Sugar-Sweetened Coffee Intake and Blood Glucose Management in Korean Patients with Diabetes Mellitus
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Demographic Information
2.3. Dietary Intake and SSC Consumption
2.4. Anthropometric Measurements and Health Indicators
2.5. Definition of Glycemic Target Achievement for DM
2.6. Statistical Analysis
3. Results
3.1. General Characteristics of the Participants According to the Frequency of SSC Consumption
3.2. Total Energy and Macronutrients Intake According to the Frequency of SSC Consumption
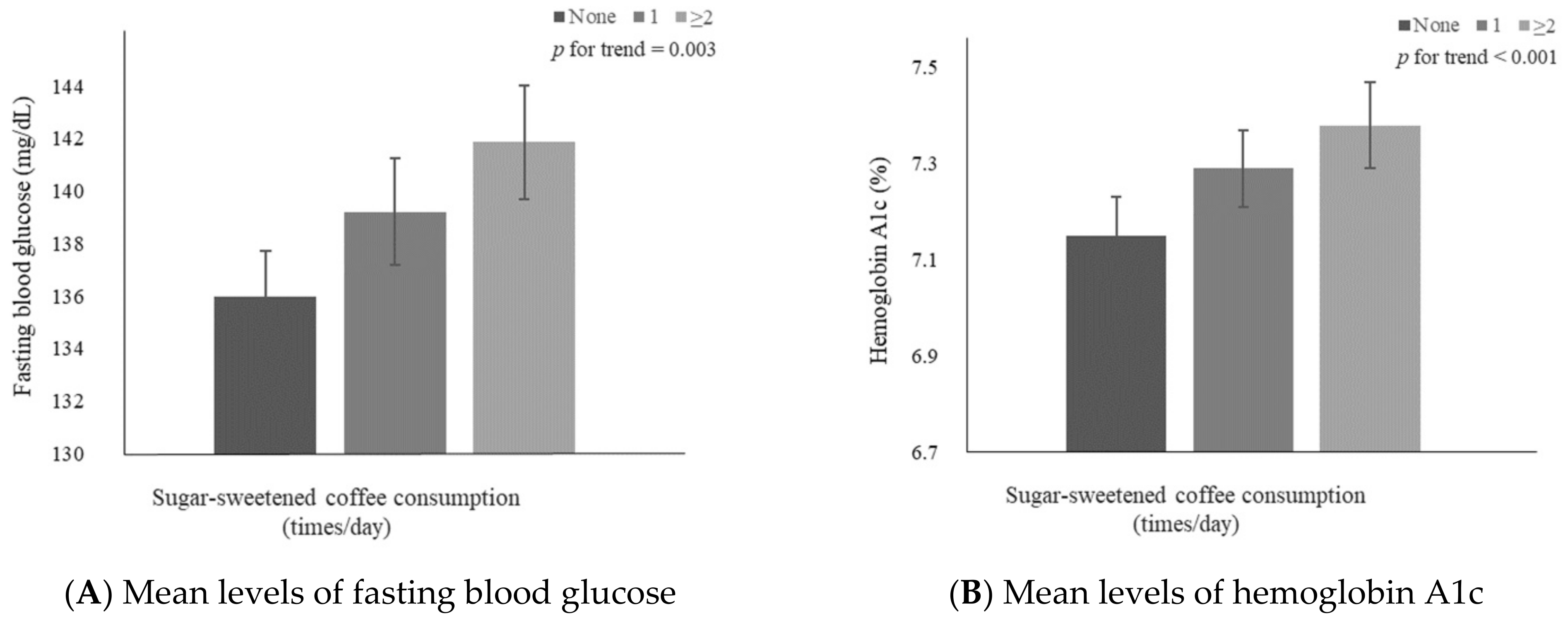
3.3. Mean FBG and HbA1c Levels According to the Frequency of SSC Consumption
3.4. Glycemic Target Levels Achieved by Participants with DM
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.N.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 2022, 183, 109119. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare, Korea Disease Control and Prevention Agency. Korea Health Statistics 2020: Korea National Health and Nutrition Examination Survey (KNHANES VIII-2). Available online: https://knhanes.kdca.go.kr/knhanes/sub04/sub04_04_01.do (accessed on 17 November 2022).
