Elevated Expression and Activation of GPR15 in Immune Cells in Graves’ Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Peripheral Blood Mononuclear Cells Isolation
2.3. RNA Extraction and Quantitative Real-Time Polymerase Chain Reaction (qRT-PCR)
2.4. Flow Cytometry
2.5. Enzyme-Linked Immunosorbent Assays (ELISA) for Plasma GPR15L
2.6. Immunohistochemistry (IHC) for GPR15
2.7. Statistical Analysis
3. Results
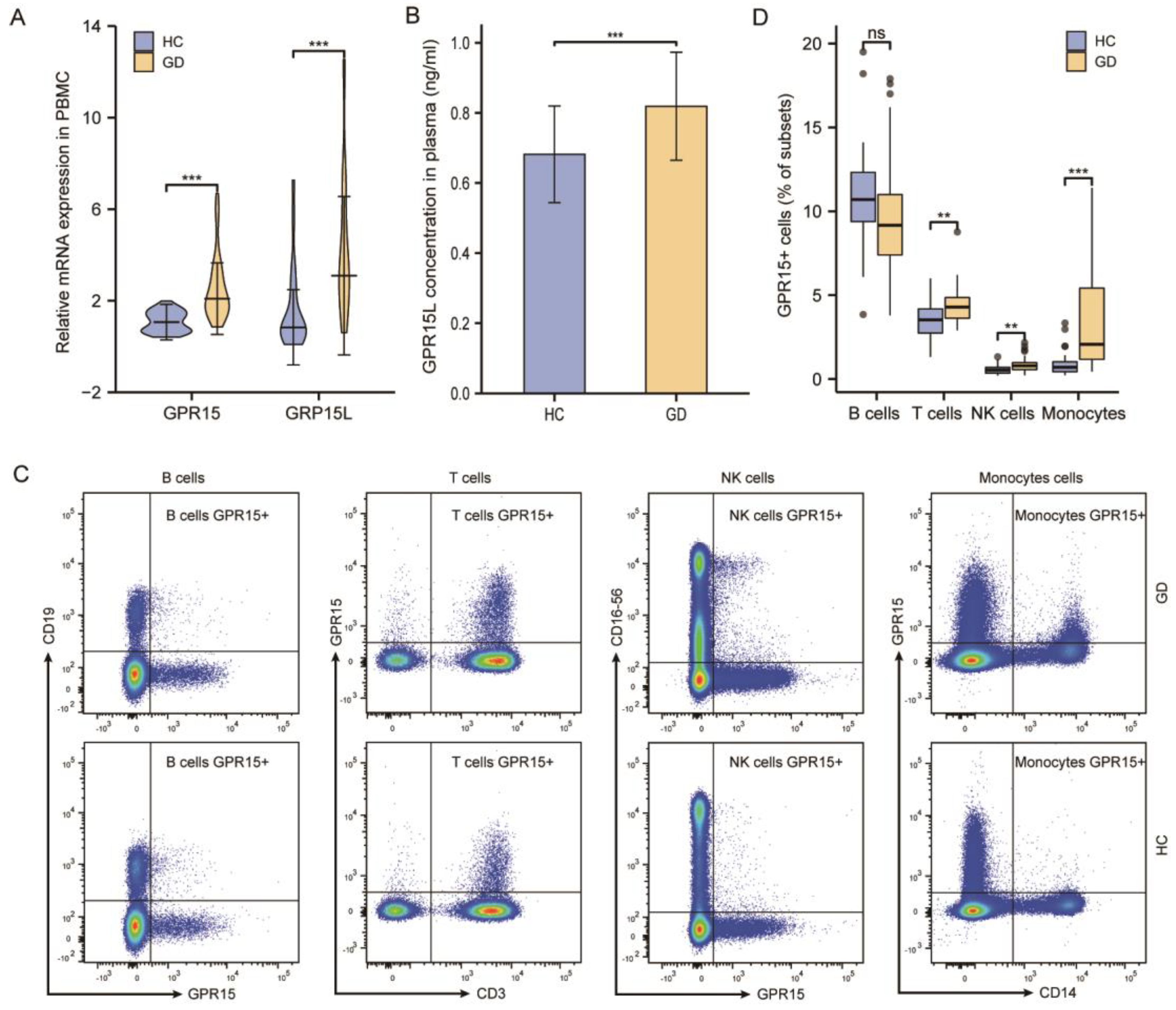
3.1. GPR15 and GPR15L Expression Levels Were Elevated in Patients with GD
3.2. The Frequency of GPR15+ Cells Increased in Specific Subsets of PBMCs of GD Patients and the Expression of GPR15 Correlated Positively with IL4 and IL21
3.2.1. The Frequency of GPR15+ Cells Increased in T cells, NK Cells, and Monocytes
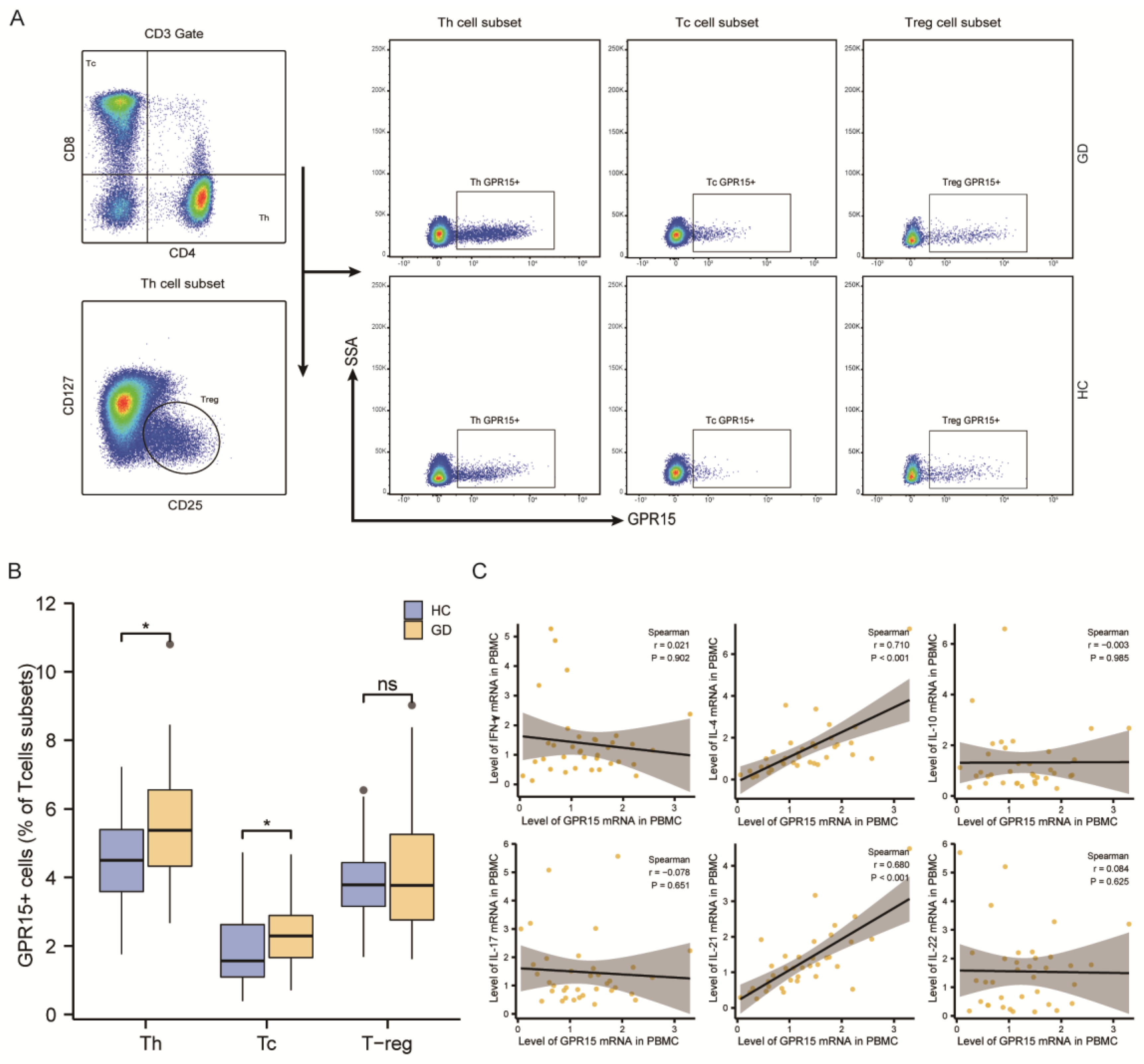
3.2.2. GPR15+ Th Cells and GPR15+ Tc Cells Were Increased in GD Patients
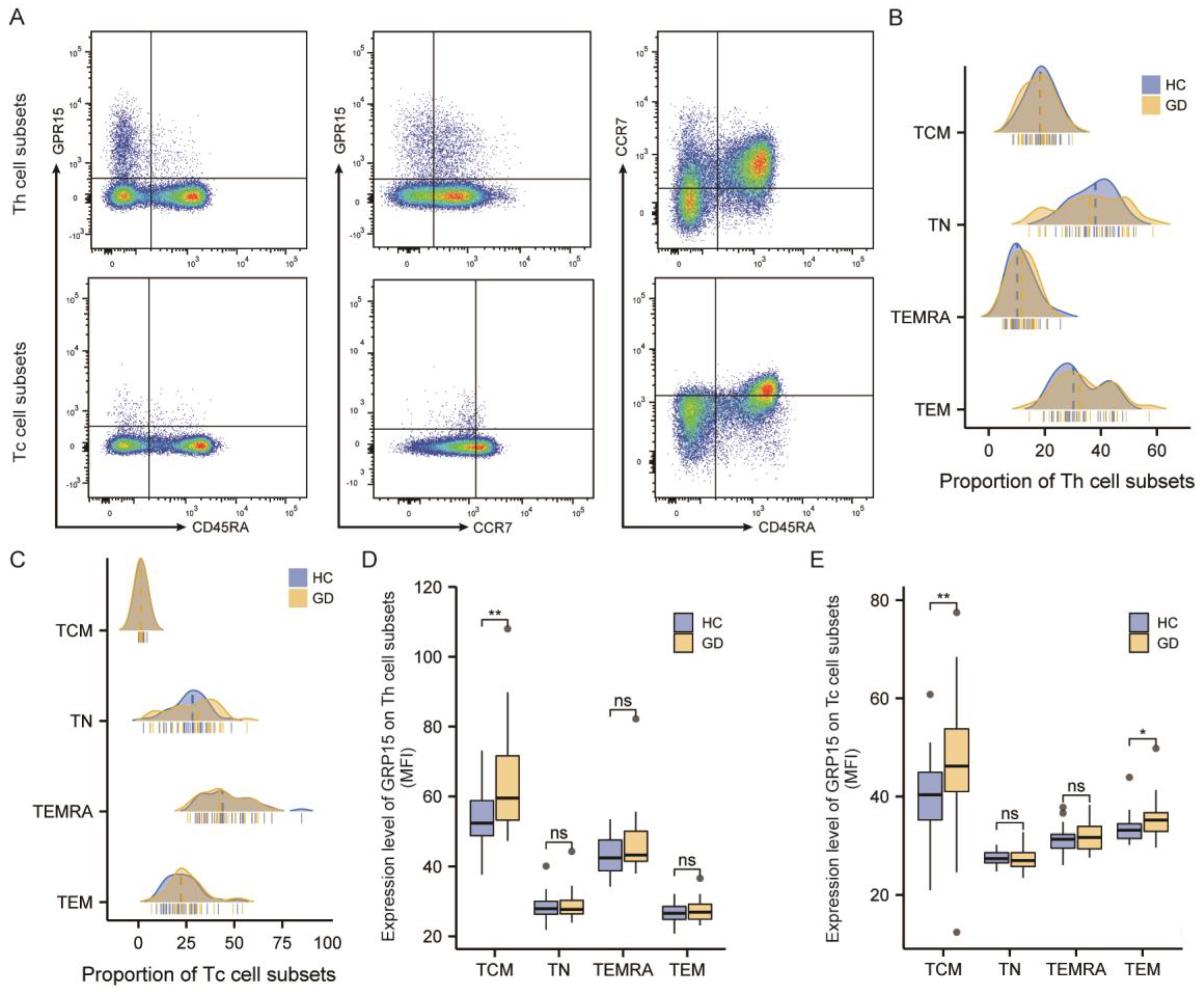
3.2.3. GPR15 Expression Was Enhanced in the TCM Subset of CD4+ T Cells and Both TCM and TEM Subsets of CD8+ T Cells in GD Patients
3.2.4. The Expression of GPR15 Correlated Positively with IL4 and IL21 in GD Patients
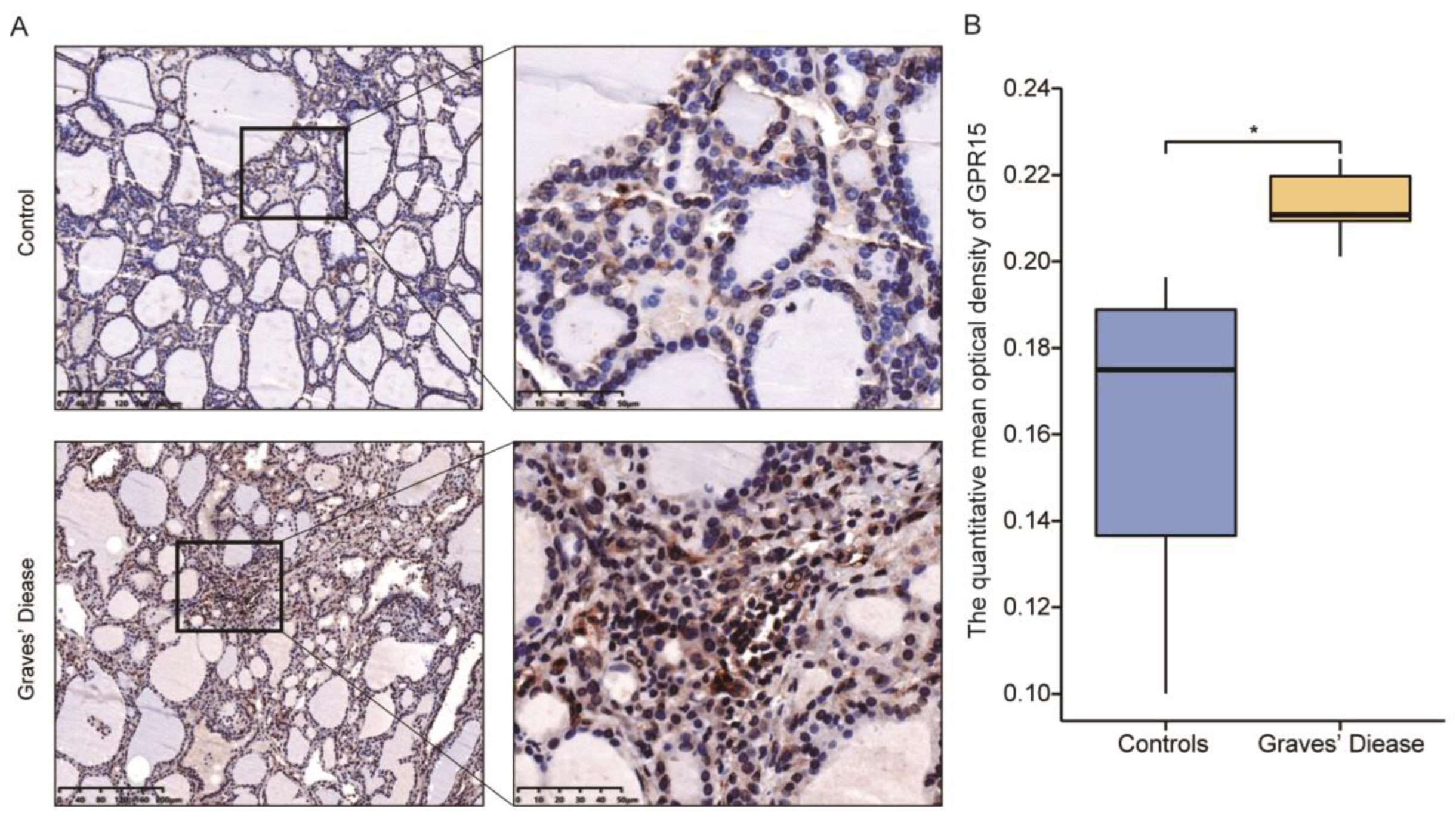
3.3. GPR15 Level Was Raised in Thyroid Tissue of GD Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Taylor, P.N.; Albrecht, D.; Scholz, A.; Gutierrez-Buey, G.; Lazarus, J.H.; Dayan, C.M.; Okosieme, O.E. Global epidemiology of hyperthyroidism and hypothyroidism. Nat. Rev. Endocrinol. 2018, 14, 301–316. [Google Scholar] [CrossRef] [PubMed]
