The Biological Mechanisms and Clinical Roles of RNA-Binding Proteins in Cardiovascular Diseases
Abstract
1. Introduction
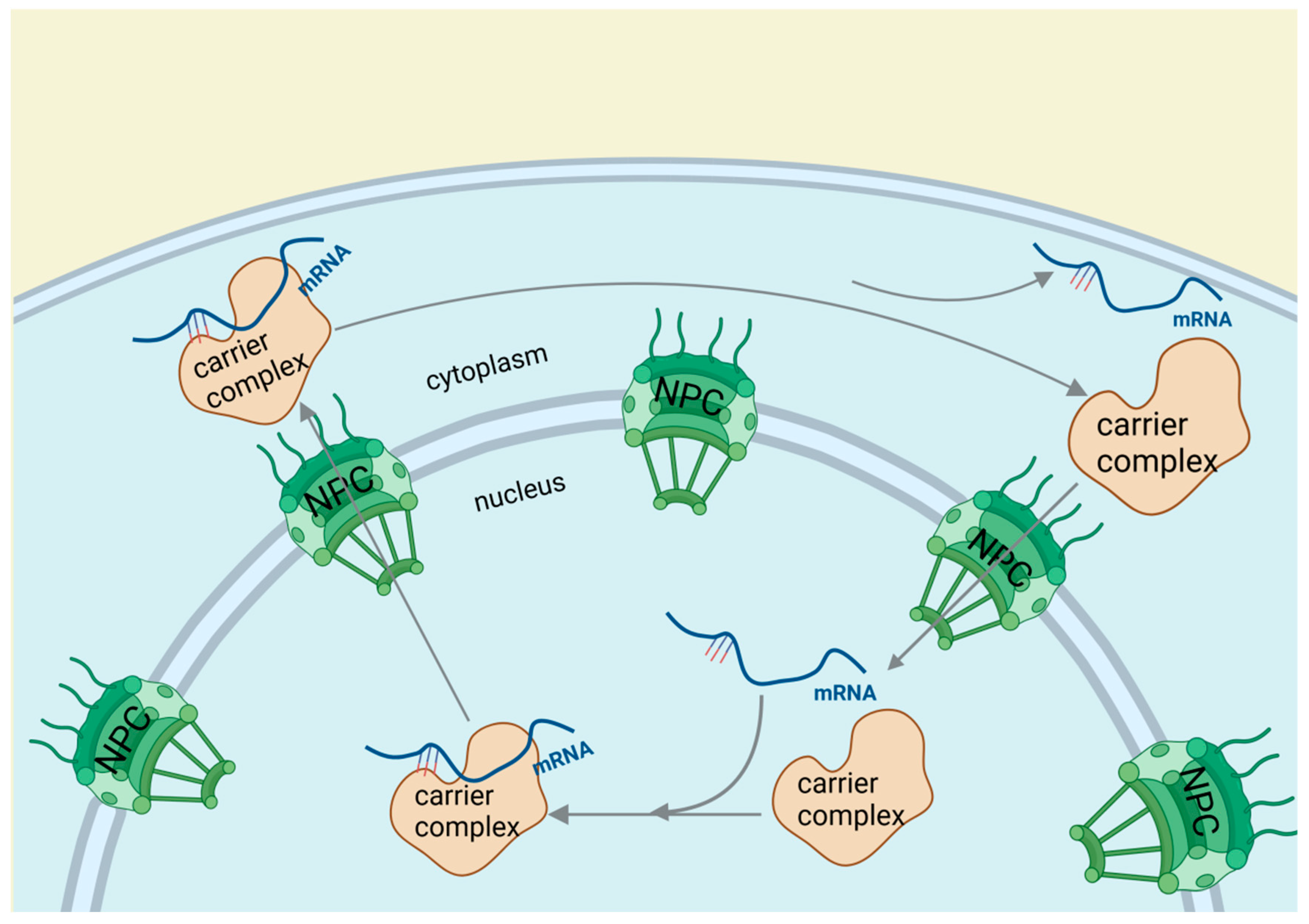
2. Function of RNA-Binding Proteins in Cardiovascular Biology through RNA Regulation
2.1. RNA-Binding Proteins Affect Cardiovascular Diseases through Polyadenylation
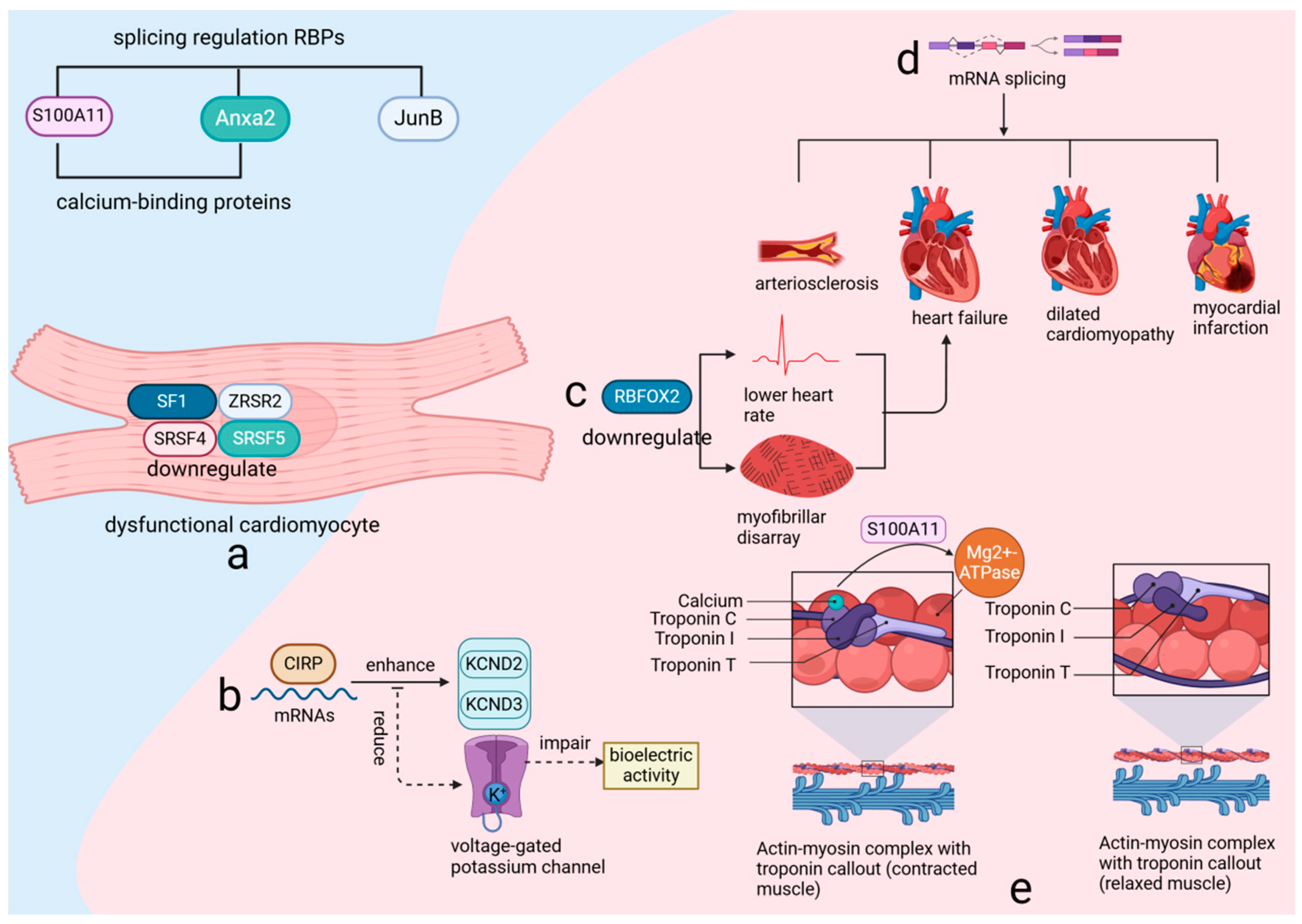
2.2. RNA-Binding Proteins Influence Cardiovascular Diseases by Regulating RNA Alternative Splicing
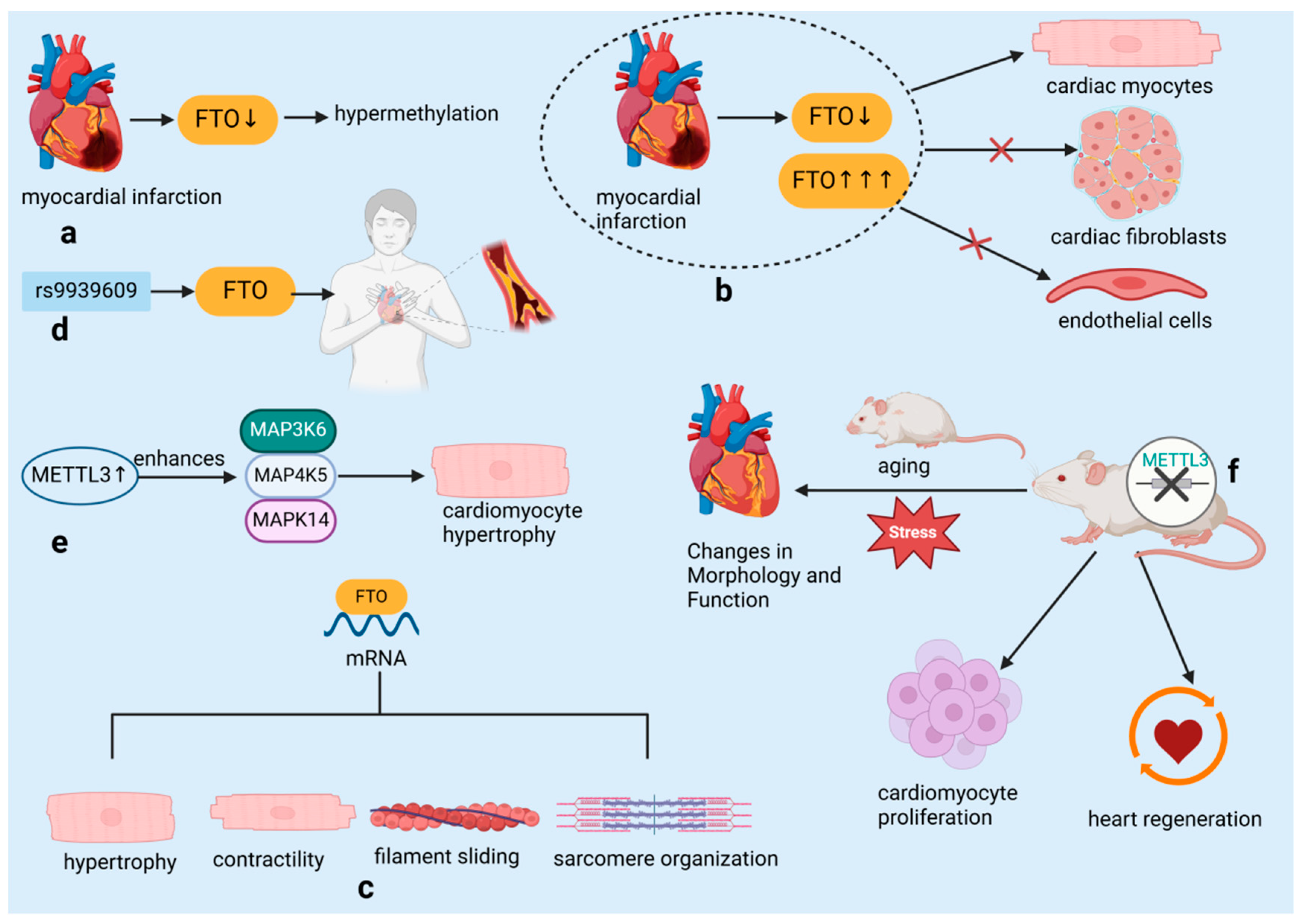
2.3. RNA-Binding Proteins Influence Cardiovascular Diseases by Regulating RNA Modification
2.4. RNA-Binding Proteins Affect Cardiovascular Diseases through RNA Editing
3. The Role of RNA-Binding Proteins in Cardiovascular Diseases
3.1. The Role of RNA-Binding Proteins in Heart Muscle Injury
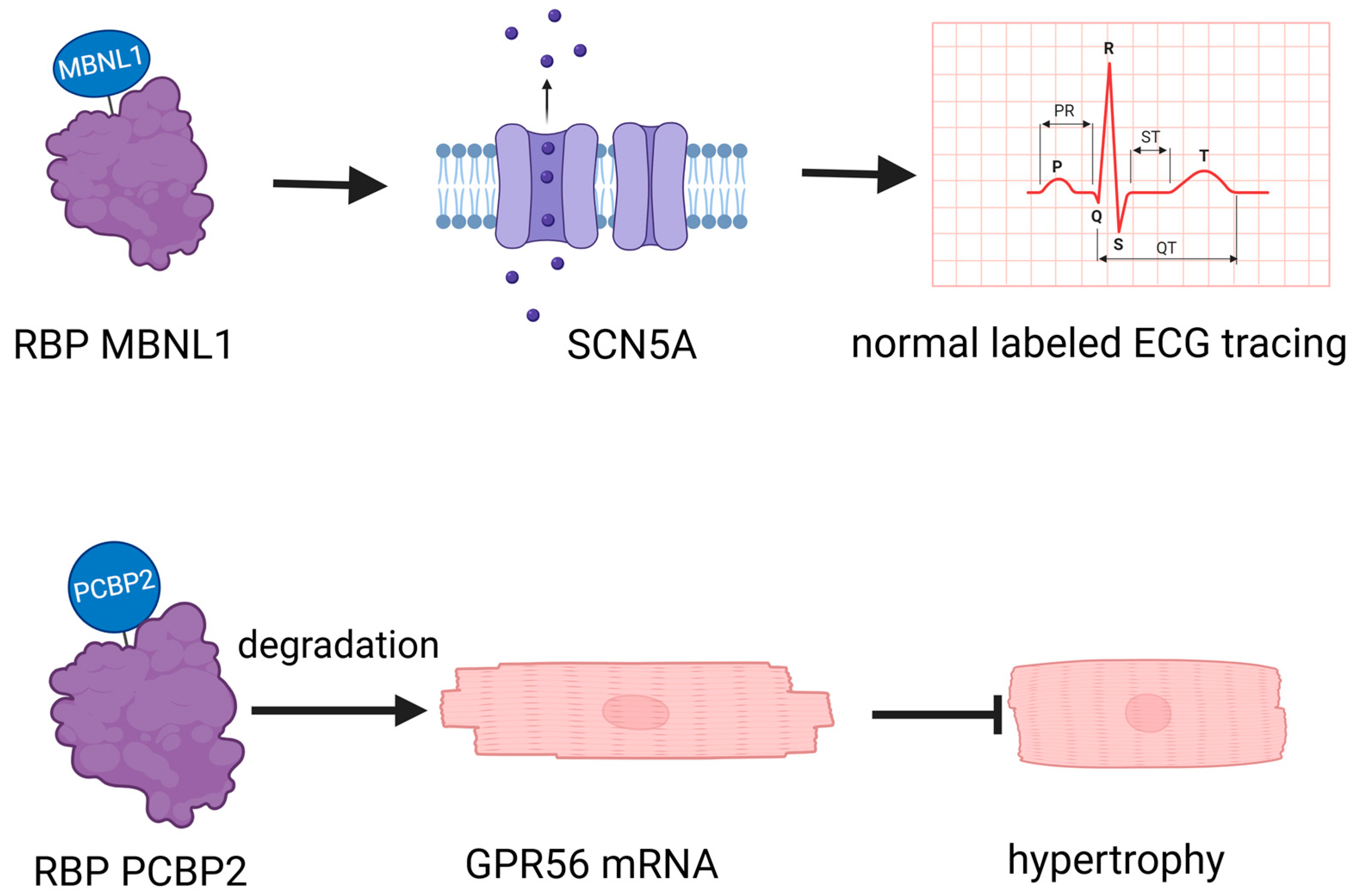
3.2. The Relationship between Arrhythmias and RNA-Binding Proteins
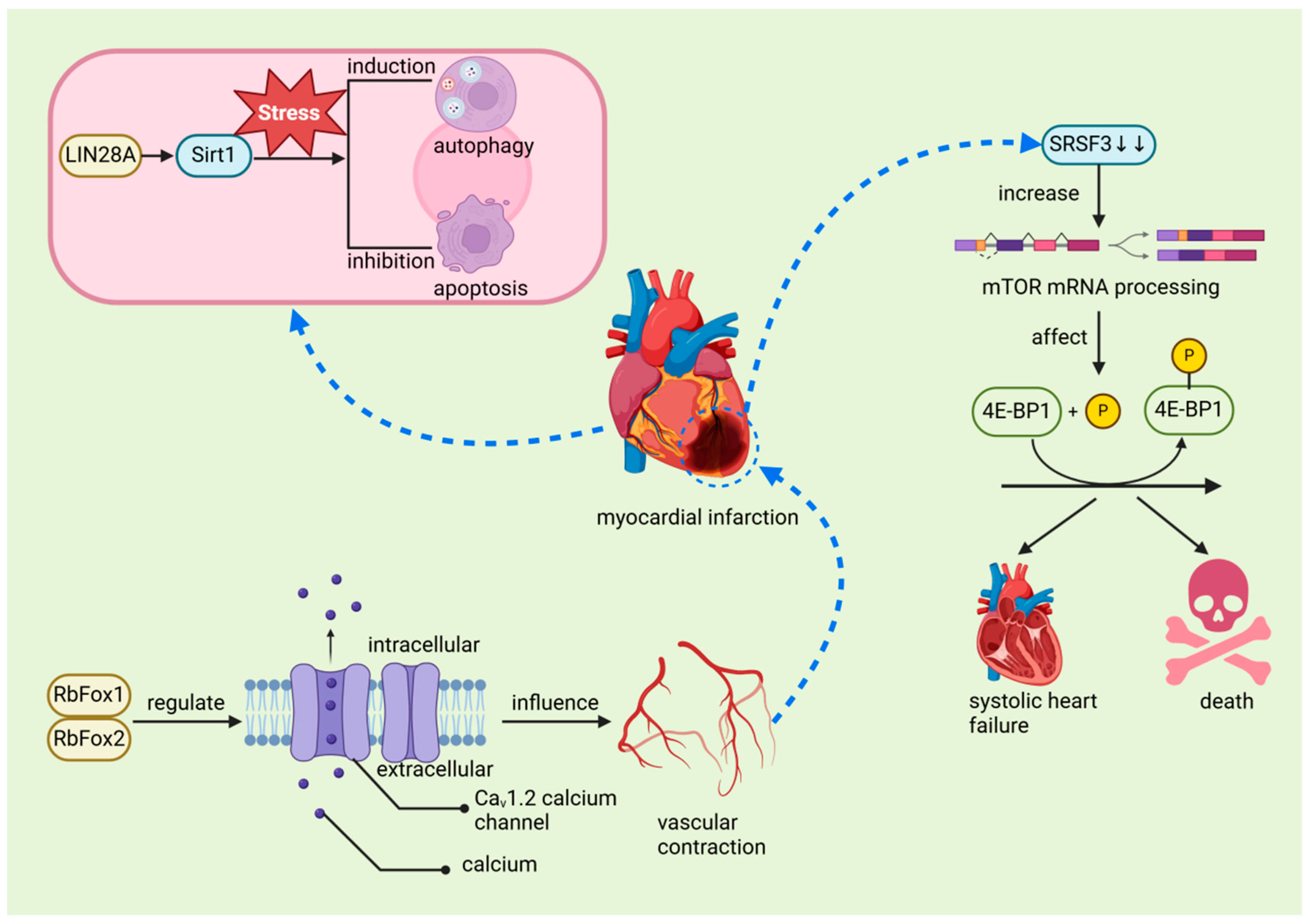
3.3. The Relationship between Myocardial Infarction and RNA-Binding Proteins
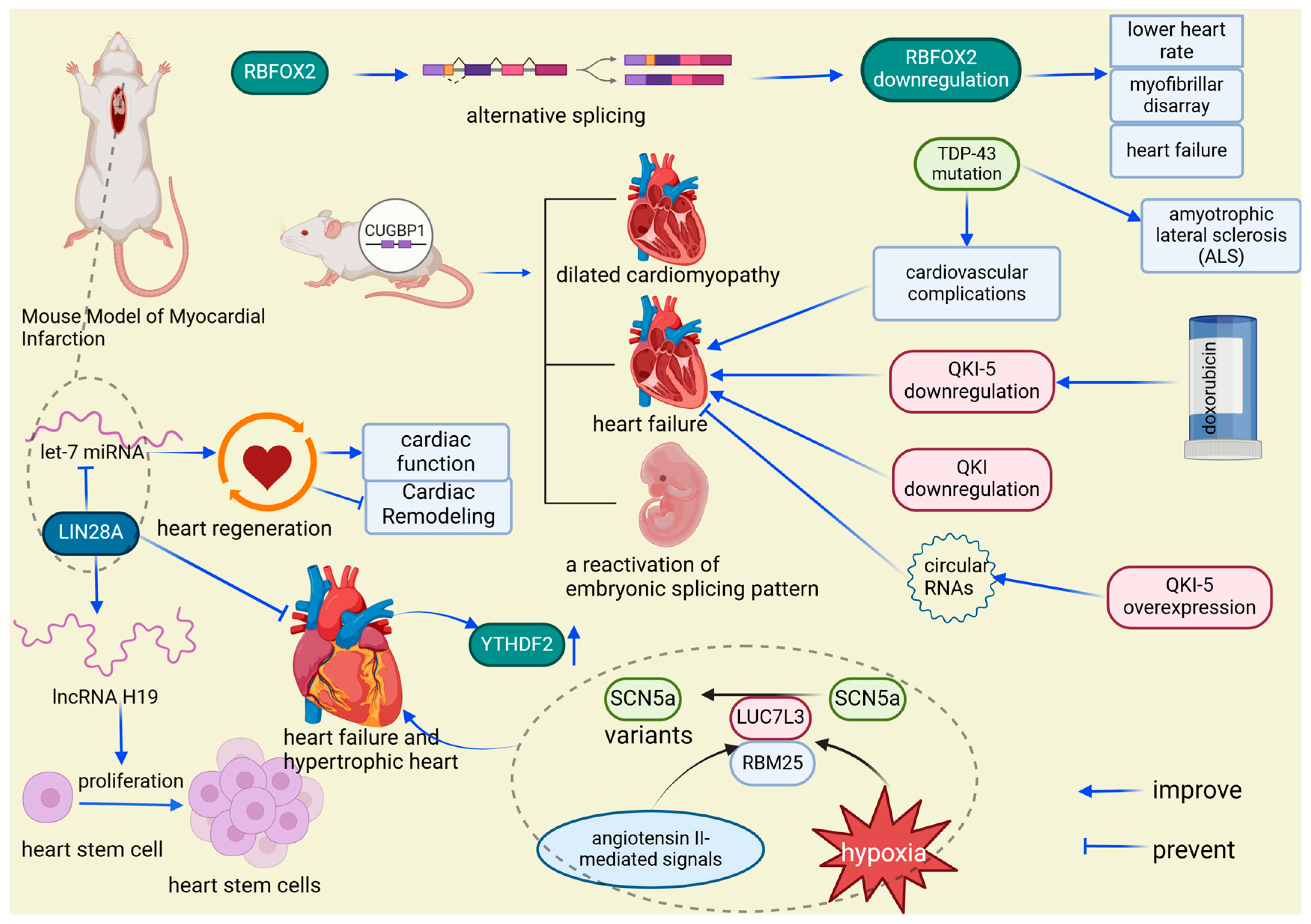
3.4. The Interaction between Heart Failure and RNA-Binding Proteins
4. Therapeutic Potential and Clinical Progress of RBPs in Cardiovascular Disease
5. Discussion
6. Conclusions and Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bansal, P.; Arora, M. RNA Binding Proteins and Non-coding RNA’s in Cardiovascular Diseases. Adv. Exp. Med. Biol. 2020, 1229, 105–118. [Google Scholar] [CrossRef]
- Ruffenach, G.; Medzikovic, L.; Sun, W.; Hong, J.; Eghbali, M. Functions of RNA-Binding Proteins in Cardiovascular Disease. Cells 2023, 12, 2794. [Google Scholar] [CrossRef] [PubMed]
- Medzikovic, L.; Azem, T.; Sun, W.; Rejali, P.; Esdin, L.; Rahman, S.; Dehghanitafti, A.; Aryan, L.; Eghbali, M. Sex Differences in Therapies against Myocardial Ischemia-Reperfusion Injury: From Basic Science to Clinical Perspectives. Cells 2023, 12, 2077. [Google Scholar] [CrossRef]
- Blech-Hermoni, Y.; Ladd, A.N. RNA binding proteins in the regulation of heart development. Int. J. Biochem. Cell Biol. 2013, 45, 2467–2478. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.K.; Kuyumcu-Martinez, M.N. RNA binding proteins in cardiovascular development and disease. Curr. Top. Dev. Biol. 2024, 156, 51–119. [Google Scholar] [CrossRef]
- Hentze, M.W.; Castello, A.; Schwarzl, T.; Preiss, T. A brave new world of RNA-binding proteins. Nat. Rev. Mol. Cell Biol. 2018, 19, 327–341. [Google Scholar] [CrossRef] [PubMed]
- Gan, P.; Wang, Z.; Bezprozvannaya, S.; McAnally, J.R.; Tan, W.; Li, H.; Bassel-Duby, R.; Liu, N.; Olson, E.N. RBPMS regulates cardiomyocyte contraction and cardiac function through RNA alternative splicing. Cardiovasc. Res. 2024, 120, 56–68. [Google Scholar] [CrossRef] [PubMed]
- Treiber, T.; Treiber, N.; Plessmann, U.; Harlander, S.; Daiß, J.L.; Eichner, N.; Lehmann, G.; Schall, K.; Urlaub, H.; Meister, G. A Compendium of RNA-Binding Proteins that Regulate MicroRNA Biogenesis. Mol. Cell 2017, 66, 270–284.e213. [Google Scholar] [CrossRef]
- Yao, Z.T.; Yang, Y.M.; Sun, M.M.; He, Y.; Liao, L.; Chen, K.S.; Li, B. New insights into the interplay between long non-coding RNAs and RNA-binding proteins in cancer. Cancer Commun. 2022, 42, 117–140. [Google Scholar] [CrossRef]
- Golubeva, V.A.; Das, A.S.; Rabolli, C.P.; Dorn, L.E.; van Berlo, J.H.; Accornero, F. YTHDF1 is pivotal for maintenance of cardiac homeostasis. J. Mol. Cell Cardiol. 2024, 193, 25–35. [Google Scholar] [CrossRef]
- Ding, Y.; Yin, R.; Zhang, S.; Xiao, Q.; Zhao, H.; Pan, X.; Zhu, X. The Combined Regulation of Long Non-coding RNA and RNA-Binding Proteins in Atherosclerosis. Front. Cardiovasc. Med. 2021, 8, 731958. [Google Scholar] [CrossRef] [PubMed]
- Gerstberger, S.; Hafner, M.; Tuschl, T. A census of human RNA-binding proteins. Nat. Rev. Genet. 2014, 15, 829–845. [Google Scholar] [CrossRef] [PubMed]
- Corley, M.; Burns, M.C.; Yeo, G.W. How RNA-Binding Proteins Interact with RNA: Molecules and Mechanisms. Mol. Cell 2020, 78, 9–29. [Google Scholar] [CrossRef] [PubMed]
- Shi, D.L. RNA-Binding Proteins as Critical Post-Transcriptional Regulators of Cardiac Regeneration. Int. J. Mol. Sci. 2023, 24, 12004. [Google Scholar] [CrossRef] [PubMed]
- Freyermuth, F.; Rau, F.; Kokunai, Y.; Linke, T.; Sellier, C.; Nakamori, M.; Kino, Y.; Arandel, L.; Jollet, A.; Thibault, C.; et al. Splicing misregulation of SCN5A contributes to cardiac-conduction delay and heart arrhythmia in myotonic dystrophy. Nat. Commun. 2016, 7, 11067. [Google Scholar] [CrossRef]
