Gypenoside XVII Reduces Synaptic Glutamate Release and Protects against Excitotoxic Injury in Rats
Abstract
:1. Introduction
2. Materials and Methods
2.1. Drugs
2.2. Animals
2.3. Synaptosomes
2.4. Evaluation of Glutamate Release and FM1-43 Release in Rat Cortical Synaptosomes
2.5. KA-Induced Excitotoxicity Animal Model and Drug Treatment
2.6. Histological Analysis of Neuronal Degeneration by Fluoro-Jade B (FJB) Staining
2.7. High-Performance Liquid Chromatography (HPLC) Assay of Glutamate and γ-Aminobutyric Acid (GABA) Concentrations in the Cortex
2.8. Cerebral Blood Flow Monitoring by Laser Speckle Imaging System
2.9. Protein Isolation and Western Blotting
2.10. Statistical Analysis
3. Results
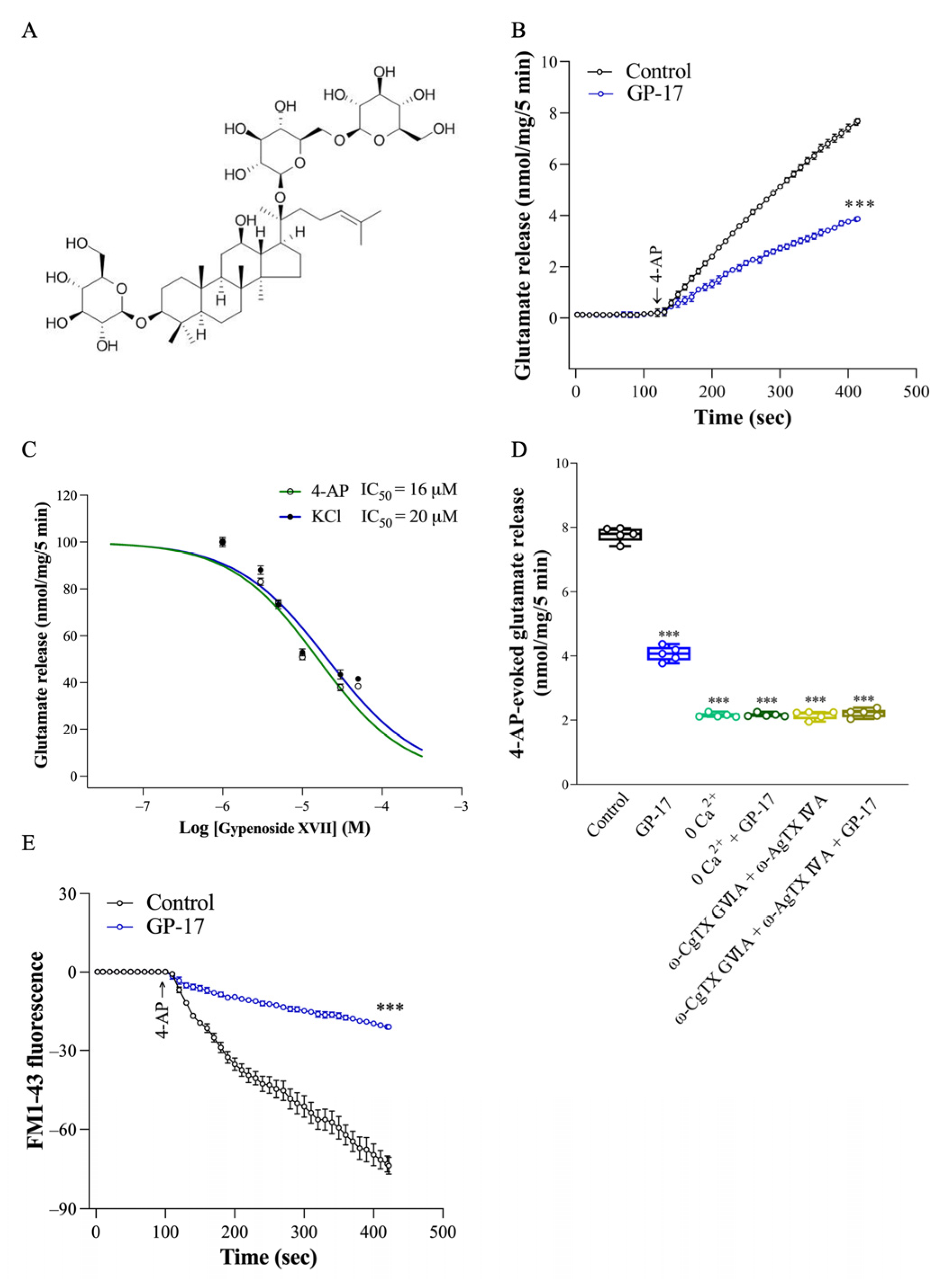
3.1. GP-17 Reduces Ca2+-Dependent Glutamate Release Evoked by 4-AP in Rat Cerebral Cortex Glutamatergic Nerve Terminals
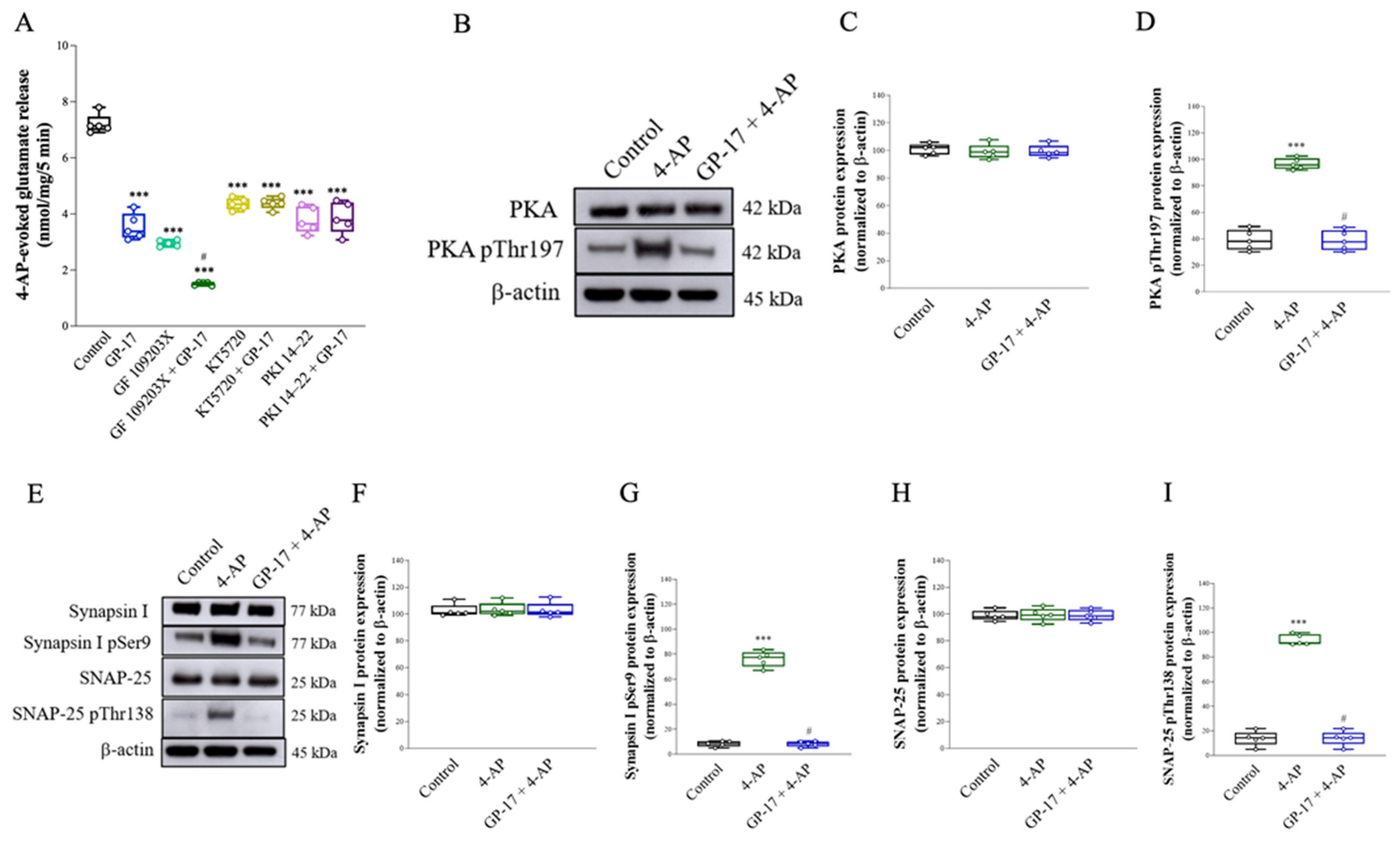
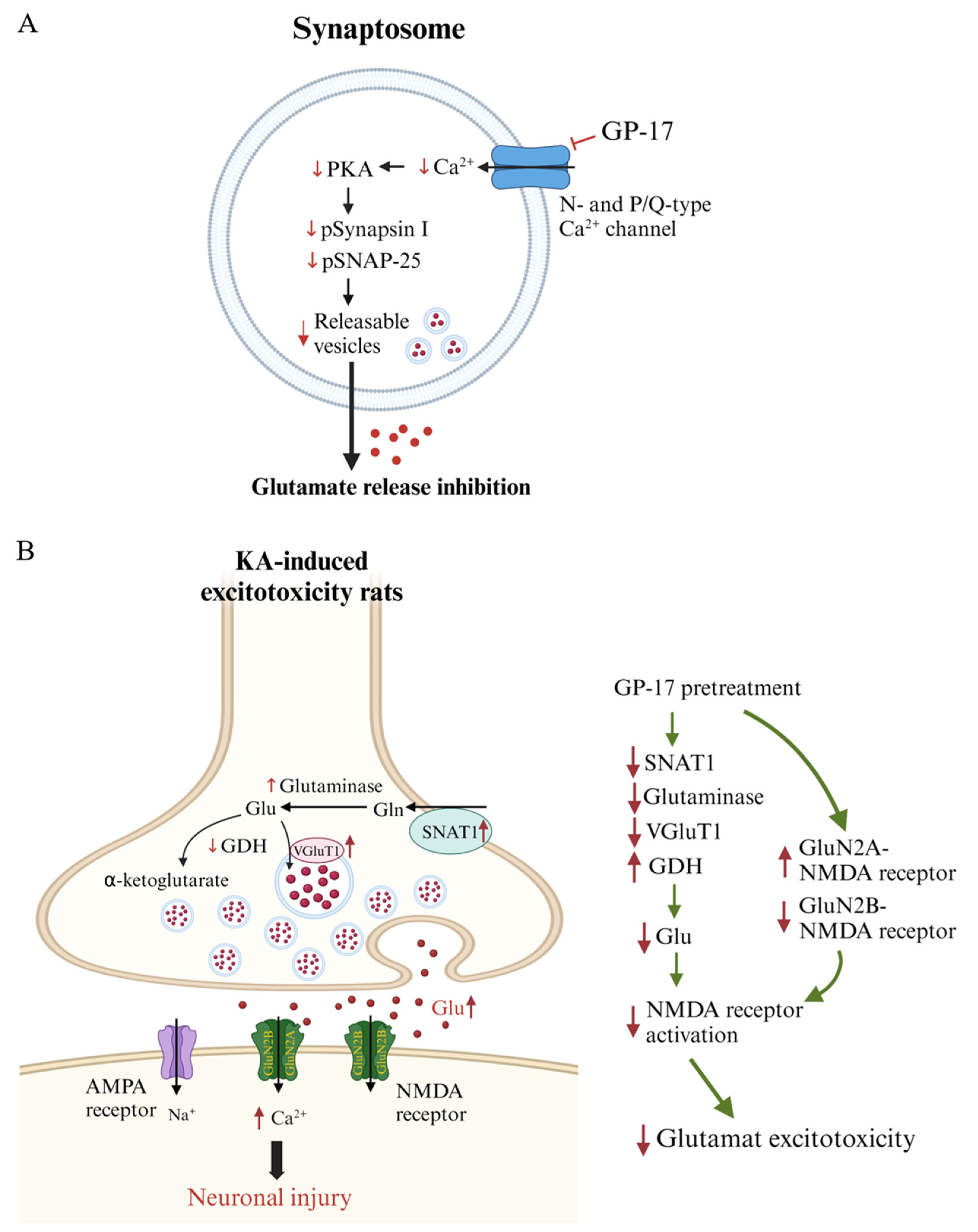
3.2. Suppression of the Protein Kinase A Pathway Is Involved in the GP-17-Mediated Inhibition of Glutamate Release from the Cerebrocortical Synaptosomes of Rats
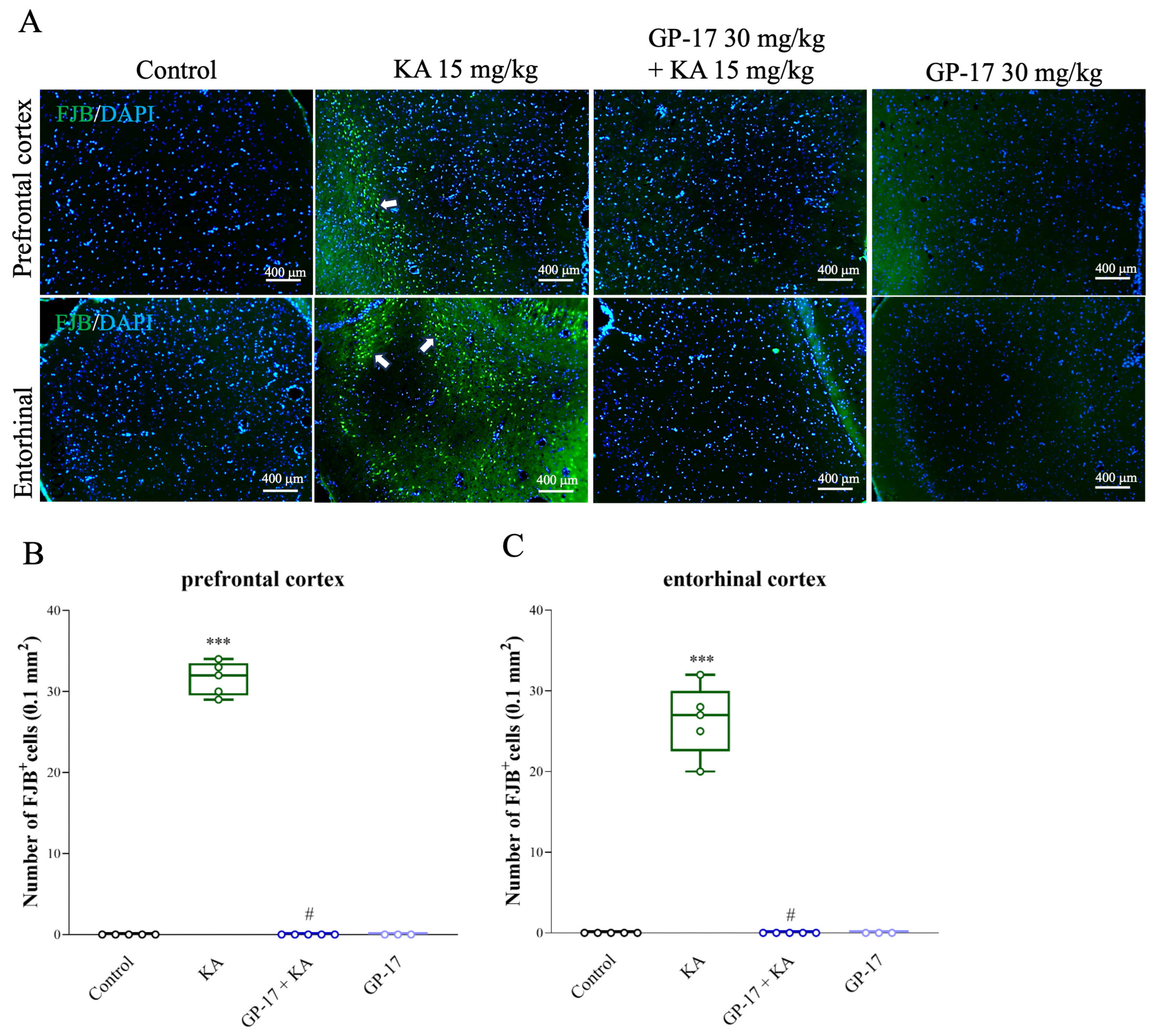
3.3. GP-17 Prevents KA-Induced Excitotoxicity in Rats
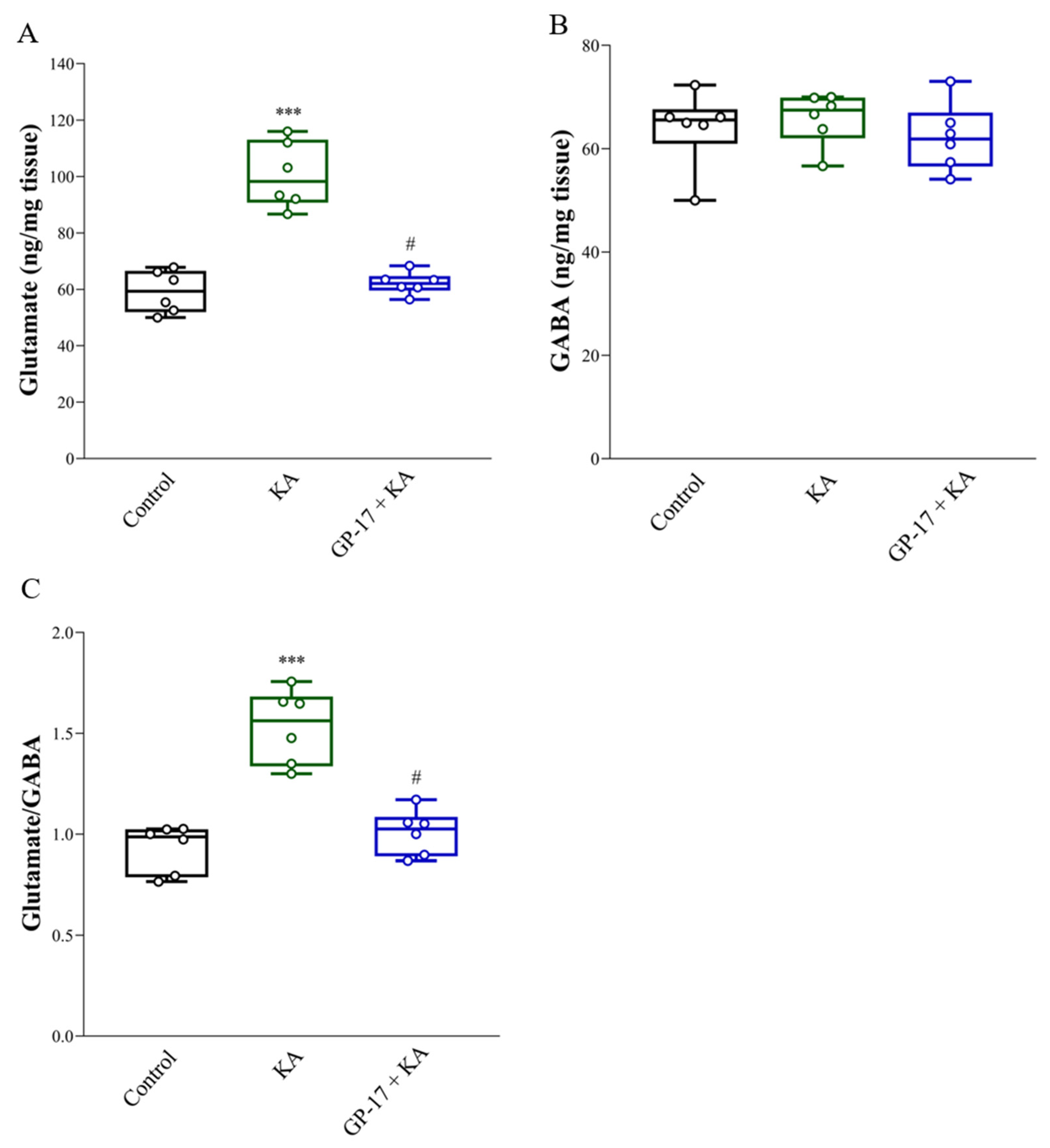
3.4. GP-17 Decreases Glutamate Concentrations in the Cortex of KA-Treated Rats
3.5. GP-17 Decreases the Protein Levels of SNAT1, Glutaminase and VGLUT1 but Increases the Protein Level of GDH in the Cortex of KA-Treated Rats
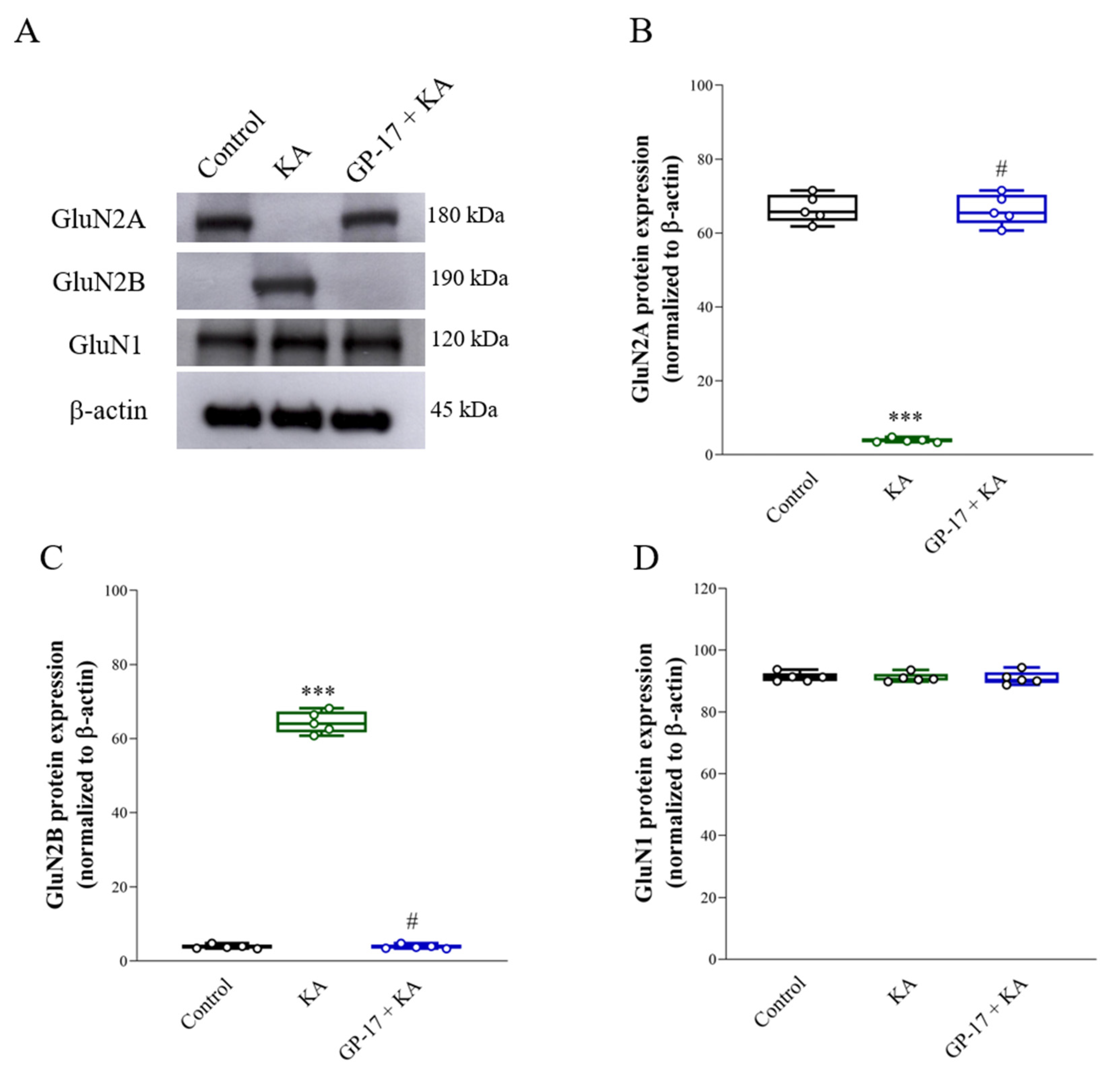
3.6. GP-17 Alters the Protein Expression of the N-methyl-D-aspartate (NMDA) Receptor Subunits GluN2A and GluN2B in the Cortex of KA-Treated Rats
3.7. GP-17 Prevents Decreases in Cerebral Blood Flow and ArgII Expression in KA-Treated Rats
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhou, Y.; Danbolt, N.C. Glutamate as a neurotransmitter in the healthy brain. J. Neural Transm. 2014, 121, 799–817. [Google Scholar] [CrossRef] [PubMed]
- Olloquequi, J.; Cornejo-Cordova, E.; Verdaguer, E.; Soriano, F.X.; Binvignat, O.; Auladell, C.; Camins, A. Excitotoxicity in the pathogenesis of neurological and psychiatric disorders: Therapeutic implications. J. Psychopharmacol. 2018, 32, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Binvignat, O.; Olloquequi, J. Excitotoxicity as a target against neurodegenerative processes. Curr. Pharm. Des. 2020, 26, 1251–1262. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.X.; Wang, Y.; Qin, Z.H. Molecular mechanisms of excitotoxicity and their relevance to pathogenesis of neurodegenerative diseases. Acta Pharmacol. Sin. 2009, 30, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Lai, T.W.; Zhang, S.; Wang, Y.T. Excitotoxicity and stroke: Identifying novel targets for neuroprotection. Prog. Neurobiol. 2014, 115, 157–188. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Liu, N.; Chen, J.; Zheng, P.; Niu, J.; Tang, S.; Peng, X.; Wu, J.; Yu, J.; Ma, L. Neuropharmacological insight into preventive intervention in posttraumatic epilepsy based on regulating glutamate homeostasis. CNS Neurosci. Ther. 2023, 29, 2430–2444. [Google Scholar] [CrossRef] [PubMed]
- Pomierny, B.; Krzyzanowska, W.; Skorkowska, A.; Jurczyk, J.; Bystrowska, B.; Budziszewska, B.; Pera, J. Inhibition of vesicular glutamate transporters (VGLUTs) with Chicago Sky Blue 6B before focal cerebral ischemia offers neuroprotection. Mol. Neurobiol. 2023, 60, 3130–3146. [Google Scholar] [CrossRef] [PubMed]
- Borbely, E.; Simon, M.; Fuchs, E.; Wiborg, O.; Czeh, B.; Helyes, Z. Novel drug developmental strategies for treatment-resistant depression. Br. J. Pharmacol. 2022, 179, 1146–1186. [Google Scholar] [CrossRef]
- Hasan, S.; Khatri, N.; Rahman, Z.N.; Menezes, A.A.; Martini, J.; Shehjar, F.; Mujeeb, N.; Shah, Z.A. Neuroprotective potential of flavonoids in brain disorders. Brain Sci. 2023, 13, 1258. [Google Scholar] [CrossRef]
- Zhou, J.C.; Li, H.L.; Zhou, Y.; Li, X.T.; Yang, Z.Y.; Tohda, C.; Komatsu, K.; Piao, X.H.; Ge, Y.W. The roles of natural triterpenoid saponins against Alzheimer’s disease. Phytother. Res. 2023, 37, 5017–5040. [Google Scholar] [CrossRef]
- Zhang, M.M.; Huo, G.M.; Cheng, J.; Zhang, Q.P.; Li, N.Z.; Guo, M.X.; Liu, Q.; Xu, G.H.; Zhu, J.X.; Li, C.F.; et al. Gypenoside XVII, an active ingredient from gynostemma pentaphyllum, inhibits C3aR-associated synaptic pruning in stressed mice. Nutrients 2022, 14, 2418. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Yu, Y.; Zhang, H.; Li, L.; Wang, J.; Su, S.; Zhang, Y.; Song, L.; Zhou, K. Gypenoside XVII attenuates renal ischemia-reperfusion injury by inhibiting endoplasmic reticulum stress and NLRP3 inflammasome-triggered pyroptosis. Eur. J. Pharmacol. 2024, 962, 176187. [Google Scholar] [CrossRef] [PubMed]
