Assessment of Selected Clock Proteins (CLOCK and CRY1) and Their Relationship with Biochemical, Anthropometric, and Lifestyle Parameters in Hypertensive Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Study Design
2.2.1. Blood Pressure Measurement
2.2.2. Anthropometric Parameters
2.2.3. Diet Content Analysis
2.2.4. Physical Activity and Quality of Sleep
2.2.5. Biochemical Parameters
2.2.6. CLOCK and CRY1 Measurement
2.2.7. TAS Measurement
2.3. Statistical Analysis
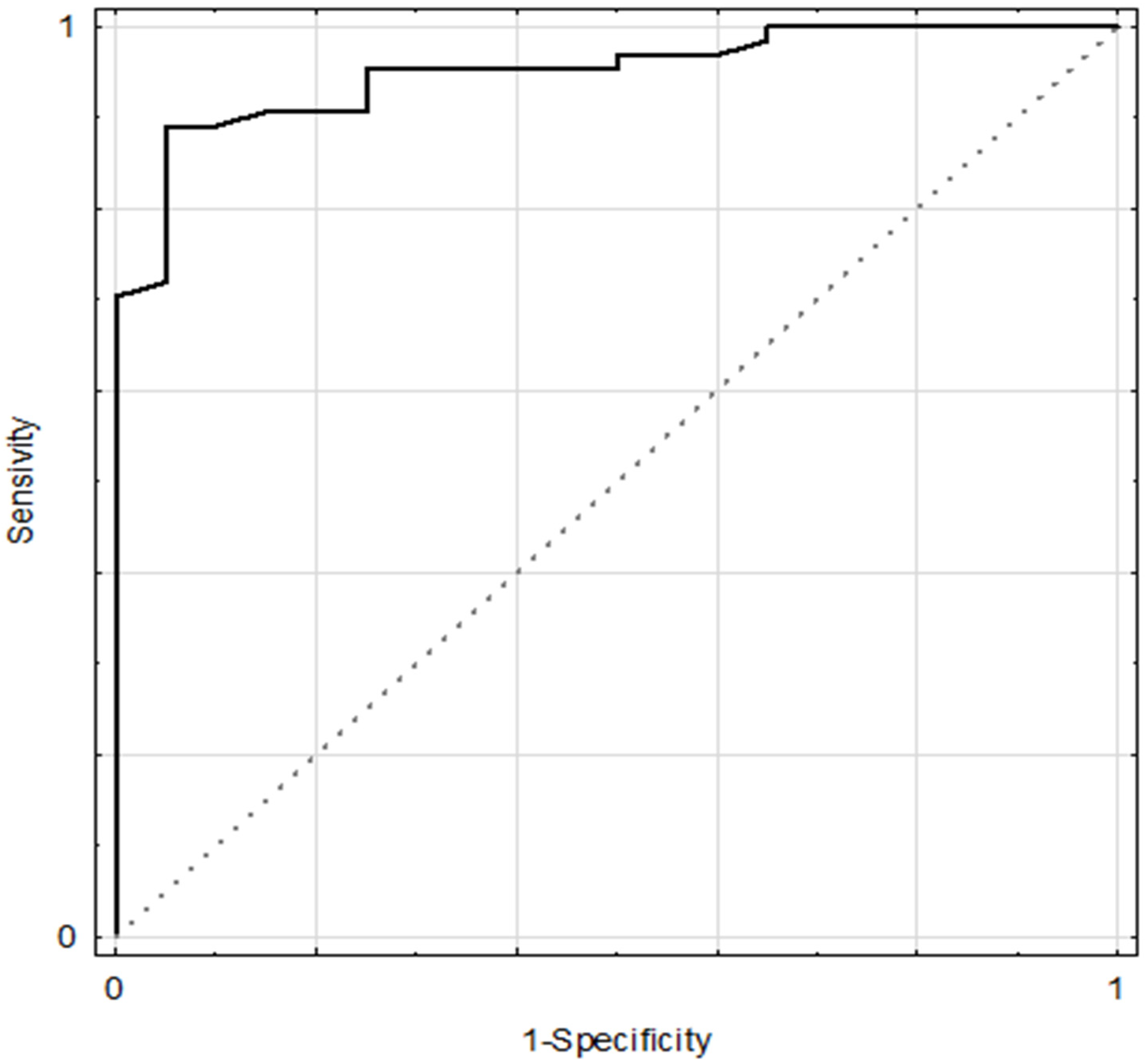
3. Results
4. Discussion
Limitations and Strength of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dibner, C.; Schibler, U.; Albrecht, U. The mammalian circadian timing system: Organization and coordination of central and peripheral clocks. Annu. Rev. Physiol. 2010, 72, 517–549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aoyama, S.; Shibata, S. The role of circadian rhythms in muscular and osseous physiology and their regulation by nutrition and exercise. Front. Neurosci. 2017, 11. [Google Scholar] [CrossRef] [Green Version]
- Richards, J.; Gumz, M.L. Advances in understanding the peripheral circadian clocks. FASEB J. 2012, 26, 3602–3613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marcheva, B.; Ramsey, K.M.; Peek, C.B.; Affinati, A.; Maury, E.; Bass, J. Circadian clocks and metabolism. Handb. Exp. Pharmacol. 2013, 127–155. [Google Scholar] [CrossRef] [Green Version]
- Partch, C.L.; Green, C.B.; Takahashi, J.S. Molecular architecture of the mammalian circadian clock. Trends Cell Biol. 2014, 24, 90–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albrecht, U.; Eichele, G. The mammalian circadian clock. Curr. Opin. Genet. Dev. 2003, 13, 271–277. [Google Scholar] [CrossRef]
- Yamanaka, Y.; Hashimoto, S.; Masubuchi, S.; Natsubori, A.; Nishide, S.; Honma, S.; Honma, K. Differential regulation of circadian melatonin rhythm and sleep-wake cycle by bright lights and nonphotic time cues in humans. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2014, 307, R546–R557. [Google Scholar] [CrossRef]
- Xie, Y.; Tang, Q.; Chen, G.; Xie, M.; Yu, S.; Zhao, J.; Chen, L. New insights into the circadian rhythm and its related diseases. Front. Physiol. 2019, 10. [Google Scholar] [CrossRef] [Green Version]
- Buijs, F.N.; León-Mercado, L.; Guzmán-Ruiz, M.; Guerrero-Vargas, N.N.; Romo-Nava, F.; Buijs, R.M. The circadian system: A regulatory feedback network of periphery and brain. Physiology (Bethesda) 2016, 31, 170–181. [Google Scholar] [CrossRef]
- Hermida, R.C.; Ayala, D.E.; Smolensky, M.H.; Mojón, A.; Fernández, J.R.; Crespo, J.J.; Moyá, A.; Ríos, M.T.; Portaluppi, F. Chronotherapy improves blood pressure control and reduces vascular risk in CKD. Nat. Rev. Nephrol. 2013, 9, 358–368. [Google Scholar] [CrossRef]
