Assessing Flight Crew Fatigue under Extra Augmented Crew Schedule Using a Multimodality Approach
Abstract
:1. Introduction
2. Methods
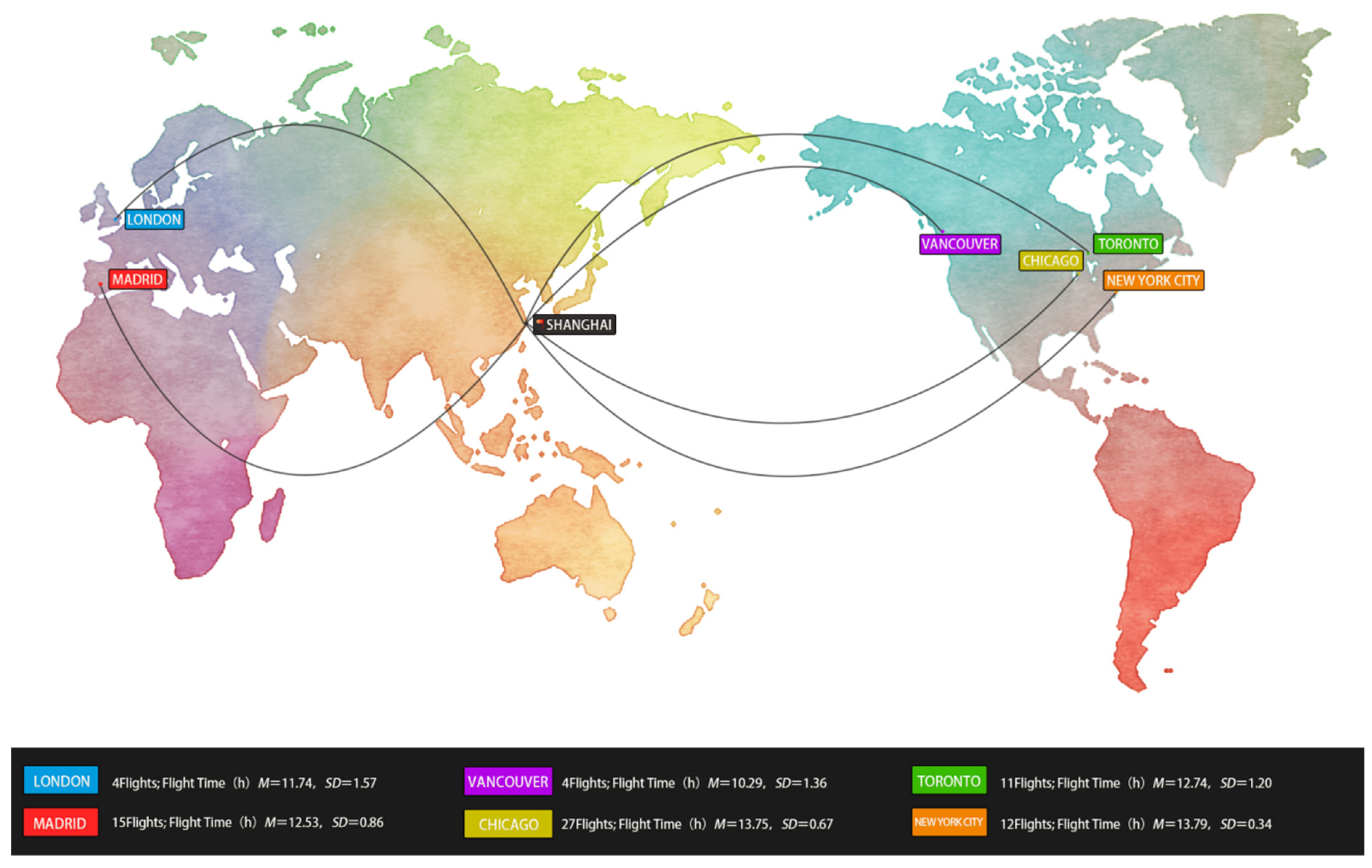
2.1. Participants
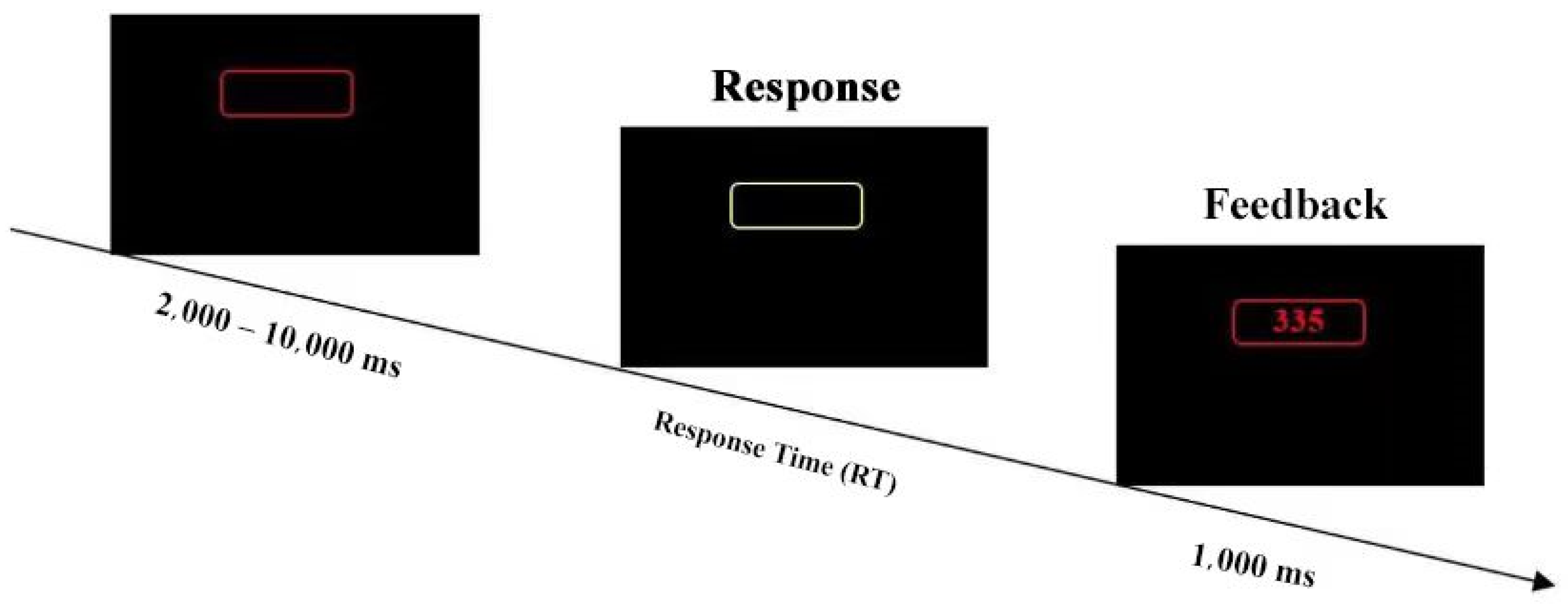
2.2. Equipment, Measures, and Tasks
2.3. Experimental Design and Procedure
2.4. Data Analysis
3. Results
3.1. Subjective Karolinska Sleepiness Scale (KSS)
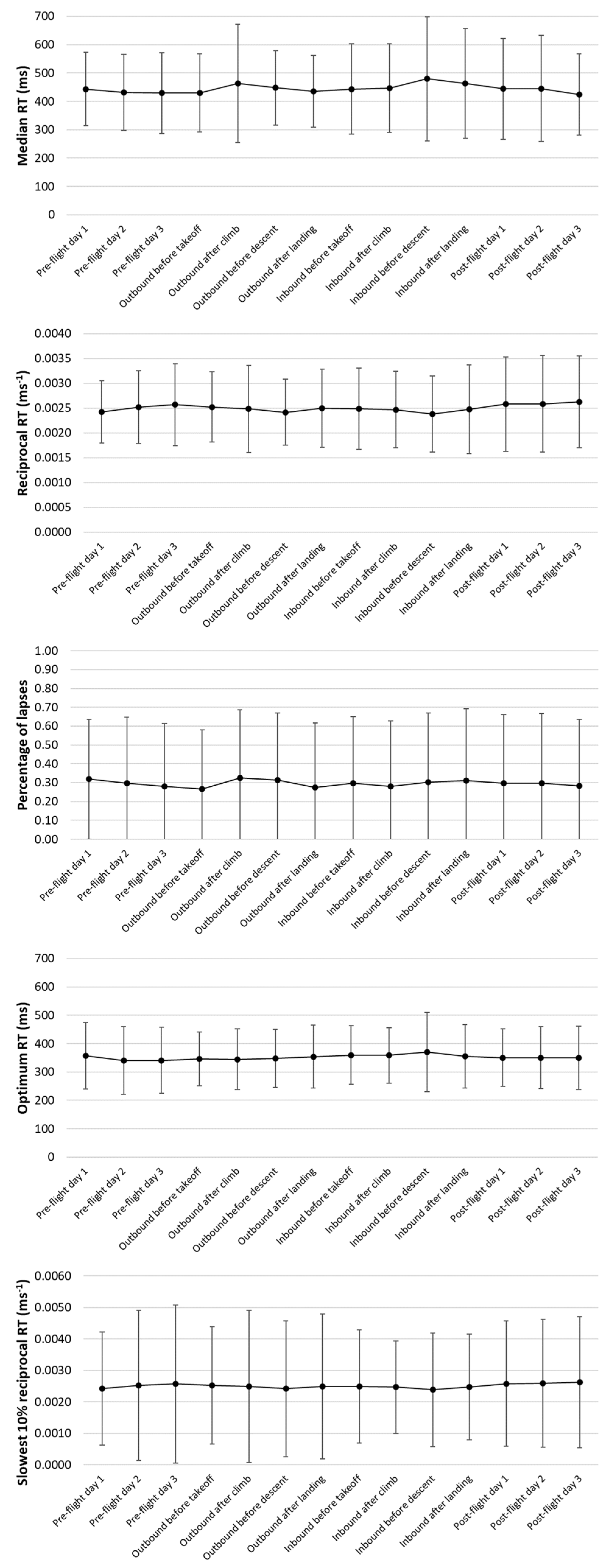
3.2. Psychomotor Vigilance Task (PVT)
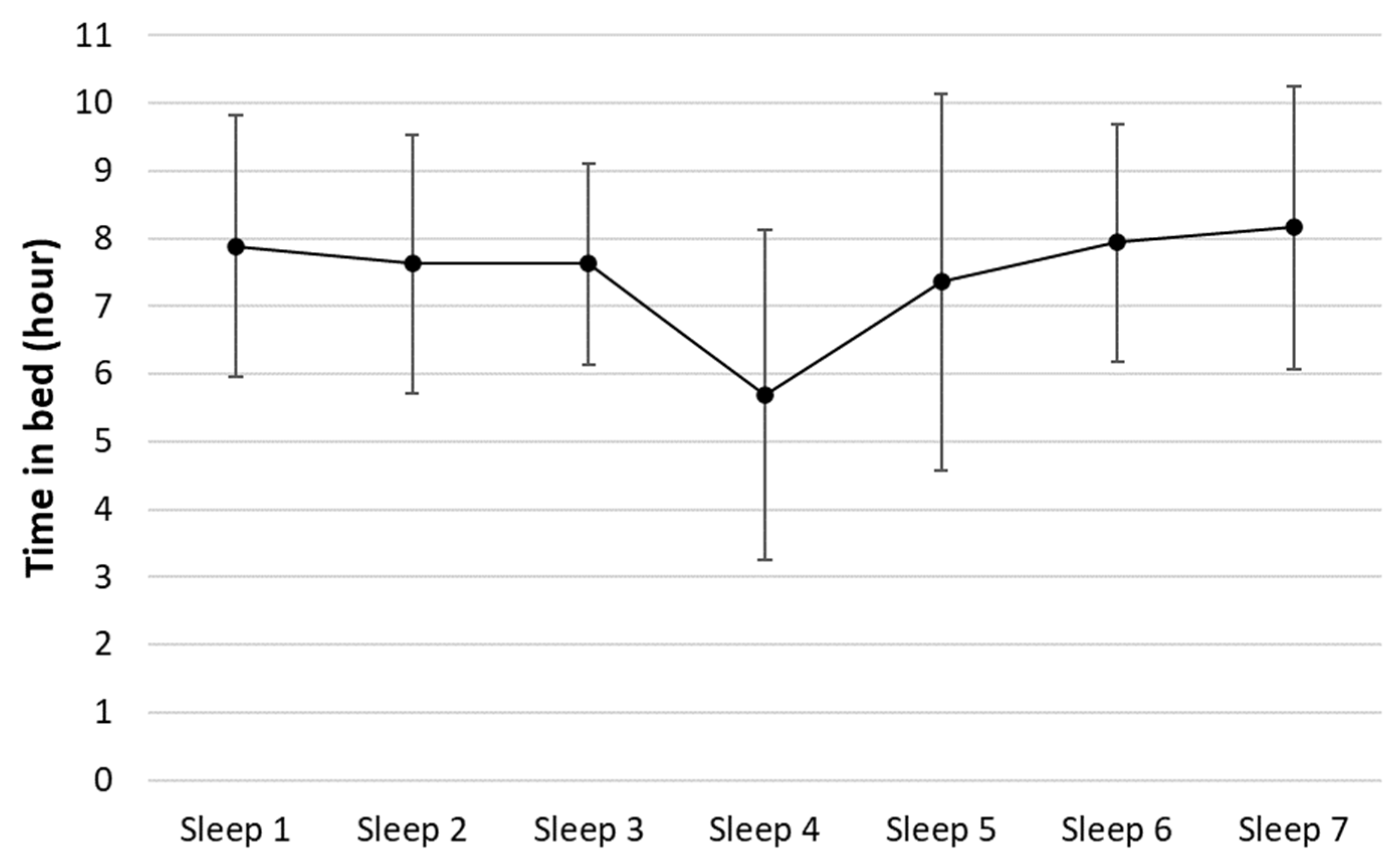
3.3. Sleep Quality
3.4. Biomathematical Models
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclaimers
Abbreviations
| ANOVA | Analysis of variance |
| BMM | Biomathematical models |
| CAAC | Civil Aviation Administration of China |
| CAS | Circadian rhythm simulator |
| COVID-19 | Coronavirus disease 2019 |
| EAC | Extra augmented crew |
| EEG | Electroencephalogram |
| FAID | Fatigue audit InterDyne |
| fMRI | Functional magnetic resonance imaging |
| FTL | FAID score tolerance level |
| ICAO | International Civil Aviation Organization |
| KSS | Karolinska Sleepiness Scale |
| KTL | KSS tolerance level |
| NIR | Near infrared |
| NREM | Non-rapid eye movement |
