Male Germ Cell Telomeres and Chemical Pollutants
Abstract
1. Introduction
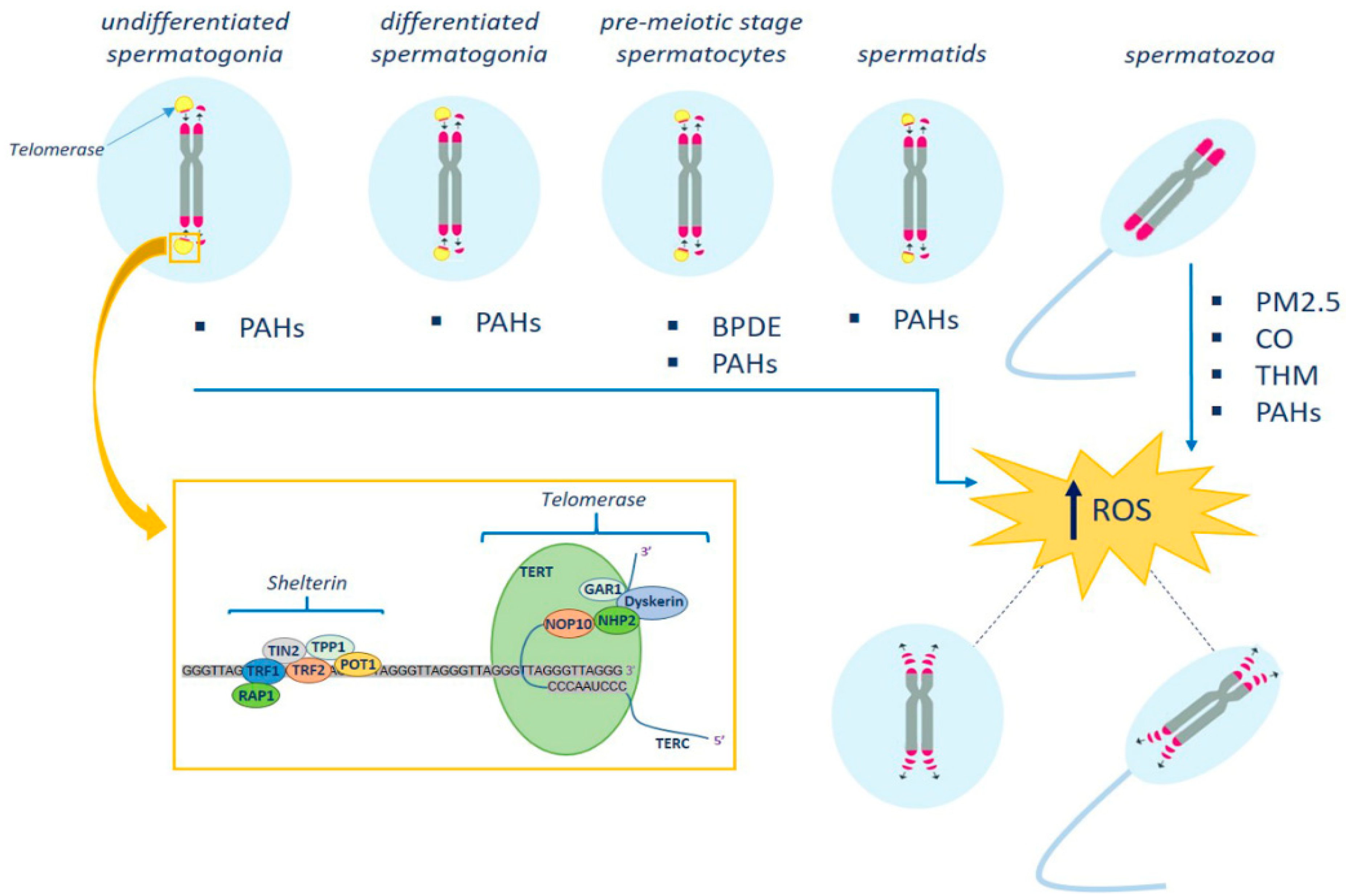
2. Telomeres and Spermatogenesis
3. Germ Cell Telomere and Environmental Pollutants
4. Germ Cell Telomere and Oxidative Stress
5. Conclusions and Perspectives
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Ager, J.; Eustache, F.; Chevrier, C.; Jégou, B. Spatiotemporal trends in human semen quality. Nat. Rev. Urol. 2022, 19, 597–626. [Google Scholar] [CrossRef] [PubMed]
- Dong, S.; Chen, C.; Zhang, J.; Gao, Y.; Zeng, X.; Zhang, X. Testicular aging, male fertility and beyond. Front. Endocrinol. 2022, 13, 1012119. [Google Scholar] [CrossRef] [PubMed]
- Selvaratnam, J.; Paul, C.; Robaire, B. Male Rat germ cells display age-dependent and cell-specific susceptibility in response to oxidative stress challenges. Biol. Reprod. 2015, 93, 72. [Google Scholar] [CrossRef]
- Laurentino, S.; Cremers, J.F.; Horsthemke, B.; Tüttelmann, F.; Czeloth, K.; Zitzmann, M.; Pohl, E.; Rahmann, S.; Schröder, C.; Berres, S.; et al. A germ cell-specific ageing pattern in otherwise healthy men. Aging Cell 2020, 19, e13242. [Google Scholar] [CrossRef] [PubMed]
- Baker, D.J.; Jeganathan, K.B.; Cameron, J.D.; Thompson, M.; Juneja, S.; Kopecka, A.; Kumar, R.; Jenkins, R.B.; De Groen, P.C.; Roche, P.; et al. BubR1 insufficiency causes early onset of aging-associated phenotypes and infertility in mice. Nat. Genet. 2004, 36, 744–799. [Google Scholar] [CrossRef]
- Kotarska, K.; Doniec, A.; Bednarska, M.; Polanski, Z.; Styrna, J. Aging deteriorates quality of sperm produced by male mice with partial yq deletion. Syst. Biol. Reprod. Med. 2017, 63, 360–363. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Vechtova, P.; Fussy, Z.; Sterba, J.; Linhartova, Z.; Rodina, M.; Tučková, V.; Gela, D.; Samarin, A.M.; Lebeda, I.; et al. Changes in phenotypes and DNA methylation of In Vitro aging sperm in common carp Cyprinus carpio. Int. J. Mol. Sci. 2021, 22, 5925. [Google Scholar] [CrossRef]
- Paul, C.; Nagano, M.; Robaire, B. Aging results in differential regulation of DNA repair pathways in pachytene spermatocytes in the brown Norway rat. Biol. Reprod. 2011, 85, 1269–1278. [Google Scholar] [CrossRef]
- Calado, R.T.; Dumitriu, B. Telomere dynamics in mice and humans. Semin. Hematol. 2013, 50, 165–174. [Google Scholar] [CrossRef]
- de Lange, T. Shelterin: The protein complex that shapes and safeguards human telomeres. Genes Dev. 2005, 19, 2100–2110. [Google Scholar] [CrossRef]
- Forsyth, N.R.; Wright, W.E.; Shay, J.W. Telomerase and differentiation in multicellular organisms: Turn it off, turn it on, and turn it off again. Differentiation 2002, 69, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Olovnikov, A.M. The principle of marginotomy in the matrix synthesis of polynucleotides. Dokl. Akad. Nauk SSSR 1971, 201, 1496–1499. [Google Scholar] [PubMed]
- Olovnikov, A.M. A Theory of marginotomy. The incomplete copying of template margin in enzymic synthesis of poly nucleotides and biological significance of the phenomenon. J. Theor. Biol. 1973, 41, 181–190. [Google Scholar] [CrossRef]
