Exploratory Review of the Takotsubo Syndrome and the Possible Role of the Psychosocial Stress Response and Inflammaging
Abstract
:1. Introduction
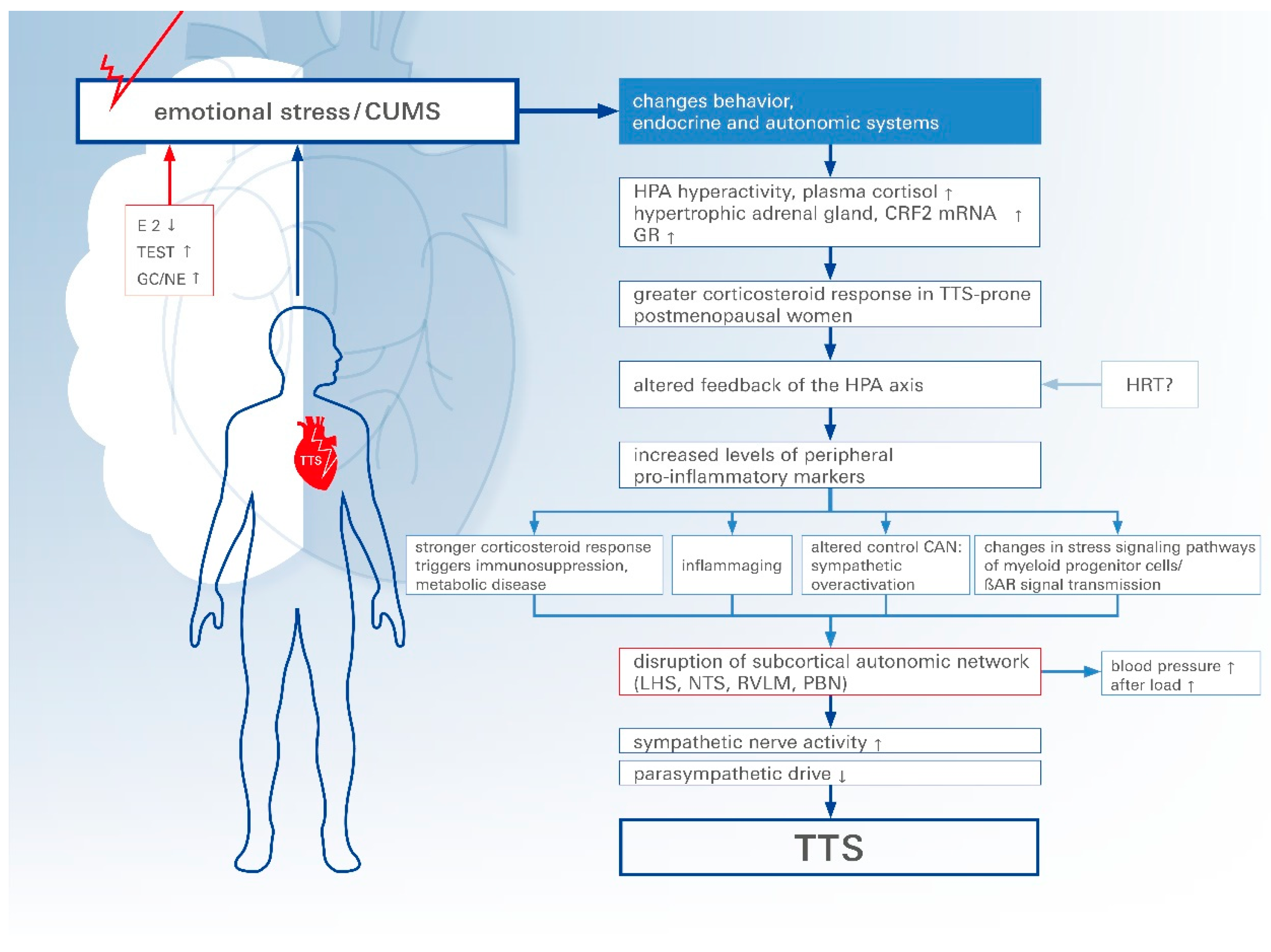
2. Brain-Heart Interaction/Axis
3. Pathophysiology (Physical and Emotional Triggers)
4. Triggers
5. Emotional Stressors
6. Physical Stressors
7. Gender Differences in TTS
8. How Does Estrogen Concentration Affect Postmenopausal Women?
9. Sympathetic Nervous System
10. Inflammaging
11. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| TTS | takotsubo syndrome |
| ACS | acute coronary syndrome |
| LVWMA | left ventricular wall motion abnormality |
| ECG | electrocardiogram |
| CMR | cardiac magnetic resonance |
| STEMI | ST-elevation myocardial infarction |
| tVNS | transcutaneous vagus nerve stimulation |
| VN | vagus nerve |
| Ic | insular cortex |
| CAN | central autonomic nervous system |
| fMRI | functional magnetic resonance imaging |
| ANS | autonomic nervous system |
| LC | locus coeruleus |
| PVH | paraventricular nucleus of the hypothalamus |
| HPA | hypothalamic-pituitary-adrenal |
| CRF | corticotropin-releasing factor |
| ACTH | adrenocorticotropin hormone |
| GC | glucocorticoid |
| NE | norepinephrine |
| CUMS | chronic unpredictable mild stress |
| GR | glucocorticoid-receptor |
| OVX | ovariectomized |
| E2 | estradiol |
| P | progesterone |
| LH | luteinizing hormone |
| FSH | follicle-stimulating hormone |
| MI | myocardial infarction |
| MESA | Multi-Ethnic Study of Atherosclerosis |
| HFrEF | heart failure with reduced ejection fraction |
| Erα/β | estrogen receptor alpha/beta |
| NO | nitric oxide |
| SNS | sympathetic nervous system |
| β-AR | β-adrenergic receptor |
| IL | interleukin |
| TNF | tumor necrosis factor |
| CRP | C-reactive protein |
| DNA | deoxyribonucleic acid |
| HRT | hormone replacement therapy |
| LHS | limbic-hypothalamic system |
| NTS | nucleus tractus solitarii |
| RVLM | rostral ventrolateral medulla |
| PBN | parabigeminal nucleus |
References
- Ghadri, J.R.; Wittstein, I.S.; Prasad, A.; Sharkey, S.; Dote, K.; Akashi, Y.J.; Cammann, V.L.; Crea, F.; Galiuto, L.; Desmet, W.; et al. International Expert Consensus Document on Takotsubo Syndrome (Part I): Clinical Characteristics, Diagnostic Criteria, and Pathophysiology. Eur. Heart J. 2018, 39, 2032–2046. [Google Scholar] [CrossRef]
- Sharkey, S.W.; Lesser, J.R.; Maron, M.S.; Maron, B.J. Why not just call it tako-tsubo cardiomyopathy: A discussion of nomenclature. J. Am. Coll. Cardiol. 2011, 57, 1496–1497. [Google Scholar] [CrossRef]
- Song, B.G.; Yang, H.S.; Hwang, H.K.; Kang, G.H.; Park, Y.H.; Chun, W.J.; Oh, J.H. The impact of stressor patterns on clinical features in patients with tako-tsubo cardiomyopathy: Experiences of two tertiary cardiovascular centers. Clin. Cardiol. 2012, 35, E6–E13. [Google Scholar] [CrossRef]
- Jung, J.M.; Kim, J.G.; Kim, J.B.; Cho, K.H.; Yu, S.; Oh, K.; Kim, Y.H.; Choi, J.Y.; Seo, W.K. Takotsubo-Like Myocardial Dysfunction in Ischemic Stroke: A Hospital-Based Registry and Systematic Literature Review. Stroke 2016, 47, 2729–2736. [Google Scholar] [CrossRef]
- Stöllberger, C.; Wegner, C.; Finsterer, J. Seizure-associated Takotsubo cardiomyopathy. Epilepsia 2011, 52, e160–e167. [Google Scholar] [CrossRef]
- Lyon, A.R.; Bossone, E.; Schneider, B.; Sechtem, U.; Citro, R.; Underwood, S.R.; Sheppard, M.N.; Figtree, G.A.; Parodi, G.; Akashi, Y.J.; et al. Current state of knowledge on Takotsubo syndrome: A Position Statement from the Taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2016, 18, 8–27. [Google Scholar] [CrossRef]
