Salmonella typhimurium Vaccine Candidate Delivering Infectious Bronchitis Virus S1 Protein to Induce Protection
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Statement
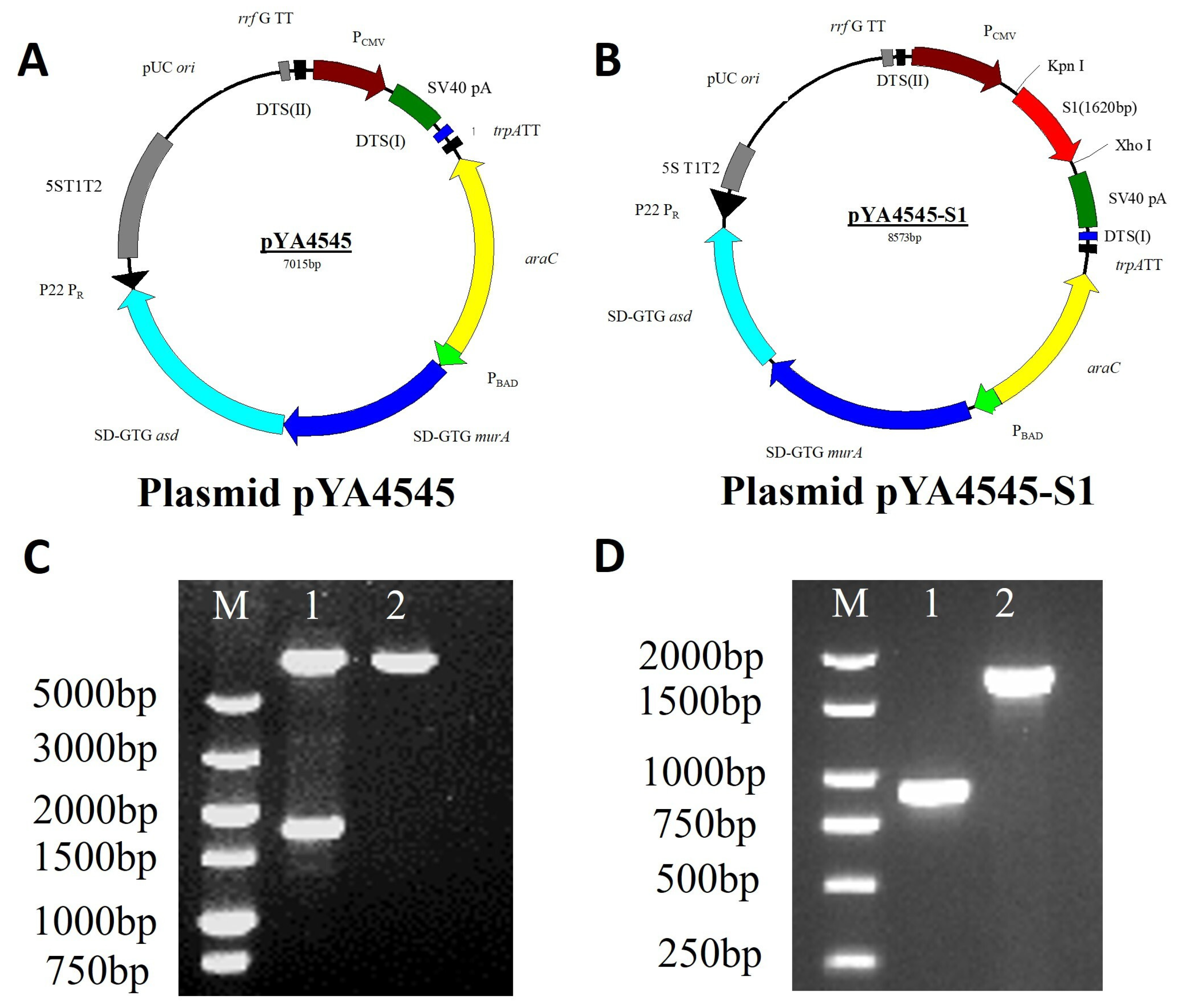
2.2. Bacterial Strains, Cells, and Plasmids
2.3. Virus Strain Propagation and Purification
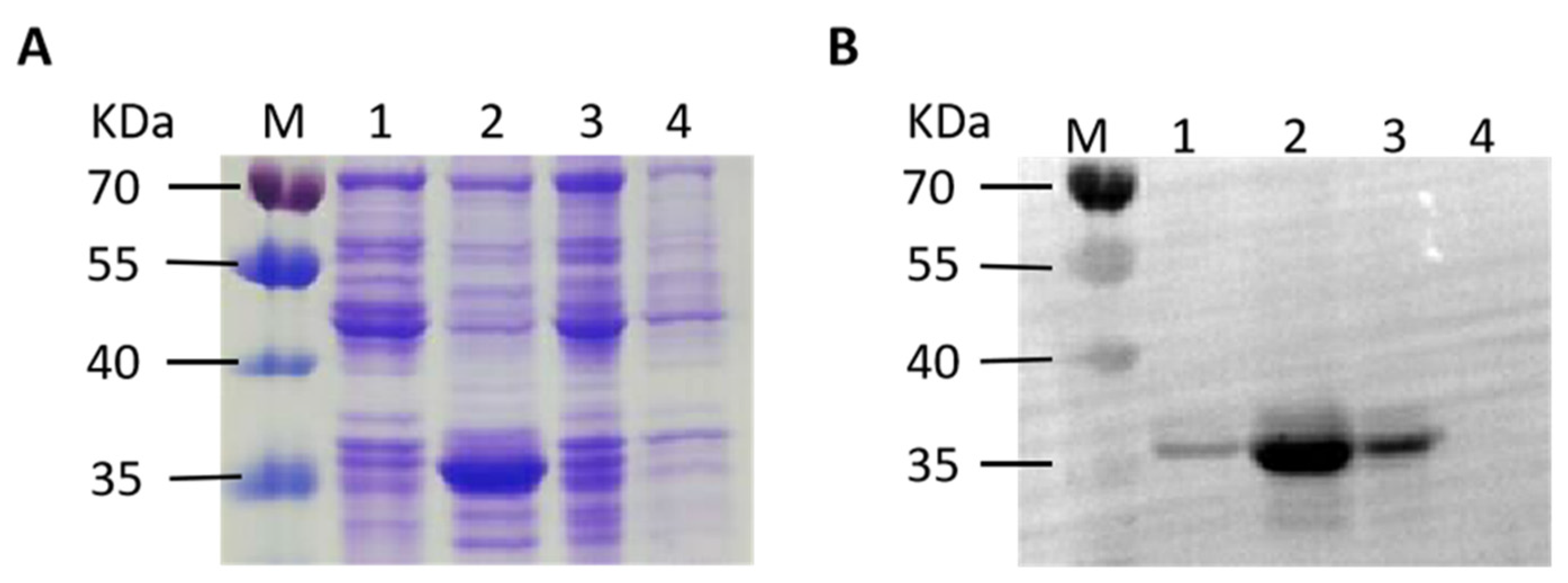
2.4. Expression and Purification of Recombinant S1 Proteins and Preparation of Antiserum
2.5. Vectors for Antigen Delivery via Regulated Delayed Attenuation and Lysis System
2.6. Analysis of Recombinant Protein Expressed In Vitro
2.7. Animal Experimental Design and Sample Collection
2.8. Immunization of SPF Chicken
2.9. EID50 of IBV Test and Challenge
2.10. Enzyme-Linked Immunosorbent Assay (ELISA) for Antibodies
2.11. Quantitative Real-Time PCR (qRT-PCR) for Cytokines
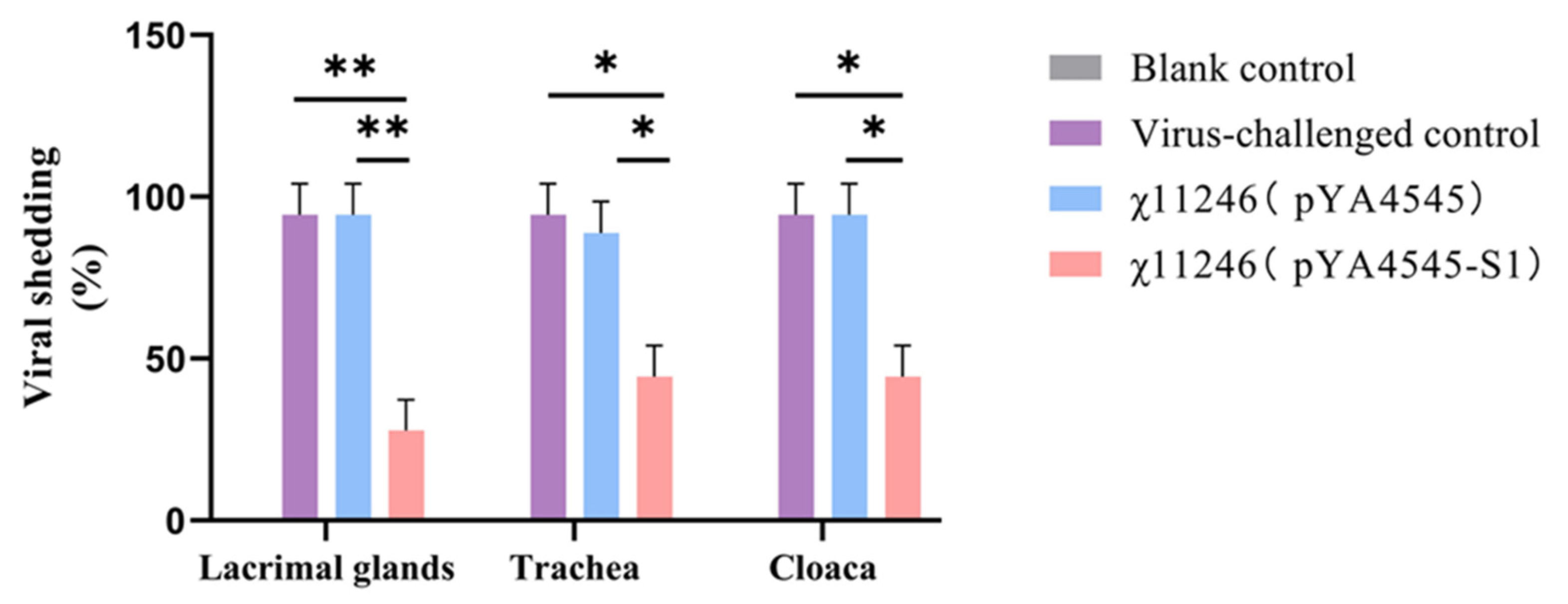
2.12. Viral Shedding Detection
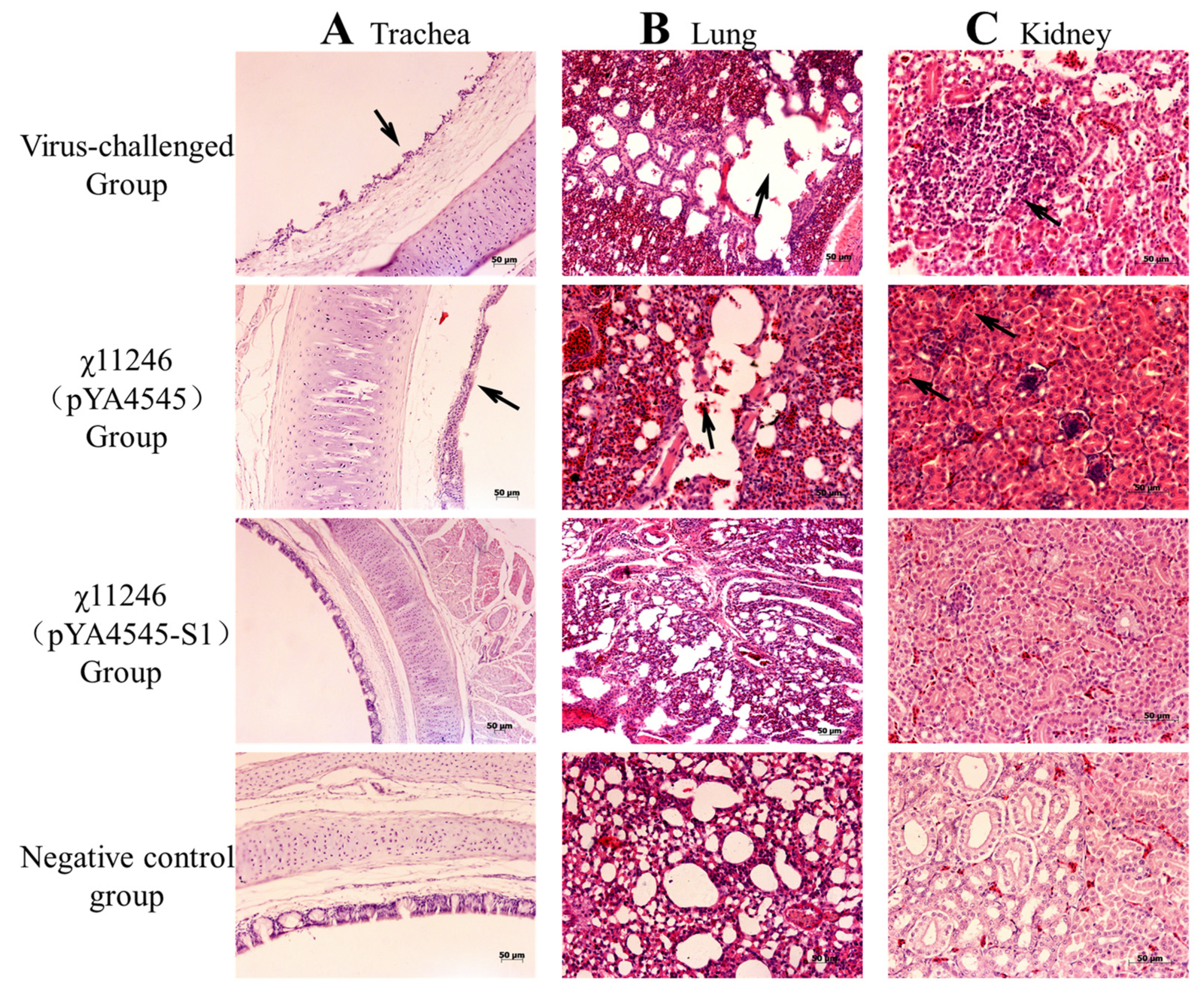
2.13. Histopathology
2.14. Statistical Analysis
3. Results
3.1. Construction and Characterization of Regulated Delayed Attenuation and Lysis S. typhimurium χ11246(pYA4545-S1)
3.2. Expression of Recombinant S1 Protein and Collection of Antisera
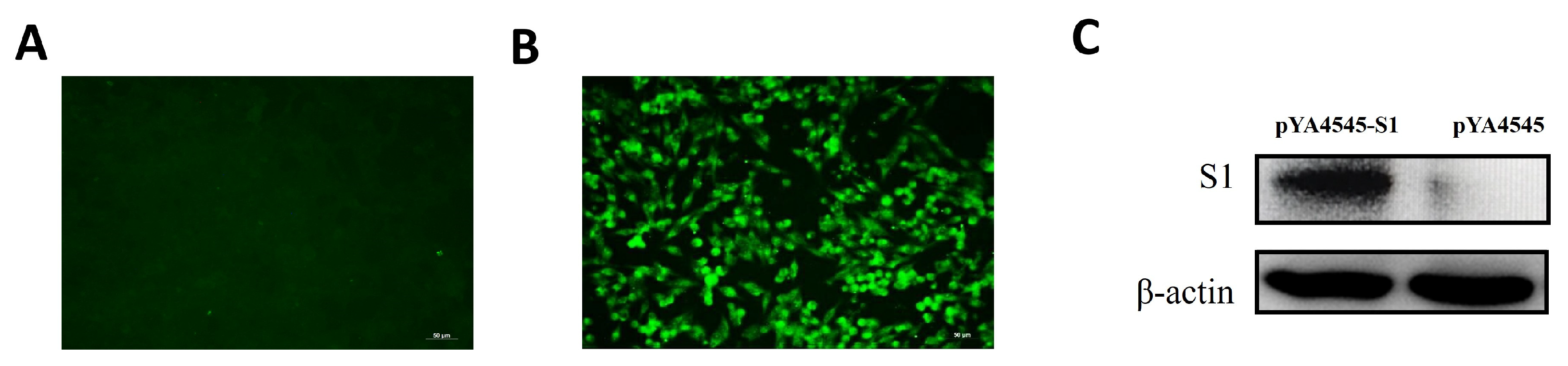
3.3. Expression of pYA4545-S1 In Vitro
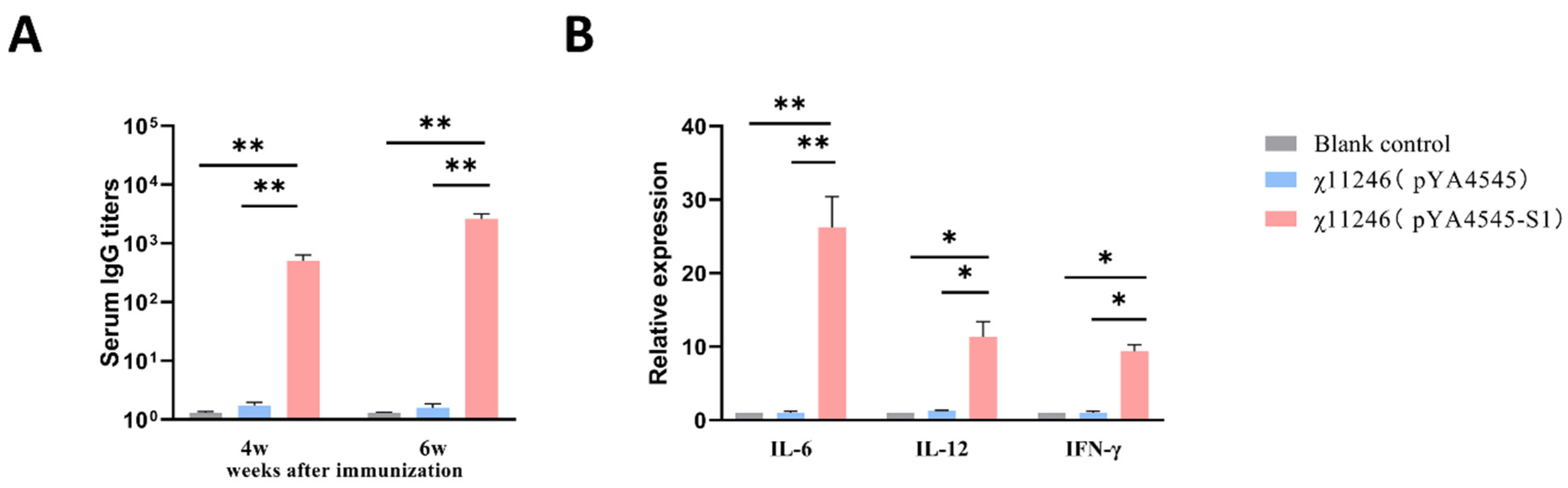
3.4. Antibody Responses after Immunization with χ11246(pYA4545-S1)
3.5. Changes of Cytokine Genes Expression Pattern
3.6. Orally Administered χ11246(pYA4545-S1) Provides Protection against 793B IBV Challenge
4. Discussion
5. Conclusions and Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Matoo, J.J.; Bashir, K.; Kumar, A.; Krishnaswamy, N.; Dey, S.; Chellappa, M.M.; Ramakrishnan, S. Resiquimod enhances mucosal and systemic immunity against avian infectious bronchitis virus vaccine in the chicken. Microb. Pathog. 2018, 119, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Hassan, M.S.H.; Najimudeen, S.M.; Farooq, M.; Shany, S.; El-Safty, M.M.; Shalaby, A.A.; Abdul-Careem, M.F. Efficacy of two vaccination strategies against infectious bronchitis in laying hens. Vaccines 2023, 11, 338. [Google Scholar] [CrossRef] [PubMed]
- Ambali, A.G.; Jones, R.C. Early pathogenesis in chicks of infection with an enterotropic strain of infectious bronchitis virus. Avian Dis. 1990, 34, 809–817. [Google Scholar] [CrossRef] [PubMed]
