Favorable Preclinical Pharmacological Profile of a Novel Antimalarial Pyrrolizidinylmethyl Derivative of 4-amino-7-chloroquinoline with Potent In Vitro and In Vivo Activities
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemistry
2.2. Biological Assays
2.2.1. P. falciparum Cultures and Drug Sensitivity Assays
2.2.2. Field Isolates of P. falciparum and P. vivax and Chemosensitivity Assays
2.2.3. In Vivo Oral Efficacy Studies
2.3. In Vitro Pre-Clinical Studies
2.3.1. Intrinsic Clearance
2.3.2. Metabolic Profiling and Metabolites Identification
2.3.3. P450 Assay
2.4. In Vivo Preclinical Studies
2.4.1. Pharmacokinetic Studies in Rat
2.4.2. Tissue Distribution in Rat
2.4.3. Plasma Protein Binding and Blood to Plasma Partitioning
2.5. Toxicology
Dose Range Finding (DRF)
3. Results and Discussion
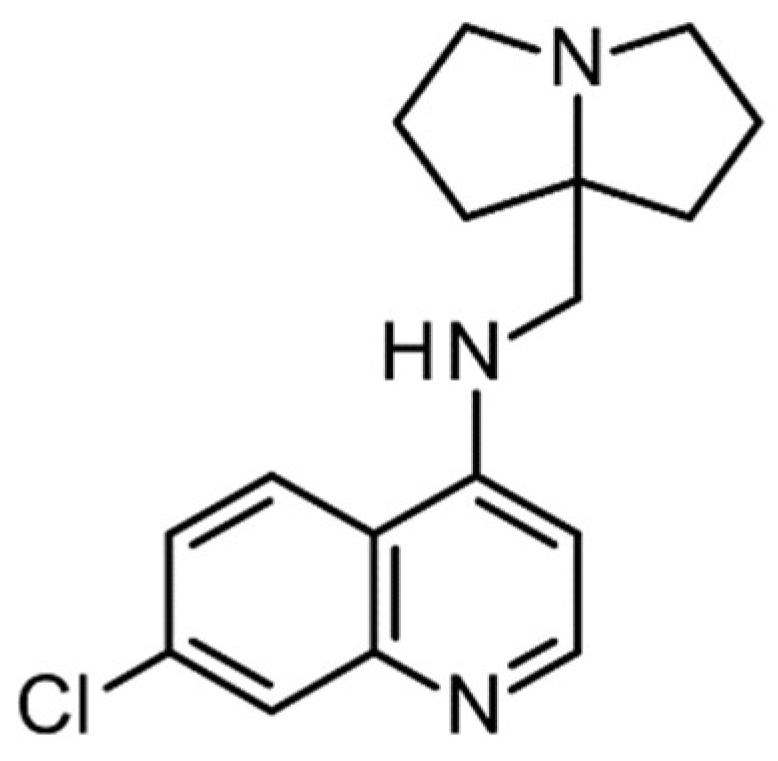
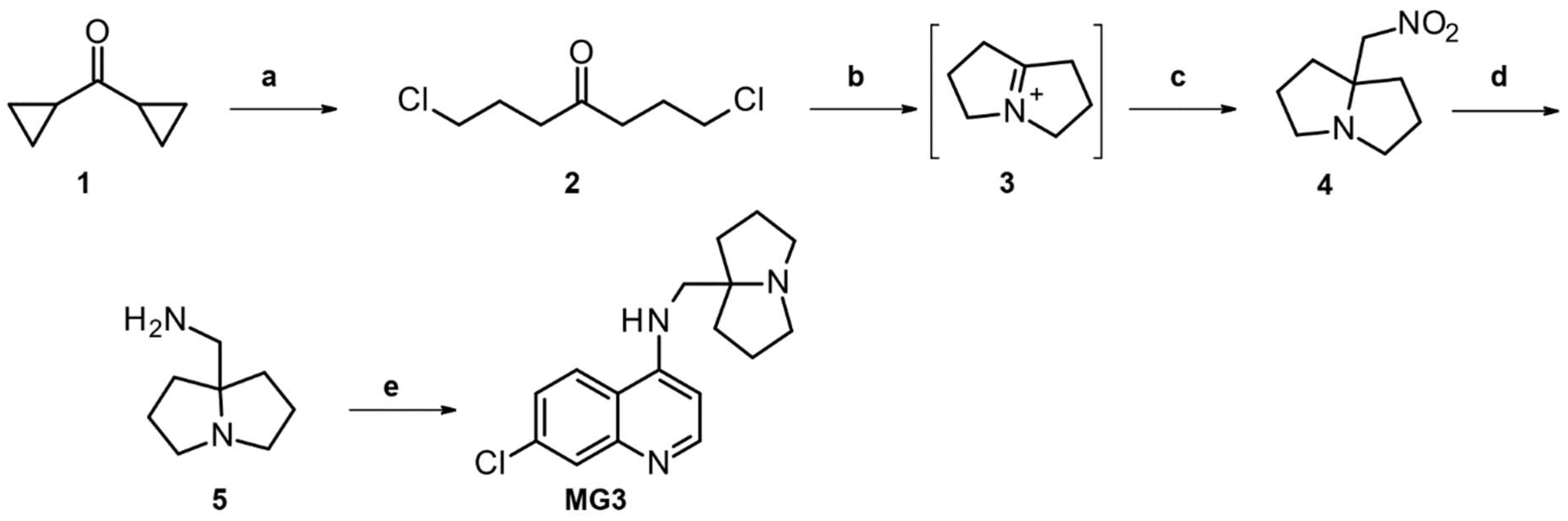
3.1. Chemistry: Novel Synthesis and Chemical Characterization of MG3
3.2. In Vitro and In Vivo Characterization of MG3
3.2.1. In Vitro Antimalarial Activity against P. falciparum Asexual Stages
3.2.2. In Vivo Oral Efficacy of MG3
3.3. Characterization of ADME-TOX Profile of MG3
