Design Optimisation of Bi-Cruciate Retaining Total Knee Arthroplasty (TKA) Prosthesis via Taguchi Methods
Abstract
:1. Introduction
2. Materials and Methods
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Comitini, S.; Tigani, D.; Leonetti, D.; Commessatti, M.; Cuoghi, F.; Barca, P.; Martucci, A.; Bettuzzi, C.; Amendola, L. Evolution in Knee Replacement Implant. Single Cell Biol. 2015, 4, 109. [Google Scholar] [CrossRef] [Green Version]
- Osmani, F.A.; Thakkar, S.C.; Collins, K.; Schwarzkopf, R. The utility of bicruciate-retaining total knee arthroplasty. Arthroplast Today 2017, 3, 61–66. [Google Scholar] [CrossRef] [Green Version]
- Dall’Oca, C.; Ricci, M.; Vecchini, E.; Giannini, N.; Lamberti, D.; Tromponi, C.; Magnan, B. Evolution of TKA design. Acta Biomed. 2017, 88, 17–31. [Google Scholar] [CrossRef]
- Mahomed, N.N.; Barrett, J.; Katz, J.N.; Baron, J.A.; Wright, J.; Losina, E. Epidemiology of Total Knee Replacement in the United States Medicare Population. J. Bone Jt. Surg. 2005, 87, 1222. [Google Scholar] [CrossRef]
- Traina, F.; De Fine, M.; Affatato, S. 5—Anatomy of the knee and suitable prostheses. In Wear of Orthopaedic Implants and Artificial Joints; Affatato, S., Ed.; Woodhead Publishing Series in Biomaterials; Woodhead Publishing: Sawston, UK, 2013; pp. 115–132. ISBN 978-0-85709-128-4. [Google Scholar]
- Zhang, Q.; Chen, Z.; Zhang, Z.; Jin, Z.; Muratoglu, O.K.; Varadarajan, K.M. Leveraging subject-specific musculoskeletal modeling to assess effect of anterior cruciate ligament retaining total knee arthroplasty during walking gait. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2020, 234, 1445–1456. [Google Scholar] [CrossRef]
- Pritchett, J.W. Bicruciate-retaining Total Knee Replacement Provides Satisfactory Function and Implant Survivorship at 23 Years. Clin. Orthop. Relat. Res. 2015, 473, 2327–2333. [Google Scholar] [CrossRef] [Green Version]
- Evans, J.T.; Walker, R.W.; Evans, J.P.; Blom, A.W.; Sayers, A.; Whitehouse, M.R. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019, 393, 655–663. [Google Scholar] [CrossRef] [Green Version]
- Kassam, A.-A.; Dieppe, P.; Toms, A. An analysis of time and money spent on investigating painful total knee replacements. Orthop. Proc. 2012, 94, 234. [Google Scholar] [CrossRef]
