Salivary Concentrations of Chemerin, α-Defensin 1, and TNF-α as Potential Biomarkers in the Early Diagnosis of Colorectal Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Patients
2.3. Analytical Methods
2.3.1. Determination of Chemerin Concentration
2.3.2. Determination of α-Defensin 1 Concentration
2.3.3. Determination of TNF-α Concentration
2.4. Statistical Analysis
3. Results
4. Discussion
5. Limitation
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferlay, J.; Shin, H.R.; Bray, F.; Forman, D.; Mathers, C.; Parkin, D.M. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int. J. Cancer. 2010, 127, 2893–2917. [Google Scholar] [CrossRef] [PubMed]
- Bozaoglu, K.; Bolton, K.; McMillan, J.; Zimmet, P.; Jowett, J.; Collier, G.; Walder, K.; Segal, D. Chemerin Is a Novel Adipokine Associated with Obesity and Metabolic Syndrome. Endocrinology 2007, 148, 4687–4694. [Google Scholar] [CrossRef] [PubMed]
- Kumar, J.D.; Holmberg, C.; Kandola, S.; Steele, I.; Hegyi, P.; Tiszlavicz, L.; Jenkins, R.; Beynon, R.; Peeney, D.; Giger, O.T.; et al. Increased Expression of Chemerin in Squamous Esophageal Cancer Myofibroblasts and Role in Recruitment of Mesenchymal Stromal Cells. PLoS ONE 2014, 9, e104877. [Google Scholar] [CrossRef]
- Chamberland, J.P.; Berman, R.L.; Aronis, K.; Mantzoros, C.S. View More Chemerin is expressed mainly in pancreas and liver, is regulated by energy deprivation, and lacks day/night variation in humans. Eur. J. Endocrinol. 2013, 169, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Wittamer, V.; Franssen, J.D.; Vulcano, M.; Mirjolet, J.F.; Le Poul, E.; Migeotte, I.; Brézillon, S.; Tyldesley, R.; Blanpain, C.; Detheux, M.; et al. Specific recruitment of antigen-presenting cells by chemerin, a novel processed ligand from human inflammatory fluids. J. Exp. Med. 2003, 198, 977–985. [Google Scholar] [CrossRef]
- Chyra, A. Plejotropowe działanie chemeryny—Białkowego produktu genu TIG2. Ann. Acad. Med. Silesiensis 2012, 66, 55–58. [Google Scholar]
- Treeck, O.; Buechler, C.; Ortmann, O. Chemerin and Cancer. Int. J. Mol. Sci. 2019, 20, 3750. [Google Scholar] [CrossRef]
- Rourke, J.; Dranse, H.; Sinal, C. CMKLR1 and GPR1 mediate chemerin signaling through the RhoA/ROCK pathway. Mol. Cell Endocrinol. 2015, 417, 36–51. [Google Scholar] [CrossRef]
- Kaur, J.; Adya, R.; Tan, B.K.; Chen, J.; Randeva, H.S. Identification of chemerin receptor (ChemR23) in human endothelial cells: Chemerin-induced endothelial angiogenesis. Biochem. Biophys. Res. Commun. 2010, 391, 1762–1768. [Google Scholar] [CrossRef]
- Dimitriadis, G.K.; Kaur, J.; Adya, R.; Miras, A.D.; Mattu, H.S.; Hattersley, J.G.; Kaltsas, G.; Tan, B.K.; Randeva, H.S. Chemerin induces endothelial cell inflammation: Activation of nuclear factor-kappa β and monocyte-endothelial adhesion. Oncotarget 2018, 9, 16678–16690. [Google Scholar] [CrossRef]
