Long-Term Exposure of Psoralen and Isopsoralen Induced Hepatotoxicity and Serum Metabolites Profiles Changes in Female Rats
Abstract
:1. Introduction
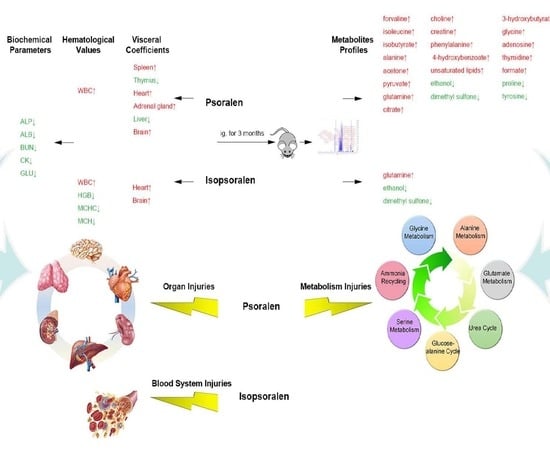
2. Results
2.1. Effects on the General Behavior and Mortality
2.2. Effects on the Body Weight
2.3. Effects on the Food and Water Intakes
2.4. Effects on the Visceral Coefficients
2.5. Effects on Hematological Parameters
2.6. Effects on Blood Biochemical Parameters
2.7. Effects on the Histopathology of the Major Organs
2.8. Metabolites Present in Serum Samples
2.9. Screening for Differential Metabolites
3. Discussion
4. Materials and Methods
4.1. Animals and Long-Term Toxicity Treatment
4.2. Organ Weights, Gross Necropsy and Histopathological Examination
4.3. Hematological and Biochemical Parameters
4.4. Sample Preparation and NMR Measurements
4.5. Data Processing for Metabonomic Analysis
4.6. Statistical Analysis
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chen, Z.M.; Hu, C.J.; Xiong, R.; Cui, Y.Y.; Zhang, M.; Pan, X.; Zhao, L. Effect of psoraleae fructus and myristicae semen in “ershen pill” on serum metabonomics in spleen-kidney yang deficiency diarrhea rats before and after processing. China J. Chin. Mater. Med. 2015, 40, 1400–1403. [Google Scholar]
- Alam, F.; Khan, G.N.; Asad, M. Psoralea corylifolia l: Ethnobotanical, biological, and chemical aspects: A review. Phytother. Res. 2018, 32, 597–615. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Lee, S.; Lee, H.; Ha, J.; Lee, J.; Choi, Y.; Oh, H.; Hong, J.; Yoon, Y.; Choi, K.H. Evaluation on antimicrobial activity of psoraleae semen extract controlling the growth of gram-positive bacteria. Korean J. Food Sci. Anim. Resour. 2017, 37, 502–510. [Google Scholar] [CrossRef] [PubMed]
- Yao, X.; Shen, H.; Fu, H.; Zhang, Y.; Wu, Z.; Hui, L. Toxic studies on various processed products of fructus psoraleae. J. Chin. Med. Mater. 1997, 20, 182–184. [Google Scholar]
- Xu, Y.; Zhao, Y.; Xie, J.; Sheng, X.; Li, Y.; Zhang, Y. The evaluation of toxicity induced by psoraleae fructus in rats using untargeted metabonomic method based on uplc-q-tof/ms. Evid. Based Complement. Altern. Med. 2017, 2017, 6207183. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.R.; Chang, C.L.; Hsieh, P.Y.; Lin, L.W.; Ching, H. Psoralen and isopsoralen, two coumarins of psoraleae fructus, can alleviate scopolamine-induced amnesia in rats. Planta Med. 2007, 73, 275–278. [Google Scholar] [CrossRef] [PubMed]