- Davies, T.F.; Ando, T.; Lin, R.-Y.; Tomer, Y.; Latif, R. Thyrotropin receptor-associated diseases: From adenomata to Graves disease. J. Clin. Investig. 2005, 115, 1972–1983. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davies, T.F.; Andersen, S.; Latif, R.; Nagayama, Y.; Barbesino, G.; Brito, M.; Eckstein, A.K.; Stagnaro-Green, A.; Kahaly, G.J. Graves’ disease. Nat. Rev. Dis. Prim. 2020, 6, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Morshed, S.A.; Ma, R.; Latif, R.; Davies, T.F. Cleavage Region Thyrotropin Receptor Antibodies Influence Thyroid Cell Survival In Vivo. Thyroid 2019, 29, 993–1002. [Google Scholar] [CrossRef]
- Morshed, S.A.; Davies, T.F. Graves’ Disease Mechanisms: The Role of Stimulating, Blocking, and Cleavage Region TSH Receptor Antibodies. Horm. Metab. Res. 2015, 47, 727–734. [Google Scholar] [CrossRef] [Green Version]
- De Leo, S.; Lee, S.Y.; Braverman, L.E. Hyperthyroidism. Lancet 2016, 388, 906–918. [Google Scholar] [CrossRef] [Green Version]
- Heiber, M.; Marchese, A.; Nguyen, T.; Heng, H.H.; George, S.R.; O’Dowd, B.F. A Novel Human Gene Encoding a G-Protein-Coupled Receptor (GPR15) Is Located on Chromosome 3. Genomics 1996, 32, 462–465. [Google Scholar] [CrossRef]
- Deng, H.; Unutmaz, D.; Kewal Ramani, V.N.; Littman, D.R. Expression cloning of new receptors used by simian and human immunodeficiency viruses. Nature 1997, 388, 296–300. [Google Scholar] [CrossRef]