- Lv, C.; Shi, T.; Zhu, P.; Peng, X.; Cao, S.; Yan, Y.; Ojha, N.K.; Liao, M.; Zhou, J. Construction of an infectious bronchitis virus vaccine strain carrying chimeric s1 gene of a virulent isolate and its pathogenicity analysis. Appl. Microbiol. Biotechnol. 2020, 104, 8427–8437. [Google Scholar] [CrossRef] [PubMed]
- Moore, K.M.; Jackwood, M.W.; Hilt, D.A. Identification of amino acids involved in a serotype and neutralization specific epitope within the s1 subunit of avian infectious bronchitis virus. Arch. Virol. 1997, 142, 2249–2256. [Google Scholar] [CrossRef] [PubMed]
- Yin, L.; Zeng, Y.; Wang, W.; Wei, Y.; Xue, C.; Cao, Y. Immunogenicity and protective efficacy of recombinant fusion proteins containing spike protein of infectious bronchitis virus and hemagglutinin of H3N2 influenza virus in chickens. Virus Res. 2016, 223, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Bande, F.; Arshad, S.S.; Bejo, M.H.; Moeini, H.; Omar, A.R. Progress and challenges toward the development of vaccines against avian infectious bronchitis. J. Immunol. Res. 2015, 2015, 424860. [Google Scholar] [CrossRef]
- Bande, F.; Arshad, S.S.; Hair Bejo, M.; Kadkhodaei, S.; Omar, A.R. Prediction and in silico identification of novel B-Cells and T-Cells epitopes in the S1-spike glycoprotein of M41 and CR88 (793/B) infectious bronchitis virus serotypes for application in peptide vaccines. Adv. Bioinform. 2016, 2016, 5484972. [Google Scholar] [CrossRef]
- Jiao, H.; Pan, Z.; Yin, Y.; Geng, S.; Sun, L.; Jiao, X. Oral and nasal DNA vaccines delivered by attenuated Salmonella enterica serovar Typhimurium induce a protective immune response against infectious bronchitis in chickens. Clin. Vaccine Immunol. CVI 2011, 18, 1041–1045. [Google Scholar] [CrossRef]
- Tan, L.; Wen, G.; Qiu, X.; Yuan, Y.; Meng, C.; Sun, Y.; Liao, Y.; Song, C.; Liu, W.; Shi, Y.; et al. A recombinant La Sota vaccine strain expressing multiple epitopes of infectious bronchitis virus (IBV) protects specific pathogen-free (SPF) chickens against IBV and NDV challenges. Vaccines 2019, 7, 170. [Google Scholar] [CrossRef]
- Ismail, Z.M.; El-Deeb, A.H.; El-Safty, M.M.; Hussein, H.A. Enhanced pathogenicity of low-pathogenic H9N2 avian influenza virus after vaccination with infectious bronchitis live attenuated vaccine. Vet. World 2018, 11, 977–985. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.S.H.; Ali, A.; Mahmoud, M.E.; Altakrouni, D.; Najimudeen, S.M.; Abdul-Careem, M.F. Protection of laying chickens against the Canadian DMV/1639 infectious bronchitis virus infection through priming with heterologous live vaccine and boosting with heterologous or homologous inactivated vaccine. Virus Res. 2023, 339, 199281. [Google Scholar] [CrossRef] [PubMed]