- Blackburn, E.H. Telomeres and telomerase: The means to the end (Nobel lecture). Angew. Chem. Int. Ed. Engl. 2010, 49, 7405–7421. [Google Scholar] [CrossRef]
- Greider, C.W. Telomerase discovery: The excitement of putting together pieces of the puzzle (Nobel lecture). Angew. Chem. Int. Ed. Engl. 2010, 49, 7422–7439. [Google Scholar] [CrossRef] [PubMed]
- Szostak, J.W. DNA ends: Just the beginning (Nobel lecture). Angew. Chem. Int. Ed. Engl. 2010, 49, 7386–7404. [Google Scholar] [CrossRef]
- Ozturk, S. Telomerase activity and telomere length in male germ cells. Biol. Reprod. 2015, 92, 53. [Google Scholar] [CrossRef]
- Güneş, S.; Kulaç, T. The role of epigenetics in spermatogenesis. Turk. J. Urol. 2013, 39, 181–187. [Google Scholar] [CrossRef]
- Cescon, M.; Chianese, R.; Tavares, R.S. Environmental Impact on Male (In)Fertility via Epigenetic Route. J. Clin. Med. 2020, 9, 2520. [Google Scholar] [CrossRef]
- Churikov, D.; Siino, J.; Svetlova, M.; Zhang, K.; Gineitis, A.; Morton Bradbury, E.; Zalensky, A. Novel human testis-specific histone H2B encoded by the interrupted gene on the X chromosome. Genomics 2004, 84, 745–756. [Google Scholar] [CrossRef]
- Thilagavathi, J.; Venkatesh, S.; Dada, R. Telomere length in reproduction. Andrologia 2013, 45, 289–304. [Google Scholar] [CrossRef]
- Reig-Viader, R.; Capilla, L.; Vila-Cejudo, M.; Garcia, F.; Anguita, B.; Garcia-Caldés, M.; Ruiz-Herrera, A. Telomere homeostasis is compromised in spermatocytes from patients with idiopathic infertility. Fertil. Steril. 2014, 102, 728–738.e1. [Google Scholar] [CrossRef] [PubMed]
- Vasilopoulos, E.; Fragkiadaki, P.; Kalliora, C.; Fragou, D.; Docea, A.O.; Vakonaki, E.; Tsoukalas, D.; Calina, D.; Buga, A.M.G.; Mamoulakis, C.; et al. The association of female and male infertility with telomere length. Int. J. Mol. Med. 2019, 44, 375–389. [Google Scholar] [CrossRef]
- Polonio, A.M.; Chico-Sordo, L.; Córdova-Oriz, I.; Medrano, M.; García-Velasco, J.A.; Varela, E.; Yale, J. Impact of ovarian aging in reproduction: From telomeres and mice models to ovarian rejuvenation. Biol. Med. 2020, 93, 561–569. [Google Scholar]
- Córdova-Oriz, I.; Chico-Sordo, L.; Varela, E. Telomeres, aging and reproduction. Curr. Opin. Obstet. Gynecol. 2022, 34, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Pech, M.F.; Garbuzov, A.; Hasegawa, K.; Sukhwani, M.; Zhang, R.J.; Benayoun, B.A.; Brockman, S.A.; Lin, S.; Brunet, A.; Orwig, K.E.; et al. High telomerase is a hallmark of undifferentiated spermatogonia and is required for maintenance of male germline stem cells. Genes Dev. 2015, 29, 2420–2434. [Google Scholar] [CrossRef]
- Keefe, D.L.; Liu, L. Telomeres and reproductive aging. Reprod. Fertil. Dev. 2009, 21, 10–14. [Google Scholar] [CrossRef]
- Ribas-Maynou, J.; Mateo-Otero, Y.; Sanchez-Quijada, M.; Recuero, S.; Delgado-Bermúdez, A.; Llavanera, M.; Yeste, M. Telomere length in pig sperm is related to in vitro embryo development outcomes. Animals 2022, 12, 204. [Google Scholar] [CrossRef]
