Recent Advances in Molecular Mechanisms of the NKG2D Pathway in Hepatocellular Carcinoma
Abstract
:1. Introduction
2. The Discovery of NKG2D
3. Chromosome Localization of NKG2D
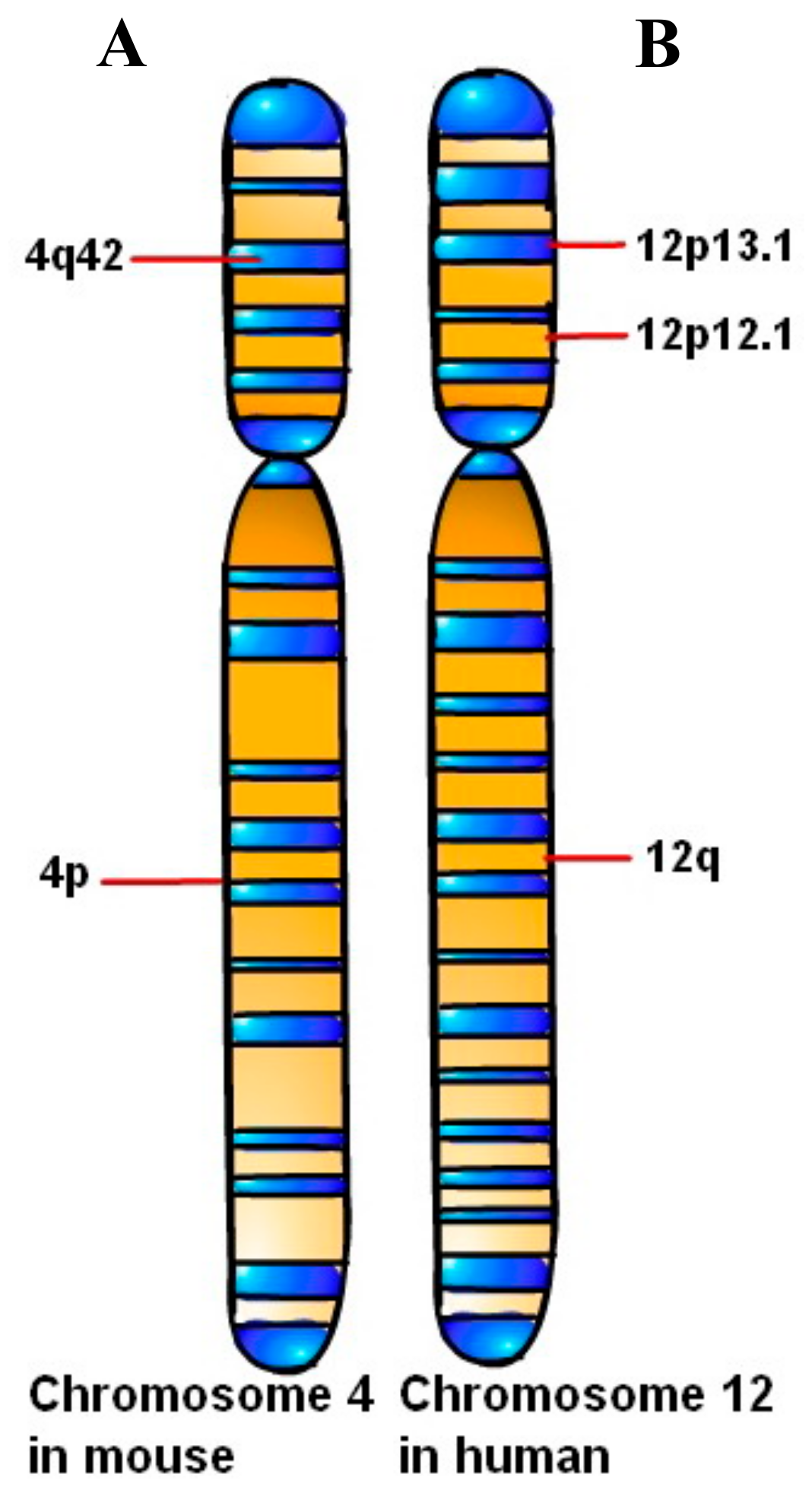
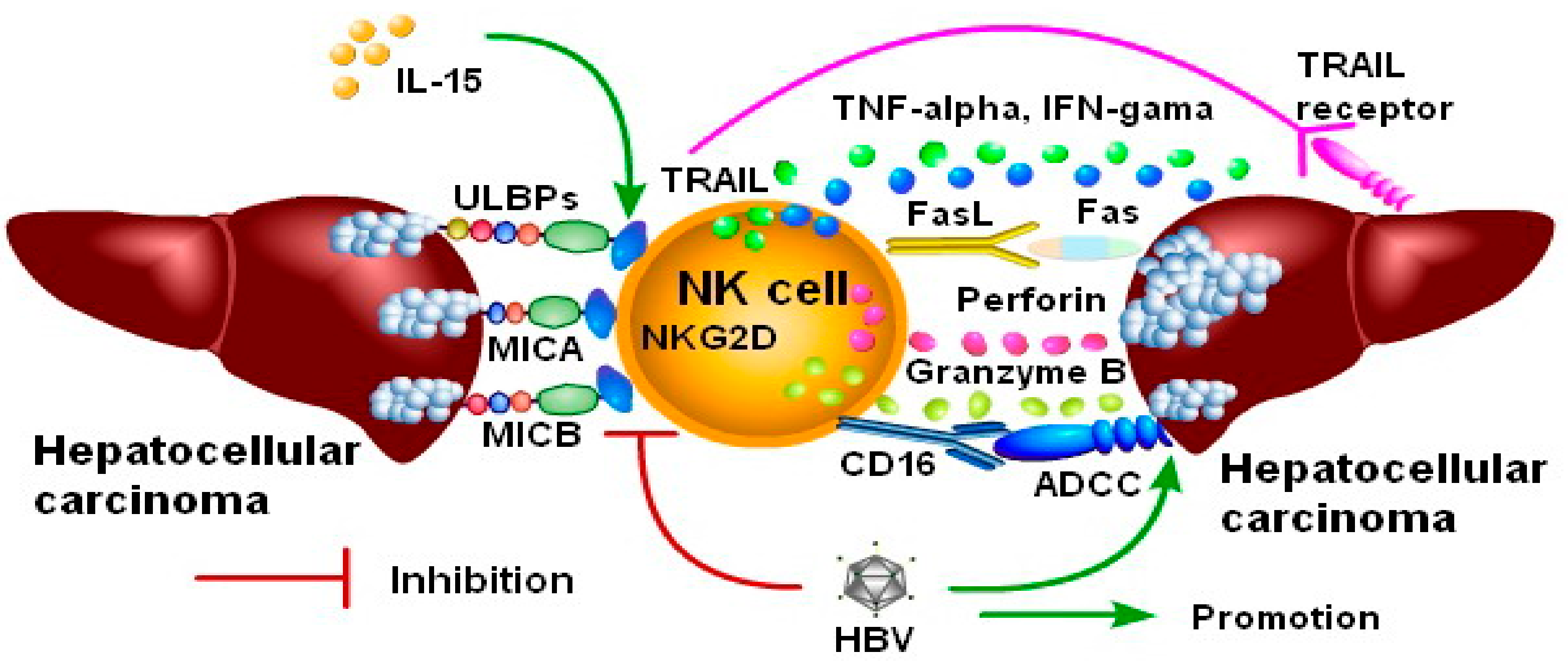
3.1. Chromosome Localization of NKG2D in the Mouse
3.2. Chromosome Localization of NKG2D in Human
3.3. The Difference Expression of NKG2D between Humans and Mice
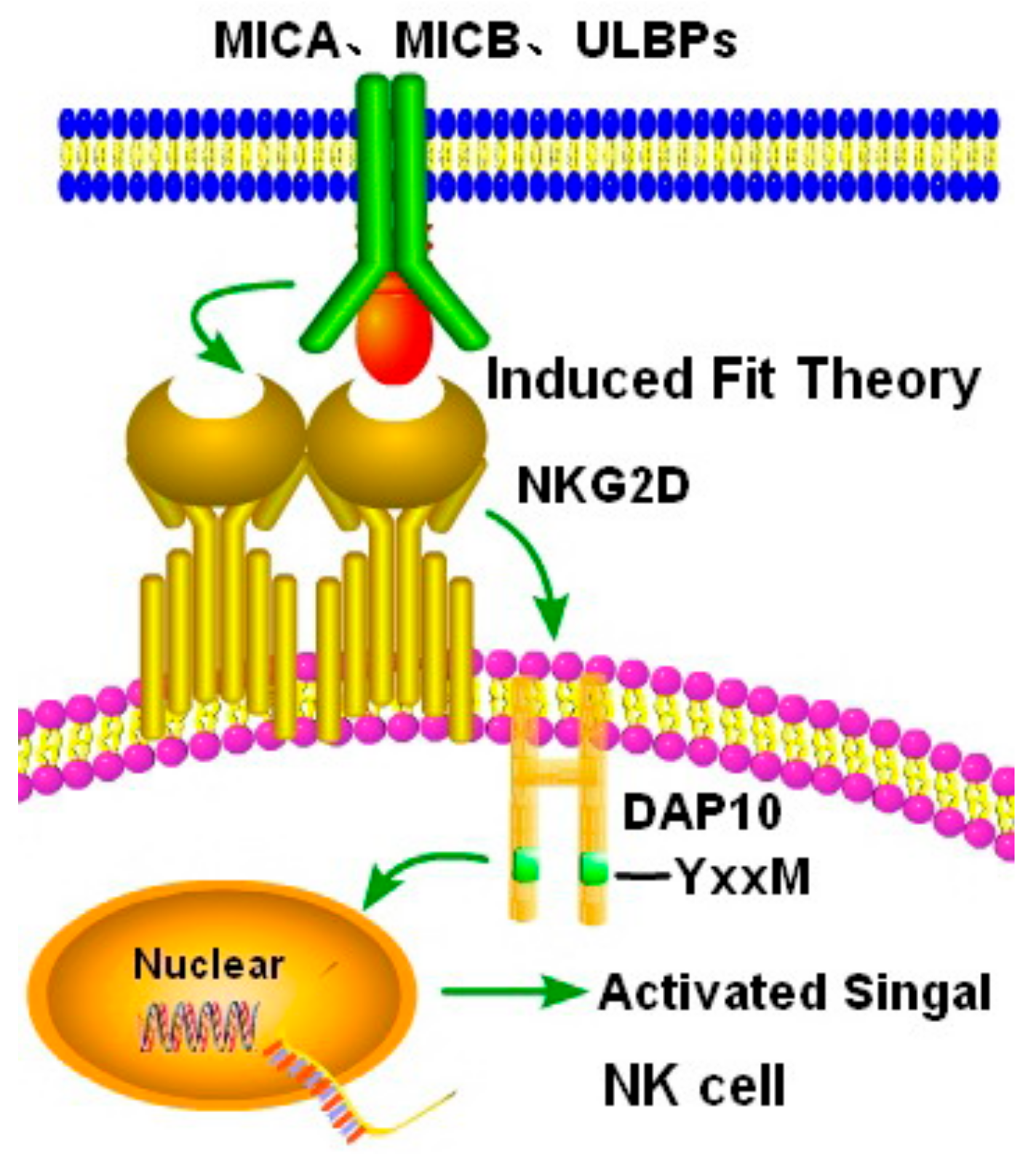
4. Interaction between NKG2D and Ligands
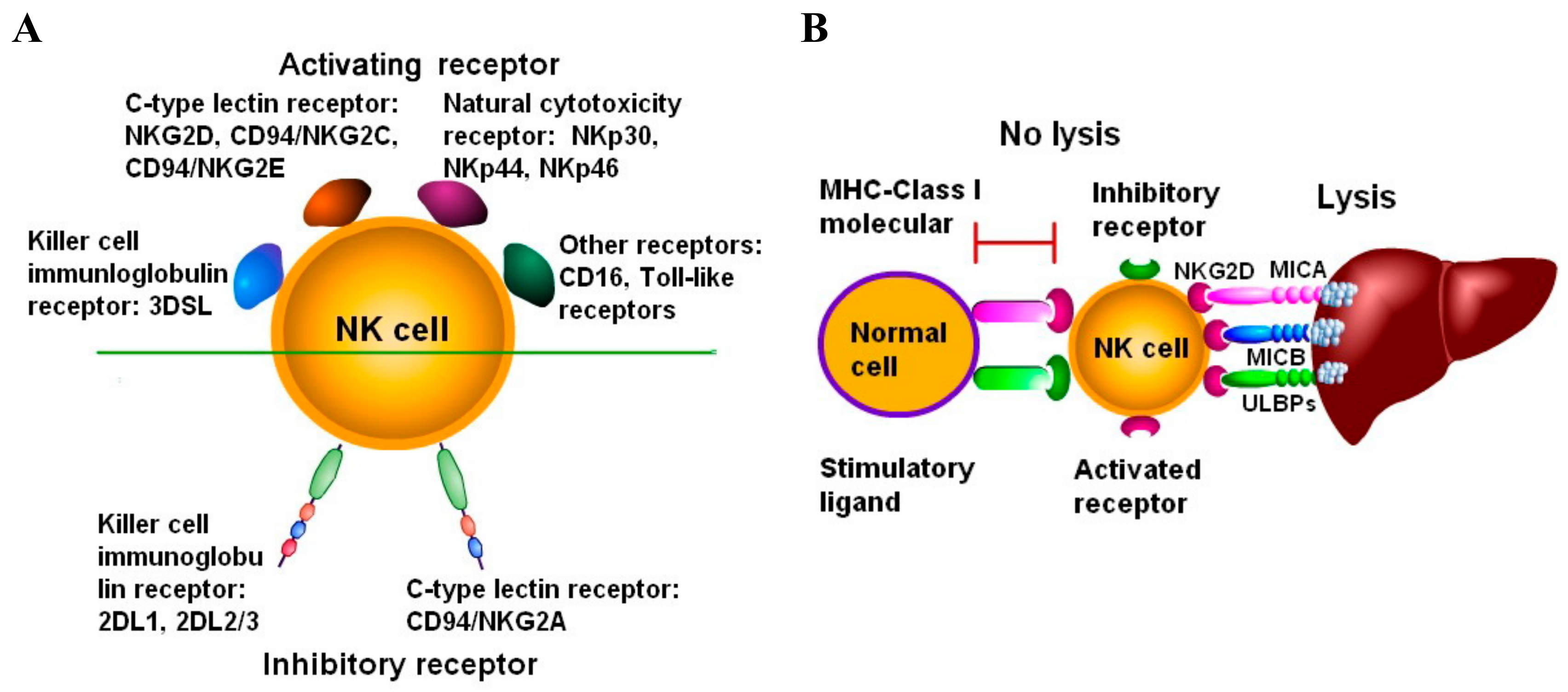
5. Activation of NKG2D Promotes the Activity of NK Cells Against Hepatocellular Carcinoma
5.1. TNF-alpha Secreted by NK Cells Exerts Anti-hepatocarcinoma Activity by Activated NKG2D
5.2. IFN-gamma Secreted by NK Cells Exerts Anti-hepatocarcinoma Activity by Activated NKG2D
5.3. FasL Expressed on NK Cells Exerts Anti-hepatocarcinoma Activity by Activated NKG2D
5.4. Perforin Secreted by NK Cells Exerts Anti-hepatocarcinoma Activity by Activating NKG2D
5.5. NKG2D Signaling Induces High Expression of CD16 on NK Cells Exerts Anti-hepatocarcinoma Activity
5.6. TRAIL Expressed on NK Cells Exerts Anti-hepatocarcinoma Activity by Activating NKG2D
5.7. Important Issues Concerning the Role of NKG2D in the Immune Response against Hepatocellular Carcinoma
5.8. Targeted Stimulation of NKG2D Improves the Therapeutic Effect of NK Cells on Hepatocellular Carcinoma Immunotherapy
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mancebo, A.; Varela, M.; González-Diéguez, M.L.; Navascués, C.A.; Cadahía, V.; Mesa-Álvarez, A.; Rodrigo, L.; Rodríguez, M. Incidence and risk factors associated with hepatocellular carcinoma surveillance failure. J. Gastroenterol Hepatol. 2018, 33, 1524–1529. [Google Scholar] [CrossRef]
- Liew, Z.H.; Goh, G.B.; Hao, Y.; Chang, P.E.; Tan, C.K. Comparison of Hepatocellular Carcinoma in Patients with Cryptogenic Versus Hepatitis B Etiology: A Study of 1079 Cases Over 3 Decades. Dig. Dis. Sci. 2019, 64, 585–590. [Google Scholar] [CrossRef]
- Schmidt, T.M.; Liu, L.I.; Abraham, I.E.; Uy, A.B.; Dudek, A.Z.; Liu, L.I.; Abraham, I.E.; Uy, A.B.; Dudek, A.Z. Efficacy and Safety of Sorafenib in a Racially Diverse Patient Population with Advanced Hepatocellular Carcinoma. Anticancer Res. 2018, 38, 4027–4034. [Google Scholar] [CrossRef] [Green Version]
- Liu, K.; McCaughan, G.W. Epidemiology and Etiologic Associations of Non-alcoholic Fatty Liver Disease and Associated HCC. Adv. Exp. Med. Biol. 2018, 1061, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Chaturvedi, V.K.; Singh, A.; Dubey, S.K.; Hetta, H.F.; John, J.; Singh, M.P.; Singh, A.; Dubey, S.K.; Hetta, H.F.; John, J.; et al. Molecular mechanistic insight of hepatitis B virus mediated hepatocellular carcinoma. Microb. Pathog. 2019, 128, 184–194. [Google Scholar] [CrossRef] [PubMed]
- Aberg, F.; Helenius-Hietala, J.; Puukka, P.; Jula, A.; Helenius-Hietala, J.; Puukka, P.; Jula, A. Binge drinking and the risk of liver events: a population-based cohort study. Liver Int. 2017, 37, 1373–1381. [Google Scholar] [CrossRef] [PubMed]
- Fathy, A.H.; Bashandy, M.A.; Bashandy, S.A.E.; Mansour, A.M.; Elsadek, B. Sequential analysis and staging of a diethylnitrosamine-induced hepatocellular carcinoma in male Wistar albino rat model. Can. J. Physiol. Pharmacol. 2017, 95, 1462–1472. [Google Scholar] [CrossRef]
- Moore, M.M.; Schoeny, R.S.; Becker, R.A.; White, K.; Pottenger, L.H. Development of an adverse outcome pathway for chemically induced hepatocellular carcinoma: case study of AFB1, a human carcinogen with a mutagenic mode of action. Crit. Rev. Toxicol. 2018, 48, 312–337. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, M.H.; Yang, H.I.; Le, A.; Henry, L.; Nguyen, N.; Lee, M.H.; Zhang, J.; Wong, C.; Wong, C.; Trinh, H. Reduced Incidence of Hepatocellular Carcinoma with Tenofovir in Chronic Hepatitis B Patients with and without Cirrhosis - a Propensity Score Matched Study. J. Infect. Dis. 2019, 219, 10–18. [Google Scholar] [CrossRef]
- Yu, M.; Li, Z. Natural killer cells in hepatocellular carcinoma: current status and perspectives for future immunotherapeutic approaches. Front Med. 2017, 11, 509–521. [Google Scholar] [CrossRef]