- Lehrke, M.; Becker, A.; Greif, A. Chemerin is associated with markers of inflammation and components of the metabolic syndrome but does not predict coronary atherosclerosis. Eur. J. Endocrinol. 2009, 161, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Weigert, J.; Obermeier, F.; Neumeier, M.; Wanninger, J.; Filarsky, M.; Bauer, S.; Aslanidis, C.; Rogler, G.; Ott, C.; Schaffler, A.; et al. Circulating levels of chemerin and adiponectin are higher in ulcerative colitis and chemerin is elevated in Crohn’s disease. Inflamm. Bowel Dis. 2010, 16, 630–637. [Google Scholar] [CrossRef] [PubMed]
- Kumar, J.D.; Tiszlavicz, A.; Reisz, Z.; Dockray, G.J.; Varro, A. Chemerin acts via CMKLR1 and GPR1 to stimulate migration and invasion of gastric cancer cells: Putative role of decreased TIMP-1 and TIMP-2. Oncotarget 2019, 10, 98–112. [Google Scholar] [CrossRef]
- Booth, A.; Magnuson, A.; Fouts, J.; Foster, M. Adipose tissue, obesity and adipokines: Role in cancer promotion. Horm. Mol. Biol. Clin. Investig. 2015, 21, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Wang, Q.J.; Feng, Y.Y.; Shang, W.; Cai, M. Overexpression of chemerin was associated with tumor angiogenesis and poor clinical outcome in squamous cell carcinoma of the oral tongue. Clin. Oral. Investig. 2014, 18, 997–1004. [Google Scholar] [CrossRef]
- Kiczmer, P.; Prawdzic Seńkowska, A.; Kula, A.; Dawidowicz, M.; Strzelczyk, J.; Nowakowska-Zajdel, E.; Walkiewicz, K.; Waniczek, D.; Ostrowska, Z.; Świętochowska, E.; et al. Assessment of CMKLR1 level in colorectal cancer and its correlation with angiogenic markers. Exp. Mol. Pathol. 2020, 113, 104377. [Google Scholar] [CrossRef]
- Buechler, C.; Feder, S.; Haberl, E.M.; Aslanidis, C. Chemerin isoforms and activity in obesity. Int. J. Mol. Sci. 2019, 20, 1128. [Google Scholar] [CrossRef]
- Rourke, J.L.; Dranse, H.J.; Sinal, C.J. Towards an integrative approach to understanding the role of chemerin in human health and disease. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2013, 14, 245–246. [Google Scholar] [CrossRef]
- Fellermann, K.; Stange, D.E.; Schaeffeler, E.; Schmalzl, H.; Wehkamp, J.; Bevins, C.; Reinisch, W.; Teml, A.; Schwab, M.; Lichter, P.; et al. A chromosome 8 gene-cluster polymorphism with low human beta-defensin 2 gene copy number predisposes to Crohn disease of the colon. Am. J. Hum. Genet. 2006, 79, 439–448. [Google Scholar] [CrossRef]
- Hill, C.P.; Yee, J.; Selsted, M.E.; Eisenberg, D. Crystal structure of defensin HNP-3, an amphiphilic dimer: Mechanisms of membrane permeabilization. Science 1991, 251, 1481–1485. [Google Scholar] [CrossRef]