- Kallala, R.F.; Vanhegan, I.S.; Ibrahim, M.S.; Sarmah, S.; Haddad, F.S. Financial analysis of revision knee surgery based on NHS tariffs and hospital costs. Bone Jt. J. 2015, 97, 197–201. [Google Scholar] [CrossRef] [Green Version]
- Jackson Irudhayam, S.; Antony Prabu, D.; Jayakumar, K.S.; Hariram, V.; Sankaralingam, T. Stress distribution in knee Implant: A FEA study. Mater. Today Proc. 2022, 62, 977–980. [Google Scholar] [CrossRef]
- Haijie, L.; Dasen, L.; Tao, J.; Yi, Y.; Xiaodong, T.; Wei, G. Implant Survival and Complication Profiles of Endoprostheses for Treating Tumor Around the Knee in Adults: A Systematic Review of the Literature Over the Past 30 Years. J. Arthroplast. 2018, 33, 1275–1287.e3. [Google Scholar] [CrossRef] [PubMed]
- Henderson, E.R.; Groundland, J.S.; Pala, E.; Dennis, J.A.; Wooten, R.; Cheong, D.; Windhager, R.; Kotz, R.I.; Mercuri, M.; Funovics, P.T.; et al. Failure mode classification for tumor endoprostheses: Retrospective review of five institutions and a literature review. J. Bone Jt. Surg. Am. 2011, 93, 418–429. [Google Scholar] [CrossRef]
- Flannery, M.; McGloughlin, T.; Jones, E.; Birkinshaw, C. Analysis of wear and friction of total knee replacements: Part I. Wear assessment on a three station wear simulator. Wear 2008, 265, 999–1008. [Google Scholar] [CrossRef]
- Archard, J.F. Contact and Rubbing of Flat Surfaces. J. Appl. Phys. 1953, 24, 981–988. [Google Scholar] [CrossRef]
- Kauzlarich, J.J.; Williams, J.A. Archard wear and component geometry. Proc. Inst. Mech. Eng. Part J J. Eng. Tribol. 2001, 215, 387–403. [Google Scholar] [CrossRef]
- Wimmer, M.A.; Laurent, M.P.; Haman, J.D.; Jacobs, J.J.; Galante, J.O. Surface Damage Versus Tibial Polyethylene Insert Conformity: A Retrieval Study. Clin. Orthop. Relat. Res. 2012, 470, 1814–1825. [Google Scholar] [CrossRef] [Green Version]
- Pascau, A.; Guardia, B.; Puertolas, J.A.; Gómez-Barrena, E. Knee model of hydrodynamic lubrication during the gait cycle and the influence of prosthetic joint conformity. J. Orthop. Sci. 2009, 14, 68–75. [Google Scholar] [CrossRef]