- Suply, T.; Hannedouche, S.; Carte, N.; Li, J.; Grosshans, B.; Schaefer, M.; Raad, L.; Beck, V.; Vidal, S.; Hiou-Feige, A.; et al. A natural ligand for the orphan receptor GPR15 modulates lymphocyte recruitment to epithelia. Sci. Signal. 2017, 10, eaal0180. [Google Scholar] [CrossRef]
- Ocón, B.; Pan, J.; Dinh, T.T.; Chen, W.; Ballet, R.; Bscheider, M.; Habtezion, A.; Tu, H.; Zabel, B.A.; Butcher, E.C. A Mucosal and Cutaneous Chemokine Ligand for the Lymphocyte Chemoattractant Receptor GPR15. Front. Immunol. 2017, 8, 1111. [Google Scholar] [CrossRef]
- Reimann, E.; Lättekivi, F.; Keermann, M.; Abram, K.; Koks, S.; Kingo, K.; Fazeli, A. Multicomponent Biomarker Approach Improves the Accuracy of Diagnostic Biomarkers for Psoriasis Vulgaris. Acta Derm. Venereol. 2019, 99, 1258–1265. [Google Scholar] [CrossRef] [PubMed]
- Bauer, M.; Hackermüller, J.; Schor, J.; Schreiber, S.; Fink, B.; Pierzchalski, A.; Herberth, G.; Dubourg, V. Specific induction of the unique GPR15 expression in heterogeneous blood lymphocytes by tobacco smoking. Biomarkers 2019, 24, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Andersen, A.M.; Lei, M.-K.; Beach, S.R.H.; Philibert, R.A.; Sinha, S.; Colgan, J.D. Cigarette and Cannabis Smoking Effects on GPR15+ Helper T Cell Levels in Peripheral Blood: Relationships with Epigenetic Biomarkers. Genes 2020, 11, 149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jia, X.; Zhai, T.; Qu, C.; Ye, J.; Zhao, J.; Liu, X.; Zhang, J.-A.; Qian, Q. Metformin Reverses Hashimoto’s Thyroiditis by Regulating Key Immune Events. Front. Cell Dev. Biol. 2021, 9, 685522. [Google Scholar] [CrossRef]