- Boniewska-Bernacka, E.; Pa´nczyszyn, A.; Cybulska, N. Telomeres as a molecular marker of male infertility. Hum. Fertil. 2019, 22, 78–87. [Google Scholar] [CrossRef]
- Rocca, M.S.; Foresta, C.; Ferlin, A. Telomere length: Lights and shadows on their role in human reproduction. Biol. Reprod. 2019, 100, 305–317. [Google Scholar] [CrossRef]
- Ferlin, A.; Rampazzo, E.; Rocca, M.S.; Keppel, S.; Frigo, A.C.; De Rossi, A.; Foresta, C. In young men sperm telomere length is related to sperm number and parental age. Hum. Reprod. 2013, 28, 3370–3376. [Google Scholar] [CrossRef] [PubMed]
- Rocca, M.S.; Speltra, E.; Menegazzo, M.; Garolla, A.; Foresta, C.; Ferlin, A. Sperm telomere length as a parameter of sperm quality in normozoospermic men. Hum. Reprod. 2013, 31, 1158–1163. [Google Scholar] [CrossRef]
- Cariati, F.; Jaroudi, S.; Alfarawati, S.; Raberi, A.; Alviggi, C.; Pivonello, R.; Wells, D. Investigation of sperm telomere length as a potential marker of paternal genome integrity and semen quality. Reprod. Biomed. Online 2016, 33, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Schrader, M.; Müller, M.; Heicappell, R.; Krause, H.; Schulze, W.; Miller, K. Telomerase activity and expression of telomerase subunits in the testicular tissue of infertile patients. Fertil. Steril. 2000, 73, 706–711. [Google Scholar] [CrossRef] [PubMed]
- Reig-Viader, R.; Garcia-Caldés, M.; Ruiz-Herrera, A. Telomere homeostasis in mammalian germ cells: A review. Chromosoma 2016, 125, 337–351. [Google Scholar] [CrossRef] [PubMed]
- Moazamian, A.; Gharagozloo, P.; Aitken, R.J.; Drevet, J.R. Oxidative stress and reproductive function: Sperm telomeres, oxidative stress, and infertility. Reproduction 2022, 164, F125–F133. [Google Scholar] [CrossRef] [PubMed]
- Fattet, A.J.; Chaillot, M.; Koscinski, I. Telomere Length, a New Biomarker of Male (in)Fertility? A Systematic Review of the Literature. Genes 2023, 14, 425. [Google Scholar] [CrossRef]
- Yang, Q.; Zhao, F.; Dai, S.; Zhang, N.; Zhao, W.; Bai, R.; Sun, Y. Sperm telomere length is positively associated with the quality of early embryonic development. Hum. Repr. 2015, 30, 1876–1881. [Google Scholar] [CrossRef]
- Torra-Massana, M.; Barragan, M.; Bellu, E.; Oliva, R.; Rodriguez, A.; Vassena, R. Sperm telomere length in donor samples is not related to ICSI outcome. J. Assist. Reprod. Genet. 2018, 35, 649–657. [Google Scholar] [CrossRef]
- Lopes, A.C.; Oliveira, P.F.; Pinto, S.; Almeida, C.; Pinho, M.J.; Sá, R.; Rocha, E.; Barros, A.; Sousa, M. Discordance between human sperm quality and telomere length following differential gradient separation/swim-up. J. Assist. Reprod. Genet. 2020, 37, 2581–2603. [Google Scholar] [CrossRef]
- Gentiluomo, M.; Luddi, A.; Cingolani, A.; Fornili, M.; Governini, L.; Lucenteforte, E.; Baglietto, L.; Piomboni, P.; Campa, D. Telomere Length and Male Fertility. Int. J. Mol. Sci. 2021, 22, 3959. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.; Tan, Y.; Qiu, X.; Luo, H.; Li, Y.; Li, R.; Yang, X. Sperm telomere length as a novel biomarker of male infertility and embryonic development: A systematic review and meta-analysis. Front. Endocrinol. 2023, 13, 1079966. [Google Scholar] [CrossRef] [PubMed]