- Bartel, D.L.; Bicknell, V.L.; Wright, T.M. The effect of conformity, thickness, and material on stresses in ultra-high molecular weight components for total joint replacement. J. Bone Jt. Surg. Am. 1986, 68, 1041–1051. [Google Scholar] [CrossRef]
- Huang, Z.; Ouyang, G.; Xiao, L. Rotating-platform knee arthroplasty: A review and update. Orthop. Surg. 2011, 3, 224–228. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Bartel, D.L.; Rimnac, C.M. Postirradiation aging affects stress and strain in polyethylene components. Clin. Orthop. Relat. Res. 1998, 350, 209–220. [Google Scholar] [CrossRef]
- Sabarish, K.V.; Pratheeba, P. An experimental analysis on structural beam with Taguchi orthogonal array. Mater. Today Proc. 2020, 22, 874–878. [Google Scholar] [CrossRef]
- Tekade, R.K.; Chougule, M.B. Formulation Development and Evaluation of Hybrid Nanocarrier for Cancer Therapy: Taguchi Orthogonal Array Based Design. BioMed Res. Int. 2013, 2013, e712678. [Google Scholar] [CrossRef] [Green Version]
- Nagarjun, P.A.; Rao, R.S.; Rajesham, S.; Rao, L.V. Optimization of lactic acid production in SSF by Lactobacillus amylovorus NRRL B-4542 using Taguchi methodology. J. Microbiol. 2005, 43, 38–43. [Google Scholar]
- Varshosaz, J.; Eskandari, S.; Tabakhian, M. Production and optimization of valproic acid nanostructured lipid carriers by the Taguchi design. Pharm. Dev. Technol. 2010, 15, 89–96. [Google Scholar] [CrossRef]
- Dong, Y.; Zhang, Z.; Dong, W.; Hu, G.; Wang, B.; Mou, Z. An optimization method for implantation parameters of individualized TKA tibial prosthesis based on finite element analysis and orthogonal experimental design. BMC Musculoskelet. Disord. 2020, 21, 165. [Google Scholar] [CrossRef]
- Brockett, C.; Carbone, S.; Fisher, J.; Jennings, L. Influence of conformity on the wear of total knee replacement: An experimental study. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2017, 232, 127–134. [Google Scholar] [CrossRef] [Green Version]
- Koh, Y.-G.; Park, K.-M.; Kang, K.-T. The biomechanical effect of tibiofemoral conformity design for patient-specific cruciate retainging total knee arthroplasty using computational simulation. J. Exp. Orthop. 2019, 6, 23. [Google Scholar] [CrossRef]
