Role of Inflammation and the NF-κB Signaling Pathway in Hirschsprung’s Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval and Samples Collection
2.2. RT-qPCR
2.3. Immunohistochemistry
2.4. Image Acquisition and Analysis
2.5. Statistical Analysis
3. Results
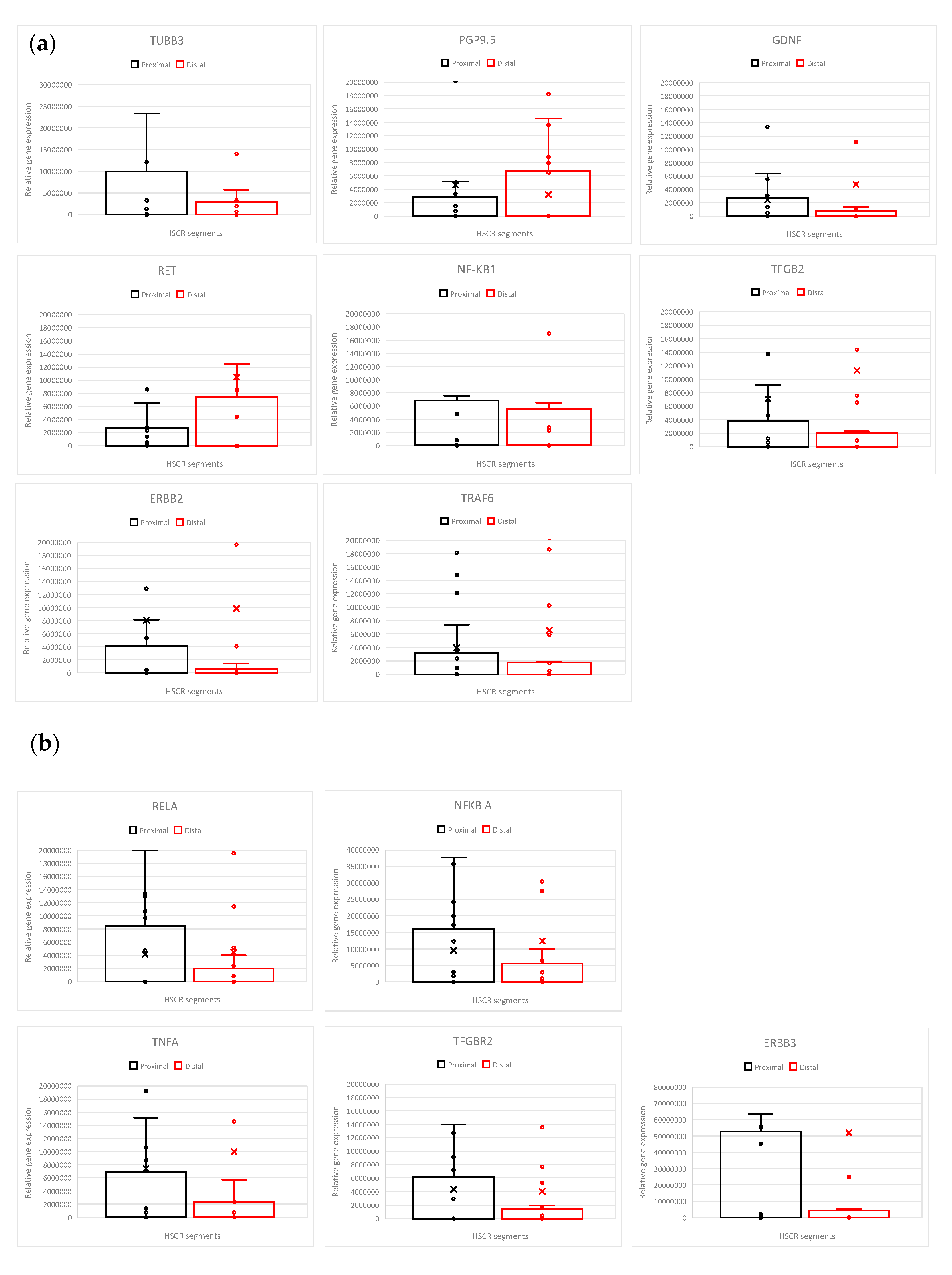
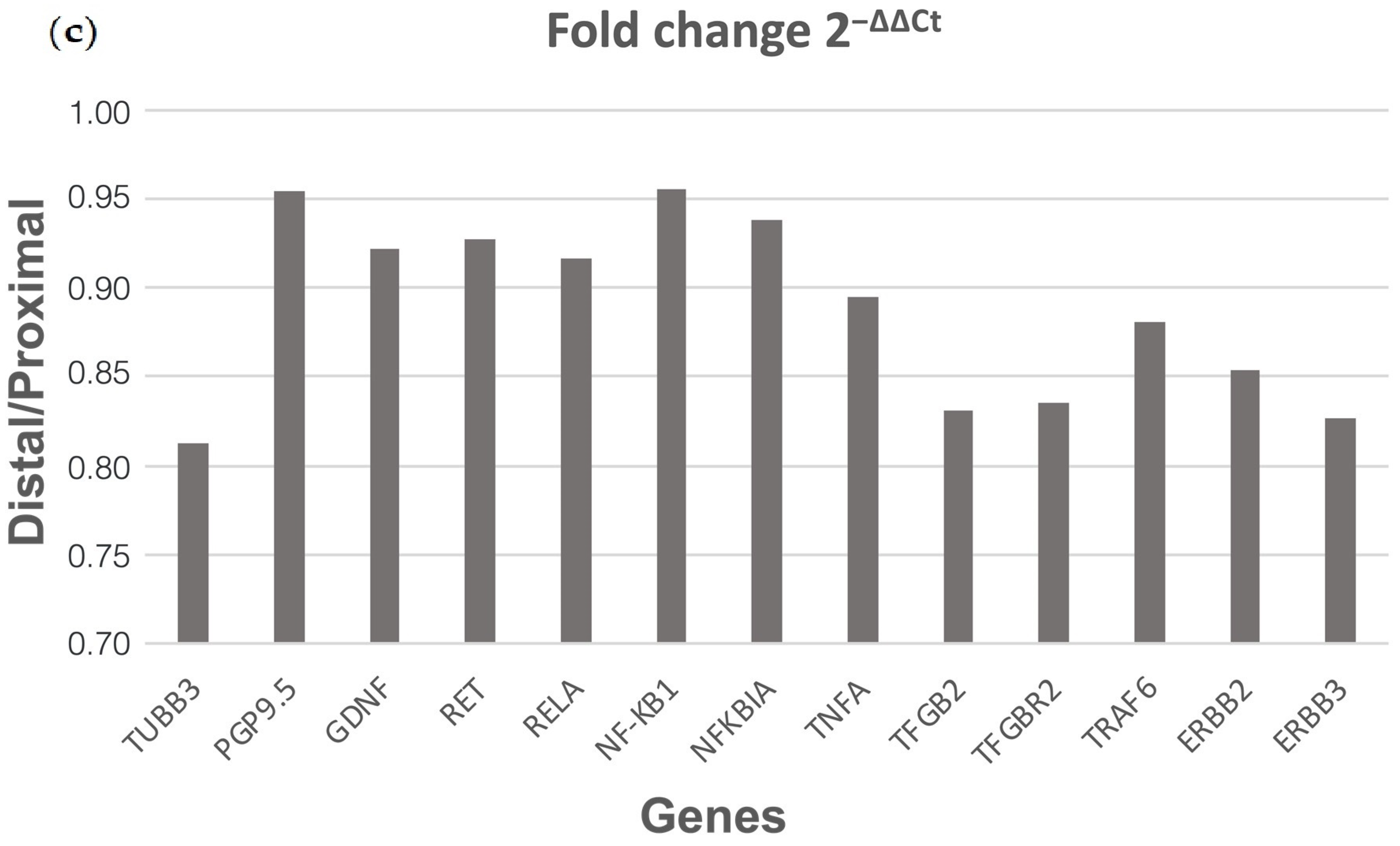
3.1. HSCR Proximal Ganglionic Segments Show Increased RELA and Pro-Inflammatory Gene Expression Profiles
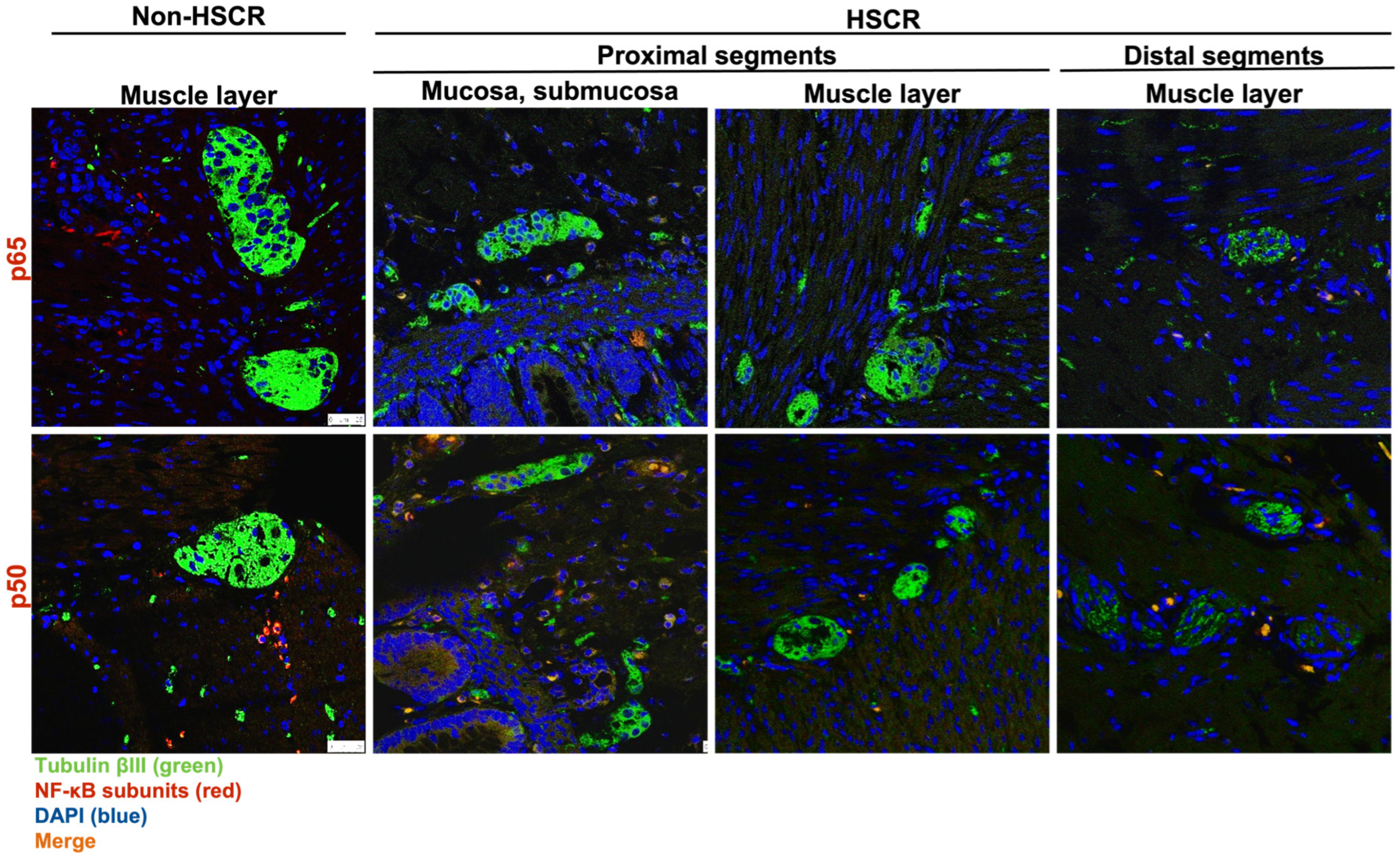
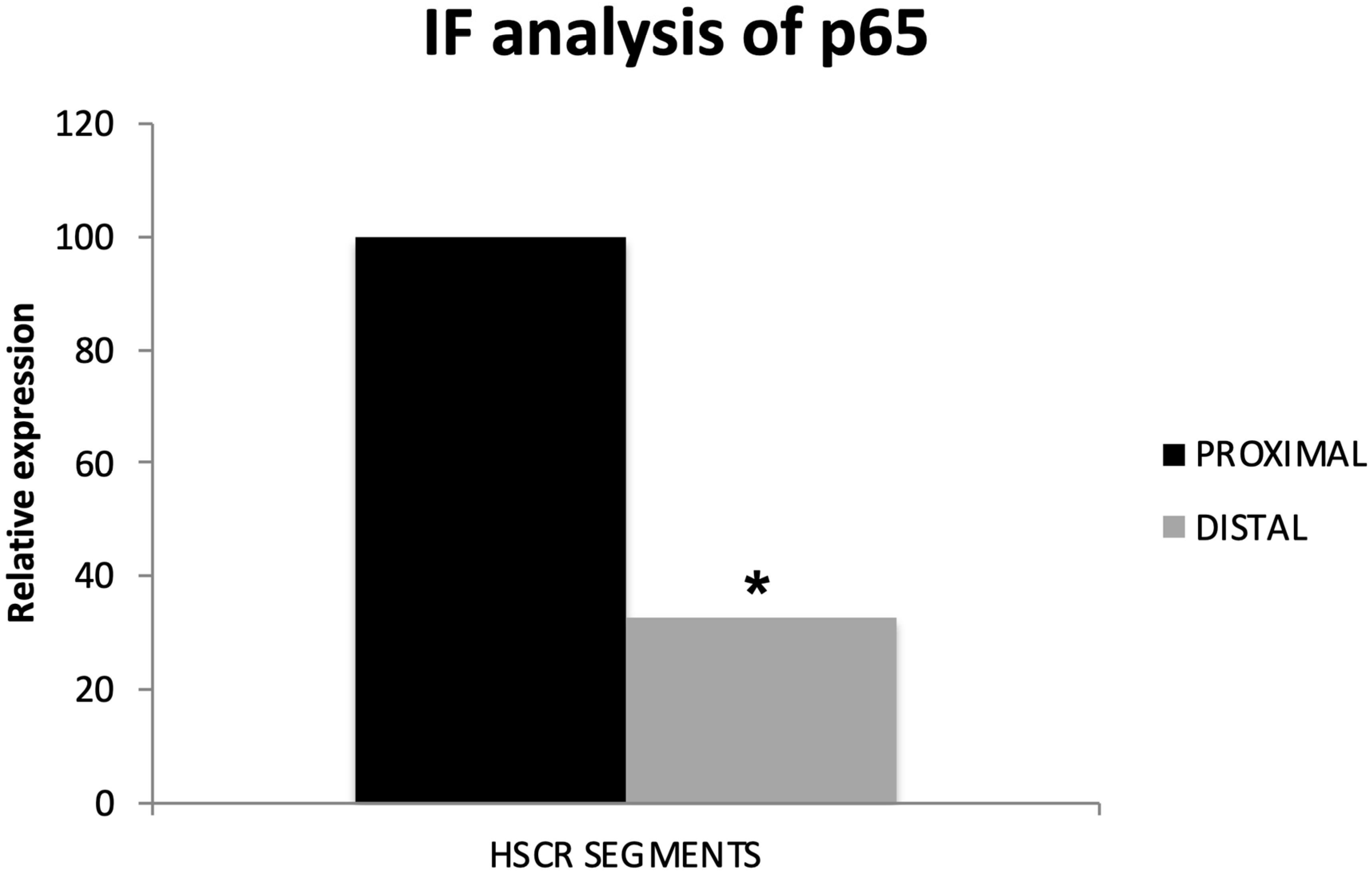
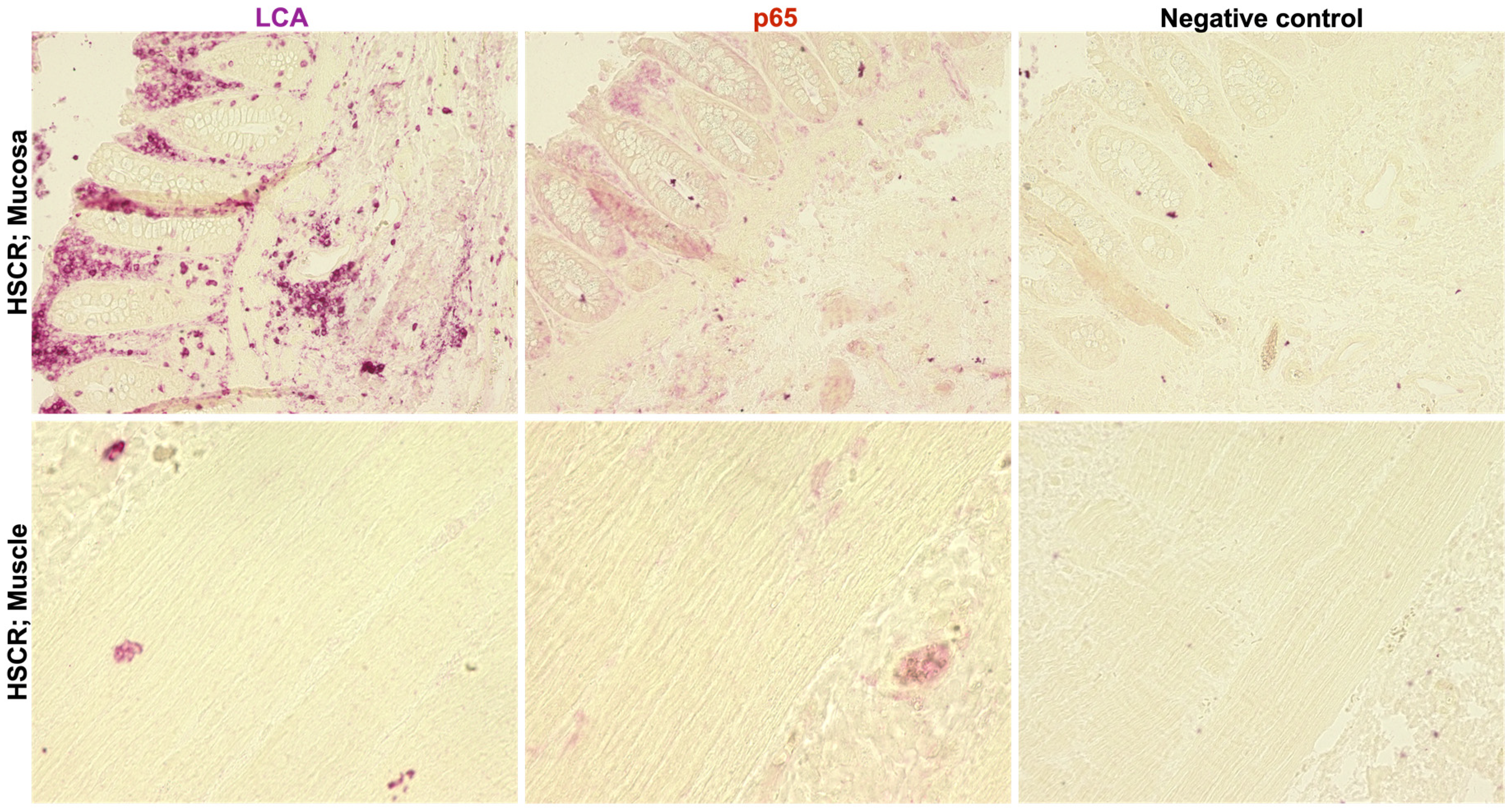
3.2. RelA/p65 Protein Levels Are Higher in HSCR Proximal Ganglionic Segments
3.3. RelA/p65 Expression in HSCR Tissue Correlates with Lymphocyte Infiltration
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Heuckeroth, R.O. Hirschsprung Disease—Integrating Basic Science and Clinical Medicine to Improve Outcomes. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 152–167. [Google Scholar] [CrossRef] [PubMed]
- Calkins, C. Hirschsprung Disease beyond Infancy. Clin. Colon Rectal Surg. 2018, 31, 051–060. [Google Scholar] [CrossRef] [PubMed]
- Lake, J.I.; Heuckeroth, R.O. Enteric Nervous System Development: Migration, Differentiation, and Disease. Am. J. Physiol.-Gastrointest. Liver Physiol. 2013, 305, G1–G24. [Google Scholar] [CrossRef] [PubMed]
- Heuckeroth, R.O. Hirschsprung’s Disease, Down Syndrome, and Missing Heritability: Too Much Collagen Slows Migration. J. Clin. Investig. 2015, 125, 4323–4326. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Ceccherini, I.; Pasini, B.; Matera, I.; Bicocchi, M.P.; Barone, V.; Bocclardi, R.; Kääriänen, H.; Weber, D.; Devoto, M.; et al. Close Linkage with the RET Protooncogene and Boundaries of Deletion Mutations in Autosomal Dominant Hirschsprung Disease. Hum. Mol. Genet. 1993, 2, 1803–1808. [Google Scholar] [CrossRef] [PubMed]
- Puffenberger, E.G.; Hosoda, K.; Washington, S.S.; Nakao, K.; Dewit, D.; Yanagisawa, M.; Chakravarti, A. A Missense Mutation of the Endothelin-B Receptor Gene in Multigenic Hirschsprung’s Disease. Cell 1994, 79, 1257–1266. [Google Scholar] [CrossRef] [PubMed]
- McCallion, A.S.; Stames, E.; Conlon, R.A.; Chakravarti, A. Phenotype Variation in Two-Locus Mouse Models of Hirschsprung Disease: Tissue-Specific Interaction between Ret and Ednrb. Proc. Natl. Acad. Sci. USA 2003, 100, 1826–1831. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.J.; Camilleri, M. Hirschsprung Disease: Insights on Genes, Penetrance, and Prenatal Diagnosis. Neurogastroenterol. Motil. 2019, 31, e13732. [Google Scholar] [CrossRef] [PubMed]