- Statistics Korea. Cause of Death Statistics in 2020. Available online: https://www.kostat.go.kr/portal/korea/kor_nw/1/6/2/index.board?bmode=read&bSeq=&aSeq=403046&pageNo=1&rowNum=10&navCount=10&currPg=&searchInfo=&sTarget=title&sTxt= (accessed on 17 November 2022).
- Lee, H.-S.; Kwon, S.-o.; Yon, M.; Kim, D.; Lee, J.-Y.; Nam, J.; Park, S.-j.; Yeon, J.-y.; Lee, S.-k.; Lee, H.-y.; et al. Dietary total sugar intake of Koreans: Based on the Korea National Health and Nutrition Examination Survey (KNHANES), 2008–2011. J. Nutr. Health 2014, 47, 268–276. [Google Scholar] [CrossRef]
- Malik, V.S.; Popkin, B.M.; Bray, G.A.; Després, J.P.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: A meta-analysis. Diabetes Care 2010, 33, 2477–2483. [Google Scholar] [CrossRef]
- Lim, H.; Lee, H.J.; Choue, R.; Wang, Y. Trends in Fast-Food and Sugar-Sweetened Beverage Consumption and Their Association with Social Environmental Status in South Korea. J. Acad. Nutr. Diet. 2018, 118, 1228–1236.e1221. [Google Scholar] [CrossRef] [PubMed]
- Korea Health Industry Development Institute. National Food & Nutrition Statistics in 2020: High frequency foods. Available online: https://www.khidi.or.kr/kps/dhraStat/result15?menuId=MENU01669&year=2020 (accessed on 17 November 2022).
- Korea Health Industry Development Institute. National Food & Nutrition Statistics in 2019: High frequency foods. Available online: https://www.khidi.or.kr/kps/dhraStat/result15?menuId=MENU01669&year=2019 (accessed on 17 November 2022).
- International Coffee Organization. World Coffee Consumption. Available online: https://www.ico.org/trade_statistics.asp?section=Statistics (accessed on 17 November 2022).
- Kim, H.; Kim, Y.J.; Lim, Y.; Kwon, O. Association of coffee consumption with health-related quality of life and metabolic syndrome in Korean adults: Based on 2013~2016 Korea National Health and Nutrition Examination Survey. J. Nutr. Health 2018, 51, 538–555. [Google Scholar] [CrossRef]
- Bhupathiraju, S.N.; Pan, A.; Manson, J.E.; Willett, W.C.; van Dam, R.M.; Hu, F.B. Changes in coffee intake and subsequent risk of type 2 diabetes: Three large cohorts of US men and women. Diabetologia 2014, 57, 1346–1354. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.M. Coffee consumption and risk of type 2 diabetes mellitus in Asians: A meta-epidemiological study of population-based cohort studies. World J. Diabetes 2021, 12, 908–915. [Google Scholar] [CrossRef] [PubMed]
- Kweon, S.; Kim, Y.; Jang, M.-j.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.-H.; Oh, K. Data Resource Profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef]
- Korea Disease Control and Prevention Agency. The Eighth Korea National Health and Nutrition Examination Survey (KNHANES VIII-2) 2020. Available online: https://knhanes.kdca.go.kr/knhanes/sub03/sub03_02_05.do (accessed on 17 November 2022).
- Ainsworth, B.E.; Haskell, W.L.; Leon, A.S.; Jacobs, D.R., Jr.; Montoye, H.J.; Sallis, J.F.; Paffenbarger, R.S., Jr. Compendium of physical activities: Classification of energy costs of human physical activities. Med. Sci. Sports Exerc. 1993, 25, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare, Korean Nutrition Society. 2020 Dietary Reference Intakes for Koreans; Ministry of Health and Welfare and Korean Nutrition Society: Sejong, Republic of Korea, 2020. Available online: http://www.kns.or.kr/FileRoom/FileRoom_view.asp?mode=mod&restring=%252FFileRoom%252FFileRoom.asp%253Fxsearch%253D0%253D%253Dxrow%253D10%253D%253DBoardID%253DKdr%253D%253Dpage%253D1&idx=108&page=1&BoardID=Kdr&xsearch=1&cn_search= (accessed on 17 November 2022).