- Su, S.; Wang, J.; Wang, J.; Yu, R.; Sun, L.; Zhang, Y.; Song, L.; Pu, W.; Tang, Y.; Yu, Y.; et al. Cardioprotective effects of gypenoside XVII against ischemia/reperfusion injury: Role of endoplasmic reticulum stress, autophagy, and mitochondrial fusion fission balance. Phytother. Res. 2022, 36, 2982–2998. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Wang, M.; Chen, R.; Sun, X.; Sun, G.; Sun, X. Gypenoside XVII protects against myocardial ischemia and reperfusion injury by inhibiting ER stress-induced mitochondrial injury. J. Ginseng Res. 2021, 45, 642–653. [Google Scholar] [CrossRef] [PubMed]
- Deng, W.Y.; Zhou, C.L.; Zeng, M.Y. Gypenoside XVII inhibits ox-LDL-induced macrophage inflammatory responses and promotes cholesterol efflux through activating the miR-182-5p/HDAC9 signaling pathway. J. Ethnopharmacol. 2024, 319, 117070. [Google Scholar] [CrossRef]
- Zhou, K.; Zhang, Y.; Zhou, Y.; Xu, M.; Yu, S. Production of gypenoside XVII from ginsenoside Rb1 by enzymatic transformation and their anti-inflammatory activity in vitro and in vivo. Molecules 2023, 28, 7001. [Google Scholar] [CrossRef] [PubMed]
- Xie, W.; Zhu, T.; Zhang, S.; Sun, X. Protective effects of Gypenoside XVII against cerebral ischemia/reperfusion injury via SIRT1-FOXO3A- and Hif1a-BNIP3-mediated mitochondrial autophagy. J. Transl. Med. 2022, 20, 622. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; Luo, Y.; Liang, T.; Wang, M.; Zhao, J.; Sun, G.; Sun, X. Gypenoside XVII enhances lysosome biogenesis and autophagy flux and accelerates autophagic clearance of amyloid-beta through TFEB activation. J. Alzheimers Dis. 2016, 52, 1135–1150. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; Wang, M.; Sun, G.; Ye, J.; Zhou, Y.; Dong, X.; Wang, T.; Lu, S.; Sun, X. Attenuation of Abeta25-35-induced parallel autophagic and apoptotic cell death by gypenoside XVII through the estrogen receptor-dependent activation of Nrf2/ARE pathways. Toxicol. Appl. Pharmacol. 2014, 279, 63–75. [Google Scholar] [CrossRef]
- Raiteri, L.; Raiteri, M. Synaptosomes still viable after 25 years of superfusion. Neurochem. Res. 2000, 25, 1265–1274. [Google Scholar] [CrossRef]
- Wang, Q.; Yu, S.; Simonyi, A.; Sun, G.Y.; Sun, A.Y. Kainic acid-mediated excitotoxicity as a model for neurodegeneration. Mol. Neurobiol. 2005, 31, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Ferkany, J.W.; Zaczek, R.; Coyle, J.T. Kainic acid stimulates excitatory amino acid neurotransmitter release at presynaptic receptors. Nature 1982, 298, 757–759. [Google Scholar] [CrossRef] [PubMed]
- Dunkley, P.R.; Jarvie, P.E.; Robinson, P.J. A rapid Percoll gradient procedure for preparation of synaptosomes. Nat. Protoc. 2008, 3, 1718–1728. [Google Scholar] [CrossRef] [PubMed]