- Khasian, M.; Meccia, B.A.; LaCour, M.T.; Komistek, R.D. Effects of the Medial Plateau Bearing Insert Conformity on Mid-Flexion Paradoxical Motion in a Posterior-Stabilized Total Knee Arthroplasty Design. J. Arthroplast. 2021, 36, 2386–2392. [Google Scholar] [CrossRef]
- Indelli, P.F.; Risitano, S.; Hall, K.E.; Leonardi, E.; Migliore, E. Effect of polyethylene conformity on total knee arthroplasty early clinical outcomes. Knee Surg. Sport. Traumatol. Arthrosc. 2019, 27, 1028–1034. [Google Scholar] [CrossRef]
- Mou, Z.; Dong, W.; Zhang, Z.; Wang, A.; Hu, G.; Wang, B.; Dong, Y. Optimization of parameters for femoral component implantation during TKA using finite element analysis and orthogonal array testing. J. Orthop. Surg. Res. 2018, 13, 179. [Google Scholar] [CrossRef]
- Tang, Q.; Twumasi, J.O.; Hu, J.; Wang, X.; Yu, T. Finite element simulation of photoacoustic fiber optic sensors for surface corrosion detection on a steel rod. In Proceedings of the Nondestructive Characterization and Monitoring of Advanced Materials, Aerospace, Civil Infrastructure, and Transportation XII, Denver, CO, USA, 5–8 March 2018; SPIE: Paris, France, 2018; Volume 10599, pp. 341–353. [Google Scholar]
- Masoudi Nejad, R.; Noroozian Rizi, P.; Zoei, M.S.; Aliakbari, K.; Ghasemi, H. Failure Analysis of a Working Roll Under the Influence of the Stress Field Due to Hot Rolling Process. J. Fail. Anal. Preven. 2021, 21, 870–879. [Google Scholar] [CrossRef]
- Bonner, B.; Law, J.I.; Dacus, E.; Hofmann, E. The Modern Universal Total Knee Arthroplasty: Maximized Value, Streamlined Efficiency. Available online: https://econpapers.repec.org/bookchap/itopchaps/226804.htm (accessed on 14 December 2022).
- Kohli, A.; Mathad, M.; V Hosamani, S.; Adagimath, M.K.; Kotturshettar, B.B. Finite element analysis of knee joint implant for varying bio material using ANSYS. Mater. Today Proc. 2022, 59, 941–950. [Google Scholar] [CrossRef]
- Bhandarkar, S.; Dhatrak, P. Optimization of a knee implant with different biomaterials using finite element analysis. Mater. Today Proc. 2022, 59, 459–467. [Google Scholar] [CrossRef]
- Kacker, R.N.; Lagergren, E.S.; Filliben, J.J. Taguchi’s Orthogonal Arrays Are Classical Designs of Experiments. J. Res. Natl. Inst. Stand. Technol. 1991, 96, 577–591. [Google Scholar] [CrossRef]