- Elgendy, A.Y.; Elgendy, I.Y.; Mansoor, H.; Mahmoud, A.N. Clinical presentations and outcomes of Takotsubo syndrome in the setting of subarachnoid hemorrhage: A systematic review and meta-analysis. Eur. Heart J. Acute Cardiovasc. Care 2018, 7, 236–245. [Google Scholar] [CrossRef]
- Eitel, I.; von Knobelsdorff-Brenkenhoff, F.; Bernhardt, P.; Carbone, I.; Muellerleile, K.; Aldrovandi, A.; Francone, M.; Desch, S.; Gutberlet, M.; Strohm, O.; et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA 2011, 306, 277–286. [Google Scholar] [CrossRef]
- Templin, C.; Ghadri, J.R.; Diekmann, J.; Napp, L.C.; Bataiosu, D.R.; Jaguszewski, M.; Cammann, V.L.; Sarcon, A.; Geyer, V.; Neumann, C.A.; et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N. Engl. J. Med. 2015, 373, 929–938. [Google Scholar] [CrossRef]
- Ghadri, J.R.; Cammann, V.L.; Napp, L.C.; Jurisic, S.; Diekmann, J.; Bataiosu, D.R.; Seifert, B.; Jaguszewski, M.; Sarcon, A.; Neumann, C.A.; et al. Differences in the Clinical Profile and Outcomes of Typical and Atypical Takotsubo Syndrome: Data From the International Takotsubo Registry. JAMA Cardiol. 2016, 1, 335–340. [Google Scholar] [CrossRef]
- Couch, L.S.; Fiedler, J.; Chick, G.; Clayton, R.; Dries, E.; Wienecke, L.M.; Fu, L.; Fourre, J.; Pandey, P.; Derda, A.A.; et al. Circulating microRNAs predispose to takotsubo syndrome following high-dose adrenaline exposure. Cardiovasc. Res. 2022, 118, 1758–1770. [Google Scholar] [CrossRef] [PubMed]
- Jaguszewski, M.; Osipova, J.; Ghadri, J.R.; Napp, L.C.; Widera, C.; Franke, J.; Fijalkowski, M.; Nowak, R.; Fijalkowska, M.; Volkmann, I.; et al. A signature of circulating microRNAs differentiates takotsubo cardiomyopathy from acute myocardial infarction. Eur. Heart J. 2014, 35, 999–1006. [Google Scholar] [CrossRef]
- Nagai, M.; Shityakov, S.; Smetak, M.; Hunkler, H.J.; Bär, C.; Schlegel, N.; Thum, T.; Förster, C.Y. Blood Biomarkers in Takotsubo Syndrome Point to an Emerging Role for Inflammaging in Endothelial Pathophysiology. Biomolecules 2023, 13, 995. [Google Scholar] [CrossRef]
- Frank, N.; Nagai, M.; Förster, C. Exploration of transcutaneous vagus nerve stimulation as a treatment option for adjuvant cancer and heart failure therapy. Explor. Neuroprotective Ther. 2023, 3, 363–397. [Google Scholar] [CrossRef]
- Ittner, C.; Burek, M.; Stork, S.; Nagai, M.; Forster, C.Y. Increased Catecholamine Levels and Inflammatory Mediators Alter Barrier Properties of Brain Microvascular Endothelial Cells in vitro. Front. Cardiovasc. Med. 2020, 7, 73. [Google Scholar] [CrossRef]
- Nagai, M.; Dote, K.; Kato, M.; Sasaki, S.; Oda, N.; Kagawa, E.; Nakano, Y.; Yamane, A.; Higashihara, T.; Miyauchi, S.; et al. The Insular Cortex and Takotsubo Cardiomyopathy. Curr. Pharm. Des. 2017, 23, 879–888. [Google Scholar] [CrossRef]
- Nagai, M.; Kishi, K.; Kato, S. Insular cortex and neuropsychiatric disorders: A review of recent literature. Eur. Psychiatry 2007, 22, 387–394. [Google Scholar] [CrossRef]
- George, M.S.; Ketter, T.A.; Parekh, P.I.; Horwitz, B.; Herscovitch, P.; Post, R.M. Brain activity during transient sadness and happiness in healthy women. Am. J. Psychiatry 1995, 152, 341–351. [Google Scholar]
- Reiman, E.M.; Lane, R.D.; Ahern, G.L.; Schwartz, G.E.; Davidson, R.J.; Friston, K.J.; Yun, L.S.; Chen, K. Neuroanatomical correlates of externally and internally generated human emotion. Am. J. Psychiatry 1997, 154, 918–925. [Google Scholar]
