The Causal Effect of Urate Level on Female Infertility: A Mendelian Randomization Study
Abstract
1. Introduction
2. Methods
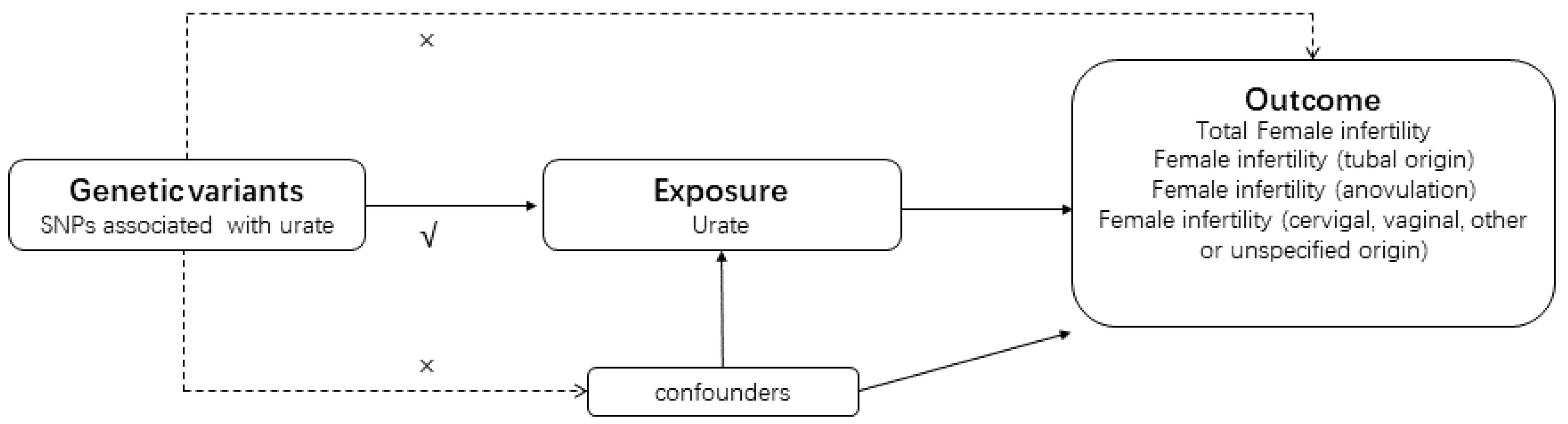
2.1. Study Design Overview
2.2. Exposure Data Sources and IV Selection
2.3. Outcome Data Sources and IV Selection
2.4. MR Analysis
2.5. Ethical Considerations and Informed Consent
3. Results
3.1. Association between Serum Urate Levels and Female Infertility
3.2. Association between Serum Urate Levels and Cause-Specific Infertility
3.3. Multivariate MR Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, Y.; Fu, Y.; Ghazi, P.; Gao, Q.; Tian, T.; Kong, F.; Zhan, S.; Liu, C.; Bloom, D.E.; Qiao, J. Prevalence of intimate partner violence against infertile women in low-income and middle-income countries: A systematic review and meta-analysis. Lancet Glob. Health 2022, 10, e820–e830. [Google Scholar] [CrossRef] [PubMed]
- Hart, V.A. Infertility and the role of psychotherapy. Issues Ment. Health Nurs. 2002, 23, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.; Velez, M.P.; Dayan, N. Infertility, Infertility Treatment, and Cardiovascular Disease: An Overview. Can. J. Cardiol. 2021, 37, 1959–1968. [Google Scholar] [CrossRef] [PubMed]
- Inhorn, M.C.; Patrizio, P. Infertility around the globe: New thinking on gender, reproductive technologies and global movements in the 21st century. Hum. Reprod. Update 2015, 21, 411–426. [Google Scholar] [CrossRef]
- Hammarberg, K.; Kirkman, M. Infertility in resource-constrained settings: Moving towards amelioration. Reprod. Biomed. Online 2013, 26, 189–195. [Google Scholar] [CrossRef]
- Vander Borght, M.; Wyns, C. Fertility and infertility: Definition and epidemiology. Clin. Biochem. 2018, 62, 2–10. [Google Scholar] [CrossRef]
- Simpson, J.L. Molecular approach to common causes of female infertility. Best. Pract. Res. Clin. Obstet. Gynaecol. 2002, 16, 685–702. [Google Scholar] [CrossRef]
- Carson, S.A.; Kallen, A.N. Diagnosis and Management of Infertility: A Review. JAMA 2021, 326, 65–76. [Google Scholar] [CrossRef]
- Ray, A.; Shah, A.; Gudi, A.; Homburg, R. Unexplained infertility: An update and review of practice. Reprod. Biomed. Online 2012, 24, 591–602. [Google Scholar] [CrossRef]
- Hoeger, K.M.; Dokras, A.; Piltonen, T. Update on PCOS: Consequences, Challenges, and Guiding Treatment. J. Clin. Endocrinol. Metab. 2021, 106, e1071–e1083. [Google Scholar] [CrossRef]
- Crawley, W.T.; Jungels, C.G.; Stenmark, K.R.; Fini, M.A. U-shaped association of uric acid to overall-cause mortality and its impact on clinical management of hyperuricemia. Redox Biol. 2022, 51, 102271. [Google Scholar] [CrossRef] [PubMed]