| NTSB | National Transportation Safety Board |
| PVT | Psychomotor vigilance task |
| REM | Rapid eye movement |
| RT | Response time |
| SAFE | Fatigue assessment system |
| SAFTE | Sleep, activity, fatigue and task effectiveness model |
| STL | Sleep tolerance level |
References
- Gander, P.H.; Mulrine, H.M.; van den Berg, M.J.; Smith, A.A.; Signal, T.L.; Wu, L.J.; Belenky, G. Effects of sleep/wake history and circadian phase on proposed pilot fatigue safety performance indicators. J. Sleep Res. 2015, 24, 110–119. [Google Scholar] [CrossRef]
- Hartzler, B.M. Fatigue on the flight deck: The consequences of sleep loss and the benefits of napping. Accid. Anal. Prev. 2014, 62, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, J.A. Fatigue in aviation. Travel Med. Infect. Dis. 2005, 3, 85–96. [Google Scholar] [CrossRef]
- Co, E.; Gregory, K.; Johnson, J.; Rosekind, M. Crew Factors in Flight Operations XI: A Survey of Fatigue Factors in Regional Airline Operations. 1999. Available online: https://www.researchgate.net/publication/244456816_Crew_Factors_in_Flight_Operations_XI_A_Survey_of_Fatigue_Factors_in_Regional_Airline_Operations (accessed on 15 December 2022).
