Analysis of Serum Exosome Metabolites Identifies Potential Biomarkers for Human Hepatocellular Carcinoma
Abstract
:1. Introduction
2. Materials and Methods
2.1. Collection of Clinical Samples
2.2. Exosome Isolation and Characterization
2.3. Extraction of Exosome Metabolites
2.4. UPLC-Q-TOF-MS/MS Analysis
2.5. Data Analysis
3. Results
3.1. Reliability of the Analytical Method
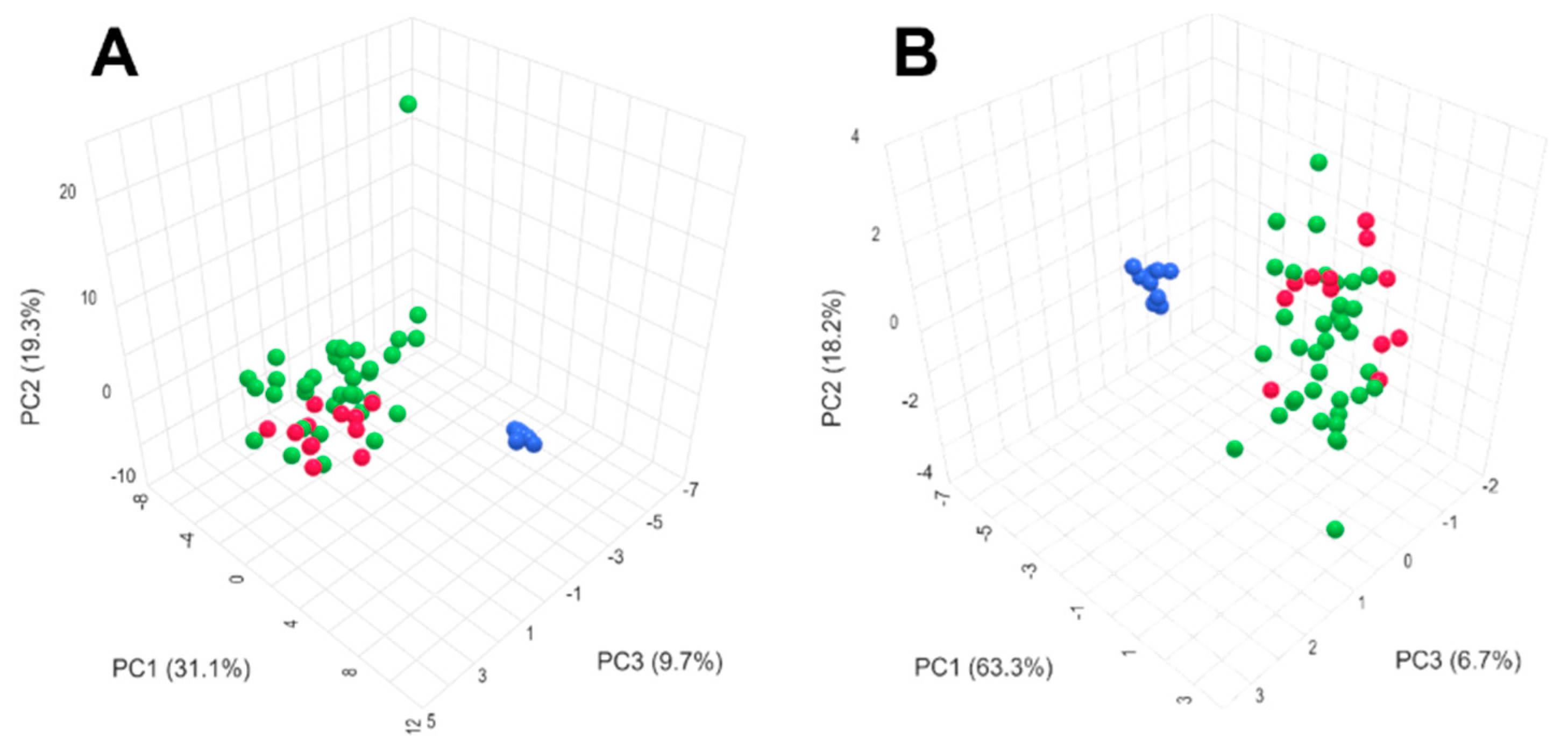
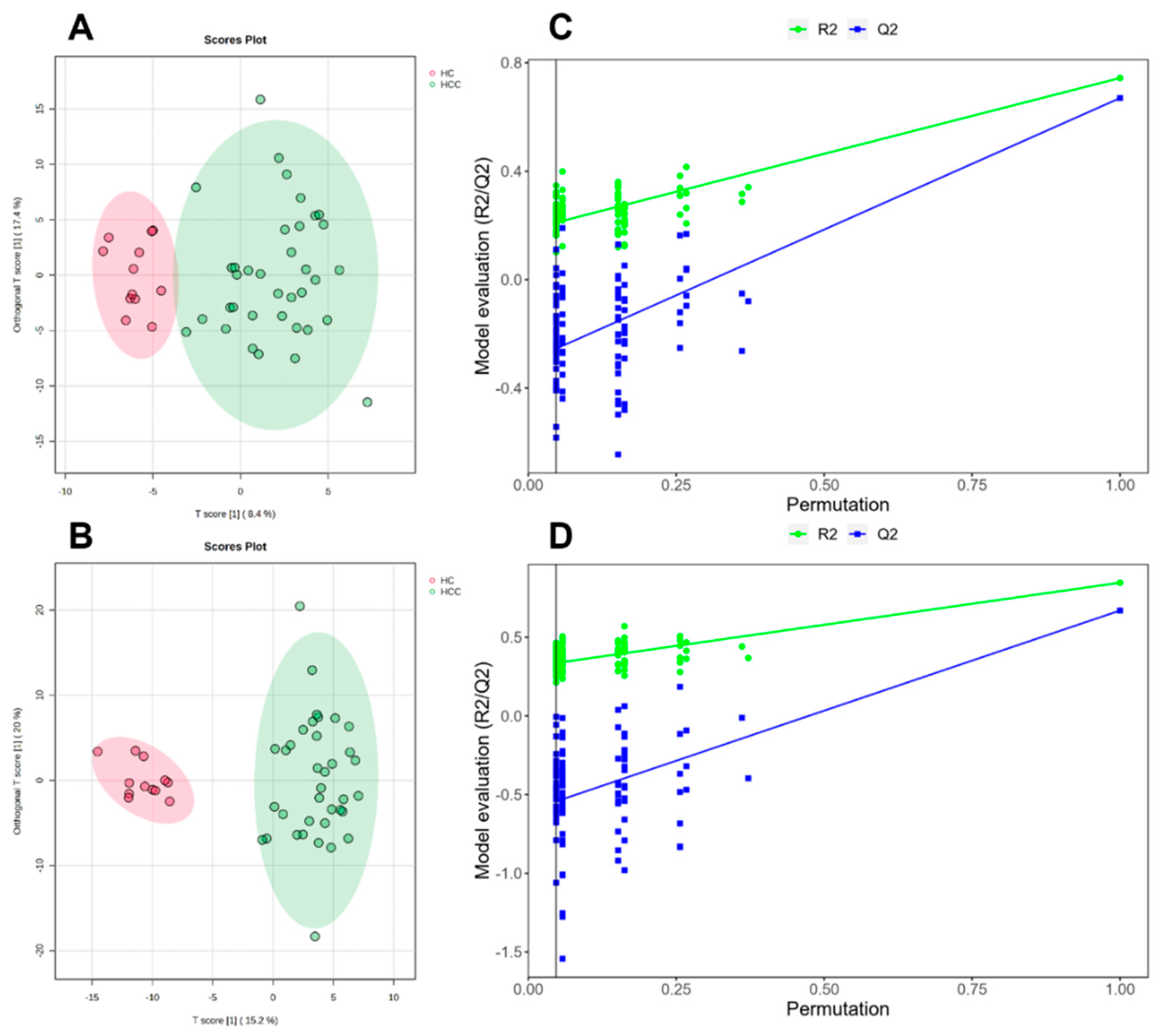
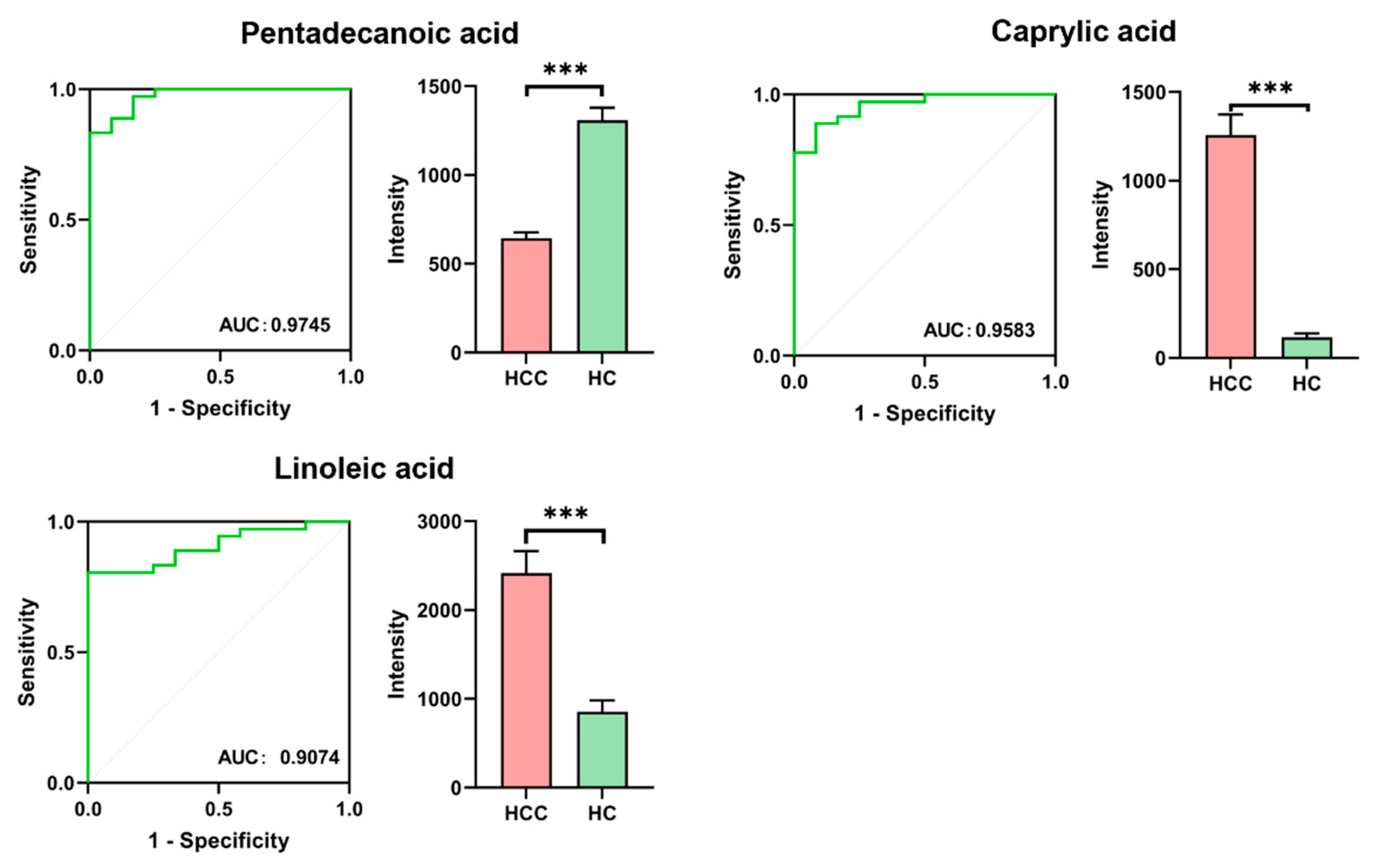
3.2. Differential Metabolite Screening
3.3. Metabolic Pathway Analysis
4. Discussion
4.1. Arachidonic Acid Metabolism
4.2. Linoleic Acid and Unsaturated Fatty Acid Metabolism
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McGlynn, K.A.; Petrick, J.L.; London, W.T. Global epidemiology of hepatocellular carcinoma: An emphasis on demographic and regional variability. Clin. Liver Dis. 2015, 19, 223–238. [Google Scholar] [CrossRef]
- Sakamoto, M. Early HCC: Diagnosis and molecular markers. J. Gastroenterol. 2009, 44 (Suppl. S19), 108–111. [Google Scholar] [CrossRef]
- Wolf, E.; Rich, N.E.; Marrero, J.A.; Parikh, N.D.; Singal, A.G. Use of Hepatocellular Carcinoma Surveillance in Patients with Cirrhosis: A Systematic Review and Meta-Analysis. Hepatology 2021, 73, 713–725. [Google Scholar] [CrossRef]
- Tzartzeva, K.; Obi, J.; Rich, N.E.; Parikh, N.D.; Marrero, J.A.; Yopp, A.; Waljee, A.K.; Singal, A.G. Surveillance Imaging and Alpha Fetoprotein for Early Detection of Hepatocellular Carcinoma in Patients with Cirrhosis: A Meta-analysis. Gastroenterology 2018, 154, 1706–1718.e1. [Google Scholar] [CrossRef] [PubMed]
- Marrero, J.A. Surveillance for Hepatocellular Carcinoma. Clin. Liver Dis. 2020, 24, 611–621. [Google Scholar] [CrossRef]