- Sepotokele, K.M.; O’Kennedy, M.M.; Hayes, M.C.; Wandrag, D.B.R.; Smith, P.; Abolnik, C. Efficacy of a plant-produced infectious bronchitis virus-like particle vaccine in specific pathogen-free chickens. Poult. Sci. 2023, 102, 102953. [Google Scholar] [CrossRef] [PubMed]
- Hajam, I.A.; Kim, J.; Lee, J.H. Oral immunization with a novel attenuated Salmonella Gallinarum encoding infectious bronchitis virus spike protein induces protective immune responses against fowl typhoid and infectious bronchitis in chickens. Vet. Res. 2018, 49, 91. [Google Scholar] [CrossRef] [PubMed]
- Wolff, J.A.; Malone, R.W.; Williams, P.; Chong, W.; Acsadi, G.; Jani, A.; Felgner, P.L. Direct gene transfer into mouse muscle in vivo. Science 1990, 247, 1465–1468. [Google Scholar] [CrossRef] [PubMed]
- Woodland, D.L. Jump-starting the immune system: Prime-boosting comes of age. Trends Immunol. 2004, 25, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Stirling, C.M.; Denyer, M.S.; Hamblin, P.; Hutchings, G.; Takamatsu, H.H.; Barnett, P.V. Dramatic improvement in FMD DNA vaccine efficacy and cross-serotype antibody induction in pigs following a protein boost. Vaccine 2008, 26, 2647–2656. [Google Scholar] [CrossRef] [PubMed]
- Ning, J.F.; Zhu, W.; Xu, J.P.; Zheng, C.Y.; Meng, X.L. Oral delivery of DNA vaccine encoding VP28 against white spot syndrome virus in crayfish by attenuated Salmonella typhimurium. Vaccine 2009, 27, 1127–1135. [Google Scholar] [CrossRef]
- Pan, Z.; Zhang, X.; Geng, S.; Cheng, N.; Sun, L.; Liu, B.; Huang, J.; Jiao, X. Priming with a DNA vaccine delivered by attenuated Salmonella typhimurium and boosting with a killed vaccine confers protection of chickens against infection with the H9 subtype of avian influenza virus. Vaccine 2009, 27, 1018–1023. [Google Scholar] [CrossRef]
- Ameiss, K.; Ashraf, S.; Kong, W.; Pekosz, A.; Wu, W.H.; Milich, D.; Billaud, J.N.; Curtiss, R., III. Delivery of woodchuck hepatitis virus-like particle presented influenza M2e by recombinant attenuated Salmonella displaying a delayed lysis phenotype. Vaccine 2010, 28, 6704–6713. [Google Scholar] [CrossRef]