- Zhang, Y.; Si, Y.; Ma, N.; Mei, J. The RNA-binding protein PCBP2 inhibits Ang II-induced hypertrophy of cardiomyocytes though promoting GPR56 mRNA degeneration. Biochem. Biophys. Res. Commun. 2015, 464, 679–684. [Google Scholar] [CrossRef]
- Potel, K.N.; Cornelius, V.A.; Yacoub, A.; Chokr, A.; Donaghy, C.L.; Kelaini, S.; Eleftheriadou, M.; Margariti, A. Effects of non-coding RNAs and RNA-binding proteins on mitochondrial dysfunction in diabetic cardiomyopathy. Front. Cardiovasc. Med. 2023, 10, 1165302. [Google Scholar] [CrossRef]
- Cornelius, V.A.; Naderi-Meshkin, H.; Kelaini, S.; Margariti, A. RNA-Binding Proteins: Emerging Therapeutics for Vascular Dysfunction. Cells 2022, 11, 2494. [Google Scholar] [CrossRef]
- Woo, C.C.; Liu, W.; Lin, X.Y.; Dorajoo, R.; Lee, K.W.; Richards, A.M.; Lee, C.N.; Wongsurawat, T.; Nookaew, I.; Sorokin, V. The interaction between 30b-5p miRNA and MBNL1 mRNA is involved in vascular smooth muscle cell differentiation in patients with coronary atherosclerosis. Int. J. Mol. Sci. 2019, 21, 11. [Google Scholar] [CrossRef]
- Verma, S.K.; Deshmukh, V.; Liu, P.; Nutter, C.A.; Espejo, R.; Hung, M.L.; Wang, G.S.; Yeo, G.W.; Kuyumcu-Martinez, M.N. Reactivation of fetal splicing programs in diabetic hearts is mediated by protein kinase C signaling. J. Biol. Chem. 2013, 288, 35372–35386. [Google Scholar] [CrossRef]
- Hoshi, S.; Onagi, A.; Tanji, R.; Honda-Takinami, R.; Matsuoka, K.; Hata, J.; Sato, Y.; Akaihata, H.; Kataoka, M.; Ogawa, S.; et al. Unilateral adrenalectomy for a drug-resistant bilateral primary aldosteronism with heart failure: Pathophysiology and surgical indication. BMC Endocr. Disord. 2023, 23, 243. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, R.; Bishop, K.; Broadbridge, E.; Yu, K.; Carrington, B.; Elkahloun, A.; Zhen, T.; Pei, W.; Burgess, S.M.; Liu, P.; et al. Zrsr2 Is Essential for the Embryonic Development and Splicing of Minor Introns in RNA and Protein Processing Genes in Zebrafish. Int. J. Mol. Sci. 2022, 23, 10668. [Google Scholar] [CrossRef] [PubMed]
- Larrasa-Alonso, J.; Villalba-Orero, M.; Martí-Gómez, C.; Ortiz-Sánchez, P.; López-Olañeta, M.M.; Rey-Martín, M.A.; Sánchez-Cabo, F.; McNicoll, F.; Müller-McNicoll, M.; García-Pavía, P.; et al. The SRSF4-GAS5-Glucocorticoid Receptor Axis Regulates Ventricular Hypertrophy. Circ. Res. 2021, 129, 669–683. [Google Scholar] [CrossRef]
- Fujita, T.; Higashitsuji, H.; Liu, Y.; Itoh, K.; Sakurai, T.; Kojima, T.; Kandori, S.; Nishiyama, H.; Fukumoto, M.; Fukumoto, M.; et al. TRPV4-dependent induction of a novel mammalian cold-inducible protein SRSF5 as well as CIRP and RBM3. Sci. Rep. 2017, 7, 2295. [Google Scholar] [CrossRef]
- Liu, C.; Cheng, X.; Xing, J.; Li, J.; Li, Z.; Jian, D.; Wang, Y.; Wang, S.; Li, R.; Zhang, W.; et al. CIRBP-OGFR axis safeguards against cardiomyocyte apoptosis and cardiotoxicity induced by chemotherapy. Int. J. Biol. Sci. 2022, 18, 2882–2897. [Google Scholar] [CrossRef] [PubMed]
- Wei, C.; Qiu, J.; Zhou, Y.; Xue, Y.; Hu, J.; Ouyang, K.; Banerjee, I.; Zhang, C.; Chen, B.; Li, H.; et al. Repression of the Central Splicing Regulator RBFox2 Is Functionally Linked to Pressure Overload-Induced Heart Failure. Cell Rep. 2015, 10, 1521–1533. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, T.L.; Arribere, J.A.; Geurts, P.A.; Exner, C.R.; McDonald, K.L.; Dill, K.K.; Marr, H.L.; Adkar, S.S.; Garnett, A.T.; Amacher, S.L.; et al. Rbfox-regulated alternative splicing is critical for zebrafish cardiac and skeletal muscle functions. Dev. Biol. 2011, 359, 251–261. [Google Scholar] [CrossRef]
- Mathiyalagan, P.; Adamiak, M.; Mayourian, J.; Sassi, Y.; Liang, Y.; Agarwal, N.; Jha, D.; Zhang, S.; Kohlbrenner, E.; Chepurko, E.; et al. FTO-Dependent N6-Methyladenosine Regulates Cardiac Function during Remodeling and Repair. Circulation 2019, 139, 518–532. [Google Scholar] [CrossRef]
- Dorn, L.E.; Lasman, L.; Chen, J.; Xu, X.; Hund, T.J.; Medvedovic, M.; Hanna, J.H.; van Berlo, J.H.; Accornero, F. The N6-Methyladenosine mRNA Methylase METTL3 Controls Cardiac Homeostasis and Hypertrophy. Circulation 2019, 139, 533–545. [Google Scholar] [CrossRef]
- Minvielle-Sebastia, L.; Keller, W. mRNA polyadenylation and its coupling to other RNA processing reactions and to transcription. Curr. Opin. Cell Biol. 1999, 11, 352–357. [Google Scholar] [CrossRef]