- Cunliffe, R.N.; Mahida, Y.R. Expression and regulation of antimicrobial peptides in the gastrointestinal tract. J. Leukoc. Biol. 2004, 75, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Cunliffe, R.N. Alpha-defensins in the gastrointestinal tract. Mol. Immunol. 2003, 40, 463–467. [Google Scholar] [CrossRef]
- Wehkamp, J.; Schwind, B.; Herrlinger, K.R.; Baxmann, S.; Schmidt, K.; Duchrow, M.; Wohschlager, C.; Feller, A.C.; Stange, E.F.; Fellermann, K. Innate immunity and colonic inflammation: Enhanced expression of epithelial alpha-defensins. Dig. Dis. Sci. 2002, 47, 1349–1355. [Google Scholar] [CrossRef]
- Negroni, A.; Stronati, L.; Pierdomenico, M.; Tirindelli, D.; Di Nardo, G.; Mancini, V.; Maiella, G.; Cucchiara, G. Activation of NOD2-mediated intestinal pathway in a pediatric population with Crohn’s disease. Inflamm. Bowel Dis. 2009, 15, 1145–1154. [Google Scholar] [CrossRef] [PubMed]
- Jin, G.; Kawsar, I.; Hirsch, S.; Zeng, C.; Jia, X.; Feng, Z.; Ghosh, S.K.; Zheng, Q.Y.; Zhou, A.; McIntyre, T.M.; et al. An antimicrobial peptide regulates tumor-associated macrophage trafficking via the chemokine receptor CCR2, a model for tumorigenesis. PLoS ONE 2010, 5, e10993. [Google Scholar] [CrossRef]
- Melle, C.; Ernst, G.; Schimmel, B.; Urbanek, A. Discovery and identification of alpha-defensins as low abundant, tumor-derived serum markers in colorectal cancer. Gastroenterology 2005, 129, 66–73. [Google Scholar] [CrossRef]
- Albrethsen, J.; Bogebo, R.; Gammeltoft, S.; Olsen, J.; Winther, H.; Raskov, H. Upregulated expression of human neutrophil peptides 1, 2 and 3 (HNP 1–3) in colon cancer serum and tumours: A biomarker study. BMC Cancer 2005, 5, 8–12. [Google Scholar] [CrossRef]
- Albrethsen, J.; Møller, C.H.; Olsen, J.; Raskov, H.; Gammeltoft, S. Human neutrophil peptides 1, 2 and 3 are biochemical markers for metastatic colorectal cancer. Eur. J. Cancer 2006, 42, 3057–3064. [Google Scholar] [CrossRef]
- Lundy, F.T.; Orr, D.F.; Gallagher, J.R.; Maxwell, P.; Shaw, C.; Napier, S.S.; Gerald Cowan, C.; Lamey, P.J.; Marley, J.J. Identification and overexpression of human neutrophil alpha-defensins (human neutrophil peptides 1, 2 and 3) in squamous cell carcinomas of the human tongue. Oral Oncol. 2004, 40, 139–144. [Google Scholar] [CrossRef]
- Muller, C.A.; Markovic-Lipkovski, J.; Klatt, T.; Gamper, J.; Schwarz, G.; Beck, H.; Deeg, M.; Kalbacher, H.; Widmann, S.; Wessels, J.T.; et al. Human alpha-defensins HNPs-1,-2, and-3 in renal cell carcinoma—Influences on tumor cell proliferation. Am. J. Pathol. 2002, 160, 1311–1324. [Google Scholar] [CrossRef]
- Droin, N.; Jean-Baptiste, H.; Ducoroy, P.; Solary, E. Human defensins as cancer biomarkers and antitumour molecules. Proteomics 2009, 72, 918–927. [Google Scholar] [CrossRef] [PubMed]