- Aljaberi, M.A.; Alareqe, N.A.; Alsalahi, A.; Qasem, M.A.; Noman, S.; Uzir, M.U.H.; Mohammed, L.A.; Fares, Z.E.A.; Lin, C.Y.; Abdallah, A.M.; et al. A cross-sectional study on the impact of the COVID-19 pandemic on psychological outcomes: Multiple indicators and multiple causes modeling. PLoS ONE 2022, 17, e0277368. [Google Scholar] [CrossRef] [PubMed]
- International Air Transport Association (IATA). International Civil Aviation Organization (ICAO), and International Federation of Air Line Pilots’ Associations (IFALPA) “Fatigue Risk Management Systems (FRMS) Implementation Guide for Operators”; International Civil Aviation Organization: Montreal, QC, Canada, 2011. [Google Scholar]
- International Civil Aviation Organization (ICAO). Manual for the Oversight of Fatigue Management Approaches (Doc 9966); Civil Aviation Organization: Montreal, QC, Canada, 2020. [Google Scholar]
- Gander, P.; Hartley, L.; Powell, D.; Cabon, P.; Hitchcock, E.; Mills, A.; Popkin, S. Fatigue risk management: Organizational factors at the regulatory and industry/company level. Accid. Anal. Prev. 2011, 43, 573–590. [Google Scholar] [CrossRef]
