A Comprehensive Review of Control Challenges and Methods in End-Effector Upper-Limb Rehabilitation Robots
Abstract
1. Introduction
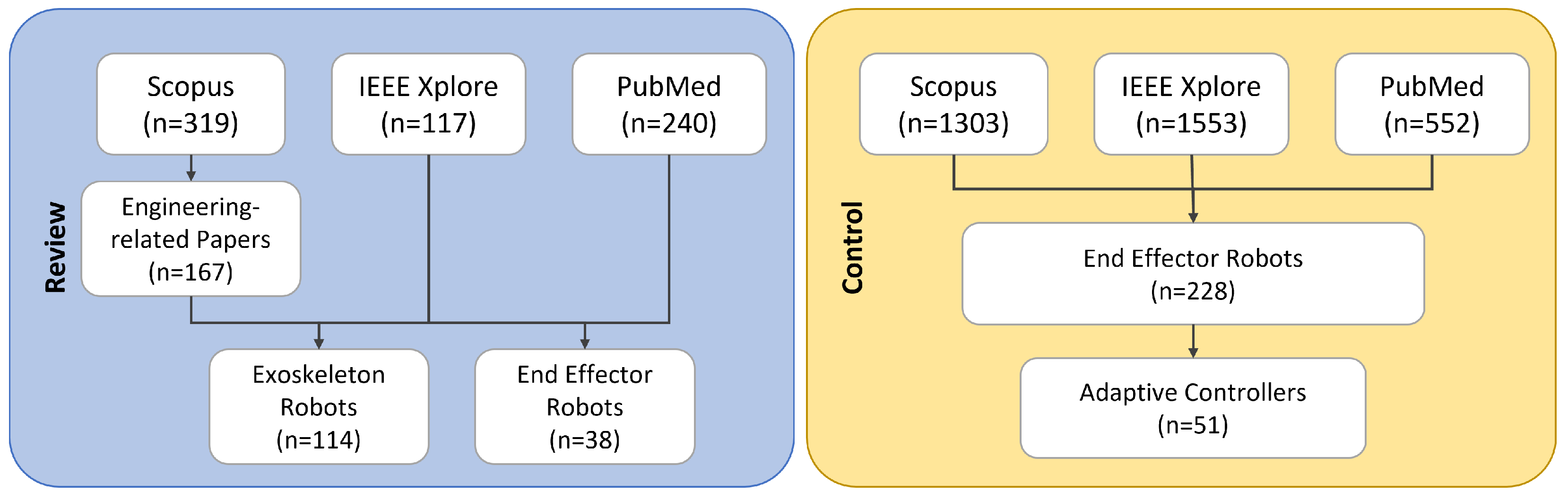
2. Literature Search Methodology
3. Overview of Upper-Limb Rehabilitation Robots
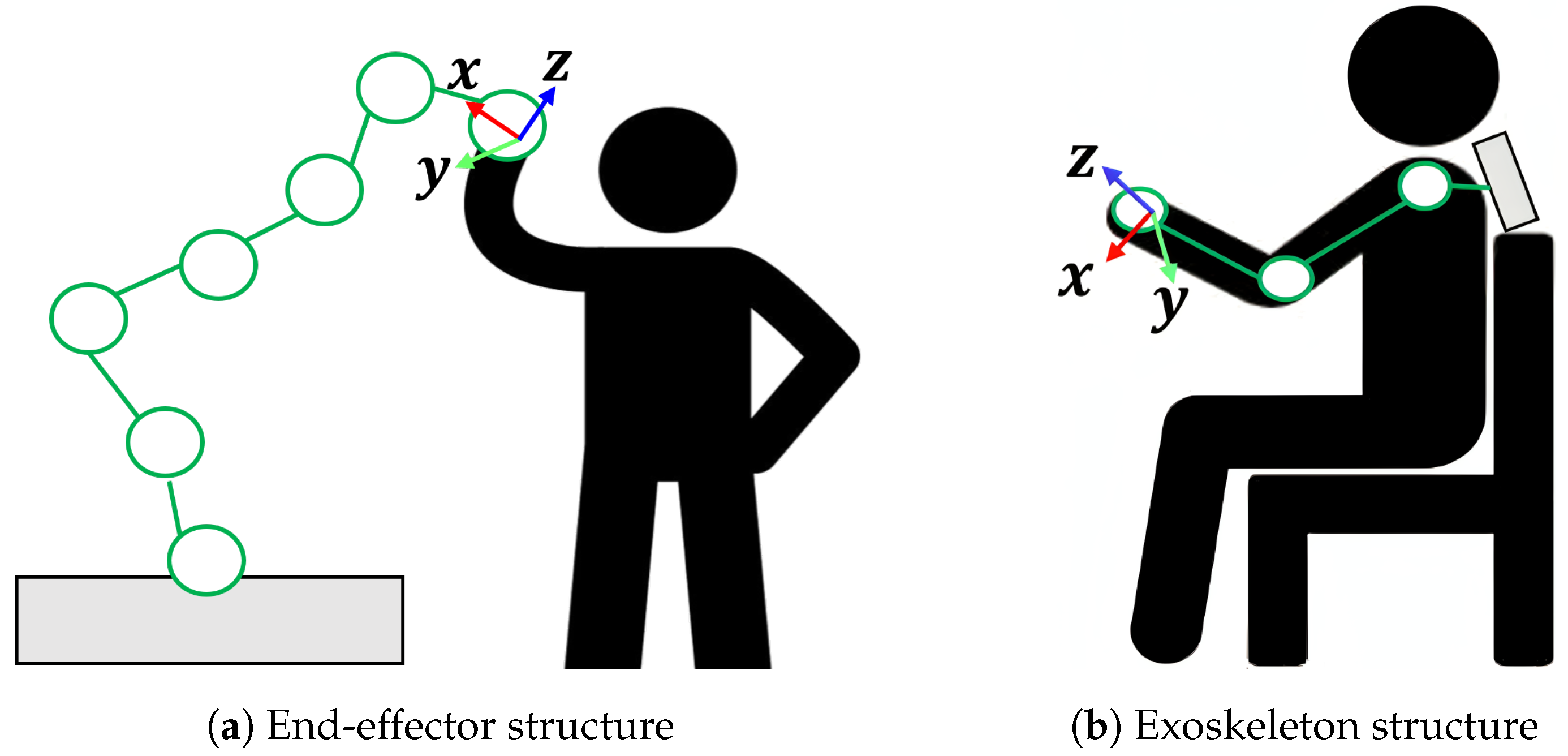
3.1. Rehabilitation Robot Mechanisms
3.2. Requirements for Upper-Limb Rehabilitation
| EE Robot | Year | Classification | DoF | Targeted Joints | Type of Disease | Clinical Testing | Software Origin | Commercial |
|---|---|---|---|---|---|---|---|---|
| MIT Manus [15] | 1994 | Planar motion | 2 | Shoulder + elbow | Stroke, CP, MS, TBI | 1000++ [38] from 1999 till 2004, 250 strokes, 3 h/wk for 12 wks [15] | Massachusetts Institute of Technology (MIT) [15] | ✓ |
| ARM-Guide [17] | 1995 | Linear motion | 1 | Shoulder + elbow | Stroke | In 2000, 3 chronic strokes, 3 h/wk for 8 wks [39] | Rehab Inst. of Chicago, University of California [40] | ✗ |
| NeReBot [21] | 1995 | Cable-driven motion | 2 | Shoulder + elbow + wrist | Stroke | In 2007, 12 early strokes and 12 unimpaired upper limbs ≈5 h/wk for 4 wks [41] | Robotics Lab, University of Padua [42] | ✗ |
| MIME [18] | 1997 | Bi-manual motion | 6 | Shoulder + elbow | Stroke | In 2004, 13 chronic strokes, 3 h/wk for 8 wks [43] In 2011, 54 hemipareses, up to 30 h [44] | Stanford University [18] | ✗ |
| Bi-Manu-Track [19] | 2001 | Bi-manual motion | 2 | Adaptive | Stroke | In 2016, 34 chronic strokes ≈20 h, for 4 wks [45] In 2023, 70 hemiplegic strokes, 6 h/wk for 3 wks [45] | Reha-Stim Co., Germany [46] | ✓ |
| GENTLE-/s [20] | 2002 | 3D motion | 3 | Shoulder + elbow + wrist | Stroke | In 2007, 31 strokes, 3 h/wk for 9 wks [47] | Moog Inc. [48] | ✗ |
| HAPTIC MASTER [49] | 2002 | 3D motion | 3 | Forearm | Stroke, dystonia | In 2014, 22 chronic strokes, 4 h/wk for 8 wks [50] | Moog Inc. [48] | ✗ |
| REHA-ROB [51] | 2007 | 3D motion | 3 | Shoulder + elbow | Stroke | In 2007, 30 hemipareses, ≈1 h for 20 days [51] | ABB & comp.: Hungary, UK, Germany, and Bulgaria [52] | ✗ |
| [22] | 2007 | Planar motion | 3 | Shoulder + elbow | Stroke | In 2009, N/A hemiparesis, 3 h/wk for 8 wks [53] | Neuro-imaging, Motor Control, Northwestern University [53] | ✗ |
| Amadeo [54] | 2010 | Hand Mobility | 5 | Hand + fingers | Stroke, CT | In 2010, 12 ischemic strokes, 3 h/wk for 8 wks [55] In 2023, 58 strokes, average 3 h/wk for 10 wks [56] | TyroS software Tyromotion GmbH [57] | ✓ |
| Braccio di Ferro [58] | 2011 | Planar motion | 2 | Shoulder + elbow | Stroke, MS | In 2010, 10 hemiplegias, 6 to 12 sessions [59] | Neurolab, University of Genova [60] | ✗ |
| Wristbot [61] | 2014 | 3D motion | 3 | Wrist | Stroke, dystonia | In 2021, 23 wrist injuries, 5 h/wk for 3 wks [62] | REACH Prog. University of Minnesota [63] | ✗ |
| Diego [64] | 2014 | Cable-driven motion | 3 | Shoulder + elbow | Stroke, CP | N/A | TyroS software Tyromotion GmbH [65] | ✓ |
| MOTORE [66] | 2016 | Mobile Planar motion | 3 | Shoulder + elbow + wrist | Stroke, MD | N/A | Humanware, Scuola Superiore Sant’Anna of Pisa [65] | ✓ |
| Exoskeletons | Year | DoF | Targeted Joints | Type of Disease | Clinical Testing | Commercial |
|---|---|---|---|---|---|---|
| RUPERT [25] | 2005 | 5 | Shoulder + humeral + elbow + forearm + wrist | Stroke | ✓ | ✗ |
| MAHI EXO-II [26] | 2006 | 5 | Elbow + forearm + wrist | Stroke, SCI | ✓ | ✗ |
| MyoPro [27] | 2006 | 4 | Elbow + wrist + hand | Stroke, BPI, BI, SCI | ✓ | ✓ |
| CADEN [29] | 2007 | 7 | Shoulder + elbow + forearm + wrist | Stroke, SCI | ✓ | ✗ |
| ARMin II, III [30,31] | 2007–2009 | 6 | Shoulder + elbow + lower arm + wrist | Stroke, SCI | ✓ | ✗ |
| SUEFUL [32] | 2009 | 7 | Shoulder + elbow + forearm + wrist | - | ✓ | ✗ |
| EXO-UL7 [33] | 2011 | 7 | Shoulder + elbow + forearm + wrist | Stroke | ✓ | ✗ |
| ARMEO Power [34] | 2011 | 6 | Shoulder + elbow + forearm + wrist | Stroke, CP | ✓ | ✓ |
| HAL-SJ [35] | 2015 | 1 | Single joint, e.g., elbow | Joint-specific injury | ✓ | ✓ |
3.2.1. Clinical Requirements
3.2.2. Functional Requirements
3.2.3. General Requirements
4. Robotic Rehabilitation Training Modes and Control Challenges
Control Challenges in Rehabilitation Robotics
5. Upper-Limb Rehabilitation Robotic End-Effector Control Methods
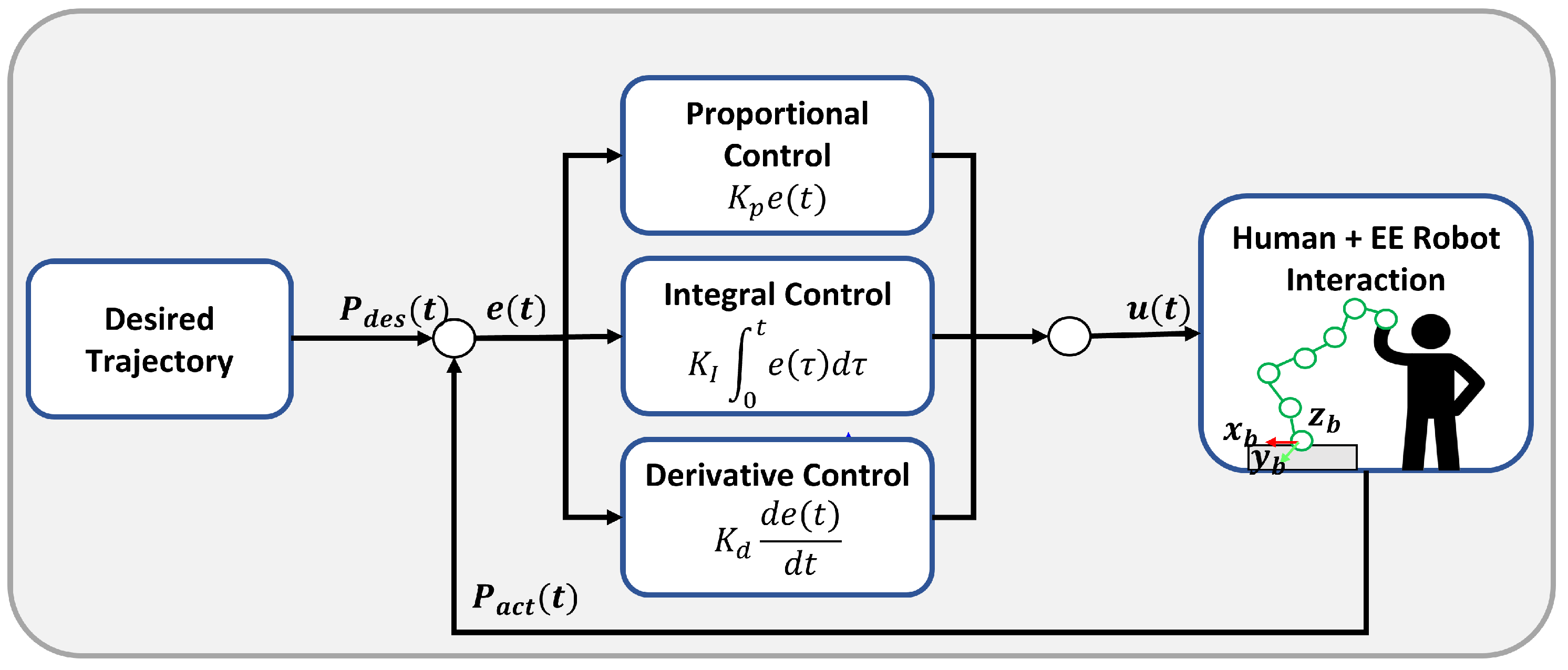
5.1. Proportional–Integral–Derivative (PID) Control
5.2. Impedance Control
5.3. Admittance Control
5.4. Robust Control
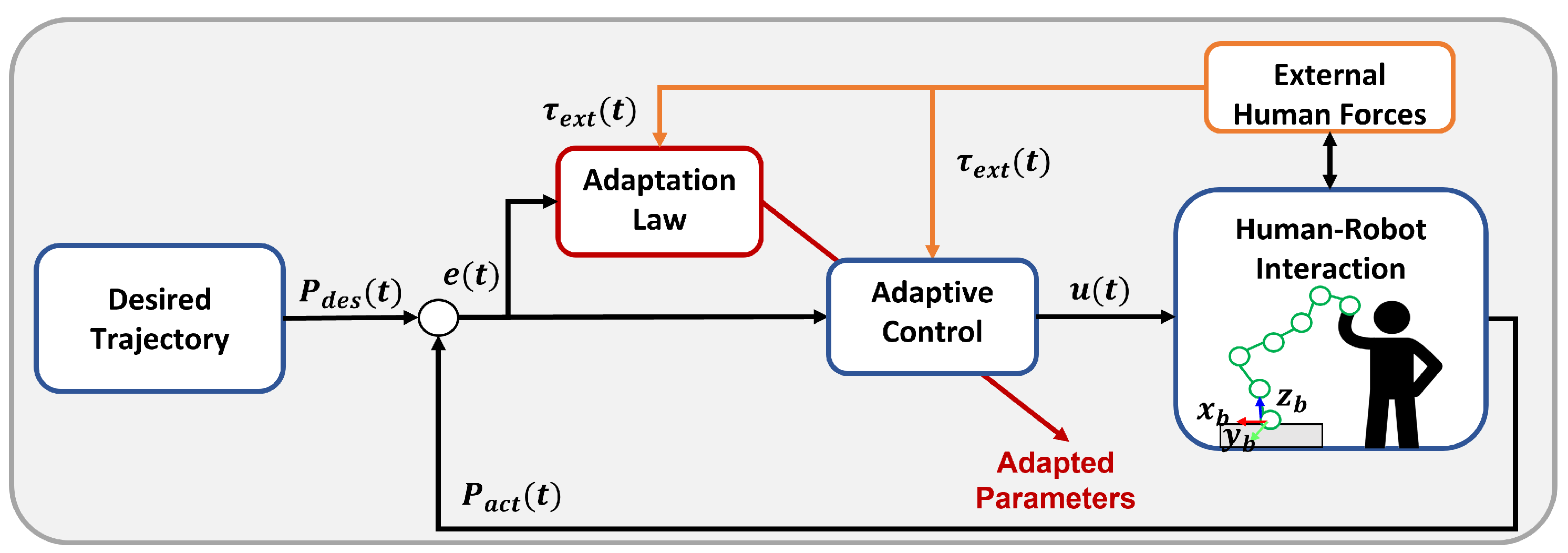
5.5. Adaptive Control
5.5.1. Adaptive Impedance/Admittance Control
5.5.2. Fuzzy-Based Adaptive Control
5.5.3. Machine Learning-Based Adaptive Control