- Heuckeroth, R.O. Even When You Know Everything, There Is Still More to Learn About Hirschsprung Disease. Gastroenterology 2018, 155, 1681–1684. [Google Scholar] [CrossRef]
- Heuckeroth, R.O.; Schäfer, K.-H. Gene-Environment Interactions and the Enteric Nervous System: Neural Plasticity and Hirschsprung Disease Prevention. Dev. Biol. 2016, 417, 188–197. [Google Scholar] [CrossRef]
- Luzón-Toro, B.; Villalba-Benito, L.; Torroglosa, A.; Fernández, R.M.; Antiñolo, G.; Borrego, S. What Is New about the Genetic Background of Hirschsprung Disease? Clin. Genet. 2020, 97, 114–124. [Google Scholar] [CrossRef] [PubMed]
- Tang, C.S.; Li, P.; Lai, F.P.-L.; Fu, A.X.; Lau, S.-T.; So, M.T.; Lui, K.N.-C.; Li, Z.; Zhuang, X.; Yu, M.; et al. Identification of Genes Associated With Hirschsprung Disease, Based on Whole-Genome Sequence Analysis, and Potential Effects on Enteric Nervous System Development. Gastroenterology 2018, 155, 1908–1922.e5. [Google Scholar] [CrossRef] [PubMed]
- Muller, P.A.; Koscsó, B.; Rajani, G.M.; Stevanovic, K.; Berres, M.-L.; Hashimoto, D.; Mortha, A.; Leboeuf, M.; Li, X.-M.; Mucida, D.; et al. Crosstalk between Muscularis Macrophages and Enteric Neurons Regulates Gastrointestinal Motility. Cell 2014, 158, 1210. [Google Scholar] [CrossRef] [PubMed]
- Geuking, M.B.; Köller, Y.; Rupp, S.; McCoy, K.D. The Interplay between the Gut Microbiota and the Immune System. Gut Microbes 2014, 5, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Demir, I.E.; Schäfer, K.-H.; Tieftrunk, E.; Friess, H.; Ceyhan, G.O. Neural Plasticity in the Gastrointestinal Tract: Chronic Inflammation, Neurotrophic Signals, and Hypersensitivity. Acta Neuropathol. 2013, 125, 491–509. [Google Scholar] [CrossRef] [PubMed]
- Niesler, B.; Kuerten, S.; Demir, I.E.; Schäfer, K.-H. Disorders of the Enteric Nervous System—A Holistic View. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 393–410. [Google Scholar] [CrossRef] [PubMed]
- Palus, K.; Bulc, M.; Całka, J.; Zielonka, Ł.; Nowicki, M. Diabetes Affects the Pituitary Adenylate Cyclase-Activating Polypeptide (PACAP)-Like Immunoreactive Enteric Neurons in the Porcine Digestive Tract. Int. J. Mol. Sci. 2021, 22, 5727. [Google Scholar] [CrossRef] [PubMed]
- Marrinan, S.; Emmanuel, A.V.; Burn, D.J. Delayed Gastric Emptying in Parkinson’s Disease. Mov. Disord. 2014, 29, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Hawkes, C.H.; Del Tredici, K.; Braak, H. Parkinson’s Disease: A Dual-hit Hypothesis. Neuropathol. Appl. Neurobiol. 2007, 33, 599–614. [Google Scholar] [CrossRef]