- Cabon, P.; Deharvengt, S.; Grau, J.Y.; Maille, N.; Berechet, I.; Mollard, R. Research and guidelines for implementing Fatigue Risk Management Systems for the French regional airlines. Accid. Anal. Prev. 2012, 45 (Suppl. S), 41–44. [Google Scholar] [CrossRef]
- Avers, K.; Johnson, W.B. A review of federal aviation administration fatigue research. Aviat. Psychol. Appl. Hum. Factors 2011, 1, 87–98. [Google Scholar] [CrossRef]
- Fletcher, A.; Hooper, B.; Dunican, I.; Kogi, K. Fatigue management in safety-critical operations: History, terminology, management system frameworks, and industry challenges. Rev. Hum. Factors Ergon. 2015, 10, 6–28. [Google Scholar] [CrossRef]
- Shahid, A.; Shen, J.; Shapiro, C.M. Measurements of sleepiness and fatigue. J. Psychosom. Res. 2010, 69, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Rosekind, M.R.; Neri, D.F.; Dinges, D.F. From Laboratory to Flightdeck: Promoting Operational Alertness. Fatigue and Duty Limitations? An International Review. The Royal Aeronautical Society: London, UK, 1997; pp. 7.1–7.14. Available online: https://www.eurocockpit.be/sites/default/files/Rosekind-Neri-Dinges-1997.pdf (accessed on 15 December 2022).