- Garanina, A.S.; Alieva, I.B.; Bragina, E.E.; Blanchard, E.; Arbeille, B.; Guerif, F.; Uzbekova, S.; Uzbekov, R.E. The Centriolar Adjunct—Appearance and Disassembly in Spermiogenesis and the Potential Impact on Fertility. Cells 2019, 8, 180. [Google Scholar] [CrossRef]
- Miri, M.; Nazarzadeh, M.; Alahabadi, A.; Ehrampoush, M.H.; Rad, A.; Lotfi, M.H.; Sheikhha, M.H.; Sakhvidi, M.J.Z.; Nawrot, T.S.; Dadvand, P. Air pollution and telomere length in adults: A systematic review and meta-analysis of observational studies. Environ. Pollut. 2019, 244, 636–647. [Google Scholar] [CrossRef]
- Zamkowska, D.; Karwacka, A.; Jurewicz, J.; Radwan, M. Environmental exposure to non-persistent endocrine disrupting chemicals and semen quality: An overview of the current epidemiological evidence. Int. J. Occup. Med. Environ. Health 2018, 31, 377–414. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Zhang, B.; Wu, L.; Zhou, Y.; Li, Y.; Mao, X.; Chen, Y.; Wang, J.; Luo, P.; Ma, J.; et al. Association of exposure to ambient fine particulate matter constituents with semen quality among men attending a fertility center in China. Environ. Sci. Technol. 2019, 53, 5957–5965. [Google Scholar] [CrossRef] [PubMed]
- Pizzol, D.; Foresta, C.; Garolla, A.; Demurtas, J.; Trott, M.; Bertoldo, A.; Smith, L. Pollutants and sperm quality: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. Int. 2021, 28, 4095–4103. [Google Scholar] [CrossRef]
- Eshkoor, S.; Ismail, P.; Rahman, S.; Moin, S. Does GSTP1 polymorphism contribute to genetic damage caused by ageing and occupational exposure? Arch. Ind. Hyg. Toxicol. 2011, 62, 291–298. [Google Scholar] [CrossRef]
- Hou, L.; Wang, S.; Dou, C.; Zhang, X.; Yu, Y.; Zheng, Y.; Avula, U.; Hoxha, M.; Díaz, A.; McCracken, J.; et al. Air pollution exposure and telomere length in highly exposed subjects in Beijing, China: A repeated-measure study. Environ. Int. 2012, 48, 71–77. [Google Scholar] [CrossRef]
- Walton, R.T.; Mudway, I.S.; Dundas, I.; Marlin, N.; Koh, L.C.; Aitlhadj, L.; Vulliamy, T.; Jamaludin, J.B.; Wood, H.E.; Barratt, B.M.; et al. Air pollution, ethnicity and telomere length in east London schoolchildren: An observational study. Environ. Int. 2016, 96, 41–47. [Google Scholar] [CrossRef]
- Liu, Y.; Zhou, Y.; Ma, J.; Bao, W.; Li, J.; Zhou, T.; Cui, X.; Peng, Z.; Zhang, H.; Feng, M.; et al. Inverse association between ambient sulfur dioxide exposure and semen quality in Wuhan, China. Environ. Sci. Technol. 2017, 51, 12806–12814. [Google Scholar] [CrossRef] [PubMed]
- Lao, X.Q.; Zhang, Z.; Lau, A.K.H.; Chan, T.C.; Chuang, Y.C.; Chan, J.; Lin, C.; Guo, C.; Jiang, W.K.; Tam, T.; et al. Exposure to ambient fine particulate matter and semen quality in Taiwan. Occup. Environ. Med. 2018, 75, 148–154. [Google Scholar] [CrossRef]
