited to perform an assessment of some clinical aspects of the patients and are not necessarily related to the visit they are undergoing.
The results of grouping the 16 articles according to the clusters identified above are reported in Table 2.

Table 2.
The purposes of smart waiting rooms addressed in the analyzed works. In this table, papers are ordered by cluster and by year.
Quantitatively, the majority of the works address solutions devoted to enhancing the quality of the time spent waiting in the waiting room (cluster A, nine papers). The enhancement is achieved by leveraging a wide range of technologies and is tackled from different perspectives, e.g., optimization of the waiting times and redistribution of patients, stress and anxiety reduction, and patient education. The second-most populated cluster (C, five papers) is related to exploiting waiting times to assess some of the patient’s vital signs or functions and symptoms related to their conditions, with the aim of acquiring more data regarding the patient—which can be delivered to the clinician leveraging the EHR. Finally, the last cluster (B, two papers) presents solutions for acquiring clinical measurements or outcomes necessary for the following visit with clinical personnel, combining waiting time exploitation with clinical needs.
3.2.2. Types of Patients Addressed by Smart Waiting Rooms
The full reading steps of the review process enabled the identification of the target patients for which the smart waiting room solutions were considered. To investigate this aspect, the patients addressed in the papers were clustered based on their “type” (gender- or age-specific limitation) and their “condition” (the disease or impairment characterizing them). Table 3 summarizes the types of patients addressed by the solutions.

Table 3.
The patients addressed by each solution, ordered by year of publication.
Most of the papers addressed a general type of patient, i.e., the solutions described in such works are not dedicated to a specific portion of the population (11 papers). However, even if these solutions address a general patient, some of them tackle a specific health condition, impairment, or disability (four works). A total of 3 works are dedicated to women, for which a specific health condition is also detailed, while 1 paper is devoted to pediatric patients undergoing dental surgery, and 1 article addresses older adults.
3.2.3. Technologies Involved in the Surveyed Smart Waiting Rooms
To identify the technologies involved for each of the solutions portrayed in the included articles, we relied on the IEEE Thesaurus, which consists of a controlled vocabulary of engineering, scientific, and technical terms based on standards [36]. For each paper, the main technologies described to make a solution “smart” or “innovative” were identified and matched with the IEEE Thesaurus.
The results of the survey related to technologies are reported in Table 4.

Table 4.
The set of technologies adopted in each included work, presented according to the IEEE Thesaurus (with the boarder term/preceding the narrower term).
Interestingly, 7 papers relied on mobile applications for different purposes [21,23,25,31,33,34,35], while 3 works provided some sort of recommendation or decision process supported by AI [21,27,33], 3 works foresaw the adoption of patients’ EHRs [31,34,35], 3 papers relied on virtual reality applications in different ways [26,28,29,35], and a total of 3 articles adopted technologies to conduct biomedical measurements on patients [30,32,34]. It is also worth observing that IoT technologies are the core of only one work [20].
3.2.4. Clinically Applicative Contexts
To answer RQ4—the clinically applicative contexts for which the smart waiting rooms were developed—all included papers were thoroughly scrutinized to identify in which type of clinical facility (ER, hospital, primary care—such as general medic practice—specific clinical practice) they were deployed.
Table 5 summarizes the results of this screening.

Table 5.
The applicative contexts addressed by each solution, ordered by year of publication.
The majority of the smart waiting rooms are developed for specific clinical practices (7), followed by primary care practices (5). Outpatient hospital waiting rooms, laboratory waiting rooms, and ER waiting rooms are represented only in one work. Finally, one article does not address any specific applicative context [32].
4. Discussion
This section discusses the results presented in Section 3, taking into account the quantitative results and the contents investigated.
4.1. Late Attention towards Waiting Rooms
The works included in this systematic review are dated 2009 and later; although the starting year for the databases’ search was set at 2000—corresponding to the strengthening of research in the fields of IoT and Ambient Intelligence, with a focus also on smart homes—it is interesting to observe that the first relevant contribution is set almost a decade after the lower extreme of the time span. While a motivation could be identified in smart homes “driving” the application contexts for such technologies between 2009 and 2016 [37], other motivations could be that in the same period, the attention devoted to waiting rooms was mostly focused on psychological (e.g., effects of music on waiting patients [38], the role of educational materials [39], the relationship between perceived level of care and wait time [40]) and architectural aspects (e.g., how a waiting room should be designed [41], how to elicit design requirements based on emotions [42]). The fact that a limited number of articles was included may be indicative of the inherent difficulty of making a waiting room “smart”; generally, waiting rooms are environments used by different types of occupants (patients, family, caregivers, clinical personnel, etc.)—each characterized by their own needs. However, the results summarized in Figure 2 show that the number of significant papers increased between 2019 and 2023. Due to the recent COVID-19 pandemic and its consequences, the stress that healthcare facilities are subjected to underline the role (and potential) that waiting rooms could have in the clinical journey. It is no coincidence that the majority of the authors registered among review papers are from North America and Europe (Table 1), the continents presenting the most advanced healthcare systems; as highlighted in the Introduction, Western countries’ healthcare systems are facing the post-pandemic fallout [13,14,16].
4.2. Acting on the Waiting
Probably as a consequence of clogs to the Western countries’ healthcare systems, it is no surprise that the majority of the studies surveyed describe solutions devoted to enhancing one (or more) of the aspects related to waiting—whether it is reducing stress and anxiety, optimizing wait times, or providing educational materials (Table 2). More than half of the articles (56%) address cluster A, with stress-reduction systems [25,26,28,29], solutions somehow devoted to the optimization of patients’ flow within the healthcare structures [20,22,24,27], and patients’ education during the waiting [23,25]. Therefore, it would seem that the attention of researchers is focused on making the waiting time shorter or more productive from a patient’s perspective.
4.3. The Role of Smart Technologies in the Surveyed Solutions
In those solutions devoted to enhancing the waiting time, two technologies are identified (with the sole exception of [20]) (Table 4): all of the occurrences of simulation technologies and virtual reality technologies are registered for Cluster A solutions. While the first technologies are evidently dedicated to the reorganization of the waiting time and patient flow, extended reality technologies are used to soothe patients through their entertainment (as in [26,29]) or to enhance their knowledge of the healthcare facility and services [28]. As already noted in Section 3.2.3, there is a significant paucity of IoT technologies; only [20] explicitly refers to the adoption of IoT buses that patients can track to estimate their transfer to other clinics or hospitals. Other works may entail the adoption of an IoT framework; for instance, [30] leverages context data to assess whether or not a patient adhered to the instructions for blood pressure self-measurement, relying on sensors; in [22], the adoption of RFID active tags combined with EHRs could also imply the adoption of an IoT framework for tracking patients, personnel, and objects in a facility.
The absence of the IoT could be explained by the “simplicity” characterizing most of the solutions retrieved; very few authors became involved in the development of structured solutions requiring the data acquisition of patients or contexts via smart objects. The majority of the smart waiting rooms primarily relied on mobile applications to be used by patients via tablets and virtual technologies. This phenomenon could be motivated by the fact that these technologies have already undergone several technology acceptance studies [43,44,45,46]; thus, both users and researchers are more familiar with them.
For similar reasons, the scarcity of solutions relying on AI is evident: less than one third of the investigated articles rely on data-driven techniques. It is also interesting to observe that those works adopting AI [21,27,33] provide some sort of decision support via the assessment of PROs, taking into account their symptoms. However, none of these smart waiting rooms taps into the potential of EHRs, as this technology is used only as the “destination” for data acquired by the smart solutions [31,34,35]; instead of exploiting patients’ health condition summarized in EHRs to provide personalized solutions, EHRs are perceived as the virtual place to store data acquired via tablet applications or sensors.
Considering those works addressing clusters B and C (pre-visit data acquisition and patient’s diagnosis or assessment, respectively), the number of technology types involved presents two peaks—[32] for cluster C and [30] for cluster B. Doyle and colleagues [32] introduce a preliminary (not tested and not fully developed) general non-invasive way to acquire patient data that could potentially be used by clinicians, leveraging software and biomedical equipment for different tests and exams; by contrast, Wagner et al. [30] present a more solid framework enabling reliable blood pressure self-measurement (validated by target users). However, with the exceptions of these two peaks, the smart waiting room presented in the remaining articles mostly rely on tablet applications [21,31,33,34,35], in three cases combined with EHRs [31,34,35] and in just as many cases combined with biomedical equipment [30,32,34]. Again, the solutions are characterized by simplicity, i.e., they are devoted to performing—in most of the investigated cases—one single task without providing any personalization or tailored recommendation.
4.4. Smart Waiting Rooms Designed Not for All
By looking at the data reported in Table 3 and Table 5, it is clear that the smart waiting rooms retrieved are mostly devoted to specific patients (i.e., to patients belonging to a specific gender or characterized by a certain health condition) and designed for specific healthcare facilities. It could be argued that the smart environment paradigm—a physical space in which smart devices continuously work for occupants’ interests [2]—is overturned in that a patient can benefit from smart waiting room services if he/she presents some characteristics. While this phenomenon can be easily explained by research interests pertaining to the retrieved works, it is worth observing that in more than half of the selected works (nine articles), the patient can access the smart service only if he/she falls into a specific gender [23,28,30] or specific age [26,34] or if he/she is affected by a particular condition [25,31,33,35].
Therefore, the retrieved smart waiting rooms are hardly generalizable, in contrast with the efforts of “universal” smart homes capable of providing services to all types of users [47,48,49]. It might be concluded that smart waiting rooms are designed to answer specific patients’ needs and, thus, are not generalizable. However, it was underlined how the adoption of EHRs combined with IoT technologies can provide tailored services in smart environments [50,51,52]—so it is plausible that this could also be applied to smart waiting rooms.