- Luna, T.D.; French, J.; Mitcha, J.L. A study of USAF air traffic controller shiftwork: Sleep, fatigue, activity, and mood analyses. Aviat. Space Environ. Med. 1997, 68, 18–23. [Google Scholar]
- Marcus, J.H.; Rosekind, M.R. Fatigue in transportation: NTSB investigations and safety recommendations. Inj. Prev. 2017, 23, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Kharoufah, H.; Murray, J.; Baxter, G.; Wild, G. A review of human factors causations in commercial air transport accidents and incidents: From to 2000–2016. Prog. Aerosp. Sci. 2018, 99, 1–13. [Google Scholar] [CrossRef]
- Bourgeois-Bougrine, S.; Carbon, P.; Gounelle, C.; Mollard, R.; Coblentz, A. Perceived fatigue for short- and long-haul flights: A survey of 739 airline pilots. Aviat. Space Environ. Med. 2003, 74, 1072–1077. [Google Scholar]
- Mallis, M.M.; Mejdal, S.; Nguyen, T.T.; Dinges, D.F. Summary of the key features of seven biomathematical models of human fatigue and performance. Aviat. Space Environ. Med. 2004, 75 (Suppl. S3), A4–A14. [Google Scholar] [PubMed]
- Dang, J.; King, K.M.; Inzlicht, M. Why are self-report and behavioral measures weakly correlated? Sci. 2020, 24, 267–269. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Transport of the People’s Republic of China. Decision on Amending CCAR121, C.A.A.C. 2021. Available online: http://www.caac.gov.cn/XXGK/XXGK/MHGZ/202104/P020210506533065323228.pdf (accessed on 20 December 2022).
- Akerstedt, T.; Gillberg, M. Subjective and objective sleepiness in the active individual. Int. J. Neurosci. 1990, 52, 29–37. [Google Scholar] [CrossRef]
- Hursh, S.R.; Raslear, T.G.; Kaye, A.S.; Fanzone, J. Validation and Calibration of a Fatigue Assessment Tool for Railroad Work Schedules, Final Report (No. DOT/FRA/ORD-08/04); United States, Department of Transportation, Federal Railroad Administration, Office of Research and Development: Washington, DC, USA, 2007. Available online: https://railroads.dot.gov/sites/fra.dot.gov/files/fra_net/2899/ord0804.pdf (accessed on 20 December 2022).
- Kandelaars, K.J.; Dorrian, J.; Fletcher, A.; Roach, G.D.; Dawson, D. A review of bio-mathematical fatigue models: Where to from here? Presented at the 6th International Conference on Fatigue Management in Transportation, Seattle, WA, USA, 11–15 September 2005; Available online: https://www.researchgate.net/publication/259010642_A_review_of_biomathematical_fatigue_models_Where_to_from_here (accessed on 20 December 2022).
- Belyavin, A.J.; Spencer, M.B. Modeling performance and alertness: The QinetiQ approach. Aviation Space Environ. Med. 2004, 75 (Suppl. 3), A93–A106. [Google Scholar]
- Achermann, P. The two-process model of sleep regulation revisited. Aviat. Space Environ. Med. 2004, 75 (Suppl. S3), A37–A43. [Google Scholar]
- Moore-Ede, M.; Heitmann, A.; Guttkuhn, R.; Trutschel, U.; Aguirre, A.; Croke, D. Circadian alertness simulator for fatigue risk assessment in transportation: Application to reduce frequency and severity of truck accidents. Aviat. Space Environ. Med. 2004, 75 (Suppl. S3), A107–A118. [Google Scholar]
- Borbély, A.A. A two process model of sleep regulation. Hum. Neurobiol. 1982, 1, 195–204. [Google Scholar]
- Akerstedt, T.; Folkard, S. Predicting duration of sleep from the three process model of regulation of alertness. Occup. Environ. Med. 1996, 53, 136–141. [Google Scholar] [CrossRef]
- Miley, A.Å.; Kecklund, G.; Åkerstedt, T. Comparing two versions of the Karolinska Sleepiness Scale (KSS). Sleep Biol. Rhythm. 2016, 14, 257–260. [Google Scholar]
- Kaida, K.; Takahashi, M.; Åkerstedt, T.; Nakata, A.; Otsuka, Y.; Haratani, T.; Fukasawa, K. Validation of the Karolinska sleepiness scale against performance and EEG variables. Clinical Neurophysiol. 2006, 117, 1574–1581. [Google Scholar] [CrossRef]