5.5.4. Adaptive Sliding Mode Control
5.5.5. Adaptive Backstepping Control
5.5.6. Model Reference Adaptive Control (MRAC)
5.5.7. Discussion
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AACNDO | Adaptive Admittance Control Neural Network-based Disturbance Observer |
| AAN | Assist-as-needed |
| ACT | Arm Coordination Training |
| ADL | Activities of daily living |
| APF | Artificial Potential Field |
| AREBO | Arm Rehabilitation Robot |
| ARM | Assisted Rehabilitation and Measurement |
| BP | Back-Propagation |
| CADEN | Cable-Actuated Dexterous Exoskeleton for Neuro-rehabilitation |
| CNA | Compensation with No robot Assistance |
| CRA | Compensation with Robot Assistance |
| D | Dimensional |
| DoF | Degree of Freedom |
| DRFNN | Dynamic Recurrent Fuzzy Neural Network |
| EDRFNN | Evolutionary Dynamic Recurrent Fuzzy Neural Network |
| EMG | Electromyography |
| FAP | Fuzzy Adaptive Potential |
| FMA | Fugl-Meyer Assessment |
| FNN | Fuzzy Neural Network |
| GA | Genetic Algorithm |
| GUI | Graphical User Interface |
| HEP | Hybrid Evolutionary Programming |
| IHME | Institute of Health Metrics and Evaluation |
| MAS | Modified Ashworth Scale |
| MIME | Mirror-Image Movement Enabler |
| MRAC | Model Reference Adaptive Control |
| MRAIC | Model Reference Adaptive Impedance Control |
| MSD | Musculoskeletal disorders |
| MTE | Mean Tracking Error |
| NAAC | Non-Adapting Admittance Control |
| NN | Neural Network |
| PD | Proportional–Derivative |
| PID | Proportional–Integral–Derivative |
| PNF | Proprioceptive Neuromuscular Facilitation |
| RBF | Radial Basis Function |
| RBFN | Radial Basis Function Network |
| RF | Reference Free |
| RIR | Restriction Interaction Region |
| RL | Reinforcement learning |
| RLS | Recursive Least Squares |
| RMSE | Root-mean-square error |
| RUPERT | Robotic Upper Extremity Repetitive Trainer |
| SAAC | Self-Adapting Admittance Control |
| sEMG | Surface Electromyography |
| SMC | Sliding Mode Control |
| TDC | Time-Delay Control |
| UAM | Unassisted Mode |
| WHO | World Health Organization |
| WSM | Weight Support Mode |
| ZIF | Zero Interaction Force |
References
- World Health Organization. Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Sebbag, E.; Felten, R.; Sagez, F.; Sibilia, J.; Devilliers, H.; Arnaud, L. The world-wide burden of musculoskeletal diseases: A systematic analysis of the World Health Organization Burden of Diseases Database. Ann. Rheum. Dis. 2019, 78, 844–848. [Google Scholar] [CrossRef]
- Belluzzi, E.; Pozzuoli, A.; Ruggieri, P. Musculoskeletal Diseases: From Molecular Basis to Therapy. Biomedicines 2023, 12, 32. [Google Scholar] [CrossRef]
- World Health Organization. Neurological Disorders: Public Health Challenges; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Feigin, V.L.; Brainin, M.; Norrving, B.; Martins, S.; Sacco, R.L.; Hacke, W.; Fisher, M.; Pandian, J.; Lindsay, P. World Stroke Organization (WSO): Global stroke fact sheet 2022. Int. J. Stroke 2022, 17, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Gimigliano, F.; Negrini, S. The World Health Organization “rehabilitation 2030: A call for action”. Eur. J. Phys. Rehabil. Med. 2017, 53, 155–168. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Guo, S.; Sun, Q. An assist-as-needed controller for passive, assistant, active, and resistive robot-aided rehabilitation training of the upper extremity. Appl. Sci. 2020, 11, 340. [Google Scholar] [CrossRef]
- Sheng, B.; Zhang, Y.; Meng, W.; Deng, C.; Xie, S. Bilateral robots for upper-limb stroke rehabilitation: State of the art and future prospects. Med. Eng. Phys. 2016, 38, 587–606. [Google Scholar] [CrossRef]
- Molteni, F.; Gasperini, G.; Cannaviello, G.; Guanziroli, E. Exoskeleton and end-effector robots for upper and lower limbs rehabilitation: Narrative review. PM&R 2018, 10, S174–S188. [Google Scholar]
- Iandolo, R.; Marini, F.; Semprini, M.; Laffranchi, M.; Mugnosso, M.; Cherif, A.; De Michieli, L.; Chiappalone, M.; Zenzeri, J. Perspectives and challenges in robotic neurorehabilitation. Appl. Sci. 2019, 9, 3183. [Google Scholar] [CrossRef]
- Proietti, T.; Ambrosini, E.; Pedrocchi, A.; Micera, S. Wearable robotics for impaired upper-limb assistance and rehabilitation: State of the art and future perspectives. IEEE Access 2022, 10, 106117–106134. [Google Scholar] [CrossRef]
- Bhujel, S.; Hasan, S. A comparative study of end-effector and exoskeleton type rehabilitation robots in human upper extremity rehabilitation. Hum.-Intell. Syst. Integr. 2023, 5, 11–42. [Google Scholar] [CrossRef]