- Gherghina, M.E.; Peride, I.; Tiglis, M.; Neagu, T.P.; Niculae, A.; Checherita, I.A. Uric Acid and Oxidative Stress-Relationship with Cardiovascular, Metabolic, and Renal Impairment. Int. J. Mol. Sci. 2022, 23, 3188. [Google Scholar] [CrossRef]
- Maiuolo, J.; Oppedisano, F.; Gratteri, S.; Muscoli, C.; Mollace, V. Regulation of uric acid metabolism and excretion. Int. J. Cardiol. 2016, 213, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Fathallah-Shaykh, S.A.; Cramer, M.T. Uric acid and the kidney. Pediatr. Nephrol. 2014, 29, 999–1008. [Google Scholar] [CrossRef] [PubMed]
- Schachter, M. Uric acid and hypertension. Curr. Pharm. Des. 2005, 11, 4139–4143. [Google Scholar] [CrossRef] [PubMed]
- Mumford, S.L.; Dasharathy, S.S.; Pollack, A.Z.; Perkins, N.J.; Mattison, D.R.; Cole, S.R.; Wactawski-Wende, J.; Schisterman, E.F. Serum uric acid in relation to endogenous reproductive hormones during the menstrual cycle: Findings from the BioCycle study. Hum. Reprod. 2013, 28, 1853–1862. [Google Scholar] [CrossRef]
- Lavy, G.; Behrman, H.R.; Polan, M.L. Purine levels and metabolism in human follicular fluid. Hum. Reprod. 1990, 5, 529–532. [Google Scholar] [CrossRef]
- Wen, X.; Perrett, D.; Jones, N.; Tozer, A.J.; Docherty, S.M.; Iles, R.K. High follicular fluid adenosine levels may be pivotal in the metabolism and recycling of adenosine nucleotides in the human follicle. Metabolism 2010, 59, 1145–1155. [Google Scholar] [CrossRef]
- Glantzounis, G.K.; Tsimoyiannis, E.C.; Kappas, A.M.; Galaris, D.A. Uric acid and oxidative stress. Curr. Pharm. Des. 2005, 11, 4145–4151. [Google Scholar] [CrossRef]
- Lanaspa, M.A.; Sanchez-Lozada, L.G.; Choi, Y.J.; Cicerchi, C.; Kanbay, M.; Roncal-Jimenez, C.A.; Ishimoto, T.; Li, N.; Marek, G.; Duranay, M.; et al. Uric acid induces hepatic steatosis by generation of mitochondrial oxidative stress: Potential role in fructose-dependent and -independent fatty liver. J. Biol. Chem. 2012, 287, 40732–40744. [Google Scholar] [CrossRef]
- Ghaemi-Oskouie, F.; Shi, Y. The role of uric acid as an endogenous danger signal in immunity and inflammation. Curr. Rheumatol. Rep. 2011, 13, 160–166. [Google Scholar] [CrossRef]
- Al-Jefout, M.; Alnawaiseh, N.; Al-Qtaitat, A. Insulin resistance and obesity among infertile women with different polycystic ovary syndrome phenotypes. Sci. Rep. 2017, 7, 5339. [Google Scholar] [CrossRef]
- Zhu, J.L.; Chen, Z.; Feng, W.J.; Long, S.L.; Mo, Z.C. Sex hormone-binding globulin and polycystic ovary syndrome. Clin. Chim. Acta 2019, 499, 142–148. [Google Scholar] [CrossRef]