- Gries, M.; Christmann, A.; Schulte, S.; Weyland, M.; Rommel, S.; Martin, M.; Baller, M.; Röth, R.; Schmitteckert, S.; Unger, M.; et al. Parkinson Mice Show Functional and Molecular Changes in the Gut Long before Motoric Disease Onset. Mol. Neurodegener. 2021, 16, 34. [Google Scholar] [CrossRef]
- Schäfer, K.; Christmann, A.; Gries, M. Can We Trust the Gut? The Role of the Intestine in Neurodegeneration. J. Physiol. 2020, 598, 4141–4142. [Google Scholar] [CrossRef] [PubMed]
- Meffert, M.K.; Chang, J.M.; Wiltgen, B.J.; Fanselow, M.S.; Baltimore, D. NF-ΚB Functions in Synaptic Signaling and Behavior. Nat. Neurosci. 2003, 6, 1072–1078. [Google Scholar] [CrossRef] [PubMed]
- Karin, M. Nuclear Factor-ΚB in Cancer Development and Progression. Nature 2006, 441, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Perkins, N.D. Integrating Cell-Signalling Pathways with NF-ΚB and IKK Function. Nat. Rev. Mol. Cell Biol. 2007, 8, 49–62. [Google Scholar] [CrossRef] [PubMed]
- Tapia, M.A.; González-Navarrete, I.; Dalmases, A.; Bosch, M.; Rodriguez-Fanjul, V.; Rolfe, M.; Ross, J.S.; Mezquita, J.; Mezquita, C.; Bachs, O.; et al. Inhibition of the Canonical IKK/NFkappaB Pathway Sensitizes Human Cancer Cells to Doxorubicin. Cell Cycle 2007, 6, 2284–2292. [Google Scholar] [CrossRef] [PubMed]
- Simmons, L.J.; Surles-Zeigler, M.C.; Li, Y.; Ford, G.D.; Newman, G.D.; Ford, B.D. Regulation of Inflammatory Responses by Neuregulin-1 in Brain Ischemia and Microglial Cells in Vitro Involves the NF-Kappa B Pathway. J. Neuroinflammation 2016, 13, 237. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Zhang, L.; Joo, D.; Sun, S.-C. NF-ΚB Signaling in Inflammation. Signal Transduct. Target. Ther. 2017, 2, 17023. [Google Scholar] [CrossRef] [PubMed]
- Mémet, S. NF-ΚB Functions in the Nervous System: From Development to Disease. Biochem. Pharmacol. 2006, 72, 1180–1195. [Google Scholar] [CrossRef]
- Zhang, Y.; Hu, W. NFκB Signaling Regulates Embryonic and Adult Neurogenesis. Front. Biol. 2012, 7, 277–291. [Google Scholar] [CrossRef]
- Dresselhaus, E.C.; Meffert, M.K. Cellular Specificity of NF-ΚB Function in the Nervous System. Front. Immunol. 2019, 10, 1043. [Google Scholar] [CrossRef]
- Camandola, S.; Mattson, M.P. NF-ΚB as a Therapeutic Target in Neurodegenerative Diseases. Expert Opin. Ther. Targets 2007, 11, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Flood, P.M.; Qian, L.; Peterson, L.J.; Zhang, F.; Shi, J.-S.; Gao, H.-M.; Hong, J.-S. Transcriptional Factor NF-KB as a Target for Therapy in Parkinson’s Disease. Park. Dis. 2011, 2011, 216298. [Google Scholar] [CrossRef]