- Singerman, R.; Dean, J.C.; Pagan, H.D.; Goldberg, V.M. Decreased posterior tibial slope increases strain in the posterior cruciate ligament following total knee arthroplasty. J. Arthroplast. 1996, 11, 99–103. [Google Scholar] [CrossRef]
- Guess, T.M.; Razu, S. Loading of the medial meniscus in the ACL deficient knee: A multibody computational study. Med. Eng. Phys. 2017, 41, 26–34. [Google Scholar] [CrossRef] [Green Version]
- Mohd Anuar, M.A.; Todo, M.; Nagamine, R.; Hirokawa, S. Dynamic Finite Element Analysis of Mobile Bearing Type Knee Prosthesis under Deep Flexional Motion. Sci. World J. 2014, 2014, 586921. [Google Scholar] [CrossRef] [Green Version]
- Anuar, M.A.M.; Todo, M.; Nagamine, R. Computational Model for Mechanics of Total Knee Replacement: Effect of Tibial Rotation during Deep Flexion in Relation to Post-Cam Design. Int. J. Biosci. Biochem. Bioinform. 2014. [Google Scholar] [CrossRef] [Green Version]
- Innocenti, B.; Bellemans, J.; Catani, F. Deviations from Optimal Alignment in TKA: Is There a Biomechanical Difference Between Femoral or Tibial Component Alignment? J. Arthroplast. 2016, 31, 295–301. [Google Scholar] [CrossRef]
- Dayyoub, T.; Maksimkin, A.V.; Kaloshkin, S.; Kolesnikov, E.; Chukov, D.; Dyachkova, T.P.; Gutnik, I. The Structure and Mechanical Properties of the UHMWPE Films Modified by the Mixture of Graphene Nanoplates with Polyaniline. Polymers 2018, 11, 23. [Google Scholar] [CrossRef] [Green Version]
- Baron, S.; Desmond, D.; Ahearne, E. The fundamental mechanisms of wear of cemented carbide in continuous cutting of medical grade cobalt chromium alloy (ASTM F75). Wear 2019, 424–425, 89–96. [Google Scholar] [CrossRef]
- Wang, A.; Yau, S.-S.; Essner, A.; Herrera, L.; Manley, M.; Dumbleton, J. A Highly Crosslinked UHMWPE for CR and PS Total Knee Arthroplasties. J. Arthroplast. 2008, 23, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Fleming, T.J.; Kavanagh, A.; Duggan, G. The effect of melt temperature on the mechanical properties of cast ASTM F75 CoCrMo alloy as explained by nitrogen and oxygen content. J. Mater. Res. Technol. 2020, 9, 9479–9486. [Google Scholar] [CrossRef]