- Qassim, H.M.; Wan Hasan, W. A review on upper limb rehabilitation robots. Appl. Sci. 2020, 10, 6976. [Google Scholar] [CrossRef]
- Ai, Q.; Liu, Z.; Meng, W.; Liu, Q.; Xie, S.Q. Machine learning in robot assisted upper limb rehabilitation: A focused review. IEEE Trans. Cogn. Dev. Syst. 2021, 15, 2053–2063. [Google Scholar] [CrossRef]
- Krebs, H.I.; Ferraro, M.; Buerger, S.P.; Newbery, M.J.; Makiyama, A.; Sandmann, M.; Lynch, D.; Volpe, B.T.; Hogan, N. Rehabilitation robotics: Pilot trial of a spatial extension for MIT-Manus. J. Neuroeng. Rehabil. 2004, 1, 5. [Google Scholar] [CrossRef]
- Hidler, J.; Nichols, D.; Pelliccio, M.; Brady, K. Advances in the understanding and treatment of stroke impairment using robotic devices. Top. Stroke Rehabil. 2005, 12, 22–35. [Google Scholar] [CrossRef] [PubMed]
- Nef, T.; Riener, R. ARMin-design of a novel arm rehabilitation robot. In Proceedings of the 9th International Conference on Rehabilitation Robotics, ICORR 2005, Chicago, IL, USA, 28 June–1 July 2005; pp. 57–60. [Google Scholar]
- Lum, P.S.; Burgar, C.G.; Van der Loos, M.; Shor, P.C.; Majmundar, M.; Yap, R. The MIME robotic system for upper-limb neuro-rehabilitation: Results from a clinical trial in subacute stroke. In Proceedings of the 9th International Conference on Rehabilitation Robotics, ICORR 2005, Chicago, IL, USA, 28 June–1 July 2005; pp. 511–514. [Google Scholar]
- Hesse, S.; Schulte-Tigges, G.; Konrad, M.; Bardeleben, A.; Werner, C. Robot-assisted arm trainer for the passive and active practice of bilateral forearm and wrist movements in hemiparetic subjects. Arch. Phys. Med. Rehabil. 2003, 84, 915–920. [Google Scholar] [CrossRef] [PubMed]
- Loureiro, R.; Amirabdollahian, F.; Harwin, W. 22 A Gentle/S Approach to Robot Assisted Neuro-Rehabilitation. In Advances in Rehabilitation Robotics: Human-Friendly Technologies on Movement Assistance and Restoration for People with Disabilities; Springer: Berlin/Heidelberg, Germany, 2004; pp. 347–363. [Google Scholar]
- Stefano, M.; Patrizia, P.; Mario, A.; Ferlini, G.; Rizzello, R.; Rosati, G. Robotic upper limb rehabilitation after acute stroke by NeReBot: Evaluation of treatment costs. BioMed Res. Int. 2014, 2014, 265634. [Google Scholar] [CrossRef] [PubMed]
- Ellis, M.D.; Sukal, T.; DeMott, T.; Dewald, J.P. ACT 3D exercise targets gravity-induced discoordination and improves reaching work area in individuals with stroke. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 12–15 June 2007; pp. 890–895. [Google Scholar]
- Stienen, A.H.; McPherson, J.G.; Schouten, A.C.; Dewald, J.P. The ACT-4D: A novel rehabilitation robot for the quantification of upper limb motor impairments following brain injury. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 29 June–1 July 2011; pp. 1–6. [Google Scholar]
- Singh, H.; Unger, J.; Zariffa, J.; Pakosh, M.; Jaglal, S.; Craven, B.C.; Musselman, K.E. Robot-assisted upper extremity rehabilitation for cervical spinal cord injuries: A systematic scoping review. Disabil. Rehabil. Assist. Technol. 2018, 13, 704–715. [Google Scholar] [CrossRef]
- Balasubramanian, S.; Wei, R.; Perez, M.; Shepard, B.; Koeneman, E.; Koeneman, J.; He, J. RUPERT: An exoskeleton robot for assisting rehabilitation of arm functions. In Proceedings of the 2008 Virtual Rehabilitation, Vancouver, BC, Canada, 25–27 August 2008; pp. 163–167. [Google Scholar]
- Fitle, K.D.; Pehlivan, A.U.; O’malley, M.K. A robotic exoskeleton for rehabilitation and assessment of the upper limb following incomplete spinal cord injury. In Proceedings of the 2015 IEEE International Conference on Robotics and Automation (ICRA), Seattle, WA, USA, 26–30 May 2015; pp. 4960–4966. [Google Scholar]
- Chang, S.R.; Hofland, N.; Chen, Z.; Tatsuoka, C.; Richards, L.G.; Bruestle, M.; Kovelman, H.; Naft, J. Myoelectric arm orthosis assists functional activities: A 3-month home use outcome report. Arch. Rehabil. Res. Clin. Transl. 2023, 5, 100279. [Google Scholar] [CrossRef] [PubMed]
- Garcia, D.A.; Arredondo, R.; Morris, M.; Tosunoglu, S. A review of rehabilitation strategies for stroke recovery. In Proceedings of the ASME Early Career Technical Conference, Atlanta, GA, USA, 30 July–1 August 2012; pp. 2–3. [Google Scholar]
- Perry, J.C.; Rosen, J.; Burns, S. Upper-limb powered exoskeleton design. IEEE/ASME Trans. Mechatron. 2007, 12, 408–417. [Google Scholar] [CrossRef]
- Nef, T.; Mihelj, M.; Kiefer, G.; Perndl, C.; Muller, R.; Riener, R. ARMin-Exoskeleton for arm therapy in stroke patients. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 12–15 June 2007; pp. 68–74. [Google Scholar]