- Zhang, H.T.; Zhang, Z.; Cao, J.; Tang, W.H.; Zhang, H.L.; Hong, K.; Lin, H.C.; Wu, H.; Chen, Q.; Jiang, H. Ambient ozone pollution is associated with decreased semen quality: Longitudinal analysis of 8945 semen samples from 2015 to 2018 and during pollution-control period in Beijing, China. Asian J. Androl. 2019, 21, 501–507. [Google Scholar] [CrossRef]
- Zhang, G.; Jiang, F.; Chen, Q.; Yang, H.; Zhou, N.; Sun, L.; Zou, P.; Yang, W.; Cao, J.; Zhou, Z.; et al. Associations of ambient air pollutant exposure with seminal plasma MDA, sperm mtDNA copy number, and mtDNA integrity. Environ. Int. 2020, 136, 105483. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhu, Q.; Lin, J.; Cai, J. Association of exposure to particulate matter air pollution with semen quality among men in China. JAMA Netw. Open 2022, 5, e2148684. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.R.; Yang, W.X. Roles of three Es-Caspases during spermatogenesis and Cadmium-induced apoptosis in Eriocheir sinensis. Aging 2018, 10, 1146–1165. [Google Scholar] [CrossRef]
- Kakavandi, B.; Rafiemanesh, H.; Giannakis, S.; Beheshtaeen, F.; Samoili, S.; Hashemi, M.; Abdi, F. Establishing the relationship between Polycyclic Aromatic Hydrocarbons (PAHs) exposure and male infertility: A systematic review. Ecotoxicol. Environ. Saf. 2023, 250, 114485. [Google Scholar] [CrossRef] [PubMed]
- Jeng, H.A.; Pan, C.H.; Chao, M.R.; Chiu, C.C.; Zhou, G.; Chou, C.K.; Lin, W.Y. Sperm quality and DNA integrity of coke oven workers exposed to polycyclic aromatic hydrocarbons. Int. J. Occup. Med. Environ. Health 2016, 29, 915–926. [Google Scholar] [CrossRef]
- Knapke, E.T.; Magalhaes, D.d.P.; Dalvie, M.A.; Mandrioli, D.; Perry, M.J. Environmental and occupational pesticide exposure and human sperm parameters: A Navigation Guide review. Toxicology 2022, 465, 153017. [Google Scholar] [CrossRef]
- Issah, I.; Arko-Mensah, J.; Agyekum, T.P.; Dwomoh, D.; Fobil, J.N. Electronic waste exposure and DNA damage: A systematic review and meta-analysis. Rev. Environ. Health 2021, 38, 15–31. [Google Scholar] [CrossRef]
- Šabović, I.; Cosci, I.; De Toni, L.; Ferramosca, A.; Stornaiuolo, M.; Di Nisio, A.; Dall’Acqua, S.; Garolla, A.; Foresta, C. Perfluoro-octanoic acid impairs spermmotility through the alteration of plasmamembrane. J. Endocrinol. Investig. 2020, 43, 641–652. [Google Scholar] [CrossRef]
- Aitken, R.J.; Baker, M.A.; Nixon, B. Are sperm capacitation and apoptosis the opposite ends of a continuum driven by oxidative stress? Asian J. Androl. 2015, 17, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Sipinen, V.; Laubenthal, J.; Baumgartner, A.; Cemeli, E.; Linschooten, J.O.; Godschalk, R.W.L.; Van Schooten, F.J.; Anderson, D.; Brunborg, G. In vitro evaluation of baseline and induced DNA damage in human sperm exposed to benzo[a]pyrene or its metabolite benzo[a]pyrene-7,8-diol-9,10-epoxide, using the comet assay. Mutagenesis 2010, 25, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Hughes, L.M.; Griffith, R.; Carey, A.; Butler, T.; Donne, S.W.; Beagley, K.W.; Aitken, R.J. The spermastatic and microbicidal actions of quinones and maleimides: Toward a dual-purpose contraceptive agent. Mol. Pharmacol. 2009, 76, 113–124. [Google Scholar] [CrossRef]