- Jha, N.K.; Jha, S.K.; Kar, R.; Nand, P.; Swati, K.; Goswami, V.K. Nuclear Factor-kappa β as a Therapeutic Target for Alzheimer’s Disease. J. Neurochem. 2019, 150, 113–137. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.-C. The Non-Canonical NF-ΚB Pathway in Immunity and Inflammation. Nat. Rev. Immunol. 2017, 17, 545–558. [Google Scholar] [CrossRef] [PubMed]
- Burgueño, J.F.; Barba, A.; Eyre, E.; Romero, C.; Neunlist, M.; Fernández, E. TLR2 and TLR9 Modulate Enteric Nervous System Inflammatory Responses to Lipopolysaccharide. J. Neuroinflammation 2016, 13, 187. [Google Scholar] [CrossRef] [PubMed]
- Sochocka, M.; Diniz, B.S.; Leszek, J. Inflammatory Response in the CNS: Friend or Foe? Mol. Neurobiol. 2017, 54, 8071–8089. [Google Scholar] [CrossRef] [PubMed]
- Di Liddo, R.; Bertalot, T.; Schuster, A.; Schrenk, S.; Tasso, A.; Zanusso, I.; Conconi, M.; Schäfer, K. Anti-Inflammatory Activity of Wnt Signaling in Enteric Nervous System: In Vitro Preliminary Evidences in Rat Primary Cultures. J. Neuroinflammation 2015, 12, 23. [Google Scholar] [CrossRef] [PubMed]
- Di Liddo, R.; Bertalot, T.; Schuster, A.; Schrenk, S.; Müller, O.; Apfel, J.; Reischmann, P.; Rajendran, S.; Sfriso, R.; Gasparella, M.; et al. Fluorescence-Based Gene Reporter Plasmid to Track Canonical Wnt Signaling in ENS Inflammation. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 310, G337–G346. [Google Scholar] [CrossRef]
- Schuster, A.; Klotz, M.; Schwab, T.; Di Liddo, R.; Bertalot, T.; Schrenk, S.; Martin, M.; Nguyen, T.D.; Nguyen, T.N.Q.; Gries, M.; et al. Maintenance of the Enteric Stem Cell Niche by Bacterial Lipopolysaccharides? Evidence and Perspectives. J. Cell. Mol. Med. 2014, 18, 1429–1443. [Google Scholar] [CrossRef]
- von Boyen, G.B.T. Proinflammatory Cytokines Increase Glial Fibrillary Acidic Protein Expression in Enteric Glia. Gut 2004, 53, 222–228. [Google Scholar] [CrossRef]
- Chen, M.; Reed, R.R.; Lane, A.P. Acute Inflammation Regulates Neuroregeneration through the NF-ΚB Pathway in Olfactory Epithelium. Proc. Natl. Acad. Sci. USA 2017, 114, 8089–8094. [Google Scholar] [CrossRef] [PubMed]
- Yi, B.; Hu, X.; Zhang, H.; Huang, J.; Liu, J.; Hu, J.; Li, W.; Huang, L. Nuclear NF-ΚB P65 in Peripheral Blood Mononuclear Cells Correlates with Urinary MCP-1, RANTES and the Severity of Type 2 Diabetic Nephropathy. PLoS ONE 2014, 9, e99633. [Google Scholar] [CrossRef] [PubMed]
- Frigo, D.E.; McDonnell, D.P. Differential Effects of Prostate Cancer Therapeutics on Neuroendocrine Transdifferentiation. Mol. Cancer Ther. 2008, 7, 659–669. [Google Scholar] [CrossRef] [PubMed]