- Bradford, M.M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal. Biochem. 1976, 72, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.C.; Hsieh, P.W.; Kuo, J.R.; Wang, S.J. Rosmarinic acid, a bioactive phenolic compound, inhibits glutamate release from rat cerebrocortical synaptosomes through GABAA receptor activation. Biomolecules 2021, 11, 1029. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.Y.; Lu, C.W.; Hsieh, P.W.; Chiu, K.M.; Lee, M.Y.; Wang, S.J. Natural product isoliquiritigenin activates GABAB receptors to decrease voltage-gate Ca2+ channels and glutamate release in rat cerebrocortical nerve terminals. Biomolecules 2021, 11, 1537. [Google Scholar] [CrossRef] [PubMed]
- Murthy, V.N. Optical detection of synaptic vesicle exocytosis and endocytosis. Curr. Opin. Neurobiol. 1999, 9, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, M.L.; Rostas, J.A.; Sim, A.T. Two modes of exocytosis from synaptosomes are differentially regulated by protein phosphatase types 2A and 2B. J. Neurochem. 2003, 85, 1190–1199. [Google Scholar] [CrossRef]
- Jean, W.H.; Huang, C.T.; Hsu, J.H.; Chiu, K.M.; Lee, M.Y.; Shieh, J.S.; Lin, T.Y.; Wang, S.J. Anticonvulsive and neuroprotective effects of eupafolin in rats are associated with the inhibition of glutamate overexcitation and upregulation of the Wnt/beta-catenin signaling pathway. ACS Chem. Neurosci. 2022, 13, 1594–1603. [Google Scholar] [CrossRef]
- Friedman, L.K.; Pellegrini-Giampietro, D.E.; Sperber, E.F.; Bennett, M.V.; Moshe, S.L.; Zukin, R.S. Kainate-induced status epilepticus alters glutamate and GABAA receptor gene expression in adult rat hippocampus: An in situ hybridization study. J. Neurosci. 1994, 14, 2697–2707. [Google Scholar] [CrossRef]
- Spigolon, G.; Veronesi, C.; Bonny, C.; Vercelli, A. c-Jun N-terminal kinase signaling pathway in excitotoxic cell death following kainic acid-induced status epilepticus. Eur. J. Neurosci. 2010, 31, 1261–1272. [Google Scholar] [CrossRef] [PubMed]
- Racine, R.J. Modification of seizure activity by electrical stimulation. II. Motor seizure. Electroencephalogr. Clin. Neurophysiol. 1972, 32, 281–294. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.Y.; Lu, C.W.; Wang, S.J. Luteolin protects the hippocampus against neuron impairments induced by kainic acid in rats. Neurotoxicology 2016, 55, 48–57. [Google Scholar] [CrossRef]