- Su, Z.; Ye, X.; Shang, L. MiR-506 Promotes Natural Killer Cell Cytotoxicity against Human Hepatocellular Carcinoma Cellsby Targeting STAT3. Yonsei Med J. 2019, 60, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Jelenčić, V.; Lenartić, M.; Wensveen, F.M.; Polić, B. NKG2D: A versatile player in the immune system. Immunol Lett. 2017, 189, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Chambers, A.M.; Wang, J.; Lupo, K.B.; Yu, H.; Atallah, L.N.M.; Matosevic, S. Adenosinergic Signaling Alters Natural Killer Cell Functional Responses. Front Immunol. 2018, 9, 2533. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.S.; Mimura, K.; Kua, L.F.; Shiraishi, K.; Kono, K. Implication of Highly Cytotoxic Natural Killer Cells for Esophageal Squamous Cell Carcinoma Treatment. J. Immunother. 2018, 41, 261–273. [Google Scholar] [CrossRef]
- López-Cobo, S.; Romera-Cárdenas, G.; García-Cuesta, E.M.; Reyburn, H.T.; Valés-Gómez, M. Transfer of the human NKG2D ligands UL16 binding proteins (ULBP) 1-3 is related to lytic granule release and leads to ligand retransfer and killing of ULBP-recipient natural killer cells. Immunology 2015, 146, 70–80. [Google Scholar] [CrossRef] [Green Version]
- Thompson, T.W.; Kim, A.B.; Li, P.J.; Wang, J.; Jackson, B.T.; Huang, K.T.H.; Zhang, L.; Raulet, D.H. Endothelial cells express NKG2D ligands and desensitize antitumor NK responses. Elife. 2017, 6, e30881. [Google Scholar] [CrossRef]
- Houchins, J.P.; Yabe, T.; McSherry, C.; Bach, F.H. DNA sequence analysis of NKG2, a family of related cDNA clones encoding type II integral membrane proteins on human natural killer cells. J. Exp. Med. 1991, 173, 1017–1020. [Google Scholar] [CrossRef] [Green Version]
- Huergo-Zapico, L.; Acebes-Huerta, A.; Gonzalez-Rodriguez, A.P.; Contesti, J.; Gonzalez-García, E.; Payer, A.R.; Villa-Alvarez, M.; Fernández-Guizán, A.; López-Soto, A.; Gonzalez, S. Expansion of NK cells and reduction of NKG2D expression in chronic lymphocytic leukemia. Correlation with progressive disease. PLoS One. 2014, 9, e108326. [Google Scholar] [CrossRef]
- Mou, X.; Zhou, Y.; Jiang, P.; Zhou, T.; Jiang, Q.; Xu, C.; Liu, H.; Zheng, T.; Yuan, G.; Zhang, Y.; et al. The regulatory effect of UL-16 binding protein-3 expression on the cytotoxicity of NK cells in cancer patients. Sci. Rep. 2014, 4, 6138. [Google Scholar] [CrossRef] [Green Version]
- Kruse, P.H.; Matta, J.; Ugolini, S.; Vivier, E. Natural cytotoxicity receptors and their ligands. Immunol. Cell Biol. 2014, 92, 221–229. [Google Scholar] [CrossRef]
- Siewiera, J.; Gouilly, J.; Hocine, H.R.; Cartron, G.; Levy, C.; Al-Daccak, R.; Jabrane-Ferrat, N. Natural cytotoxicity receptor splice variants orchestrate the distinct functions of human natural killer cell subtypes. Nat. Commun. 2015, 6, 10183. [Google Scholar] [CrossRef] [PubMed]
- Rozbeský, D.; Ivanova, L.; Hernychová, L.; Grobárová, V.; Novák, P.; Černý, J. Nkrp1 Family, from Lectins to Protein Interacting Molecules. Biomolecules. 2015, 20, 3463–3472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Czaja, K.; Borer, A.S.; Schmied, L.; Terszowski, G.; Stern, M.; Gonzalez, A. A comprehensive analysis of the binding of anti-KIR antibodies to activating KIRs. Genes. Immun. 2014, 15, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Erbe, A.K.; Alderson, K.A.; Phillips, E.; Gallenberger, M.; Gan, J.; Campana, D.; Hank, J.A.; Sondel, P.M. Human NK cells maintain licensing status and are subject to killer immunoglobulin-like receptor (KIR) and KIR-ligand inhibition following ex vivo expansion. Cancer Immunol. Immunother. 2016, 65, 1047–1059. [Google Scholar] [CrossRef] [Green Version]
- Sivori, S.; Vacca, P.; Del Zotto, G.; Munari, E.; Mingari, M.C.; Moretta, L. Human NK cells: surface receptors, inhibitory checkpoints, and translational applications. Cell Mol. Immunol. 2019, 16, 430–441. [Google Scholar] [CrossRef]
- Zhang, Q.; Bi, J.; Zheng, X.; Chen, Y.; Wang, H.; Wu, W.; Wang, Z.; Wu, Q.; Peng, H.; Wei, H.; et al. Blockade of the checkpoint receptor TIGIT prevents NK cell exhaustion and elicits potent anti-tumor immunity. Nat Immunol. 2018, 19, 723–732. [Google Scholar] [CrossRef]