- de Bruin, R.G.; Rabelink, T.J.; van Zonneveld, A.J.; van der Veer, E.P. Emerging roles for RNA-binding proteins as effectors and regulators of cardiovascular disease. Eur. Heart J. 2017, 38, 1380–1388. [Google Scholar] [CrossRef]
- Li, J.; Xie, D.; Huang, J.; Lv, F.; Shi, D.; Liu, Y.; Lin, L.; Geng, L.; Wu, Y.; Liang, D.; et al. Cold-Inducible RNA-Binding Protein Regulates Cardiac Repolarization by Targeting Transient Outward Potassium Channels. Circ. Res. 2015, 116, 1655–1659. [Google Scholar] [CrossRef] [PubMed]
- Hasimbegovic, E.; Schweiger, V.; Kastner, N.; Spannbauer, A.; Traxler, D.; Lukovic, D.; Gyöngyösi, M.; Mester-Tonczar, J. Alternative Splicing in Cardiovascular Disease-A Survey of Recent Findings. Genes 2021, 12, 1457. [Google Scholar] [CrossRef] [PubMed]
- Beqqali, A. Alternative splicing in cardiomyopathy. Biophys. Rev. 2018, 10, 1061–1071. [Google Scholar] [CrossRef] [PubMed]
- Feng, L.; Guo, M.; Jin, C. Identification of alternative splicing and RNA-binding proteins involved in myocardial ischemia-reperfusion injury. Genome 2023, 66, 261–268. [Google Scholar] [CrossRef]
- Nilsen, T.W.; Graveley, B.R. Expansion of the eukaryotic proteome by alternative splicing. Nature 2010, 463, 457–463. [Google Scholar] [CrossRef]
- Chen, M.; Manley, J.L. Mechanisms of alternative splicing regulation: Insights from molecular and genomics approaches. Nat. Rev. Mol. Cell Biol. 2009, 10, 741–754. [Google Scholar] [CrossRef]
- Liu, C.; Mou, S.; Pan, C. The FTO gene rs9939609 polymorphism predicts risk of cardiovascular disease: A systematic review and meta-analysis. PLoS ONE 2013, 8, e71901. [Google Scholar] [CrossRef]
- Hess, M.E.; Hess, S.; Meyer, K.D.; Verhagen, L.A.; Koch, L.; Brönneke, H.S.; Dietrich, M.O.; Jordan, S.D.; Saletore, Y.; Elemento, O.; et al. The fat mass and obesity associated gene (Fto) regulates activity of the dopaminergic midbrain circuitry. Nat. Neurosci. 2013, 16, 1042–1048. [Google Scholar] [CrossRef]
- Wang, X.; Huang, N.; Yang, M.; Wei, D.; Tai, H.; Han, X.; Gong, H.; Zhou, J.; Qin, J.; Wei, X.; et al. FTO is required for myogenesis by positively regulating mTOR-PGC-1α pathway-mediated mitochondria biogenesis. Cell Death Dis. 2017, 8, e2702. [Google Scholar] [CrossRef]
- Su, R.; Dong, L.; Li, C.; Nachtergaele, S.; Wunderlich, M.; Qing, Y.; Deng, X.; Wang, Y.; Weng, X.; Hu, C.; et al. R-2HG Exhibits Anti-tumor Activity by Targeting FTO/m6A/MYC/CEBPA Signaling. Cell 2018, 172, 90–105.e123. [Google Scholar] [CrossRef] [PubMed]
- Jiang, F.Q.; Liu, K.; Chen, J.X.; Cao, Y.; Chen, W.Y.; Zhao, W.L.; Song, G.H.; Liang, C.Q.; Zhou, Y.M.; Huang, H.L.; et al. Mettl3-mediated m6A modification of Fgf16 restricts cardiomyocyte proliferation during heart regeneration. eLife 2022, 11, e77014. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Zhang, S.; Wu, X.; Zhou, X. m6A RNA Methylation in Cardiovascular Diseases. Mol. Ther. 2020, 28, 2111–2119. [Google Scholar] [CrossRef]
- Stellos, K.; Gatsiou, A.; Stamatelopoulos, K.; Perisic Matic, L.; John, D.; Lunella, F.F.; Jaé, N.; Rossbach, O.; Amrhein, C.; Sigala, F.; et al. Adenosine-to-inosine RNA editing controls cathepsin S expression in atherosclerosis by enabling HuR-mediated post-transcriptional regulation. Nat. Med. 2016, 22, 1140–1150. [Google Scholar] [CrossRef]
- Song, J.; Yi, C. Chemical Modifications to RNA: A New Layer of Gene Expression Regulation. ACS Chem. Biol. 2017, 12, 316–325. [Google Scholar] [CrossRef]
- Brennicke, A.; Marchfelder, A.; Binder, S. RNA editing. FEMS Microbiol. Rev. 1999, 23, 297–316. [Google Scholar] [CrossRef]
- Shaw, J.M.; Feagin, J.E.; Stuart, K.; Simpson, L. Editing of kinetoplastid mitochondrial mRNAs by uridine addition and deletion generates conserved amino acid sequences and AUG initiation codons. Cell 1988, 53, 401–411. [Google Scholar] [CrossRef]
- Quinones-Valdez, G.; Tran, S.S.; Jun, H.I.; Bahn, J.H.; Yang, E.W.; Zhan, L.; Brümmer, A.; Wei, X.; Van Nostrand, E.L.; Pratt, G.A.; et al. Regulation of RNA editing by RNA-binding proteins in human cells. Commun. Biol. 2019, 2, 19. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, T.; Ladd, A.N. The importance of CELF control: Molecular and biological roles of the CUG-BP, Elav-like family of RNA-binding proteins. Wiley Interdiscip. Rev. RNA 2012, 3, 104–121. [Google Scholar] [CrossRef]