- Nef, T.; Guidali, M.; Klamroth-Marganska, V.; Riener, R. ARMin-exoskeleton robot for stroke rehabilitation. In Proceedings of the World Congress on Medical Physics and Biomedical Engineering, Munich, Germany, 7–12 September 2009: Vol. 25/9 Neuroengineering, Neural Systems, Rehabilitation and Prosthetics; Springer: Berlin/Heidelberg, Germany, 2009; pp. 127–130. [Google Scholar]
- Gopura, R.A.R.C.; Kiguchi, K.; Li, Y. SUEFUL-7: A 7DOF upper-limb exoskeleton robot with muscle-model-oriented EMG-based control. In Proceedings of the 2009 IEEE/RSJ International Conference on Intelligent Robots and Systems, St. Louis, MO, USA, 11–15 October 2009; pp. 1126–1131. [Google Scholar]
- Perry, J.C.; Powell, J.M.; Rosen, J. Isotropy of an upper limb exoskeleton and the kinematics and dynamics of the human arm. Appl. Bionics Biomech. 2009, 6, 175–191. [Google Scholar] [CrossRef]
- El-Shamy, S.M. Efficacy of Armeo® robotic therapy versus conventional therapy on upper limb function in children with hemiplegic cerebral palsy. Am. J. Phys. Med. Rehabil. 2018, 97, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Hyakutake, K.; Morishita, T.; Saita, K.; Fukuda, H.; Shiota, E.; Higaki, Y.; Inoue, T.; Uehara, Y. Effects of Home-Based Robotic Therapy Involving the Single-Joint Hybrid Assistive Limb Robotic Suit in the Chronic Phase of Stroke: A Pilot Study. BioMed Res. Int. 2019, 2019, 5462694. [Google Scholar] [CrossRef]
- van Delden, A.E.; Peper, C.E.; Kwakkel, G.; Beek, P.J. A systematic review of bilateral upper limb training devices for poststroke rehabilitation. Stroke Res. Treat. 2012, 2012, 972069. [Google Scholar] [CrossRef] [PubMed]
- Proietti, T.; Crocher, V.; Roby-Brami, A.; Jarrasse, N. Upper-limb robotic exoskeletons for neurorehabilitation: A review on control strategies. IEEE Rev. Biomed. Eng. 2016, 9, 4–14. [Google Scholar] [CrossRef] [PubMed]
- Krebs, H.I.; Edwards, D.J.; Volpe, B.T. Forging mens et manus: The mit experience in upper extremity robotic therapy. In Neurorehabilitation Technology; Springer: Cham, Switzerland, 2022; pp. 597–621. [Google Scholar]
- Reinkensmeyer, D.J.; Kahn, L.E.; Averbuch, M.; McKenna-Cole, A.; Schmit, B.D.; Rymer, W.Z. Understanding and treating arm movement impairment after chronic brain injury: Progress with the ARM guide. J. Rehabil. Res. Dev. 2000, 37, 653–662. [Google Scholar] [PubMed]
- Sadeghnejad, S.; Abadi, V.S.E.; Jafari, B. Rehabilitation robotics: History, applications, and recent advances. In Medical and Healthcare Robotics; Academic Press: Cambridge, MA, USA, 2023; pp. 63–85. [Google Scholar]
- Rosati, G.; Gallina, P.; Masiero, S. Design, implementation and clinical tests of a wire-based robot for neurorehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2007, 15, 560–569. [Google Scholar] [CrossRef]
- Rosati, G.; Gallina, P.; Masiero, S.; Rossi, A. Design of a new 5 dof wire-based robot for rehabilitation. In Proceedings of the 9th International Conference on Rehabilitation RoboticsICORR 2005, Chicago, IL, USA, 28 June–1 July 2005; pp. 430–433. [Google Scholar]
- Lum, P.S.; Burgar, C.G.; Shor, P.C. Evidence for improved muscle activation patterns after retraining of reaching movements with the MIME robotic system in subjects with post-stroke hemiparesis. IEEE Trans. Neural Syst. Rehabil. Eng. 2004, 12, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Burgar, C.G.; Scremin, A.E.; Garber, S.L.; Van der Loos, H.M.; Deborah Kenney, O.T.R. Robot-assisted upper-limb therapy in acute rehabilitation setting following stroke: Department of Veterans Affairs multisite clinical trial. J. Rehabil. Res. Dev. 2011, 48, 445. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, Y.W.; Liing, R.J.; Lin, K.C.; Wu, C.Y.; Liou, T.H.; Lin, J.C.; Hung, J.W. Sequencing bilateral robot-assisted arm therapy and constraint-induced therapy improves reach to press and trunk kinematics in patients with stroke. J. Neuroeng. Rehabil. 2016. [Google Scholar] [CrossRef]
- Wu, C.Y.; Yang, C.L.; Chen, M.D.; Lin, K.C.; Wu, L.L. Unilateral versus bilateral robot-assisted rehabilitation on arm-trunk control and functions post stroke: A randomized controlled trial. J. Neuroeng. Rehabil. 2013, 10, 35. [Google Scholar] [CrossRef] [PubMed]
- Amirabdollahian, F.; Loureiro, R.; Gradwell, E.; Collin, C.; Harwin, W.; Johnson, G. Multivariate analysis of the Fugl-Meyer outcome measures assessing the effectiveness of GENTLE/S robot-mediated stroke therapy. J. Neuroeng. Rehabil. 2007, 4, 4. [Google Scholar] [CrossRef] [PubMed]
- van der Linde, R.Q.; Lammertse, P. HapticMaster–a generic force controlled robot for human interaction. Ind. Robot. Int. J. 2003, 30, 515–524. [Google Scholar] [CrossRef]