- Pai, M.S.; Wang, K.C.; Yeh, K.C.; Wang, S.J. Stabilization of mitochondrial function by chlorogenic acid protects against kainic acid-induced seizures and neuronal cell death in rats. Eur. J. Pharmacol. 2023, 961, 176197. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.; Chang, Y.; Wang, S.J. Rutin prevents seizures in kainic acid-treated rats: Evidence of glutamate levels, inflammation and neuronal loss modulation. Food Funct. 2022, 13, 10401–10414. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Mu, Y.; Ding, H.; Du, B.; Zhou, M.; Li, Q.; Gong, S.; Zhang, F.; Geng, D.; Wang, Y. 1alpha,25-Dihydroxyvitamin D3 Promotes Angiogenesis After Cerebral Ischemia Injury in Rats by Upregulating the TGF-beta/Smad2/3 Signaling Pathway. Front. Cardiovasc. Med. 2022, 9, 769717. [Google Scholar] [CrossRef] [PubMed]
- Yeh, K.C.; Hung, C.F.; Lee, H.L.; Hsieh, T.Y.; Wang, S.J. Soybean meal extract preserves memory ability by increasing presynaptic function and modulating gut microbiota in rats. Mol. Neurobiol. 2022, 59, 1649–1664. [Google Scholar] [CrossRef] [PubMed]
- Millan, C.; Sanchez-Prieto, J. Differential coupling of N- and P/Q-type calcium channels to glutamate exocytosis in the rat cerebral cortex. Neurosci. Lett. 2002, 330, 29–32. [Google Scholar] [CrossRef] [PubMed]
- Coffey, E.T.; Sihra, T.S.; Nicholls, D.G. Protein kinase C and the regulation of glutamate exocytosis from cerebrocortical synaptosomes. J. Biol. Chem. 1993, 268, 21060–21065. [Google Scholar] [CrossRef]
- Millan, C.; Torres, M.; Sanchez-Prieto, J. Co-activation of PKA and PKC in cerebrocortical nerve terminals synergistically facilitates glutamate release. J. Neurochem. 2003, 87, 1101–1111. [Google Scholar] [CrossRef]
- Greengard, P.; Valtorta, F.; Czernik, A.J.; Benfenati, F. Synaptic vesicle phosphoproteins and regulation of synaptic function. Science 1993, 259, 780–785. [Google Scholar] [CrossRef] [PubMed]
- Kyllo, T.; Singh, V.; Shim, H.; Latika, S.; Nguyen, H.M.; Chen, Y.J.; Terry, E.; Wulff, H.; Erickson, J.D. Riluzole and novel naphthalenyl substituted aminothiazole derivatives prevent acute neural excitotoxic injury in a rat model of temporal lobe epilepsy. Neuropharmacology 2023, 224, 109349. [Google Scholar] [CrossRef]
- Ferkany, J.W.; Coyle, J.T. Kainic acid selectively stimulates the release of endogenous excitatory acidic amino acids. J. Pharmacol. Exp. Ther. 1983, 225, 399–406. [Google Scholar]
- Mohd Sairazi, N.S.; Sirajudeen, K.N.; Asari, M.A.; Muzaimi, M.; Mummedy, S.; Sulaiman, S.A. Kainic acid-induced excitotoxicity experimental model: Protective merits of natural products and plant extracts. Evid. Based Complement. Alternat. Med. 2015, 2015, 972623. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Zhang, X.; Chen, X.; Wei, Y. Neuronal injuries in cerebral infarction and ischemic stroke: From mechanisms to treatment (Review). Int. J. Mol. Med. 2022, 49, 15. [Google Scholar] [CrossRef]