- Chen, H.Y.; Xiao, Z.Z.; Ling, X.; Xu, R.N.; Zhu, P.; Zheng, S.Y. ELAVL1 is transcriptionally activated by FOXC1 and promotes ferroptosis in myocardial ischemia/reperfusion injury by regulating autophagy. Mol. Med. 2021, 27, 14. [Google Scholar] [CrossRef]
- Tijsen, A.J.; Cócera Ortega, L.; Reckman, Y.J.; Zhang, X.; van der Made, I.; Aufiero, S.; Li, J.; Kamps, S.C.; van den Bout, A.; Devalla, H.D.; et al. Titin Circular RNAs Create a Back-Splice Motif Essential for SRSF10 Splicing. Circulation 2021, 143, 1502–1512. [Google Scholar] [CrossRef] [PubMed]
- Ross, E.A.; Smallie, T.; Ding, Q.; O’Neil, J.D.; Cunliffe, H.E.; Tang, T.; Rosner, D.R.; Klevernic, I.; Morrice, N.A.; Monaco, C.; et al. Dominant Suppression of Inflammation via Targeted Mutation of the mRNA Destabilizing Protein Tristetraprolin. J. Immunol. 2015, 195, 265–276. [Google Scholar] [CrossRef]
- Bohnsack, B.L.; Lai, L.; Northrop, J.L.; Justice, M.J.; Hirschi, K.K. Visceral endoderm function is regulated by quaking and required for vascular development. Genesis 2006, 44, 93–104. [Google Scholar] [CrossRef]
- Caines, R.; Cochrane, A.; Kelaini, S.; Vila-Gonzalez, M.; Yang, C.; Eleftheriadou, M.; Moez, A.; Stitt, A.W.; Zeng, L.; Grieve, D.J.; et al. The RNA-binding protein QKI controls alternative splicing in vascular cells, producing an effective model for therapy. J. Cell Sci. 2019, 132, jcs230276. [Google Scholar] [CrossRef] [PubMed]
- Xie, D.; Geng, L.; Wang, S.; Xiong, K.; Zhao, T.; Wang, G.; Feng, Z.; Lv, F.; Wang, C.; Liang, D.; et al. Cold-inducible RNA-binding protein modulates atrial fibrillation onset by targeting multiple ion channels. Heart Rhythm. 2020, 17, 998–1008. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.; Wu, J.; Li, L.; Song, X.; Xue, J.; Shi, Y.; Zou, Y.; Ma, J.; Ge, J. RBM15 Protects from Myocardial Infarction by Stabilizing NAE1. JACC Basic. Transl. Sci. 2024, 9, 631–648. [Google Scholar] [CrossRef] [PubMed]
- Krumbein, M.; Oberman, F.; Cinnamon, Y.; Golomb, M.; May, D.; Vainer, G.; Belzer, V.; Meir, K.; Fridman, I.; Haybaeck, J.; et al. RNA binding protein IGF2BP2 expression is induced by stress in the heart and mediates dilated cardiomyopathy. Commun. Biol. 2023, 6, 1229. [Google Scholar] [CrossRef]
- Hao, Y.; Lu, Q.; Yang, G.; Ma, A. Lin28a protects against postinfarction myocardial remodeling and dysfunction through Sirt1 activation and autophagy enhancement. Biochem. Biophys. Res. Commun. 2016, 479, 833–840. [Google Scholar] [CrossRef]
- Jung, S.; Ko, S.H.; Ahn, N.; Lee, J.; Park, C.H.; Hwang, J. Role of UPF1-LIN28A interaction during early differentiation of pluripotent stem cells. Nat. Commun. 2024, 15, 158. [Google Scholar] [CrossRef]
- Poore, C.P.; Yang, J.; Wei, S.; Fhu, C.K.; Bichler, Z.; Wang, J.; Soong, T.W.; Liao, P. Enhanced isradipine sensitivity in vascular smooth muscle cells due to hypoxia-induced Cav1.2 splicing and RbFox1/Fox2 downregulation. FEBS J. 2024; epub ahead of print. [Google Scholar] [CrossRef]
- Ortiz-Sánchez, P.; Villalba-Orero, M.; López-Olañeta, M.M.; Larrasa-Alonso, J.; Sánchez-Cabo, F.; Martí-Gómez, C.; Camafeita, E.; Gómez-Salinero, J.M.; Ramos-Hernández, L.; Nielsen, P.J.; et al. Loss of SRSF3 in Cardiomyocytes Leads to Decapping of Contraction-Related mRNAs and Severe Systolic Dysfunction. Circ. Res. 2019, 125, 170–183. [Google Scholar] [CrossRef] [PubMed]
- Riechert, E.; Kmietczyk, V.; Stein, F.; Schwarzl, T.; Sekaran, T.; Jürgensen, L.; Kamuf-Schenk, V.; Varma, E.; Hofmann, C.; Rettel, M.; et al. Identification of dynamic RNA-binding proteins uncovers a Cpeb4-controlled regulatory cascade during pathological cell growth of cardiomyocytes. Cell Rep. 2021, 35, 109100. [Google Scholar] [CrossRef]
- D’Antonio, M.; Nguyen, J.P.; Arthur, T.D.; Matsui, H.; Donovan, M.K.R.; D’Antonio-Chronowska, A.; Frazer, K.A. In heart failure reactivation of RNA-binding proteins is associated with the expression of 1,523 fetal-specific isoforms. PLoS Comput. Biol. 2022, 18, e1009918. [Google Scholar] [CrossRef] [PubMed]
- Rigaud, V.O.C.; Hoy, R.C.; Kurian, J.; Zarka, C.; Behanan, M.; Brosious, I.; Pennise, J.; Patel, T.; Wang, T.; Johnson, J.; et al. RNA-Binding Protein LIN28a Regulates New Myocyte Formation in the Heart Through Long Noncoding RNA-H19. Circulation 2023, 147, 324–337. [Google Scholar] [CrossRef] [PubMed]