- Damasio, A.R.; Grabowski, T.J.; Bechara, A.; Damasio, H.; Ponto, L.L.; Parvizi, J.; Hichwa, R.D. Subcortical and cortical brain activity during the feeling of self-generated emotions. Nat. Neurosci. 2000, 3, 1049–1056. [Google Scholar] [CrossRef]
- Gu, X.; Hof, P.R.; Friston, K.J.; Fan, J. Anterior insular cortex and emotional awareness. J. Comp. Neurol. 2013, 521, 3371–3388. [Google Scholar] [CrossRef]
- Ulrich-Lai, Y.M.; Herman, J.P. Neural regulation of endocrine and autonomic stress responses. Nat. Rev. Neurosci. 2009, 10, 397–409. [Google Scholar] [CrossRef]
- Templin, C.; Hänggi, J.; Klein, C.; Topka, M.S.; Hiestand, T.; Levinson, R.A.; Jurisic, S.; Lüscher, T.F.; Ghadri, J.R.; Jäncke, L. Altered limbic and autonomic processing supports brain-heart axis in Takotsubo syndrome. Eur. Heart J. 2019, 40, 1183–1187. [Google Scholar] [CrossRef]
- Béjean, S.; Sultan-Taïeb, H. Modeling the economic burden of diseases imputable to stress at work. Eur. J. Health Econ. 2005, 6, 16–23. [Google Scholar] [CrossRef]
- de Kloet, E.R.; Joëls, M.; Holsboer, F. Stress and the brain: From adaptation to disease. Nat. Rev. Neurosci. 2005, 6, 463–475. [Google Scholar] [CrossRef]
- Romier, C.; Bernassau, J.M.; Cambillau, C.; Darbon, H. Solution structure of human corticotropin releasing factor by 1H NMR and distance geometry with restrained molecular dynamics. Protein Eng. 1993, 6, 149–156. [Google Scholar] [CrossRef]
- Trainer, P.J.; Faria, M.; Newell-Price, J.; Browne, P.; Kopelman, P.; Coy, D.H.; Besser, G.M.; Grossman, A.B. A comparison of the effects of human and ovine corticotropin-releasing hormone on the pituitary-adrenal axis. J. Clin. Endocrinol. Metab. 1995, 80, 412–417. [Google Scholar]
- Hillhouse, E.W.; Grammatopoulos, D.K. The molecular mechanisms underlying the regulation of the biological activity of corticotropin-releasing hormone receptors: Implications for physiology and pathophysiology. Endocr. Rev. 2006, 27, 260–286. [Google Scholar] [CrossRef]
- Henckens, M.J.; Deussing, J.M.; Chen, A. Region-specific roles of the corticotropin-releasing factor-urocortin system in stress. Nat. Rev. Neurosci. 2016, 17, 636–651. [Google Scholar] [CrossRef]
- Carrasco, G.A.; Van de Kar, L.D. Neuroendocrine pharmacology of stress. Eur. J. Pharmacol. 2003, 463, 235–272. [Google Scholar] [CrossRef]
- McEwen, B.S.; Sapolsky, R.M. Stress and cognitive function. Curr. Opin. Neurobiol. 1995, 5, 205–216. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Protective and damaging effects of stress mediators. N. Engl. J. Med. 1998, 338, 171–179. [Google Scholar] [CrossRef] [PubMed]
- De Kloet, E.R.; Derijk, R. Signaling pathways in brain involved in predisposition and pathogenesis of stress-related disease: Genetic and kinetic factors affecting the MR/GR balance. Ann. N. Y. Acad. Sci. 2004, 1032, 14–34. [Google Scholar] [CrossRef]
- Joëls, M.; Karst, H.; Alfarez, D.; Heine, V.M.; Qin, Y.; Riel, E.V.; Verkuyl, M.; Lucassen, P.J.; Krugers, H.J. Effects of chronic stress on structure and cell function in rat hippocampus and hypothalamus. Stress 2004, 7, 221–231. [Google Scholar] [CrossRef] [PubMed]
- Willner, P. Chronic mild stress (CMS) revisited: Consistency and behavioural-neurobiological concordance in the effects of CMS. Neuropsychobiology 2005, 52, 90–110. [Google Scholar] [CrossRef] [PubMed]
- Malta, M.B.; Martins, J.; Novaes, L.S.; Dos Santos, N.B.; Sita, L.; Camarini, R.; Scavone, C.; Bittencourt, J.; Munhoz, C.D. Norepinephrine and Glucocorticoids Modulate Chronic Unpredictable Stress-Induced Increase in the Type 2 CRF and Glucocorticoid Receptors in Brain Structures Related to the HPA Axis Activation. Mol. Neurobiol. 2021, 58, 4871–4885. [Google Scholar] [CrossRef] [PubMed]