- Witte, K.; Schnecko, A.; Buijs, R.M.; van der Vliet, J.; Scalbert, E.; Delagrange, P.; Guardiola-Lemaitre, B.; Lemmer, B. Effects of SCN lesions on orcadian blood pressure rhythm in normotensive and transgenic hypertensive rats. Chronobiol. Int. 1998, 15, 135–145. [Google Scholar] [CrossRef]
- Dierickx, P.; Van Laake, L.W.; Geijsen, N. Circadian clocks: From stem cells to tissue homeostasis and regeneration. EMBO Rep. 2018, 19, 18–28. [Google Scholar] [CrossRef]
- Asher, G.; Sassone-Corsi, P. Time for food: The intimate interplay between nutrition, metabolism, and the circadian clock. Cell 2015, 161, 84–92. [Google Scholar] [CrossRef] [Green Version]
- Froy, O. Circadian rhythms, nutrition and implications for longevity in urban environments. Proc. Nutr. Soc. 2018, 77, 216–222. [Google Scholar] [CrossRef]
- Johnston, J.D. Physiological links between circadian rhythms, metabolism and nutrition. Exp. Physiol. 2014, 99, 1133–1137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bollinger, T.; Schibler, U. Circadian rhythms – from genes to physiology and disease. Swiss Med. Wkly. 2014, 144. [Google Scholar] [CrossRef]
- Bass, J. Circadian topology of metabolism. Nature 2012, 491, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Lahens, N.F.; Ballance, H.I.; Hughes, M.E.; Hogenesch, J.B. A circadian gene expression atlas in mammals: Implications for biology and medicine. Proc. Natl. Acad. Sci. USA 2014, 111, 16219–16224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richards, J.; Diaz, A.N.; Gumz, M.L. Clock genes in hypertension: Novel insights from rodent models. Blood Press. Monit. 2014, 19, 249–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rhoads, M.K.; Balagee, V.; Thomas, S.J. Circadian regulation of blood pressure: Of mice and men. Curr. Hypertens. Rep. 2020, 22, 40. [Google Scholar] [CrossRef] [PubMed]
- Lamia, K.A.; Papp, S.J.; Yu, R.T.; Barish, G.D.; Uhlenhaut, N.H.; Jonker, J.W.; Downes, M.; Evans, R.M. Cryptochromes mediate rhythmic repression of the glucocorticoid receptor. Nature 2011, 480, 552–556. [Google Scholar] [CrossRef] [PubMed]
- Bhatnagar, A. Environmental determinants of cardiovascular disease. Circ. Res. 2017, 121, 162–180. [Google Scholar] [CrossRef] [PubMed]
- Douma, L.G.; Gumz, M.L. Circadian clock-mediated regulation of blood pressure. Free Radic. Biol. Med. 2018, 119, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J. Hypertens. 2018, 36, 1953–2041. [Google Scholar] [CrossRef] [Green Version]
- Timio, M.; Venanzi, S.; Lolli, S.; Lippi, G.; Verdura, C.; Monarca, C.; Guerrini, E. “Non-dipper” hypertensive patients and progressive renal insufficiency: A 3-year longitudinal study. Clin. Nephrol. 1995, 43, 382–387. [Google Scholar]
- Krzych, Ł.J.; Bochenek, A. Blood pressure variability: Epidemiological and clinical issues. Cardiol. J. 2013, 20, 112–120. [Google Scholar] [CrossRef]