- Galán, J.E.; Curtiss, R. Cloning and molecular characterization of genes whose products allow Salmonella typhimurium to penetrate tissue culture cells. Proc. Natl. Acad. Sci. USA 1989, 86, 6383–6387. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, S.; Kong, W.; Wang, S.; Yang, J.; Curtiss, R. Protective cellular responses elicited by vaccination with influenza nucleoprotein delivered by a live recombinant attenuated Salmonella vaccine. Vaccine 2011, 29, 3990–4002. [Google Scholar] [CrossRef] [PubMed]
- Kong, W. Development of antiviral vaccine utilizing self-destructing salmonella for antigen and DNA vaccine delivery. Methods Mol. Biol. 2021, 2225, 39–61. [Google Scholar] [CrossRef] [PubMed]
- Török, I.; Kari, C. Accumulation of ppGpp in a relA mutant of Escherichia coli during amino acid starvation. J. Biol. Chem. 1980, 255, 3838–3840. [Google Scholar] [CrossRef] [PubMed]
- De Groote, M.A.; Testerman, T.; Xu, Y.; Stauffer, G.; Fang, F.C. Homocysteine antagonism of nitric oxide-related cytostasis in Salmonella typhimurium. Science 1996, 272, 414–417. [Google Scholar] [CrossRef] [PubMed]
- Kong, W.; Wanda, S.Y.; Zhang, X.; Bollen, W.; Tinge, S.A.; Roland, K.L.; Curtiss, R., III. Regulated programmed lysis of recombinant Salmonella in host tissues to release protective antigens and confer biological containment. Proc. Natl. Acad. Sci. USA 2008, 105, 9361–9366. [Google Scholar] [CrossRef] [PubMed]
- Clark-Curtiss, J.E.; Curtiss, R. Salmonella vaccines: Conduits for protective antigens. J. Immunol. 2018, 200, 39–48. [Google Scholar] [CrossRef]
- Bandara, R.; Torrey, S.; Turner, P.V.; Zur Linden, A.; Schwean-Lardner, K.; Widowski, T.M. Efficacy of three different cervical dislocation methods for on-farm killing of layer chicks. Poult. Sci. 2023, 102, 102538. [Google Scholar] [CrossRef]
- Curtiss, R.; Hassan, J.O. Nonrecombinant and recombinant avirulent Salmonella vaccines for poultry. Vet. Immunol. Immunopathol. 1996, 54, 365–372. [Google Scholar] [CrossRef]
- Bertani, G. Studies on lysogenesis I. The mode of phage liberation by lysogenic Escherichia coli. J. Bacteriol. 1951, 62, 293–300. [Google Scholar] [CrossRef]