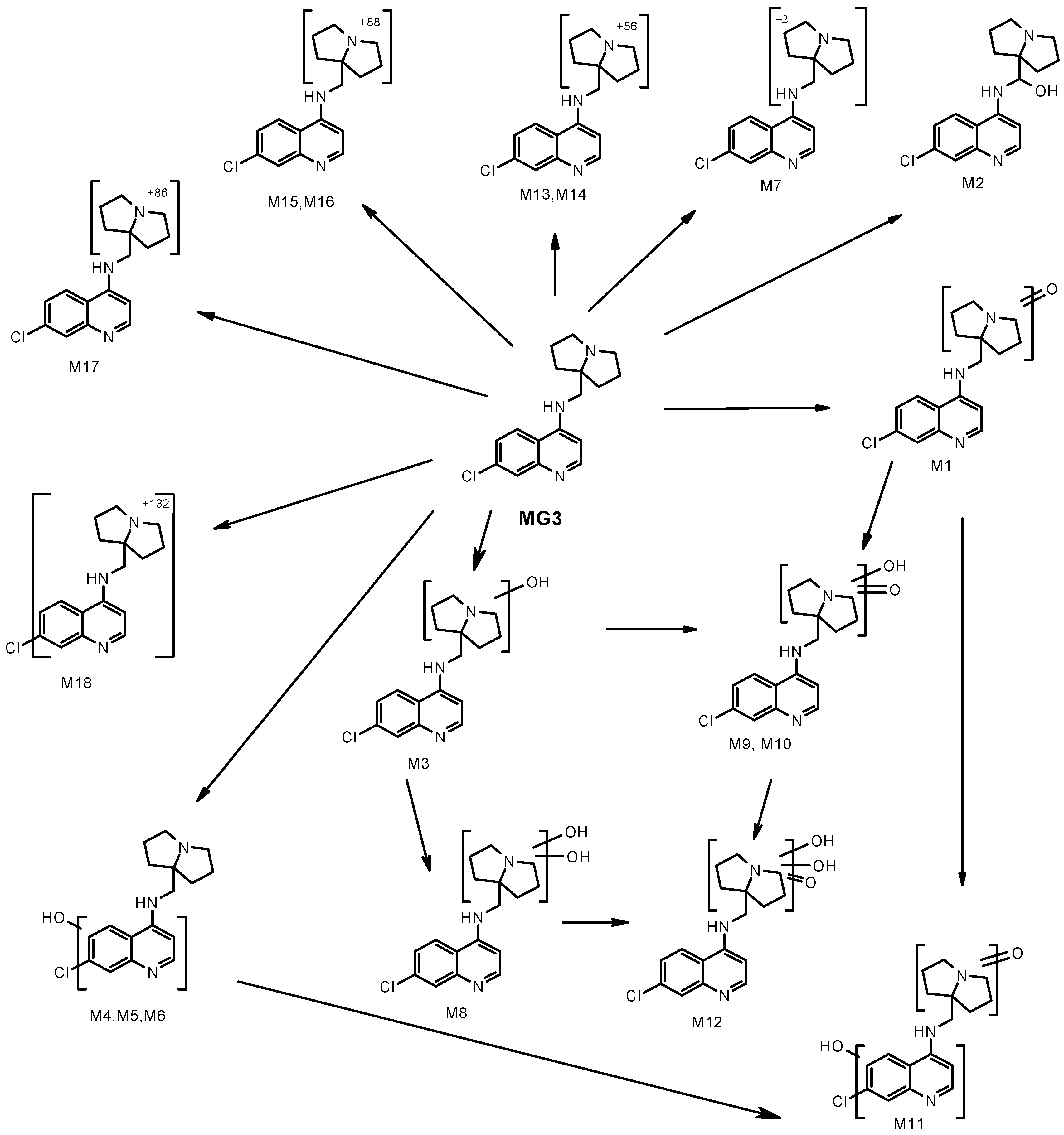
3.3.1. Intrinsic Clearance, Metabolism and P450 Interactions of MG3
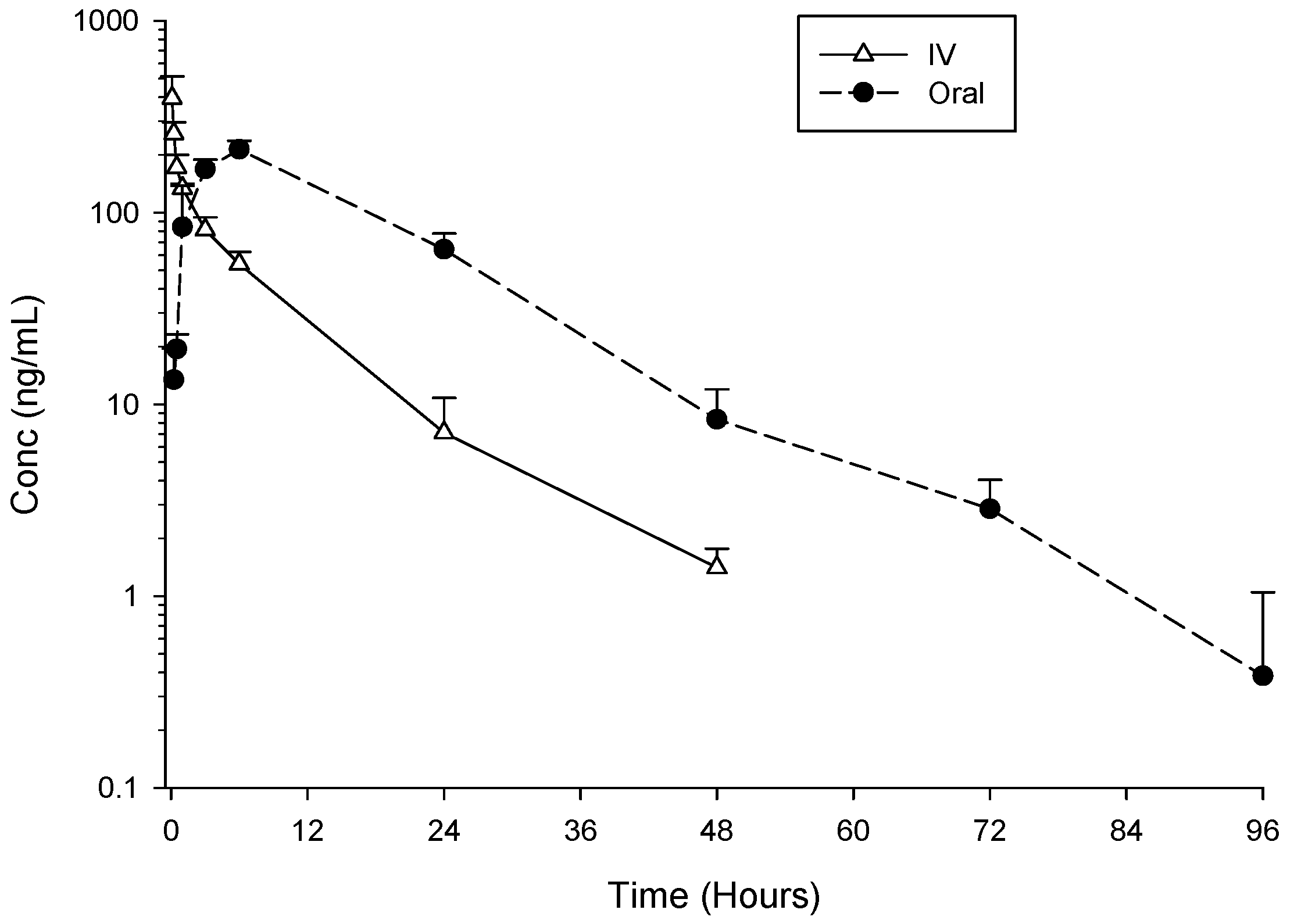
3.3.2. In Vivo Pharmacokinetics Study in Rats
3.3.3. Tissue Distribution, Plasma Protein Binding and Blood Partitioning of MG3
3.3.4. Preclinical Toxicology
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. World Malaria Report; WHO: Geneva, Switzerland, 2022.
- Noedl, H.; Se, Y.; Schaecher, K.; Smith, B.L.; Socheat, D.; Fukuda, M.M.; Artemisinin Resistance in Cambodia 1 (ARC1) Study Consortium. Evidence of artemisinin-resistant malaria in western Cambodia. N. Engl. J. Med. 2008, 359, 2619–2620. [Google Scholar] [CrossRef]
- Balikagala, B.; Fukuda, N.; Ikeda, M.; Katuro, O.T.; Tachibana, S.I.; Yamauchi, M.; Opio, W.; Emoto, S.; Anywar, D.A.; Kimura, E.; et al. Evidence of Artemisinin-Resistant Malaria in Africa. N. Engl. J. Med. 2021, 385, 1163–1171. [Google Scholar] [CrossRef]
- Ndwiga, L.; Kimenyi, K.M.; Wamae, K.; Osoti, V.; Akinyi, M.; Omedo, I.; Ishengoma, D.S.; Duah-Quashie, N.; Andagalu, B.; Ghansah, A.; et al. A review of the frequencies of Plasmodium falciparum Kelch 13 artemisinin resistance mutations in Africa. Int. J. Parasitol. Drugs Drug Resist. 