- Van der Linde, R.Q.; Lammertse, P.; Frederiksen, E.; Ruiter, B. The HapticMaster, a new high-performance haptic interface. In Proc. Eurohaptics; Edinburgh University: Edinburgh, UK, 2002; pp. 1–5. [Google Scholar]
- Timmermans, A.A.; Lemmens, R.J.; Monfrance, M.; Geers, R.P.; Bakx, W.; Smeets, R.J.; Seelen, H.A. Effects of task-oriented robot training on arm function, activity, and quality of life in chronic stroke patients: A randomized controlled trial. J. Neuroeng. Rehabil. 2014, 11, 45. [Google Scholar] [CrossRef]
- Fazekas, G.; Horvath, M.; Troznai, T.; Toth, A. Robot-mediated upper limb physiotherapy for patients with spastic hemiparesis: A preliminary study. J. Rehabil. Med. 2007, 39, 580–582. [Google Scholar] [CrossRef]
- Bratanov, D.; Vitliemov, P. The experience behind the reharob project–a new robotic system for simultaneous rehabilitation of upper and lower human limbs. In Proceedings of the 2020 International Conference on Assistive and Rehabilitation Technologies (iCareTech), Gaza, Palestine, 28–29 August 2020; pp. 19–23. [Google Scholar]
- Ellis, M.D.; Dewald, J.P. Application of the ACT 3D Robot in the Evaluation of Functional Reaching Performance and the Administration of Experimental Interventions. In Proceedings of the World Congress on Medical Physics and Biomedical Engineering, Munich, Germany, 7–12 September 2009: Vol. 25/9 Neuroengineering, Neural Systems, Rehabilitation and Prosthetics; Springer: Berlin/Heidelberg, Germany, 2009; pp. 374–376. [Google Scholar]
- Serrano-Lopez-Terradas, P.A.; Seco-Rubio, R. Effectiveness of robotic therapy in the proximal and distal rehabilitation of the upper limb in patients after stroke using the Amadeo® and Armeo® devices: A systematic review of randomized clinical trials (Efectividad de la terapia robótica en la rehabilitación proximal y distal del miembro superior en personas tras un ictus con los dispositivos Amadeo® y Armeo®: Una revisión sistemática de ensayos clínicos aleatorizados). Stud. Psychol. 2022, 43, 132–178. [Google Scholar]
- Helbok, R.; Schoenherr, G.; Spiegel, M.; Sojer, M.; Brenneis, C. Robot-Assisted Hand Training (Amadeo) Compared with Conventional Physiotherapy Techniques in Chronic Ischemic Stroke Patients: A Pilot Study; DGNR: Bremen, Germany, 2010. [Google Scholar]
- Serrano-López Terradas, P.A.; Criado Ferrer, T.; Jakob, I.; Calvo-Arenillas, J.I. Quo Vadis, Amadeo Hand Robot? A Randomized Study with a Hand Recovery Predictive Model in Subacute Stroke. Int. J. Environ. Res. Public Health 2022, 20, 690. [Google Scholar] [CrossRef] [PubMed]
- López-Terradas, P.A.S.; Rosendo, D.M.; Lago, M.R. Hand Functional Recovery in Sub-acute Brain Injury Stage Patients using AMADEO® Robotic-assisted Therapy-A Pilot Clinical Study with Apraxic and Neglect Patients. In Special Session on Virtual and Augmented Reality Systems for Upper Limbs Rehabilitation; Scitepress: Setúbal, Portugal, 2013; Volume 1. [Google Scholar]
- Colombo, R.; Sterpi, I.; Mazzone, A.; Delconte, C.; Pisano, F. Taking a lesson from patients’ recovery strategies to optimize training during robot-aided rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2012, 20, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Vergaro, E.; Casadio, M.; Squeri, V.; Giannoni, P.; Morasso, P.; Sanguineti, V. Self-adaptive robot training of stroke survivors for continuous tracking movements. J. Neuroeng. Rehabil. 2010, 7, 13. [Google Scholar] [CrossRef][Green Version]
- Casadio, M.; Sanguineti, V.; Morasso, P.G.; Arrichiello, V. Braccio di Ferro: A new haptic workstation for neuromotor rehabilitation. Technol. Health Care 2006, 14, 123–142. [Google Scholar] [CrossRef]
- Elangovan, N.; Yeh, I.L.; Holst-Wolf, J.; Konczak, J. A robot-assisted sensorimotor training program can improve proprioception and motor function in stroke survivors. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; pp. 660–664. [Google Scholar]
- Albanese, G.A.; Taglione, E.; Gasparini, C.; Grandi, S.; Pettinelli, F.; Sardelli, C.; Catitti, P.; Sandini, G.; Masia, L.; Zenzeri, J. Efficacy of wrist robot-aided orthopedic rehabilitation: A randomized controlled trial. J. Neuroeng. Rehabil. 2021, 18, 130. [Google Scholar] [CrossRef] [PubMed]
- Konczak, J. WristBot: A Robotic System for the Diagnosis and Physical Rehabilitation of Sensory and Motor Dysfunction of the Wrist and Hand. 2024. Available online: https://news.cehd.umn.edu/konczak-receives-grant-to-advance-robotic-rehabilitation-technology/ (accessed on 24 November 2024).