- Sethi, G.; Sung, B.; Aggarwal, B.B. TNF: A master switch for inflammation to cancer. Front Biosci. 2008, 13, 5094–5107. [Google Scholar] [CrossRef] [PubMed]
- Muc-Wierzgoń, M.; Nowakowska-Zajdel, E.; Kokot, T.; Zubelewicz, B.; Klakla, K.; Wilczok, T.; Sosada, K.; Wierzgoń, J. Genetic disregulation of gene coding tumor necrosis factor α receptors (TNFα Rs) in colorectal cancer cells. J. Biol. Homeost. Agents. 2004, 23, 651–660. [Google Scholar]
- Hoving, S.; Seynhaeve, A.L.; van Tiel, S.T.; Ambagtsheer, G. Early destruction of tumor vasculature in tumor necrosis factor-alpha-based isolated limb perfusion is responsible for tumor response. Anticancer Drugs 2006, 17, 949–959. [Google Scholar] [CrossRef] [PubMed]
- Tzanavari, T.; Giannogonas, P.; Karalis., K.P. TNF-alpha and obesity. Curr. Dir. Autoimmun. 2010, 11, 145–156. [Google Scholar]
- Guadagni, F.; Ferroni, P.; Palmirotta, R.; Portarena, I.; Formica, V.; Roselli, M. TNF/VEGF cross-talk in chronic inflammation-related cancer initiation and progression: An early target in anticancer therapeutic strategy. In Vivo 2007, 21, 147–161. [Google Scholar]
- Zidi, I.; Mestiri, S.; Bartegi, A.; Amor, N.B. TNF-alpha and its inhibitors in cancer. Med. Oncol. 2010, 27, 185–198. [Google Scholar] [CrossRef]
- Balkwill, F. Tumour necrosis factor and cancer. Nat. Rev. Cancer 2009, 9, 361–371. [Google Scholar] [CrossRef]
- Obeed, O.A.; Alkhayal, K.A.; Sheikh, A.; Zubaidi, A.; Vaali-Mohammed, M.; Boushey, R.; Mckerrow, J.; Abdulla, M. Increased expression of tumor necrosis factor-alpha is associated with advanced colorectal cancer stages. World J. Gastroenterol. 2014, 20, 18390–18396. [Google Scholar] [CrossRef]
- Grimm, M.; Lazariotou, M.; Kircher, M.; Höfelmayr, A.; Germer, C.T.; Rahden, B.H.; Waaga-Gasser, A.M.; Gasser, M. Tumor necrosis factor-alpha is associated with positive lymph node status in patients with recurrence of colorectal cancer-indications for anti-TNF-alpha agents in cancer treatment. Cell Oncol. 2011, 34, 315–326. [Google Scholar] [CrossRef]
- Stanilov, N.; Miteva, L.; Dobreva, Z.; Stanilova, S. Colorectal cancer severity and survival in correlation with tumour necrosis factor-alpha. Biotechnol. Biotechnol. Equip. 2014, 28, 911–917. [Google Scholar] [CrossRef]
- Erdogan, S.; Yilmaz, F.M.; Yazici, O.; Yozgat, A.; Sezer, S.; Ozdemir, N.; Uysal, S.; Purnak, T.; Sendur, M.A.; Ozaslan, E. Inflammation and chemerin in colorectal cancer. Tumour Biol. 2016, 37, 6337. [Google Scholar] [CrossRef] [PubMed]