2021, 16, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Dondorp, A.M.; Nosten, F.; Yi, P.; Das, D.; Phyo, A.P.; Tarning, J.; Lwin, K.M.; Ariey, F.; Hanpithakpong, W.; Lee, S.J.; et al. Artemisinin resistance in Plasmodium falciparum malaria. N. Engl. J. Med. 2009, 361, 455–467. [Google Scholar] [CrossRef]
- Mok, S.; Ashley, E.A.; Ferreira, P.E.; Zhu, L.; Lin, Z.; Yeo, T.; Chotivanich, K.; Imwong, M.; Pukrittayakamee, S.; Dhorda, M.; et al. Drug resistance. Population transcriptomics of human malaria parasites reveals the mechanism of artemisinin resistance. Science 2015, 347, 431–435. [Google Scholar] [CrossRef]
- Straimer, J.; Gnädig, N.F.; Witkowski, B.; Amaratunga, C.; Duru, V.; Ramadani, A.P.; Dacheux, M.; Khim, N.; Zhang, L.; Lam, S.; et al. Drug resistance. K13-propeller mutations confer artemisinin resistance in Plasmodium falciparum clinical isolates. Science 2015, 347, 428–431. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Malaria Programme; WHO: Geneva, Switzerland, 2020.
- WWARN. WorldWide Artemisinin Resistance Network. Available online: https://www.wwarn.org/ (accessed on 5 May 2023).
