Exhaled Breath Analysis Using Selected Ion Flow Tube Mass Spectrometry and Disease Severity in Heart Failure
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Study Design
2.3. Exhaled Breath Collection
2.4. Volatile Organic Compounds Testing Using Mass Spectrometry
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics and Exhaled VOC Levels
3.2. Acute Changes in VOC Following Diuresis
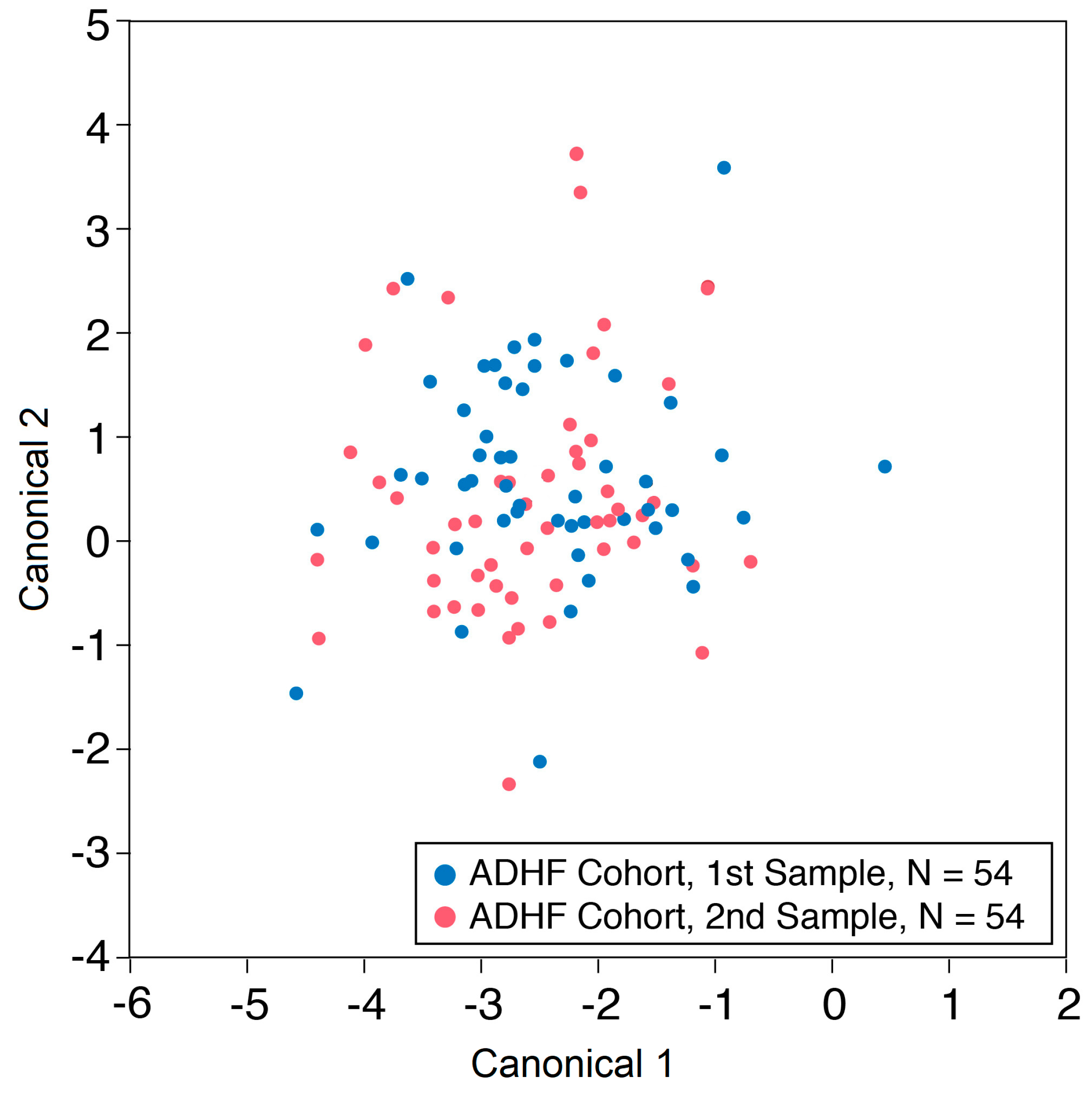
3.3. Acute Changes in VOC Following Exercise
3.4. Relationship between Prespecified VOCs and Hemodynamic and Cardiopulmonary Exercise Parameters
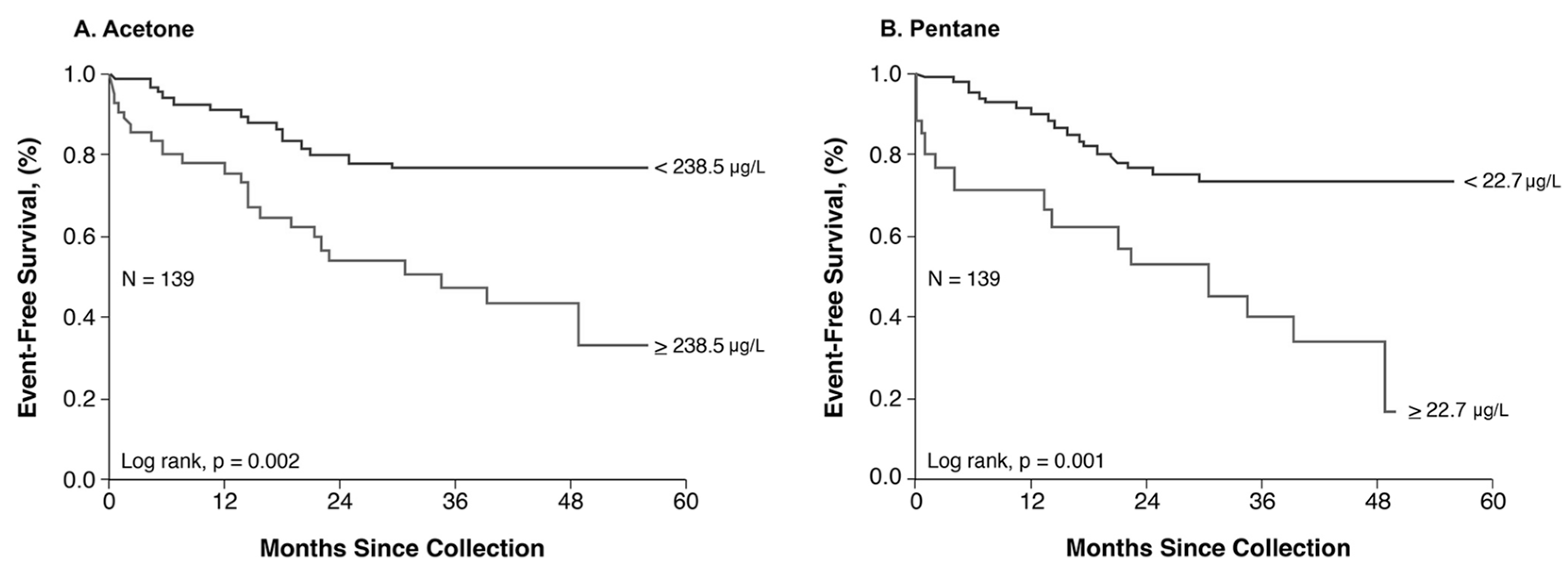
3.5. Relationship between Exhaled VOC and Long-Term Outcomes
4. Discussion
4.1. Key Findings
4.2. Exhaled Acetone and Pentane in Heart Failure
4.3. Clinical Implications
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Samara, M.A.; Tang, W.H.; Cikach, F., Jr.; Gul, Z.; Tranchito, L.; Paschke, K.M.; Viterna, J.; Wu, Y.; Laskowski, D.; Dweik, R.A. Single exhaled breath metabolomic analysis identifies unique breathprint in patients with acute decompensated heart failure. J. Am. Coll. Cardiol. 2013, 61, 1463–1464. [Google Scholar] [CrossRef] [PubMed]
- Biagini, D.; Pugliese, N.R.; Vivaldi, F.M.; Ghimenti, S.; Lenzi, A.; De Angelis, F.; Ripszam, M.; Bruderer, T.; Armenia, S.; Cappeli, F.; et al. Breath analysis combined with cardiopulmonary exercise testing and echocardiography for monitoring heart failure patients: The AEOLUS protocol. J. Breath. Res. 2023, 17. [Google Scholar] [CrossRef] [PubMed]
- Gouzi, F.; Ayache, D.; Hedon, C.; Molinari, N.; Vicet, A. Breath acetone concentration: Too heterogeneous to constitute a diagnosis or prognosis biomarker in heart failure? A systematic review and meta-analysis. J. Breath. Res. 2021, 16, 016001. [Google Scholar] [CrossRef] [PubMed]
- Marcondes-Braga, F.G.; Gioli-Pereira, L.; Bernardez-Pereira, S.; Batista, G.L.; Mangini, S.; Issa, V.S.; Fernandes, F.; Bocchi, E.A.; Ayub-Ferreira, S.M.; Mansur, A.J.; et al. Exhaled breath acetone for predicting cardiac and overall mortality in chronic heart failure patients. ESC Heart Fail. 2020, 7, 1744–1752. [Google Scholar] [CrossRef] [PubMed]