- Korea Disease Control and Prevention Agency. The Eighth Korea National Health and Nutrition Survey Guide (KNHANES VIII-2). 2020. Available online: https://knhanes.kdca.go.kr/knhanes/sub04/sub04_02_02.do?classType=4 (accessed on 17 November 2022).
- Korean Diabetes Association. Clinical Practice Guidelines for Diabetes, 7th ed.; Korean Diabetes Association: Seoul, Republic of Korea, 2021. [Google Scholar]
- Korean Diabetes Association. Treatment Guideline for Diabetes, 6th ed.; Korean Diabetes Association: Seoul, Republic of Korea, 2019. [Google Scholar]
- Korean Diabetes Association. Treatment Guideline for Diabetes, 5th ed.; Korean Diabetes Association: Seoul, Republic of Korea, 2015. [Google Scholar]
- Elnour, M.A.A.; Saleh, A.A.; Kalantan, M.M.; Mirghani, H.O. The relationship between coffee intake, obstructive sleep apnea risk, and type 2 diabetes glycemic control, in Tabuk City, The Kingdom of Saudi Arabia: A case-control study. BMC Res. Notes 2019, 12, 798. [Google Scholar] [CrossRef] [PubMed]
- Komorita, Y.; Iwase, M.; Fujii, H.; Ohkuma, T.; Ide, H.; Jodai-Kitamura, T.; Yoshinari, M.; Oku, Y.; Higashi, T.; Nakamura, U.; et al. Additive effects of green tea and coffee on all-cause mortality in patients with type 2 diabetes mellitus: The Fukuoka Diabetes Registry. BMJ Open Diabetes Res. Care 2020, 8, e001252. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.W.; Woo, H.D.; Cho, M.J.; Park, J.K.; Kim, S.S. Identification of Dietary Patterns Associated with Incidence of Hyperglycemia in Middle-Aged and Older Korean Adults. Nutrients 2019, 11, 1801. [Google Scholar] [CrossRef] [PubMed]
- Ding, M.; Satija, A.; Bhupathiraju, S.N.; Hu, Y.; Sun, Q.; Han, J.; Lopez-Garcia, E.; Willett, W.; van Dam, R.M.; Hu, F.B. Association of Coffee Consumption With Total and Cause-Specific Mortality in 3 Large Prospective Cohorts. Circulation 2015, 132, 2305–2315. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.J.; Jeon, H.J.; Park, S.; Kim, S.A.; Lim, K.; Chung, S.; Chang, P.S.; Lee, J.K.; Kang, D.; Shin, S. Association of Coffee Consumption and Its Types According to Addition of Sugar and Creamer with Metabolic Syndrome Incidence in a Korean Population from the Health Examinees (HEXA) Study. Nutrients 2021, 13, 920. [Google Scholar] [CrossRef]
- Kennedy-Martin, T.; Boye, K.S.; Kennedy-Martin, M. The Association Between Body Mass Index and Glycemic Control in Patients with Type 2 Diabetes Across Eight Countries: A Literature Review. Curr. Res. Diabetes Obes. J. 2021, 15, 1–6. [Google Scholar]
- Martinell, M.; Pingel, R.; Hallqvist, J.; Dorkhan, M.; Groop, L.; Rosengren, A.; Storm, P.; Stålhammar, J. Education, immigration and income as risk factors for hemoglobin A1c >70 mmol/mol when diagnosed with type 2 diabetes or latent autoimmune diabetes in adult: A population-based cohort study. BMJ Open Diabetes Res. Care 2017, 5, e000346. [Google Scholar] [CrossRef]
- Fanelli, S.M.; Kelly, O.J.; Krok-Schoen, J.L.; Taylor, C.A. Low Protein Intakes and Poor Diet Quality Associate with Functional Limitations in US Adults with Diabetes: A 2005–2016 NHANES Analysis. Nutrients 2021, 13, 2582. [Google Scholar] [CrossRef]