- Lau, K.M.; Fu, L.H.; Cheng, L.; Wong, C.W.; Wong, Y.L.; Lau, C.P.; Han, S.Q.; Chan, P.K.; Fung, K.P.; Lau, C.B.; et al. Two antifungal components isolated from fructus psoraleae and folium eucalypti globuli by bioassay-guided purification. Am. J. Chin. Med. 2010, 38, 1005–1014. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Hwang, T.L.; Chen, L.C.; Chang, T.H.; Wei, C.S.; Chen, J.J. Isoflavones and anti-inflammatory constituents from the fruits of psoralea corylifolia. Phytochemistry 2017, 143, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Oldham, M.; Yoon, P.; Fathi, Z.; Beyer, W.F.; Adamson, J.; Liu, L.; Alcorta, D.; Xia, W.; Osada, T.; Liu, C.; et al. X-ray psoralen activated cancer therapy (x-pact). PLoS ONE 2016, 11, e0162078. [Google Scholar] [CrossRef]
- Li, W.D.; Yan, C.P.; Wu, Y.; Weng, Z.B.; Yin, F.Z.; Yang, G.M.; Cai, B.C.; Chen, Z.P. Osteoblasts proliferation and differentiation stimulating activities of the main components of fructus psoraleae corylifoliae. Phytomedicine 2014, 21, 400–405. [Google Scholar] [CrossRef]
- Zhou, W.; Chen, X.; Zhao, G.; Xu, D.; Jiang, Z.; Zhang, L.; Wang, T. Psoralen induced liver injury by attenuating liver regenerative capability. Front. Pharmacol. 2018, 9, 1179. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yuan, X.M.; Wang, Y.F.; Jiang, M.M.; Bi, Y.N.; Liu, Y.; Pu, W.L.; Song, L.; Huang, J.Y.; Sun, L.K.; et al. Isopsoralen induces different subchronic toxicities and metabolomic outcomes between male and female wistar rats. Regul. Toxicol. Pharmacol. 2019, 103, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Cai, T.; Huang, N.; Wang, L.; Sun, X.; Li, X.; Sun, R. Experimental comparison study on acute toxicity of different processing methods of psoraleae fructus on normal mice. Chin. J. Pharmacovigil. 2017, 14, 730–736. [Google Scholar]
- Han, H.; Xiao, H.; Lu, Z. Short-term toxicity assessments of an antibiotic metabolite in wistar rats and its metabonomics analysis by ultra-high performance liquid chromatography coupled to quadrupole time-of-flight mass spectrometry. Toxicol. Appl. Pharmacol. 2016, 293, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Boonchaisri, S.; Rochfort, S.; Stevenson, T.; Dias, D.A. Recent developments in metabolomics-based research in understanding transgenic grass metabolism. Metabolomics 2019, 15, 47. [Google Scholar] [CrossRef]
- Komorowska, K.; Doyle, A.; Wahlestedt, M.; Subramaniam, A.; Debnath, S.; Chen, J.; Soneji, S.; Van Handel, B.; Mikkola, H.K.A.; Miharada, K.; et al. Hepatic leukemia factor maintains quiescence of hematopoietic stem cells and protects the stem cell pool during regeneration. Cell Rep. 2017, 21, 3514–3523. [Google Scholar] [CrossRef]