- Burrows, J.N.; Duparc, S.; Gutteridge, W.E.; Hooft van Huijsduijnen, R.; Kaszubska, W.; Macintyre, F.; Mazzuri, S.; Möhrle, J.J.; Wells, T.N.C. New developments in anti-malarial target candidate and product profiles. Malar. J. 2017, 16, 26. [Google Scholar] [CrossRef]
- van der Pluijm, R.W.; Amaratunga, C.; Dhorda, M.; Dondorp, A.M. Triple Artemisinin-Based Combination Therapies for Malaria—A New Paradigm? Trends Parasitol. 2021, 37, 15–24. [Google Scholar] [CrossRef]
- Peto, T.J.; Tripura, R.; Callery, J.J.; Lek, D.; Nghia, H.D.T.; Nguon, C.; Thuong, N.T.H.; van der Pluijm, R.W.; Dung, N.T.P.; Sokha, M.; et al. Triple therapy with artemether-lumefantrine plus amodiaquine versus artemether-lumefantrine alone for artemisinin-resistant, uncomplicated falciparum malaria: An open-label, randomised, multicentre trial. Lancet Infect. Dis. 2022, 22, 867–878. [Google Scholar] [CrossRef] [PubMed]
- Yadav, P.; Shah, K. Quinolines, a perpetual, multipurpose scaffold in medicinal chemistry. Bioorg. Chem. 2021, 109, 104639. [Google Scholar] [CrossRef] [PubMed]
- Koita, O.A.; Sangaré, L.; Miller, H.D.; Sissako, A.; Coulibaly, M.; Thompson, T.A.; Fongoro, S.; Diarra, Y.; Ba, M.; Maiga, A.; et al. AQ-13, an investigational antimalarial, versus artemether plus lumefantrine for the treatment of uncomplicated Plasmodium falciparum malaria: A randomised, phase 2, non-inferiority clinical trial. Lancet Infect. Dis. 2017, 17, 1266–1275. [Google Scholar] [CrossRef]
- Mengue, J.B.; Held, J.; Kreidenweiss, A. AQ-13—An investigational antimalarial drug. Expert Opin. Investig. Drugs 2019, 28, 217–222. [Google Scholar] [CrossRef]
- Nardella, F.; Mairet-Khedim, M.; Roesch, C.; Maher, S.P.; Ke, S.; Leang, R.; Leroy, D.; Witkowski, B. Cross-resistance of the chloroquine-derivative AQ-13 with amodiaquine in Cambodian Plasmodium falciparum isolates. J. Antimicrob. Chemother. 2021, 76, 2565–2568. [Google Scholar] [CrossRef] [PubMed]
- Adoke, Y.; Zoleko-Manego, R.; Ouoba, S.; Tiono, A.B.; Kaguthi, G.; Bonzela, J.E.; Duong, T.T.; Nahum, A.; Bouyou-Akotet, M.; Ogutu, B.; et al. A randomized, double-blind, phase 2b study to investigate the efficacy, safety, tolerability and pharmacokinetics of a single-dose regimen of ferroquine with artefenomel in adults and children with uncomplicated Plasmodium falciparum malaria. Malar. J. 2021, 20, 222. [Google Scholar] [CrossRef] [PubMed]
- Biot, C.; Nosten, F.; Fraisse, L.; Ter-Minassian, D.; Khalife, J.; Dive, D. The antimalarial ferroquine: From bench to clinic. Parasite 2011, 18, 207–214. [Google Scholar] [CrossRef]
- MMV. Medicine for Malaria Venture, Geneva, Switzerland. Available online: www.mmv.org (accessed on 5 May 2023).
- Van Voorhis, W.C.; Adams, J.H.; Adelfio, R.; Ahyong, V.; Akabas, M.H.; Alano, P.; Alday, A.; Alemán Resto, Y.; Alsibaee, A.; Alzualde, A.; et al. Open Source Drug Discovery with the Malaria Box Compound Collection for Neglected Diseases and Beyond. PLoS Pathog. 2016, 12, e1005763. [Google Scholar] [CrossRef]
- Battle, K.E.; Lucas, T.C.D.; Nguyen, M.; Howes, R.E.; Nandi, A.K.; Twohig, K.A.; Pfeffer, D.A.; Cameron, E.; Rao, P.C.; Casey, D.; et al. Mapping the global endemicity and clinical burden of Plasmodium vivax, 2000–2017: A spatial and temporal modelling study. Lancet 2019, 394, 332–343. [Google Scholar] [CrossRef]
- Sparatore, A.; Basilico, N.; Parapini, S.; Romeo, S.; Novelli, F.; Sparatore, F.; Taramelli, D. 4-Aminoquinoline quinolizidinyl- and quinolizidinylalkyl-derivatives with antimalarial activity. Bioorg. Med. Chem. 2005, 13, 5338–5345. [Google Scholar] [CrossRef] [PubMed]
- Basilico, N.; Parapini, S.; Sparatore, A.; Romeo, S.; Misiano, P.; Vivas, L.; Yardley, V.; Croft, S.L.; Habluetzel, A.; Lucantoni, L.; et al. In Vivo and In Vitro Activities and ADME-Tox Profile of a Quinolizidine-Modified 4-Aminoquinoline: A Potent Anti-P. falciparum and Anti-P. vivax Blood-Stage Antimalarial. Molecules 2017, 22, 2102. [Google Scholar] [CrossRef]
- Sparatore, A.; Basilico, N.; Casagrande, M.; Parapini, S.; Taramelli, D.; Brun, R.; Wittlin, S.; Sparatore, F. Antimalarial activity of novel pyrrolizidinyl derivatives of 4-aminoquinoline. Bioorg. Med. Chem. Lett. 2008, 18, 3737–3740. [Google Scholar] [CrossRef]