4.5. Challenges and Research Directions for Smart Waiting Room
A few challenges and research directions can be identified in light of the findings elicited in this systematic literature review.
- The review results underlined the lack of generalizability of the smart waiting rooms surveyed; the majority of the solutions were designed for specific types of patients, thus hindering the adoption of such solutions on a larger scale. However, a few works also tackled exploiting EHRs; these data can be adopted to understand patients’ needs and provide them with tailored solutions—similar to what occurs in smart homes and environments [53,54,55]. Smart waiting rooms should, thus, be able to provide layered services—i.e., smart services for every waiter with the possibility of personalizing each of them in some regard according to the user’s specific needs. For example, the self-assessment of blood pressure relying on biomedical equipment and mobile applications should take into account the patient’s age and health condition (sight, cognitive abilities, and other information entailed by patient’s EHR) and their familiarity with technologies; for older patients or non-tech-savvy patients, the smart waiting room system should adapt the interface and provide a detailed tutorial regarding how to conduct a self-assessment using the equipment at hand. Similarly to [30], such a system should also be able to assess whether or not the patient was able to perform the required measurement in an appropriate way.
- Virtual reality is a powerful technology for stress relief in waiting rooms; however, this technology can also be exploited for diagnostic purposes and to acquire relevant insights regarding patients’ conditions. Virtual technologies are indeed known for the possibility of supporting the diagnosis and assessment of both cognitive and neurological conditions [56,57]. Smart waiting rooms should provide virtual technologies with the dual aim of reducing pre-intervention anxiety and stress while acquiring diagnostic data. This, combined with the possibility of leveraging EHRs, could enhance diagnostic processes and make wait times both more bearable and fruitful.
- It is striking that AI adoption in smart waiting rooms is limited to patients’ flow prediction or simulation, with only three works addressing decision support; wearable IoT technologies combined with AI can support the early diagnosis of several diseases and conditions (see, for example, [58,59,60]). The integration of non-invasive wearable monitoring technologies into smart waiting rooms is more than plausible, supporting the prompt identification of conditions that should be monitored and, ultimately, reducing the burden on healthcare structures.
- There is a relevant absence in the solutions reviewed; none of the works analyzed referred to the physical and built environment of the waiting room. However, researchers have spent a large amount of effort to identify the interactions and effects between the waiting room environment and waiters [38,42,61]. On the other hand, the design of waiting spaces (physical and environmental features) can completely change the healthcare experience. A significant challenge could be the integration between physical and digital IoT-enabled environments to meet one or more of the purposes identified by the three clusters (Section 3.2.1). Patients’ physical interactions with one or more components of the environment could be used for diagnostic and monitoring purposes, as well as for entertainment and relaxation purposes by stimulating the senses, enhancing psychological comfort, and physical activities.
- Emerging from the discussions in Section 4, smart waiting rooms should be characterized by a variety of technologies. Although the adoption of “safe and sound” technologies such as mobile applications makes the whole smart solution more acceptable, it hinders the “smartness” of the solution itself and its generalizability. More studies on adopting IoT technologies within smart waiting room environments should be conducted to investigate the acceptance of such technologies from both the patients’ and clinical personnel’s perspectives.
5. A proposal for a Smart Waiting Room
Considering the research directions described above, we propose a prototypical waiting room incorporating smart aspects (digital layer) and environmental features (physical layer). This smart waiting room aims to integrate the environment’s characteristics with digital services to enhance patients’ waiting while supporting the non-invasive diagnosis of specific conditions. This prototype leverages EHRs to identify patients and a novel AI- and VR-based system as a means to diagnose Mild Cognitive Impairment (MCI). The smart waiting room prototype is currently being developed within the framework of the research project “A novel public-private alliance to generate socioeconomic, biomedical and technological solutions for an inclusive Italian ageing society” (Age-IT), and its architecture is represented in Figure 3.
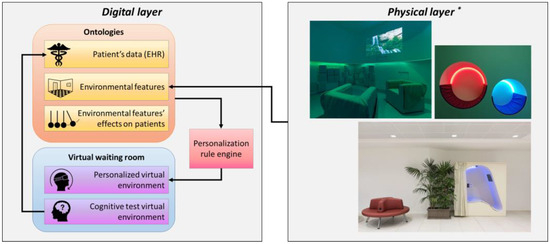
Figure 3.
The architecture for the Age-IT smart waiting room prototype, combining physical and digital aspects into one solution (* physical layer pictures are property of DU IIT srl).
The following details each component participating in the prototypical Age-IT smart waiting room.
5.1. Physical Layer
Many studies have investigated the impact of the environment on people’s healthcare experience. Healthcare design can promote patients’ and outpatients’ satisfaction and decrease staff stress and burnout (e.g., Urlich, 2019).
“Humanized environments” are defined as environments that respond to patients’ necessities and promote their well-being [62]. Older people are more likely to be suffering from chronic conditions and multi-morbidities, and their functional capacity is frequently limited. Environments should be customized to fit the specific and diverse needs of people, such as older people, people with cognitive diseases, and people with reduced mobility, to ensure that suitable access and facilities are provided for all users regardless of physical and mental condition. According to older people’s vulnerability, it is necessary to consider the presence of caregivers, who add up to the number of people who use the waiting spaces and represent another user typology with different characteristics.
For the outpatient journey, the waiting room experience is critical to forming a perception of quality of care and satisfaction [63]. In this context, the physical environment could be used to counteract the negative effects of waiting, which can be very challenging. The waiting room is often viewed as a space where people passively wait. On the contrary, studies have shown that individuals prefer being engaged in alternative activities instead of persevering and waiting. The experience of engaged time is entirely different from the time spent passively waiting [64]. The lack of activity while waiting allows an individual to pay more attention to the passage of time and increase one’s awareness of oneself [65]. In the outpatient department, people spend a great amount of time in waiting areas, affecting their stress, well-being, satisfaction, and perception of the quality of care. The physical environment affects both the processes of stress and coping [66], generated by the relation of the person with the environment. In other words, a positive environment represents a salutogenic source and can improve coping strategies. According to this idea, the physical environment has an impact on people’s health [67]. Enhancing the physical environment can be a successful strategy to improve the waiting experience for outpatients, caregivers, and, consequently, the staff. For this reason, waiting spaces should be considered in the healthcare design process as spaces with health-specific functions.
The user experience is not only related to anxiety and comfort; it is a holistic phenomenon influenced by ergonomic and affective dimensions [68] related to physical settings. It is well known that the physical environment affects human behaviors. In the outpatient department, the waiting experience influences behavioral responses and intentions, such as the willingness to recommend and return [68].
Evans and McCoy [67] define some architectural features which have a specific role in stress and, consequently, in people’s health:
- It is important to maintain a good balance in sensory stimulation, to not be overwhelmed with too many stimuli, and, on the contrary, to not cause boredom and sensory deprivation. As an example, noise and strong lights, such as crowded environments, activate people’s sensory stimulation and can produce stress.
- The coherence and the comprehension of spaces reduce the level of stress in people (both outpatients and staff).
- The affordances of spaces and components improve the user experience, affecting people’s behaviors.
- One of the most important elements affecting stress is the possibility of controlling aspects of the physical and social environment and customizing spaces (acting on light, indoor temperature, etc.). Privacy is another example of perception control, as it affects the ability to control social interactions.
These aspects are more related to psychological stress. Other features have a specific role in physical stress, such as microclimatic conditions, temperature, ventilation, and humidity.
According to these theories, many aspects can be considered in the design process to provide adequate and enhanced waiting spaces [69]:
Privacy/social interaction: Waiting spaces can be an opportunity to share experiences and emotions to promote relations between outpatients and caregivers. On the other hand, it will be important to use strategies to ensure privacy, such as not listening to private conversations (e.g., playing soft music or providing a TV).
Large spaces are perceived as crowded. On the contrary, small spaces are perceived as intimate. Large waiting areas should be broken down into smaller groups of seats to make the space less daunting and institutional and to enable patients to sit close to the suite to which they will be called [70]. Comfortable and grouped seats can promote spontaneous relations. On the other hand, seats should not be too close (to ensure privacy and to reduce infection diffusion), and possibly not along the corridors, to be adequate to the standard of privacy and comfort. At the same time, the provision of separate waiting areas may help to reduce cross-infection (especially after the COVID pandemic). Moreover, intimate spaces support both privacy and social interaction. For example, using circular-shaped furniture with high backs can create different and smaller seating areas with different orientations in a large waiting area, and the curves can promote free movement. Using perforated walls as filters between small waiting areas and the medical rooms can promote privacy but also reduce stress by providing a constant view of the access.
Safety and usability: According to the previous point, good visual contact is fundamental to not being stressed during the waiting time. Both for outpatients and caregivers, it is important to look at the staff to feel reassured and to call them if they need information or assistance. It is also necessary to support orientation, wayfinding, and navigation to ensure the autonomy to move freely and safely in the spaces, especially for vulnerable people.
Welcoming and familiar environment: The quality of the space (e.g., natural light, comfortable furniture, pleasant finishes) promotes a welcoming environment and can increase satisfaction and confidence in the healthcare facility. A familiar space can promote a sense of identity and belonging. As an example, the use of local and domestic furniture can enhance familiarity.