- Mahabala, C.; Kamath, P.; Bhaskaran, U.; Pai, N.D.; Pai, A.U. Antihypertensive therapy: Nocturnal dippers and nondippers. Do we treat them differently? Vasc. Health Risk Manag. 2013, 9, 125–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de la Sierra, A.; Gorostidi, M.; Banegas, J.R.; Segura, J.; de la Cruz, J.J.; Ruilope, L.M. Nocturnal hypertension or nondipping: Which is better associated with the cardiovascular risk profile? Am. J. Hypertens. 2014, 27, 680–687. [Google Scholar] [CrossRef]
- Aksit, E.; Gursul, E.; Aydin, F.; Samsa, M.; Ozcelik, F. Non-dipper hypertension is associated with slow coronary flow among hypertensives with normal coronary angiogram. Cardiovasc. J. Afr. 2017, 28, 14–18. [Google Scholar] [CrossRef] [Green Version]
- Takeda, N.; Maemura, K. Circadian clock and cardiovascular disease. J. Cardiol. 2011, 57, 249–256. [Google Scholar] [CrossRef] [Green Version]
- Morris, C.J.; Purvis, T.E.; Hu, K.; Scheer, F.A.J.L. Circadian misalignment increases cardiovascular disease risk factors in humans. Proc. Natl. Acad. Sci. USA 2016, 113, E1402–E1411. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Mei, H.; Jiang, Y.-R.; Sun, W.-Q.; Song, Y.-J.; Liu, S.-J.; Jiang, F. Relationship between duration of sleep and hypertension in adults: A meta-analysis. J. Clin. Sleep Med. 2015, 11, 1047–1056. [Google Scholar] [CrossRef]
- Wehrens, S.M.T.; Christou, S.; Isherwood, C.; Middleton, B.; Gibbs, M.A.; Archer, S.N.; Skene, D.J.; Johnston, J.D. Meal timing regulates the human circadian system. Curr. Biol. 2017, 27, 1768–1775.e3. [Google Scholar] [CrossRef] [Green Version]
- Serin, Y.; Acar Tek, N. Effect of circadian rhythm on metabolic processes and the regulation of energy balance. Ann. Nutr. Metab. 2019, 74, 322–330. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Yang, G. Recent advances in circadian rhythms in cardiovascular system. Front. Pharmacol. 2015, 6. [Google Scholar] [CrossRef] [Green Version]
- Morris, C.J.; Purvis, T.E.; Mistretta, J.; Hu, K.; Scheer, F.A.J.L. Circadian misalignment increases c-reactive protein and blood pressure in chronic shift workers. J. Biol. Rhythm. 2017, 32, 154–164. [Google Scholar] [CrossRef] [Green Version]
- Yan, B.; Yan, H.; Sun, L.; Yan, X.; Peng, L.; Wang, Y.; Wang, G. Novel association between the reverse-dipper pattern of ambulatory blood pressure monitoring and metabolic syndrome in men but not in women. Medicine (Baltimore) 2015, 94. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson Kenneth, A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [CrossRef] [PubMed] [Green Version]
- Tykarski, A.; Filipiak, K.J.; Januszewicz, A.; Litwin, M.; Narkiewicz, K.; Prejbisz, A.; Ostalska-Nowicka, D.; Widecka, K.; Kostka-Jeziorny, K. 2019 Guidelines for the management of hypertension—Part 1–7. Arter. Hypertens. 2019, 23, 41–87. [Google Scholar] [CrossRef] [Green Version]
- Knopfholz, J.; Disserol, C.C.D.; Pierin, A.J.; Schirr, F.L.; Streisky, L.; Takito, L.L.; Massucheto Ledesma, P.; Faria-Neto, J.R.; Olandoski, M.; da Cunha, C.L.P.; et al. Validation of the Friedewald formula in patients with metabolic syndrome. Cholesterol 2014, 2014, 261878. [Google Scholar] [CrossRef] [Green Version]