- Miyano, S.; Sumoto, K.; Satoh, F.; Shima, K.; Hayashimatsu, M.; Morita, M.; Aisaka, K.; Noguchi, T. New antiarrhythmic agents. N-aryl-8-pyrrolizidinealkanamides. J. Med. Chem. 1985, 28, 714–717. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, O.A.; Belley-Côté, E.P.; Um, K.J.; Baranchuk, A.; Benz, A.P.; Dalmia, S.; Wang, C.N.; Alhazzani, W.; Conen, D.; Devereaux, P.J.; et al. Single-dose oral anti-arrhythmic drugs for cardioversion of recent-onset atrial fibrillation: A systematic review and network meta-analysis of randomized controlled trials. Europace 2021, 23, 1200–1210. [Google Scholar] [CrossRef]
- Garcia-Delgado, N.; Bertrand, S.; Nguyen, K.T.; van Deursen, R.; Bertrand, D.; Reymond, J.L. Exploring α7-Nicotinic Receptor Ligand Diversity by Scaffold Enumeration from the Chemical Universe Database GDB. ACS Med. Chem. Lett. 2010, 1, 422–426. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bréthous, L.; Garcia-Delgado, N.; Schwartz, J.; Bertrand, S.; Bertrand, D.; Reymond, J.L. Synthesis and nicotinic receptor activity of chemical space analogues of N-(3R)-1-azabicyclo[2.2.2]oct-3-yl-4-chlorobenzamide (PNU-282,987) and 1,4-diazabicyclo[3.2.2]nonane-4-carboxylic acid 4-bromophenyl ester (SSR180711). J. Med. Chem. 2012, 55, 4605–4618. [Google Scholar] [CrossRef]
- Oka, M.; Matsumoto, Y.; Hirooka, K.; Suzuki, T. Synthesis of 1-azabicyclo[3.3.0]octane derivatives and their effects as piracetam-like nootropics. Chem. Pharm. Bull. 2000, 48, 1121–1124. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Suzuki, T.; Usui, T.; Oka, M.; Kataoka, T. Synthesis and muscarinic activity of a series of quinolines and naphthalenes with a 1-azabicyclo[3.3.0]octane moiety. Chem. Pharm. Bull. 1998, 46, 1265–1273. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Suzuki, T.; Oka, M.; Maeda, K.; Furusawa, K.; Uesaka, H.; Kataoka, T. Synthesis and muscarinic activity of novel aniline derivatives with a 1-azabicyclo[3.3.0]octane moiety. Chem. Pharm. Bull. 1999, 47, 28–36. [Google Scholar] [CrossRef][Green Version]
- Takeda, M.; Tsukamoto, K.; Yamano, M.; Uesaka, H. Effects of SK-951, a benzofuran derivative, as a prokinetic agent in rats and dogs. Jpn. J. Pharmacol. 1999, 81, 292–297. [Google Scholar] [CrossRef]
- Parapini, S.; Basilico, N.; Pasini, E.; Egan, T.J.; Olliaro, P.; Taramelli, D.; Monti, D. Standardization of the physicochemical parameters to assess in vitro the beta-hematin inhibitory activity of antimalarial drugs. Exp. Parasitol. 2000, 96, 249–256. [Google Scholar] [CrossRef]
- de Villiers, K.A.; Egan, T.J. Heme Detoxification in the Malaria Parasite: A Target for Antimalarial Drug Development. Acc. Chem. Res. 2021, 54, 2649–2659. [Google Scholar] [CrossRef]
- Vivas, L.; Rattray, L.; Stewart, L.B.; Robinson, B.L.; Fugmann, B.; Haynes, R.K.; Peters, W.; Croft, S.L. Antimalarial efficacy and drug interactions of the novel semi-synthetic endoperoxide artemisone in vitro and in vivo. J. Antimicrob. Chemother. 2007, 59, 658–665. [Google Scholar] [CrossRef] [PubMed]
- Trager, W.; Jensen, J.B. Human malaria parasites in continuous culture. Science 1976, 193, 673–675. [Google Scholar] [CrossRef]
- Makler, M.T.; Hinrichs, D.J. Measurement of the lactate dehydrogenase activity of Plasmodium falciparum as an assessment of parasitemia. Am. J. Trop. Med. Hyg. 1993, 48, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Suwanarusk, R.; Russell, B.; Ong, A.; Sriprawat, K.; Chu, C.S.; PyaePhyo, A.; Malleret, B.; Nosten, F.; Renia, L. Methylene blue inhibits the asexual development of vivax malaria parasites from a region of increasing chloroquine resistance. J. Antimicrob. Chemother. 2015, 70, 124–129. [Google Scholar] [CrossRef][Green Version]
- Peters, W. Drug resistance in Plasmodium berghei Vincke and Lips, 1948. I. Chloroquine resistance. Exp. Parasitol. 1965, 17, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Peretto, I.; Radaelli, S.; Parini, C.; Zandi, M.; Raveglia, L.F.; Dondio, G.; Fontanella, L.; Misiano, P.; Bigogno, C.; Rizzi, A.; et al. Synthesis and biological activity of flurbiprofen analogues as selective inhibitors of beta-amyloid(1)(-)(42) secretion. J. Med. Chem. 2005, 48, 5705–5720. [Google Scholar] [CrossRef]
- Clarke, H.; Bean, H. Working with Hazardous Chemicals. Org. Synth. 1931, 11, 4. [Google Scholar] [CrossRef]
- Wang, B.; Zhang, W.; Zhang, L.; Du, D.; Liu, G.; Xu, J. Versatile Synthesis of Free and N-Benzyloxycarbonyl-Protected 2,2-Disubstituted Taurines. Eur. J. Org. Chem. 2008, 2008, 350–355. [Google Scholar] [CrossRef]