- Galán, J.E.; Nakayama, K.; Curtiss, R. Cloning and characterization of the asd gene of Salmonella typhimurium: Use in stable maintenance of recombinant plasmids in Salmonella vaccine strains. Gene 1990, 94, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Ruano, M.; El-Attrache, J.; Villegas, P. A rapid-plate hemagglutination assay for the detection of infectious bronchitis virus. Avian Dis. 2000, 44, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Munuswamy, P.; Ramakrishnan, S.; Latheef, S.K.; Kappala, D.; Mariappan, A.K.; Kaore, M.; Anbazhagan, K.; Puvvala, B.; Singh, K.P.; Dhama, K. First description of natural concomitant infection of avian nephritis virus and infectious bronchitis virus reveals exacerbated inflammatory response and renal damage in broiler chicks. Microb. Pathog. 2021, 154, 104830. [Google Scholar] [CrossRef] [PubMed]
- Guzman, L.M.; Belin, D.; Carson, M.J.; Beckwith, J. Tight regulation, modulation, and high-level expression by vectors containing the arabinose PBAD promoter. J. Bacteriol. 1995, 177, 4121–4130. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Gao, X.; Xu, K.; Wang, J.; Huang, H.; Shi, C.; Yang, W.; Kang, Y.; Curtiss, R., III; Yang, G.; et al. A novel cre recombinase-mediated minicircle DNA (CRIM) vaccine provides partial protection against newcastle disease virus. Appl. Environ. Microbiol. 2019, 85, e00407-19. [Google Scholar] [CrossRef]
- Darbyshire, J.H.; Peters, R.W. Humoral antibody response and assessment of protection following primary vaccination of chicks with maternally derived antibody against avian infectious bronchitis virus. Res. Vet. Sci. 1985, 38, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Chhabra, R.; Chantrey, J.; Ganapathy, K. Immune responses to virulent and vaccine strains of infectious bronchitis viruses in chickens. Viral Immunol. 2015, 28, 478–488. [Google Scholar] [CrossRef]
- Bande, F.; Arshad, S.S.; Bejo, M.H.; Omar, A.R.; Moeini, H.; Khadkodaei, S.; Wei, T.S.; Keong, Y.S.; Abba, Y.; Anka, I.A. Development and immunogenic potentials of chitosan-saponin encapsulated DNA vaccine against avian infectious bronchitis coronavirus. Microb. Pathog. 2020, 149, 104560. [Google Scholar] [CrossRef]
- Zhang, X.; Chen, T.; Chen, S.; Nie, Y.; Xie, Z.; Feng, K.; Zhang, H.; Xie, Q. The efficacy of a live attenuated TW I-type infectious bronchitis virus vaccine candidate. Virol. Sin. 2021, 36, 1431–1442. [Google Scholar] [CrossRef]
- Zuo, L.; Yan, W.; Song, Z.; Li, H.; Xie, X.; Gu, K.; Ma, P.; Tian, Y.; Zhou, C.; Zhao, Y.; et al. Design and characterization of a DNA vaccine based on spike with consensus nucleotide sequence against infectious bronchitis virus. Vaccines 2021, 9, 50. [Google Scholar] [CrossRef]