- Passon, A.; Schauer, T.; Seel, T. Inertial-robotic motion tracking in end-effector-based rehabilitation robots. Front. Robot. AI 2020, 7, 554639. [Google Scholar] [CrossRef]
- MOTIONrehab. Robot-Assisted Arm Rehabilitation with DIEGO. 2024. Available online: https://www.motionrehab.co.uk/intensive-neurological-rehabilitation-centre/diego/ (accessed on 27 November 2024).
- Saracino, L.; Avizzano, C.A.; Ruffaldi, E.; Cappiello, G.; Curto, Z.; Scoglio, A. MOTORE++ a portable haptic device for domestic rehabilitation. In Proceedings of the IECON 2016-42nd Annual Conference of the IEEE Industrial Electronics Society, Florence, Italy, 24–27 October 2016; pp. 728–734. [Google Scholar]
- O’Flaherty, D.; Ali, K. Recommendations for upper limb motor recovery: An overview of the UK and European rehabilitation after stroke guidelines (2023). Healthcare 2024, 12, 1433. [Google Scholar] [CrossRef]
- Irgens, E.L.; Henriksen, N.; Moe, S. Variations in physiotherapy practice in neurological rehabilitation trajectories–an explorative interview and observational study. Physiother. Theory Pract. 2020, 36, 95–107. [Google Scholar] [CrossRef]
- Harmelink, K.; Dandis, R.; der Van der Wees Pj, P.; Zeegers, A.; der Sanden, M.N.V.; Staal, J. Recovery trajectories over six weeks in patients selected for a high-intensity physiotherapy program after Total knee Arthroplasty: A latent class analysis. BMC Musculoskelet. Disord. 2021, 22, 179. [Google Scholar] [CrossRef]
- Coratti, G.; Pera, M.C.; Montes, J.; Pasternak, A.; Scoto, M.; Baranello, G.; Messina, S.; Dunaway Young, S.; Glanzman, A.M.; Duong, T.; et al. Different trajectories in upper limb and gross motor function in spinal muscular atrophy. Muscle Nerve 2021, 64, 552–559. [Google Scholar] [CrossRef]
- de Assis, I.S.A.; Luvizutto, G.J.; Bruno, A.C.M.; de Souza, L.A.P.S. The proprioceptive neuromuscular facilitation concept in parkinson disease: A systematic review and meta-analysis. J. Chiropr. Med. 2020, 19, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Adler, S.S.; Beckers, D.; Buck, M. PNF in Practice: An Illustrated Guide; Springer: Berlin/Heidelberg, Germany, 2007. [Google Scholar]
- Chaturvedi, P.; Singh, A.K.; Kulshreshtha, D.; Thacker, A.K. PNF in acute stroke. MOJ Anat. Physiol. 2018, 5, 391–399. [Google Scholar] [CrossRef]
- Babaiasl, M.; Mahdioun, S.H.; Jaryani, P.; Yazdani, M. A review of technological and clinical aspects of robot-aided rehabilitation of upper-extremity after stroke. Disabil. Rehabil. Assist. Technol. 2016, 11, 263–280. [Google Scholar] [CrossRef]
- Le Danseur, M. Stroke rehabilitation. Crit. Care Nurs. Clin. 2020, 32, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Fu, Q.; Tyson, S.; Preston, N.; Weightman, A. A scoping review of design requirements for a home-based upper limb rehabilitation robot for stroke. Top. Stroke Rehabil. 2022, 29, 449–463. [Google Scholar] [CrossRef] [PubMed]
- Casals, A. Adaptive control in neurorehabilitation. In Converging Clinical and Engineering Research on Neurorehabilitation; Springer: Berlin/ Heidelberg, Germany, 2013; pp. 123–127. [Google Scholar]
- Maciejasz, P.; Eschweiler, J.; Gerlach-Hahn, K.; Jansen-Troy, A.; Leonhardt, S. A survey on robotic devices for upper limb rehabilitation. J. Neuroeng. Rehabil. 2014, 11, 3. [Google Scholar] [CrossRef] [PubMed]
- Yeh, T.N.; Chou, L.W. Clinical Demands of Designs for Rehabilitation Robots in Taiwan. Innovation 2022, 1, 42–47. [Google Scholar] [CrossRef]
- Richardson, R.; Brown, M.; Bhakta, B.; Levesley, M. Design and control of a three degree of freedom pneumatic physiotherapy robot. Robotica 2003, 21, 589–604. [Google Scholar] [CrossRef]
- Akdoğan, E.; Aktan, M.E.; Koru, A.T.; Arslan, M.S.; Atlıhan, M.; Kuran, B. Hybrid impedance control of a robot manipulator for wrist and forearm rehabilitation: Performance analysis and clinical results. Mechatronics 2018, 49, 77–91. [Google Scholar] [CrossRef]
- Hesse, S.; Schmidt, H.; Werner, C. Machines to support motor rehabilitation after stroke: 10 years of experience in Berlin. J. Rehabil. Res. Dev. 2006, 43, 671. [Google Scholar] [CrossRef]
- Loureiro, R.C.; Harwin, W.S. Reach & grasp therapy: Design and control of a 9-DOF robotic neuro-rehabilitation system. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007; pp. 757–763. [Google Scholar]
- Tóth, A.; Arz, G.; Fazekas, G.; Bratanov, D.; Zlatov, N. 25 Post stroke shoulder-elbow physiotherapy with industrial robots. In Advances in Rehabilitation Robotics: Human-Friendly Technologies on Movement Assistance and Restoration for People with Disabilities; Springer: Berlin/Heidelberg, Germany, 2004; pp. 391–411. [Google Scholar]
- Yao, J.; Sheaff, C.; Dewald, J.P. Usage of the ACT 3D Robot in a Brain Machine Interface for Hand Opening and Closing in Stroke Survivors. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 12–15 June 2007; pp. 938–942. [Google Scholar]
- Huang, X.; Naghdy, F.; Du, H.; Naghdy, G.; Todd, C. Temporal difference (TD) based critic-actor adaptive control for a fine hand motion rehabilitation robot. In Mechatronics and Machine Vision in Practice 3; Springer: Cham, Switzerland, 2018; pp. 195–207. [Google Scholar]
- Pippo, I.; Albanese, G.A.; Zenzeri, J.; Torazza, D.; Berselli, G. Understanding human–robot interaction forces: A new mechanical solution. Int. J. Interact. Des. Manuf. (IJIDeM) 2024, 18, 4765–4774. [Google Scholar] [CrossRef]
- Fareh, R.; Elsabe, A.; Baziyad, M.; Kawser, T.; Brahmi, B.; Rahman, M.H. Will your next therapist be a robot?—A review of the advancements in robotic upper extremity rehabilitation. Sensors 2023, 23, 5054. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Zhang, J.; Zuo, G.; Feng, G.; Zhang, X. Assist-as-needed control strategy of bilateral upper limb rehabilitation robot based on GMM. Machines 2022, 10, 76. [Google Scholar] [CrossRef]
- Guatibonza, A.; Solaque, L.; Velasco, A.; Peñuela, L. Assistive Robotics for Upper Limb Physical Rehabilitation: A Systematic Review and Future Prospects. Chin. J. Mech. Eng. 2024, 37, 69. [Google Scholar] [CrossRef]
- Bauer, G.; Pan, Y.J. Review of control methods for upper limb telerehabilitation with robotic exoskeletons. IEEE Access 2020, 8, 203382–203397. [Google Scholar] [CrossRef]
- Li, L.; Han, J.; Li, X.; Guo, B.; Wang, X.; Du, G. A novel end-effector upper limb rehabilitation robot: Kinematics modeling based on dual quaternion and low-speed spiral motion tracking control. Int. J. Adv. Robot. Syst. 2022, 19, 17298806221118855. [Google Scholar] [CrossRef]