- Doyle, L.M.; Wang, M.Z. Overview of Extracellular Vesicles, Their Origin, Composition, Purpose, and Methods for Exosome Isolation and Analysis. Cells 2019, 8, 727. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Deep, G. Exosomes in hypoxia-induced remodeling of the tumor microenvironment. Cancer Lett. 2020, 488, 1–8. [Google Scholar] [CrossRef]
- Tao, L.; Zhou, J.; Yuan, C.; Zhang, L.; Li, D.; Si, D.; Xiu, D.; Zhong, L. Metabolomics identifies serum and exosomes metabolite markers of pancreatic cancer. Metabolomics 2019, 15, 86. [Google Scholar] [CrossRef]
- Cheng, L.; Zhang, K.; Qing, Y.; Li, D.; Cui, M.; Jin, P.; Xu, T. Proteomic and lipidomic analysis of exosomes derived from ovarian cancer cells and ovarian surface epithelial cells. J. Ovarian Res. 2020, 13, 9. [Google Scholar] [CrossRef] [PubMed]
- Scavo, M.P.; Depalo, N.; Tutino, V.; De Nunzio, V.; Ingrosso, C.; Rizzi, F.; Notarnicola, M.; Curri, M.L.; Giannelli, G. Exosomes for Diagnosis and Therapy in Gastrointestinal Cancers. Int. J. Mol. Sci. 2020, 21, 367. [Google Scholar] [CrossRef]
- Fiehn, O. Metabolomics—The link between genotypes and phenotypes. Plant Mol. Biol. 2002, 48, 155–171. [Google Scholar] [CrossRef]
- Schrimpe-Rutledge, A.C.; Codreanu, S.G.; Sherrod, S.D.; McLean, J.A. Untargeted Metabolomics Strategies—Challenges and Emerging Directions. J. Am. Soc. Mass. Spectrom. 2016, 27, 1897–1905. [Google Scholar] [CrossRef]
- Nassar, A.F.; Wu, T.; Nassar, S.F.; Wisnewski, A.V. UPLC-MS for metabolomics: A giant step forward in support of pharmaceutical research. Drug Discov. Today 2017, 22, 463–470. [Google Scholar] [CrossRef]
- Zhang, J.; Tang, C.; Oberly, P.J.; Minnigh, M.B.; Achilles, S.L.; Poloyac, S.M. A sensitive and robust UPLC-MS/MS method for quantitation of estrogens and progestogens in human serum. Contraception 2019, 99, 244–250. [Google Scholar] [CrossRef]