- Allen, A.P.; Kennedy, P.J.; Cryan, J.F.; Dinan, T.G.; Clarke, G. Biological and psychological markers of stress in humans: Focus on the Trier Social Stress Test. Neurosci. Biobehav. Rev. 2014, 38, 94–124. [Google Scholar] [CrossRef]
- Wallström, S.; Ulin, K.; Määttä, S.; Omerovic, E.; Ekman, I. Impact of long-term stress in Takotsubo syndrome: Experience of patients. Eur. J. Cardiovasc. Nurs. 2016, 15, 522–528. [Google Scholar] [CrossRef]
- Chan, C.; Elliott, J.; Troughton, R.; Frampton, C.; Smyth, D.; Crozier, I.; Bridgman, P. Acute myocardial infarction and stress cardiomyopathy following the Christchurch earthquakes. PLoS ONE 2013, 8, e68504. [Google Scholar] [CrossRef]
- Sharkey, S.W.; Windenburg, D.C.; Lesser, J.R.; Maron, M.S.; Hauser, R.G.; Lesser, J.N.; Haas, T.S.; Hodges, J.S.; Maron, B.J. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J. Am. Coll. Cardiol. 2010, 55, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Tagawa, M.; Nakamura, Y.; Ishiguro, M.; Satoh, K.; Chinushi, M.; Kodama, M.; Aizawa, Y. Transient left ventricular apical ballooning developing after the Central Niigata Prefecture Earthquake: Two case reports. J. Cardiol. 2006, 48, 153–158. [Google Scholar] [PubMed]
- Ghadri, J.R.; Sarcon, A.; Diekmann, J.; Bataiosu, D.R.; Cammann, V.L.; Jurisic, S.; Napp, L.C.; Jaguszewski, M.; Scherff, F.; Brugger, P.; et al. Happy heart syndrome: Role of positive emotional stress in takotsubo syndrome. Eur. Heart J. 2016, 37, 2823–2829. [Google Scholar] [CrossRef]
- Scheitz, J.F.; Mochmann, H.C.; Witzenbichler, B.; Fiebach, J.B.; Audebert, H.J.; Nolte, C.H. Takotsubo cardiomyopathy following ischemic stroke: A cause of troponin elevation. J. Neurol. 2012, 259, 188–190. [Google Scholar] [CrossRef]
- Modi, S.; Baig, W. Radiotherapy-induced Tako-tsubo cardiomyopathy. Clin. Oncol. 2009, 21, 361–362. [Google Scholar] [CrossRef] [PubMed]
- Y-Hassan, S.; Settergren, M.; Henareh, L. Sepsis-induced myocardial depression and takotsubo syndrome. Acute Card. Care 2014, 16, 102–109. [Google Scholar] [CrossRef]
- Brezina, P.; Isler, C.M. Takotsubo cardiomyopathy in pregnancy. Obstet. Gynecol. 2008, 112 Pt 2, 450–452. [Google Scholar] [CrossRef]
- Riera, M.; Llompart-Pou, J.A.; Carrillo, A.; Blanco, C. Head injury and inverted Takotsubo cardiomyopathy. J. Trauma Acute Care Surg. 2010, 68, E13–E15. [Google Scholar] [CrossRef] [PubMed]
- Hjalmarsson, C.; Oras, J.; Redfors, B. A case of intracerebral hemorrhage and apical ballooning: An important differential diagnosis in ST-segment elevation. Int. J. Cardiol. 2015, 186, 90–92. [Google Scholar] [CrossRef]
- Murakami, T.; Yoshikawa, T.; Maekawa, Y.; Ueda, T.; Isogai, T.; Sakata, K.; Nagao, K.; Yamamoto, T.; Takayama, M. Gender Differences in Patients with Takotsubo Cardiomyopathy: Multi-Center Registry from Tokyo CCU Network. PLoS ONE 2015, 10, e0136655. [Google Scholar] [CrossRef]
- Krishnamoorthy, P.; Garg, J.; Sharma, A.; Palaniswamy, C.; Shah, N.; Lanier, G.; Patel, N.C.; Lavie, C.J.; Ahmad, H. Gender Differences and Predictors of Mortality in Takotsubo Cardiomyopathy: Analysis from the National Inpatient Sample 2009–2010 Database. Cardiology 2015, 132, 131–136. [Google Scholar] [CrossRef]