- Ahmad, A.S.; Shah, Z.A.; Dore, S. Protective role of arginase II in cerebral ischemia and excitotoxicity. J. Neurol. Neurosci. 2016, 7, 88. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.J.; Sihra, T.S. Opposing facilitatory and inhibitory modulation of glutamate release elicited by cAMP production in cerebrocortical nerve terminals (synaptosomes). Neuropharmacology 2003, 44, 686–697. [Google Scholar] [CrossRef]
- Nagy, G.; Reim, K.; Matti, U.; Brose, N.; Binz, T.; Rettig, J.; Neher, E.; Sorensen, J.B. Regulation of releasable vesicle pool sizes by protein kinase A-dependent phosphorylation of SNAP-25. Neuron 2004, 41, 417–429. [Google Scholar] [CrossRef]
- Ceccaldi, P.E.; Grohovaz, F.; Benfenati, F.; Chieregatti, E.; Greengard, P.; Valtorta, F. Dephosphorylated synapsin I anchors synaptic vesicles to actin cytoskeleton: An analysis by videomicroscopy. J. Cell Biol. 1995, 128, 905–912. [Google Scholar] [CrossRef]
- Menegon, A.; Bonanomi, D.; Albertinazzi, C.; Lotti, F.; Ferrari, G.; Kao, H.T.; Benfenati, F.; Baldelli, P.; Valtorta, F. Protein kinase A-mediated synapsin I phosphorylation is a central modulator of Ca2+-dependent synaptic activity. J. Neurosci. 2006, 26, 11670–11681. [Google Scholar] [CrossRef]
- Hsu, S.K.; Lu, C.W.; Chiu, K.M.; Lee, M.Y.; Lin, T.Y.; Wang, S.J. Mangiferin depresses vesicular glutamate release in synaptosomes from the rat cerebral cortex by decreasing synapsin I phosphorylation. Eur. J. Pharmacol. 2023, 950, 175772. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.W.; Lin, T.Y.; Hsieh, P.W.; Chiu, K.M.; Lee, M.Y.; Wang, S.J. Cynarin, a caffeoylquinic acid derivative in artichoke, inhibits exocytotic glutamate release from rat cortical nerve terminals (synaptosomes). Neurochem. Int. 2023, 167, 105537. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.K.; Yeh, K.C.; Pai, M.S.; Hsieh, P.W.; Wang, S.J. Ursolic acid inhibits the synaptic release of glutamate and prevents glutamate excitotoxicity in rats. Eur. J. Pharmacol. 2024, 963, 176280. [Google Scholar] [CrossRef]
- Lu, C.W.; Wu, C.C.; Chiu, K.M.; Lee, M.Y.; Lin, T.Y.; Wang, S.J. Inhibition of synaptic glutamate exocytosis and prevention of glutamate neurotoxicity by eupatilin from artemisia argyi in the rat cortex. Int. J. Mol. Sci. 2022, 23, 13406. [Google Scholar] [CrossRef] [PubMed]