- Dukovska, D.; Fernández-Soto, D.; Valés-Gómez, M.; Reyburn, H.T. NKG2H-Expressing T Cells Negatively Regulate Immune Responses. Front. Immunol. 2018, 9, 390. [Google Scholar] [CrossRef] [Green Version]
- Brostjan, C.; Sobanov, Y.; Glienke, J.; Hayer, S.; Lehrach, H.; Francis, F.; Hofer, E. The NKG2 natural killer cell receptor family: comparative analysis of promoter sequences. Genes Immun. 2000, 1, 504–508. [Google Scholar] [CrossRef] [Green Version]
- Kabat, J.; Borrego, F.; Brooks, A.; Coligan, J.E. Role that each NKG2A immunoreceptor tyrosine-based inhibitory motif plays in mediating the human CD94/NKG2A inhibitory signal. J. Immunol. 2002, 169, 1948–1958. [Google Scholar] [CrossRef] [Green Version]
- Dobromylskyj, M.; Ellis, S. Complexity in cattle KIR genes: transcription and genome analysis. Immunogenetics. 2007, 59, 463–472. [Google Scholar] [CrossRef]
- Wen, L.Z.; Ding, K.; Wang, Z.R.; Ding, C.H.; Lei, S.J.; Liu, J.P.; Yin, C.; Hu, P.F.; Ding, J.; Chen, W.S.; et al. SHP-1 acts as a Tumor Suppressor in Hepatocarcinogenesis and HCC Progression. Cancer Res. 2018, 78, 4680–4691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ho, E.L.; Heusel, J.W.; Brown, M.G.; Matsumoto, K.; Scalzo, A.A.; Yokoyama, W.M. Murine Nkg2d and Cd94 are clustered within the natural killer complex and are expressed independently in natural killer cells. Proc. Natl. Acad. Sci. USA 1998, 95, 6320–6325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dissen, E.; Ryan, J.C.; Seaman, W.E.; Fossum, S. An autosomal dominant locus, Nka, mapping to the Ly-49 region of a rat natural killer (NK) gene complex, controls NK cell lysis of allogeneic lymphocytes. J. Exp. Med. 1996, 183, 2197–2207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ritter, C.; Fan, K.; Paulson, K.G.; Nghiem, P.; Schrama, D.; Becker, J.C. Reversal of epigenetic silencing of MHC class I chain-related protein A and B improves immune recognition of Merkel cell carcinoma. Sci. Rep. 2016, 6, 21678. [Google Scholar] [CrossRef] [Green Version]
- Imai, K.; Hayashi, T.; Yamaoka, M.; Kajimura, J.; Yoshida, K.; Kusunoki, Y.; Nakachi, K. Effects of NKG2D haplotypes on the cell-surface expression of NKG2D protein on natural killer and CD8 T cells of peripheral blood among atomic-bomb survivors. Hum. Immunol. 2012, 73, 686–691. [Google Scholar] [CrossRef]
- Hara, R.; Onizuka, M.; Matsusita, E.; Kikkawa, E.; Nakamura, Y.; Matsushita, H.; Ohgiya, D.; Murayama, H.; Machida, S.; Ohmachi, K.; et al. NKG2D gene polymorphisms are associated with disease control of chronic myeloid leukemia by dasatinib. Int. J. Hematol. 2017, 106, 666–674. [Google Scholar] [CrossRef]
- Xu, Y.; Zhou, R.; Huang, C.; Zhang, M.; Li, J.; Zong, J.; Qiu, S.; Lin, S.; Chen, H.; Ye, Y.; et al. Analysis of the Expression of Surface Receptors on NK Cells and NKG2D on Immunocytes in Peripheral Blood of Patients with Nasopharyngeal Carcinoma. Asian Pac. J. Cancer Prev. 2018, 19, 661–665. [Google Scholar] [CrossRef]
- Lanier, L.L. NKG2D Receptor and Its Ligands in Host Defense. Cancer Immunol. Res. 2015, 3, 575–582. [Google Scholar] [CrossRef] [Green Version]
- Stojanovic, A.; Correia, M.P.; Cerwenka, A. The NKG2D/NKG2DL Axis in the Crosstalk Between Lymphoid and Myeloid Cells in Health and Disease. Front Immunol. 2018, 9, 827. [Google Scholar] [CrossRef] [Green Version]
- Pistoia, V.; Tumino, N.; Vacca, P.; Veneziani, I.; Moretta, A.; Locatelli, F.; Moretta, L. Human γδ T-Cells: From Surface Receptors to the Therapy of High-Risk Leukemias. Front Immunol. 2018, 9, 984. [Google Scholar] [CrossRef] [Green Version]
- Li, X.; Kang, N.; Zhang, X.; Dong, X.; Wei, W.; Cui, L.; Ba, D.; He, W. Generation of human regulatory gammadelta T cells by TCRgammadelta stimulation in the presence of TGF-beta and their involvement in the pathogenesis of systemic lupus erythematosus. J Immunol. 2011, 186, 6693–6700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ye, J.; Ma, C.; Hsueh, E.C.; Eickhoff, C.S.; Zhang, Y.; Varvares, M.A.; Hoft, D.F.; Peng, G. Tumor-derived γδ regulatory T cells suppress innate and adaptive immunity through the induction of immunosenescence. J Immunol. 2013, 190, 2403–2414. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Morrissey, S.; Chen, F.; Yan, J. Novel Insight Into the Molecular and Metabolic Mechanisms Orchestrating IL-17 Production in γδ T Cells. Front Immunol. 2019, 10, 2828. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, D.; Yan, W.M.; Wang, H.W.; Huang, D.; Luo, X.P.; Ning, Q. γδ T Cells Contribute to the Outcome of Murine Fulminant Viral Hepatitis via Effector Cytokines TNF-α and IFN-γ. Curr. Med. Sci. 2018, 38, 648–655. [Google Scholar] [CrossRef]