- Yoshizawa, M.; Itoh, T.; Morino, Y.; Taniai, S.; Ishibashi, Y.; Komatsu, T.; Taguchi, I.; Nishinari, M.; Ako, J.; Kyono, H.; et al. Gender Differences in the Circadian and Seasonal Variations in Patients with Takotsubo Syndrome: A Multicenter Registry at Eight University Hospitals in East Japan. Intern. Med. 2021, 60, 2749–2755. [Google Scholar] [CrossRef]
- Angelini, P.; Tobis, J.M. Is high-dose catecholamine administration in small animals an appropriate model for takotsubo syndrome? Circ. J. 2015, 79, 897. [Google Scholar] [CrossRef]
- Duma, D.; Collins, J.B.; Chou, J.W.; Cidlowski, J.A. Sexually dimorphic actions of glucocorticoids provide a link to inflammatory diseases with gender differences in prevalence. Sci. Signal. 2010, 3, ra74. [Google Scholar] [CrossRef]
- Lindheim, S.R.; Legro, R.S.; Bernstein, L.; Stanczyk, F.Z.; Vijod, M.A.; Presser, S.C.; Lobo, R.A. Behavioral stress responses in premenopausal and postmenopausal women and the effects of estrogen. Am. J. Obstet. Gynecol. 1992, 167, 1831–1836. [Google Scholar] [CrossRef]
- Kudielka, B.M.; Schmidt-Reinwald, A.K.; Hellhammer, D.H.; Kirschbaum, C. Psychological and endocrine responses to psychosocial stress and dexamethasone/corticotropin-releasing hormone in healthy postmenopausal women and young controls: The impact of age and a two-week estradiol treatment. Neuroendocrinology 1999, 70, 422–430. [Google Scholar] [CrossRef]
- Ueyama, T.; Hano, T.; Kasamatsu, K.; Yamamoto, K.; Tsuruo, Y.; Nishio, I. Estrogen attenuates the emotional stress-induced cardiac responses in the animal model of Tako-tsubo (Ampulla) cardiomyopathy. J. Cardiovasc. Pharmacol. 2003, 42 (Suppl. 1), S117–S120. [Google Scholar] [CrossRef] [PubMed]
- Ueyama, T.; Ishikura, F.; Matsuda, A.; Asanuma, T.; Ueda, K.; Ichinose, M.; Kasamatsu, K.; Hano, T.; Akasaka, T.; Tsuruo, Y.; et al. Chronic estrogen supplementation following ovariectomy improves the emotional stress-induced cardiovascular responses by indirect action on the nervous system and by direct action on the heart. Circ. J. 2007, 71, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Rivera, C.M.; Grossardt, B.R.; Rhodes, D.J.; Brown, R.D., Jr.; Roger, V.L.; Melton, L.J., 3rd. Increased cardiovascular mortality after early bilateral oophorectomy. Menopause 2009, 16, 15–23. [Google Scholar] [CrossRef]
- Brenner, R.; Weilenmann, D.; Maeder, M.T.; Jörg, L.; Bluzaite, I.; Rickli, H.; De Pasquale, G.; Ammann, P. Clinical characteristics, sex hormones, and long-term follow-up in Swiss postmenopausal women presenting with Takotsubo cardiomyopathy. Clin. Cardiol. 2012, 35, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Guallar, E.; Ouyang, P.; Subramanya, V.; Vaidya, D.; Ndumele, C.E.; Lima, J.A.; Allison, M.A.; Shah, S.J.; Bertoni, A.G.; et al. Endogenous Sex Hormones and Incident Cardiovascular Disease in Post-Menopausal Women. J. Am. Coll. Cardiol. 2018, 71, 2555–2566. [Google Scholar] [CrossRef]
- Barros, R.P.; Machado, U.F.; Gustafsson, J.A. Estrogen receptors: New players in diabetes mellitus. Trends Mol. Med. 2006, 12, 425–431. [Google Scholar] [CrossRef]
- Zhu, Y.; Bian, Z.; Lu, P.; Karas, R.H.; Bao, L.; Cox, D.; Hodgin, J.; Shaul, P.W.; Thorén, P.; Smithies, O.; et al. Abnormal vascular function and hypertension in mice deficient in estrogen receptor β. Science 2002, 295, 505–508. [Google Scholar] [CrossRef]
- Komesaroff, P.A.; Esler, M.D.; Sudhir, K. Estrogen supplementation attenuates glucocorticoid and catecholamine responses to mental stress in perimenopausal women. J. Clin. Endocrinol. Metab. 1999, 84, 606–610. [Google Scholar] [CrossRef]