- Pietrancosta, N.; Djibo, M.; Daumas, S.; El Mestikawy, S.; Erickson, J.D. Molecular, structural, functional, and pharmacological sites for vesicular glutamate transporter regulation. Mol. Neurobiol. 2020, 57, 3118–3142. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, F.A.; Schmitz, D.; Reimer, R.J.; Larsson, P.; Gray, A.T.; Nicoll, R.; Kavanaugh, M.; Edwards, R.H. Glutamine uptake by neurons: Interaction of protons with system a transporters. J. Neurosci. 2002, 22, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Daniels, R.W.; Miller, B.R.; DiAntonio, A. Increased vesicular glutamate transporter expression causes excitotoxic neurodegeneration. Neurobiol. Dis. 2011, 41, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Lynch, D.R.; Guttmann, R.P. Excitotoxicity: Perspectives based on N-methyl-D-aspartate receptor subtypes. J. Pharmacol. Exp. Ther. 2002, 300, 717–723. [Google Scholar] [CrossRef]
- Paoletti, P.; Bellone, C.; Zhou, Q. NMDA receptor subunit diversity: Impact on receptor properties, synaptic plasticity and disease. Nat. Rev. Neurosci. 2013, 14, 383–400. [Google Scholar] [CrossRef]
- Ladagu, A.D.; Olopade, F.E.; Adejare, A.; Olopade, J.O. GluN2A and GluN2B N-methyl-D-aspartate receptor (NMDARs) subunits: Their roles and therapeutic antagonists in neurological diseases. Pharmaceuticals 2023, 16, 1535. [Google Scholar] [CrossRef]
- Choo, A.M.; Geddes-Klein, D.M.; Hockenberry, A.; Scarsella, D.; Mesfin, M.N.; Singh, P.; Patel, T.P.; Meaney, D.F. NR2A and NR2B subunits differentially mediate MAP kinase signaling and mitochondrial morphology following excitotoxic insult. Neurochem. Int. 2012, 60, 506–516. [Google Scholar] [CrossRef] [PubMed]
- Shi, Z.; Zhu, L.; Li, T.; Tang, X.; Xiang, Y.; Han, X.; Xia, L.; Zeng, L.; Nie, J.; Huang, Y.; et al. Neuroprotective mechanisms of Lycium barbarum polysaccharides against ischemic insults by regulating NR2B and NR2A containing NMDA receptor signaling pathways. Front. Cell. Neurosci. 2017, 11, 288. [Google Scholar] [CrossRef] [PubMed]
- Saito, A.; Maier, C.M.; Narasimhan, P.; Nishi, T.; Song, Y.S.; Yu, F.; Liu, J.; Lee, Y.S.; Nito, C.; Kamada, H.; et al. Oxidative stress and neuronal death/survival signaling in cerebral ischemia. Mol. Neurobiol. 2005, 31, 105–116. [Google Scholar] [CrossRef] [PubMed]