- Akerstedt, T.; Anund, A.; Axelsson, J.; Kecklund, G. Subjective sleepiness is a sensitive indicator of insufficient sleep and impaired waking function. J. Sleep Res. 2014, 23, 240–252. [Google Scholar] [CrossRef] [PubMed]
- Dinges, D.F.; Powell, J.W. Microcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behav. Res. Methods Instrum. Comput. 1985, 17, 652–655. [Google Scholar] [CrossRef]
- Arsintescu, L.; Kato, K.H.; Hilditch, C.J.; Gregory, K.B.; Flynn-Evans, E. Collecting sleep, circadian, fatigue, and performance data in complex operational environments. J. Vis. Exp. 2019, 150, e59851. [Google Scholar] [CrossRef]
- Arsintescu, L.; Kato, K.H.; Cravalho, P.F.; Feick, N.H.; Stone, L.S.; Flynn-Evans, E.E. Validation of a touchscreen psychomotor vigilance task. Accid. Anal. Prev. 2019, 126, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Grant, D.A.; Honn, K.A.; Layton, M.E.; Riedy, S.M.; Van Dongen, H.P.A. 3-minute smartphone-based and tablet-based psychomotor vigilance tests for the assessment of reduced alertness due to sleep deprivation. Behav. Res. Methods 2017, 49, 1020–1029. [Google Scholar] [CrossRef]
- Roach, G.D.; Dawson, D.; Lamond, N. Can a shorter psychomotor vigilance task be used as a reasonable substitute for the ten-minute psychomotor vigilance task? Int. 2006, 23, 1379–1387. [Google Scholar] [CrossRef]
- Matsangas, P.; Shattuck, N.L. Hand-held and wrist-worn field-based PVT devices vs. the standardized laptop PVT. Aerosp. Med. Hum. Perform. 2020, 91, 409–415. [Google Scholar] [CrossRef]
- Khitrov, M.Y.; Laxminarayan, S.; Thorsley, D.; Ramakrishnan, S.; Rajaraman, S.; Wesensten, N.J.; Reifman, J. PC-PVT: A platform for psychomotor vigilance task testing, analysis, and prediction. Behav. Res. Methods 2014, 46, 140–147. [Google Scholar] [CrossRef]
- Gander, P.H.; Signal, T.L.; van den Berg, M.J.; Mulrine, H.M.; Jay, S.M.; Mangie, C.J. In-flight sleep, pilot fatigue and Psychomotor Vigilance Task performance on ultra-long range versus long range flights. J. Sleep Res. 2013, 22, 697–706. [Google Scholar] [CrossRef]
- Svensson, T.; Saito, E.; Svensson, A.K.; Melander, O.; Orho-Melander, M.; Mimura, M.; Rahman, S.; Sawada, N.; Koh, W.P.; Shu, X.O.; et al. Association of sleep duration with all- and major-cause mortality among adults in Japan, China, Singapore, and Korea. JAMA Netw. Open 2021, 4, e2122837. [Google Scholar] [CrossRef] [PubMed]
- Darwent, D.J.; Dawson, D.; Roach, G. A model of shiftworker sleep/wake behaviour. Accid. Anal. Prev. 2012, 45 (Suppl. S), 6–10. [Google Scholar] [CrossRef] [PubMed]
- Dawson, D.; Reid, K. Fatigue, alcohol and performance impairment. Nature 1997, 388, 235. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, A.; Lamond, N.; Van Den Heuvel, C.J.; Dawson, D. Prediction of performance during sleep deprivation and alcohol intoxication using a quantitative model of work-related fatigue. Sleep Res. 2003, 5, 67–75. [Google Scholar]
- Cohen, J. Statistical power analysis and research results. Am. Educ. Res. J. 1973, 10, 225–229. [Google Scholar] [CrossRef]
- Bano-Otalora, B.; Martial, F.; Harding, C.; Bechtold, D.A.; Allen, A.E.; Brown, T.M.; Belle, M.D.C.; Lucas, R.J. Bright daytime light enhances circadian amplitude in a diurnal mammal. Proc. Natl. Acad. Sci. USA 2021, 118, e2100094118. [Google Scholar] [CrossRef]
- Meijer, J.H.; Schaap, J.; Watanabe, K.; Albus, H. Multiunit activity recordings in the suprachiasmatic nuclei: In vivo versus in vitro models. Brain Res. 1997, 753, 322–327. [Google Scholar] [CrossRef]
- Gander, P.H.; Rosekind, M.R.; Gregory, K.B. Flight crew fatigue VI: A synthesis. Aviat. Space Environ. Med. 1998, 69 (Suppl. S9), B49–B60. [Google Scholar]
- Mecham, J. Requirements Analysis and Architecture for an Operational Study of Fatigue in USAF Mobility Aircrew. Theses and Dissertations. 2021. Available online: https://scholar.afit.edu/etd/5099 (accessed on 15 December 2022).