- Takian, W.; Rooppakhun, S.; Ariyarit, A.; Sucharitpwatskul, S. Optimal Conformity Design of Tibial Insert Component Based on ISO Standard Wear Test Using Finite Element Analysis and Surrogate Model. Symmetry 2021, 13, 2377. [Google Scholar] [CrossRef]
- D’Lima, D.D.; Fregly, B.J.; Patil, S.; Steklov, N.; Colwell, C.W. Knee joint forces: Prediction, measurement, and significance. Proc. Inst. Mech. Eng. H 2012, 226, 95–102. [Google Scholar] [CrossRef] [Green Version]
- Kang, K.-T.; Son, J.; Kwon, S.K.; Kwon, O.-R.; Park, J.-H.; Koh, Y.-G. Finite element analysis for the biomechanical effect of tibial insert materials in total knee arthroplasty. Compos. Struct. 2018, 201, 141–150. [Google Scholar] [CrossRef]
- Kwon, O.-R.; Kang, K.-T.; Son, J.; Kwon, S.-K.; Jo, S.-B.; Suh, D.-S.; Choi, Y.-J.; Kim, H.-J.; Koh, Y.-G. Biomechanical comparison of fixed- and mobile-bearing for unicomparmental knee arthroplasty using finite element analysis. J. Orthop. Res. 2014, 32, 338–345. [Google Scholar] [CrossRef]
- Koh, Y.-G.; Park, K.-M.; Lee, H.-Y.; Kang, K.-T. Influence of tibiofemoral congruency design on the wear of patient-specific unicompartmental knee arthroplasty using finite element analysis. Bone Jt. Res. 2019, 8, 156–164. [Google Scholar] [CrossRef]
- Kang, K.-T.; Son, J.; Kim, H.-J.; Baek, C.; Kwon, O.-R.; Koh, Y.-G. Wear predictions for UHMWPE material with various surface properties used on the femoral component in total knee arthroplasty: A computational simulation study. J. Mater. Sci. Mater. Med. 2017, 28, 105. [Google Scholar] [CrossRef]
- Fang, D.M.; Ritter, M.A.; Davis, K.E. Coronal alignment in total knee arthroplasty: Just how important is it? J. Arthroplast. 2009, 24, 39–43. [Google Scholar] [CrossRef]
- Shen, Y.; Li, X.; Fu, X.; Wang, W. A 3D finite element model to investigate prosthetic interface stresses of different posterior tibial slope. Knee Surg. Sport. Traumatol. Arthrosc. 2015, 23, 3330–3336. [Google Scholar] [CrossRef] [PubMed]
- Dhaka, P.; Prakash, R.V. Effect of Contact Geometry on the Contact Stresses in a Flat with Round Edge Contact. Frat. Ed Integrità Strutt. 2019, 13, 630–638. [Google Scholar] [CrossRef]