- Yokokawa, T.; Sato, T.; Suzuki, S.; Oikawa, M.; Yoshihisa, A.; Kobayashi, A.; Yamaki, T.; Kunii, H.; Nakazato, K.; Suzuki, H.; et al. Change of Exhaled Acetone Concentration Levels in Patients with Acute Decompensated Heart Failure. Int. Heart J. 2018, 59, 808–812. [Google Scholar] [CrossRef] [PubMed]
- Yokokawa, T.; Sato, T.; Suzuki, S.; Oikawa, M.; Yoshihisa, A.; Kobayashi, A.; Yamaki, T.; Kunii, H.; Nakazato, K.; Suzuki, H.; et al. Elevated exhaled acetone concentration in stage C heart failure patients with diabetes mellitus. BMC Cardiovasc. Disord. 2017, 17, 280. [Google Scholar] [CrossRef] [PubMed]
- Yokokawa, T.; Ichijo, Y.; Houtsuki, Y.; Matsumoto, Y.; Oikawa, M.; Yoshihisa, A.; Sugimoto, K.; Nakazato, K.; Suzuki, H.; Saitoh, S.I.; et al. Change of Exhaled Acetone Concentration in a Diabetic Patient with Acute Decompensated Heart Failure. Int. Heart J. 2017, 58, 828–830. [Google Scholar] [CrossRef] [PubMed]
- Biagini, D.; Lomonaco, T.; Ghimenti, S.; Bellagambi, F.G.; Onor, M.; Scali, M.C.; Barletta, V.; Marzilli, M.; Salvo, P.; Trivella, M.G.; et al. Determination of volatile organic compounds in exhaled breath of heart failure patients by needle trap micro-extraction coupled with gas chromatography-tandem mass spectrometry. J. Breath. Res. 2017, 11, 047110. [Google Scholar] [CrossRef] [PubMed]
- American Thoracic Society; American College of Chest Physicians. ATS/ACCP Statement on cardiopulmonary exercise testing. Am. J. Respir. Crit. Care Med. 2003, 167, 211–277. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.; Spanel, P. Selected ion flow tube mass spectrometry (SIFT-MS) for on-line trace gas analysis. Mass. Spectrom. Rev. 2005, 24, 661–700. [Google Scholar] [CrossRef] [PubMed]
- Yokokawa, T.; Sugano, Y.; Shimouchi, A.; Shibata, A.; Nakayama, T.; Ohara, T.; Jinno, N.; Kanzaki, H.; Anzai, T. A case of acute decompensated heart failure evaluated by series of exhaled acetone concentrations as noninvasive biomarker of heart failure severity. Int. J. Cardiol. 2016, 204, 112–113. [Google Scholar] [CrossRef] [PubMed]