- Viereck, J.; Bührke, A.; Foinquinos, A.; Chatterjee, S.; Kleeberger, J.A.; Xiao, K.; Janssen-Peters, H.; Batkai, S.; Ramanujam, D.; Kraft, T.; et al. Targeting muscle-enriched long non-coding RNA H19 reverses pathological cardiac hypertrophy. Eur. Heart J. 2020, 41, 3462–3474. [Google Scholar] [CrossRef]
- Aguirre, A.; Montserrat, N.; Zacchigna, S.; Nivet, E.; Hishida, T.; Krause, M.N.; Kurian, L.; Ocampo, A.; Vazquez-Ferrer, E.; Rodriguez-Esteban, C.; et al. In vivo activation of a conserved microRNA program induces mammalian heart regeneration. Cell Stem Cell 2014, 15, 589–604. [Google Scholar] [CrossRef]
- Hu, Y.; Jin, G.; Li, B.; Chen, Y.; Zhong, L.; Chen, G.; Chen, X.; Zhong, J.; Liao, W.; Liao, Y.; et al. Suppression of miRNA let-7i-5p promotes cardiomyocyte proliferation and repairs heart function post injury by targetting CCND2 and E2F2. Clin. Sci. 2019, 133, 425–441. [Google Scholar] [CrossRef]
- Tolonen, A.M.; Magga, J.; Szabó, Z.; Viitala, P.; Gao, E.; Moilanen, A.M.; Ohukainen, P.; Vainio, L.; Koch, W.J.; Kerkelä, R.; et al. Inhibition of Let-7 microRNA attenuates myocardial remodeling and improves cardiac function postinfarction in mice. Pharmacol. Res. Perspect. 2014, 2, e00056. [Google Scholar] [CrossRef]
- Garikipati, V.N.S.; Verma, S.K.; Cheng, Z.; Liang, D.; Truongcao, M.M.; Cimini, M.; Yue, Y.; Huang, G.; Wang, C.; Benedict, C.; et al. Circular RNA CircFndc3b modulates cardiac repair after myocardial infarction via FUS/VEGF-A axis. Nat. Commun. 2019, 10, 4317. [Google Scholar] [CrossRef]
- Lai, L.; Xu, Y.; Kang, L.; Yang, J.; Zhu, G. LncRNA KCNQ1OT1 contributes to cardiomyocyte apoptosis by targeting FUS in heart failure. Exp. Mol. Pathol. 2020, 115, 104480. [Google Scholar] [CrossRef]
- Long, Q.; Lv, B.; Jiang, S.; Lin, J. The Landscape of Circular RNAs in Cardiovascular Diseases. Int. J. Mol. Sci. 2023, 24, 4571. [Google Scholar] [CrossRef] [PubMed]
- Radke, M.H.; Badillo-Lisakowski, V.; Britto-Borges, T.; Kubli, D.A.; Jüttner, R.; Parakkat, P.; Carballo, J.L.; Hüttemeister, J.; Liss, M.; Hansen, A.; et al. Therapeutic inhibition of RBM20 improves diastolic function in a murine heart failure model and human engineered heart tissue. Sci. Transl. Med. 2021, 13, eabe8952. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Wang, Z.; Chen, M.; Zhao, W.; Tao, T.; Ma, L.; Ni, Y.; Li, W. YTHDF2 alleviates cardiac hypertrophy via regulating Myh7 mRNA decoy. Cell Biosci. 2021, 11, 132. [Google Scholar] [CrossRef]
- Gao, G.; Xie, A.; Huang, S.C.; Zhou, A.; Zhang, J.; Herman, A.M.; Ghassemzadeh, S.; Jeong, E.M.; Kasturirangan, S.; Raicu, M.; et al. Role of RBM25/LUC7L3 in abnormal cardiac sodium channel splicing regulation in human heart failure. Circulation 2011, 124, 1124–1131. [Google Scholar] [CrossRef]
- Yang, C.; Wang, H.; Qiao, T.; Yang, B.; Aliaga, L.; Qiu, L.; Tan, W.; Salameh, J.; McKenna-Yasek, D.M.; Smith, T.; et al. Partial loss of TDP-43 function causes phenotypes of amyotrophic lateral sclerosis. Proc. Natl. Acad. Sci. USA 2014, 111, E1121–E1129. [Google Scholar] [CrossRef]
- Mori, F.; Tada, M.; Kon, T.; Miki, Y.; Tanji, K.; Kurotaki, H.; Tomiyama, M.; Ishihara, T.; Onodera, O.; Kakita, A.; et al. Phosphorylated TDP-43 aggregates in skeletal and cardiac muscle are a marker of myogenic degeneration in amyotrophic lateral sclerosis and various conditions. Acta Neuropathol. Commun. 2019, 7, 165. [Google Scholar] [CrossRef]
- Koshelev, M.; Sarma, S.; Price, R.E.; Wehrens, X.H.; Cooper, T.A. Heart-specific overexpression of CUGBP1 reproduces functional and molecular abnormalities of myotonic dystrophy type 1. Hum. Mol. Genet. 2010, 19, 1066–1075. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.K.; Deshmukh, V.; Thatcher, K.; Belanger, K.K.; Rhyner, A.M.; Meng, S.; Holcomb, R.J.; Bressan, M.; Martin, J.F.; Cooke, J.P.; et al. RBFOX2 is required for establishing RNA regulatory networks essential for heart development. Nucleic Acids Res. 2022, 50, 2270–2286. [Google Scholar] [CrossRef]
- Gupta, S.K.; Garg, A.; Bär, C.; Chatterjee, S.; Foinquinos, A.; Milting, H.; Streckfuß-Bömeke, K.; Fiedler, J.; Thum, T. Quaking Inhibits Doxorubicin-Mediated Cardiotoxicity Through Regulation of Cardiac Circular RNA Expression. Circ. Res. 2018, 122, 246–254. [Google Scholar] [CrossRef]
- Brooks, S.A.; Blackshear, P.J. Tristetraprolin (TTP): Interactions with mRNA and proteins, and current thoughts on mechanisms of action. Biochim. Biophys. Acta 2013, 1829, 666–679. [Google Scholar] [CrossRef]