- Alkady, M.M.; Abdel-Messeih, A.; Neveen, M.N. Assessment of Serum Levels of the Adipocytokine Chemerin in Colorectal Cancer Patients. J. Med. Biochem. 2018, 37, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Coşkun, Ö.; Öztopuz, Ö.; Özkan, Ö.F. Determination of IL-6, TNF-α and VEGF levels in the serums of patients with colorectal cancer. Cell Mol. Biol. (Noisy-le-Grand) 2017, 63, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Eichelmann, F.; Schulze, M.B.; Wittenbecher, C.; Menzel, J.; Weikert, C.; Giuseppe, R.; Biemann, R.; Isermann, B.; Fritsche, A.; Boeing, H.; et al. Association of Chemerin Plasma Concentration With Risk of Colorectal Cancer. JAMA Netw. Open 2019, 2, e190896. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, B.; Shishodia, S.; Takada, Y.; Jackson-Bernitsas, D.; Ahn, K.S.; Sethi, G.; Ichikawa, H. TNF blockade: An inflammatory issue. Ernst Schering Res. Found. Workshop 2006, 16, 161–186. [Google Scholar]
- Zhang, X.; Liu, S.; Zhou, Z. Circulating levels of C-reactive protein, interleukin-6 and tumor necrosis factor-α and risk of colorectal adenomas: A meta-analysis. Oncotarget 2016, 7, 64371–64379. [Google Scholar] [CrossRef]
- Perwez Hussain, M.; Harris, C. Inflammation and cancer: An ancient link with novel potentials. Int. J. Cancer. 2007, 121, 2373–2380. [Google Scholar] [CrossRef]
- Lin, W.; Karin, M. A cytokine-mediated link between innate immunity, inflammation, and cancer. J. Clin. Investig. 2007, 117, 1175–1183. [Google Scholar] [CrossRef]
- Zaloudik, J.; Lauerova, L.; Janakova, L.; Talac, R.; Simickova, M.; Nekulova, M.; Kovarik, J.; Sheard, M. Significance of pretreatment immunological parameters in colorectal cancer patients with unresectable metastases to the liver. Hepatogastroenterology 1999, 46, 220–227. [Google Scholar]
- Il’yasova, D.; Colbert, L.H.; Harris, T.B.; Newman, A.B.; Bauer, D.; Satterfield, S.; Kritchchevsky, S. Circulating Levels of Inflammatory Markers and Cancer Risk in the Health Aging and Body Composition Cohort. Cancer Epidemiol. Biomark. Prev. 2005, 14, 2413–2418. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Keku, T.O.; Martin, C.; Galanko, J.; Woosley, J.T.; Schroeder, J.C.; Satia, J.; Halabi, S.; Sandler, R.S. Circulating levels of inflammatory cytokines and risk of colorectal adenomas. Cancer Res. 2008, 68, 323–328. [Google Scholar] [CrossRef]
- Yagi, M.; Sasaki, Y.; Abe, Y.; Yaoita, T.; Sakuta, K.; Mizumoto, N.; Shoji, M.; Onozato, Y.; Kon, T.; Nishise, S.; et al. Association between High Levels of Circulating Chemerin and Colorectal Adenoma in Men. Digestion 2020, 101, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Ardizzoia, A.; Lissoni, P.; Brivio, F.; Tisi, E.; Perego, M.S.; Grassi, M.G.; Pittalis, S.; Crispino, S.; Barni, S.; Tancini, G. Tumor necrosis factor in solid tumors: Increased blood levels in the metastatic disease. J. Biol. Regul. Homeost. Agents 1992, 6, 103–107. [Google Scholar]