- Böttner, M.; Bär, F.; Von Koschitzky, H.; Tafazzoli, K.; Roblick, U.J.; Bruch, H.P.; Wedel, T. Laser Microdissection as a New Tool to Investigate Site-Specific Gene Expression in Enteric Ganglia of the Human Intestine. Neurogastroenterol. Motil. 2010, 22, 168-e52. [Google Scholar] [CrossRef] [PubMed]
- Kramer, F.; Stöver, T.; Warnecke, A.; Diensthuber, M.; Lenarz, T.; Wissel, K. BDNF MRNA Expression Is Significantly Upregulated in Vestibular Schwannomas and Correlates with Proliferative Activity. J. Neurooncol. 2010, 98, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Metzger, M.; Bareiss, P.M.; Danker, T.; Wagner, S.; Hennenlotter, J.; Guenther, E.; Obermayr, F.; Stenzl, A.; Koenigsrainer, A.; Skutella, T.; et al. Expansion and Differentiation of Neural Progenitors Derived From the Human Adult Enteric Nervous System. Gastroenterology 2009, 137, 2063–2073.e4. [Google Scholar] [CrossRef] [PubMed]
- Le, F.; Zhang, J.-Y.; Liu, W.; Huang, X.-M.; Luo, W.-Z. The Levels of NF-ΚB P50 and NF-ΚB P65 Play a Role in Thyroid Carcinoma Malignancy in Vivo. J. Int. Med. Res. 2018, 46, 4092–4099. [Google Scholar] [CrossRef]
- Hosaka, Y.; Kirisawa, R.; Ueda, H.; Yamaguchi, M.; Takehana, K. Differences in Tumor Necrosis Factor (TNF).ALPHA. and TNF Receptor-1-Mediated Intracellular Signaling Factors in Normal, Inflamed and Scar-Formed Horse Tendons. J. Vet. Med. Sci. 2005, 67, 985–991. [Google Scholar] [CrossRef] [PubMed]
- Song, Z.; Yao, C.; Yin, J.; Tong, C.; Zhu, D.; Sun, Z.; Jiang, J.; Shao, M.; Zhang, Y.; Deng, Z.; et al. Genetic Variation in the TNF Receptor-Associated Factor 6 Gene Is Associated with Susceptibility to Sepsis-Induced Acute Lung Injury. J. Transl. Med. 2012, 10, 166. [Google Scholar] [CrossRef]
- Li, F.; Li, F.; Chen, W. Propofol Inhibits Cell Proliferation, Migration, and Invasion via Mir-410-3p/Transforming Growth Factor-β Receptor Type 2 (TGFBR2) Axis in Glioma. Med. Sci. Monit. 2020, 26, e919523. [Google Scholar] [CrossRef]
- El Hadi, H.; Abdellaoui-Maane, I.; Kottwitz, D.; El Amrani, M.; Bouchoutrouch, N.; Qmichou, Z.; Karkouri, M.; ElAttar, H.; Errihani, H.; Fernandez, P.L.; et al. Development and Evaluation of a Novel RT-QPCR Based Test for the Quantification of ERBB2 Gene Expression in Breast Cancer. Gene 2017, 605, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Kawano, O.; Sasaki, H.; Endo, K.; Suzuki, E.; Haneda, H.; Yukiue, H.; Kobayashi, Y.; Yano, M.; Fujii, Y. ErbB3 MRNA Expression Correlated with Specific Clinicopathologic Features of Japanese Lung Cancers. J. Surg. Res. 2008, 146, 43–48. [Google Scholar] [CrossRef]