- Chen, H.; Ji, X.; Cui, L.; Zhang, J.; He, W. Characterization of complementary determinant region 3δ in human MutS homologue 2-specific γδ T cells. Scand J Immunol. 2015, 81, 121–128. [Google Scholar] [CrossRef]
- He, Y.; Ma, N.; Xing, C.; Wang, X.; Xiao, H.; Zheng, M.; Han, G.; Chen, G.; Hou, C.; Shen, B.; et al. Novel IL-6-secreting γδT cells increased in patients with atherosclerotic cerebral infarction. Mol Med Rep. 2015, 11, 1497–1503. [Google Scholar] [CrossRef] [Green Version]
- Yang, X.; Kuang, S.; Wang, L.; Wei, Y. MHC class I chain-related A: Polymorphism, regulation and therapeutic value in cancer. Biomed Pharmacother. 2018, 103, 111–117. [Google Scholar] [CrossRef]
- Deng, W.; Gowen, B.G.; Zhang, L.; Wang, L.; Lau, S.; Iannello, A.; Xu, J.; Rovis, T.L.; Xiong, N.; Raulet, D.H. Antitumor immunity. A shed NKG2D ligand that promotes natural killer cell activation and tumor rejection. Science. 2015, 348, 136–139. [Google Scholar] [CrossRef] [Green Version]
- Steigerwald, J.; Raum, T.; Pflanz, S.; Cierpka, R.; Mangold, S.; Rau, D.; Hoffmann, P.; Kvesic, M.; Zube, C.; Linnerbauer, S.; et al. Human IgG1 antibodies antagonizing activating receptor NKG2D on natural killer cells. MAbs. 2009, 1, 115–127. [Google Scholar] [CrossRef] [Green Version]
- Cédile, O.; Popa, N.; Pollet-Villard, F.; Garmy, N.; Ibrahim, E.C.; Boucraut, J. The NKG2D ligands RAE-1δ and RAE-1ε differ with respect to their receptor affinity, expression profiles and transcriptional regulation. PLoS One. 2010, 5, e13466. [Google Scholar] [CrossRef] [Green Version]
- Routes, J.M.; Ryan, S.; Morris, K.; Takaki, R.; Cerwenka, A.; Lanier, L.L. Adenovirus serotype 5 E1A sensitizes tumor cells to NKG2D-dependent NK cell lysis and tumor rejection. J. Exp. Med. 2005, 202, 1477–1482. [Google Scholar] [CrossRef] [PubMed]
- Easom, N.J.W.; Stegmann, K.A.; Swadling, L.; Pallett, L.J.; Burton, A.R.; Odera, D.; Schmidt, N.; Huang, W.C.; Fusai, G.; Davidson, B.; et al. IL-15 Overcomes Hepatocellular Carcinoma-Induced NK Cell Dysfunction. Front Immunol. 2018, 9, 1009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, Q.; Ye, X.; Qu, X.; Cui, D.; Zhang, L.; Xu, Z.; Wan, H.; Zhang, L.; Tao, W. Discovery of a novel IL-15 based protein with improved developability and efficacy for cancer immunotherapy. Sci. Rep. 2018, 8, 7675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kavazović, I.; Lenartić, M.; Jelenčić, V.; Jurković, S.; Lemmermann, N.A.W.; Jonjić, S.; Polić, B.; Wensveen, F.M. NKG2D stimulation of CD8+ T cells during priming promotes their capacity to produce cytokines in response to viral infection in mice. Eur. J. Immunol. 2017, 47, 1123–1135. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Lotze, C.; Corso, M.; Baum, S.; Franke, K.J.; Pascual, J.I. Direct Imaging of the Induced-Fit Effect in Molecular Self-Assembly. Small. 2019, 15, e1804713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garrity, D.; Call, M.E.; Feng, J.; Wucherpfennig, K.W. The activating NKG2D receptor assembles in the membrane with two signaling dimers into a hexameric structure. Proc. Natl. Acad. Sci. USA 2005, 102, 7641–7646. [Google Scholar] [CrossRef] [Green Version]
- Molfetta, R.; Quatrini, L.; Santoni, A.; Paolini, R. Regulation of NKG2D-Dependent NK Cell Functions: The Yin and the Yang of Receptor Endocytosis. Int. J. Mol. Sci. 2017, 18, 1677. [Google Scholar] [CrossRef] [Green Version]
- Rojas, J.M.; Spada, R.; Sanz-Ortega, L.; Morillas, L.; Mejías, R.; Mulens-Arias, V.; Pérez-Yagüe, S.; Barber, D.F. PI3K p85 β regulatory subunit deficiency does not affect NK cell differentiation and increases NKG2D-mediated activation. J. Leukoc. Biol. 2016, 100, 1285–1296. [Google Scholar] [CrossRef]