- Jonard, S.; Dewailly, D. The follicular excess in polycystic ovaries, due to intra-ovarian hyperandrogenism, may be the main culprit for the follicular arrest. Hum. Reprod. Update 2004, 10, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Berga, S.L.; Zou, W.; Taylor, R.N. Interleukin-1β inhibits estrogen receptor-α, progesterone receptors A and B and biomarkers of human endometrial stromal cell differentiation: Implications for endometriosis. Mol. Hum. Reprod. 2019, 25, 625–637. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Bai, W.; Jiang, B.; Wang, Z.; Wang, X.; Sun, Y.; Liu, F.; Cui, G.; Song, X.; Li, J.; et al. Effects of a ketogenic diet in women with PCOS with different uric acid concentrations: A prospective cohort study. Reprod. Biomed. Online 2022, 45, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.N.; Luo, H.; Che, X.; Peng, H.; Li, M.; Liu, K.X. Uric acid metabolism in polycystic ovary syndrome. Clin. Chim. Acta 2021, 517, 74–80. [Google Scholar] [CrossRef]
- Lambert, S.; Santulli, P.; Chouzenoux, S.; Marcellin, L.; Borghese, B.; de Ziegler, D.; Batteux, F.; Chapron, C. Endometriosis: Increasing concentrations of serum interleukin-1β and interleukin-1sRII is associated with the deep form of this pathology. J. Gynecol. Obstet. Biol. Reprod. 2014, 43, 735–743. [Google Scholar] [CrossRef]
- Hong, X.; Zhao, F.; Wang, W.; Wu, J.; Zhu, X.; Wang, B. Elevated serum uric acid is associated with infertility in women living in America. Sci. Rep. 2023, 13, 7687. [Google Scholar] [CrossRef]
- Bowden, J.; Holmes, M.V. Meta-analysis and Mendelian randomization: A review. Res. Synth. Methods 2019, 10, 486–496. [Google Scholar] [CrossRef]
- Burgess, S.; Small, D.S.; Thompson, S.G. A review of instrumental variable estimators for Mendelian randomization. Stat. Methods Med. Res. 2017, 26, 2333–2355. [Google Scholar] [CrossRef] [PubMed]
- Hartwig, F.P.; Davies, N.M.; Hemani, G.; Davey Smith, G. Two-sample Mendelian randomization: Avoiding the downsides of a powerful, widely applicable but potentially fallible technique. Int. J. Epidemiol. 2016, 45, 1717–1726. [Google Scholar] [CrossRef]
- Tin, A.; Marten, J.; Halperin Kuhns, V.L.; Li, Y.; Wuttke, M.; Kirsten, H.; Sieber, K.B.; Qiu, C.; Gorski, M.; Yu, Z.; et al. Target genes, variants, tissues and transcriptional pathways influencing human serum urate levels. Nat. Genet. 2019, 51, 1459–1474. [Google Scholar] [CrossRef] [PubMed]
- Huffman, J.E.; Albrecht, E.; Teumer, A.; Mangino, M.; Kapur, K.; Johnson, T.; Kutalik, Z.; Pirastu, N.; Pistis, G.; Lopez, L.M.; et al. Modulation of genetic associations with serum urate levels by body-mass-index in humans. PLoS ONE 2015, 10, e0119752. [Google Scholar] [CrossRef]
- Release, T.F.C.F.D.o.R. Available online: https://finngen.gitbook.io/documentation/ (accessed on 21 July 2024).