- Deng, S.L.; Liu, D. Studies on Phosphoroheterocycle Chemistry II: A Simple and New Route to 1, 3, 2-Diazaphospholidine-4-thione 2-sulfide Derivatives. Synthesis 2001, 16, 2445–2449. [Google Scholar] [CrossRef]
- Jenny, C.; Heimgartner, H. Synthese von 4,4-disubstituierten 1,3-Thiazol-5(4H)-thionen. Helvetica 1986, 69, 374–388. [Google Scholar] [CrossRef]
- O’Neill, P.M.; Shone, A.E.; Stanford, D.; Nixon, G.; Asadollahy, E.; Park, B.K.; Maggs, J.L.; Roberts, P.; Stocks, P.A.; Biagini, G.; et al. Synthesis, antimalarial activity, and preclinical pharmacology of a novel series of 4′-fluoro and 4′-chloro analogues of amodiaquine. Identification of a suitable “back-up” compound for N-tert-butyl isoquine. J. Med. Chem. 2009, 52, 1828–1844. [Google Scholar] [CrossRef]
- Warhurst, D.C.; Craig, J.C.; Adagu, I.S.; Guy, R.K.; Madrid, P.B.; Fivelman, Q.L. Activity of piperaquine and other 4-aminoquinoline antiplasmodial drugs against chloroquine-sensitive and resistant blood-stages of Plasmodium falciparum. Role of beta-haematin inhibition and drug concentration in vacuolar water- and lipid-phases. Biochem. Pharmacol. 2007, 73, 1910–1926. [Google Scholar] [CrossRef]
- O’Neill, P.M.; Amewu, R.K.; Nixon, G.L.; Bousejra ElGarah, F.; Mungthin, M.; Chadwick, J.; Shone, A.E.; Vivas, L.; Lander, H.; Barton, V.; et al. Identification of a 1,2,4,5-tetraoxane antimalarial drug-development candidate (RKA 182) with superior properties to the semisynthetic artemisinins. Angew. Chem. Int. Ed. Engl. 2010, 49, 5693–5697. [Google Scholar] [CrossRef] [PubMed]
- Benoit-Vical, F.; Robert, A.; Meunier, B. In vitro and in vivo potentiation of artemisinin and synthetic endoperoxide antimalarial drugs by metalloporphyrins. Antimicrob. Agents Chemother. 2000, 44, 2836–2841. [Google Scholar] [CrossRef]
- Bell, A. Antimalarial drug synergism and antagonism: Mechanistic and clinical significance. FEMS Microbiol. Lett. 2005, 253, 171–184. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, S.; Silvestrini, F.; Dechering, K.; Corbett, Y.; Parapini, S.; Timmerman, M.; Galastri, L.; Basilico, N.; Sauerwein, R.; Alano, P.; et al. A Plasmodium falciparum screening assay for anti-gametocyte drugs based on parasite lactate dehydrogenase detection. J. Antimicrob. Chemother. 2013, 68, 2048–2058. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, S.; Camarda, G.; Corbett, Y.; Siciliano, G.; Parapini, S.; Cevenini, L.; Michelini, E.; Roda, A.; Leroy, D.; Taramelli, D.; et al. A chemical susceptibility profile of the Plasmodium falciparum transmission stages by complementary cell-based gametocyte assays. J. Antimicrob. Chemother. 2016, 71, 1148–1158. [Google Scholar] [CrossRef]
- Moore, B.R.; Page-Sharp, M.; Stoney, J.R.; Ilett, K.F.; Jago, J.D.; Batty, K.T. Pharmacokinetics, pharmacodynamics, and allometric scaling of chloroquine in a murine malaria model. Antimicrob. Agents Chemother. 2011, 55, 3899–3907. [Google Scholar] [CrossRef]
- Davis, C.B.; Bambal, R.; Moorthy, G.S.; Hugger, E.; Xiang, H.; Park, B.K.; Shone, A.E.; O’Neill, P.M.; Ward, S.A. Comparative preclinical drug metabolism and pharmacokinetic evaluation of novel 4-aminoquinoline anti-malarials. J. Pharm. Sci. 2009, 98, 362–377. [Google Scholar] [CrossRef]
- McLean, E.K. The toxic actions of pyrrolizidine (senecio) alkaloids. Pharmacol. Rev. 1970, 22, 429–483. [Google Scholar]
- Swick, R.A. Hepatic metabolism and bioactivation of mycotoxins and plant toxins. J. Anim. Sci. 1984, 58, 1017–1028. [Google Scholar] [CrossRef] [PubMed]
- Rendic, S.; Guengerich, F.P. Metabolism and Interactions of Chloroquine and Hydroxychloroquine with Human Cytochrome P450 Enzymes and Drug Transporters. Curr. Drug Metab. 2020, 21, 1127–1135. [Google Scholar] [CrossRef] [PubMed]
- Ericsson, T.; Sundell, J.; Torkelsson, A.; Hoffmann, K.J.; Ashton, M. Effects of artemisinin antimalarials on Cytochrome P450 enzymes in vitro using recombinant enzymes and human liver microsomes: Potential implications for combination therapies. Xenobiotica 2014, 44, 615–626. [Google Scholar] [CrossRef] [PubMed]
- Ramanathan-Girish, S.; Catz, P.; Creek, M.R.; Wu, B.; Thomas, D.; Krogstad, D.J.; De, D.; Mirsalis, J.C.; Green, C.E. Pharmacokinetics of the antimalarial drug, AQ-13, in rats and cynomolgus macaques. Int. J. Toxicol. 2004, 23, 179–189. [Google Scholar] [CrossRef]
