Galacto-Oligosaccharide Alleviates Alcohol-Induced Liver Injury by Inhibiting Oxidative Stress and Inflammation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Reagents
2.2. Cell Culture
2.3. Determination of L02 Cell Damage and the Oxidation–Antioxidant Index
2.4. Animal Grouping and Administration
2.5. Serum Biochemical Analysis
2.6. Detection of Liver Oxidation and Antioxidant Indexes
2.7. Histopathological Observation of the Liver
2.8. Western Blot Analysis
2.9. RT‒PCR Analysis
2.10. Statistical Analysis
3. Results
3.1. Protective Effects of GOS on Alcohol-Induced Injury in L02 Liver Cells
3.2. Effects of GOS on the Oxidative Damage Indexes of L02 Liver Cells
3.3. Effects of GOS on the L02 Liver Cell Antioxidant Enzyme Index
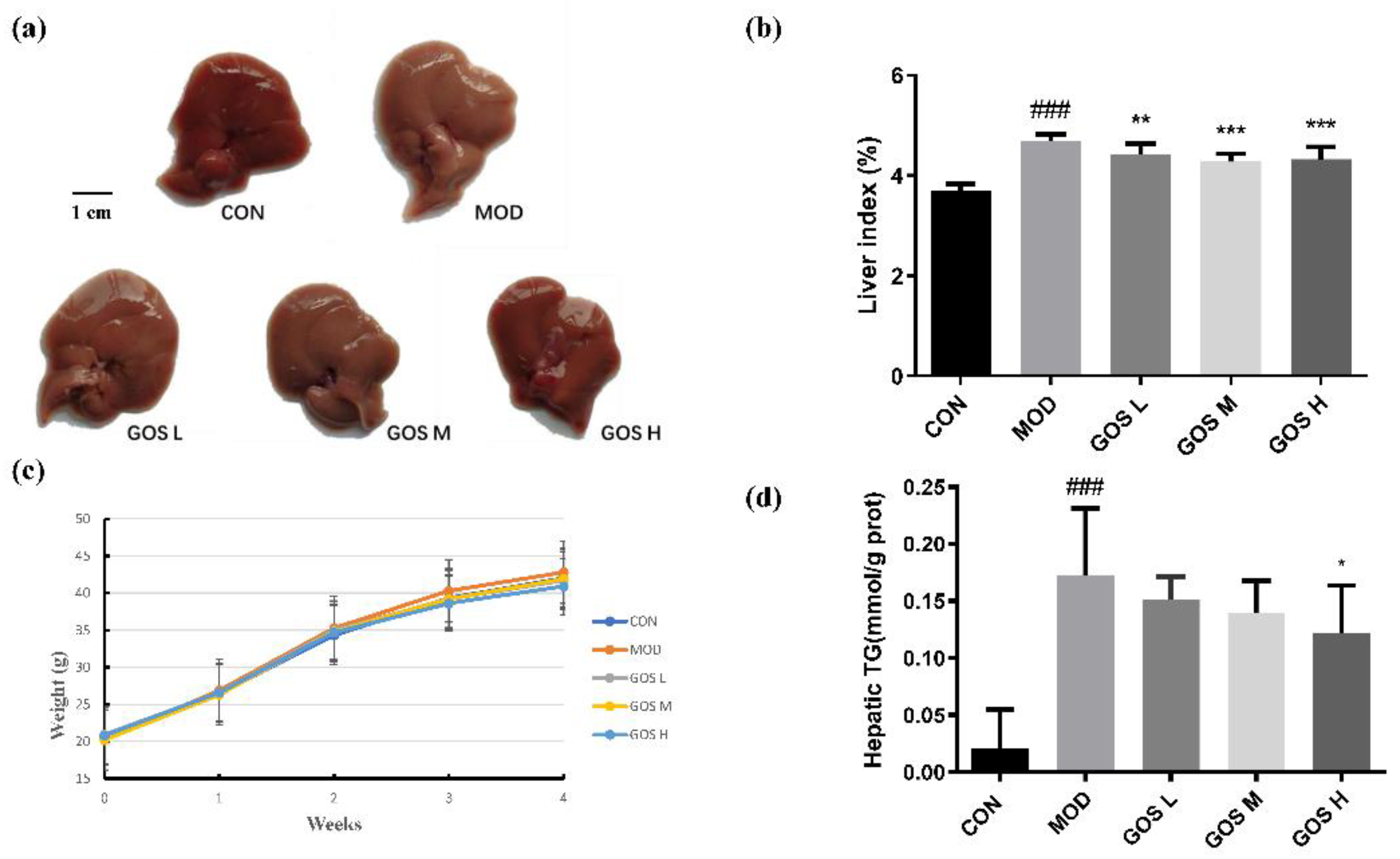
3.4. Effects of GOS on the Body Weight and Liver of Mice
3.5. Effects of GOS on Serum Levels of Proteins Related to Liver Function in Mice
3.6. Effects of GOS on Serum Levels of Inflammatory Factors in Mice
3.7. Effects of GOS on the Oxidative Damage Indexes in the Mouse Liver
3.8. Effects of GOS on the Activity of Antioxidant Enzymes in Mouse Liver
3.9. Effects of GOS on the Alcohol Metabolism Enzyme CYP2E1
3.10. Effects of GOS on the Antioxidant Keap1/Nrf2/HO-1 Pathway
3.11. Effects of GOS on the MAPK/NF-κB Pathways
3.12. Effects of GOS on the NOD-like Receptor Family Pyrin Domain Containing 3 (NLRP3) Inflammasome and Inflammatory Genes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ALD | alcoholic liver disease |
| GOS | galacto-oligosaccharide |
| CYP2E1 | cytochrome P450 protein 2E1 |
| Keap1 | Kelch-like ECH-associated protein 1 |
| Nrf2 | nuclear factor erythroid-2-related factor 2 |
| HO-1 | haem oxygenase-1 |
| FDA | Food and Drug Administration |
| ALT | alanine aminotransferase |
| AST | aspartate aminotransferase |
| MDA | malondialdehyde |
| GSH | glutathione |
| SOD | superoxide dismutase |
| CAT | catalase |
| GSH-Px | glutathione peroxidase |
| T-AOC | total antioxidant capacity |
| ALP | alkaline phosphatase |
| LDH | lactate dehydrogenase |
| TNF-α | tumour necrosis factor-α |
| IL-1β | interleukin-1β |
| IL-6 | interleukin-6 |
| TC | serum total cholesterol |
| TG | triglyceride |
| VLDL | very low-density lipoprotein |
| ROS | reactive oxygen species |
| MAPK | mitogen-activated protein kinase |
| JNK | c-Jun N-terminal kinase |
| NF-κB | nuclear factor kappa-B |
| p38 MAPK | p38 mitogen-activated protein kinase |
| NLRP3 | NOD-like receptor family pyrin domain containing 3 |
| SCFA | short-chain fatty acid |
References