- Chen, R.; Schirmer, A.; Lee, Y.; Lee, H.; Kumar, V.; Yoo, S.-H.; Takahashi, J.S.; Lee, C. Rhythmic PER abundance defines a critical nodal point for negative feedback within the circadian clock mechanism. Mol. Cell 2009, 36, 417–430. [Google Scholar] [CrossRef] [Green Version]
- Doi, M.; Takahashi, Y.; Komatsu, R.; Yamazaki, F.; Yamada, H.; Haraguchi, S.; Emoto, N.; Okuno, Y.; Tsujimoto, G.; Kanematsu, A.; et al. Salt-sensitive hypertension in circadian clock-deficient Cry-null mice involves dysregulated adrenal Hsd3b6. Nat. Med. 2010, 16, 67–74. [Google Scholar] [CrossRef]
- Nugrahaningsih, D.A.A.; Emoto, N.; Vignon-Zellweger, N.; Purnomo, E.; Yagi, K.; Nakayama, K.; Doi, M.; Okamura, H.; Hirata, K. Chronic hyperaldosteronism in Cryptochrome-null mice induces high-salt- and blood pressure-independent kidney damage in mice. Hypertens. Res. 2014, 37, 202–209. [Google Scholar] [CrossRef] [Green Version]
- Jordan, S.D.; Kriebs, A.; Vaughan, M.; Duglan, D.; Fan, W.; Henriksson, E.; Huber, A.-L.; Papp, S.J.; Nguyen, M.; Afetian, M.; et al. CRY1/2 selectively repress PPARδ and limit exercise capacity. Cell Metab. 2017, 26, 243–255.e6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kriebs, A.; Jordan, S.D.; Soto, E.; Henriksson, E.; Sandate, C.R.; Vaughan, M.E.; Chan, A.B.; Duglan, D.; Papp, S.J.; Huber, A.-L.; et al. Circadian repressors CRY1 and CRY2 broadly interact with nuclear receptors and modulate transcriptional activity. Proc. Natl. Acad. Sci. USA 2017, 114, 8776–8781. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyer-Kovac, J.; Kolbe, I.; Ehrhardt, L.; Leliavski, A.; Husse, J.; Salinas, G.; Lingner, T.; Tsang, A.H.; Barclay, J.L.; Oster, H. Hepatic gene therapy rescues high-fat diet responses in circadian Clock mutant mice. Mol. Metab. 2017, 6, 512–523. [Google Scholar] [CrossRef] [PubMed]
- Zuber, A.M.; Centeno, G.; Pradervand, S.; Nikolaeva, S.; Maquelin, L.; Cardinaux, L.; Bonny, O.; Firsov, D. Molecular clock is involved in predictive circadian adjustment of renal function. Proc. Natl. Acad. Sci. USA 2009, 106, 16523–16528. [Google Scholar] [CrossRef] [Green Version]
- Nikolaeva, S.; Pradervand, S.; Centeno, G.; Zavadova, V.; Tokonami, N.; Maillard, M.; Bonny, O.; Firsov, D. The circadian clock modulates renal sodium handling. J. Am. Soc. Nephrol. JASN 2012, 23, 1019–1026. [Google Scholar] [CrossRef]
- Alibhai, F.J.; LaMarre, J.; Reitz, C.J.; Tsimakouridze, E.V.; Kroetsch, J.T.; Bolz, S.-S.; Shulman, A.; Steinberg, S.; Burris, T.P.; Oudit, G.Y.; et al. Disrupting the key circadian regulator CLOCK leads to age-dependent cardiovascular disease. J. Mol. Cell. Cardiol. 2017, 105, 24–37. [Google Scholar] [CrossRef] [Green Version]