- Yang, T.; Wang, H.N.; Wang, X.; Tang, J.N.; Gao, R.; Li, J.; Guo, Z.C.; Li, Y.L. Multivalent DNA vaccine enhanced protection efficacy against infectious bronchitis virus in chickens. J. Vet. Med. Sci. 2009, 71, 1585–1590. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Wang, H.; Yang, T.; Wang, X.; Lu, D.; Li, Y.; Zhang, Y. Priming with a DNA vaccine and boosting with an inactivated vaccine enhance the immune response against infectious bronchitis virus. J. Virol. Methods 2010, 167, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekar, S.S.; Kingstad-Bakke, B.; Wu, C.W.; Suresh, M.; Talaat, A.M. A novel mucosal adjuvant system for immunization against avian coronavirus causing infectious bronchitis. J. Virol. 2020, 94, 1128. [Google Scholar] [CrossRef] [PubMed]
- Shao, L.; Zhao, J.; Li, L.; Huang, X.; Yang, H.; Cheng, J.; Liu, C.; Zhang, G. Pathogenic characteristics of a QX-like infectious bronchitis virus strain SD in chickens exposed at different ages and protective efficacy of combining live homologous and heterologous vaccination. Vet. Res. 2020, 51, 86. [Google Scholar] [CrossRef] [PubMed]
- Buharideen, S.M.; Hassan, M.S.H.; Najimudeen, S.M.; Niu, D.; Czub, M.; Gomis, S.; Abdul-Careem, M.F. Immune responses in laying hens after an infectious bronchitis vaccination of pullets: A comparison of two vaccination strategies. Vaccines 2021, 9, 531. [Google Scholar] [CrossRef] [PubMed]
- Vacik, J.; Dean, B.S.; Zimmer, W.E.; Dean, D.A. Cell-specific nuclear import of plasmid DNA. Gene Ther. 1999, 6, 1006–1014. [Google Scholar] [CrossRef]
- Kong, W.; Brovold, M.; Koeneman, B.A.; Clark-Curtiss, J.; Curtiss, R. Turning self-destructing Salmonella into a universal DNA vaccine delivery platform. Proc. Natl. Acad. Sci. USA 2012, 109, 19414–19419. [Google Scholar] [CrossRef]
- Brumell, J.H.; Tang, P.; Zaharik, M.L.; Finlay, B.B. Disruption of the Salmonella-containing vacuole leads to increased replication of Salmonella enterica serovar typhimurium in the cytosol of epithelial cells. Infect. Immun. 2002, 70, 3264–3270. [Google Scholar] [CrossRef]
- O’Garra, A.; Arai, N. The molecular basis of T helper 1 and T helper 2 cell differentiation. Trends Cell Biol. 2000, 10, 542–550. [Google Scholar] [CrossRef]