Well-being and distress: Environmental conditions (e.g., light, temperature) affect people’s wellbeing. Visual well-being is provided by natural light, by the quality and the difference in artificial lighting, and by avoiding glare effects, such as using flooring materials that reflect the light [71]. Acoustic well-being can be promoted by noise reduction, such as using soft floor coverings, curtains, and the acoustic treatment of walls and ceilings. Then, some features in the environment can promote positive distractions and the restoration process [72] to promote positive feelings and reduce the sense of isolation, anxiety, and depression, such as the use of nature (outdoor views, interior gardens or plants, representation of nature in pictures or paintings), the use of music or nature sounds (e.g., [73]), and the use of aromas, which can cover the smell of medicines and disinfectants [74]. As an example, there are studies on the benefit of the use of live music for people with stroke [75], cardiovascular disease [76], and insomnia [77], but there are no studies to understand the role of live music in the waiting rooms for outpatients [78]. Collins et al. [78] showed that both live and recorded music interventions in waiting rooms promote the reduction in outpatients’ perception of stress, anxiety, and pain and improve the waiting time.
Enriching the sensory input in an environment, such as through the therapeutic use of multisensory environments, has been found to achieve health and well-being outcomes in clinical settings [79]. The benefits of sensory spaces have been shown for mental health, psychiatric wards, people with dementia, people with autism spectrum disorder, people with traumatic brain injuries, the birthing environment, children, emergency departments, etc. In a waiting room, sensory stimulations can be provided by a dedicated sensory environment and sensory equipment in the main waiting area. For example, a sensory alcove can equilibrate the senses by controlled and customized sensory stimulation without completely abstracting from the waiting area.
Distractions such as playing can have an important role in enhancing waiting time. There are many examples of integrating playing activities in the design of the space in waiting areas for children, such as sensory and engaging installations, and immersive and interactive projections. These elements can also make people move and be engaged in physical activity, which is one of the most important strategies for health promotion.
Health promotion strategies for older adults generally focus on maintaining and increasing functional capacity, maintaining or improving self-care, and stimulating one’s social network [80].
Introducing media and technologies to promote movement, sensory experiences, and positive distractions can generate social interactions and facilitate relations, increase health information and education, and promote active and healthy aging in a proactive environment.
5.2. Digital Layer
The digital layer constitutes two sub-components: the first is devoted to the representation of a patient’s EHR and conditions in the form of domain ontologies, while the second is a set of virtual environments aimed at (a) reducing a patient’s stress during the waiting time and (b) assessing a patient’s cognitive status.
5.2.1. Ontologies for EHR and Personalization
Ontologies are shared and formal conceptualizations of a domain of knowledge [81]. They provide computable and Description Logic-based [82] representations of concepts and their relationships, enabling monotonic reasoning to infer new knowledge from the one modeled [83]. While ontologies are widely adopted in different domains (ranging from IoT devices to clinical applications), their reasoning capabilities are appreciated in decision-support systems—including clinical decision making [84,85]. Therefore, they are also adopted in the representation of a patient’s EHR [86,87]. The Age-IT digital layer relies on an EHR representation that comprises the patient’s information included in the Electronic Health File—which tracks down the clinical history of a patient [88]—with the addition of clinical information pertaining to the patient’s health condition modeled with the World Health Organization standards, International Classification of Functioning, Disability and Health (ICF) [89] and International Classification of Diseases (ICD) [90]. This approach has already been adopted in several knowledge-based systems [91], including some works related to the personalization of smart environments according to occupants’ desires and characteristics [48,92,93].
The result of such modeling consists of an ontology network capable of representing the patient’s clinical history, the set of diseases and conditions characterizing him/her, and the impairments and functional limitations that the patient may have acquired in his/her life. Moreover, the ontological layer is capable of storing data acquired from the cognitive test virtual environment (see Section 5.2.2) so that, in the case of a deterioration in the monitored cognitive functions, clinicians can update the patient’s health condition (in the EHR as well as adopting ICD- or ICF-related codes).
The ontologies are developed using the W3C-endorsed languages Resource Description Framework (RDF) [94] and Ontology Web Language (OWL) [95], while rules for the personalization of VR environments are formalized by adopting the Semantic Web Rule Language (SWRL) [96]. Data exchange between the ontological layer and the VR environments is performed via middleware (detailed in [97,98]).
This middleware is introduced to the system to enable the VR environment to communicate with the ontological layer, retrieve the user’s data from the ontology, and insert the results of the VR interactions back into the semantic layer. Considering the Open-World Assumption (OWA) of the monotonic nature of Description Logic (DL) [82], inserting new pieces of data into the ontology is not a trivial task. As a result, this work relies on a simple middleware program that allows the exchange of information between the VR environment and the ontology by generating and executing the proper SPARQL Protocol and RDF Query Language (SPARQL) [99].
For the VR environment to understand the user’s health condition and the proper game scenario, the middleware generates an SPARQL query SELECT to retrieve the user’s data from the ontology. The SPARQL query will then be executed on the DL reasoner to fetch the inferred data regarding the suitable VR game scenario based on the user’s health condition.
5.2.2. Virtual Environment for Cognitive Assessment
In line with the previously described challenges, the proposed smart waiting room can integrate smart technologies to support the assessment of cognitive functions. Through different tasks that can span from designed games to other activities, these smart waiting rooms can assess a range of cognitive functions, including memory, attention, visuospatial abilities, problem-solving, and decision-making skills. For instance, a memory assessment might involve pattern recognition games or recalling sequences of numbers or objects. At the same time, attention assessments could employ tasks that measure sustained attention, such as tracking moving objects amidst distractions.
Furthermore, collecting and processing patients’ digital biomarkers can enhance smart waiting rooms. Digital biomarkers can be defined as quantitative objective physiological and behavioral data obtained from a VR scenario that serve as indicators of normal biological processes, pathological processes, or responses to an exposure [100,101,102]. In the context of VR, digital biomarkers are predominantly addressed to head, hand, and gait movements in predictive AI models via machine learning (ML) techniques for earlier diagnosis in a variety of clinical conditions [103,104,105,106,107].
Specifically, the proposed smart waiting room aims to adopt AI as a predictive tool for assessing cognitive decline in Mild Cognitive Impairment (MCI). MCI represents a transitional stage between normal aging and more severe cognitive decline, such as Alzheimer’s disease or other forms of dementia. Preliminary studies on the kinematic analysis of elders showed the feasibility of tracking the head, hand, and gait during the performance, as indicators of MCI [108]. Hence, the integration of digital biomarker assessment within smart virtual waiting rooms can provide an effective approach to identifying and predicting cognitive changes, particularly in individuals with MCI [109].
Starting from this, the proposal plans to develop a smart virtual waiting room that can be used in hospitals or rehabilitative facilities with older adults to measure and assess several core cognitive functions that are compromised in elderly populations suffering from MCI. The smart waiting room is able to collect digital biomarkers connected to bodily movements (e.g., head, hands, and body), and these digital biomarkers are used to test different supervised ML models (i.e., support vector machines, decision tree, random forest, gradient boosting, logistic regression, k-nearest neighbors) to identify the best model to predict alterations in the core cognitive functions that are usually compromised in MCI [110]. Therefore, the proposed smart virtual waiting room collects digital biomarkers connected to three primary core dimensions that can effectively be deployed in a virtual reality environment: spatial orientation, attention, and memory [111]. The smart virtual waiting room is considered for a head-mounted display (HMD), and its architecture is similar to a real waiting room, including typical furniture and objects: chairs, windows, plants, waste bins, tables, desks, etc. [102].
The cognitive assessment task consists of four phases:
- Familiarization: In this phase, the user familiarizes her/himself with the VR scenario (e.g., looking around and observing all the objects) and VR equipment use (e.g., use of the controllers, movements in the virtual environment, selecting the items). Simultaneously, users receive straightforward instructions on the key actions they must perform in subsequent phases and are prompted to rehearse them. For example, to select objects in the scenario, the user physically approaches the object, and when the hand is in proximity to the object, the object lights up. To select it, the user must click the button in the controller.
- Encoding: In this phase, the user must memorize the location of four objects. The objects are presented one at a time, and each is presented four times for 12 searches. The user is asked to search for each object within the waiting room by physically reaching for it. Once the subject’s hands are near the object, the object will light up, and the user can pick it up by clicking on the controller button. The four objects are randomized in the four presentations, and the objects always appear in the same position (e.g., object 1 is always on the coffee table, object 2 is always next to the plant).
- Forgetting: in this phase, the user spends 10 min outside the virtual waiting room with the aim of generating oblivion.
- Recall: In this phase, the user, adhering to the instructions, must reposition the objects they found during the encoding phase to their original positions, exactly as they were initially discovered. The user starts the task in the middle of the room, and an object appears in front of him/her. Therefore, the user is instructed to bring the object to the original location when presented during the encoding phase. Once positioned, a second object appears in front of him/her, which must be positioned like the previous one. The total duration of the cognitive assessment in the virtual waiting room, including the four phases, is approximately 30–35 min.
During the four phases, a large amount of data will be gathered, including cognitive performance information (position of correct and incorrect objects, total and latency times, and the distance from the correct original position) and digital biomarker information, including head, hand, and body movements. These large amounts of data will subsequently be elaborated by AI tools, and specifically, machine learning (ML) techniques will be used to discriminate healthy elderly subjects and MCI subjects and to identify the best and the most optimal features for an earlier MCI detection [105,106,107].
5.3. Use Cases
Two use cases are introduced to exemplify the features characterizing the proposed smart waiting room. Two different personas, identified following the methodology described in [112], are introduced to illustrate the services provided within the smart waiting room.