- Subramaniyan, V.; Chakravarthi, S.; Jegasothy, R.; Seng, W.; Fuloria, N.; Fuloria, S.; Hazarika, I.; Das, A. Alcohol-associated liver disease: A review on its pathophysiology, diagnosis and drug therapy. Toxicol. Rep. 2021, 8, 376–385. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Khambu, B.; Hong, H.; Liu, G.; Huda, N.; Yin, X.M. Autophagy, Metabolism, and Alcohol-Related Liver Disease: Novel Modulators and Functions. Int. J. Mol. Sci. 2019, 20, 5029. [Google Scholar] [CrossRef] [PubMed]
- Louvet, A.; Mathurin, P. Alcoholic liver disease: Mechanisms of injury and targeted treatment. Nat. Rev. Gastroenterol. Hepatol. 2015, 12, 231–242. [Google Scholar] [CrossRef]
- Xiao, J.; Wang, F.; Wong, N.K.; He, J.; Zhang, R.; Sun, R.; Xu, Y.; Liu, Y.; Li, W.; Koike, K.; et al. Global liver disease burdens and research trends: Analysis from a Chinese perspective. J. Hepatol. 2019, 71, 212–221. [Google Scholar] [CrossRef] [PubMed]
- Singal, A.K.; Bataller, R.; Ahn, J.; Kamath, P.S.; Shah, V.H. ACG Clinical Guideline: Alcoholic Liver Disease. Am. J. Gastroenterol. 2018, 113, 175–194. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, W.E.; Wahlang, B.; Wang, Y.; Zhang, J.; Vadhanam, M.V.; Joshi-Barve, S.; Bauer, P.; Cannon, R.; Ahmadi, A.R.; Sun, Z.; et al. Phosphodiesterase 4 Inhibition as a Therapeutic Target for Alcoholic Liver Disease: From Bedside to Bench. Hepatology 2019, 70, 1958–1971. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.Z.; Chandimali, N.; Han, Y.H.; Lee, D.H.; Kim, J.S.; Kim, S.U.; Kim, T.D.; Jeong, D.K.; Sun, H.N.; Lee, D.S.; et al. Pathogenesis, Early Diagnosis, and Therapeutic Management of Alcoholic Liver Disease. Int. J. Mol. Sci. 2019, 20, 2712. [Google Scholar] [CrossRef]
- Dorrington, M.; Fraser, I. NF-κB Signaling in Macrophages: Dynamics, Crosstalk, and Signal Integration. Front. Immunol. 2019, 10, 705. [Google Scholar] [CrossRef]
- Osman, A.; Tzortzis, G.; Rastall, R.A.; Charalampopoulos, D. A comprehensive investigation of the synthesis of prebiotic galactooligosaccharides by whole cells of Bifidobacterium bifidum NCIMB 41171. J. Biotechnol. 2010, 150, 140–148. [Google Scholar] [CrossRef]
- Kimura, K.; Matsumoto, K.; Ishihara, C.; Harada, K.; Miyagi, A. Structure determination of galacto-oligosaccharides by pyridylamination and NMR spectroscopy. Carbohydr. Res. 1995, 270, 33–42. [Google Scholar] [CrossRef]
- Macfarlane, G.T.; Steed, H.; Macfarlane, S. Bacterial metabolism and health-related effects of galacto-oligosaccharides and other prebiotics. J. Appl. Microbiol. 2008, 104, 305–344. [Google Scholar] [CrossRef] [PubMed]
- de Jesus, L.; Guimaraes, L.H.S. Production of beta-galactosidase by Trichoderma sp. through solid-state fermentation targeting the recovery of galactooligosaccharides from whey cheese. J. Appl. Microbiol. 2021, 130, 865–877. [Google Scholar] [CrossRef]