- Spellberg, B.; Edwards, J.E. Type 1/Type 2 immunity in infectious diseases. Clin. Infect. Dis. 2001, 32, 76–102. [Google Scholar] [CrossRef]
- Raj, G.D.; Jones, R.C. Cross-reactive cellular immune responses in chickens vaccinated with live infectious bronchitis virus vaccine. Avian Pathol. 1997, 26, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.Y.; Yao, B.Y.; Hu, C.J.; Chen, H.W. Induction of robust immune responses by CpG-ODN-loaded hollow polymeric nanoparticles for antiviral and vaccine applications in chickens. Int. J. Nanomed. 2020, 15, 3303–3318. [Google Scholar] [CrossRef] [PubMed]
- Manswr, B.; Ball, C.; Forrester, A.; Chantrey, J.; Ganapathy, K. Host immune response to infectious bronchitis virus Q1 in two commercial broiler chicken lines. Res. Vet. Sci. 2021, 136, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Quinteros, J.A.; Noormohammadi, A.H.; Lee, S.W.; Browning, G.F.; Diaz-Méndez, A. Genomics and pathogenesis of the avian coronavirus infectious bronchitis virus. Aust. Vet. J. 2022, 100, 496–512. [Google Scholar] [CrossRef]
- Raggi, L.G.; Lee, G.G. Lack of correlation between infectivity, serologic response and challenge results in immunization with an avian infectious bronchitis vaccine. J. Immunol. 1965, 94, 538–543. [Google Scholar] [CrossRef]

| Strains, Plasmid, or Primer | Characteristics | Sources or References |
|---|---|---|
| E. coli. strains | ||
| BL21 (DE3) | For expression of the recombinant plasmids | Invitrogen |
| χ7213 | thi 1 thr 1 leuB6 fhuA21 lacY1 glnV44 asdA4 recA1 RP4 2 Tc:: Mu[λ pir]ΔasdA4 (Δzhf-2::Tn10) | [22] |
| S. enterica serovar Typhimurium UK-1 strains | ||
| χ11246 | ΔasdA::TT araC PBADc2 ΔaraBAD Δ(gmd-fcl) Δpmi ΔrelA::araC PBADlacI, TT ΔPmurA::TT araC PBADmurA ΔsifA | [23] |
| Plasmids | ||
| pYA4545 | pUC ori araC PBAD SD-GTG murA SD-GTG asdA P22 PR antisense mRNA eukaryotic expression cassette of with DTS (I), DTS (II), and SV 40 polyA | [23] |
| pET28a | Expression vector | Novage |
| PMD-19T | Cloning vector; Ampr | TaKaRa |
| pET28a-S1 | A recombinant expression vector containing S1; Kanr | This study |
| pYA4545-S1 | pYA4545 with s1 gene | This study |
| Primers | Sequences (5′–3′) | Product Size (bp) | Function |
|---|---|---|---|
| S1-P1 | CGGGGTACCATGTTGGGCAAACCGCTTTTACT | 1620 | Cloning of plasmid pYA4545-S1 |
| S1-P2 | TAAAATAACCTCTTGTGCGGTTCCATTAATAAAGTAGGCTAGGGCTT | ||
| S1-P3 | AAGCCCTAGCCTACTTTATTAATGGAACCGCACAAGAGGTTATTTTA | ||