- Pfeiffer, A.F.H.; Pedersen, E.; Schwab, U.; Risérus, U.; Aas, A.M.; Uusitupa, M.; Thanopoulou, A.; Kendall, C.; Sievenpiper, J.L.; Kahleová, H.; et al. The Effects of Different Quantities and Qualities of Protein Intake in People with Diabetes Mellitus. Nutrients 2020, 12, 365. [Google Scholar] [CrossRef]
- Khazrai, Y.M.; Defeudis, G.; Pozzilli, P. Effect of diet on type 2 diabetes mellitus: A review. Diabetes Metab. Res. Rev. 2014, 30 (Suppl. 1), 24–33. [Google Scholar] [CrossRef]
- Leenders, M.; Verdijk, L.B.; van der Hoeven, L.; Adam, J.J.; van Kranenburg, J.; Nilwik, R.; van Loon, L.J. Patients with type 2 diabetes show a greater decline in muscle mass, muscle strength, and functional capacity with aging. J. Am. Med. Dir. Assoc. 2013, 14, 585–592. [Google Scholar] [CrossRef]
- Yamaoka, T.; Araki, A.; Tamura, Y.; Tanaka, S.; Fujihara, K.; Horikawa, C.; Aida, R.; Kamada, C.; Yoshimura, Y.; Moriya, T.; et al. Association between Low Protein Intake and Mortality in Patients with Type 2 Diabetes. Nutrients 2020, 12, 1629. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.; Lee, J.E.; Loftfield, E.; Shu, X.O.; Abe, S.K.; Rahman, M.S.; Saito, E.; Islam, M.R.; Tsugane, S.; Sawada, N.; et al. Coffee and tea consumption and mortality from all causes, cardiovascular disease and cancer: A pooled analysis of prospective studies from the Asia Cohort Consortium. Int. J. Epidemiol. 2022, 51, 626–640. [Google Scholar] [CrossRef]
- Shahinfar, H.; Jayedi, A.; Khan, T.A.; Shab-Bidar, S. Coffee consumption and cardiovascular diseases and mortality in patients with type 2 diabetes: A systematic review and dose-response meta-analysis of cohort studies. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2526–2538. [Google Scholar] [CrossRef]
- Lee, J.; Kim, H.Y.; Kim, J. Coffee Consumption and the Risk of Obesity in Korean Women. Nutrients 2017, 9, 1340. [Google Scholar] [CrossRef]
- Kim, J.H.; Park, Y.S. Light coffee consumption is protective against sarcopenia, but frequent coffee consumption is associated with obesity in Korean adults. Nutr. Res. 2017, 41, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Cho, S.; Jacobs, D.R., Jr.; Park, K. Instant coffee consumption may be associated with higher risk of metabolic syndrome in Korean adults. Diabetes Res. Clin. Pract. 2014, 106, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.H.; Tan, L.; Hiramatsu, N.; Ishisaka, A.; Alfonso, H.; Tanaka, A.; Uemura, N.; Fujiwara, Y.; Takechi, R. Plasma concentrations of coffee polyphenols and plasma biomarkers of diabetes risk in healthy Japanese women. Nutr. Diabetes 2016, 6, e212. [Google Scholar] [CrossRef]
- Johnston, K.L.; Clifford, M.N.; Morgan, L.M. Coffee acutely modifies gastrointestinal hormone secretion and glucose tolerance in humans: Glycemic effects of chlorogenic acid and caffeine. Am. J. Clin. Nutr. 2003, 78, 728–733. [Google Scholar] [CrossRef]
- Whitehead, N.; White, H. Systematic review of randomised controlled trials of the effects of caffeine or caffeinated drinks on blood glucose concentrations and insulin sensitivity in people with diabetes mellitus. J. Hum. Nutr. Diet. 2013, 26, 111–125. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Xue, W.; Liang, S.; Zhao, J.; Zhang, X. Acute caffeine ingestion reduces insulin sensitivity in healthy subjects: A systematic review and meta-analysis. Nutr. J. 2016, 15, 103. [Google Scholar] [CrossRef]