- Sung, B.H.; Ching, M.; Izzo, J.L., Jr.; Dandona, P.; Wilson, M.F. Estrogen improves abnormal norepinephrine-induced vasoconstriction in postmenopausal women. J. Hypertens. 1999, 17, 523–528. [Google Scholar] [CrossRef]
- Sader, M.A.; Celermajer, D.S. Endothelial function, vascular reactivity and gender differences in the cardiovascular system. Cardiovasc. Res. 2002, 53, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Förster, C.; Kietz, S.; Hultenby, K.; Warner, M.; Gustafsson, J.A. Characterization of the ERβ−/−mouse heart. Proc. Natl. Acad. Sci. USA 2004, 101, 14234–14239. [Google Scholar] [CrossRef] [PubMed]
- Dimberg, U.; Petterson, M. Facial reactions to happy and angry facial expressions: Evidence for right hemisphere dominance. Psychophysiology 2000, 37, 693–696. [Google Scholar] [CrossRef] [PubMed]
- Drača, S. A possible relationship between Takotsubo cardiomyopathy and female sex steroid-related modulation of functional cerebral asymmetry. Med. Hypotheses 2015, 84, 238–240. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Carson, K.; Shah, R.; Sawhney, G.; Singh, B.; Parsaik, A.; Gilutz, H.; Usmani, Z.; Horowitz, J. Meta-analysis of clinical correlates of acute mortality in takotsubo cardiomyopathy. Am. J. Cardiol. 2014, 113, 1420–1428. [Google Scholar] [CrossRef]
- Pelliccia, F.; Parodi, G.; Greco, C.; Antoniucci, D.; Brenner, R.; Bossone, E.; Cacciotti, L.; Capucci, A.; Citro, R.; Delmas, C.; et al. Comorbidities frequency in Takotsubo syndrome: An international collaborative systematic review including 1109 patients. Am. J. Med. 2015, 128, 654.e11–654.e19. [Google Scholar] [CrossRef]
- Pelliccia, F.; Sinagra, G.; Elliott, P.; Parodi, G.; Basso, C.; Camici, P.G. Takotsubo: One, no one and one hundred thousand diseases. Int. J. Cardiol. 2018, 261, 35. [Google Scholar] [CrossRef] [PubMed]
- Jänig, W. The Integrative Action of the Autonomic Nervous System: Neurobiology of Homeostasis; Cambridge University Press: Cambridge, UK, 2006. [Google Scholar]
- Li, Y.; Jiang, W.; Li, Z.Z.; Zhang, C.; Huang, C.; Yang, J.; Kong, G.Y.; Li, Z.F. Repetitive restraint stress changes spleen immune cell subsets through glucocorticoid receptor or β-adrenergic receptor in a stage dependent manner. Biochem. Biophys. Res. Commun. 2018, 495, 1108–1114. [Google Scholar] [CrossRef] [PubMed]
- Duma, D.; Jewell, C.M.; Cidlowski, J.A. Multiple glucocorticoid receptor isoforms and mechanisms of post-translational modification. J. Steroid Biochem. Mol. Biol. 2006, 102, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Rhen, T.; Cidlowski, J.A. Antiinflammatory action of glucocorticoids--new mechanisms for old drugs. N. Engl. J. Med. 2005, 353, 1711–1723. [Google Scholar] [CrossRef]
- Nagai, M.; Förster, C.Y.; Dote, K. Sex Hormone-Specific Neuroanatomy of Takotsubo Syndrome: Is the Insular Cortex a Moderator? Biomolecules 2022, 12, 110. [Google Scholar] [CrossRef]
- Walsh, C.P.; Bovbjerg, D.H.; Marsland, A.L. Glucocorticoid resistance and β2-adrenergic receptor signaling pathways promote peripheral pro-inflammatory conditions associated with chronic psychological stress: A systematic review across species. Neurosci. Biobehav. Rev. 2021, 128, 117–135. [Google Scholar] [CrossRef]
- Walsh, C.P.; Ewing, L.J.; Cleary, J.L.; Vaisleib, A.D.; Farrell, C.H.; Wright, A.G.; Gray, K.; Marsland, A.L. Development of glucocorticoid resistance over one year among mothers of children newly diagnosed with cancer. Brain Behav. Immun. 2018, 69, 364–373. [Google Scholar] [CrossRef]