Patient with cardiovascular and anxiety condition: Vincent is a 68-year-old man who lives autonomously and suffers from coronary heart disease (ICD-10 code I2510), which is characterized by heart arrhythmia and hypertension. In the past two months, he has started suffering from panic disorders (with symptoms such as hot flashes, rapid heart rate, shortness of breath, and dizziness). He is currently under medication for his heart-related conditions, and he is visiting a cardiologist for a check-up. Vincent’s health condition is described in his EHR using the ICF codes related to the Comprehensive ICF Core Set for Chronic Ischemic Heart Disease [113] (e.g., b410 “Heart function”, b4200—“Increased blood pressure”, and b460 “Sensations associated with cardiovascular and respiratory functions”) with the addition of ICF codes to represent his anxiety-related conditions (e.g., b152 “Emotional functions”, b440 “Respiratory functions”, and d2401 “Handling stress”). At the time of his reservation, Vincent was indicated to show up in the waiting room 30 min before the time of his appointment to check in and to wear the HMD set available in the waiting room; in this case, the patient has a dedicated lodge separated from other waiters. The smart waiting room system, acknowledging Vincent’s presence after the check-in, assesses his health conditions and infers the VR features to load. Therefore, taking into account that the patient is characterized by anxiety and panic disorders (which can ultimately impact his cardiovascular condition), the inferred features of the VR environment are aimed at reducing his anxiety while waiting for his visit. The inferred features of the VR environment consist in reproducing a multisensory environment with customized scenarios through Vincent’s interaction with the technological system. In the scenarios, different sensory stimulations are integrated, such as colors and controlled lights, a video and sounds of nature, tactile vibration, and aromas, which can promote a state of calm and positive distraction during the waiting time. Moreover, considering Vincent’s specific health issues and his waiting inside a private lodge, indoor comfort metrics (humidity rate, temperature, and CO2 concentration) are monitored—since these metrics are known to affect people with respiratory and cardiovascular issues. Therefore, in the ontological layer, the proper thresholds for each comfort metric are modeled (indoor temperature between 19 and 22 during winter and between 23 and 26 in summer; humidity rate set at 50% [114,115,116]), while inside the waiting room lodge, a thermohygrometric sensor captures data every 5 min. Each time one of the comfort metrics exceeds the thresholds, the ontological layer triggers the proper actuation (activating the HVAC system).
In this way, after 30 min, Vincent is ready to be visited by the cardiologist.
Patient with MCI: Sandra is a 71-year-old woman who, in the past 18 months, reported to her family doctor suffering from short-term memory loss, difficulties in spatial abilities (orientation), and attention difficulties, causing, for example, difficulty in following a conversation. Sandra was diagnosed with MCI, and her doctor noted these changes in her EHR. The patient is visiting a neuropsychologist for a check-up on her memory-related impairments. Sandra is chaperoned by her daughter; in the waiting room, Sandra has been instructed to wear an HMD (with the help of her daughter if necessary). Acknowledging her health condition via Sandra’s EHR, the smart waiting room system administers the VR environment for cognitive assessment, with the aim of acquiring further data to be ultimately delivered to the neuropsychologist. Since this is the third time Sandra visits her neuropsychologist, the clinician can leverage historical data regarding patient interactions with the smart waiting room system. Data acquired via the smart waiting room are assessed by the neuropsychologist, who can use them to evaluate whether Sandra’s short-term memory is deteriorating any further or not.
5.4. Relevance of the Use Cases
The two personas were selected because they represent significant examples of the Italian and European populations.
Cardiovascular diseases are responsible for 44% of deaths in Italy [117] and for 32.7% of deaths in the European Union [118]. Moreover, patients surviving a cardiovascular disease become chronic patients, requiring continuous care—constituting a relevant outlay in healthcare costs; in 2019, the European Society of Cardiology calculated that the overall expenditure for cardiovascular diseases in the European Union was EUR 210 billion per year [119]. Medications for these conditions account for 23% of Italy’s pharmaceutical expenditure.
While no data are available for the economic impact of MCI, there are several estimations of the costs related to this disease’s evolution. Cimler et al. [120] estimated that the EU will spend up to EUR 222 billion in 2030 to treat Alzheimer’s disease in its mildest form. This condition affects more than 10 million people in Europe, which is expected to increase in the following decades.
Both chronic cardiovascular diseases and cognitive decline have become more and more prevalent with the population’s ageing; Western countries are characterized by longer life expectancies, which translates into older citizens [121]. This ageing process brings challenges, among which the increasing amount of chronic health conditions is one of the most relevant and impactful on the national healthcare systems.
For these reasons, as mentioned above, smart systems are perceived as promising solutions to tackle some of the age-related issues, and the prompt identification and management of chronic conditions can contribute to enhancing older adults’ quality of life and limiting healthcare expenditure.
6. Challenges and Limitations of the Age-IT Smart Waiting Room
The proposed Age-IT smart waiting room revolves around a set of technologies that, although widely discussed in the scientific literature, is still settling from market and legislative perspectives. Therefore, as with many IoT-based solutions, the prototype has some implementation challenges and limitations.
From a digital point of view, the solution relies on semantic representations to personalize VR environment content and—prospectively—indoor comfort metrics. The representations include the EHR, a well-known way to report patients’ clinical information. However, the implementation of this framework in hospitals is far from complete; some “classic” barriers still persist (e.g., appropriate training for both clinical and administrative personnel; the lack of a standardized way to represent EHRs in Europe, which ultimately results in limited interoperability; technical, logistic, manufacturing challenges related to the adoption and use of an EHR technology) [122] and are inherited by Age-IT. However, it is worth observing that the Italian Electronic Health File already encompasses all the necessary information related to the Patient Summary and Electronic Prescriptions—recommended by the European Committee in 2008—and, therefore, Age-IT’s EHR already complies with the European norm [123].
Nonetheless, Age-IT deals with patients’ data and leverages personal and sensitive information. Therefore, the proposed smart waiting room is subject to data security issues for IoT and digital solutions [124]. The inherent interconnection between devices and the adoption of health-related data poses a security concern, as sensitive information may be hijacked from weak nodes or other types of attacks [125]. As a consequence, privacy concerns may arise at different levels (patients, caregivers, and clinical levels). Some patients may only want some nodes of the smart waiting room to be aware of their personal information and health condition rather than granting free access to all intelligent or smart devices deployed in a waiting room.
These IoT challenges are being actively addressed by several researchers worldwide, with international laws and standards being issued every year since 2019. In particular, the European Union is developing the ePrivacy Regulation, focusing on data protection and enabling the secure electronic communication of information in IoT systems [126].
Another set of challenges characterizing IoT (and, more in general, monitoring) devices is related to personal privacy. Researchers have already underlined the concerns afflicting dwellers in smart homes; intimacy and privacy are perceived as essential in AAL domestic solutions [127,128], independently from a person’s age and gender [47]. Although Age-IT does not actively monitor the patient, it acquires—and, possibly, modifies—her/his EHR when necessary, raising similar concerns of loss of control. Age-IT adopts a “less-invasive” approach [92] when adapting its solutions to specific patients, allowing the monitoring of the environment surrounding the patient and intervening in that.
Nevertheless, any smart waiting room requires a rethink of the role of personal data in the context of digital health, and it also needs to take into account elderlies and those citizens who do not want to share their personal and health data in a digital form. Protecting the confidentiality of data, granting patients’ anonymity when necessary, allowing them to withdraw access to their data, and ensuring data security throughout the healthcare systems are fundamental (and well-known) ethical issues permeating the adoption of IoT in healthcare, including AAL solutions [129].
To conclude, it is necessary to note that novel (potentially disruptive) smart technologies require significant investments. Even for Age-IT, the costs play a pivotal role. As underlined in different studies, national health systems are currently re-targeting their activities to face the long-term consequences of the pandemic. After the COVID-19 pandemic, public healthcare systems are now facing a two-year backlog in delayed essential care and are also having to cope with fewer clinicians available [16,130]. It is plausible to assume that, in the next few years, financial resources will be mostly dedicated to putting national healthcare systems “back on track” before investing in disruptive technology on national levels.
7. Conclusions and Future Works
This paper introduces a novel smart waiting room framework integrating the physical environment’s features and digital aspects into a novel prototype. Considering the limited adoption of IoT, AI-based, and virtual technologies in this type of environment, the smart waiting room can help to effectively tackle some of the issues characterizing patients’ waiting time, the patient burdens of hospitals and practices, and the necessity of acquiring more data regarding patients’ health conditions.
To this aim, this work investigates existing solutions in Ambient Intelligence and smart environments, identifying some possible research challenges. These challenges drive the development of the proposed smart waiting room prototype, capable of adapting some of its features to patients’ needs, and considering their needs and health conditions while leveraging contextual (physical and virtual) features to administer anxiety relief or diagnostic actions. The Age-IT prototype uses AI-based solutions—for both diagnostic and personalization activities—and leverages a set of novel technologies (VR, IoT sensors, etc.) to modify a patient’s context, thus modifying his/her waiting room experience. Moreover, since the prototypical smart waiting room leverages knowledge bases and semantic reasoning to manage facts about the patients and the environment, the framework can be extended to all types of patients (and health conditions), thus making it generalizable.
As an IoT and digital prototype of a smart waiting room, Age-IT needs to tackle the implementation issues discussed in this paper and the ethical concerns. Therefore, future works foresee the investigation of the most suitable solutions to tackle data security and privacy concerns, taking into account the European framework and initiatives as a reference. The next steps in the development of Age-IT include deploying the solution in a real environment to simulate a real waiting room. This will pave the way for tests with people to acquire users’ feedback (in terms of the solution’s usability, willingness to adopt Age-IT, and perceived usefulness, as well as investigating the modifications in the perceived waiting time). Moreover, an on-site deployment will also accelerate the identification of technical solutions for some implementation challenges, enabling a phase of fine-tuning of the digital layer. Finally, the interactions between the physical and the digital layers (and patients experiencing the two waiting conditions) will be investigated.