- Muc-Wierzgoń, M.; Baranowski, M.; Madej, K.; Wierzgoń, J.; Kokot, T.; Brodziak, A. Dynamics of diurnal changes in serum concentrations of TNF alfa soluble receptors in gastrointestinal cancer patients. J. Biol. Regul. Homeost. Agents 2000, 14, 204–208. [Google Scholar]
- Boyuk, C.; Guzel, M.; Atalay, H.; Guzel, S.; Mutlu, L.; Kucukyalcin, V. Relationship between plasma chemerin levels and disease severity in COPD patients. Clin. Respir. J. 2015, 9, 468–474. [Google Scholar] [CrossRef]
- Alzamil, X. Elevated Serum TNF-α is Related to Obesity in Type 2 Diabetes Mellitus and Is Associated with Glycemic Control and Insulin Resistance. J. Obes. 2020, 20, 5076858. [Google Scholar] [CrossRef]
- Wang, C.; Wu, K.; Liu, X.; To, K.-H.; Chen, G.; Yu, J.; Ng, E.K. Increased serum chemerin level promotes cellular invasiveness in gastric cancer: A clinical and experimental study. Peptides 2014, 51, 131–138. [Google Scholar] [CrossRef]
- Liu, J.; Duan, Y. Saliva: A potential media for disease diagnostics and monitoring. Oral Oncol. 2012, 48, 569–577. [Google Scholar] [CrossRef]
- Mizukawa, N.; Sugiyama, K.; Fukunaga, J.; Mishima, K.; Takagi, S.; Sugahara, T. Defensin-1, a peptide detected in the saliva of oral squamous cell carcinoma patients. Anticancer Res. 1998, 18, 4645–4649. [Google Scholar] [PubMed]
- Pfaffe, T.; Cooper-White, J.; Beyerlein, P.; Kostner, K.; Punyadeera, C. Diagnostic Potential of Saliva: Current State and Future Applications. Clin. Chem. 2011, 57, 675–687. [Google Scholar] [CrossRef] [PubMed]
- Lyudmila, V.; Belskaya, E.; Sarf, A.; Kosenok, V.K. Age and gender characteristics of the biochemical composition of saliva: Correlations with the composition of blood plasma. J. Oral. Biol. Craniofac. Res. 2020, 10, 59–65. [Google Scholar]


| Feature | Value |
|---|---|
| Tumor location | Cecum: 2 (5.13%) Ascending colon: 6 (15.38%) Transverse colon: 3 (7.69%) Descending colon: 1 (2.56%) Sigmoid colon and rectosigmoid junction: 6 (15.36%) Rectum: 13 (33.33%) left colon: 13 (33.33%) Left colon and rectum: 26 (66.67%) Colon: 26 (66.67%) Rectum: 13 (33.33%) |
| Gender | Male:18 (46.2%); Female: 21(53.8%) |
| Grading | G1:0 (0%); G2: 22 (56.4%); G3: 17(43.6%) |
| T | I: 1 (2.56%); II: 16 (41.03%); III: 20 (51.28%); IV: 2 (5.13%) |
| N | N0: 24 (61.54%); N1: 4 (10.26%); N2: 11 (28.21%) |
| M | M0: 36 (92.31%); M1: 3 (7.69%) |
| TNM staging | I: 14 (35.9%); II: 9 (23.08%); III: 13 (33.33%); IV: 3 (7.69%) |
| Astler-Coller staging | A1: 1 (2.56%); B1: 13 (33.33%); B2: 8 (20.51%); C1: 3 (7.69%); C2: 11 (28.21%); D: 3 (7.69%) |
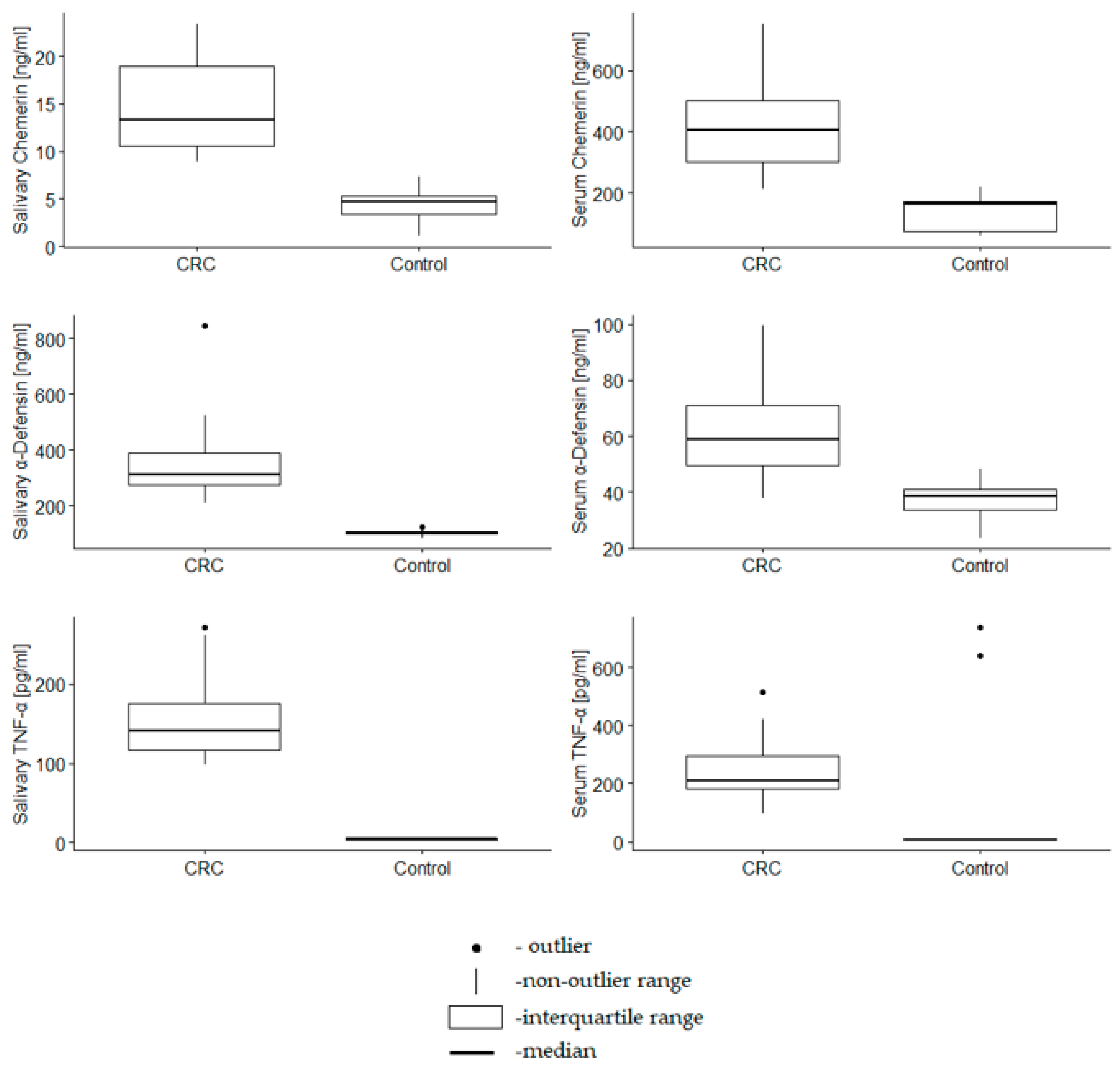
| Marker Concentration | Control | CRC | p | ||||
|---|---|---|---|---|---|---|---|
| Median | Q1 | Q3 | Median | Q1 | Q3 | ||