- Li, C.C.; Wang, T.L.; Zhang, Z.Q.; Yang, W.Q.; Wang, Y.F.; Chai, X.; Wang, C.H.; Li, Z. Phytochemical and pharmacological studies on the genus psoralea: A mini review. Evid. Based Complement. Altern. Med. 2016, 2016, 8108643. [Google Scholar] [CrossRef]
- Gebremeskel, A.K.; Wijerathne, T.D.; Kim, J.H.; Kim, M.J.; Seo, C.S.; Shin, H.K.; Lee, K.P. Psoralea corylifolia extract induces vasodilation in rat arteries through both endothelium-dependent and -independent mechanisms involving inhibition of trpc3 channel activity and elaboration of prostaglandin. Pharm. Biol. 2017, 55, 2136–2144. [Google Scholar] [CrossRef]
- Tian, W.; Lan, S.; Zhang, L.; Sun, L.; Huang, J.; Yang, X.; Sun, G.; Gao, X.; Sun, X. Safety evaluation and risk control measures of psoralea corylifolia. China J. Chin. Mater. Med. 2017, 42, 4059–4066. [Google Scholar]
- Wang, Y.; Lin, Z.; Wang, X.; Chu, M.; Zhang, B. Analysis and pharmacovigilance thinking on chinese patent medicine containing psoraleae fructus. Chin. J. Pharmacovigil. 2018, 15, 300–303. [Google Scholar]
- Nishizawa, A.; Suemoto, C.K.; Farias-Itao, D.S.; Campos, F.M.; Silva, K.C.S.; Bittencourt, M.S.; Grinberg, L.T.; Leite, R.E.P.; Ferretti-Rebustini, R.E.L.; Farfel, J.M.; et al. Morphometric measurements of systemic atherosclerosis and visceral fat: Evidence from an autopsy study. PLoS ONE 2017, 12, e0186630. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, H.; Jiang, J.M.; Zheng, D.; Chen, Y.Y.; Wan, S.J.; Tan, H.S.; Tang, L.M.; Xu, H.X. Hepatotoxicity induced by psoralen and isopsoralen from fructus psoraleae: Wistar rats are more vulnerable than icr mice. Food Chem. Toxicol. 2019, 125, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.J.; Chen, Y.; Huang, J.Q.; Li, K.M.; Razmovski-Naumovski, V.; Poon, J.; Chan, K.; Roufogalis, B.D.; McLachlan, A.J.; Mo, S.L.; et al. Evidence-based toxicity evaluation and scheduling of Chinese herbal medicines. J. Ethnopharmacol. 2013, 146, 40–61. [Google Scholar] [CrossRef] [PubMed]
- Hill, C.E.; Myers, J.P.; Vandenberg, L.N. Nonmonotonic dose-response curves occur in dose ranges that are relevant to regulatory decision-making. Dose-Response 2018, 16, 1559325818798282. [Google Scholar] [CrossRef]
- Song, L.; Yu, B.; Yang, L.; Wang, Z.X.; Zhang, Y.; Yu, Y.L.; Zhou, K. The mechanism of psoralen and isopsoralen hepatotoxicity as revealed by hepatic gene expression profiling in sd rats. Basic Clin. Pharmacol. Toxicol. 2019. [Google Scholar] [CrossRef]
- Shaw, D. Toxicological risks of chinese herbs. Planta Med. 2010, 76, 2012–2018. [Google Scholar] [CrossRef]