In conclusion, the proposed smart waiting room represents a first step towards a paradigm shift in healthcare, transforming mundane waiting times into purposeful diagnostic and therapeutic activities. Beyond mere entertainment, these rooms harness the power of technology to evaluate cognitive functions accurately, offering a proactive approach to healthcare by detecting potential cognitive issues early and enabling personalized interventions. Moreover, the IoT and AI are adopted to ensure the patient’s best comfort while reducing monitoring discomfort. As technology evolves, these smart waiting rooms will undoubtedly play an increasingly integral role in healthcare, revolutionizing how patient care is approached.
Author Contributions
Conceptualization, D.S., M.M., D.D.L., E.B. and N.S.; methodology, D.S., M.M. and M.S.; software, D.S., A.M. and S.D.G.; investigation, D.S.; resources, M.S., G.R. and N.S.; data curation, D.S.; writing—original draft preparation, D.S., M.M., A.M., I.A.C.-G. and E.B.; writing—review and editing, D.S., M.M., A.M., I.A.C.-G. and E.B.; visualization, D.S.; supervision, D.S.; project administration, D.S., D.D.L. and E.B.; funding acquisition, M.S., G.R. and N.S. All authors have read and agreed to the published version of the manuscript.
Funding
This work has been co-funded by the European Union—Next Generation EU under Project: “A novel public-private alliance to generate socioeconomic, biomedical and technological solutions for an inclusive Italian ageing society” (Age-IT), CUP: B83C22004800006.
Data Availability Statement
Data is contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Alaa, M.; Zaidan, A.A.; Zaidan, B.B.; Talal, M.; Kiah, M.L.M. A Review of Smart Home Applications Based on Internet of Things. J. Netw. Comput. Appl. 2017, 97, 48–65. [Google Scholar] [CrossRef]
- Hutton, D.M. Smart Environments: Technology, Protocols and Applications. Kybernetes 2005, 34, 903–904. [Google Scholar] [CrossRef]
- Solaimani, S.; Bouwman, H.; Baken, N. The Smart Home Landscape: A Qualitative Meta-Analysis. In Proceedings of the toward Useful Services for Elderly and People with Disabilities—9th International Conference on Smart Homes and Health Telematics, ICOST 2011, Montreal, QC, Canada, 20–22 June 2011; pp. 192–199. [Google Scholar]
- Liu, P.; Li, G.; Jiang, S.; Liu, Y.; Leng, M.; Zhao, J.; Wang, S.; Meng, X.; Shang, B.; Chen, L.; et al. The Effect of Smart Homes on Older Adults with Chronic Conditions: A Systematic Review and Meta-Analysis. Geriatr. Nurs. 2019, 40, 522–530. [Google Scholar] [CrossRef] [PubMed]
- McIlvennie, C.; Sanguinetti, A.; Pritoni, M. Of Impacts, Agents, and Functions: An Interdisciplinary Meta-Review of Smart Home Energy Management Systems Research. Energy Res. Soc. Sci. 2020, 68, 101555. [Google Scholar] [CrossRef]
- Thompson, D.A.; Yarnold, P.R.; Williams, D.R.; Adams, S.L. Effects of Actual Waiting Time, Perceived Waiting Time, Information Delivery, and Expressive Quality on Patient Satisfaction in the Emergency Department. Ann. Emerg. Med. 1996, 28, 657–665. [Google Scholar] [CrossRef]
- Camacho, F.; Anderson, R.; Safrit, A.; Jones, A.S.; Hoffmann, P. The Relationship between Patient’s Perceived Waiting Time and Office-Based Practice Satisfaction. N. Carol. Med. J. 2006, 67, 409–413. [Google Scholar] [CrossRef]
- Bleustein, C.; Rothschild, D.B.; Valen, A.; Valatis, E.; Schweitzer, L.; Jones, R. Wait Times, Patient Satisfaction Scores, and the Perception of Care. Am. J. Manag. Care 2014, 20, 393–400. [Google Scholar]
- Reichert, A.; Jacobs, R. The Impact of Waiting Time on Patient Outcomes: Evidence from Early Intervention in Psychosis Services in England. Health Econ. 2018, 27, 1772–1787. [Google Scholar] [CrossRef]
- Mowen, J.C.; Licata, J.W.; McPhail, J. Waiting in the Emergency Room: How to Improve Patient Satisfaction. J. Health Care Mark. 1993, 13, 26–33. [Google Scholar]
- Arneill, A.B.; Devlin, A.S. Perceived quality of Care: The influence of the waiting room environment. J. Environ. Psychol. 2002, 22, 345–360. [Google Scholar] [CrossRef]
- Naiker, U.; FitzGerald, G.; Dulhunty, J.M.; Rosemann, M. Time to Wait: A Systematic Review of Strategies that Affect out-Patient Waiting Times. Aust. Health Rev. 2018, 42, 286. [Google Scholar] [CrossRef]
- Fernández-Aguilar, C.; Casado-Aranda, L.-A.; Farrés Fernández, M.; Minué Lorenzo, S. Has COVID-19 Changed the Workload for Primary Care Physicians? The Case of Spain. Fam. Pract. 2021, 38, 780–785. [Google Scholar] [CrossRef]
- Katz, G.M.; Bach, K.; Bobos, P.; Cheung, A.; Décary, S.; Goulding, S.; Herridge, M.S.; McNaughton, C.D.; Palmer, K.S.; Razak, F.A.; et al. Understanding How Post–COVID-19 Condition Affects Adults and Health Care Systems. JAMA Health Forum 2023, 4, e231933. [Google Scholar] [CrossRef]
- KFF Health Tracking Poll—May 2020. Available online: https://www.kff.org/report-section/kff-health-tracking-poll-may-2020-health-and-economic-impacts/ (accessed on 12 December 2023).
- Macdonald, N.; Clements, C.; Sobti, A.; Rossiter, D.; Unnithan, A.; Bosanquet, N. The Building Backlog of NHS Elective Cases Post COVID-19. Br. J. Surg. 2020, 107, e377–e378. [Google Scholar] [CrossRef] [PubMed]
- Thomas, E.E.; Haydon, H.M.; Mehrotra, A.; Caffery, L.J.; Snoswell, C.L.; Banbury, A.; Smith, A.C. Building on the Momentum: Sustaining Telehealth beyond COVID-19. J. Telemed. Telecare 2022, 28, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Biddiss, E.; Knibbe, T.J.; McPherson, A. The Effectiveness of Interventions Aimed at Reducing Anxiety in Health Care Waiting Spaces. Anesth. Analg. 2014, 119, 433–448. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Mtonga, K.; Kumaran, S.; Mikeka, C.; Jayavel, K.; Nsenga, J. Machine Learning-Based Patient Load Prediction and IoT Integrated Intelligent Patient Transfer Systems. Future Internet 2019, 11, 236. [Google Scholar] [CrossRef]
- Miller, S.; Gilbert, S.; Virani, V.; Wicks, P. Patients’ Utilization and Perception of an Artificial Intelligence–Based Symptom Assessment and Advice Technology in a British Primary Care Waiting Room: Exploratory Pilot Study. JMIR Hum. Factors 2020, 7, e19713. [Google Scholar] [CrossRef]
- Lin, Y.-C.; Padman, R. Process Visibility Analysis in Ambulatory Care: A Simulation Study with RFID Data. Stud. Health Technol. Inform. 2013, 192, 768–772. [Google Scholar]
- Gilliam, M.L.; Martins, S.L.; Bartlett, E.; Mistretta, S.Q.; Holl, J.L. Development and Testing of an IOS Waiting Room “App” for Contraceptive Counseling in a Title X Family Planning Clinic. Am. J. Obstet. Gynecol. 2014, 211, 481.e1–481.e8. [Google Scholar] [CrossRef] [PubMed]
- Hossain, N.U.I.; Jaradat, R.M.; Khasawneh, M.T. Reducing Patient Waiting Time in an Outpatient Clinic: A Discrete Event Simulation (DES) Based Approach. In Proceedings of the 2017 Industrial and Systems Engineering Conference, Pittsburgh, PA, USA, 20–23 May 2017. [Google Scholar]
- Bao, T.; Deng, G.; DeMarzo, L.A.; Zhi, W.I.; DeRito, J.L.; Blinder, V.; Chen, C.; Li, Q.S.; Green, J.; Pendleton, E.; et al. A Technology-Assisted, Brief Mind-Body Intervention to Improve the Waiting Room Experience for Chemotherapy Patients: Randomized Quality Improvement Study. JMIR Cancer 2019, 5, e13217. [Google Scholar] [CrossRef] [PubMed]
- Al-Nerabieah, Z.; Alhalabi, M.-N.; Owayda, A.; Alsabek, L.; Bshara, N.; Kouchaji, C. Effectiveness of Using Virtual Reality Eyeglasses in the Waiting Room on Preoperative Anxiety: A Randomized Controlled Trial. Perioper. Care Oper. Room Manag. 2020, 21, 100129. [Google Scholar] [CrossRef]
- Ehrler, F.; Rochat, J.; Siebert, J.N.; Guessous, I.; Lovis, C.; Spechbach, H. Use of a Semiautomatic Text Message System to Improve Satisfaction with Wait Time in the Adult Emergency Department: Cross-Sectional Survey Study. JMIR Med. Inform. 2022, 10, e34488. [Google Scholar] [CrossRef]
- Reinders, I.M.A.; Cremers, G.R.; van Rooijen, S.J.; Leemans, J.C.; Perquin, C.W.; Geomini, P.M.A.J.; Maas, J.W.M.; Bongers, M.Y. The Effect of an Informative 360-Degree Virtual Reality Video on Anxiety for Women Visiting the One-Stop Clinic for Abnormal Uterine Bleeding: A Randomized Controlled Trial (VISION-Trial). Eur. J. Obstet. Gynecol. Reprod. Biol. 2022, 272, 96–103. [Google Scholar] [CrossRef]
- Liu, B.; Wang, W.; Zhang, Y.; Huang, R.; Raiti, J. Lullaland: A Multisensory Virtual Reality Experience to Reduce Stress. In Proceedings of the Extended Abstracts of the 2023 CHI Conference on Human Factors in Computing Systems, Hamburg, Germany, 23–28 April 2023; ACM: New York, NY, USA, 2023; pp. 1–6. [Google Scholar]
- Wagner, S.; Kamper, C.H.; Rasmussen, N.H.; Ahrendt, P.; Toftegaard, T.S.; Bertelsen, O.W. Reliable Blood Pressure Self-Measurement in the Obstetric Waiting Room. Methods Inf. Med. 2014, 53, 225–234. [Google Scholar] [CrossRef]
- Desai, S.; Stevens, E.; Emani, S.; Meyers, P.; Iversen, M.; Solomon, D.H. Improving Quality of Care in Rheumatoid Arthritis Through Mobile Patient-Reported Outcome Measurement: Focus Group Study. JMIR Form. Res. 2020, 4, e15158. [Google Scholar] [CrossRef]
- Doyle, T.E.; Kalsi, M.; Aiyush, B.; Yousuf, J.; Waseem, O. Non-Invasive Health Monitoring System (NIHMS). In Proceedings of the 2009 IEEE Toronto International Conference Science and Technology for Humanity (TIC-STH), Toronto, ON, Canada, 26–27 September 2009; pp. 703–707. [Google Scholar]
- Grant, R.W.; Lyles, C.; Uratsu, C.S.; Vo, M.T.; Bayliss, E.A.; Heisler, M. Visit Planning Using a Waiting Room Health IT Tool: The Aligning Patients and Providers Randomized Controlled Trial. Ann. Fam. Med. 2019, 17, 141–149. [Google Scholar] [CrossRef]
- Giskes, K.; Lowres, N.; Orchard, J.; Li, J.; McKenzie, K.; Hespe, C.M.; Freedman, B. Increasing Screening for Atrial Fibrillation in General Practice: The Atrial Fibrillation Self-Screening, Management and guideline-Recommended Therapy (AF Self-SMART) Study. Med. J. Aust. 2023, 218, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Alberts, J.L.; Shuaib, U.; Fernandez, H.; Walter, B.L.; Schindler, D.; Miller Koop, M.; Rosenfeldt, A.B. The Parkinson’s Disease Waiting Room of the Future: Measurements, Not Magazines. Front. Neurol. 2023, 14, 1212113. [Google Scholar] [CrossRef]
- IEEE. IEEE Thesaurus (July 2023). Available online: https://www.ieee.org/content/dam/ieee-org/ieee/web/org/pubs/ieee-thesaurus.pdf (accessed on 12 December 2023).