- Zhou, L.; Li, L.; Hao, G.; Li, B.; Yang, S.; Wang, N.; Liang, J.; Sun, H.; Ma, S.; Yan, L.; et al. Sperm mtDNA copy number, telomere length, and seminal spermatogenic cells in relation to ambient air pollution: Results of a cross-sectional study in Jing-Jin-Ji region of China. J. Hazard. Mater. 2021, 406, 124308. [Google Scholar] [CrossRef]
- Vecoli, C.; Montano, L.; Borghini, A.; Notari, T.; Guglielmino, A.; Mercuri, A.; Turchi, S.; Andreassi, M.G. Effects of Highly Polluted Environment on Sperm Telomere Length: A Pilot Study. Int. J. Mol. Sci. 2017, 18, 1703. [Google Scholar] [CrossRef]
- Liu, C.; Chen, Y.J.; Sun, B.; Chen, H.G.; Mustieles, V.; Messerlian, C.; Sun, Y.; Meng, T.Q.; Lu, W.Q.; Pan, X.F.; et al. Blood trihalomethane concentrations in relation to sperm mitochondrial DNA copy number and telomere length among 958 healthy men. Environ. Res. 2023, 216, 114737. [Google Scholar] [CrossRef]
- Ling, X.; Zhang, G.; Chen, Q.; Yang, H.; Sun, L.; Zhou, N.; Wang, Z.; Zou, P.; Wang, X.; Cui, Z.; et al. Shorter sperm telomere length in association with exposure to polycyclic aromatic hydrocarbons: Results from the MARHCS cohort study in Chongqing, China and in vivo animal experiments. Environ. Int. 2016, 95, 79–85. [Google Scholar] [CrossRef]
- Ling, X.; Yang, W.; Zou, P.; Zhang, G.; Wang, Z.; Zhang, X.; Chen, H.; Peng, K.; Han, F.; Liu, J.; et al. TERT regulates telomere-related senescence and apoptosis through DNA damage response in male germ cells exposed to BPDE in vitro and to B[a]P in vivo. Environ. Pollut. 2018, 235, 836–849. [Google Scholar] [CrossRef]
- Li, X.; Liu, J.; Zhou, G.; Sang, Y.; Zhang, Y.; Jing, L.; Shi, Z.; Zhou, X.; Sun, Z. BDE-209 and DBDPE induce male reproductive toxicity through telomere-related cell senescence and apoptosis in SD rat. Environ. Int. 2021, 146, 106307. [Google Scholar] [CrossRef]
- Morimoto, H.; Kanastu-Shinohara, M.; Ogonuki, N.; Kamimura, S.; Ogura, A.; Yabe-Nishimura, C.; Mori, Y.; Morimoto, T.; Watanabe, S.; Otsu, K.; et al. ROS amplification drives mouse spermatogonial stem cell selfrenewal. Life Sci. Alliance 2019, 2, e201900374. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, H.; Yamamoto, T.; Miyazaki, T.; Ogonuki, N.; Ogura, A.; Tanaka, T.; Kanatsu-Shinohara, M.; Yabe-Nishimura, C.; Zhang, H.; Pommier, Y.; et al. An interplay of NOX1-derived ROS and oxygen determines the spermatogonial stem cell self-renewal efficiency under hypoxia. Genes Dev. 2021, 35, 250–260. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zhang, Z.; Chang, C.; Yang, Z.; Wang, P.; Fu, H.; Wei, X.; Chen, E.; Tan, S.; Huang, W.; et al. A bioenergetic shift is required for spermatogonial differentiation. Cell Discov. 2020, 6, 56. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.L.; Chakraborty, S.; Rajan, S.S.; Wang, R.; Huang, F. Effects of oxidative stress on mouse embryonic stem cell proliferation, apoptosis, senescence, and self-renewal. Stem Cells Dev. 2010, 19, 1321–1331. [Google Scholar] [CrossRef] [PubMed]