- Yavorska, O.O.; Burgess, S. MendelianRandomization: An R package for performing Mendelian randomization analyses using summarized data. Int. J. Epidemiol. 2017, 46, 1734–1739. [Google Scholar] [CrossRef] [PubMed]
- Burgess, S.; Butterworth, A.; Thompson, S.G. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet. Epidemiol. 2013, 37, 658–665. [Google Scholar] [CrossRef]
- Bowden, J.; Davey Smith, G.; Burgess, S. Mendelian randomization with invalid instruments: Effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 2015, 44, 512–525. [Google Scholar] [CrossRef]
- Burgess, S.; Bowden, J.; Fall, T.; Ingelsson, E.; Thompson, S.G. Sensitivity Analyses for Robust Causal Inference from Mendelian Randomization Analyses with Multiple Genetic Variants. Epidemiology 2017, 28, 30–42. [Google Scholar] [CrossRef]
- Bowden, J.; Del Greco, M.F.; Minelli, C.; Davey Smith, G.; Sheehan, N.A.; Thompson, J.R. Assessing the suitability of summary data for two-sample Mendelian randomization analyses using MR-Egger regression: The role of the I2 statistic. Int. J. Epidemiol. 2016, 45, 1961–1974. [Google Scholar] [CrossRef]
- Verbanck, M.; Chen, C.Y.; Neale, B.; Do, R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat. Genet. 2018, 50, 693–698. [Google Scholar] [CrossRef]
- Abuja, P.M. Ascorbate prevents prooxidant effects of urate in oxidation of human low density lipoprotein. FEBS Lett. 1999, 446, 305–308. [Google Scholar] [CrossRef] [PubMed]
- Battelli, M.G.; Bortolotti, M.; Polito, L.; Bolognesi, A. The role of xanthine oxidoreductase and uric acid in metabolic syndrome. Biochim. Biophys. Acta Mol. Basis Dis. 2018, 1864, 2557–2565. [Google Scholar] [CrossRef] [PubMed]
- Martinon, F.; Pétrilli, V.; Mayor, A.; Tardivel, A.; Tschopp, J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature 2006, 440, 237–241. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Xu, W.; Yang, H.; Mu, L. Uric acid participating in female reproductive disorders: A review. Reprod. Biol. Endocrinol. 2021, 19, 65. [Google Scholar] [CrossRef]
- Mu, L.; Pan, J.; Yang, L.; Chen, Q.; Chen, Y.; Teng, Y.; Wang, P.; Tang, R.; Huang, X.; Chen, X.; et al. Association between the prevalence of hyperuricemia and reproductive hormones in polycystic ovary syndrome. Reprod. Biol. Endocrinol. 2018, 16, 104. [Google Scholar] [CrossRef]
- Kokot, I.; Piwowar, A.; Jędryka, M.; Kratz, E.M. Is There a Balance in Oxidative-Antioxidant Status in Blood Serum of Patients with Advanced Endometriosis? Antioxidants 2021, 10, 1097. [Google Scholar] [CrossRef]
- Luo, C.; Cheng, H.; He, X.; Tan, X.; Huang, X. Association between serum uric acid and female infertility: A cross-sectional study of National Health and Nutrition Examination Survey (NHANES) 2013–2018. BMC Womens Health 2023, 23, 224. [Google Scholar] [CrossRef]
- Tan, Z.; Shen, J.; Huang, Y.; Li, J.; Ding, M.; Sun, A.; Hong, J.; Yang, Y.; He, S.; Zhu, X.; et al. Decoding connections in the European population: Serum uric acid, sex hormone-binding globulin, total testosterone, estradiol, and female infertility—Advanced bidirectional and mediative Mendelian randomization. Front. Endocrinol. 2024, 15, 1398600. [Google Scholar] [CrossRef]
| Outcomes | No. of SNPs | Method | Beta (SE) | OR (95% CI) | p Value | Heterogeneity Test | Pleiotropy Test | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Cochran’s Q (I2) | p Value | MR Egger | MR-Presso Global-Test | |||||||