- Ross, D.S.; Burch, H.B.; Cooper, D.S.; Greenlee, M.C.; Laurberg, P.; Maia, A.L.; Rivkees, S.A.; Samuels, M.; Sosa, J.A.; Stan, M.N.; et al. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid 2016, 26, 1343–1421. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.V.; Xiang, W.V.; Kwak, C.; Yang, Y.; Lin, X.W.; Ota, M.; Sarpel, U.; Rifkin, D.B.; Xu, R.; Littman, D.R. GPR15-Mediated Homing Controls Immune Homeostasis in the Large Intestine Mucosa. Science 2013, 340, 1456–1459. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, L.P.; Pan, J.; Dinh, T.T.; Hadeiba, H.; O’Hara, E.; Ebtikar, A.; Hertweck, A.; Gökmen, M.R.; Lord, G.; Jenner, R.; et al. Role and species-specific expression of colon T cell homing receptor GPR15 in colitis. Nat. Immunol. 2015, 16, 207–213. [Google Scholar] [CrossRef]
- Cartwright, A.; Schmutz, C.; Askari, A.; Kuiper, J.-H.; Middleton, J. Orphan receptor GPR15/BOB is up-regulated in rheumatoid arthritis. Cytokine 2014, 67, 53–59. [Google Scholar] [CrossRef] [Green Version]
- Chen, X.; Wang, Y.; Qi, Y.; Yan, J.; Huang, F.; Zhou, M.; Wang, W.; Ning, G.; Zhou, Y.; Wang, S. Expansion of inflammatory monocytes in periphery and infiltrated into thyroid tissue in Graves’ disease. Sci. Rep. 2021, 11, 13443. [Google Scholar] [CrossRef]