- Jiang, T.; Zhu, A.S.; Yang, C.Q.; Xu, C.; Yang, D.; Lou, Z.; Zhang, G. Cytochrome P450 2A6 is associated with macrophage polarization and is a potential biomarker for hepatocellular carcinoma. FEBS Open Bio 2021, 11, 670–683. [Google Scholar] [CrossRef]
- Zeldin, D.C. Epoxygenase pathways of arachidonic acid metabolism. J. Biol. Chem. 2001, 276, 36059–36062. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Tang, Q.; Zhao, L.; Zhang, Q.; Wu, Y.; Hu, H.; Liu, L.; Liu, X.; Zhu, Y.; Guo, A.; et al. Time serial transcriptome reveals Cyp2c29 as a key gene in hepatocellular carcinoma development. Cancer Biol. Med. 2020, 17, 401–417. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, L.; Wang, H.; Xiao, F.; Ning, Q. Epoxyeicosatrienoic acids alleviate methionine-choline-deficient diet-induced non-alcoholic steatohepatitis in mice. Scand. J. Immunol. 2019, 90, e12791. [Google Scholar] [CrossRef] [PubMed]
- Panigrahy, D.; Kalish, B.T.; Huang, S.; Bielenberg, D.R.; Le, H.D.; Yang, J.; Edin, M.L.; Lee, C.R.; Benny, O.; Mudge, D.K.; et al. Epoxyeicosanoids promote organ and tissue regeneration. Proc. Natl. Acad. Sci. USA 2013, 110, 13528–13533. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Kodani, S.; Hammock, B.D. Stabilized epoxygenated fatty acids regulate inflammation, pain, angiogenesis and cancer. Prog. Lipid Res. 2014, 53, 108–123. [Google Scholar] [CrossRef]
- Panigrahy, D.; Edin, M.L.; Lee, C.R.; Huang, S.; Bielenberg, D.R.; Butterfield, C.E.; Barnés, C.M.; Mammoto, A.; Mammoto, T.; Luria, A.; et al. Epoxyeicosanoids stimulate multiorgan metastasis and tumor dormancy escape in mice. J. Clin. Investig. 2012, 122, 178–191. [Google Scholar] [CrossRef]