- Krumbeck, J.A.; Rasmussen, H.E.; Hutkins, R.W.; Clarke, J.; Shawron, K.; Keshavarzian, A.; Walter, J. Probiotic Bifidobacterium strains and galactooligosaccharides improve intestinal barrier function in obese adults but show no synergism when used together as synbiotics. Microbiome 2018, 6, 121. [Google Scholar] [CrossRef] [PubMed]
- Azcarate-Peril, M.A.; Ritter, A.J.; Savaiano, D.; Monteagudo-Mera, A.; Anderson, C.; Magness, S.T.; Klaenhammer, T.R. Impact of short-chain galactooligosaccharides on the gut microbiome of lactose-intolerant individuals. Proc. Natl. Acad. Sci. USA 2017, 114, E367–E375. [Google Scholar] [CrossRef]
- Nath, A.; Molnar, M.A.; Csighy, A.; Koszegi, K.; Galambos, I.; Huszar, K.P.; Koris, A.; Vatai, G. Biological Activities of Lactose-Based Prebiotics and Symbiosis with Probiotics on Controlling Osteoporosis, Blood-Lipid and Glucose Levels. Medicina 2018, 54, 98. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.S.; Wang, J.; Yannie, P.J.; Sandhu, Y.K.; Korzun, W.J.; Ghosh, S. Dietary Supplementation with Galactooligosaccharides Attenuates High-Fat, High-Cholesterol Diet-Induced Glucose Intolerance and Disruption of Colonic Mucin Layer in C57BL/6 Mice and Reduces Atherosclerosis in Ldlr-/- Mice. J. Nutr. 2020, 150, 285–293. [Google Scholar] [CrossRef]
- Serino, M.; Luche, E.; Gres, S.; Baylac, A.; Bergé, M.; Cenac, C.; Waget, A.; Klopp, P.; Iacovoni, J.; Klopp, C.; et al. Metabolic adaptation to a high-fat diet is associated with a change in the gut microbiota. Gut 2012, 61, 543–553. [Google Scholar] [CrossRef]
- Efsa Panel on Nutrition, N.F.; Food, A.; Turck, D.; Castenmiller, J.; De Henauw, S.; Hirsch-Ernst, K.I.; Kearney, J.; Maciuk, A.; Mangelsdorf, I.; McArdle, H.J.; et al. Safety of a change in the conditions of use of galacto-oligosaccharides as a novel food ingredient in food supplements pursuant to Regulation (EU) 2015/2283. EFSA J. 2021, 19, e06384. [Google Scholar] [CrossRef]
- Morel, F.B.; Dai, Q.; Ni, J.; Thomas, D.; Parnet, P.; Fanca-Berthon, P. alpha-Galacto-oligosaccharides Dose-Dependently Reduce Appetite and Decrease Inflammation in Overweight Adults. J. Nutr. 2015, 145, 2052–2059. [Google Scholar] [CrossRef] [PubMed]
- Qiu, S.; Chen, J.; Bai, Y.; He, J.; Cao, H.; Che, Q.; Guo, J.; Su, Z. GOS Ameliorates Nonalcoholic Fatty Liver Disease Induced by High Fat and High Sugar Diet through Lipid Metabolism and Intestinal Microbes. Nutrients 2022, 14, 2749. [Google Scholar] [CrossRef]
- Kong, S.; Huang, X.; Cao, H.; Bai, Y.; Che, Q.; Nie, H.; Su, Z. Anti-obesity effects of galacto-oligosaccharides in obese rats. Eur. J. Pharmacol. 2022, 917, 174728. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Liu, J.; Tang, Y.; Li, Y.; Yan, Q.; Jiang, Z. Hepatoprotective Potential of Partially Hydrolyzed Guar Gum against Acute Alcohol-Induced Liver Injury in Vitro and Vivo. Nutrients 2019, 11, 963. [Google Scholar] [CrossRef] [PubMed]