- O’Neill, P.M.; Park, B.K.; Shone, A.E.; Maggs, J.L.; Roberts, P.; Stocks, P.A.; Biagini, G.A.; Bray, P.G.; Gibbons, P.; Berry, N.; et al. Candidate selection and preclinical evaluation of N-tert-butyl isoquine (GSK369796), an affordable and effective 4-aminoquinoline antimalarial for the 21st century. J. Med. Chem. 2009, 52, 1408–1415. [Google Scholar] [CrossRef]
- Liu, X.; Jusko, W.J. Physiologically Based Pharmacokinetics of Lysosomotropic Chloroquine in Rat and Human. J. Pharmacol. Exp. Ther. 2021, 376, 261–272. [Google Scholar] [CrossRef]
- Browning, D.J. Pharmacology of Chloroquine and Hydroxychloroquine. In Hydroxychloroquine and Chloroquine Retinopathy; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Winstanley, P.A.; Edwards, G.; Curtis, C.G.; Orme, M.L.; Powell, G.M.; Breckenridge, A.M. Tissue distribution and excretion of amodiaquine in the rat. J. Pharm. Pharmacol. 1988, 40, 343–349. [Google Scholar] [CrossRef]
- Mortelmans, K.; Zeiger, E. The Ames Salmonella/microsome mutagenicity assay. Mutat. Res. 2000, 455, 29–60. [Google Scholar] [CrossRef]
- Mortelmans, K.; Riccio, E.S. The bacterial tryptophan reverse mutation assay with Escherichia coli WP2. Mutat. Res. 2000, 455, 61–69. [Google Scholar] [CrossRef]
- Chiu, P.J.; Marcoe, K.F.; Bounds, S.E.; Lin, C.H.; Feng, J.J.; Lin, A.; Cheng, F.C.; Crumb, W.J.; Mitchell, R. Validation of a [3H]astemizole binding assay in HEK293 cells expressing HERG K+ channels. J. Pharmacol. Sci. 2004, 95, 311–319. [Google Scholar] [CrossRef]
- Duru, V.; Khim, N.; Leang, R.; Kim, S.; Domergue, A.; Kloeung, N.; Ke, S.; Chy, S.; Eam, R.; Khean, C.; et al. Plasmodium falciparum dihydroartemisinin-piperaquine failures in Cambodia are associated with mutant K13 parasites presenting high survival rates in novel piperaquine in vitro assays: Retrospective and prospective investigations. BMC Med. 2015, 13, 305. [Google Scholar] [CrossRef] [PubMed]
- Ménard, S.; Ben Haddou, T.; Ramadani, A.P.; Ariey, F.; Iriart, X.; Beghain, J.; Bouchier, C.; Witkowski, B.; Berry, A.; Mercereau-Puijalon, O.; et al. Induction of Multidrug Tolerance in Plasmodium falciparum by Extended Artemisinin Pressure. Emerg. Infect. Dis. 2015, 21, 1733–1741. [Google Scholar] [CrossRef] [PubMed]


| Time (min) | % A | % B |
|---|---|---|
| 0 | 98 | 2 |
| 4 | 98 | 2 |
| 13 | 85 | 15 |
| 18 | 5 | 95 |
| 23 | 5 | 95 |
| 23.5 | 98 | 2 |
| 35 | 98 | 2 |
| Compounds | P. falciparum IC50 nM | P. falciparum IC50 nM d | P. vivax IC50 nM d | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| D10 a (CQ-S) | W2 a (CQ-R) | 3D7 b (CQ-S) | K1 b (CQ-R) | V1-S (CQ-R) b | TM90C2A (CQ-R) b | FCR3 (CQ-R) b | IPC5202 (ARM-R) c | Field Isolates | ||
| MG3 | 30.6 | 28.9 | 12.6 | 21.2 | 25.7 | 14.4 | 13.2 | 10.7 | 20.9 | 50.3 |
| CQ | 16.5 | 293.5 | 12.1 | 708.5 | 773.7 | 145.4 | 193.8 | 162.8 | 251.9 | 86.6 |
| ASN | NT | NT | 2.9 | 2.6 | 2.7 | 2.6 | 2.6 | NT | 4.2 | 2.3 |
| DHA | 3.9 | 2.0 | 3.0 | 1.4 | 1.8 | NT | 1.23 | 2.2 | NT | NT |
| Compound | P. berghei ANKA | P. chabaudi AS | P. yoelii NS | |||
|---|---|---|---|---|---|---|
| ED50 b (95% CI c) | ED90 b (95% CI) | ED50 (95% CI) | ED90 (95% CI) | ED50 (95% CI) | ED90 (95% CI) | |
| Mean (mg/kg) | Mean (mg/kg) | Mean (mg/kg) | ||||
| MG3 | 5.22 (2.86–7.58) | 7.55 (6.38–8.72) | 4.69 (3.49–5.90) | 9.80 (8.86–10.6) | 5.01 (4.21–5.95) | 8.98 (6.70–12.02) |
| FAQ4 d | 5.30 (4.10–6.80) | 12.40 (10.7–14.4) | n.a. | n.a. | 7.70 (6.70–8.90) | 10.60 (9.40–11.80) |
| CQ | 3.82 (3.32–4.32) | 6.59 (5.60–7.58) | 2.53 (2.44–2.63) | 6.37 (5.60–7.14) | 3.61 (2.75–4.73) | 22.59 (12.6–40.5) |
| Mouse | Rat | Dog | Monkey | Human | |
|---|---|---|---|---|---|
| Half/life (min) | 31 | 65 | 48 | 86 | 340 |
| Intrinsic clearance (mL/min/kg) | 196 | 51 | 111 | 44 | 4.9 |
| Met ID | Molecular Formula | m/z | RT (min) | % of Total Drug Related Material a | ||||
|---|---|---|---|---|---|---|---|---|
| Mouse | Rat | Dog | Monkey | Human | ||||
| MG3 | C17H20N3Cl | 302.14 | 9.9 | 31 | 53 | 29 | 28 | 82 |
| M1 | C17H18N3OCl | 316.12 | 16.5 | 24 | 17 | 10 | 44 | 11 |
| M2 | C17H20N3OCl | 318.14 | 9.6 | 3 | 6 | 27 | 1 | 1 |
| M3 b | C17H20N3OCl | 318.14 | 11.5 | 4 | 3 | 11 | 4 | <1 |
| M4 | C17H20N3OCl | 318.14 | 12.3 | 1 | nd | nd | nd | nd |