- Risteska Stojkoska, B.L.; Trivodaliev, K.V. A Review of Internet of Things for Smart Home: Challenges and Solutions. J. Clean. Prod. 2017, 140, 1454–1464. [Google Scholar] [CrossRef]
- Lai, J.C.-Y.; Amaladoss, N. Music in Waiting Rooms: A Literature Review. HERD Health Environ. Res. Des. J. 2022, 15, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Cass, S.J.; Ball, L.E.; Leveritt, M.D. Passive Interventions in Primary Healthcare Waiting Rooms Are Effective in Promoting Healthy Lifestyle Behaviours: An Integrative Review. Aust. J. Prim. Health 2016, 22, 198. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, D.; Chow, C.K. Waiting Time as an Indicator for Health Services Under Strain: A Narrative Review. INQUIRY J. Health Care Organ. Provis. Financ. 2020, 57, 004695802091030. [Google Scholar] [CrossRef]
- Bishop, P. Surveying “The Waiting Room”. Archit. Theory Rev. 2013, 18, 135–149. [Google Scholar] [CrossRef]
- Keirnan, A.; Murphy, A.; Pedell, S.; Marcello, F. Exploring Emotions for Technology and Service Design in Health Care Setting Waiting Rooms. In Proceedings of the 28th Australian Conference on Computer-Human Interaction—OzCHI ’16, Launceston, TAS, Australia, 29 November–2 December 2016; ACM Press: New York, NY, USA, 2016; pp. 348–352. [Google Scholar]
- Garavand, A.; Samadbeik, M.; Kafashi, M.; Abhari, S. Acceptance of Health Information Technologies, Acceptance of Mobile Health: A Review Article. J. Biomed. Phys. Eng. 2017, 7, 403–408. [Google Scholar] [PubMed]
- Nadal, C.; Sas, C.; Doherty, G. Technology Acceptance in Mobile Health: Scoping Review of Definitions, Models, and Measurement. J. Med. Internet Res. 2020, 22, e17256. [Google Scholar] [CrossRef] [PubMed]
- Roberts, A.R.; De Schutter, B.; Franks, K.; Radina, M.E. Older Adults’ Experiences with Audiovisual Virtual Reality: Perceived Usefulness and Other Factors Influencing Technology Acceptance. Clin. Gerontol. 2019, 42, 27–33. [Google Scholar] [CrossRef]
- Mahalil, I.; Yusof, A.M.; Ibrahim, N. A Literature Review on the Usage of Technology Acceptance Model for Analysing a Virtual Reality’s Cycling Sport Applications with Enhanced Realism Fidelity. In Proceedings of the 2020 8th International Conference on Information Technology and Multimedia (ICIMU), Selangor, Malaysia, 24–25 August 2020; pp. 237–242. [Google Scholar]
- Wilson, C.; Hargreaves, T.; Hauxwell-Baldwin, R. Smart Homes and Their Users: A Systematic Analysis and Key Challenges. Pers. Ubiquitous Comput. 2015, 19, 463–476. [Google Scholar] [CrossRef]
- Spoladore, D.; Arlati, S.; Colombo, V.; Modoni, G.; Sacco, M. A Semantic-Enabled Smart Home for AAL and Continuity of Care. In Studies in Computational Intelligence; Springer: Berlin/Heidelberg, Germany, 2021; Volume 933. [Google Scholar]
- Tanabe, S.; Saitoh, E.; Koyama, S.; Kiyono, K.; Tatemoto, T.; Kumazawa, N.; Kagaya, H.; Otaka, Y.; Mukaino, M.; Tsuzuki, A.; et al. Designing a Robotic Smart Home for Everyone, Especially the Elderly and People with Disabilities. Fujita Med. J. 2019, 5, 31–35. [Google Scholar] [CrossRef]
- Dafferianto Trinugroto, Y.B.; Reichert, F.; Fensli, R.W. A SOA-Based Health Service Platform in Smart Home Environment. In Proceedings of the 2011 IEEE 13th International Conference on e-Health Networking, Applications and Services, Columbia, MO, USA, 13–15 June 2011; pp. 201–204. [Google Scholar]
- Knaup, P.; Schöpe, L. Using Data from Ambient Assisted Living and Smart Homes in Electronic Health Records. Methods Inf. Med. 2014, 53, 149–151. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.M.S.; Halooq, A.; Dening, J.; Uddin, R.; Laranjo, L.; Chow, C.K.; Maddison, R. Healthcare Providers’ Perspectives on Using Smart Home Systems to Improve Self-Management and Care in People with Heart Failure: A Qualitative Study. Int. J. Med. Inform. 2022, 167, 104837. [Google Scholar] [CrossRef] [PubMed]
- Baldassini, D.; Colombo, V.; Spoladore, D.; Sacco, M.; Arlati, S. Customization of Domestic Environment and Physical Training Supported by Virtual Reality and Semantic Technologies: A Use-Case. In Proceedings of the RTSI 2017—IEEE 3rd International Forum on Research and Technologies for Society and Industry, Modena, Italy, 11–13 September 2017. [Google Scholar]
- Spoladore, D.; Mahroo, A.; Trombetta, A.; Sacco, M. Comfont: A Semantic Framework for Indoor Comfort and Energy Saving in Smart Homes. Electronics 2019, 8, 1449. [Google Scholar] [CrossRef]
- Nolich, M.; Spoladore, D.; Carciotti, S.; Buqi, R.; Sacco, M. Cabin as a Home: A Novel Comfort Optimization Framework for IoT Equipped Smart Environments and Applications on Cruise Ships. Sensors 2019, 19, 1060. [Google Scholar] [CrossRef]
- Tsirlin, I.; Dupierrix, E.; Chokron, S.; Coquillart, S.; Ohlmann, T. Uses of Virtual Reality for Diagnosis, Rehabilitation and Study of Unilateral Spatial Neglect: Review and Analysis. CyberPsychology Behav. 2009, 12, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Tan, W.; Chen, C.; Liu, C.; Yang, J.; Zhang, Y. A Review of the Application of Virtual Reality Technology in the Diagnosis and Treatment of Cognitive Impairment. Front. Aging Neurosci. 2019, 11, 280. [Google Scholar] [CrossRef] [PubMed]
- Muthu, B.; Sivaparthipan, C.B.; Manogaran, G.; Sundarasekar, R.; Kadry, S.; Shanthini, A.; Dasel, A. IOT Based Wearable Sensor for Diseases Prediction and Symptom Analysis in Healthcare Sector. Peer Peer Netw. Appl. 2020, 13, 2123–2134. [Google Scholar] [CrossRef]
- Pavitra, B.; Singh, D.N.; Sharma, S.K. Predictive and Interactive IOT Diagnosis System with AI and ML Tools: Review. In Advances in Computational Intelligence and Informatics; Springer: Berlin/Heidelberg, Germany, 2020; pp. 9–16. [Google Scholar]
- Awotunde, J.B.; Folorunso, S.O.; Bhoi, A.K.; Adebayo, P.O.; Ijaz, M.F. Disease Diagnosis System for IoT-Based Wearable Body Sensors with Machine Learning Algorithm. In Hybrid Artificial Intelligence and IoT in Healthcare; Springer: Berlin/Heidelberg, Germany, 2021; pp. 201–222. [Google Scholar]
- Halpern, N.A. Innovative Designs for the Smart ICU. Chest 2014, 145, 646–658. [Google Scholar] [CrossRef]
- Fornara, F.; Bonaiuto, M.; Bonnes, M. Perceived Hospital Environment Quality Indicators: A Study of Orthopaedic Units. J. Environ. Psychol. 2006, 26, 321–334. [Google Scholar] [CrossRef]
- Becker, F.; Sweeney, B.; Parsons, K. Ambulatory Facility Design and Patients’ Perceptions of Healthcare Quality. HERD Health Environ. Res. Des. J. 2008, 1, 35–54. [Google Scholar] [CrossRef]
- Ehret, S.; Trukenbrod, A.K.; Thomaschke, R. Dynamics of Temporal Experience in Active and Passive Waiting Situations. Appl. Cogn. Psychol. 2021, 35, 900–908. [Google Scholar] [CrossRef]
- Jokic, T.; Zakay, D.; Wittmann, M. Individual Differences in Self-Rated Impulsivity Modulate the Estimation of Time in a Real Waiting Situation. Timing Time Percept. 2018, 6, 71–89. [Google Scholar] [CrossRef]
- Cohen, S.; Evans, G.W.; Stokols, D.; Krantz, D.S. Behavior, Health, and Environmental Stress; Springer: Boston, MA, USA, 1986; ISBN 978-1-4757-9382-6. [Google Scholar]
- Evans, G.W.; McCoy, J.M. When Buildings Don’t Work: The Role of Architecture In Human Health. J. Environ. Psychol. 1998, 18, 85–94. [Google Scholar] [CrossRef]
- Juliá-Nehme, B.; Yoon, S.-Y.; Cumsille, P.; Rodríguez, E. Assessing Spatial User Experience for Design Guidelines: A Comparative Study of Outpatient Waiting Rooms with Conventional versus Modern Features. HERD Health Environ. Res. Des. J. 2023, 16, 83–103. [Google Scholar] [CrossRef] [PubMed]
- Del Nord, R.; Peretti, G. L’umanizzazione Degli Spazi Cura; 2012; Available online: https://www.dors.it/documentazione/testo/201904/Umanizzazione_degli_spazi_di_cura_LG.pdf (accessed on 12 December 2023).