- De Iuliis, G.N.; Thomson, L.K.; Mitchell, L.A.; Finnie, J.M.; Koppers, A.J.; Hedges, A.; Nixon, B.; Aitken, R.J. DNA damage in human spermatozoa is highly correlated with the efficiency of chromatin remodeling and the formation of 8-hydroxy-2′-deoxyguanosine, a marker of oxidative stress. Biol. Reprod. 2009, 81, 517–524. [Google Scholar] [CrossRef]
- Aitken, R.J.; Gibb, Z.; Baker, M.A.; Drevet, J.; Gharagozloo, P. Causes and consequences of oxidative stress in spermatozoa. Reprod. Fertil. Dev. 2016, 28, 1–10. [Google Scholar] [CrossRef]
- Bui, A.D.; Sharma, R.; Henkel, R.; Agarwal, A. Reactive oxygen species impact on sperm DNA and its role in male infertility. Andrologia 2018, 50, e13012. [Google Scholar] [CrossRef]
- Barnes, R.P.; Fouquerel, E.; Opresko, P.L. The impact of oxidative DNA damage and stress on telomere homeostasis. Mech. Ageing Dev. 2019, 177, 37–45. [Google Scholar] [CrossRef]
- Grollman, A.P.; Moriya, M. Mutagenesis by 8-oxoguanine: An enemy within. Trends Genet. 1993, 9, 246–249. [Google Scholar] [CrossRef]
- Coluzzi, E.; Leone, S.; Sgura, A. Oxidative stress induces telomere dysfunction and senescence by replication fork arrest. Cells 2019, 8, 19. [Google Scholar] [CrossRef]
- von Zglinicki, T. Oxidative stress shortens telomeres. Trends Biochem. Sci. 2002, 27, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Palm, W.; de Lange, T. How shelterin protects mammalian telomeres. Annu. Rev. Genet. 2008, 42, 301–334. [Google Scholar] [CrossRef] [PubMed]
- Smogorzewska, A.; van Steensel, B.; Bianchi, A.; Oelmann, S.; Schaefer, M.R.; Schnapp, G.; de Lange, T. Control of human telomere length by TRF1 and TRF2. Mol. Cell Biol. 2000, 20, 1659–1668. [Google Scholar] [CrossRef] [PubMed]
- Opresko, P.L.; Fan, J.; Danzy, S.; Wilson, D.M.; Bohr, V.A. Oxidative damage in telomeric DNA disrupts recognition by TRF1 and TRF2. Nucleic Acids Res. 2005, 33, 1230–1239. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, W.; Lingner, J. Impact of oxidative stress on telomere biology. Differentiation 2018, 99, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Abey, E.; Ahmed, W.; Redon, S.; Simanis, V.; Lingner, J. Peroxiredoxin 1 protects telomeres from oxidative damage and preserves telomeric DNA for extension by telomerase. Cell Rep. 2016, 17, 3107–3114. [Google Scholar] [CrossRef]
- Smith, T.B.; Dun, M.D.; Smith, N.D.; Curry, B.J.; Connaughton, H.S.; Aitken, R.J. The presence of a truncated base excision repair pathway in human spermatozoa that is mediated by OGG1. J. Cell Sci. 2013, 126, 1488–1497. [Google Scholar] [CrossRef] [PubMed]
- Ko, E.Y.; Sabanegh, E.S., Jr.; Agarwal, A. Male infertility testing: Reactive oxygen species and antioxidant capacity. Fertil. Steril. 2014, 102, 1518–1527. [Google Scholar] [CrossRef]