| Organs | Dose | Brain | Heart | Liver | Thymus | Spleen | Kidney | Adrenal Gland | Ovary | Uterus |
|---|---|---|---|---|---|---|---|---|---|---|
| 12 weeks | Control | 0.648 ± 0.064 | 0.295 ± 0.023 | 3.000 ± 0.202 | 0.150 ± 0.025 | 0.180 ± 0.020 | 0.675 ± 0.062 | 0.026 ± 0.005 | 0.063 ± 0.011 | 0.175 ± 0.036 |
| P14 mg/kg | 0.687 ± 0.044 | 0.320 ± 0.028 * | 2.653 ± 0.207 ** | 0.140 ± 0.026 | 0.216 ± 0.041 * | 0.673 ± 0.040 | 0.031 ± 0.003 * | 0.066 ± 0.007 | 0.155 ± 0.028 | |
| P28 mg/kg | 0.710 ± 0.050 * | 0.325 ± 0.030 | 2.731 ± 0.318 * | 0.120 ± 0.028 ** | 0.211 ± 0.027 ** | 0.714 ± 0.060 | 0.029 ± 0.006 | 0.070 ± 0.015 | 0.160 ± 0.036 | |
| P56 mg/kg | 0.685 ± 0.046 | 0.307 ± 0.021 | 2.876 ± 0.181 | 0.121 ± 0.026 ** | 0.230 ± 0.040 ** | 0.672 ± 0.029 | 0.027 ± 0.005 | 0.064 ± 0.010 | 0.183 ± 0.068 | |
| IP28 mg/kg | 0.696 ± 0.045 * | 0.348 ± 0.028 *** | 2.793 ± 0.368 | 0.149 ± 0.046 | 0.209 ± 0.051 | 0.696 ± 0.043 | 0.028 ± 0.006 | 0.065 ± 0.009 | 0.153 ± 0.031 | |
| Recovery | Control | 0.575 ± 0.040 | 0.335 ± 0.020 | 2.584 ± 0.230 | 0.168 ± 0.018 | 0.180 ± 0.021 | 0.603 ± 0.046 | 0.021 ± 0.005 | 0.050 ± 0.004 | 0.192 ± 0.075 |
| P14 mg/kg | 0.590 ± 0.043 | 0.355 ± 0.020 | 2.894 ± 0.131 * | 0.157 ± 0.016 | 0.178 ± 0.021 | 0.557 ± 0.153 | 0.021 ± 0.004 | 0.048 ± 0.009 | 0.162 ± 0.022 | |
| P28 mg/kg | 0.583 ± 0.077 | 0.354 ± 0.020 | 2.781 ± 0.137 | 0.182 ± 0.031 | 0.192 ± 0.020 | 0.618 ± 0.029 | 0.020 ± 0.004 | 0.045 ± 0.007 | 0.147 ± 0.015 | |
| P56 mg/kg | 0.567 ± 0.034 | 0.334 ± 0.015 | 2.592 ± 0.138 | 0.153 ± 0.021 | 0.186 ± 0.014 | 0.624 ± 0.038 | 0.023 ± 0.002 | 0.044 ± 0.003 * | 0.227 ± 0.111 | |
| IP28 mg/kg | 0.605 ± 0.048 | 0.350 ± 0.028 | 2.491 ± 0.194 | 0.153 ± 0.017 | 0.198 ± 0.018 | 0.593 ± 0.021 | 0.024 ± 0.004 | 0.048 ± 0.006 | 0.179 ± 0.090 |
| Parameters | ALT | AST | ALP | TBIL | TC | TG | TP | ALB | BUN | CRE | CK | GLU | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 12 weeks | Control | 29.00 ± 5.59 | 121.09 ± 19.11 | 150.36 ± 52.87 | 0.23 ± 0.10 | 1.00 ± 0.17 | 0.84 ± 0.20 | 56.48 ± 7.46 | 25.87 ± 1.68 | 5.95 ± 2.03 | 69.71 ± 11.18 | 968.55 ± 373.69 | 13.86 ± 1.28 |
| P14 mg/kg | 27.92 ± 8.34 | 116.75 ± 11.96 | 54.00 ± 12.38 *** | 0.22 ± 0.07 | 1.18 ± 0.26 | 0.50 ± 0.09 *** | 54.54 ± 2.01 | 23.34 ± 0.96 *** | 3.26 ± 0.69 *** | 66.13 ± 3.12 | 375.67 ± 110.47 *** | 11.68 ± 2.47 * | |
| P28 mg/kg | 26.25 ± 8.55 | 130.67 ± 38.00 | 46.25 ± 9.92 *** | 0.30 ± 0.12 | 1.02 ± 0.42 | 0.86 ± 0.43 | 55.81 ± 3.25 | 24.12 ± 1.13 ** | 3.85 ± 0.67 ** | 66.58 ± 5.56 | 420.92 ± 210.98 *** | 8.48 ± 2.24 *** | |