- Graham, D.B.; Cella, M.; Giurisato, E.; Fujikawa, K.; Miletic, A.V.; Kloeppel, T.; Brim, K.; Takai, T.; Shaw, A.S.; Colonna, M.; et al. Vav1 controls DAP10-mediated natural cytotoxicity by regulating actin and microtubule dynamics. J. Immunol. 2006, 177, 2349–2355. [Google Scholar] [CrossRef]
- Giurisato, E.; Cella, M.; Takai, T.; Kurosaki, T.; Feng, Y.; Longmore, G.D.; Colonna, M.; Shaw, A.S. Phosphatidylinositol 3-kinase activation is required to form the NKG2D immunological synapse. Mol. Cell Biol. 2007, 27, 8583–8599. [Google Scholar] [CrossRef] [Green Version]
- Qu, X.; Lan, X.; Deng, C.; Zhou, J.; Du, J.; Huang, S.; Li, Y. Molecular mechanisms underlying the evolution of the slp76 signalosome. Sci. Rep. 2017, 7, 1509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiang, Y.J.; Jordan, M.S.; Horai, R.; Schwartzberg, P.L.; Koretzky, G.A.; Hodes, R.J. Cbl enforces an SLP76-dependent signaling pathway for T cell differentiation. J. Biol. Chem. 2009, 284, 4429–4438. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, Y.K.; Song, S.K.; Kim, B.W.; Park, S.K.; Chung, C.W.; Wang, H.J. Prognostic significance of microvascular invasion in tumor stage for hepatocellular carcinoma. World J. Surg. Oncol. 2017, 15, 225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, M.; Doyle, M.M.; Banan, B.; Vachharajani, N.; Wang, X.; Saad, N.; Fowler, K.; Brunt, E.M.; Lin, Y.; Chapman, W.C. Neoadjuvant Locoregional Therapy and Recurrent Hepatocellular Carcinoma after Liver Transplantation. J. Am. Coll. Surg. 2017, 225, 28–40. [Google Scholar] [CrossRef] [PubMed]
- Porsok, S.; Mego, M.; Pinďák, D.; Duchoň, R.; Beniak, J.; Mardiak, J. The Chest Wall Tumor as a Rare Clinical Presentation of Hepatocellular Carcinoma Metastasis. Klin Onkol. 2017, 30, 299–301. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.; Han, J.; Baek, J.S.; Tak, E.; Song, G.W.; Lee, S.G.; Jung, D.H.; Park, G.C.; Ahn, C.S.; Kim, N. Cytotoxicity of Human Hepatic Intrasinusoidal CD56bright Natural Killer Cells against Hepatocellular Carcinoma Cells. Int. J. Mol. Sci. 2019, 20, 1564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.S.; Fu, S.H.; Lu, K.C.; Chen, J.S.; Hsieh, H.Y.; Sytwu, H.K.; Wu, C.C. Inhibition of tumor necrosis factor signaling attenuates renal immune cell infiltration in experimental membranous nephropathy. Oncotarget. 2017, 8, 111631–111641. [Google Scholar] [CrossRef]
- Fan, S.; Zhang, J.; Nie, W.; Zhou, W.; Jin, L.; Chen, X.; Lu, J. Antitumor effects of polysaccharide from Sargassum fusiforme against human hepatocellular carcinoma HepG2 cells. Food Chem. Toxicol. 2017, 102, 53–62. [Google Scholar] [CrossRef]
- Mo, Z.; Lu, H.; Mo, S.; Fu, X.; Chang, S.; Yue, J. Ultrasound-guided radiofrequency ablation enhances natural killer-mediated antitumor immunity against liver cancer. Oncol. Lett. 2018, 15, 7014–7020. [Google Scholar] [CrossRef] [Green Version]
- Zekri, A.N.; El Deeb, S.; Bahnassy, A.A.; Badr, A.M.; Abdellateif, M.S.; Esmat, G.; Salama, H.; Mohanad, M.; El-Dien, A.E.; Rabah, S.; et al. Role of relevant immune-modulators and cytokines in hepatocellular carcinoma and premalignant hepatic lesions. World J. Gastroenterol. 2018, 24, 1228–1238. [Google Scholar] [CrossRef]
- Xu, P.; Sun, Z.; Wang, Y.; Miao, C. Long-term use of indomethacin leads to poor prognoses through promoting the expression of PD-1 and PD-L2 via TRIF/NF-κB pathway and JAK/STAT3 pathway to inhibit TNF-α and IFN-γ in hepatocellular carcinoma. Exp. Cell Res. 2015, 337, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Kuang, D.M.; Pan, W.D.; Wan, Y.L.; Lao, X.M.; Wang, D.; Li, X.F.; Zheng, L. Monocyte/macrophage-elicited natural killer cell dysfunction in hepatocellular carcinoma is mediated by CD48/2B4 interactions. Hepatology. 2013, 57, 1107–1116. [Google Scholar] [CrossRef] [PubMed]