- Hagl, C.I.; Wink, E.; Weiss, C.; Wessel, L.; Gretz, N.; Schäfer, K.H. Enteric Neurons from Postnatal Fgf2 Knockout Mice Differ in Neurite Outgrowth Responses. Auton. Neurosci. 2012, 170, 56–61. [Google Scholar] [CrossRef]
- Le, T.-L.; Galmiche, L.; Levy, J.; Suwannarat, P.; Hellebrekers, D.M.E.I.; Morarach, K.; Boismoreau, F.; Theunissen, T.E.J.; Lefebvre, M.; Pelet, A.; et al. Dysregulation of the NRG1/ERBB Pathway Causes a Developmental Disorder with Gastrointestinal Dysmotility in Humans. J. Clin. Investig. 2021, 131, e145837. [Google Scholar] [CrossRef]
- Ohgami, N.; Ida-Eto, M.; Shimotake, T.; Sakashita, N.; Sone, M.; Nakashima, T.; Tabuchi, K.; Hoshino, T.; Shimada, A.; Tsuzuki, T.; et al. C-Ret–Mediated Hearing Loss in Mice with Hirschsprung Disease. Proc. Natl. Acad. Sci. USA 2010, 107, 13051–13056. [Google Scholar] [CrossRef] [PubMed]
- Poirier, A.-A.; Côté, M.; Bourque, M.; Morissette, M.; Di Paolo, T.; Soulet, D. Neuroprotective and Immunomodulatory Effects of Raloxifene in the Myenteric Plexus of a Mouse Model of Parkinson’s Disease. Neurobiol. Aging 2016, 48, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Meng, X.; Zhang, H.; Feng, C.; Wang, B.; Li, N.; Abdullahi, K.M.; Wu, X.; Yang, J.; Li, Z.; et al. Intestinal Proinflammatory Macrophages Induce a Phenotypic Switch in Interstitial Cells of Cajal. J. Clin. Investig. 2020, 130, 6443–6456. [Google Scholar] [CrossRef]
- Gao, Y.; Tang, Y.; Zhang, H.; Chu, X.; Yan, B.; Li, J.; Liu, C. Vincristine Leads to Colonic Myenteric Neurons Injury via Pro-Inflammatory Macrophages Activation. Biochem. Pharmacol. 2021, 186, 114479. [Google Scholar] [CrossRef]
- Gosain, A.; Brinkman, A.S. Hirschsprung’s Associated Enterocolitis. Curr. Opin. Pediatr. 2015, 27, 364–369. [Google Scholar] [CrossRef]
- Schreiber, D.; Klotz, M.; Laures, K.; Clasohm, J.; Bischof, M.; Schäfer, K.-H. The Mesenterially Perfused Rat Small Intestine: A Versatile Approach for Pharmacological Testings. Ann. Anat. Anat. Anz. 2014, 196, 158–166. [Google Scholar] [CrossRef]
- Farro, G.; Gomez-Pinilla, P.J.; Di Giovangiulio, M.; Stakenborg, N.; Auteri, M.; Thijs, T.; Depoortere, I.; Matteoli, G.; Boeckxstaens, G.E. Smooth Muscle and Neural Dysfunction Contribute to Different Phases of Murine Postoperative Ileus. Neurogastroenterol. Motil. 2016, 28, 934–947. [Google Scholar] [CrossRef] [PubMed]