| Serum chemerin (ng/mL) | 164.07 | 73.37 | 173.39 | 406.52 | 302.54 | 502.10 | <0.001 |
| Salivary chemerin (ng/mL) | 4.71 | 3.39 | 5.25 | 13.28 | 10.21 | 18.94 | <0.001 |
| Serum α -defensin1 (ng/mL) | 38.51 | 33.58 | 40.95 | 58.83 | 49.47 | 72.84 | <0.001 |
| Salivary α -defensin1 (ng/mL) | 104.39 | 98.23 | 108.95 | 310.92 | 274.09 | 398.84 | <0.001 |
| Serum TNF α (ng/mL) | 7.23 | 6.49 | 7.87 | 207.66 | 176.59 | 302.31 | <0.001 |
| Salivary TNF α (ng/mL) | 4.60 | 3.83 | 5.26 | 141.28 | 115.91 | 176.48 | <0.001 |
| Cut-Off Value | AUC | SE | Lower AUC 95% | Upper AUC 95% | z-Score | p | Specificity | Sensitivity | |
|---|---|---|---|---|---|---|---|---|---|
| Serum chemerin | 231.24 | 1.00 | 0.00 | 1.00 | 1.00 | 281.31 | 0.00 | 1.00 | 0.99 |
| Salivary chemerin | 8.85 | 1.00 | 0.00 | 1.00 | 1.00 | - | 0.00 | 1.00 | 1.00 |
| Serum α-defensin1 | 46.79 | 0.95 | 0.02 | 0.91 | 1.00 | 19.69 | 0.00 | 1.00 | 0.91 |
| Salivary α-defensin 1 | 211.46 | 1.00 | 0.00 | 1.00 | 1.00 | - | 0.00 | 1.00 | 1.00 |
| Serum TNF-α | 95.64 | 0.95 | 0.03 | 0.88 | 1.00 | 13.06 | 0.00 | 1.00 | 0.95 |
| Salivary TNF-α | 97.86 | 1.00 | 0.00 | 1.00 | 1.00 | - | 0.00 | 1.00 | 1.00 |
| Marker Concentration | BMI < 25 | BMI ≥ 25 | p | ||||
|---|---|---|---|---|---|---|---|
| Median | Q1 | Q3 | Median | Q1 | Q3 | ||
| Serum chemerin (ng/mL) | 190.26 | 163.22 | 302.54 | 289.39 | 164.92 | 439.01 | 0.18 |
| Salivary chemerin (ng/mL) | 5.64 | 4.88 | 11.45 | 9.49 | 4.27 | 14.37 | 0.82 |
| Serum α-defensin 1(ng/mL) | 41.92 | 36.36 | 51.91 | 45.75 | 39.71 | 63.84 | 0.27 |
| Salivary α-defensin 1(ng/mL) | 110.52 | 102.37 | 299.31 | 213.04 | 107.28 | 313.67 | 0.40 |
| Serum TNF-α (ng/mL) | 9.35 | 7.23 | 202.37 | 175.63 | 7.23 | 221.37 | 0.40 |
| Salivary TNF-α (ng/mL) | 6.15 | 4.57 | 118.36 | 99.29 | 4.62 | 143.49 | 0.56 |
| Marker Concentration | Stage I + II | Stage III + IV | p | ||||
|---|---|---|---|---|---|---|---|
| Median | Q1 | Q3 | Median | Q1 | Q3 | ||
| Serum chemerin (ng/mL) | 384.69 | 265.18 | 491.30 | 416.09 | 375.91 | 502.10 | 0.24 |
| Salivary chemerin (ng/mL) | 16.04 | 10.36 | 20.72 | 12.47 | 10.21 | 17.65 | 0.42 |
| Serum α-defensin 1(ng/mL) | 66.22 | 50.00 | 81.10 | 55.22 | 49.47 | 65.67 | 0.25 |
| Salivary α-defensin 1(ng/mL) | 322.15 | 281.92 | 465.06 | 285.63 | 254.20 | 318.12 | 0.10 |
| Serum TNF-α (ng/mL) | 229.56 | 196.00 | 305.51 | 205.61 | 153.27 | 286.01 | 0.12 |
| Salivary TNF-α (ng/mL) | 149.17 | 114.05 | 176.81 | 131.06 | 115.91 | 176.48 | 0.47 |
| Marker Concentration | Rectum | Colon | p | ||||
|---|---|---|---|---|---|---|---|
| Median | Q1 | Q3 | Median | Q1 | Q3 | ||
| Serum chemerin (ng/mL) | 389.50 | 261.45 | 472.10 | 411.31 | 312.84 | 503.66 | 0.40 |
| Salivary chemerin (ng/mL) | 13.28 | 10.90 | 18.82 | 14.63 | 10.21 | 20.07 | 0.48 |