- Chen, X.; Liu, Y.; Xu, C.; Ba, L.; Liu, Z.; Li, X.; Huang, J.; Simpson, E.; Gao, H.; Cao, D.; et al. QKI is a critical pre-mRNA alternative splicing regulator of cardiac myofibrillogenesis and contractile function. Nat. Commun. 2021, 12, 89. [Google Scholar] [CrossRef] [PubMed]
- Beisaw, A.; Kuenne, C.; Guenther, S.; Dallmann, J.; Wu, C.C.; Bentsen, M.; Looso, M.; Stainier, D.Y.R. AP-1 Contributes to Chromatin Accessibility to Promote Sarcomere Disassembly and Cardiomyocyte Protrusion During Zebrafish Heart Regeneration. Circ. Res. 2020, 126, 1760–1778. [Google Scholar] [CrossRef] [PubMed]
- Bongiovanni, C.; Bueno-Levy, H.; Posadas Pena, D.; Del Bono, I.; Miano, C.; Boriati, S.; Da Pra, S.; Sacchi, F.; Redaelli, S.; Bergen, M.; et al. BMP7 promotes cardiomyocyte regeneration in zebrafish and adult mice. Cell Rep. 2024, 43, 114162. [Google Scholar] [CrossRef]
- Zhao, Y.; Lv, H.; Yu, C.; Liang, J.; Yu, H.; Du, Z.; Zhang, R. Systemic inhibition of mitochondrial fatty acid β-oxidation impedes zebrafish ventricle regeneration. Biochim. Biophys. Acta Mol. Basis Dis. 2024, 1870, 167442. [Google Scholar] [CrossRef]
- Boos, A.; Gahr, B.M.; Park, D.D.; Braun, V.; Buhler, A.; Rottbauer, W.; Just, S. Hdac1-deficiency affects the cell cycle axis Cdc25-Cdk1 causing impaired G2/M phase progression and reduced cardiomyocyte proliferation in zebrafish. Biochem. Biophys. Res. Commun. 2023, 665, 98–106. [Google Scholar] [CrossRef]
- Gong, J.; Huang, M.; Wang, F.; Ma, X.; Liu, H.; Tu, Y.; Xing, L.; Zhu, X.; Zheng, H.; Fang, J.; et al. RBM45 competes with HDAC1 for binding to FUS in response to DNA damage. Nucleic Acids Res. 2017, 45, 12862–12876. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Shi, J.; Liu, W. The role of Wnt/β-catenin-lin28a/let-7 axis in embryo implantation competency and epithelial-mesenchymal transition (EMT). Cell Commun. Signal 2020, 18, 108. [Google Scholar] [CrossRef]
- Zhang, L.; Zhang, Y.; Yu, F.; Li, X.; Gao, H.; Li, P. The circRNA-miRNA/RBP regulatory network in myocardial infarction. Front. Pharmacol. 2022, 13, 941123. [Google Scholar] [CrossRef]
- Wen, Z.J.; Xin, H.; Wang, Y.C.; Liu, H.W.; Gao, Y.Y.; Zhang, Y.F. Emerging roles of circRNAs in the pathological process of myocardial infarction. Mol. Ther. Nucleic Acids 2021, 26, 828–848. [Google Scholar] [CrossRef]
- Gao, G.; Xie, A.; Zhang, J.; Herman, A.M.; Jeong, E.M.; Gu, L.; Liu, M.; Yang, K.C.; Kamp, T.J.; Dudley, S.C. Unfolded protein response regulates cardiac sodium current in systolic human heart failure. Circ. Arrhythm. Electrophysiol. 2013, 6, 1018–1024. [Google Scholar] [CrossRef]
- Shang, L.L.; Pfahnl, A.E.; Sanyal, S.; Jiao, Z.; Allen, J.; Banach, K.; Fahrenbach, J.; Weiss, D.; Taylor, W.R.; Zafari, A.M.; et al. Human heart failure is associated with abnormal C-terminal splicing variants in the cardiac sodium channel. Circ. Res. 2007, 101, 1146–1154. [Google Scholar] [CrossRef] [PubMed]
- Nutter, C.A.; Jaworski, E.A.; Verma, S.K.; Deshmukh, V.; Wang, Q.; Botvinnik, O.B.; Lozano, M.J.; Abass, I.J.; Ijaz, T.; Brasier, A.R.; et al. Dysregulation of RBFOX2 Is an Early Event in Cardiac Pathogenesis of Diabetes. Cell Rep. 2016, 15, 2200–2213. [Google Scholar] [CrossRef]
- Nutter, C.A.; Jaworski, E.; Verma, S.K.; Perez-Carrasco, Y.; Kuyumcu-Martinez, M.N. Developmentally regulated alternative splicing is perturbed in type 1 diabetic skeletal muscle. Muscle Nerve 2017, 56, 744–749. [Google Scholar] [CrossRef] [PubMed]
- Ule, J.; Blencowe, B.J. Alternative Splicing Regulatory Networks: Functions, Mechanisms, and Evolution. Mol. Cell 2019, 76, 329–345. [Google Scholar] [CrossRef] [PubMed]
- Laina, A.; Gatsiou, A.; Georgiopoulos, G.; Stamatelopoulos, K.; Stellos, K. RNA Therapeutics in Cardiovascular Precision Medicine. Front. Physiol. 2018, 9, 953. [Google Scholar] [CrossRef] [PubMed]
- Childs-Disney, J.L.; Yang, X.; Gibaut, Q.M.R.; Tong, Y.; Batey, R.T.; Disney, M.D. Targeting RNA structures with small molecules. Nat. Rev. Drug Discov. 2022, 21, 736–762. [Google Scholar] [CrossRef]
- Liao, Y.; Castello, A.; Fischer, B.; Leicht, S.; Föehr, S.; Frese, C.K.; Ragan, C.; Kurscheid, S.; Pagler, E.; Yang, H.; et al. The Cardiomyocyte RNA-Binding Proteome: Links to Intermediary Metabolism and Heart Disease. Cell Rep. 2016, 16, 1456–1469. [Google Scholar] [CrossRef]