- Ursini, F.; Maiorino, M. Lipid peroxidation and ferroptosis: The role of GSH and GPx4. Free Radic. Biol. Med. 2020, 152, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Park, S.; Kim, J.; Boyd, J.; Beld, J.; Taton, A.; Lee, K.; Kim, I.; Golden, J.; Yoon, H. OsDHARExpression of Heterologous Gene Improves Glutathione (GSH)-Dependent Antioxidant System and Maintenance of Cellular Redox Status in PCC 7942. Front. Plant Sci. 2020, 11, 231. [Google Scholar] [CrossRef]
- Oneta, C.; Lieber, C.; Li, J.; Rüttimann, S.; Schmid, B.; Lattmann, J.; Rosman, A.; Seitz, H. Dynamics of cytochrome P4502E1 activity in man: Induction by ethanol and disappearance during withdrawal phase. J. Hepatol. 2002, 36, 47–52. [Google Scholar] [CrossRef]
- Chappuis, E.; Morel-Depeisse, F.; Bariohay, B.; Roux, J. Alpha-Galacto-Oligosaccharides at Low Dose Improve Liver Steatosis in a High-Fat Diet Mouse Model. Molecules 2017, 22, 1725. [Google Scholar] [CrossRef]
- Dai, Z.; Feng, S.; Liu, A.B.; Wang, H.; Zeng, X.; Yang, C.S. Protective effects of alpha-galacto-oligosaccharides against a high-fat/western-style diet-induced metabolic abnormalities in mice. Food Funct. 2019, 10, 3660–3670. [Google Scholar] [CrossRef]
- Ambade, A.; Lowe, P.; Kodys, K.; Catalano, D.; Gyongyosi, B.; Cho, Y.; Iracheta-Vellve, A.; Adejumo, A.; Saha, B.; Calenda, C.; et al. Pharmacological Inhibition of CCR2/5 Signaling Prevents and Reverses Alcohol-Induced Liver Damage, Steatosis, and Inflammation in Mice. Hepatology 2019, 69, 1105–1121. [Google Scholar] [CrossRef]
- Correia, M.A.; Kwon, D. Why Hepatic CYP2E1-Elevation by Itself Is Insufficient for Inciting NAFLD/NASH: Inferences from Two Genetic Knockout Mouse Models. Biology 2020, 9, 419. [Google Scholar] [CrossRef]
- Zeng, T.; Zhang, C.; Zhao, N.; Guan, M.; Xiao, M.; Yang, R.; Zhao, X.; Yu, L.; Zhu, Z.; Xie, K. Impairment of Akt activity by CYP2E1 mediated oxidative stress is involved in chronic ethanol-induced fatty liver. Redox Biol. 2018, 14, 295–304. [Google Scholar] [CrossRef]
- Abdelmegeed, M.; Banerjee, A.; Jang, S.; Yoo, S.; Yun, J.; Gonzalez, F.; Keshavarzian, A.; Song, B. CYP2E1 potentiates binge alcohol-induced gut leakiness, steatohepatitis, and apoptosis. Free Radic. Biol. Med. 2013, 65, 1238–1245. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Wu, D.; Wang, X.; Ward, S.; Cederbaum, A. Chronic alcohol-induced liver injury and oxidant stress are decreased in cytochrome P4502E1 knockout mice and restored in humanized cytochrome P4502E1 knock-in mice. Free Radic. Biol. Med. 2010, 49, 1406–1416. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Jiang, Z.; Li, X.; Zhang, X. Kaempferol’s Protective Effect on Ethanol-Induced Mouse Primary Hepatocytes Injury Involved in the Synchronous Inhibition of SP1, Hsp70 and CYP2E1. Am. J. Chin. Med. 2018, 46, 1093–1110. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Koh, H.; Joo, D.; Nedumaran, B.; Jeon, H.; Park, C.; Harris, R.; Kim, Y. Induction of SIRT1 by melatonin improves alcohol-mediated oxidative liver injury by disrupting the CRBN-YY1-CYP2E1 signaling pathway. J. Pineal Res. 2020, 68, e12638. [Google Scholar] [CrossRef]