- Costa, D.V.S.; Bon-Frauches, A.C.; Silva, A.M.H.P.; Lima-Júnior, R.C.P.; Martins, C.S.; Leitão, R.F.C.; Freitas, G.B.; Castelucci, P.; Bolick, D.T.; Guerrant, R.L.; et al. 5-Fluorouracil Induces Enteric Neuron Death and Glial Activation During Intestinal Mucositis via a S100B-RAGE-NFκB-Dependent Pathway. Sci. Rep. 2019, 9, 665. [Google Scholar] [CrossRef] [PubMed]
- Domingo-Domènech, J.; Pippa, R.; Tápia, M.; Gascón, P.; Bachs, O.; Bosch, M. Inactivation of NF-ΚB by Proteasome Inhibition Contributes to Increased Apoptosis Induced by Histone Deacetylase Inhibitors in Human Breast Cancer Cells. Breast Cancer Res. Treat. 2008, 112, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Ramadass, V.; Vaiyapuri, T.; Tergaonkar, V. Small Molecule NF-ΚB Pathway Inhibitors in Clinic. Int. J. Mol. Sci. 2020, 21, 5164. [Google Scholar] [CrossRef] [PubMed]
- Verzella, D.; Cornice, J.; Arboretto, P.; Vecchiotti, D.; Di Vito Nolfi, M.; Capece, D.; Zazzeroni, F.; Franzoso, G. The NF-ΚB Pharmacopeia: Novel Strategies to Subdue an Intractable Target. Biomedicines 2022, 10, 2233. [Google Scholar] [CrossRef] [PubMed]
- Dekamin, S.; Ghasemi, M.; Dehpour, A.R.; Ghazi-Khansari, M.; Shafaroodi, H. Protective Effects of Glatiramer Acetate Against Paclitaxel-Induced Peripheral Neuropathy in Rats: A Role for Inflammatory Cytokines and Oxidative Stress. Neurochem. Res. 2024, 49, 1049–1060. [Google Scholar] [CrossRef]
- Chen, L.; Du, Y.; Qiao, H.; Yang, L.; Zhang, P.; Wang, J.; Zhang, C.; Jiang, W.; Xu, R.; Zhang, X. Proprotein Convertase Subtilisin/Kexin Type 9 Inhibitor Ameliorates Cerebral Ischemia in Mice by Inhibiting Inflammation. J. Stroke Cerebrovasc. Dis. 2024, 33, 107517. [Google Scholar] [CrossRef]
- Wang, J.; Akbari, A.; Chardahcherik, M.; Wu, J. Ginger (Zingiber Officinale Roscoe) Ameliorates Ethanol-Induced Cognitive Impairment by Modulating NMDA and GABA-A Receptors in Rat Hippocampus. Metab. Brain Dis. 2023, 39, 67–76. [Google Scholar] [CrossRef]
- Zhao, T.; Jia, J. Polygalacic Acid Attenuates Cognitive Impairment by Regulating Inflammation through PPARγ/NF-κB Signaling Pathway. CNS Neurosci. Ther. 2024, 30, e14581. [Google Scholar] [CrossRef]
- Vasudevan Sajini, D.; Thaggikuppe Krishnamurthy, P.; Chakkittukandiyil, A.; Mudavath, R.N. Orientin Modulates Nrf2-ARE, PI3K/Akt, JNK-ERK1/2, and TLR4/NF-KB Pathways to Produce Neuroprotective Benefits in Parkinson’s Disease. Neurochem. Res. 2024, 49, 1577–1587. [Google Scholar] [CrossRef]