- Maithani, H.; Ramon, J.A.C.; Mezouar, Y. Predicting human intent for cooperative physical human-robot interaction tasks. In Proceedings of the 2019 IEEE 15th International Conference on Control and Automation (ICCA), Edinburgh, UK, 16–19 July 2019; pp. 1523–1528. [Google Scholar]
- Khan, M.M.R.; Swapnil, A.A.Z.; Ahmed, T.; Rahman, M.M.; Islam, M.R.; Brahmi, B.; Fareh, R.; Rahman, M.H. Development of an end-effector type therapeutic robot with sliding mode control for upper-limb rehabilitation. Robotics 2022, 11, 98. [Google Scholar] [CrossRef]
- Wang, J.; Li, Y. Hybrid impedance control of a 3-DOF robotic arm used for rehabilitation treatment. In Proceedings of the 2010 IEEE International Conference on Automation Science and Engineering, Toronto, ON, Canada, 21–24 August 2010; pp. 768–773. [Google Scholar]
- Papaleo, E.; Zollo, L.; Spedaliere, L.; Guglielmelli, E. Patient-tailored adaptive robotic system for upper-limb rehabilitation. In Proceedings of the 2013 IEEE International Conference on Robotics and Automation, Karlsruhe, Germany, 6–10 May 2013; pp. 3860–3865. [Google Scholar]
- Zhang, J.; Cheah, C.C. Passivity and stability of human–robot interaction control for upper-limb rehabilitation robots. IEEE Trans. Robot. 2015, 31, 233–245. [Google Scholar] [CrossRef]
- Luo, L.; Peng, L.; Hou, Z.; Wang, W. An adaptive impedance controller for upper limb rehabilitation based on estimation of patients’ stiffness. In Proceedings of the 2017 IEEE International Conference on Robotics and Biomimetics (ROBIO), Macau, China, 5–8 December 2017; pp. 532–537. [Google Scholar]
- Li, X.; Liu, Y.H.; Yu, H. Adaptive impedance control for compliantly actuated robots with a unified safety measure. In Proceedings of the 2018 13th World Congress on Intelligent Control and Automation (WCICA), Changsha, China, 4–8 July 2018; pp. 444–449. [Google Scholar]
- Zhang, L.; Guo, S.; Sun, Q. Development and assist-as-needed control of an end-effector upper limb rehabilitation robot. Appl. Sci. 2020, 10, 6684. [Google Scholar] [CrossRef]
- Zhang, L.; Guo, S.; Xi, F. Performance-based assistance control for robot-mediated upper-limbs rehabilitation. Mechatronics 2023, 89, 102919. [Google Scholar] [CrossRef]
- Guatibonza, A.; Solaque, L.; Velasco, A.; Penuela, L. Hybrid Impedance and Nonlinear Adaptive Control for a 7-DoF Upper Limb Rehabilitation Robot: Formulation and Stability Analysis. In Proceedings of the ICINCO, Paris, France, 6–8 July 2021; pp. 685–692. [Google Scholar]
- Sidek, S.N.; Fatai, S. Design and Control of a 3D Robot-Assisted Rehabilitation Device for Post-Stroke. In Control Engineering in Robotics and Industrial Automation: Malaysian Society for Automatic Control Engineers (MACE) Technical Series 2018; Springer: Cham, Switzerland, 2022; pp. 5–18. [Google Scholar]
- Arantes, A.P.; Bressan, N.; Borges, L.R.; McGibbon, C.A. Evaluation of a novel real-time adaptive assist-as-needed controller for robot-assisted upper extremity rehabilitation following stroke. PLoS ONE 2023, 18, e0292627. [Google Scholar] [CrossRef]
- Mathavan Jeyabalan, P.K.; Nehrujee, A.; Elias, S.; Magesh Kumar, M.; Sujatha, S.; Balasubramanian, S. Design and Characterization of a Self-Aligning End-Effector Robot for Single-Joint Arm Movement Rehabilitation. Robotics 2023, 12, 149. [Google Scholar] [CrossRef]
- Lai, Y.; Sutjipto, S.; Clout, M.D.; Carmichael, M.G.; Paul, G. GAVRe 2: Towards data-driven upper-limb rehabilitation with adaptive-feedback gamification. In Proceedings of the 2018 IEEE International Conference on Robotics and Biomimetics (ROBIO), Kuala Lumpur, Malaysia, 12–15 December 2018; pp. 164–169. [Google Scholar]
- Mashayekhi, M.; Moghaddam, M.M. EMG-driven fatigue-based self-adapting admittance control of a hand rehabilitation robot. J. Biomech. 2022, 138, 111104. [Google Scholar] [CrossRef]
- Cai, S.; Xie, P.; Li, G.; Xie, L. Compensation-corrective adaptive control strategy for upper-limb rehabilitation robots. Robot. Auton. Syst. 2024, 177, 104701. [Google Scholar] [CrossRef]
- Xu, G.; Song, A. Adaptive impedance control based on dynamic recurrent fuzzy neural network for upper-limb rehabilitation robot. In Proceedings of the 2009 IEEE International Conference on Control and Automation, Christchurch, New Zealand, 9–11 December 2009; pp. 1376–1381. [Google Scholar]
- Xu, G.; Song, A.; Li, H. Adaptive impedance control for upper-limb rehabilitation robot using evolutionary dynamic recurrent fuzzy neural network. J. Intell. Robot. Syst. 2011, 62, 501–525. [Google Scholar] [CrossRef]
- Xu, G.; Song, A.; Li, H. Control system design for an upper-limb rehabilitation robot. Adv. Robot. 2011, 25, 229–251. [Google Scholar] [CrossRef]
- Bai, J.; Song, A.; Wang, T.; Li, H. A novel backstepping adaptive impedance control for an upper limb rehabilitation robot. Comput. Electr. Eng. 2019, 80, 106465. [Google Scholar] [CrossRef]
- Wang, C.; Peng, L.; Hou, Z.G.; Wang, W.; Su, T. A novel assist-as-needed controller based on fuzzy-logic inference and human impedance identification for upper-limb rehabilitation. In Proceedings of the 2019 IEEE Symposium Series on Computational Intelligence (SSCI), Xiamen, China, 6–9 December 2019; pp. 1133–1139. [Google Scholar]
- Li, X.; Yang, Q.; Song, R. Performance-based hybrid control of a cable-driven upper-limb rehabilitation robot. IEEE Trans. Biomed. Eng. 2020, 68, 1351–1359. [Google Scholar] [CrossRef]
- Hu, Y.; Meng, J.; Li, G.; Zhao, D.; Feng, G.; Zuo, G.; Liu, Y.; Zhang, J.; Shi, C. Fuzzy Adaptive Passive Control Strategy Design for Upper-Limb End-Effector Rehabilitation Robot. Sensors 2023, 23, 4042. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Chen, B.; Wu, H. Adaptive admittance control of an upper extremity rehabilitation robot with neural-network-based disturbance observer. IEEE Access 2019, 7, 123807–123819. [Google Scholar] [CrossRef]
- Ting, W.; Aiguo, S. An adaptive iterative learning based impedance control for robot-aided upper-limb passive rehabilitation. Front. Robot. AI 2019, 6, 41. [Google Scholar] [CrossRef]
- Miao, Q.; Li, Z.; Chu, K.; Liu, Y.; Peng, Y.; Xie, S.; Zhang, M. Performance-based iterative learning control for task-oriented rehabilitation: A pilot study in robot-assisted bilateral training. IEEE Trans. Cogn. Dev. Syst. 2021, 15, 2031–2040. [Google Scholar] [CrossRef]
- Shoaib, M.; Asadi, E.; Cheong, J.; Bab-Hadiashar, A. Cable driven rehabilitation robots: Comparison of applications and control strategies. IEEE Access 2021, 9, 110396–110420. [Google Scholar] [CrossRef]