- Xu, Y.; Chen, D.; Lin, X.; Zhao, Q.; Guo, J.; Chen, L.; Zhang, W.; Xiao, J.; Lian, G.; Peng, S.; et al. The LRP6 functional mutation rs2302685 contributes to individual susceptibility to alcoholic liver injury related to the Wnt/β-catenin-TCF1-CYP2E1 signaling pathway. Arch. Toxicol. 2019, 93, 1679–1695. [Google Scholar] [CrossRef]
- Dai, X.; Yan, X.; Wintergerst, K.; Cai, L.; Keller, B.; Tan, Y. Nrf2: Redox and Metabolic Regulator of Stem Cell State and Function. Trends Mol. Med. 2020, 26, 185–200. [Google Scholar] [CrossRef]
- Galicia-Moreno, M.; Lucano-Landeros, S.; Monroy-Ramirez, H.C.; Silva-Gomez, J.; Gutierrez-Cuevas, J.; Santos, A.; Armendariz-Borunda, J. Roles of Nrf2 in Liver Diseases: Molecular, Pharmacological, and Epigenetic Aspects. Antioxidants 2020, 9, 980. [Google Scholar] [CrossRef]
- Wang, Z.; Dou, X.; Li, S.; Zhang, X.; Sun, X.; Zhou, Z.; Song, Z. Nuclear factor (erythroid-derived 2)-like 2 activation-induced hepatic very-low-density lipoprotein receptor overexpression in response to oxidative stress contributes to alcoholic liver disease in mice. Hepatology 2014, 59, 1381–1392. [Google Scholar] [CrossRef]
- Albillos, A.; de Gottardi, A.; Rescigno, M. The gut-liver axis in liver disease: Pathophysiological basis for therapy. J. Hepatol. 2020, 72, 558–577. [Google Scholar] [CrossRef]
- Plaza-Diaz, J.; Solis-Urra, P.; Rodriguez-Rodriguez, F.; Olivares-Arancibia, J.; Navarro-Oliveros, M.; Abadia-Molina, F.; Alvarez-Mercado, A.I. The Gut Barrier, Intestinal Microbiota, and Liver Disease: Molecular Mechanisms and Strategies to Manage. Int. J. Mol. Sci. 2020, 21, 8351. [Google Scholar] [CrossRef]
- Kim, H.H.; Choi, S.E.; Jeong, W.I. Oxidative stress and glutamate excretion in alcoholic steatosis: Metabolic synapse between hepatocyte and stellate cell. Clin. Mol. Hepatol. 2020, 26, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, A.; Debelius, J.; Brenner, D.A.; Karin, M.; Loomba, R.; Schnabl, B.; Knight, R. Publisher Correction: The gut-liver axis and the intersection with the microbiome. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 785. [Google Scholar] [CrossRef] [PubMed]
- He, N.; Wang, Y.; Zhou, Z.; Liu, N.; Jung, S.; Lee, M.S.; Li, S. Preventive and Prebiotic Effect of alpha-Galacto-Oligosaccharide against Dextran Sodium Sulfate-Induced Colitis and Gut Microbiota Dysbiosis in Mice. J. Agric. Food Chem. 2021, 69, 9597–9607. [Google Scholar] [CrossRef] [PubMed]