- Yokokawa, T.; Sugano, Y.; Shimouchi, A.; Shibata, A.; Jinno, N.; Nagai, T.; Kanzaki, H.; Aiba, T.; Kusano, K.; Shirai, M.; et al. Exhaled Acetone Concentration Is Related to Hemodynamic Severity in Patients with Non-Ischemic Chronic Heart Failure. Circ. J. Off. J. Jpn. Circ. Society. 2016, 80, 1178–1186. [Google Scholar] [CrossRef] [PubMed]
- Marcondes-Braga, F.G.; Batista, G.L.; Gutz, I.G.; Saldiva, P.H.; Mangini, S.; Issa, V.S.; Ayub-Ferreira, S.M.; Bocchi, E.A.; Pereira, A.C.; Bacal, F. Impact of Exhaled Breath Acetone in the Prognosis of Patients with Heart Failure with Reduced Ejection Fraction (HFrEF). One Year of Clinical Follow-up. PLoS ONE 2016, 11, e0168790. [Google Scholar] [CrossRef] [PubMed]
- Kupari, M.; Lommi, J.; Ventila, M.; Karjalainen, U. Breath acetone in congestive heart failure. Am. J. Cardiol. 1995, 76, 1076–1078. [Google Scholar] [CrossRef] [PubMed]
- Marcondes-Braga, F.G.; Gutz, I.G.; Batista, G.L.; Saldiva, P.H.; Ayub-Ferreira, S.M.; Issa, V.S.; Mangini, S.; Bocchi, E.A.; Bacal, F. Exhaled acetone as a new biomaker of heart failure severity. Chest 2012, 142, 457–466. [Google Scholar] [CrossRef] [PubMed]
- Dryahina, K.; Španěl, P.; Pospíšilová, V.; Sovová, K.; Hrdlička, L.; Machková, N.; Lukáš, M.; Smith, D. Quantification of pentane in exhaled breath, a potential biomarker of bowel disease, using selected ion flow tube mass spectrometry. Rapid Commun. Mass. Spectrom. 2013, 27, 1983–1989. [Google Scholar] [CrossRef] [PubMed]
- Sobotka, P.A.; Brottman, M.D.; Weitz, Z.; Birnbaum, A.J.; Skosey, J.L.; Zarling, E.J. Elevated breath pentane in heart failure reduced by free radical scavenger. Free Radic. Biol. Med. 1993, 14, 643–647. [Google Scholar] [CrossRef] [PubMed]
- Kostikas, K.; Minas, M.; Papaioannou, A.I.; Papiris, S.; Dweik, R.A. Exhaled nitric oxide in asthma in adults: The end is the beginning? Curr. Med. Chem. 2011, 18, 1423–1431. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Bai, J.; Chen, W.N.; Ching, C.B. Metabolomic Profiling of Cellular Responses to Carvedilol Enantiomers in Vascular Smooth Muscle Cells. PLoS ONE 2010, 5, e15441. [Google Scholar] [CrossRef] [PubMed]