- Keijzers, G.B.; De Galan, B.E.; Tack, C.J.; Smits, P. Caffeine can decrease insulin sensitivity in humans. Diabetes Care 2002, 25, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Thong, F.S.; Graham, T.E. Caffeine-induced impairment of glucose tolerance is abolished by beta-adrenergic receptor blockade in humans. J. Appl. Physiol. (1985) 2002, 92, 2347–2352. [Google Scholar] [CrossRef]
- Bunsawat, K.; White, D.W.; Kappus, R.M.; Baynard, T. Caffeine delays autonomic recovery following acute exercise. Eur. J. Prev. Cardiol. 2015, 22, 1473–1479. [Google Scholar] [CrossRef]
- Steinke, L.; Lanfear, D.E.; Dhanapal, V.; Kalus, J.S. Effect of “energy drink” consumption on hemodynamic and electrocardiographic parameters in healthy young adults. Ann. Pharmacother. 2009, 43, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Harpaz, E.; Tamir, S.; Weinstein, A.; Weinstein, Y. The effect of caffeine on energy balance. J. Basic Clin. Physiol. Pharmacol. 2017, 28, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Westerterp-Plantenga, M.S.; Lejeune, M.P.; Kovacs, E.M. Body weight loss and weight maintenance in relation to habitual caffeine intake and green tea supplementation. Obes. Res. 2005, 13, 1195–1204. [Google Scholar] [CrossRef]
- Lecoultre, V.; Egli, L.; Carrel, G.; Theytaz, F.; Kreis, R.; Schneiter, P.; Boss, A.; Zwygart, K.; Lê, K.A.; Bortolotti, M.; et al. Effects of fructose and glucose overfeeding on hepatic insulin sensitivity and intrahepatic lipids in healthy humans. Obesity (Silver Spring) 2013, 21, 782–785. [Google Scholar] [CrossRef]
- Goran, M.I.; Ulijaszek, S.J.; Ventura, E.E. High fructose corn syrup and diabetes prevalence: A global perspective. Glob. Public Health 2013, 8, 55–64. [Google Scholar] [CrossRef]
- Stanhope, K.L.; Schwarz, J.M.; Keim, N.L.; Griffen, S.C.; Bremer, A.A.; Graham, J.L.; Hatcher, B.; Cox, C.L.; Dyachenko, A.; Zhang, W.; et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J. Clin. Investig. 2009, 119, 1322–1334. [Google Scholar] [CrossRef]
- Sarwar, N.; Gao, P.; Seshasai, S.R.; Gobin, R.; Kaptoge, S.; Di Angelantonio, E.; Ingelsson, E.; Lawlor, D.A.; Selvin, E.; Stampfer, M.; et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet 2010, 375, 2215–2222. [Google Scholar]
- Aune, D.; Schlesinger, S.; Neuenschwander, M.; Feng, T.; Janszky, I.; Norat, T.; Riboli, E. Diabetes mellitus, blood glucose and the risk of heart failure: A systematic review and meta-analysis of prospective studies. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 1081–1091. [Google Scholar] [CrossRef] [PubMed]
- Liye, H.; Lvyun, Z.; Guangyao, S.; Luping, R. Investigation of early change of endothelial function and related factors in individuals with hyperglycemia. Diabetes Res. Clin. Pract. 2011, 92, 194–197. [Google Scholar] [CrossRef] [PubMed]
- National Diabetes Service Scheme. Fact Sheet: Diabetes-Related Complications. Available online: https://www.ndss.com.au/wp-content/uploads/fact-sheets/fact-sheet-diabetes-related-complications.pdf (accessed on 17 November 2022).