- Belenky, G.; Wesensten, N.J.; Thorne, D.R.; Thomas, M.L.; Sing, H.C.; Redmond, D.P.; Russo, M.B.; Balkin, T.J. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: A sleep dose-response study. J. Sleep Res. 2003, 12, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Rupp, T.L.; Wesensten, N.J.; Bliese, P.D.; Balkin, T.J. Banking sleep: Realization of benefits during subsequent sleep restriction and recovery. Sleep 2009, 32, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Roach, G.D.; Petrilli, R.M.A.; Dawson, D.; Lamond, N. Impact of Layover Length on Sleep, Subjective Fatigue Levels, and Sustained Attention of Long-Haul Airline Pilots. Chraonobiol. Int. 2012, 29, 580–586. [Google Scholar] [CrossRef]
- Gander, P.H.; Graeber, R.C.; Foushee, H.C.; Lauber, J.K.; Connell, L.J. Crew Factors in Flight Operations II: Psychophysiological Responses to Short-Haul Air Transport Operations (NASA-TM-108856). 1994. Available online: https://ntrs.nasa.gov/citations/19950009235 (accessed on 20 December 2022).
- Lee, I.S.; Bardwell, W.A.; Ancoli-Israel, S.; Dimsdale, J.E. Number of lapses during the psychomotor vigilance task as an objective measure of fatigue. J. Clinical Sleep Med. 2010, 6, 163–168. [Google Scholar] [CrossRef]
- Gander, P.H.; Marshall, N.S.; Harris, R.; Reid, P. The Epworth Sleepiness Scale: Influence of age, ethnicity, and socioeconomic deprivation. Epworth Sleepiness scores of adults in New Zealand. Sleep 2005, 28, 249–253. [Google Scholar] [CrossRef]
- International Air Transport Association. Fatigue Risk Management Systems: Implementation Guide for Operators, 1st ed.; International Air Transport Association: Montréal, QC, Canada, 2011. [Google Scholar]
- Dawson, D.; Noy, Y.I.; Härmä, M.; Akerstedt, T.; Belenky, G. Modelling fatigue and the use of fatigue models in work settings. Accid. Anal. Prev. 2011, 43, 549–564. [Google Scholar] [CrossRef] [PubMed]
- Federal Aviation Administration. Fatigue Risk Management Systems for Aviation Safety Circular 120-103A; US Department of Transportation: Washington, DC, USA, 2013. [Google Scholar]