- Lasfar, A.; de laTorre, A.; Abushahba, W.; Cohen-Solal, K.A.; Castaneda, I.; Yuan, Y.; Reuhl, K.; Zloza, A.; Raveche, E.; Laskin, D.L.; et al. Concerted action of IFN-α and IFN-λ induces local NK cell immunity and halts cancer growth. Oncotarget. 2016, 7, 49259–49267. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Q.F.; Yin, W.W.; Xia, Y.; Yi, Y.Y.; He, Q.F.; Wang, X.; Ren, H.; Zhang, D.Z. Liver-infiltrating CD11b-CD27- NK subsets account for NK-cell dysfunction in patients with hepatocellular carcinoma and are associated with tumor progression. Cell Mol. Immunol. 2017, 14, 819–829. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Lu, X.; Liu, W.; Chen, A.; Meng, G.; Zhang, H.; Li, B.; Zhang, Y.; Wu, J.; Wei, J. CD8+ T cells mediate the antitumor activity of frankincense and myrrh in hepatocellular carcinoma. J. Transl. Med. 2018, 16, 132. [Google Scholar] [CrossRef] [PubMed]
- Kishore Kumar, G.; Rajesh Kumar, G.; Mrudula Spurthi, K.; Nivas, S.; Chiranjeevi, P.; Ali, A.; Sahu, S.K.; Pratibha, N.; Surekha Rani, H. Polymorphisms of extrinsic death receptor apoptotic genes (FAS -670 G>A, FASL -844 T>C) in coronary artery disease. Apoptosis. 2016, 21, 558–565. [Google Scholar] [CrossRef]
- Ma, Y.; Han, C.C.; Li, Y.; Wang, Y.; Wei, W. Insulin-like growth factor-binding protein-3 inhibits IGF-1-induced proliferation of human hepatocellular carcinoma cells by controlling bFGF and PDGF autocrine/paracrine loops. Biochem. Biophys Res. Commun. 2016, 478, 964–969. [Google Scholar] [CrossRef]
- Zhang, S.; Xia, C.; Xu, C.; Liu, J.; Zhu, H.; Yang, Y.; Xu, F.; Zhao, J.; Chang, Y.; Zhao, Q. Early growth response 3 inhibits growth of hepatocellular carcinoma cells via upregulation of Fas ligand. Int. J. Oncol. 2017, 50, 805–814. [Google Scholar] [CrossRef]
- Ma, Y.; Gong, J.; Liu, Y.; Guo, W.; Jin, B.; Wang, X.; Chen, L. MicroRNA-30c promotes natural killer cell cytotoxicity via up-regulating the expression level of NKG2D. Life Sci. 2016, 151, 174–181. [Google Scholar] [CrossRef]
- Cai, E.; Guo, S.; Yang, L.; Han, M.; Xia, J.; Zhao, Y.; Gao, X.; Wang, Y. Synthesis and antitumour activity of arctigenin amino acid ester derivatives against H22 hepatocellular carcinoma. Nat. Prod. Res. 2018, 32, 406–411. [Google Scholar] [CrossRef]
- Lu, Z.; Cao, S.; Zhou, H.; Hua, L.; Zhang, S.; Cao, J. Mechanism of Arctigenin-Induced Specific Cytotoxicity against Human Hepatocellular CarcinomaCell Lines: Hep G2 and SMMC7721. PLoS One. 2015, 10, e0125727. [Google Scholar] [CrossRef]
- Lin, C.Z.; Xiang, G.L.; Zhu, X.H.; Xiu, L.L.; Sun, J.X.; Zhang, X.Y. Advances in the mechanisms of action of cancer-targeting oncolytic viruses. Oncol. Lett. 2018, 15, 4053–4060. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.; Zhang, Y.; Meng, G.; Jiang, D.; Zhang, H.; Zheng, M.; Xia, M.; Jiang, A.; Wu, J.; Beltinger, C.; et al. Oncolytic measles virus enhances antitumour responses of adoptive CD8+NKG2D+ cells in hepatocellular carcinoma treatment. Sci. Rep. 2017, 7, 5170. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Hagelsieb, G.; Vitug, B.; Medrano-Soto, A.; Saier, M.H., Jr. The Membrane Attack Complex/Perforin Superfamily. J. Mol. Microbiol. Biotechnol. 2017, 27, 252–267. [Google Scholar] [CrossRef] [Green Version]
- Li, X.F.; Dai, D.; Song, X.Y.; Liu, J.J.; Zhu, L.; Zhu, X.; Ma, W.; Xu, W. A different representation of natural T cells and natural killer cells between tumor-infiltrating and periphery lymphocytes in human hepatocellular carcinoma. Oncol. Lett. 2017, 13, 3291–3298. [Google Scholar] [CrossRef]
- Cheung, P.F.; Yip, C.W.; Ng, L.W.; Wong, C.K.; Cheung, T.T.; Lo, C.M.; Fan, S.T.; Cheung, S.T. Restoration of natural killer activity in hepatocellular carcinoma by treatment with antibody against granulin-epithelin precursor. Oncoimmunology. 2015, 4, e1016706. [Google Scholar] [CrossRef] [Green Version]
- Sun, H.; Huang, Q.; Huang, M.; Wen, H.; Lin, R.; Zheng, M.; Qu, K.; Li, K.; Wei, H.; Xiao, W.; et al. Human CD96 Correlates to Natural Killer Cell Exhaustion and Predicts the Prognosis of Human Hepatocellular Carcinoma. Hepatology. 2018, 70, 168–183. [Google Scholar] [CrossRef]
- Jiang, N.; Chen, W.; Jothikumar, P.; Patel, J.M.; Shashidharamurthy, R.; Selvaraj, P.; Zhu, C. Effects of anchor structure and glycosylation of Fcγ receptor III on ligand binding affinity. Mol. Biol. Cell. 2016, 27, 3449–3458. [Google Scholar] [CrossRef]