- Forbes, J.M.; Cooper, M.E. Mechanisms of diabetic complications. Physiol. Rev. 2013, 93, 137–188. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.A.; Lee, Y.; Seo, J.H. Renal Complication and Glycemic Control in Korean Veterans with Type 2 Diabetes: A 10-Year Retrospective Cohort Study. J. Diabetes Res. 2020, 2020, 9806790. [Google Scholar] [CrossRef]
- Bytzer, P.; Talley, N.J.; Hammer, J.; Young, L.J.; Jones, M.P.; Horowitz, M. GI symptoms in diabetes mellitus are associated with both poor glycemic control and diabetic complications. Am. J. Gastroenterol. 2002, 97, 604–611. [Google Scholar] [CrossRef]
- Bytzer, P.; Talley, N.J.; Leemon, M.; Young, L.J.; Jones, M.P.; Horowitz, M. Prevalence of gastrointestinal symptoms associated with diabetes mellitus: A population-based survey of 15,000 adults. Arch. Intern. Med. 2001, 161, 1989–1996. [Google Scholar] [CrossRef]
- Thorve, V.S.; Kshirsagar, A.D.; Vyawahare, N.S.; Joshi, V.S.; Ingale, K.G.; Mohite, R.J. Diabetes-induced erectile dysfunction: Epidemiology, pathophysiology and management. J. Diabetes Complicat. 2011, 25, 129–136. [Google Scholar] [CrossRef]
- Bryan, R.N.; Bilello, M.; Davatzikos, C.; Lazar, R.M.; Murray, A.; Horowitz, K.; Lovato, J.; Miller, M.E.; Williamson, J.; Launer, L.J. Effect of diabetes on brain structure: The action to control cardiovascular risk in diabetes MR imaging baseline data. Radiology 2014, 272, 210–216. [Google Scholar] [CrossRef]
- Li, F.R.; Yang, H.L.; Zhou, R.; Zheng, J.Z.; Chen, G.C.; Wu, X.X.; Zou, M.C.; Wang, J.Y.; Fu, Q.; Wu, X.B. Influence of Diabetes Duration and Glycemic Control on Dementia: A Cohort Study. J. Gerontol. A Biol. Sci. Med. Sci. 2021, 76, 2062–2070. [Google Scholar] [CrossRef]
- Zheng, B.; Su, B.; Price, G.; Tzoulaki, I.; Ahmadi-Abhari, S.; Middleton, L. Glycemic Control, Diabetic Complications, and Risk of Dementia in Patients With Diabetes: Results From a Large U.K. Cohort Study. Diabetes Care 2021, 44, 1556–1563. [Google Scholar] [CrossRef]
- Korea Disease Control and Prevention Agency. Quality Control of the Clinical Laboratory for the Korea National Health and Nutrition Examination Survey (KNHANES) (2019–2021, 8th); Korea Disease Control and Prevention Agency: Cheongju, Republic of Korea, 2021.
| Frequency of SSC Consumption (Day) | p-Value | |||
|---|---|---|---|---|
| Characteristics | None | 1 | ≥2 | |
| N (%) | 3030 (53.43) | 1501 (26.47) | 1140 (20.10) | |
| Age | 64.99 ± 0.19 | 66.28 ± 0.27 | 64.51 ± 0.31 | 0.9 |
| Sex | <0.001 | |||
| Men | 1270 (41.91) | 671 (44.70) | 796 (69.82) | |
| Women | 1760 (58.09) | 830 (55.30) | 344 (30.18) | |
| Household income | 0.003 | |||
| Low | 1121 (37.29) | 584 (39.25) | 396 (34.92) | |
| Mid-low | 811 (26.98) | 415 (27.89) | 299 (26.37) | |
| Mid-high | 536 (17.83) | 275 (18.48) | 252 (22.22) | |
| High | 538 (17.90) | 214 (14.38) | 187 (16.49) | |
| Education level | 0.04 | |||
| Middle school graduation or lower | 1821 (62.28) | 952 (65.52) | 675 (61.14) | |