- Lordan, C.; Thapa, D.; Ross, R.P.; Cotter, P.D. Potential for enriching next-generation health-promoting gut bacteria through prebiotics and other dietary components. Gut Microbes 2020, 11, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Liang, Q.; Balakrishnan, B.; Belobrajdic, D.P.; Feng, Q.J.; Zhang, W. Role of Dietary Nutrients in the Modulation of Gut Microbiota: A Narrative Review. Nutrients 2020, 12, 381. [Google Scholar] [CrossRef]
- van der Hee, B.; Wells, J.M. Microbial Regulation of Host Physiology by Short-chain Fatty Acids. Trends Microbiol. 2021, 29, 700–712. [Google Scholar] [CrossRef]










| Gene Name | Primer Sequence (5′→3′) |
|---|---|
| CYP2E1 | F: ACAGAGACCACCAGCACAAC |
| R: TCCTTGATGGCAGGGATTCG | |
| NLRP3 | F: GCATTTCCTCTCTAGCTGTTCCT |
| R: TTAGGCTTCGGTCCACACAGAAAG | |
| ASC | F: TACCTGGAGACCTACGGCG |
| R: TATAAAGTGCAGGCCCTGGTG | |
| Caspase-1 | F: ATCCGTTCCATGGGTGAAGG |
| R: CGTGCTGTCAGAGGTCTTGT | |
| β-actin | F: CATGTACGTTGCTATCCAGGC |
| R: CTCCTTAATGTCACGCACGAT |
| Gene Name | Primer Sequence (5′→3′) |
|---|---|
| CYP2E1 | F: CGTTGCCTTGCTTGTCTGGA |
| R: AAGAAAGGAATTGGGAAAGGTCC | |
| NLRP3 | F: CCACATCTGATTGTGTTAATGGCT |
| R: GGGCTTAGGTCCACACAGAA | |
| ASC | F: CCATCCTGGACGCTCTTGAA |
| R: GTGAGCTCCAAGCCATACGA | |
| Caspase-1 | F: CCGCGGTTGAATCCTTTTCAG |
| R: TGTGCGCATGTTTCTTTCCC | |
| TNF-α | F:GATCGGTCCCCAAAGGGATG |
| R: CCACTTGGTGGTTTGTGAGTG | |
| IL-1β | F: TGCCACCTTTTGACAGTGATG |
| R: TGATGTGCTGCTGCGAGATT | |
| F4/80 | F: TGACTCACCTTGTGGTCCTAA |
| R: CTTCCCAGAATCCAGTCTTTCC | |
| β-actin | F: AGCAAGCAGGAGTACGATGAG |
| R: GGTGTAAAACGCAGCTCAGTAA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, S.; Tan, Q.; Wen, B.; Bai, Y.; Che, Q.; Cao, H.; Guo, J.; Su, Z. Galacto-Oligosaccharide Alleviates Alcohol-Induced Liver Injury by Inhibiting Oxidative Stress and Inflammation. Metabolites 2022, 12, 867. https://doi.org/10.3390/metabo12090867
Zhou S, Tan Q, Wen B, Bai Y, Che Q, Cao H, Guo J, Su Z. Galacto-Oligosaccharide Alleviates Alcohol-Induced Liver Injury by Inhibiting Oxidative Stress and Inflammation. Metabolites. 2022; 12(9):867. https://doi.org/10.3390/metabo12090867
Chicago/Turabian StyleZhou, Shipeng, Qiuhua Tan, Bingjian Wen, Yan Bai, Qishi Che, Hua Cao, Jiao Guo, and Zhengquan Su. 2022. "Galacto-Oligosaccharide Alleviates Alcohol-Induced Liver Injury by Inhibiting Oxidative Stress and Inflammation" Metabolites 12, no. 9: 867. https://doi.org/10.3390/metabo12090867
APA StyleZhou, S., Tan, Q., Wen, B., Bai, Y., Che, Q., Cao, H., Guo, J., & Su, Z. (2022). Galacto-Oligosaccharide Alleviates Alcohol-Induced Liver Injury by Inhibiting Oxidative Stress and Inflammation. Metabolites, 12(9), 867. https://doi.org/10.3390/metabo12090867