- Ma, J.; Zhang, L.; Zhang, J.; Liu, M.; Wei, L.; Shen, T.; Ma, C.; Wang, Y.; Chen, Y.; Zhu, D. 15-lipoxygenase-1/15-hydroxyeicosatetraenoic acid promotes hepatocellular cancer cells growth through protein kinase B and heat shock protein 90 complex activation. Int. J. Biochem. Cell Biol. 2013, 45, 1031–1041. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Kesarwala, A.H.; Eggert, T.; Medina-Echeverz, J.; Kleiner, D.E.; Jin, P.; Stroncek, D.F.; Terabe, M.; Kapoor, V.; ElGindi, M.; et al. NAFLD causes selective CD4(+) T lymphocyte loss and promotes hepatocarcinogenesis. Nature 2016, 531, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Muir, K.; Hazim, A.; He, Y.; Peyressatre, M.; Kim, D.-Y.; Song, X.; Beretta, L. Proteomic and lipidomic signatures of lipid metabolism in NASH-associated hepatocellular carcinoma. Cancer Res. 2013, 73, 4722–4731. [Google Scholar] [CrossRef]
- Brown, Z.J.; Fu, Q.; Ma, C.; Kruhlak, M.; Zhang, H.; Luo, J.; Heinrich, B.; Yu, S.J.; Zhang, Q.; Wilson, A.; et al. Carnitine palmitoyltransferase gene upregulation by linoleic acid induces CD4+ T cell apoptosis promoting HCC development. Cell Death Dis. 2018, 9, 620. [Google Scholar] [CrossRef]
- Pfister, D.; Núñez, N.G.; Pinyol, R.; Govaere, O.; Pinter, M.; Szydlowska, M.; Gupta, R.; Qiu, M.; Deczkowska, A.; Weiner, A.; et al. NASH limits anti-tumour surveillance in immunotherapy-treated HCC. Nature 2021, 592, 450–456. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Martínez, R.; Cruz-Gil, S.; Gómez de Cedrón, M.; Alvarez-Fernandez, M.; Vargas, T.; Molina, S.; García, B.; Herranz, J.; Moreno-Rubio, J.; Reglero, G.; et al. A link between lipid metabolism and epithelial-mesenchymal transition provides a target for colon cancer therapy. Oncotarget 2015, 6, 38719–38736. [Google Scholar] [CrossRef] [PubMed]