| High school graduation or higher | 1103 (37.72) | 501 (34.48) | 429 (38.86) | |
| Alcohol consumption status | <0.001 | |||
| Non-drinkers | 1463 (48.95) | 653 (43.91) | 410 (36.35) | |
| Drinkers | 1526 (51.05) | 834 (56.09) | 718 (63.65) | |
| Smoking status | <0.001 | |||
| Non-smokers | 2640 (88.32) | 1249 (83.99) | 744 (66.13) | |
| Smokers | 349 (11.68) | 238 (16.01) | 381 (33.87) | |
| DM medical treatment status | 0.09 | |||
| Oral hypoglycemic agents or insulin treatments | 2757 (90.99) | 1379 (91.87) | 1019 (89.39) | |
| Non-care | 273 (9.01) | 122 (8.13) | 121 (10.61) | |
| Physical activity level (METs-h/week) | 24.64 ± 0.80 | 25.24 ± 1.13 | 27.12 ± 1.30 | 0.1 |
| Body mass index (kg/m2) | 24.96 ± 0.06 | 24.99 ± 0.09 | 24.96 ± 0.10 | 0.9 |
| Diabetes duration (year) | 9.35 ± 0.16 | 9.51 ± 0.22 | 9.36 ± 0.25 | 0.8 |
| Total energy intake (kcal/day) | 1667.31 ± 12.73 | 1699.79 ± 18.08 | 1941.49 ± 20.75 | <0.001 |
| Frequency of SSC Consumption (Day) | None | 1 | ≥2 | p-Value |
|---|---|---|---|---|
| Total energy (%, KDRIs) (1) | 91.94 ± 1.37 B | 95.07 ± 1.59 B | 99.69 ± 1.65 A | <0.001 |
| Carbohydrate (% of total energy) (2) | 69.76 ± 0.42 | 69.97 ± 0.47 | 70.54 ± 0.46 | 0.2 |
| Protein (% of total energy) (2) | 14.63 ± 0.20 A | 14.12 ± 0.20 B | 13.57 ± 0.21 C | <0.001 |
| Fat (% of total energy) (2) | 15.62 ± 0.32 | 15.92 ± 0.37 | 15.89 ± 0.34 | 0.6 |
| Frequency of SSC Consumption (Day) | None | 1 | ≥2 | p for Trend |
|---|---|---|---|---|
| Fasting blood glucose | ||||
| Cases (%) | 1421 (48.22) | 736 (50.62) | 565 (52.03) | |
| Model 1 | Ref | 1.18 (1.01–1.36) | 1.25 (1.06–1.48) | 0.005 |
| Model 2 | Ref | 1.21 (1.04–1.40) | 1.20 (1.01–1.43) | 0.01 |
| Model 3 | Ref | 1.18 (1.01–1.38) | 1.24 (1.03–1.48) | 0.01 |
| Hemoglobin A1c | ||||
| Cases (%) | 2157 (71.19) | 1112 (74.08) | 853 (74.82) | |
| Model 1 | Ref | 1.16 (0.98–1.37) | 1.26 (1.04–1.52) | 0.009 |
| Model 2 | Ref | 1.18 (1.00–1.40) | 1.28 (1.06–1.56) | 0.005 |
| Model 3 | Ref | 1.15 (0.96–1.38) | 1.29 (1.05–1.58) | 0.009 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoo, H.; Park, K. Sugar-Sweetened Coffee Intake and Blood Glucose Management in Korean Patients with Diabetes Mellitus. Metabolites 2022, 12, 1177. https://doi.org/10.3390/metabo12121177
Yoo H, Park K. Sugar-Sweetened Coffee Intake and Blood Glucose Management in Korean Patients with Diabetes Mellitus. Metabolites. 2022; 12(12):1177. https://doi.org/10.3390/metabo12121177
Chicago/Turabian StyleYoo, Hyeonji, and Kyong Park. 2022. "Sugar-Sweetened Coffee Intake and Blood Glucose Management in Korean Patients with Diabetes Mellitus" Metabolites 12, no. 12: 1177. https://doi.org/10.3390/metabo12121177
APA StyleYoo, H., & Park, K. (2022). Sugar-Sweetened Coffee Intake and Blood Glucose Management in Korean Patients with Diabetes Mellitus. Metabolites, 12(12), 1177. https://doi.org/10.3390/metabo12121177