| M5 | C17H20N3OCl | 318.14 | 12.9 | 1 | <1 | nd | nd | nd |
| M6 | C17H20N3OCl | 318.14 | 13.3 | 12 | 15 | 3 | 1 | 3 |
| M7 | C17H18N3Cl | 300.13 | 4.0 | 1 | nd | nd | nd | nd |
| M8 | C17H20N3O2Cl | 334.12 | 6.9 | 2 | nd | 4 | 10 | nd |
| M9 | C17H18N3O2Cl | 332.12 | 13.1 | 4 | 1 | <1 | 2 | nd |
| M10 | C17H18N3O2Cl | 332.12 | 17.2 | 2 | <1 | <1 | <1 | nd |
| M11 | C17H18N3O2Cl | 332.12 | 17.5 | <1 | <1 | nd | <1 | nd |
| M12 | C17H18N3O3Cl | 348.11 | 14.2 | 2 | <1 | <1 | 1 | nd |
| M13 | C20H24N3OCl | 358.17 | 11.7 | <1 | <1 | 3 | <1 | nd |
| M14 | C20H24N3OCl | 358.17 | 12.6 | 4 | 2 | 9 | 2 | <1 |
| M15 | C20H24N3O3Cl | 390.16 | 11.2 | 3 | <1 | <1 | <1 | nd |
| M16 | C20H24N3O3Cl | 390.16 | 11.8 | 3 | nd | <1 | <1 | nd |
| M17 | C20H22N3O3Cl | 388.15 | 12.0 | <1 | nd | 2 | 1 | nd |
| M18 | C22H28N3O4Cl | 434.18 | 11.7 | nd | <1 | <1 | 2 | 2 |
| P450 Interaction a | |||||
|---|---|---|---|---|---|
| Compounds | CYP1A2 | CYP2C9 | CYP2C19 | CYP2D6 | CYP3A4 |
| CEC | MFC | CEC | AMMC | BFC | |
| Mean % inhibition at 3 µM | |||||
| MG3 | 12.1 ± 1.2 | 8.8 ± 2.2 | <3 | 5.7 ±1.2 | 4.3 ± 1.0 |
| CQ | <3 | <3 | <3 | 20.4 ± 1.1 | 6.8 ± 1.7 |
| Parameter (Unit) | MG3 Oral 30 mg/kg | MG3 IV 10 mg/kg |
|---|---|---|
| Mean ± SD | Mean ± SD | |
| Cmax (ng/mL) a | 213.0 ± 23.7 | 395 ± 118 |
| AUC0-t(last) (ng·h/mL) | 4360 ± 630 | 1290 ± 217 |
| t1/2 (h) | 10.7 ± 1.2 | 7.7 ± 0.6 |
| tlast (h) | 80.0 ± 13.9 | 48.0 ± 0.1 |
| AUC0-∞ (ng·h/mL) | 4400 ± 633 | 1300 ± 223 |
| CL (mL/min/kg) | 139.0 ± 20.2 | |
| Vss (mL/kg) | 59,900 ± 7580 | |
| F% AUC0-∞ | 112 |
| Dose (a) | Male | Female | |||||
|---|---|---|---|---|---|---|---|
| Cmax (b) (µg/mL) | AUC0–24 (c) (µg·h/mL) | Cmax (b) (µg /mL) | AUC0–24 (c) (µg·h/mL) | ||||
| Day 1 | |||||||
| 30 | 0.143 ± 0.029 | 1.88 ± 0.19 | 0.17 ± 0.04 | 2.53 ± 0.50 | |||
| 60 | 0.22 ± 0.01 | 3.53 ± 0.18 | 0.259 ± 0.046 | 4.74 ± 0.77 | |||
| 120 | 0.209 ± 0.049 | 3.84 ± 0.70 | 0.411 ± 0.288 | 5.21 ± 1.60 | |||
| Day 7 | |||||||
| Cmax (b) | AUC0–24 (c) | AUC0–48 (d) | Cmax (b) | AUC0–24 (c) | AUC0–48 (d) | ||
| 30 | 0.14 ± 0.03 | 1.88 ± 0.38 | 2.46 ± 0.55 | 0.149 ± 0.034 | 2.56 ± 0.65 | 3.8 ± 1.0 | |
| 60 | 0.321 ± 0.050 | 5.09 ± 0.45 | 7.33 ± 0.31 | 0.646 ± 0.201 | 8.63 ± 0.87 | 15.0 ± 0.9 | |
| 120 | 1.09 ± 0.26 | 17.4 ± 3.2 | 27.5 ± 3.9 | 1.57 ± 0.27 | 19.4 ± 7.5 | 29.8 ± 9.6 | |
| Parameter | Period | Dose (50 mg/kg) a | ||
|---|---|---|---|---|
| Male | Female | Mean ± SD | ||
| Cmax (ng/mL) | Day 5 | 67.5 | 72.7 | 70.1 ± 3.68 |
| AUC0–24 (ng.h/mL) | Day 5 | 802 | 989 | 896 ± 132 |
| tmax (h) | Day 5 | 2 | 0.5 | 1.25 ± 1.06 |
| t1/2, z (h) | Day 5 | 7.66 | 22.2 | 14.9 ± 10.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Basilico, N.; Parapini, S.; D’Alessandro, S.; Misiano, P.; Romeo, S.; Dondio, G.; Yardley, V.; Vivas, L.; Nasser, S.; Rénia, L.; et al. Favorable Preclinical Pharmacological Profile of a Novel Antimalarial Pyrrolizidinylmethyl Derivative of 4-amino-7-chloroquinoline with Potent In Vitro and In Vivo Activities. Biomolecules 2023, 13, 836. https://doi.org/10.3390/biom13050836
Basilico N, Parapini S, D’Alessandro S, Misiano P, Romeo S, Dondio G, Yardley V, Vivas L, Nasser S, Rénia L, et al. Favorable Preclinical Pharmacological Profile of a Novel Antimalarial Pyrrolizidinylmethyl Derivative of 4-amino-7-chloroquinoline with Potent In Vitro and In Vivo Activities. Biomolecules. 2023; 13(5):836. https://doi.org/10.3390/biom13050836
Chicago/Turabian StyleBasilico, Nicoletta, Silvia Parapini, Sarah D’Alessandro, Paola Misiano, Sergio Romeo, Giulio Dondio, Vanessa Yardley, Livia Vivas, Shereen Nasser, Laurent Rénia, and et al. 2023. "Favorable Preclinical Pharmacological Profile of a Novel Antimalarial Pyrrolizidinylmethyl Derivative of 4-amino-7-chloroquinoline with Potent In Vitro and In Vivo Activities" Biomolecules 13, no. 5: 836. https://doi.org/10.3390/biom13050836
APA StyleBasilico, N., Parapini, S., D’Alessandro, S., Misiano, P., Romeo, S., Dondio, G., Yardley, V., Vivas, L., Nasser, S., Rénia, L., Russell, B. M., Suwanarusk, R., Nosten, F., Sparatore, A., & Taramelli, D. (2023). Favorable Preclinical Pharmacological Profile of a Novel Antimalarial Pyrrolizidinylmethyl Derivative of 4-amino-7-chloroquinoline with Potent In Vitro and In Vivo Activities. Biomolecules, 13(5), 836. https://doi.org/10.3390/biom13050836