| P56 mg/kg | 25.00 ± 4.61 | 115.92 ± 26.82 | 55.83 ± 14.86 *** | 0.28 ± 0.11 | 1.01 ± 0.39 | 0.84 ± 0.40 | 54.99 ± 2.52 | 24.47 ± 1.46 * | 3.21 ± 0.62 *** | 67.50 ± 4.12 | 535.58 ± 209.83 ** | 11.67 ± 1.39 *** | |
| IP28 mg/kg | 27.00 ± 5.95 | 109.83 ± 25.96 | 50.17 ± 9.19 *** | 0.22 ± 0.08 | 1.27 ± 0.41 | 0.68 ± 0.19 | 55.71 ± 1.99 | 24.32 ± 1.25 * | 3.59 ± 0.6 *** | 66.39 ± 8.78 | 518.33 ± 246.45 ** | 10.39 ± 3.94 * | |
| Recovery | Control | 36.33 ± 5.92 | 97.33 ± 11.33 | 71.33 ± 30.03 | 0.23 ± 0.09 | 1.54 ± 0.28 | 0.61 ± 0.36 | 59.45 ± 2.70 | 26.27 ± 1.44 | 3.81 ± 0.22 | 68.20 ± 2.05 | 564.83 ± 166.87 | 12.53 ± 2.81 |
| P14 mg/kg | 37.33 ± 3.67 | 108.17 ± 7.76 | 88.83 ± 29.55 | 0.18 ± 0.06 | 1.49 ± 0.15 | 1.31 ± 0.83 | 61.00 ± 3.48 | 27.41 ± 1.84 | 4.50 ± 0.47 ** | 68.58 ± 2.63 | 895.00 ± 342.46 | 13.56 ± 2.70 | |
| P28 mg/kg | 38.50 ± 4.23 | 104.50 ± 17.74 | 60.33 ± 7.94 | 0.23 ± 0.09 | 1.58 ± 0.25 | 0.62 ± 0.22 | 60.40 ± 0.85 | 26.72 ± 0.87 | 3.86 ± 0.51 | 69.09 ± 4.47 | 689.83 ± 206.08 | 13.83 ± 0.92 | |
| P56 mg/kg | 38.00 ± 4.60 | 114.33 ± 11.33 * | 91.17 ± 29.26 | 0.21 ± 0.05 | 1.23 ± 0.18 * | 0.55 ± 0.18 | 59.49 ± 1.84 | 26.25 ± 1.49 | 4.50 ± 0.49 * | 67.44 ± 3.32 | 840.83 ± 442.98 | 13.61 ± 1.94 | |
| IP28 mg/kg | 34.40 ± 3.13 | 89.60 ± 7.89 | 60.80 ± 14.81 | 0.23 ± 0.07 | 1.49 ± 0.41 | 0.44 ± 0.13 | 59.56 ± 1.65 | 25.91 ± 1.47 | 3.62 ± 0.54 | 67.09 ± 3.65 | 814.40 ± 550.44 | 12.46 ± 2.13 |
| Parameters | WBC (109/L) | RBC (1012/L) | HGB (g/L) | MCV (fl%) | MCH (pg) | MCHC (g/L) | PLT (1010/L) | |
|---|---|---|---|---|---|---|---|---|
| 12 weeks | Control | 1.88 ± 1.14 | 4.34 ± 1.93 | 85.42 ± 37.08 | 54.67 ± 2.50 | 19.83 ± 0.73 | 362.67 ± 13.55 | 421.67 ± 233.20 |
| P14 mg/kg | 4.07 ± 2.66 * | 5.59 ± 1.47 | 111.08 ± 24.58 | 53.74 ± 2.90 | 20.08 ± 1.25 | 373.92 ± 12.84 * | 650.58 ± 346.52 | |
| P28 mg/kg | 2.98 ± 4.77 | 3.96 ± 2.10 | 76.25 ± 41.05 | 53.55 ± 3.04 | 19.34 ± 1.01 | 361.67 ± 14.39 | 430.33 ± 425.39 | |
| P56 mg/kg | 2.72 ± 2.09 | 4.10 ± 2.36 | 72.00 ± 48.09 | 55.04 ± 4.31 | 16.84 ± 6.47 | 304.00 ± 112.82 | 515.83 ± 396.29 | |
| IP28 mg/kg | 3.53 ± 2.38 * | 5.11 ± 1.94 | 38.58 ± 17.45 *** | 54.10 ± 3.54 | 7.34 ± 2.60 *** | 135.00 ± 45.26 *** | 620.17 ± 423.04 | |
| Recovery | Control | 3.02 ± 0.75 | 6.91 ± 0.51 | 138.67 ± 3.39 | 53.42 ± 2.61 | 20.15 ± 1.36 | 377.17 ± 7.73 | 959.83 ± 75.28 |
| P14 mg/kg | 2.73 ± 0.87 | 6.44 ± 1.24 | 128.33 ± 26.17 | 53.42 ± 1.95 | 19.88 ± 0.65 | 372.00 ± 7.75 | 913.33 ± 193.37 | |
| P28 mg/kg | 2.35 ± 0.40 | 6.68 ± 1.19 | 130.52 ± 2.97 | 53.25 ± 1.47 | 19.55 ± 0.53 | 367.33 ± 9.79 | 970.17 ± 274.90 | |