- Zhang, Y.; Lv, G.; Lou, X.; Peng, D.; Qu, X.; Yang, X.; Ayana, D.A.; Guo, H.; Jiang, Y. NKG2A expression and impaired function of NK cells in patients with new onset of Graves’ disease. Int. Immunopharmacol. 2015, 24, 133–139. [Google Scholar] [CrossRef]
- Imam, S.; Dar, P.; Paparodis, R.; Almotah, K.; Al-Khudhair, A.; Hasan, S.A.-M.; Salim, N.; Jaume, J.C. Nature of coexisting thyroid autoimmune disease determines success or failure of tumor immunity in thyroid cancer. J. Immunother. Cancer 2019, 7, 3. [Google Scholar] [CrossRef] [Green Version]
- Magnusson, L.; Barcenilla, H.; Pihl, M.; Bensing, S.; Espes, D.; Carlsson, P.-O.; Casas, R. Mass Cytometry Studies of Patients With Autoimmune Endocrine Diseases Reveal Distinct Disease-Specific Alterations in Immune Cell Subsets. Front. Immunol. 2020, 11, 288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wenzel, B.; Chow, A.; Baur, R.; Schleusener, H.; Wall, J. Natural Killer Cell Activity in Patients with Graves’ Disease and Hashimoto’s Thyroiditis. Thyroid 1998, 8, 1019–1022. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.; Zundler, S.; Atreya, R.; Rath, T.; Bosch-Voskens, C.; Hirschmann, S.; López-Posadas, R.; Watson, A.; Becker, C.; Schuler, G.; et al. Differential effects of α4β7 and GPR15 on homing of effector and regulatory T cells from patients with UC to the inflamed gut in vivo. Gut 2016, 65, 