- Giampietri, C.; Tomaipitinca, L.; Scatozza, F.; Facchiano, A. Expression of Genes Related to Lipid Handling and the Obesity Paradox in Melanoma: Database Analysis. JMIR Cancer 2020, 6, e16974. [Google Scholar] [CrossRef]
- Fontana, A.; Spolaore, B.; Polverino de Laureto, P. The biological activities of protein/oleic acid complexes reside in the fatty acid. Biochim. Biophys. Acta 2013, 1834, 1125–1143. [Google Scholar] [CrossRef]
- Ning, J.; Zhao, C.; Chen, J.X.; Liao, D.F. Oleate inhibits hepatic autophagy through p38 mitogen-activated protein kinase (MAPK). Biochem. Biophys. Res. Commun. 2019, 514, 92–97. [Google Scholar] [CrossRef]
- Giulitti, F.; Petrungaro, S.; Mandatori, S.; Tomaipitinca, L.; de Franchis, V.; D’Amore, A.; Filippini, A.; Gaudio, E.; Ziparo, E.; Giampietri, C. Anti-tumor Effect of Oleic Acid in Hepatocellular Carcinoma Cell Lines via Autophagy Reduction. Front. Cell Dev. Biol. 2021, 9, 629182. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | HC Group | HCC Group |
|---|---|---|
| Number | 12 | 36 |
| Gender (male/female) | 9/3 | 30/6 |
| Age (years) | 49.2 ± 7.5 | 59.2 ± 8.2 |
| AFP (ng/mL) | 3.0 ± 1.5 | 106.8 ± 126.3 |
| CEA (ng/mL) | 1.8 ± 0.5 | 3.5 ± 1.8 |
| Metabolite | VIP | FC | p | Pathway |
|---|---|---|---|---|
| Linoleic acid ↑ | 1.39 | 2.02 | <0.001 | Biosynthesis of unsaturated fatty acids Linoleic acid metabolism |
| Caprylic acid ↑ | 1.50 | 10.55 | <0.001 | Fatty acid biosynthesis |
| Taurochenodeoxycholic acid ↑ | 1.29 | 17.92 | 0.030 | Primary bile acid biosynthesis |
| Tauroursodeoxycholic acid ↑ | 1.34 | 17.92 | 0.034 | NA |
| Taurodeoxycholic acid ↑ | 1.36 | 17.92 | 0.028 | NA |
| Pentadecanoic acid ↓ | 1.13 | 0.49 | <0.001 | NA |
| Hexacosanoic acid ↓ | 3.78 | 0.22 | 0.009 | NA |
| PC(16:0/20:4) ↓ | 2.57 | 0.40 | 0.002 | NA |