- Capitanio, J.P.; Mendoza, S.P.; Lerche, N.W.; Mason, W.A. Social stress results in altered glucocorticoid regulation and shorter survival in simian acquired immune deficiency syndrome. Proc. Natl. Acad. Sci. USA 1998, 95, 4714–4719. [Google Scholar] [CrossRef]
- Cole, S.W.; Mendoza, S.P.; Capitanio, J.P. Social stress desensitizes lymphocytes to regulation by endogenous glucocorticoids: Insights from in vivo cell trafficking dynamics in rhesus macaques. Psychosom. Med. 2009, 71, 591–597. [Google Scholar] [CrossRef]
- Cole, S.W.; Capitanio, J.P.; Chun, K.; Arevalo, J.M.; Ma, J.; Cacioppo, J.T. Myeloid differentiation architecture of leukocyte transcriptome dynamics in perceived social isolation. Proc. Natl. Acad. Sci. USA 2015, 112, 15142–15147. [Google Scholar] [CrossRef]
- Oakley, R.H.; Cidlowski, J.A. The biology of the glucocorticoid receptor: New signaling mechanisms in health and disease. J. Allergy Clin. Immunol. 2013, 132, 1033–1044. [Google Scholar] [CrossRef]
- Ramírez, C.G.; Queijeiro, A.V.; Morales, S.J.; López, D.B.; Miranda, A.H.; Chow, A.R.; Cárdenas, L.T.; Estrada, M.G. The NR3C1 gene expression is a potential surrogate biomarker for risk and diagnosis of posttraumatic stress disorder. Psychiatry Res. 2020, 284, 112797. [Google Scholar] [CrossRef]
- Ueyama, T.; Kasamatsu, K.; Hano, T.; Yamamoto, K.; Tsuruo, Y.; Nishio, I. Emotional stress induces transient left ventricular hypocontraction in the rat via activation of cardiac adrenoceptors: A possible animal model of ‘tako-tsubo’ cardiomyopathy. Circ. J. 2002, 66, 712–713. [Google Scholar] [CrossRef]
- Ueyama, T. Emotional stress-induced Tako-tsubo cardiomyopathy: Animal model and molecular mechanism. Ann. N. Y. Acad. Sci. 2004, 1018, 437–444. [Google Scholar] [CrossRef]
- Ueyama, T.; Yamamoto, Y.; Ueda, K.; Kawabe, T.; Hano, T.; Ito, T.; Tsuruo, Y.; Ichinose, M.; Yoshida, K.I. Cardiac and vascular gene profiles in an animal model of takotsubo cardiomyopathy. Heart Vessel. 2011, 26, 321–337. [Google Scholar] [CrossRef] [PubMed]
- Kume, T.; Kawamoto, T.; Okura, H.; Toyota, E.; Neishi, Y.; Watanabe, N.; Hayashida, A.; Okahashi, N.; Yoshimura, Y.; Saito, K.; et al. Local release of catecholamines from the hearts of patients with tako-tsubo-like left ventricular dysfunction. Circ. J. 2008, 72, 106–108. [Google Scholar] [CrossRef] [PubMed]
- Ortak, J.; Khattab, K.; Barantke, M.; Wiegand, U.K.; Baensch, D.; Ince, H.; Nienaber, C.A.; Bonnemeier, H. Evolution of cardiac autonomic nervous activity indices in patients presenting with transient left ventricular apical ballooning. Pacing Clin. Electrophysiology 2009, 32 (Suppl. 1), S21–S25. [Google Scholar] [CrossRef] [PubMed]
- Vaccaro, A.; Despas, F.; Delmas, C.; Lairez, O.; Lambert, E.; Lambert, G.; Labrunee, M.; Guiraud, T.; Esler, M.; Galinier, M.; et al. Direct evidences for sympathetic hyperactivity and baroreflex impairment in Tako Tsubo cardiopathy. PLoS ONE 2014, 9, e93278. [Google Scholar] [CrossRef] [PubMed]
- Pelliccia, F.; Kaski, J.C.; Crea, F.; Camici, P.G. Pathophysiology of Takotsubo Syndrome. Circulation 2017, 135, 2426–2441. [Google Scholar] [CrossRef]
- Ferrucci, L.; Semba, R.D.; Guralnik, J.M.; Ershler, W.B.; Bandinelli, S.; Patel, K.V.; Sun, K.; Woodman, R.C.; Andrews, N.C.; Cotter, R.J.; et al. Proinflammatory state, hepcidin, and anemia in older persons. Blood 2010, 115, 3810–3816. [Google Scholar] [CrossRef]
- Cohen, H.J.; Pieper, C.F.; Harris, T.; Rao, K.M.; Currie, M.S. The association of plasma IL-6 levels with functional disability in community-dwelling elderly. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1997, 52, M201–M208. [Google Scholar] [CrossRef]