- Anea, C.B.; Zhang, M.; Stepp, D.W.; Simkins, G.B.; Reed, G.; Fulton, D.J.; Rudic, R.D. Vascular disease in mice with a dysfunctional circadian clock. Circulation 2009, 119, 1510–1517. [Google Scholar] [CrossRef] [Green Version]
- Tedjasukmana, R.; Purba, J.S.; Wanandi, S.I.; Suyatna, F.D. Neuroglobin correlates with cryptochrome-1 in obstructive sleep apnea with primary aldosteronism. PLoS ONE 2018, 13, e0204390. [Google Scholar] [CrossRef] [PubMed]
- Kovanen, L.; Donner, K.; Kaunisto, M.; Partonen, T. CRY1, CRY2 and PRKCDBP genetic variants in metabolic syndrome. Hypertens. Res. 2015, 38, 186–192. [Google Scholar] [CrossRef]
- Lamia, K.A.; Sachdeva, U.M.; DiTacchio, L.; Williams, E.C.; Alvarez, J.G.; Egan, D.F.; Vasquez, D.S.; Juguilon, H.; Panda, S.; Shaw, R.J.; et al. AMPK regulates the circadian clock by cryptochrome phosphorylation and degradation. Science 2009, 326, 437–440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hardie, D.G. AMP-activated/SNF1 protein kinases: Conserved guardians of cellular energy. Nat. Rev. Mol. Cell Biol. 2007, 8, 774–785. [Google Scholar] [CrossRef] [PubMed]
- Faulkner, J.L.; Belin de Chantemèle, E.J. Sex differences in mechanisms of hypertension associated with obesity. Hypertension 2018, 71, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Nwankwo, M.; Okamkpa, J.C.; Danborno, B. Association between high blood pressure with risk of type 2 diabetes, metabolic syndrome and its predictors: A cross-sectional study. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 1549–1554. [Google Scholar] [CrossRef]
- Choudhury, K.N.; Mainuddin, A.K.M.; Wahiduzzaman, M.; Islam, S.M.S. Serum lipid profile and its association with hypertension in Bangladesh. Vasc. Health Risk Manag. 2014, 10, 327–332. [Google Scholar] [CrossRef] [Green Version]
- Aronow, W.S. Association of obesity with hypertension. Ann. Transl. Med. 2017, 5. [Google Scholar] [CrossRef] [Green Version]
- Mulè, G.; Calcaterra, I.; Nardi, E.; Cerasola, G.; Cottone, S. Metabolic syndrome in hypertensive patients: An unholy alliance. World J. Cardiol. 2014, 6, 890–907. [Google Scholar] [CrossRef]
- Lee, S.-R.; Cha, M.-J.; Kang, D.-Y.; Oh, K.-C.; Shin, D.-H.; Lee, H.-Y. Increased prevalence of metabolic syndrome among hypertensive population: Ten years’ trend of the Korean National Health and Nutrition Examination Survey. Int. J. Cardiol. 2013, 166, 633–639. [Google Scholar] [CrossRef]
- Kharroubi, A.T.; Darwish, H.M.; Akkawi, M.A.; Ashareef, A.A.; Almasri, Z.A.; Bader, K.A.; Khammash, U.M. Total antioxidant status in type 2 diabetic patients in Palestine. J. Diabetes Res. 2015, 2015, 461271. [Google Scholar] [CrossRef] [Green Version]
- Chaudhary, P.; Pandey, A.; Azad, C.S.; Tia, N.; Singh, M.; Gambhir, I.S. Association of oxidative stress and endothelial dysfunction in hypertension. Anal. Biochem. 2020, 590, 113535. [Google Scholar] [CrossRef] [PubMed]