| P56 mg/kg | 2.77 ± 0.59 | 7.08 ± 1.68 | 137.00 ± 31.10 | 53.00 ± 1.75 | 19.4 ± 50.85 | 366.67 ± 6.09 * | 737.33 ± 313.05 | |
| IP28 mg/kg | 2.23 ± 0.99 | 7.98 ± 0.89 * | 159.17 ± 18.05 * | 53.22 ± 1.57 | 19.95 ± 0.63 | 375.00 ± 9.19 | 678.05 ± 414.28 |
| PLS-DA Model | R2X (cum a) | R2Y (cum) | Q2 (cum) | Intercept of R2 | Intercept of Q2 | P value (CV-ANOVA) |
|---|---|---|---|---|---|---|
| TControl vs. TP14 | 0.542 | 0.983 | 0.762 | 0.973 | 0.281 | 0.044 * |
| TControl vs. TP28 | 0.402 | 0.989 | 0.813 | 0.947 | −0.101 | 0.012 * |
| TControl vs. TP56 | 0.381 | 0.983 | 0.779 | 0.939 | 0.046 | 0.003 ** |
| TControl vs. TIP28 | 0.445 | 0.995 | 0.814 | 0.988 | 0.211 | 0.066 |
| RControl vs. RP14 | 0.304 | 0.965 | 0.284 | 0.923 | 0.138 | 0.952 |
| RControl vs. RP28 | 0.374 | 0.923 | 0.310 | 0.930 | 0.186 | 0.872 |
| RControl vs. RP56 | 0.389 | 0.997 | 0.932 | 0.961 | 0.032 | 0.393 |
| RControl vs. RIP28 | 0.374 | 0.995 | 0.603 | 0.976 | 0.256 | 0.572 |
| Metabolites | Chemical Shifts | TControl vs. TP56 | TControl vs. TP28 | TControl vs.TP14 | TControl vs.TIP28 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| VIP | FC | P | VIP | FC | P | VIP | FC | P | VIP | FC | P | ||
| Valine | 0.968 | 1.958 | 0.665 | 0.007 | 2.091 | 0.531 | 0.009 | 1.071 | 0.825 | 0.458 | 0.880 | 0.905 | 0.843 |
| Isoleucine | 0.998 | 1.629 | 0.644 | 0.040 | 1.967 | 0.485 | 0.015 | 1.050 | 0.802 | 0.516 | 0.638 | 1.019 | 0.977 |
| Isobutyrate | 1.050 | 1.828 | 0.640 | 0.013 | 1.801 | 0.631 | 0.026 | 1.170 | 0.753 | 0.377 | 1.381 | 0.738 | 0.404 |
| Ethanol | 1.157 | 2.060 | 2.384 | 0.006 | 1.911 | 2.620 | 0.018 | 0.684 | 1.253 | 0.613 | 2.204 | 1.988 | 0.046 |
| 3-Hydroxybutyrate | 1.187 | 1.604 | 0.361 | 0.040 | 1.543 | 0.287 | 0.073 | 1.057 | 0.644 | 0.470 | 1.534 | 0.332 | 0.291 |
| Alanine | 1.459 | 1.802 | 0.625 | 0.015 | 1.662 | 0.613 | 0.047 | 1.209 | 0.740 | 0.343 | 0.247 | 0.985 | 0.977 |
| Acetone | 2.218 | 2.011 | 0.366 | 0.007 | 2.137 | 0.271 | 0.007 | 1.132 | 0.602 | 0.421 | 1.782 | 0.310 | 0.148 |
| Pyruvate | 2.361 | 1.787 | 0.658 | 0.017 | 1.758 | 0.607 | 0.035 | 1.433 | 0.696 | 0.226 | 0.868 | 0.910 | 0.744 |
| Glutamine | 2.431 | 2.114 | 0.644 | 0.006 | 2.075 | 0.687 | 0.011 | 1.949 | 0.651 | 0.059 | 2.200 | 0.610 | 0.040 |
| Citrate | 2.527 | 1.945 | 0.474 | 0.007 | 1.999 | 0.447 | 0.013 | 1.067 | 0.838 | 0.623 | 1.050 | 0.774 | 0.574 |
| PUFA | 2.775 | 2.011 | 0.578 | 0.007 | 1.763 | 0.538 | 0.030 | 1.802 | 0.708 | 0.052 | 1.970 | 0.601 | 0.082 |