| Metabolite | Precursor | Product Mass (m/z) | Ions Measured | Branching Ratio |
|---|---|---|---|---|
| Acetone | H3O+ | 59 | C3H7O+ | 100% |
| NO+ | 88 | NO+*C3H6O | 100% | |
| Pentane | O2+ | 42 | C3H6+ | 40% |
| 72 | C5H12+ | 10% |
| Characteristics | Total Population (n = 55) | Weight Loss ≥4.5 kg (n = 29) | Weight Loss <4.5 kg (n = 26) | p-Value |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) | 65 (54, 70) | 65 (55, 69) | 64 (52, 70) | 0.717 |
| Male, n (%) | 37 (67.3) | 19 (65.5) | 18 (69.2) | 0.996 |
| BMI (kg/m2) | 30.6 (25.9, 35.9) | 33.8 (27.4, 37.3) | 29.8 (25.1, 33.4) | 0.079 |
| Comorbidities | ||||
| Hypertension, n (%) | 33 (60) | 18 (62.1) | 15 (57.7) | 0.956 |
| Diabetes mellitus, n (%) | 29 (52.7) | 17 (58.6) | 12 (46.2) | 0.513 |
| Coronary artery disease, n (%) | 31 (56.4) | 16 (55.2) | 15 (57.7) | 1.000 |
| Atrial fibrillation, n (%) | 32 (59.3) | 17 (60.7) | 15 (57.7) | 1.000 |
| COPD, n (%) | 11 (20) | 4 (13.8) | 7 (26.9) | 0.380 |
| Laboratory data | ||||
| NT-pro BNP (pg/mL) | 4226 (1726, 8627) | 4408 (1752, 5809) | 3018 (1654, 10,980) | 0.936 |
| eGFR (mL/min/1.73 m2) | 45 (29, 61) | 45 (32, 56) | 45 (24, 68) | 0.952 |
| Sodium (mmol/L) | 139 (136, 140) | 139 (136, 141) | 138 (135, 140) | 0.451 |
| AST (U/L) | 28 (19, 35) | 22 (17, 37) | 30 (23, 35) | 0.202 |
| ALT (U/L) | 21 (16, 30) | 18 (15, 28) | 24 (19, 30) | 0.062 |
| Echocardiographic data | ||||
| LVEF (%-units) | 36 (20, 50) | 35 (19, 48) | 38 (24, 57) | 0.367 |
| LVIDd (mm) | 52.5 (45, 62.2) | 56 (46.5, 65) | 51 (44.2, 61) | 0.272 |
| Hemodynamic data | ||||
| PCWP (mmHg) | 27 (24, 30) | 30 (30, 34) | 24 (22, 25) | 0.004 * |
| RAP (mmHg) | 16 (12, 21) | 19 (14, 22) | 15 (11, 18) | 0.161 |
| Medications | ||||
| ACE-i/ARB, n (%) | 25 (49) | 15 (53.6) | 10 (43.5) | 0.663 |
| β-blocker, n (%) | 44 (86.3) | 27 (96.4) | 17 (73.9) | 0.055 |
| Statin, n (%) | 32 (64) | 20 (74.1) | 12 (52.2) | 0.189 |
| Loop diuretic, n (%) | 47 (92.2) | 26 (92.9) | 21 (91.3) | 1.000 |