- Yavari, A.; Javadi, M.; Mirmiran, P.; Bahadoran, Z. Exercise-induced oxidative stress and dietary antioxidants. Asian J. Sports Med. 2015, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Villaverde, P.; Lajous, M.; MacDonald, C.-J.; Fagherazzi, G.; Bonnet, F.; Boutron-Ruault, M.-C. High dietary total antioxidant capacity is associated with a reduced risk of hypertension in French women. Nutr. J. 2019, 18, 31. [Google Scholar] [CrossRef] [PubMed]
- Ozemek, C.; Laddu, D.R.; Arena, R.; Lavie, C.J. The role of diet for prevention and management of hypertension. Curr. Opin. Cardiol. 2018, 33, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Pescatello, L.S.; Buchner, D.M.; Jakicic, J.M.; Powell, K.E.; Kraus, W.E.; Bloodgood, B.; Campbell, W.W.; Dietz, S.; Dipietro, L.; George, S.M.; et al. Physical activity to prevent and treat hypertension: A systematic review. Med. Sci. Sports Exerc. 2019, 51, 1314–1323. [Google Scholar] [CrossRef]
- Diaz, K.M.; Shimbo, D. Physical activity and the prevention of hypertension. Curr. Hypertens. Rep. 2013, 15, 659–668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rossi, A.; Dikareva, A.; Bacon, S.L.; Daskalopoulou, S.S. The impact of physical activity on mortality in patients with high blood pressure: A systematic review. J. Hypertens. 2012, 30, 1277–1288. [Google Scholar] [CrossRef] [Green Version]
- Nicoll, R.; Henein, M.Y. Caloric restriction and its effect on blood pressure, heart rate variability and arterial stiffness and dilatation: A review of the evidence. Int. J. Mol. Sci. 2018, 19, 751. [Google Scholar] [CrossRef] [Green Version]
- Ndanuko, R.N.; Tapsell, L.C.; Charlton, K.E.; Neale, E.P.; Batterham, M.J. Dietary patterns and blood pressure in adults: A systematic review and meta-analysis of randomized controlled trials. Adv. Nutr. (Bethesda) 2016, 7, 76–89. [Google Scholar] [CrossRef] [PubMed]
- Turek, F.W.; Joshu, C.; Kohsaka, A.; Lin, E.; Ivanova, G.; McDearmon, E.; Laposky, A.; Losee-Olson, S.; Easton, A.; Jensen, D.R.; et al. Obesity and metabolic syndrome in circadian Clock mutant mice. Science 2005, 308, 1043–1045. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kohsaka, A.; Laposky, A.D.; Ramsey, K.M.; Estrada, C.; Joshu, C.; Kobayashi, Y.; Turek, F.W.; Bass, J. High-fat diet disrupts behavioral and molecular circadian rhythms in mice. Cell Metab. 2007, 6, 414–421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pendergast, J.S.; Branecky, K.L.; Yang, W.; Ellacott, K.L.J.; Niswender, K.D.; Yamazaki, S. High-fat diet acutely affects circadian organisation and eating behavior. Eur. J. Neurosci. 2013, 37, 1350–1356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grandner, M.; Mullington, J.M.; Hashmi, S.D.; Redeker, N.S.; Watson, N.F.; Morgenthaler, T.I. Sleep duration and hypertension: Analysis of > 700,000 adults by age and sex. J. Clin. Sleep Med. 2018, 14, 1031–1039. [Google Scholar] [CrossRef]