| PC(18:2/18:2) ↓ | 2.64 | 0.40 | 0.003 | NA |
| Oleic acid ↓ | 1.31 | 0.47 | 0.023 | Biosynthesis of unsaturated fatty acids |
| 5,6-EET ↓ | 1.84 | 0.29 | 0.002 | Arachidonic acid metabolism |
| 14,15-EET ↓ | 1.85 | 0.29 | 0.002 | NA |
| 16(R)-HETE ↓ | 1.81 | 0.29 | 0.002 | NA |
| 8,9-EET ↓ | 1.87 | 0.29 | 0.002 | Arachidonic acid metabolism |
| 11,12-EET ↓ | 1.86 | 0.29 | 0.002 | Arachidonic acid metabolism |
| 20-HETE ↓ | 1.85 | 0.29 | 0.002 | Arachidonic acid metabolism |
| 15(S)-HETE ↓ | 1.85 | 0.29 | 0.002 | Arachidonic acid metabolism |
| 19(S)-HETE ↓ | 1.84 | 0.29 | 0.002 | Arachidonic acid metabolism |
| Pathway | Total | Hits | Raw P | Impact |
|---|---|---|---|---|
| Arachidonic acid metabolism | 36 | 8 | <0.001 | 0.06 |
| Linoleic acid metabolism | 5 | 2 | <0.001 | 1.00 |
| Biosynthesis of unsaturated fatty acids | 36 | 2 | 0.030 | 0.01 |
| Primary bile acid biosynthesis | 46 | 1 | 0.304 | 0.01 |
| Fatty acid biosynthesis | 47 | 1 | 0.310 | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, T.; Liang, Y.; Zhen, X.; Wang, H.; Song, L.; Xing, D.; Li, H. Analysis of Serum Exosome Metabolites Identifies Potential Biomarkers for Human Hepatocellular Carcinoma. Metabolites 2024, 14, 462. https://doi.org/10.3390/metabo14080462
Zhao T, Liang Y, Zhen X, Wang H, Song L, Xing D, Li H. Analysis of Serum Exosome Metabolites Identifies Potential Biomarkers for Human Hepatocellular Carcinoma. Metabolites. 2024; 14(8):462. https://doi.org/10.3390/metabo14080462
Chicago/Turabian StyleZhao, Tingting, Yan Liang, Xiaolan Zhen, Hong Wang, Li Song, Didi Xing, and Hui Li. 2024. "Analysis of Serum Exosome Metabolites Identifies Potential Biomarkers for Human Hepatocellular Carcinoma" Metabolites 14, no. 8: 462. https://doi.org/10.3390/metabo14080462