- Victor, A.R.; Weigel, C.; Scoville, S.D.; Chan, W.K.; Chatman, K.; Nemer, M.M.; Mao, C.; Young, K.A.; Zhang, J.; Yu, J.; et al. Epigenetic and Posttranscriptional Regulation of CD16 Expression during Human NK Cell Development. J. Immunol. 2018, 200, 565–572. [Google Scholar] [CrossRef]
- Di Modica, M.; Sfondrini, L.; Regondi, V.; Varchetta, S.; Oliviero, B.; Mariani, G.; Bianchi, G.V.; Generali, D.; Balsari, A.; Triulzi, T.; et al. Taxanes enhance trastuzumab-mediated ADCC on tumor cells through NKG2D-mediated NK cell recognition. Oncotarget. 2016, 7, 255–265. [Google Scholar] [CrossRef] [Green Version]
- Srpan, K.; Ambrose, A.; Karampatzakis, A.; Saeed, M.; Cartwright, A.N.R.; Guldevall, K.; De Matos, G.D.S.C.; Önfelt, B.; Davis, D.M. Shedding of CD16 disassembles the NK cell immune synapse and boosts serial engagement of target cells. J. Cell Biol. 2018, 217, 3267–3283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, H.R.; Son, C.H.; Koh, E.K.; Bae, J.H.; Kang, C.D.; Yang, K.; Park, Y.S. Expansion of cytotoxic natural killer cells using irradiated autologous peripheral blood mononuclear cells and anti-CD16 antibody. Sci. Rep. 2017, 7, 11075. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, G.; Chen, Y.C.; Reis, B.; Belousov, A.; Jukofsky, L.; Rossin, C.; Muehlig, A.; Xu, C.; Essioux, L.; Ohtomo, T.; et al. Combining expression of GPC3 in tumors and CD16 on NK cells from peripheral blood to identify patients responding to codrituzumab. Oncotarget. 2018, 9, 10436–10444. [Google Scholar] [CrossRef]
- Muntasell, A.; Ochoa, M.C.; Cordeiro, L.; Berraondo, P.; de Lopez-Díaz, C.A.; Cabo, M.; López-Botet, M.; Melero, I. Targeting NK-cell checkpoints for cancer immunotherapy. Curr Opin Immunol. 2017, 45, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Ding, H.; Yang, X.; Wei, Y. Fusion Proteins of NKG2D/NKG2DL in Cancer Immunotherapy. Int. J. Mol. Sci. 2018, 19, 177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Figiel, M.; Bonarek, P.; Górecki, A.; Pawlak, S.D.; Zerek, B.; Checinska, B.; Pieczykolan, J.; Dziedzicka-Wasylewska, M. Improved cytotoxicity of novel TRAIL variants produced as recombinant fusion proteins. Protein Eng. Des. Sel. 2018, 31, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Thakor, P.; Subramanian, R.B.; Thakkar, S.S.; Ray, A.; Thakkar, V.R. Phytol induces ROS mediated apoptosis by induction of caspase 9 and 3 through activation of TRAIL, FAS and TNF receptors and inhibits tumor progression factor Glucose 6 phosphate dehydrogenase in lung carcinoma cell line (A549). Biomed Pharmacother. 2017, 92, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Ohira, M.; Nishida, S.; Tryphonopoulos, P.; Tekin, A.; Selvaggi, G.; Moon, J.; Levi, D.; Ricordi, C.; Ishiyama, K.; Tanaka, Y.; et al. Clinical-scale isolation of interleukin-2-stimulated liver natural killer cells for treatment of liver transplantation with hepatocellular carcinoma. Cell Transplant. 2012, 21, 1397–1406. [Google Scholar] [CrossRef] [Green Version]
- Jiang, W.; Zhang, C.; Tian, Z.; Zhang, J. hIL-15 gene-modified human natural killer cells (NKL-IL15) augments the anti-human hepatocellular carcinoma effect in vivo. Immunobiology. 2014, 219, 547–553. [Google Scholar] [CrossRef]
- Bálint, Š.; Lopes, F.B.; Davis, D.M. A nanoscale reorganization of the IL-15 receptor is triggered by NKG2D in a ligand-dependent manner. Sci. Signal. 2018, 11, eaal3606. [Google Scholar] [CrossRef] [Green Version]
- Liu, P.; Chen, L.; Zhang, H. Natural Killer Cells in Liver Disease and Hepatocellular Carcinoma and the NK Cell-Based Immunotherapy. J Immunol Res. 2018, 2018, 1206737. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cai, L.; Zhang, Z.; Zhou, L.; Wang, H.; Fu, J.; Zhang, S.; Shi, M.; Zhang, H.; Yang, Y.; Wu, H.; et al. Functional impairment in circulating and intrahepatic NK cells and relative mechanism in hepatocellular carcinoma patients. Clin Immunol. 2008, 129, 428–437. [Google Scholar] [CrossRef] [PubMed]
- Pollicino, T.; Koumbi, L. Role natural killer group 2D-ligand interactions in hepatitis B infection. World J Hepatol. 2015, 7, 819–824. [Google Scholar] [CrossRef] [PubMed]