- Dawson, V.L.; Dawson, T.M.; London, E.D.; Bredt, D.S.; Snyder, S.H. Nitric oxide mediates glutamate neurotoxicity in primary cortical cultures. Proc. Natl. Acad. Sci. USA 1991, 88, 6368–6371. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; Duan, L.; Li, J.; Guo, H.; Xiong, M. Gypenoside XVII protects against spinal cord injury in mice by regulating the microRNA-21-mediated PTEN/AKT/mTOR pathway. Int. J. Mol. Med. 2021, 48, 146. [Google Scholar] [CrossRef] [PubMed]
- Lazarevic, V.; Yang, Y.; Ivanova, D.; Fejtova, A.; Svenningsson, P. Riluzole attenuates the efficacy of glutamatergic transmission by interfering with the size of the readily releasable neurotransmitter pool. Neuropharmacology 2018, 143, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Cheng, X.; Zhao, M.; Zhao, T.; Zhang, M.; Shi, Z.; Yue, X.; Geng, Y.; Gao, J.; Wang, C.; et al. Gypenoside-14 Reduces Depression via downregulation of the nuclear factor kappa B (NF-kB) signaling pathway on the lipopolysaccharide (LPS)-induced depression model. Pharmaceuticals 2023, 16, 1152. [Google Scholar] [CrossRef]
- Zhang, G.L.; Deng, J.P.; Wang, B.H.; Zhao, Z.W.; Li, J.; Gao, L.; Liu, B.L.; Xong, J.R.; Guo, X.D.; Yan, Z.Q.; et al. Gypenosides improve cognitive impairment induced by chronic cerebral hypoperfusion in rats by suppressing oxidative stress and astrocytic activation. Behav. Pharmacol. 2011, 22, 633–644. [Google Scholar] [CrossRef]


| KA 15 mg/kg | GP-17 10 mg/kg + KA 15 mg/kg | GP-17 30 mg/kg + KA 15 mg/kg | |
|---|---|---|---|
| Seizure score | 4.7 ± 0.1 | 4.3 ± 0.2 | 0.8 ± 0.3 *** |
| Latency to first seizure (min) | 84.4 ± 6.5 | 111.1 ± 13.4 | - |
| % Seizure | 20/20 (100%) | 9/10 (90%) | 0/14 (0%) |
| Mortality | 6/20 | 2/10 | 0/14 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, C.-W.; Lin, T.-Y.; Chiu, K.-M.; Lee, M.-Y.; Wang, S.-J. Gypenoside XVII Reduces Synaptic Glutamate Release and Protects against Excitotoxic Injury in Rats. Biomolecules 2024, 14, 589. https://doi.org/10.3390/biom14050589
Lu C-W, Lin T-Y, Chiu K-M, Lee M-Y, Wang S-J. Gypenoside XVII Reduces Synaptic Glutamate Release and Protects against Excitotoxic Injury in Rats. Biomolecules. 2024; 14(5):589. https://doi.org/10.3390/biom14050589
Chicago/Turabian StyleLu, Cheng-Wei, Tzu-Yu Lin, Kuan-Ming Chiu, Ming-Yi Lee, and Su-Jane Wang. 2024. "Gypenoside XVII Reduces Synaptic Glutamate Release and Protects against Excitotoxic Injury in Rats" Biomolecules 14, no. 5: 589. https://doi.org/10.3390/biom14050589
APA StyleLu, C.-W., Lin, T.-Y., Chiu, K.-M., Lee, M.-Y., & Wang, S.-J. (2024). Gypenoside XVII Reduces Synaptic Glutamate Release and Protects against Excitotoxic Injury in Rats. Biomolecules, 14(5), 589. https://doi.org/10.3390/biom14050589