| S1-P4 | CCGCTCGAGAGAACGTCTAGAGCGACGTGTTCCGTT | ||
| S1-F1 | ATGGGTCGCGGATCCGAATTCTTTACTACTACCAAAGTGCCTTTAGGC | 909 | Cloning of plasmid pET28a-S1 |
| S1-R1 | GTGGTGGTGGTGGTGCTCGAGTGGGTGGTATGACCCATACATAAA | ||
| ΔsifA-F1 | TGATGAGCTCTTTCTCTTCTCCAAAATCTC | 850 | |
| ΔsifA-R1 | CTTAGGTACCGGTCGATTTAATCAATTATG | ||
| sifA-F | CTCTTCTCCAAAATCTCTCCAAA | 1683 | |
| sifA-R | CATTACGCTGACCATTGTGA | ||
| β-Actin | F: TATGTGCAAGGCCGGTTTC R: TGTCTTTCTGGCCCATACCAA | 110 | |
| IFN-γ | F: TGAGCCAGATTGTTTCGATG R: CTTGGCCAGGTCCATGATA | 152 | |
| IL-6 | F: CAAGAAGTTCACCGTGTGCGAGA R: ATTCCAGGTAGGTCTGAAAGGCG | 254 | |
| IL-12 | F: CGAAGTGAAGGAGTTCCCAGAT R: GACCGTATCATTTGCCCATTG | 123 |
| Groups | Sample Type | No. of Affected a | Protection Rate (%) c | ||
|---|---|---|---|---|---|
| 1 b | 2 b | 3 b | |||
| Blank control | Lacrimal gland | 0/6 | 0/6 | 0/6 | / |
| Trachea | 0/6 | 0/6 | 0/6 | ||
| Cloaca | 0/6 | 0/6 | 0/6 | ||
| Virus-challenged control | Lacrimal gland | 6/6 | 5/6 | 6/6 | / |
| Trachea | 6/6 | 6/6 | 5/6 | ||
| Cloaca | 6/6 | 6/6 | 5/6 | ||
| χ11246(pYA4545) | Lacrimal gland | 6/6 | 6/6 | 5/6 | 6% |
| Trachea | 6/6 | 5/6 | 5/6 | 11% | |
| Cloaca | 5/6 | 6/6 | 6/6 | 6% | |
| χ11246(pYA4545-S1) | Lacrimal gland | 2/6 | 1/6 | 2/6 | 72% |
| Trachea | 3/6 | 2/6 | 3/6 | 56% | |
| Cloaca | 3/6 | 3/6 | 2/6 | 56% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, K.; Li, Z.; Li, Q.; Wang, S.; Curtiss, R., III; Shi, H. Salmonella typhimurium Vaccine Candidate Delivering Infectious Bronchitis Virus S1 Protein to Induce Protection. Biomolecules 2024, 14, 133. https://doi.org/10.3390/biom14010133
Liu K, Li Z, Li Q, Wang S, Curtiss R III, Shi H. Salmonella typhimurium Vaccine Candidate Delivering Infectious Bronchitis Virus S1 Protein to Induce Protection. Biomolecules. 2024; 14(1):133. https://doi.org/10.3390/biom14010133
Chicago/Turabian StyleLiu, Kaihui, Zewei Li, Quan Li, Shifeng Wang, Roy Curtiss, III, and Huoying Shi. 2024. "Salmonella typhimurium Vaccine Candidate Delivering Infectious Bronchitis Virus S1 Protein to Induce Protection" Biomolecules 14, no. 1: 133. https://doi.org/10.3390/biom14010133
APA StyleLiu, K., Li, Z., Li, Q., Wang, S., Curtiss, R., III, & Shi, H. (2024). Salmonella typhimurium Vaccine Candidate Delivering Infectious Bronchitis Virus S1 Protein to Induce Protection. Biomolecules, 14(1), 133. https://doi.org/10.3390/biom14010133