1642–1664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adamczyk, A.; Gageik, D.; Frede, A.; Pastille, E.; Hansen, W.; Rueffer, A.; Buer, J.; Büning, J.; Langhorst, J.; Westendorf, A.M. Differential expression of GPR15 on T cells during ulcerative colitis. JCI Insight 2017, 2, e90585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adamczyk, A.; Pastille, E.; Kehrmann, J.; Vu, V.P.; Geffers, R.; Wasmer, M.-H.; Kasper, S.; Schuler, M.; Lange, C.M.; Muggli, B.; et al. GPR15 Facilitates Recruitment of Regulatory T Cells to Promote Colorectal Cancer. Cancer Res. 2021, 81, 2970–2982. [Google Scholar] [CrossRef]
- Ammitzbøll, C.; von Essen, M.R.; Börnsen, L.; Petersen, E.R.; McWilliam, O.; Ratzer, R.; Christensen, J.R.; Oturai, A.B.; Søndergaard, H.B.; Sellebjerg, F. GPR15+ T cells are Th17 like, increased in smokers and associated with multiple sclerosis. J. Autoimmun. 2019, 97, 114–121. [Google Scholar] [CrossRef]
- Walker, J.A.; McKenzie, A.N.J. TH2 cell development and function. Nat. Rev. Immunol. 2018, 18, 121–133. [Google Scholar] [CrossRef]
- Zhang, J.; Zeng, H.; Ren, M.; Yan, H.; Xu, M.; Feng, Z.; Liang, W.; Yang, C.; Cheng, H.; Ding, H.; et al. Interleukin-21 is associated with disease activity in patients with Graves’ disease. Endocrine 2014, 46, 539–548. [Google Scholar] [CrossRef]
- Vinuesa, C.G.; Linterman, M.A.; Yu, D.; MacLennan, I.C. Follicular Helper T Cells. Annu. Rev. Immunol. 2016, 34, 335–368. [Google Scholar] [CrossRef]