- Kusuma, S.; Shen, Y.I.; Hanjaya-Putra, D.; Mali, P.; Cheng, L.; Gerecht, S. Self-organized vascular networks from human pluripotent stem cells in a synthetic matrix. Proc. Natl. Acad. Sci. USA 2013, 110, 12601–12606. [Google Scholar] [CrossRef]
- Sachse, M.; Tual-Chalot, S.; Ciliberti, G.; Amponsah-Offeh, M.; Stamatelopoulos, K.; Gatsiou, A.; Stellos, K. RNA-binding proteins in vascular inflammation and atherosclerosis. Atherosclerosis 2023, 374, 55–73. [Google Scholar] [CrossRef]
- Wu, X.; Lan, L.; Wilson, D.M.; Marquez, R.T.; Tsao, W.C.; Gao, P.; Roy, A.; Turner, B.A.; McDonald, P.; Tunge, J.A.; et al. Identification and validation of novel small molecule disruptors of HuR-mRNA interaction. ACS Chem. Biol. 2015, 10, 1476–1484. [Google Scholar] [CrossRef]
- Green, L.C.; Anthony, S.R.; Slone, S.; Lanzillotta, L.; Nieman, M.L.; Wu, X.; Robbins, N.; Jones, S.M.; Roy, S.; Owens, A.P., 3rd; et al. Human antigen R as a therapeutic target in pathological cardiac hypertrophy. JCI Insight 2019, 4, e121541. [Google Scholar] [CrossRef]
- Majmudar, M.D.; Keliher, E.J.; Heidt, T.; Leuschner, F.; Truelove, J.; Sena, B.F.; Gorbatov, R.; Iwamoto, Y.; Dutta, P.; Wojtkiewicz, G.; et al. Monocyte-directed RNAi targeting CCR2 improves infarct healing in atherosclerosis-prone mice. Circulation 2013, 127, 2038–2046. [Google Scholar] [CrossRef]
- Gilbert, J.; Lekstrom-Himes, J.; Donaldson, D.; Lee, Y.; Hu, M.; Xu, J.; Wyant, T.; Davidson, M. Effect of CC chemokine receptor 2 CCR2 blockade on serum C-reactive protein in individuals at atherosclerotic risk and with a single nucleotide polymorphism of the monocyte chemoattractant protein-1 promoter region. Am. J. Cardiol. 2011, 107, 906–911. [Google Scholar] [CrossRef] [PubMed]
- Hong, S. RNA Binding Protein as an Emerging Therapeutic Target for Cancer Prevention and Treatment. J. Cancer Prev. 2017, 22, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Bajan, S.; Hutvagner, G. RNA-Based Therapeutics: From Antisense Oligonucleotides to miRNAs. Cells 2020, 9, 137. [Google Scholar] [CrossRef]
- Lieberman, J. Tapping the RNA world for therapeutics. Nat. Struct. Mol. Biol. 2018, 25, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Everett, B.M.; Thuren, T.; MacFadyen, J.G.; Chang, W.H.; Ballantyne, C.; Fonseca, F.; Nicolau, J.; Koenig, W.; Anker, S.D.; et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N. Engl. J. Med. 2017, 377, 1119–1131. [Google Scholar] [CrossRef]
- Ridker, P.M.; MacFadyen, J.G.; Thuren, T.; Libby, P. Residual inflammatory risk associated with interleukin-18 and interleukin-6 after successful interleukin-1β inhibition with canakinumab: Further rationale for the development of targeted anti-cytokine therapies for the treatment of atherothrombosis. Eur. Heart J. 2020, 41, 2153–2163. [Google Scholar] [CrossRef]


| RBPs | Amino Acids/aa | Mass/Da | Expression or Activity in Cardiovascular Diseases | Function | Targets | Organism | Refs. |
|---|---|---|---|---|---|---|---|
| MBNL1 | 343 | 36,551 | Increased | Regulates VSMC proliferation and differentiation | Not explicitly mentioned, but involved in miR-30b-5p interaction | Homo sapiens | [19] |
| PCBP2 | 335 | 35,347 | Decreased | Inhibits hypertrophy | GPR56 mRNA | Homo sapiens, Mus musculus | [16] |
| CELF1 | 486 | 52,107 | Decreases in adult heart; increases during heart development and in response to cardiac stress | Regulates alternative splicing | Not explicitly mentioned | Mus musculus | [20] |
| SF1 | 111 | 11,695 | Increased | Regulation of steroidogenesis | Steroidogenic enzymes | Homo sapiens | [21] |
| ZRSR2 | 462 | 54,905 | Increased | Splicing | Not explicitly mentioned | Branchiostoma lanceolatum | [22] |
| SRSF4 | 489 | 55,979 | Decreased | Inhibits hypertrophy | GAS5 (growth arrest-specific 5) | Mus musculus | [23] |
| SRSF5 | 55 | 6205 | Increased | Facilitates production of p19 H-RAS | p19 H-RAS | Homo sapiens | [24] |
| CIRP | 172 | 18,648 | Increases under chemotherapy-induced stress | Inhibits apoptosis | OGFR mRNA | Homo sapiens | [25] |
| RBFOX2 | 449 | 47,330 | Decreases under pressure overload-induced heart failure | Regulates splicing | Exon of fxr1 | Mus musculus | [26,27] |
| FTO | 505 | 58,282 | Decreases in failing mammalian hearts and hypoxic cardiomyocytes | Regulates cardiac contractility | SERCA2A, MYH6/7, RYR2 | Homo sapiens | [28] |
| METTL3 | 580 | 64,616 | Increases in response to hypertrophic stimulation | Catalyzes m6A methylation, promoting cardiac hypertrophy | mRNAs encoding kinases involved in the MAPK pathway, such as SERCA2A, MYH6/7, and RYR2. | Mus musculus | [29] |