- Baj, T.; Seth, R. Role of Curcumin in Regulation of TNF-α Mediated Brain Inflammatory Responses. Recent Pat. Inflamm. Allergy Drug Discov. 2018, 12, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zheng, Y.; Luo, Y.; Du, Y.; Zhang, X.; Fu, J. Curcumin Inhibits LPS-Induced Neuroinflammation by Promoting Microglial M2 Polarization via TREM2/TLR4/NF-ΚB Pathways in BV2 Cells. Mol. Immunol. 2019, 116, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Li, M.; Kang, N.; Jin, W.; Xiao, Y.; Li, Z.; Qi, Q.; Zhang, J.; Duan, Y.; Feng, X.; et al. Baicalein Ameliorates Cognitive Impairment of Vascular Dementia Rats via Suppressing Neuroinflammation and Regulating Intestinal Microbiota. Brain Res. Bull. 2024, 208, 110888. [Google Scholar] [CrossRef] [PubMed]

| Gene Name | Forward Primers Sequence 5′ → 3′ | Reverse Primers Sequence 5′ → 3′ | References |
|---|---|---|---|
| hGAPDH | GCACCGTCAAGGCTGAGAAC | TGGTGAAGACGCCAGTGGA | [42] |
| hTUBB3 | GCCTCTTCTCACAAGTACGTG | CCCCACTCTGACCAAAGATGAA | [43] |
| hPGP9.5 | AAGGCCAATGTCGGGTAGATG | CGGAAAAGGCATTCGTCCAT | [44] |
| hGDNF | CACTGACTTGGGTCTGGGCTATGA | GTCTGCAACATGCCTGCCCTACTT | [45] |
| hRET | AGATTTCGGATTTCGGCTTGT | CCACAGCAGGACACCAAAAGA | [46] |
| hRELA | ATC CCA TCT TTG ACA ATCGTGC | CTG GTC CCG TGA AAT ACA CCT C | [42] |
| hNF-KB1 | TGG ACA GCA AAT CCG CCC TG | TGT TGT AAT GAG TCG TCA TCC T | [47] |
| hNFKBIA | ATT CAC AGA GGA TGA GCT GCCC | TCCACATTCTTTTTGCCACTTTCC A | [41] |
| hTNFA | AGC CCA TGT TGT AGC AAA CC | GTT GGG CTG ATT GAT CTC AGC | [48] |
| hTRAF6 | AGG GAC CCA GCT TTC TTT GT | GCC AAG TGA TTC CTC TGC AT | [49] |
| hTGFB2 | CCA TCC CGC CCA CTT TCT AC | AGC TCA ATC CGT TGT TCA GGC | |
| hTGFBR2 | CTA ACC TGC TGC CTG TGT GA | TCT GGA GCC ATG TAT CTT GC | [50] |
| hERBB2 | AAT GCC AGG CAC TGT TTG | GTC CTT ATA GTG GGC ACA GG | [51] |
| hERBB3 | AAG CTC TAC GAG AGG TGT GA | TGG GCA ATG GTA GAG TAG AG | [52] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elkrewi, E.Z.; Al Abdulqader, A.A.; Khasanov, R.; Maas-Omlor, S.; Boettcher, M.; Wessel, L.M.; Schäfer, K.-H.; Tapia-Laliena, M.Á. Role of Inflammation and the NF-κB Signaling Pathway in Hirschsprung’s Disease. Biomolecules 2024, 14, 992. https://doi.org/10.3390/biom14080992
Elkrewi EZ, Al Abdulqader AA, Khasanov R, Maas-Omlor S, Boettcher M, Wessel LM, Schäfer K-H, Tapia-Laliena MÁ. Role of Inflammation and the NF-κB Signaling Pathway in Hirschsprung’s Disease. Biomolecules. 2024; 14(8):992. https://doi.org/10.3390/biom14080992
Chicago/Turabian StyleElkrewi, Enas Zoheer, Ahmad A. Al Abdulqader, Rasul Khasanov, Silke Maas-Omlor, Michael Boettcher, Lucas M. Wessel, Karl-Herbert Schäfer, and María Ángeles Tapia-Laliena. 2024. "Role of Inflammation and the NF-κB Signaling Pathway in Hirschsprung’s Disease" Biomolecules 14, no. 8: 992. https://doi.org/10.3390/biom14080992