- European Union Aviation Safety Agency. European Union Aviation Safety Agency J.K. Effectiveness of Flight Time Limitation (FTL). 2019. Available online: https://www.easa.europa.eu/document-library/general-publications/effectiveness-flight-time-limitation-ftl-report (accessed on 20 December 2022).
- Wingelaar-Jagt, Y.Q.; Wingelaar, T.T.; Riedel, W.J.; Ramaekers, J.G. Fatigue in aviation: Safety risks, preventive strategies and pharmacological interventions. Front. Physiol. 2021, 12, 712628. [Google Scholar] [CrossRef]
- Morris, C.H.; Leung, Y.K. Pilot mental workload: How well do pilots really perform? Ergonomics 2006, 49, 1581–1596. [Google Scholar] [CrossRef]

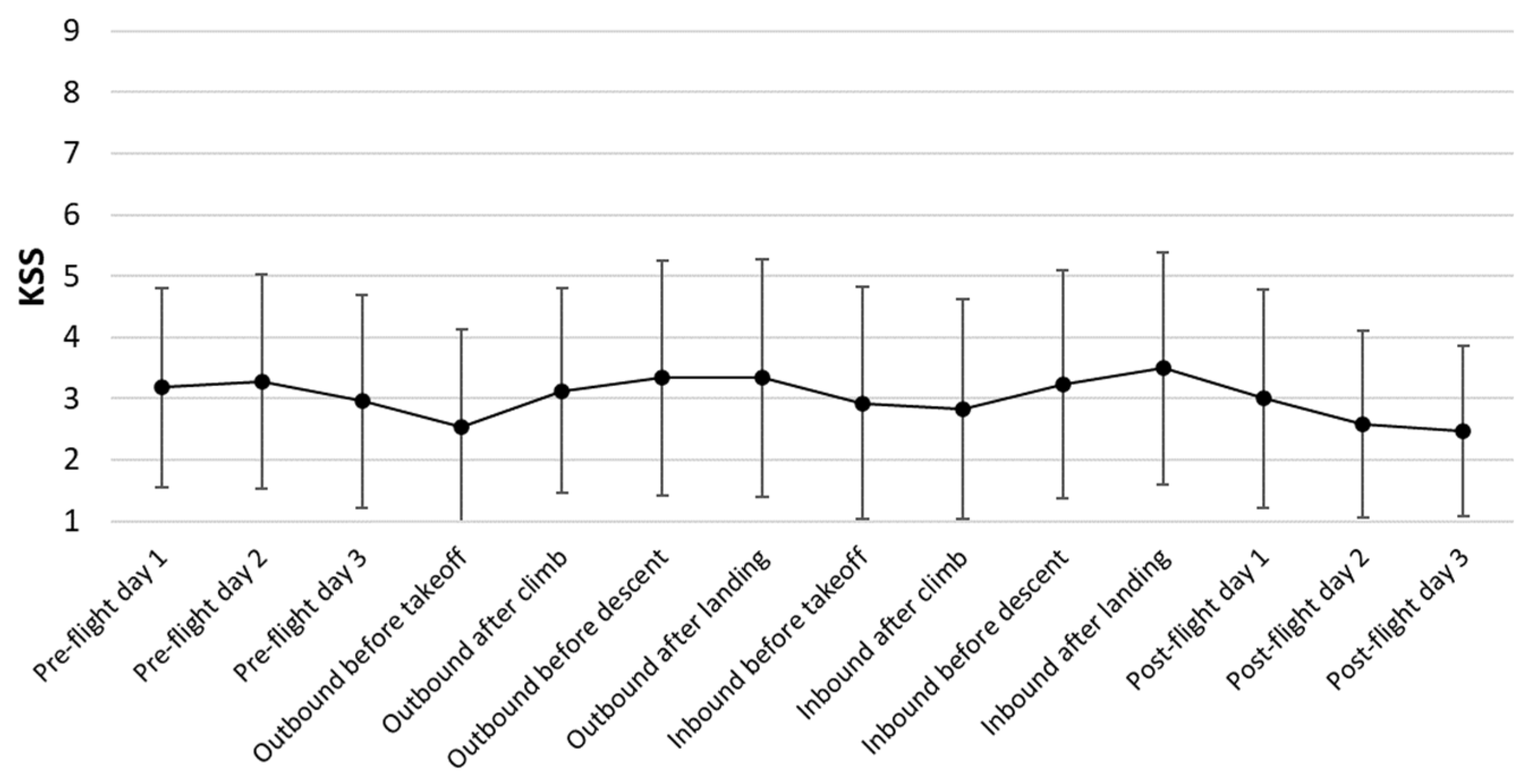

| KSS | Outbound | Inbound | ||||||
|---|---|---|---|---|---|---|---|---|
| Before Takeoff | After Climb | Before Descent | After Landing | Before Takeoff | After Climb | Before Descent | After Landing | |
| Mean ± SD | 2.55 ± 1.57 | 3.13 ± 1.67 | 3.34 ± 1.92 | 3.34 ± 1.93 | 2.93 ± 1.89 | 2.83 ± 1.80 | 3.24 ± 1.86 | 3.49 ± 1.89 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; He, J.; Cao, S.; Zheng, J.; Dou, Y.; Liu, C.; Liu, X. Assessing Flight Crew Fatigue under Extra Augmented Crew Schedule Using a Multimodality Approach. Aerospace 2023, 10, 933. https://doi.org/10.3390/aerospace10110933
Li Y, He J, Cao S, Zheng J, Dou Y, Liu C, Liu X. Assessing Flight Crew Fatigue under Extra Augmented Crew Schedule Using a Multimodality Approach. Aerospace. 2023; 10(11):933. https://doi.org/10.3390/aerospace10110933
Chicago/Turabian StyleLi, Yan, Jibo He, Shi Cao, Jiajie Zheng, Yazhou Dou, Chenxi Liu, and Xufeng Liu. 2023. "Assessing Flight Crew Fatigue under Extra Augmented Crew Schedule Using a Multimodality Approach" Aerospace 10, no. 11: 933. https://doi.org/10.3390/aerospace10110933
APA StyleLi, Y., He, J., Cao, S., Zheng, J., Dou, Y., Liu, C., & Liu, X. (2023). Assessing Flight Crew Fatigue under Extra Augmented Crew Schedule Using a Multimodality Approach. Aerospace, 10(11), 933. https://doi.org/10.3390/aerospace10110933