- Hashemi, A.; McPhee, J. Assistive sliding mode control of a rehabilitation robot with automatic weight adjustment. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Virtual, 1–5 November 2021; pp. 4891–4896. [Google Scholar]
- Wu, Q.; Chen, Y. Development of an intention-based adaptive neural cooperative control strategy for upper-limb robotic rehabilitation. IEEE Robot. Autom. Lett. 2020, 6, 335–342. [Google Scholar] [CrossRef]
- Abbas, M.; Narayan, J.; Dwivedy, S.K. Event-triggered adaptive control for upper-limb robot-assisted passive rehabilitation exercises with input delay. Proc. Inst. Mech. Eng. Part I J. Syst. Control Eng. 2022, 236, 832–845. [Google Scholar] [CrossRef]
- Abbas, M.; Narayan, J.; Dwivedy, S.K. Event-triggered adaptive control for upper-extremity therapeutic robot in active-assist mode: A simulation study. Proc. Inst. Mech. Eng. Part C J. Mech. Eng. Sci. 2024, 238, 4628–4643. [Google Scholar] [CrossRef]
- Sharifi, M.; Behzadipour, S.; Vossoughi, G. Model reference adaptive impedance control of rehabilitation robots in operational space. In Proceedings of the 2012 4th IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics (BioRob), Rome, Italy, 24–27 June 2012; pp. 1698–1703. [Google Scholar]
- Sharifi, M.; Behzadipour, S.; Vossoughi, G. Model reference adaptive impedance control in Cartesian coordinates for physical human–robot interaction. Adv. Robot. 2014, 28, 1277–1290. [Google Scholar] [CrossRef]
- Omrani, J.; Moghaddam, M.M. Nonlinear time delay estimation based model reference adaptive impedance control for an upper-limb human-robot interaction. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2022, 236, 385–398. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.R.; Spiewak, C.; Rahman, M.H.; Fareh, R. A brief review on robotic exoskeletons for upper extremity rehabilitation to find the gap between research porotype and commercial type. Adv. Robot. Autom. 2017, 6, 10-4172. [Google Scholar] [CrossRef]


| EE Robot | Trajectory | DoF | Therapy Intensity | Control | Feedback | Potability | Interactive Games |
|---|---|---|---|---|---|---|---|
| MIT Manus [15] | RTT planar motion | 2 | 3 h/wk for 12 wks [15] | Impedance control [60,80,81] | Handle torque and position, joint position, velocity, and torque | ✗ | ✓ InMotion |
| ARM-Guide [17] | Reaching motion, linear motion | 1 | 3 h/wk for 8 wks [39] | PD control [81] | Forearm position and torque | ✗ | N/A |
| NeReBot [21] | Cable-driven motion | 2 | ≈5 h/wk for 4 wks [42] | PID control [42] | Motor positions | ✗ | N/A |
| MIME [18] | Bi-manual Motion | 6 | 3 h/wk for 8 wks [43] | PID control [81] | Forearm pose and torque | ✗ | N/A |
| Bi-Manu-Track [19] | Bi-manual motion | 2 | 6 h/wk for 3 wks [45] | Position/force control [82] | Visual and force | ✗ | ✓ |
| GENTLE-/s [20] | 3D motion | 3 | 3 h/wk for 9 wks [47] | Admittance control [83] | End-point torque, position, and velocity | ✗ | ✓ |
| HAPTIC MASTER [49] | 3D motion | 3 | 4 h/wk for 8 wks [50] | Admittance control [83] | End-point torque, position, and velocity | ✗ | ✓ |
| REHA-ROB [51] | 3D motion | 3 | ≈1 h for 20 days [51] | Indirect Force control [84] | End-point torques | ✗ | N/A |
| [22] | Reaching motion, planar motion | 3 | 3 h/wk for 8 wks [53] | Force control [85] | End-point torque, position, and velocity | ✗ | N/A |
| Amadeo [54] | Hand mobility | 5 | 3 h/wk for 10 wks [56] | Position control [86] | End-point position and force | ✓ | ✓ |
| Braccio di Ferro [58] | Planar motion | 2 | 6–12 sessions [59] | Impedance control [60,80,81] | Joint angles and end-point force | ✗ | ✓ |
| Wristbot [61] | 3D motion | 3 | 5 h/wk for 3 wks [62] | Impedance control [87] | Handle force and position and motor torque | ✓ | ✓ |
| Diego [64] | Cable-driven motion | 3 | 3–5 h/wk | N/A | Forearm pose | ✗ | ✓ |
| MOTORE [66] | Mobile planar motion | 3 | 3–5 h/wk | N/A | N/A | ✓ | ✓ |
| Controller | Class | Advantages | Disadvantages |
|---|---|---|---|
| PID [81,92] | Model-based | - Simple | - Needs parameters tuning - Suffers from noise amplification - Nonoptimal and can be unstable |
| Impedance admittance [7,11,89,90,93] [60,80,81,83] | Model-based | - Tracks target position/force - Considers human interactive forces | - Sensitive to sudden changes - Unstable at high impedance |
| SMC [11,92,94] | Model-based | - Robust to uncertainties, nonlinearities, and disturbances - Stable | - Chattering effect |
| Adaptive impedance/admittance [95,96,97,98,99,100,101,102,103,104,105,106,107,108,108] | Model-based | - Adaptive performance - Tracks target position/force - Considers human interactive forces | - Not practical for large dimension systems |
| Fuzzy-based adaptive control [109,110,111,112,113,114,115] | Model-free | - Adaptive performance - Model independent - Robust to uncertainties and nonlinearities | - Highly dependent on the choice of fuzzy sets and rules - Adaptation for sets and rules is desirable |
| Machine learning-based adaptive control [14,116,117,118,119] | Data-driven |
- Adaptive performance - Model independent - Handles uncertainties and nonlinearities - Predicts models |
- Needs to be trained - Needs a large dataset - High computations - Overfitting problem |
| Robust adaptive control [120,121,122,123] | Model-based | - Robust to uncertainties, nonlinearities, and disturbances - Stable | - Chattering effect (SMC) - Slow response (backstepping) |
| MRAC [124,125,126] | Model-based |
- Adaptive performance - Tracks the reference model - Considers human interactive forces | - Depends on reference model |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahfouz, D.M.; Shehata, O.M.; Morgan, E.I.; Arrichiello, F. A Comprehensive Review of Control Challenges and Methods in End-Effector Upper-Limb Rehabilitation Robots. Robotics 2024, 13, 181. https://doi.org/10.3390/robotics13120181
Mahfouz DM, Shehata OM, Morgan EI, Arrichiello F. A Comprehensive Review of Control Challenges and Methods in End-Effector Upper-Limb Rehabilitation Robots. Robotics. 2024; 13(12):181. https://doi.org/10.3390/robotics13120181
Chicago/Turabian StyleMahfouz, Dalia M., Omar M. Shehata, Elsayed I. Morgan, and Filippo Arrichiello. 2024. "A Comprehensive Review of Control Challenges and Methods in End-Effector Upper-Limb Rehabilitation Robots" Robotics 13, no. 12: 181. https://doi.org/10.3390/robotics13120181
APA StyleMahfouz, D. M., Shehata, O. M., Morgan, E. I., & Arrichiello, F. (2024). A Comprehensive Review of Control Challenges and Methods in End-Effector Upper-Limb Rehabilitation Robots. Robotics, 13(12), 181. https://doi.org/10.3390/robotics13120181