| Dimethyl sulfone | 3.14 | 1.876 | 1.555 | 0.011 | 1.862 | 1.814 | 0.020 | 1.604 | 1.272 | 0.379 | 2.302 | 1.881 | 0.026 |
| Choline | 3.187 | 1.799 | 0.582 | 0.016 | 1.987 | 0.538 | 0.013 | 0.989 | 1.066 | 0.809 | 1.148 | 1.173 | 0.611 |
| Proline | 3.318 | 1.718 | 1.594 | 0.026 | 1.389 | 1.550 | 0.126 | 1.774 | 1.573 | 0.252 | 2.161 | 2.076 | 0.050 |
| Glycine | 3.55 | 1.916 | 0.624 | 0.011 | 1.517 | 0.560 | 0.099 | 1.278 | 0.610 | 0.401 | 1.349 | 0.693 | 0.404 |
| Creatine | 3.919 | 2.096 | 0.532 | 0.006 | 2.048 | 0.471 | 0.012 | 1.694 | 0.459 | 0.158 | 1.753 | 0.561 | 0.159 |
| Adenosine | 6.045 | 1.621 | 0.532 | 0.040 | 1.141 | 0.566 | 0.342 | 1.329 | 0.492 | 0.302 | 2.030 | 0.454 | 0.069 |
| Thymidine | 6.259 | 1.838 | 0.296 | 0.012 | 1.489 | 0.354 | 0.104 | 1.595 | 0.361 | 0.120 | 1.652 | 0.366 | 0.211 |
| Tyrosine | 7.185 | 1.553 | 1.997 | 0.049 | 1.377 | 1.713 | 0.123 | 0.555 | 1.117 | 0.820 | 1.412 | 1.631 | 0.389 |
| Phenylalanine | 7.304 | 1.682 | 0.581 | 0.029 | 1.823 | 0.496 | 0.025 | 0.945 | 0.739 | 0.506 | 0.827 | 0.816 | 0.722 |
| 4-Hydroxybenzoate | 7.822 | 1.759 | 0.500 | 0.024 | 1.741 | 0.407 | 0.041 | 1.195 | 0.484 | 0.395 | 1.610 | 0.549 | 0.262 |
| Formate | 8.441 | 1.819 | 0.382 | 0.029 | 1.590 | 0.236 | 0.072 | 0.842 | 0.634 | 0.578 | 1.581 | 2.223 | 0.251 |
| Metabolites | Chemical Shifts | RControl vs. RP56 | RControl vs. TP28 | RControl vs. RP14 | RControl vs. RIP28 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| VIP | FC | P | VIP | FC | P | VIP | FC | P | VIP | FC | P | ||
| Valine | 0.968 | 1.229 | 1.322 | 0.537 | 0.753 | 1.048 | 0.926 | 1.233 | 0.923 | 0.918 | 1.490 | 1.228 | 0.878 |
| Isoleucine | 0.998 | 1.209 | 1.264 | 0.546 | 0.651 | 1.030 | 0.959 | 1.642 | 0.876 | 0.840 | 1.666 | 1.360 | 0.797 |
| Isobutyrate | 1.050 | 0.741 | 0.864 | 0.687 | 1.388 | 0.752 | 0.848 | 1.159 | 0.853 | 0.937 | 1.602 | 0.779 | 0.723 |
| Ethanol | 1.157 | 0.343 | 1.017 | 0.975 | 0.542 | 0.908 | 0.929 | 0.734 | 1.183 | 0.999 | 0.700 | 0.900 | 0.894 |
| 3-Hydroxybutyrate | 1.187 | 0.861 | 1.434 | 0.656 | 0.853 | 0.966 | 0.986 | 0.267 | 1.009 | 0.999 | 0.665 | 1.044 | 0.981 |
| Alanine | 1.459 | 0.018 | 1.003 | 0.995 | 1.059 | 0.836 | 0.848 | 2.120 | 0.838 | 0.663 | 0.407 | 0.989 | 0.983 |
| Acetone | 2.218 | 0.185 | 0.950 | 0.941 | 0.673 | 0.981 | 0.993 | 0.681 | 1.157 | 0.999 | 0.251 | 0.985 | 0.986 |
| Pyruvate | 2.361 | 1.052 | 1.176 | 0.603 | 0.928 | 1.113 | 0.867 | 0.428 | 1.075 | 0.999 | 0.970 | 1.195 | 0.884 |
| Glutamine | 2.431 | 1.679 | 0.780 | 0.416 | 2.011 | 0.683 | 0.848 | 1.816 | 0.828 | 0.763 | 1.968 | 0.732 | 0.575 |