- Subramanian, V.; Ravichandran, A.; Thiagarajan, N.; Govindarajan, M.; Dhandayuthapani, S.; Suresh, S. Seminal reactive oxygen species and total antioxidant capacity: Correlations with sperm parameters and impact on male infertility. Clin. Exp. Reprod. Med. 2018, 45, 88–93. [Google Scholar] [CrossRef]
- Berby, B.; Bichara, C.; Rives-Feraille, A.; Jumeau, F.; Di Pizio, P.D.; Setif, V.; Sibert, L.; Dumont, L.; Rondanino, C.; Rives, N. Oxidative stress is associated with telomere interaction impairment and chromatin defect in spermatozoa of infertile males. Antioxidants 2021, 10, 593. [Google Scholar] [CrossRef]
- Mishra, S.; Kumar, R.; Malhotra, N.; Singh, N.; Dada, R. Mild oxidative stress is beneficial for sperm telomere length maintenance. World J. Methodol. 2016, 6, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Wagner, H.; Cheng, J.W.; Ko, E.Y. Role of reactive oxygen species in male infertility: An updated review of literature. Arab. J. Urol. 2018, 16, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Lafuente, R.; Bosch-Rue, E.; Ribas-Maynou, J.; Alvarez, J.; Brassesco, C.; Amengual, M.J.; Benet, J.; Garcia-Peiró, A.; Brassesco, M. Sperm telomere length in motile sperm selection techniques: A qFISH approach. Andrologia 2018, 50, e12840. [Google Scholar] [CrossRef] [PubMed]
- Tunc, O.; Bakos, H.W.; Tremellen, K. Impact of body mass index on seminal oxidative stress. Andrologia 2011, 43, 121–128. [Google Scholar] [CrossRef]
- Silva, J.V.; Cruz, D.; Gomes, M.; Correia, B.R.; Freitas, M.J.; Sousa, L.; Silva, V.; Fardilha, M. Study on the short-term effects of increased alcohol and cigarette consumption in healthy young men’s seminal quality. Sci. Rep. 2017, 7, 45457. [Google Scholar] [CrossRef]
| Pollutans | Sample | Damage | Refs | |
|---|---|---|---|---|
| CO | Human sperm | Shorting STL | [65] | |
| PM2.5 | Human sperm | Shorting STL | [65] | |
| THM | TCM, BDCM, DBCM, TBM | Human sperm | Shorting STL | [67] |
| PAHs | 1-OHPyr, 1-OHNap B[a]P BPDE | Human sperm Rat testis Rat testis GC-2 | Shorting STL Shorting germ cell TL; Telomerase inhibition; decrease in TERT protein expression Shorting TL; telomere-associated DNA damage; telomerase inhibition; decrease in TERT protein expression | [68] [68] [69] [69] |
| BDE-209 DBDPE | Rat testis | Shorting STL; telomerase inhibition | [70] | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chieffi Baccari, G.; Iurato, G.; Santillo, A.; Dale, B. Male Germ Cell Telomeres and Chemical Pollutants. Biomolecules 2023, 13, 745. https://doi.org/10.3390/biom13050745
Chieffi Baccari G, Iurato G, Santillo A, Dale B. Male Germ Cell Telomeres and Chemical Pollutants. Biomolecules. 2023; 13(5):745. https://doi.org/10.3390/biom13050745
Chicago/Turabian StyleChieffi Baccari, Gabriella, Giuseppe Iurato, Alessandra Santillo, and Brian Dale. 2023. "Male Germ Cell Telomeres and Chemical Pollutants" Biomolecules 13, no. 5: 745. https://doi.org/10.3390/biom13050745
APA StyleChieffi Baccari, G., Iurato, G., Santillo, A., & Dale, B. (2023). Male Germ Cell Telomeres and Chemical Pollutants. Biomolecules, 13(5), 745. https://doi.org/10.3390/biom13050745