- Liu, Y.; Yuan, X.; Li, X.; Cui, D.; Xie, J. Constitutive Changes in Circulating Follicular Helper T Cells and Their Subsets in Patients with Graves’ Disease. J. Immunol. Res. 2018, 2018, 8972572. [Google Scholar] [CrossRef] [PubMed]
| Graves’ Disease | Health Control | p Value | |
|---|---|---|---|
| Total | 56 | 74 | - |
| Age (years) | 33.75 ± 11.00 | 35.10 ± 10.01 | 0.469 |
| Gender (F/M) | 45/11 | 48/26 | 0.052 |
| FT3 (pmol/L) | 21.29(12.16, 30.72) | - | - |
| FT4 (pmol/L) | 34.52(27.75, 43.65) | - | - |
| TSH (IU/mL) | 0.001(0.001, 0.003) | - | - |
| TRAb (IU/L) | 8.59(4.75, 22.35) | - | - |
| TPOAb (IU/mL) | 254.13(427.24, 62.59) | 7.05(13.11, 5) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, J.; Liu, X.; Xu, J.; Fang, Y.; Du, P.; Gao, C.; Cai, T.; Gu, Z.; Qin, Q.; Zhang, J. Elevated Expression and Activation of GPR15 in Immune Cells in Graves’ Disease. Biomolecules 2022, 12, 1899. https://doi.org/10.3390/biom12121899
Zhao J, Liu X, Xu J, Fang Y, Du P, Gao C, Cai T, Gu Z, Qin Q, Zhang J. Elevated Expression and Activation of GPR15 in Immune Cells in Graves’ Disease. Biomolecules. 2022; 12(12):1899. https://doi.org/10.3390/biom12121899
Chicago/Turabian StyleZhao, Jing, Xuerong Liu, Jianbin Xu, Yudie Fang, Peng Du, Chaoqun Gao, Tiantian Cai, Zhaohua Gu, Qiu Qin, and Jin’an Zhang. 2022. "Elevated Expression and Activation of GPR15 in Immune Cells in Graves’ Disease" Biomolecules 12, no. 12: 1899. https://doi.org/10.3390/biom12121899