- National Health Service—England. Health Building Note 11-01: Facilities for Primary and Community Care Services; National Health Service: London, UK, 2013.
- Arakawa Martins, B.; Barrie, H.; Visvanathan, R.; Daniel, L.; Martins, L.A.; Ranasinghe, D.; Wilson, A.; Soebarto, V. A Multidisciplinary Exploratory Approach for Investigating the Experience of Older Adults Attending Hospital Services. HERD Health Environ. Res. Des. J. 2021, 14, 141–163. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R.S.; Simons, R.F.; Losito, B.D.; Fiorito, E.; Miles, M.A.; Zelson, M. Stress Recovery during Exposure to Natural and Urban Environments. J. Environ. Psychol. 1991, 11, 201–230. [Google Scholar] [CrossRef]
- Pouyesh, V.; Amaniyan, S.; Haji Mohammad Hoseini, M.; Bashiri, Y.; Sieloff, C.; Griffiths, P.; Vaismoradi, M. The Effects of Environmental Factors in Waiting Rooms on Anxiety among Patients Undergoing Coronary Angiography: A Randomized Controlled Trial. Int. J. Nurs. Pract. 2018, 24, 12682. [Google Scholar] [CrossRef]
- Dijkstra, K.; Pieterse, M.; Pruyn, A. Physical Environmental Stimuli That Turn Healthcare Facilities into Healing Environments through Psychologically Mediated Effects: Systematic Review. J. Adv. Nurs. 2006, 56, 166–181. [Google Scholar] [CrossRef]
- Sarkamo, T.; Tervaniemi, M.; Laitinen, S.; Forsblom, A.; Soinila, S.; Mikkonen, M.; Autti, T.; Silvennoinen, H.M.; Erkkila, J.; Laine, M.; et al. Music Listening Enhances Cognitive Recovery and Mood after Middle Cerebral Artery Stroke. Brain 2008, 131, 866–876. [Google Scholar] [CrossRef]
- Selle, E.W.; Silverman, M.J. A Randomized Feasibility Study on the Effects of Music Therapy in the Form of Patient-Preferred Live Music on Mood and Pain in Patients on a Cardiovascular Unit. Arts Health 2017, 9, 213–223. [Google Scholar] [CrossRef]
- Jespersen, K.V.; Koenig, J.; Jennum, P.; Vuust, P. Music for Insomnia in Adults. Cochrane Database Syst. Rev. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- Collins, M.; Fitzpatrick, K.; Kiernan, A.M.; Moss, H.; Harmon, D. Pilot Study on Music in the Waiting Room of Outpatient Pain Clinics. Pain Manag. Nurs. 2022, 23, 318–323. [Google Scholar] [CrossRef]
- Cavanagh, B.; Haracz, K.; Lawry, M.; James, C. Receptive Arts Engagement for Health: A Holistic and Trans-Disciplinary Approach to Creating a Multisensory Environment. Sage Open 2020, 10, 215824402097842. [Google Scholar] [CrossRef]
- Golinowska, S.; Groot, W.; Baji, P.; Pavlova, M. Health Promotion Targeting Older People. BMC Health Serv. Res. 2016, 16, 345. [Google Scholar] [CrossRef] [PubMed]
- Gruber, T.R. A Translation Approach to Portable Ontology Specifications. Knowl. Acquis. 1993, 5, 199–220. [Google Scholar] [CrossRef]
- Baader, F.; Horrocks, I.; Sattler, U. Description Logics as Ontology Languages for the Semantic Web. In Mechanizing Mathematical Reasoning; Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics); Springer: Berlin/Heidelberg, Germany, 2005. [Google Scholar] [CrossRef]
- Bienvenu, M.; Leclère, M.; Mugnier, M.-L.; Rousset, M.-C. Reasoning with Ontologies. In A Guided Tour of Artificial Intelligence Research; Springer: Cham, Switzerland, 2020; pp. 185–215. [Google Scholar]
- Shoaip, N.; El-Sappagh, S.; Barakat, S.; Elmogy, M. Reasoning Methodologies in Clinical Decision Support Systems: A Literature Review. In U-Healthcare Monitoring Systems; Elsevier: Amsterdam, The Netherlands, 2019; pp. 61–87. [Google Scholar]
- Dissanayake, P.I.; Colicchio, T.K.; Cimino, J.J. Using Clinical Reasoning Ontologies to Make Smarter Clinical Decision Support Systems: A Systematic Review and Data Synthesis. J. Am. Med. Inform. Assoc. 2020, 27, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Legaz-García, M.d.C.; Martínez-Costa, C.; Menárguez-Tortosa, M.; Fernández-Breis, J.T. A Semantic Web Based Framework for the Interoperability and Exploitation of Clinical Models and EHR Data. Knowl.-Based Syst. 2016, 105, 175–189. [Google Scholar] [CrossRef]
- Adel, E.; El-Sappagh, S.; Barakat, S.; Elmogy, M. Ontology-Based Electronic Health Record Semantic Interoperability: A Survey. In U-Healthcare Monitoring Systems; Elsevier: Amsterdam, The Netherlands, 2019; pp. 315–352. [Google Scholar]
- Agenzia per l’Italia Digitale Digital Healthcare System. Available online: https://www.agid.gov.it/en/piattaforme/digital-healthcare-system (accessed on 12 December 2023).
- Stucki, G.; Cieza, A.; Ewert, T.; Kostanjsek, N.; Chatterji, S.; Üstün, T.B. Application of the International Classification of Functioning, Disability and Health (ICF) in Clinical Practice. Disabil. Rehabil. 2002, 24, 281–282. [Google Scholar] [CrossRef]
- DiSantostefano, J. International Classification of Diseases 10th Revision (ICD-10). J. Nurse Pract. 2009, 5, 56–57. [Google Scholar] [CrossRef]
- Spoladore, D.; Sacco, M.; Trombetta, A. A Review of Domain Ontologies for Disability Representation. Expert. Syst. Appl. 2023, 228, 120467. [Google Scholar] [CrossRef]
- Spoladore, D.; Mondellini, M.; Sacco, M.; Spoladore, D.; Trombetta, A. An Ontology-Based Framework for a Less Invasive Domestic Management System (LIDoMS). In Proceedings of the 2020 16th International Conference on Intelligent Environments, Madrid, Spain, 20–23 July 2020. IE 2020. [Google Scholar]
- Spoladore, D.; Arlati, S.; Carciotti, S.; Nolich, M.; Sacco, M. RoomFort: An Ontology-Based Comfort Management Application for Hotels. Electronics 2018, 7, 345. [Google Scholar] [CrossRef]
- Pan, J.Z. Resource Description Framework. In Handbook on Ontologies; Springer: Berlin/Heidelberg, Germany, 2009; pp. 71–90. [Google Scholar]
- Antoniou, G.; Harmelen, F. van Web Ontology Language: OWL. In Handbook on Ontologies; Springer: Berlin/Heidelberg, Germany, 2009. [Google Scholar]
- Horrocks, I.; Patel-Schneider, P.F.; Boley, H.; Tabet, S.; Grosof, B.; Dean, M. SWRL: A Semantic Web Rule Language Combining OWL and RuleML. W3C Memb. Submiss. 2004, 21, 1–31. [Google Scholar]
- Barsocchi, P.; Ferro, E.; La Rosa, D.; Mahroo, A.; Spoladore, D. E-Cabin: A Software Architecture for Passenger Comfort and Cruise Ship Management. Sensors 2019, 19, 4978. [Google Scholar] [CrossRef] [PubMed]
- Spoladore, D.; Mahroo, A.; Trombetta, A.; Sacco, M. DOMUS: A Domestic Ontology Managed Ubiquitous System. J. Ambient. Intell. Humaniz. Comput. 2022, 13, 3037–3052. [Google Scholar] [CrossRef]
- Hommeaux, E.P.; Seaborne, A. SPARQL Query Language for RDF. W3C Recommendation. 2008. Available online: http://www.w3.org/TR/rdf-sparql-query/ (accessed on 12 December 2023).