| Aspirin, n (%) | 36 (75) | 22 (81.5) | 14 (66.7) | 0.401 |
| Insulin, n (%) | 15 (29.4) | 9 (32.1) | 6 (26.1) | 0.870 |
| Characteristics | Total Population (n = 51) | VE/VCO2 ≥ 35.5 (n = 24) | VE/VCO2 < 35.5 (n = 27) | p-Value |
|---|---|---|---|---|
| Age (years) | 59 (50, 64) | 62 (58, 66) | 56 (46, 60) | 0.007 * |
| Male, n (%) | 36 (70.6) | 19 (79.2) | 17 (63) | 0.337 |
| BMI (kg/m2) | 29.7 (27.1, 34.1) | 30 (27.3, 33.7) | 29.2 (26.9, 34.1) | 0.928 |
| Hypertension, n (%) | 30 (60) | 17 (70.8) | 13 (50) | 0.225 |
| Diabetes mellitus, n (%) | 12 (24) | 8 (33.3) | 4 (15.4) | 0.249 |
| Coronary artery disease, n (%) | 20 (40) | 13 (54.2) | 7 (26.9) | 0.094 |
| Atrial fibrillation, n (%) | 16 (32) | 10 (41.7) | 6 (23.1) | 0.269 |
| COPD, n (%) | 3 (6) | 1 (4.2) | 2 (7.7) | 1 |
| LVEF (%-units) | 32 (25, 60) | 25 (25, 44) | 51 (23, 64) | 0.359 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, W.H.W.; Tranchito, L.; Albert, C.; Gul, Z.G.; Cikach, F.S., Jr.; Grove, D.; Wu, Y.; Dweik, R.A. Exhaled Breath Analysis Using Selected Ion Flow Tube Mass Spectrometry and Disease Severity in Heart Failure. Metabolites 2023, 13, 1049. https://doi.org/10.3390/metabo13101049
Tang WHW, Tranchito L, Albert C, Gul ZG, Cikach FS Jr., Grove D, Wu Y, Dweik RA. Exhaled Breath Analysis Using Selected Ion Flow Tube Mass Spectrometry and Disease Severity in Heart Failure. Metabolites. 2023; 13(10):1049. https://doi.org/10.3390/metabo13101049
Chicago/Turabian StyleTang, Wai Hong Wilson, Lily Tranchito, Chonyang Albert, Zeynep G. Gul, Frank S. Cikach, Jr., David Grove, Yuping Wu, and Raed A. Dweik. 2023. "Exhaled Breath Analysis Using Selected Ion Flow Tube Mass Spectrometry and Disease Severity in Heart Failure" Metabolites 13, no. 10: 1049. https://doi.org/10.3390/metabo13101049
APA StyleTang, W. H. W., Tranchito, L., Albert, C., Gul, Z. G., Cikach, F. S., Jr., Grove, D., Wu, Y., & Dweik, R. A. (2023). Exhaled Breath Analysis Using Selected Ion Flow Tube Mass Spectrometry and Disease Severity in Heart Failure. Metabolites, 13(10), 1049. https://doi.org/10.3390/metabo13101049