| Egger Intercept | p Value | p Value | ||||||||
| Total female infertility | 93 | Inverse variance weighted | 0.13 (0.05) | 1.14 (1.04, 1.25) | 0.009 | 112.45 | 0.063 | |||
| 93 | MR Egger | 0.18 (0.07) | 1.25 (1.05, 1.36) | 0.006 | 113.65 | 0.063 | −0.004 | 0.33 | 0.061 | |
| 93 | Weighted median | 0.17 (0.06) | 1.19 (1.04, 1.34) | 0.005 | ||||||
| 93 | Weighted model | 0.16 (0.06) | 1.17 (1.05, 1.31) | 0.53 | ||||||
| Female infertility (tubal origin) | 93 | Inverse variance weighted | 0.10 (0.11) | 1.00 (0.80, 1.24) | 0.98 | 87.31 | 0.59 | |||
| 93 | MR Egger | 0.04 (0.17) | 1.14 (0.82, 1.57) | 0.44 | 88.51 | 0.58 | −0.001 | 0.28 | 0.057 | |
| 93 | Weighted median | 0.06 (0.17) | 1.06 (0.76, 1.47) | 0.73 | ||||||
| 93 | Weighted model | 0.03 (0.15) | 1.01 (0.74, 1.37) | 0.95 | ||||||
| Female infertility (anovulation) | 93 | Inverse variance weighted | 0.09 (0.10) | 1.10 (0.89, 1.35) | 0.37 | 112.45 | 0.06 | |||
| 93 | MR Egger | 0.14 (0.15) | 1.16 (0.86, 1.56) | 0.34 | 113.65 | 0.06 | −0.004 | 0.33 | 0.085 | |
| 93 | Weighted median | 0.10 (0.15) | 1.11 (0.83, 1.49) | 0.49 | ||||||
| 93 | Weighted model | 0.13 (0.12) | 1.14 (0.89, 1.45) | 0.30 | ||||||
| Female infertility (cervigal, vaginal, other, or unspecified origin) | 93 | Inverse variance weighted | 0.15 (0.04) | 1.16 (1.06, 1.26) | 0.001 | 87.07 | 0.60 | |||
| 93 | MR Egger | 0.18 (0.06) | 1.19 (1.05, 1.35) | 0.007 | 87.46 | 0.61 | −0.002 | 0.54 | 0.076 | |
| 93 | Weighted median | 0.18 (0.07) | 1.19 (1.05, 1.35) | 0.007 | ||||||
| 93 | Weighted model | 0.15 (0.06) | 1.17 (1.04, 1.31) | 0.008 | ||||||
| Outcomes | Exposures | Beta | SE | OR (95% CI) | p Value |
|---|---|---|---|---|---|
| Total female infertility | Urate levels | 0.120 | 0.040 | 1.13 (1.04, 1.22) | 0.003 |
| Body mass index | −0.086 | 0.086 | 0.92 (0.78, 1.09) | 0.32 | |
| Female infertility (tubal origin) | Urate levels | 0.038 | 0.103 | 1.04 (0.85, 1.27) | 0.71 |
| Body mass index | −0.076 | 0.219 | 0.93 (0.60, 1.43) | 0.73 | |
| Female infertility (anovulation) | Urate levels | 0.196 | 0.092 | 1.22 (1.02, 1.46) | 0.06 |
| Body mass index | 0.111 | 0.196 | 1.12 (0.76, 1.64) | 0.57 | |
| Female infertility (cervical, vaginal, other or unspecified origin) | Urate levels | 0.117 | 0.042 | 1.12 (1.04, 1.22) | 0.006 |
| Body mass index | −0.164 | 0.091 | 0.85 (0.71, 1.02) | 0.072 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, J.; Shen, T.; Guan, Y.; Jiang, Y.; Xu, X. The Causal Effect of Urate Level on Female Infertility: A Mendelian Randomization Study. Metabolites 2024, 14, 516. https://doi.org/10.3390/metabo14100516
Sun J, Shen T, Guan Y, Jiang Y, Xu X. The Causal Effect of Urate Level on Female Infertility: A Mendelian Randomization Study. Metabolites. 2024; 14(10):516. https://doi.org/10.3390/metabo14100516
Chicago/Turabian StyleSun, Jiawei, Ting Shen, Yining Guan, Yixin Jiang, and Xiaoling Xu. 2024. "The Causal Effect of Urate Level on Female Infertility: A Mendelian Randomization Study" Metabolites 14, no. 10: 516. https://doi.org/10.3390/metabo14100516
APA StyleSun, J., Shen, T., Guan, Y., Jiang, Y., & Xu, X. (2024). The Causal Effect of Urate Level on Female Infertility: A Mendelian Randomization Study. Metabolites, 14(10), 516. https://doi.org/10.3390/metabo14100516