| Citrate | 2.527 | 0.200 | 1.041 | 0.950 | 1.013 | 0.871 | 0.867 | 1.949 | 0.757 | 0.692 | 1.494 | 1.346 | 0.878 |
| PUFA | 2.775 | 0.548 | 1.081 | 0.852 | 0.128 | 0.981 | 0.977 | 0.778 | 1.085 | 0.999 | 0.324 | 1.015 | 0.984 |
| Dimethyl sulfone | 3.140 | 1.141 | 0.717 | 0.562 | 1.340 | 0.776 | 0.848 | 1.110 | 0.834 | 0.938 | 1.831 | 0.670 | 0.636 |
| Choline | 3.187 | 1.790 | 1.535 | 0.405 | 0.671 | 1.087 | 0.883 | 0.132 | 0.990 | 0.999 | 1.993 | 1.473 | 0.575 |
| Proline | 3.318 | 0.732 | 0.790 | 0.691 | 0.947 | 0.810 | 0.857 | 1.504 | 0.649 | 0.904 | 1.687 | 0.680 | 0.693 |
| Glycine | 3.550 | 1.603 | 0.680 | 0.422 | 1.361 | 0.776 | 0.848 | 1.978 | 0.799 | 0.687 | 1.309 | 0.836 | 0.852 |
| Creatine | 3.919 | 1.401 | 0.772 | 0.481 | 1.617 | 0.746 | 0.848 | 1.219 | 0.881 | 0.918 | 1.213 | 0.786 | 0.878 |
| Adenosine | 6.045 | 0.272 | 0.923 | 0.916 | 1.071 | 0.712 | 0.848 | 1.472 | 0.684 | 0.904 | 1.269 | 0.674 | 0.876 |
| Thymidine | 6.259 | 0.888 | 1.265 | 0.653 | 0.815 | 0.891 | 0.874 | 1.138 | 0.811 | 0.938 | 1.159 | 0.841 | 0.878 |
| Tyrosine | 7.185 | 1.364 | 0.525 | 0.496 | 0.875 | 0.799 | 0.848 | 0.427 | 1.047 | 0.999 | 1.593 | 0.676 | 0.737 |
| Phenylalanine | 7.304 | 1.273 | 1.262 | 0.524 | 0.899 | 0.910 | 0.848 | 0.186 | 1.009 | 0.999 | 0.684 | 1.068 | 0.929 |
| 4-Hydroxybenzoate | 7.822 | 0.474 | 0.880 | 0.823 | 0.472 | 0.915 | 0.932 | 0.262 | 1.046 | 0.999 | 1.568 | 0.719 | 0.742 |
| Formate | 8.441 | 1.600 | 2.000 | 0.426 | 1.194 | 1.474 | 0.848 | 0.868 | 1.099 | 0.999 | 2.145 | 1.797 | 0.432 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, Y.; Wang, P.; Yu, R.; Lu, J.; Jiang, M.; Zhou, K. Long-Term Exposure of Psoralen and Isopsoralen Induced Hepatotoxicity and Serum Metabolites Profiles Changes in Female Rats. Metabolites 2019, 9, 263. https://doi.org/10.3390/metabo9110263
Yu Y, Wang P, Yu R, Lu J, Jiang M, Zhou K. Long-Term Exposure of Psoralen and Isopsoralen Induced Hepatotoxicity and Serum Metabolites Profiles Changes in Female Rats. Metabolites. 2019; 9(11):263. https://doi.org/10.3390/metabo9110263
Chicago/Turabian StyleYu, Yingli, Pengli Wang, Ruili Yu, Jiaxi Lu, Miaomiao Jiang, and Kun Zhou. 2019. "Long-Term Exposure of Psoralen and Isopsoralen Induced Hepatotoxicity and Serum Metabolites Profiles Changes in Female Rats" Metabolites 9, no. 11: 263. https://doi.org/10.3390/metabo9110263
APA StyleYu, Y., Wang, P., Yu, R., Lu, J., Jiang, M., & Zhou, K. (2019). Long-Term Exposure of Psoralen and Isopsoralen Induced Hepatotoxicity and Serum Metabolites Profiles Changes in Female Rats. Metabolites, 9(11), 263. https://doi.org/10.3390/metabo9110263