- Kamiya, T.; Chang, Y.H.; Campana, D. Expanded and Activated Natural Killer Cells for Immunotherapy of Hepatocellular Carcinoma. Cancer Immunol Res. 2016, 4, 574–581. [Google Scholar] [CrossRef] [Green Version]
- Han, Y.; Sun, F.; Zhang, X.; Wang, T.; Jiang, J.; Cai, J.; Gao, Q.; Hezam, K.; Liu, Y.; Xie, J.; et al. CD24 targeting bi-specific antibody that simultaneously stimulates NKG2D enhances the efficacy of cancer immunotherapy. J Cancer Res Clin Oncol. 2019, 145, 1179–1190. [Google Scholar] [CrossRef]
- Sun, B.; Yang, D.; Dai, H.; Liu, X.; Jia, R.; Cui, X.; Li, W.; Cai, C.; Xu, J.; Zhao, X. Eradication of Hepatocellular Carcinoma by NKG2D-Based CAR-T Cells. Cancer Immunol Res. 2019, 7, 1813–1823. [Google Scholar] [CrossRef]
- Sheppard, S.; Guedes, J.; Mroz, A.; Zavitsanou, A.M.; Kudo, H.; Rothery, S.M.; Angelopoulos, P.; Goldin, R.; Guerra, N. The immunoreceptor NKG2D promotes tumour growth in a model of hepatocellular carcinoma. Nat. Commun. 2017, 8, 13930. [Google Scholar] [CrossRef]
- Oh, S.; Lee, J.H.; Kwack, K.; Choi, S.W. Natural Killer Cell Therapy: A New Treatment Paradigm for Solid Tumors. Cancers 2019, 11, E1534. [Google Scholar] [CrossRef] [Green Version]
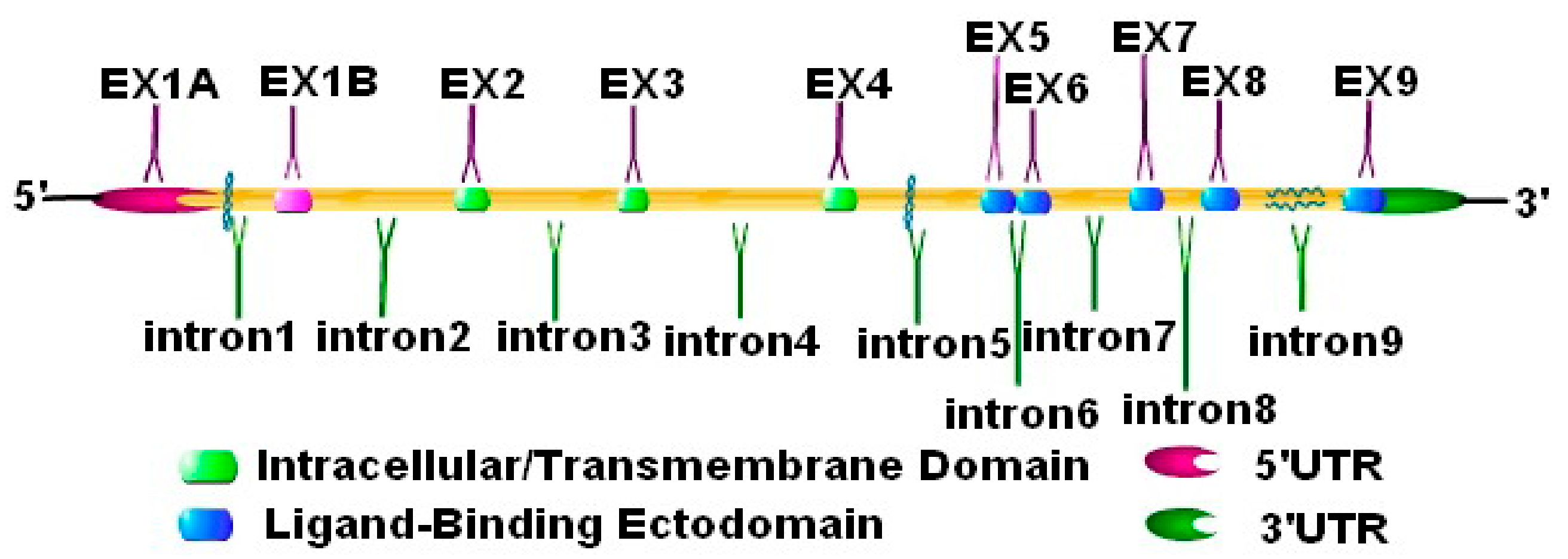
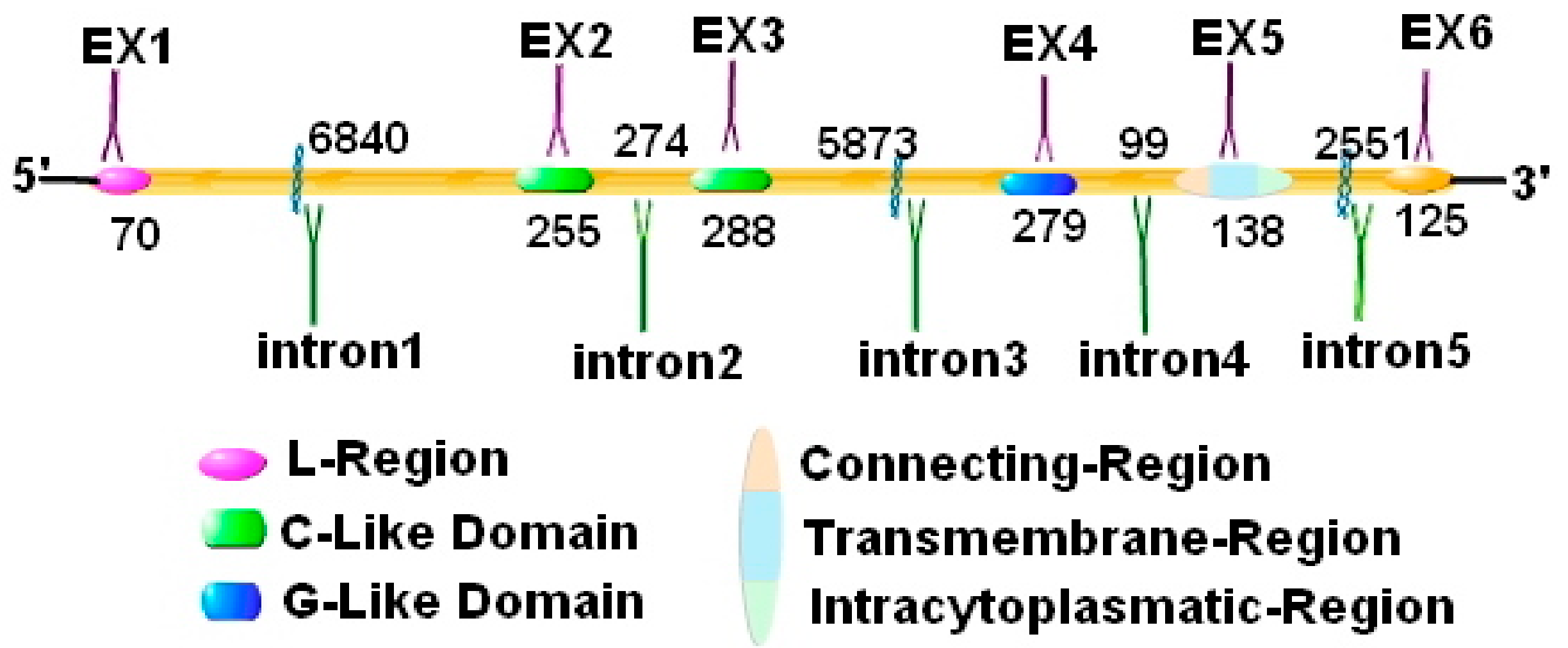
| Functional Classification | Structural Classification | Receptor in Human | Chromosome Localization | Number of Exons | Receptor in Mouse | Chromosome Localization | Number of Exons |
|---|---|---|---|---|---|---|---|
| Activating receptor | NCR | NKp46 or Ly94 or Mar-1 | 19p13.42 | 9 | NKp46 or NCR1 | 7; 7 A1 | 7 |
| NKp30 | 6p21.32 | 5 | \ | \ | \ | ||
| NKp44 | 6p21.1 | 6 | \ | \ | \ | ||
| FcγRⅢ/CD16/FCG3/FCGR3 | 1q23.3 | 7 | FcγRⅢ/CD16 | 1H3; 178.8 cM | 9 | ||
| Type C lectin like receptor (CD94/NKG2 family) | NKG2D | 12p12.3-p13.1 | 8\9\10 | NKG2D (Main) | 6 F3; 6 63.44 cM | 9 | |
| CD94/NKG2C | 12p13.2 | 6 | CD94/NKG2C | 6; 6 F3 | 7 | ||
| CD94/NKG2E | 12p13.2 | 7 | CD94/NKG2E | 6; 6 F3 | 7 | ||
| CD94/NKG2F | 12p13.2 | 4 | CD94/NKG2F | \ | \ | ||
| CD161 | 12p13.31 | 6 | CD161 | 6 F3; 6 63.09 cM | 6 | ||
| Ly49d Ly49h | 6 F3; 6 63.44 cM 6 F3; 6 63.44 cM | 7 8 | |||||
| KIRs | KIR2DS1 | 19q13.4 | 11 | — | — | — | |
| KIR2DS4 | 19q13.42 | 8 | — | — | — | ||
| KIR2DL4 | 19q13.42 | 8 | — | — | — | ||
| Inhibitory receptor | Type C lectin like receptor | CD94/NKG2A | 12p13.2 | 9 | Ly49a、c、g、i | 6 F3; 6 63.44 cM 6 F3; 6 63.44 cM 6 F3; 6 63.44 cM 6 F3; 6 63.44 cM | 9 7 9 9 |
| CD94/NKG2B | 12p13.2 | 13 | — | — | — | ||
| PD-1 [26] | 2q37.35 | 6 | PD-1/Pdc1/Ly101 | 1;1D | 5 | ||
| Siglec-7 | 19q13.41 | 7 | — | — | — | ||
| KIRs | KIR2DL1 | 19q13.42 | 11 | — | — | — | |
| KIR2DL2 KIR2DL3 | 19q13.4 19q13.42 | 9 8 | — | — | — | ||
| KIR3DL1 | 19q13.42 | 9 | — | — | — |
| Type | Human | Murine Mouse |
|---|---|---|
| NK cells | 100%; Unactivated: 100% | 100% |
| CD8+ αβT cells | After activation: 100%; Memory cells: 100% | After activation: 100%; Memory cells: 100% |
| CD4+ αβ T cells | Usually lack | Few express |
| γδT cells | Peripheral γδT cells: 100%; Small intestinal epithelial cells: Absent | Dendritic epithelium γδT cells: 100%; Unactivated: absent. The spleen γδT Cells: 25%. Small intestinal epithelial cells: absent |
| NK1.1+ T cells | Undiscover | 70% Positive |
| Invariant NKT cells (iNKT) [38] | Usually express | Usually express |
| Innate lymphoid cells (ILCs) [39] | Usually express | Usually express |
| Macrophages | Absent | LPS; IFNα/β or IFN-γ; After activation: 100% |
| Thymocyte | Single positive CD8+ T cells | Undiscover |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, J.; Li, C.-D.; Sun, L. Recent Advances in Molecular Mechanisms of the NKG2D Pathway in Hepatocellular Carcinoma. Biomolecules 2020, 10, 301. https://doi.org/10.3390/biom10020301
Wang J, Li C-D, Sun L. Recent Advances in Molecular Mechanisms of the NKG2D Pathway in Hepatocellular Carcinoma. Biomolecules. 2020; 10(2):301. https://doi.org/10.3390/biom10020301
Chicago/Turabian StyleWang, Jian, Cun-Di Li, and Lin Sun. 2020. "Recent Advances in Molecular Mechanisms of the NKG2D Pathway in Hepatocellular Carcinoma" Biomolecules 10, no. 2: 301. https://doi.org/10.3390/biom10020301