- Newman, A.B.; Sanders, J.L.; Kizer, J.R.; Boudreau, R.M.; Odden, M.C.; Zeki Al Hazzouri, A.; Arnold, A.M. Trajectories of function and biomarkers with age: The CHS All Stars Study. Int. J. Epidemiol. 2016, 45, 1135–1145. [Google Scholar] [CrossRef]
- Gerli, R.; Monti, D.; Bistoni, O.; Mazzone, A.M.; Peri, G.; Cossarizza, A.; Di Gioacchino, M.; Cesarotti, M.E.; Doni, A.; Mantovani, A.; et al. Chemokines, sTNF-Rs and sCD30 serum levels in healthy aged people and centenarians. Mech. Ageing Dev. 2000, 121, 37–46. [Google Scholar] [CrossRef]
- Pallauf, K.; Rimbach, G. Autophagy, polyphenols and healthy ageing. Ageing Res. Rev. 2013, 12, 237–252. [Google Scholar] [CrossRef]
- Salminen, A.; Kaarniranta, K.; Kauppinen, A. Inflammaging: Disturbed interplay between autophagy and inflammasomes. Aging (Albany NY) 2012, 4, 166–175. [Google Scholar] [CrossRef]
- O’Donovan, A.; Pantell, M.S.; Puterman, E.; Dhabhar, F.S.; Blackburn, E.H.; Yaffe, K.; Cawthon, R.M.; Opresko, P.L.; Hsueh, W.C.; Satterfield, S.; et al. Cumulative inflammatory load is associated with short leukocyte telomere length in the Health, Aging and Body Composition Study. PLoS ONE 2011, 6, e19687. [Google Scholar] [CrossRef] [PubMed]
- Shiels, P.G.; McGlynn, L.M.; MacIntyre, A.; Johnson, P.C.; Batty, G.D.; Burns, H.; Cavanagh, J.; Deans, K.A.; Ford, I.; McConnachie, A.; et al. Accelerated telomere attrition is associated with relative household income, diet and inflammation in the pSoBid cohort. PLoS ONE 2011, 6, e22521. [Google Scholar] [CrossRef]
- Aviv, A.; Valdes, A.; Gardner, J.P.; Swaminathan, R.; Kimura, M.; Spector, T.D. Menopause modifies the association of leukocyte telomere length with insulin resistance and inflammation. J. Clin. Endocrinol. Metab. 2006, 91, 635–640. [Google Scholar] [CrossRef] [PubMed]
- Houben, J.M.; Moonen, H.J.; van Schooten, F.J.; Hageman, G.J. Telomere length assessment: Biomarker of chronic oxidative stress? Free. Radic. Biol. Med. 2008, 44, 235–246. [Google Scholar] [CrossRef] [PubMed]
| Country | Registry | Study Period | Age | Preceding Stress | Reference | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Emotional Stress | Physical Stress | Absence of Stress | |||||||||
| Female | Male | Female [%] | Male [%] | Female [%] | Male [%] | Female [%] | Male [%] | ||||
| USA | NI Sample | 2009–2010 | 66.2 | 59.2 | - | - | - | - | - | - | [50] |
| USA/Europe | Inter TAK Registry | 1998–2014 | 66.8 | 62.9 | 29.2 | 14.5 | 34.3 | 50.8 | 28.8 | 25.7 | [9] |
| Japan | Tokyo CCU Network | 2010–2012 | 76 | 72 | 31.0 | 19.0 | 31.3 | 50.0 | 37.7 | 31.0 | [49] |
| Japan | CIRC-8U | 1997–2014 | 71.5 | 71.8 | 26.0 | 10.0 | 46.0 | 64.0 | 28.0 | 26.0 | [51] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frank, N.; Herrmann, M.J.; Lauer, M.; Förster, C.Y. Exploratory Review of the Takotsubo Syndrome and the Possible Role of the Psychosocial Stress Response and Inflammaging. Biomolecules 2024, 14, 167. https://doi.org/10.3390/biom14020167
Frank N, Herrmann MJ, Lauer M, Förster CY. Exploratory Review of the Takotsubo Syndrome and the Possible Role of the Psychosocial Stress Response and Inflammaging. Biomolecules. 2024; 14(2):167. https://doi.org/10.3390/biom14020167
Chicago/Turabian StyleFrank, Niklas, Martin J. Herrmann, Martin Lauer, and Carola Y. Förster. 2024. "Exploratory Review of the Takotsubo Syndrome and the Possible Role of the Psychosocial Stress Response and Inflammaging" Biomolecules 14, no. 2: 167. https://doi.org/10.3390/biom14020167