| RBPs | Amino Acids/aa | Mass/Da | Expression or Activity in Cardiac Diseases | Function | Targets | Study Model | Refs. |
|---|---|---|---|---|---|---|---|
| MIRI | |||||||
| ELAVL1 | 326 | 36,153 | Upregulated | Promotes ferroptosis, modulates autophagy | Beclin-1, FOXC1 | Mus musculus | [50] |
| SRSF10 | 262 | 31,301 | Downregulated | Regulates splicing of key muscle genes | MEF2A, CASQ2, TTN | Homo sapiens | [51] |
| QKI-5 | 341 | 37,671 | Downregulated | Enhances ischemic tolerance, reduces apoptosis | FOXO1 pathway | Mus musculus | [52] |
| cardiac arrhythmias | |||||||
| QKI-6 | 341 | 37,671 | Downregulated | Regulates splicing of HDAC7, promotes VSMC differentiation | HDAC7, SM22 | Homo sapiens | [53,54] |
| CIRP | 172 | 18,607 | Upregulated | Prevents AF onset by posttranscriptionally regulating ion channels | Kv1.5 and Kv4.2/4.3 ion channels | Mus musculus | [55] |
| MI | |||||||
| RBM15 | 962 | 105,722 | Upregulated | Stabilizes m6A modification, improves cardiac function | NEDD8 | Mus musculus | [56] |
| IGF2BP2 | 592 | 65,584 | Upregulated | Modulates RNA localization, enhances stress response | Sarcomeric and mitochondrial proteins | Mus musculus | [57] |
| LIN28A | 209 | 22,720 | Upregulated | Inhibits cardiac remodeling and apoptosis, improves cardiac function | UPF1 | Mus musculus | [58,59] |
| RbFox1 | 396 | 42,678 | Downregulated | Regulates the alternative splicing of Cav1.2 channels | Exon 9* and exon 33 of the Cav1.2 calcium channel gene | Mus musculus | [60] |
| RbFox2 | 449 | 47,330 | Downregulated | Regulates the alternative splicing of Cav1.2 channels | Exon 9* and exon 33 of the Cav1.2 calcium channel gene | Mus musculus | [60] |
| SRSF3 | 164 | 19,330 | Downregulated | Prevents mRNA decapping involved in cardiac contraction | mTOR mRNA | Mus musculus | [61] |
| HF | |||||||
| Cpeb4 | 729 | 80,122 | Dynamically expressed in cardiomyocytes | Regulates cardiac remodeling | Zeb1, Zbtb20 | Mus musculus | [62,63] |
| LIN28A | 209 | 22,720 | Upregulated | Regulates cardiac remodeling genes, alleviates cardiac hypertrophy, promotes cardiac regeneration | lncRNA H19, let-7 miRNA | Mus musculus | [64,65,66,67,68] |
| FUS | 518 | 52,673 | Downregulated | Regulates cardiomyocyte apoptosis | circFndc3b, KCNQ1OT1 | Mus musculus | [69,70] |
| RBM20 | 1199 | 130,124 | Upregulated | Splicing regulation | cTTN1, titin | Mus musculus | [71,72] |
| YTHDF2 | 579 | 62,280 | Upregulated | Suppresses cardiac hypertrophy via m6A-dependent regulation of Myh7 mRNA | Myh7 mRNA | Mus musculus | [73] |
| RBM25 | 843 | 100,185 | Upregulated | Mediates abnormal mRNA splicing of SCN5A, reducing Na+ channel current | SCN5A mRNA | Homo sapiens | [74] |
| LUC7L3 | 118 | 13,445 | Upregulated | Mediates abnormal mRNA splicing of SCN5A, reducing Na+ channel current | SCN5A mRNA | Homo sapiens | [74] |
| TDP-43 | 414 | 44,740 | Upregulated | Promotes cardiac muscle degeneration | Not explicitly mentioned | Homo sapiens | [75,76] |
| CUGBP1 | 486 | 52,107 | Upregulated | Disrupts splicing in DM1 | Not explicitly mentioned | Mus musculus | [77] |
| RBFOX2 | 449 | 47,330 | Downregulated | Regulates alternative splicing | Rho GTPase cycling genes | Mus musculus | [78] |
| QKI-5 | 341 | 37,671 | Downregulated | Inhibits doxorubicin-induced cardiac damage | Ttn (titin), Fhod3, Strn3 | Mus musculus | [79] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, L.; Chu, J.; An, S.; Liu, X.; Tan, R. The Biological Mechanisms and Clinical Roles of RNA-Binding Proteins in Cardiovascular Diseases. Biomolecules 2024, 14, 1056. https://doi.org/10.3390/biom14091056
Lin L, Chu J, An S, Liu X, Tan R. The Biological Mechanisms and Clinical Roles of RNA-Binding Proteins in Cardiovascular Diseases. Biomolecules. 2024; 14(9):1056. https://doi.org/10.3390/biom14091056
Chicago/Turabian StyleLin, Lizhu, Jiemei Chu, Sanqi An, Xinli Liu, and Runxian Tan. 2024. "The Biological Mechanisms and Clinical Roles of RNA-Binding Proteins in Cardiovascular Diseases" Biomolecules 14, no. 9: 1056. https://doi.org/10.3390/biom14091056
APA StyleLin, L., Chu, J., An, S., Liu, X., & Tan, R. (2024). The Biological Mechanisms and Clinical Roles of RNA-Binding Proteins in Cardiovascular Diseases. Biomolecules, 14(9), 1056. https://doi.org/10.3390/biom14091056