- Li, M.; Yan, S.; Jiang, S.; Ma, X.; Gao, T.; Li, B. Relationship between sleep duration and hypertension in northeast China: A cross-sectional study. BMJ Open 2019, 9, e023916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Parameter (Unit) | HT (n = 31) | NHT (n = 55) | p-Value |
|---|---|---|---|
| SBP (mmHg) | 144.10 ± 19.18 | 114.80 ± 12.13 | p < 0.0000001 ** |
| DBP (mmHg) | 89.81 ± 11.36 | 71.17 ± 7.8 | p < 0.0000001 ** |
| Body weight (kg) | 90.94 ± 21.65 | 72.35 ± 13.93 | p < 0.00003 ** |
| BMI (kg/m2) | 31.18 ± 6.95 | 25.19 ± 4.75 | p < 0.0001 ** |
| WHR | 0.88 ± 0.07 | 0.79 ± 0.06 | p < 0.0000001 ** |
| Total body fat mass (%) | 38.25 ± 6.50 | 31.38 ± 6.76 | p < 0.0004 ** |
| FBG (mmol/L) | 5.71 ± 1.06 | 5.03 ± 0.43 | p < 0.00002 ** |
| TC (mmol/L) | 5.35 ± 1.24 | 4.95 ± 0.95 | NS * |
| TG (mmol/L) | 1.58 ± 0.81 | 0.99 ± 0.57 | p < 0.00005 ** |
| HDL (mmol/L) | 1.54 ± 0.4 | 1.7 ± 0.44 | NS * |
| LDL (mmol/L) | 3.29 ± 1.32 | 2.95 ± 0.9 | NS * |
| CLOCK (ng/mL) | 1.89 ± 0.67 | 1.96 ± 0.63 | NS ** |
| CRY1 (ng/mL) | 0.67 ± 0.32 | 1.07 ± 0.89 | p < 0.01 * |
| TAS (mmol/L) | 1.32 ± 0.28 | 1.34 ± 0.25 | NS * |
| Parameter (Unit) | Fat-Free Mass Index | A Body Shape Index | TAS (mmol/L) |
|---|---|---|---|
| CRY1 (ng/mL) | R = −0.45 ** p < 0.041 ** | R = 0.40 * p < 0.035 * | R = 0.47 * p < 0.032 * |
| CLOCK (ng/mL) | NS ** | R = 0.49 ** p < 0.006 ** | R = 0.46 * p < 0.036 * |
| Statistical Parameters | A Model Including Two Variables: SBP and TAS Level | an Extended Model with a New Variable (CLOCK Level) |
|---|---|---|
| R2adj | 0.026 | 0.182 |
| F | 1.097 | 6.415 |
| p-value | 0.339 | <0.0007 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mikulska, A.A.; Grzelak, T.; Pelczyńska, M.; Bogdański, P.; Czyżewska, K. Assessment of Selected Clock Proteins (CLOCK and CRY1) and Their Relationship with Biochemical, Anthropometric, and Lifestyle Parameters in Hypertensive Patients. Biomolecules 2021, 11, 517. https://doi.org/10.3390/biom11040517
Mikulska AA, Grzelak T, Pelczyńska M, Bogdański P, Czyżewska K. Assessment of Selected Clock Proteins (CLOCK and CRY1) and Their Relationship with Biochemical, Anthropometric, and Lifestyle Parameters in Hypertensive Patients. Biomolecules. 2021; 11(4):517. https://doi.org/10.3390/biom11040517
Chicago/Turabian StyleMikulska, Aniceta Ada, Teresa Grzelak, Marta Pelczyńska, Paweł Bogdański, and Krystyna Czyżewska. 2021. "Assessment of Selected Clock Proteins (CLOCK and CRY1) and Their Relationship with Biochemical, Anthropometric, and Lifestyle Parameters in Hypertensive Patients" Biomolecules 11, no. 4: 517. https://doi.org/10.3390/biom11040517
APA StyleMikulska, A. A., Grzelak, T., Pelczyńska, M., Bogdański, P., & Czyżewska, K. (2021). Assessment of Selected Clock Proteins (CLOCK and CRY1) and Their Relationship with Biochemical, Anthropometric, and Lifestyle Parameters in Hypertensive Patients. Biomolecules, 11(4), 517. https://doi.org/10.3390/biom11040517