- U.S. Food & Drug Administration. Patient-Focused Drug Development: Collecting Comprehensive and Representative Input. 2020. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-focused-drug-development-collecting-comprehensive-and-representative-input (accessed on 12 December 2023).
- Piau, A.; Wild, K.; Mattek, N.; Kaye, J. Current State of Digital Biomarker Technologies for Real-Life, Home-Based Monitoring of Cognitive Function for Mild Cognitive Impairment to Mild Alzheimer Disease and Implications for Clinical Care: Systematic Review. J. Med. Internet Res. 2019, 21, e12785. [Google Scholar] [CrossRef]
- Vasudevan, S.; Saha, A.; Tarver, M.E.; Patel, B. Digital Biomarkers: Convergence of Digital Health Technologies and Biomarkers. NPJ Digit. Med. 2022, 5, 36. [Google Scholar] [CrossRef]
- Cavedoni, S.; Chirico, A.; Pedroli, E.; Cipresso, P.; Riva, G. Digital Biomarkers for the Early Detection of Mild Cognitive Impairment: Artificial Intelligence Meets Virtual Reality. Front. Hum. Neurosci. 2020, 14, 245. [Google Scholar] [CrossRef]
- Ding, Z.; Lee, T.; Chan, A.S. Digital Cognitive Biomarker for Mild Cognitive Impairments and Dementia: A Systematic Review. J. Clin. Med. 2022, 11, 4191. [Google Scholar] [CrossRef]
- Ansart, M.; Epelbaum, S.; Bassignana, G.; Bône, A.; Bottani, S.; Cattai, T.; Couronné, R.; Faouzi, J.; Koval, I.; Louis, M.; et al. Predicting the Progression of Mild Cognitive Impairment Using Machine Learning: A Systematic, Quantitative and Critical Review. Med. Image Anal. 2021, 67, 101848. [Google Scholar] [CrossRef]
- Tsai, C.-F.; Chen, C.-C.; Wu, E.H.-K.; Chung, C.-R.; Huang, C.-Y.; Tsai, P.-Y.; Yeh, S.-C. A Machine-Learning-Based Assessment Method for Early-Stage Neurocognitive Impairment by an Immersive Virtual Supermarket. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 2124–2132. [Google Scholar] [CrossRef]
- Wang, S.; Yin, H.; Li, G.; Jia, Y.; Leng, M.; Meng, Q.; Wang, C.; Chen, L. Detection of Mild Cognitive Impairment Based on Virtual Reality: A Scoping Review. Curr. Alzheimer Res. 2020, 17, 126–140. [Google Scholar] [CrossRef] [PubMed]
- de los Reyes-Guzmán, A.; Dimbwadyo-Terrer, I.; Trincado-Alonso, F.; Monasterio-Huelin, F.; Torricelli, D.; Gil-Agudo, A. Quantitative Assessment Based on Kinematic Measures of Functional Impairments during Upper Extremity Movements: A Review. Clin. Biomech. 2014, 29, 719–727. [Google Scholar] [CrossRef]
- Cooper, C.; Li, R.; Lyketsos, C.; Livingston, G. Treatment for Mild Cognitive Impairment: Systematic Review. Br. J. Psychiatry 2013, 203, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.; Zhu, H. Hyper-Parameter Optimization: A Review of Algorithms and Applications. arXiv 2020, arXiv:2003.05689. [Google Scholar]
- Castegnaro, A.; Howett, D.; Li, A.; Harding, E.; Chan, D.; Burgess, N.; King, J. Assessing Mild Cognitive Impairment Using Object-Location Memory in Immersive Virtual Environments. Hippocampus 2022, 32, 660–678. [Google Scholar] [CrossRef] [PubMed]
- Adlin, T.; Pruitt, J. The Essential Persona Lifecycle: Your Guide to Building and Using Personas; Elsevier: Amsterdam, The Netherlands, 2010; ISBN 9780123814180. [Google Scholar]
- Cieza, A.; Stucki, A.; Geyh, S.; Berteanu, M.; Quittan, M.; Simon, A.; Kostanjsek, N.; Stucki, G.; Walsh, N. ICF Core Sets for Chronic Ischaemic Heart Disease. J. Rehabil. Med. 2004, 36, 94–99. [Google Scholar] [CrossRef]
- Jung, C.-C.; Hsia, Y.-F.; Hsu, N.-Y.; Wang, Y.-C.; Su, H.-J. Cumulative Effect of Indoor Temperature on Cardiovascular Disease–Related Emergency Department Visits among Older Adults in Taiwan. Sci. Total Environ. 2020, 731, 138958. [Google Scholar] [CrossRef]
- Higuma, T.; Yoneyama, K.; Nakai, M.; Kaihara, T.; Sumita, Y.; Watanabe, M.; Doi, S.; Miyamoto, Y.; Yasuda, S.; Ishibashi, Y.; et al. Effects of Temperature and Humidity on Acute Myocardial Infarction Hospitalization in a Super-Aging Society. Sci. Rep. 2021, 11, 22832. [Google Scholar] [CrossRef]
- Janssen, H.; Ford, K.; Gascoyne, B.; Hill, R.; Roberts, M.; Bellis, M.A.; Azam, S. Cold Indoor Temperatures and Their Association with Health and Well-Being: A Systematic Literature Review. Public Health 2023, 224, 185–194. [Google Scholar] [CrossRef]
- Istituto Superiore di Sanità Malattie Cardiovascolari—Online. Available online: https://www.epicentro.iss.it/cardiovascolare/ (accessed on 10 January 2024).
- Eurostat Cardiovascular Diseases Statistics—Online. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=cardiovascular_diseases_statistics (accessed on 10 January 2024).
- Timmis, A.; Townsend, N.; Gale, C.P.; Torbica, A.; Lettino, M.; Petersen, S.E.; Mossialos, E.A.; Maggioni, A.P.; Kazakiewicz, D.; May, H.T.; et al. European Society of Cardiology: Cardiovascular Disease Statistics 2019. Eur. Heart J. 2020, 41, 12–85. [Google Scholar] [CrossRef]
- Cimler, R.; Maresova, P.; Kuhnova, J.; Kuca, K. Predictions of Alzheimer’s Disease Treatment and Care Costs in European Countries. PLoS ONE 2019, 14, e0210958. [Google Scholar] [CrossRef]
- Christensen, K.; Doblhammer, G.; Rau, R.; Vaupel, J.W. Ageing Populations: The Challenges Ahead. Lancet 2009, 374, 1196–1208. [Google Scholar] [CrossRef] [PubMed]
- Bonacina, S.; Marceglia, S.; Pinciroli, F. Barriers Against Adoption of Electronic Health Record in Italy. J. Healthc. Eng. 2011, 2, 509–526. [Google Scholar] [CrossRef]
- Nalin, M.; Baroni, I.; Faiella, G.; Romano, M.; Matrisciano, F.; Gelenbe, E.; Martinez, D.M.; Dumortier, J.; Natsiavas, P.; Votis, K.; et al. The European Cross-Border Health Data Exchange Roadmap: Case Study in the Italian Setting. J. Biomed. Inform. 2019, 94, 103183. [Google Scholar] [CrossRef]
- Rouhani, S.; Deters, R. Security, Performance, and Applications of Smart Contracts: A Systematic Survey. IEEE Access 2019, 7, 50759–50779. [Google Scholar] [CrossRef]
- Tawalbeh, L.; Muheidat, F.; Tawalbeh, M.; Quwaider, M. IoT Privacy and Security: Challenges and Solutions. Appl. Sci. 2020, 10, 4102. [Google Scholar] [CrossRef]
- Grafenstein, M.; Heumüller, J.; Belgacem, E.; Jakobi, T.; Smiesko, P. Effective Regulation through Design—Aligning the EPrivacy Regulation with the EU General Data Protection Regulation (GDPR): Tracking Technologies in Personalised Internet Content and the Data Protection by Design Approach. SSRN Electron. J. 2021. [Google Scholar] [CrossRef]
- Demiris, G.; Hensel, B.K.; Skubic, M.; Rantz, M. Senior Residents’ Perceived Need of and Preferences for “Smart Home” Sensor Technologies. Int. J. Technol. Assess. Health Care 2008, 24, 120–124. [Google Scholar] [CrossRef]
- Balta-Ozkan, N.; Davidson, R.; Bicket, M.; Whitmarsh, L. Social Barriers to the Adoption of Smart Homes. Energy Policy 2013, 63, 363–374. [Google Scholar] [CrossRef]
- Zakerabasali, S.; Ayyoubzadeh, S.M. Internet of Things and Healthcare System: A Systematic Review of Ethical Issues. Health Sci. Rep. 2022, 5, e863. [Google Scholar] [CrossRef]
- van Ginneken, E.; Reed, S.; Siciliani, L.; Eriksen, A.; Schlepper, L.; Tille, F.; Zapata, T. Addressing Backlogs and Managing Waiting Lists during and beyond the COVID-19 Pandemic; European Observatory on Health Systems and Policies: Brussels, Belgium, 2022.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).