| Serum α-defensin | 55.22 | 46.79 | 68.59 | 61.82 | 51.00 | 72.84 | 0.36 |
| Salivary α-defensin | 285.63 | 227.58 | 316.25 | 312.62 | 277.74 | 404.20 | 0.17 |
| Serum TNF-α | 206.58 | 189.63 | 261.36 | 212.35 | 175.63 | 304.51 | 0.73 |
| Salivary TNF-α | 132.75 | 124.12 | 159.74 | 145.44 | 109.73 | 179.84 | 0.75 |
| Left | Right | ||||||
| Serum chemerin (ng/mL) | 427.55 | 298.16 | 541.23 | 386.77 | 312.84 | 425.06 | 0.38 |
| Salivary chemerin (ng/mL) | 12.43 | 10.12 | 18.82 | 16.73 | 11.53 | 21.08 | 0.11 |
| Serum α-defensin | 58.51 | 49.47 | 72.84 | 61.17 | 51.00 | 68.95 | 0.99 |
| Salivary α-defensin | 312.62 | 236.02 | 398.84 | 293.96 | 277.74 | 373.47 | 0.96 |
| Serum TNF-α | 207.12 | 176.59 | 271.49 | 216.54 | 197.68 | 305.41 | 0.53 |
| Salivary TNF-α | 131.91 | 116.49 | 179.84 | 153.05 | 103.79 | 164.62 | 0.74 |
| Marker Concentration | G2 | G3 | p | ||||
|---|---|---|---|---|---|---|---|
| Median | Q1 | Q3 | Median | Q1 | Q3 | ||
| Salivary chemerin (ng/mL) | 12.47 | 11.29 | 18.92 | 16.32 | 10.21 | 20.36 | 0.42 |
| Serum chemerin (ng/mL) | 439.01 | 387.95 | 503.66 | 303.45 | 276.51 | 472.10 | 0.04 |
| Salivary α-defensin (ng/mL) | 310.92 | 275.64 | 318.12 | 293.96 | 274.09 | 404.20 | 0.79 |
| Serum α-defensin (ng/mL) | 51.91 | 48.90 | 62.47 | 68.59 | 58.19 | 78.84 | 0.03 |
| Salivary TNF-α (ng/mL) | 124.12 | 103.79 | 147.38 | 159.74 | 143.49 | 185.72 | 0.01 |
| Serum TNF-α ng/mL) | 205.71 | 175.63 | 286.01 | 221.37 | 197.68 | 305.41 | 0.35 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Waniczek, D.; Świętochowska, E.; Śnietura, M.; Kiczmer, P.; Lorenc, Z.; Muc-Wierzgoń, M. Salivary Concentrations of Chemerin, α-Defensin 1, and TNF-α as Potential Biomarkers in the Early Diagnosis of Colorectal Cancer. Metabolites 2022, 12, 704. https://doi.org/10.3390/metabo12080704
Waniczek D, Świętochowska E, Śnietura M, Kiczmer P, Lorenc Z, Muc-Wierzgoń M. Salivary Concentrations of Chemerin, α-Defensin 1, and TNF-α as Potential Biomarkers in the Early Diagnosis of Colorectal Cancer. Metabolites. 2022; 12(8):704. https://doi.org/10.3390/metabo12080704
Chicago/Turabian StyleWaniczek, Dariusz, Elżbieta Świętochowska, Mirosław Śnietura, Paweł Kiczmer, Zbigniew Lorenc, and Małgorzata Muc-Wierzgoń. 2022. "Salivary Concentrations of Chemerin, α-Defensin 1, and TNF-α as Potential Biomarkers in the Early Diagnosis of Colorectal Cancer" Metabolites 12, no. 8: 704. https://doi.org/10.3390/metabo12080704
APA StyleWaniczek, D., Świętochowska, E., Śnietura, M., Kiczmer, P., Lorenc, Z., & Muc-Wierzgoń, M. (2022). Salivary Concentrations of Chemerin, α-Defensin 1, and TNF-α as Potential Biomarkers in the Early Diagnosis of Colorectal Cancer. Metabolites, 12(8), 704. https://doi.org/10.3390/metabo12080704