- Mall, S.; Naboulsi, S.; Namjoshi, S.A. Contact geometry effects on fretting fatigue crack initiation behaviour of Ti–6Al–4V. Tribol. Mater. Surf. Interfaces 2008, 2, 25–32. [Google Scholar] [CrossRef]
- Juoksukangas, J.; Lehtovaara, A.; Mäntylä, A. The effect of contact edge geometry on fretting fatigue behavior in complete contacts. Wear 2013, 308, 206–212. [Google Scholar] [CrossRef]


| Experimental Factors | Level 1 | Level 2 | Level 3 |
|---|---|---|---|
| A: Curvature ratio on sagittal plane | 1.5 | 1.2 | 1.0 |
| B: Curvature ratio on coronal plane | 1.5 | 1.2 | 1.0 |
| C: Tibial slope | 0° | 5° | 10° |
| Material | Ultimate Tensile Strength (Megapascals) | Young’s Modulus (Megapascals) | Yield Strength (Megapascals) | Poisson’s Ratio | Elongation (Percent) |
|---|---|---|---|---|---|
| Ultra-high molecular weight polyethylene (UHMWPE) | 27 | 800 | 23 | 0.4 | 7.0 |
| ASTM F75 cobalt chromium molybdenum (Co-Cr-Mo) | 920 | 210,000 | 540 | 0.29 | 16.5 |
| Component | Type of Mesh | Element Size (Millimeters) | Number of Elements |
|---|---|---|---|
| Femoral | Tetahedral | 1.2 | 182,186 |
| Right tibial insert | Tetahedral | 1.2 | 23,838 |
| Left tibial insert | Tetahedral | 1.2 | 23,703 |
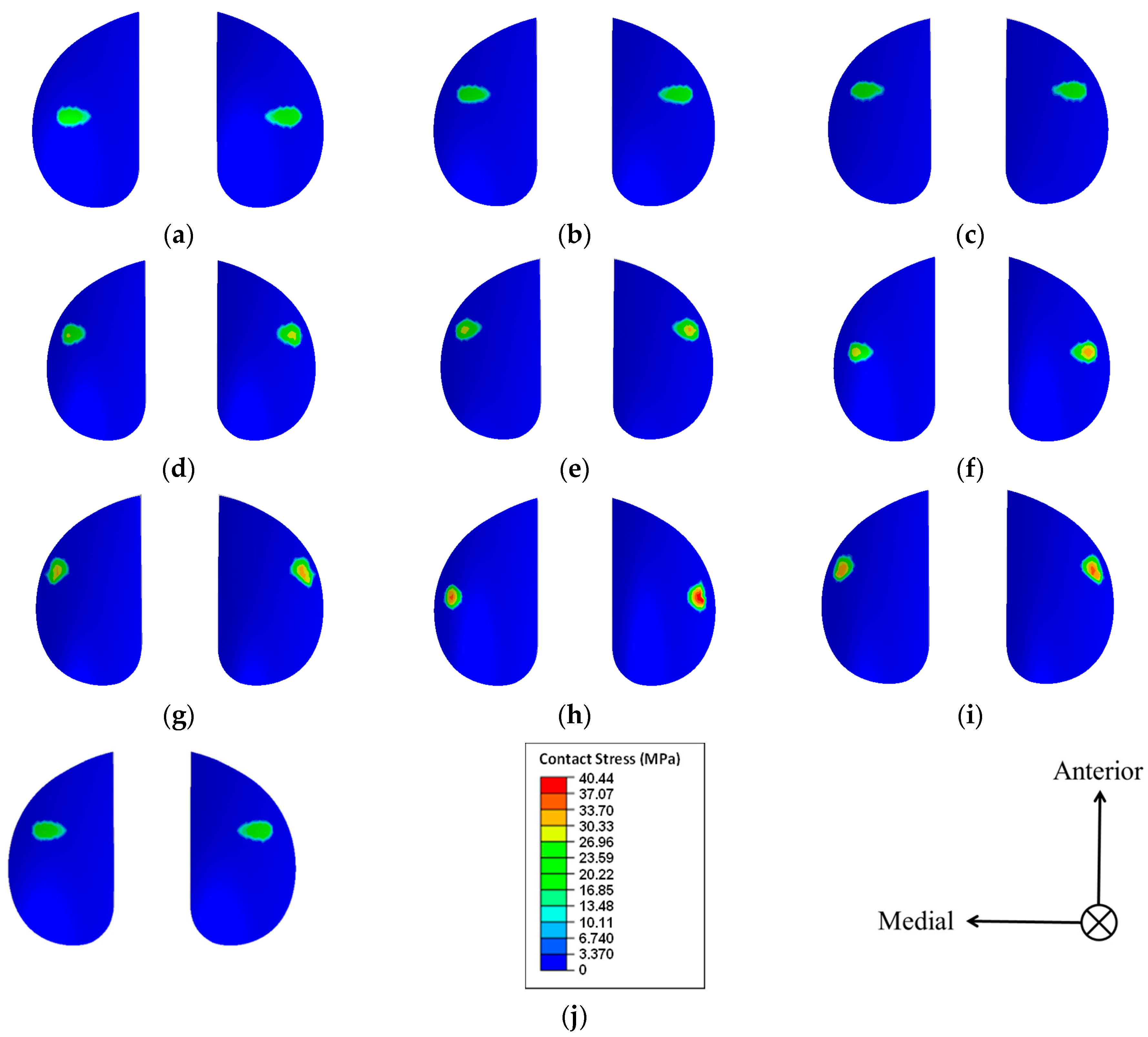
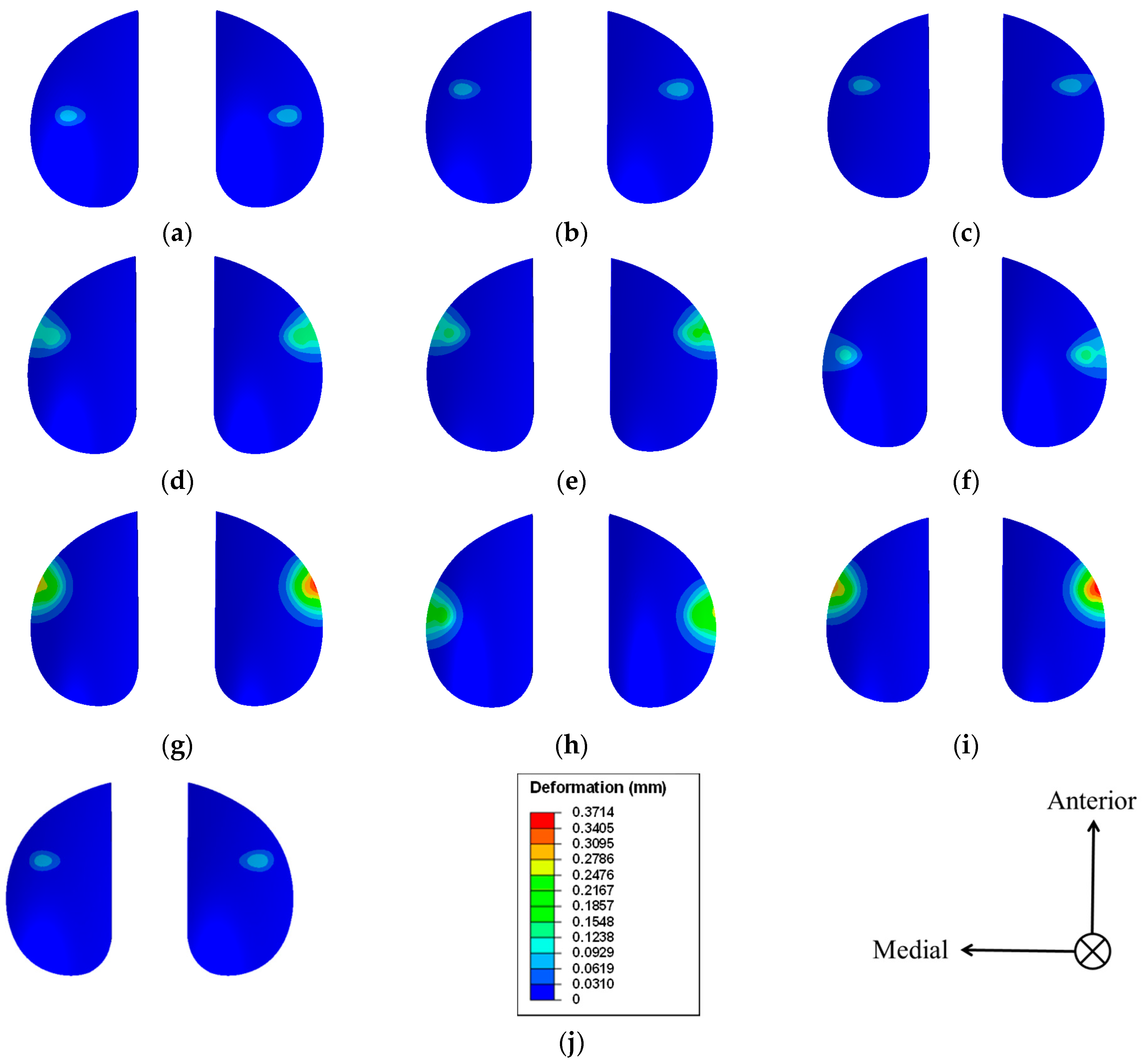
| Model | Experimental Level Combination | Curvature Ratio on Saggital Plane | Curvature Ratio on Coronal Plane | Tibial Slope (Degrees) | Peak Value of Contact Stress (Megapascals) | Deformation (Millimeters) |
|---|---|---|---|---|---|---|
| 1 | A1B1C1 | 1.5 | 1.5 | 0 | 24.89 | 0.0822 |
| 2 | A1B2C2 | 1.5 | 1.2 | 5 | 25.69 | 0.0851 |
| 3 | A1B3C3 | 1.5 | 1.0 | 10 | 26.78 | 0.0885 |
| 4 | A2B1C2 | 1.2 | 1.5 | 5 | 29.39 | 0.1533 |
| 5 | A2B2C3 | 1.2 | 1.2 | 10 | 32.53 | 0.1710 |
| 6 | A2B3C1 | 1.2 | 1.0 | 0 | 33.49 | 0.1371 |
| 7 | A3B1C3 | 1.0 | 1.5 | 10 | 33.75 | 0.3506 |
| 8 | A3B2C1 | 1.0 | 1.2 | 0 | 40.44 | 0.2595 |
| 9 | A3B3C2 | 1.0 | 1.0 | 5 | 36.05 | 0.3714 |
| Model | Experimental Factor j (j = 1,2,3) | Peak Value of Contact Stress (Megapascals) | ||
|---|---|---|---|---|
| A | B | C | ||
| 1 | 1 | 1 | 1 | 24.89 |
| 2 | 1 | 2 | 2 | 25.69 |
| 3 | 1 | 3 | 3 | 26.78 |
| 4 | 2 | 1 | 2 | 29.39 |
| 5 | 2 | 2 | 3 | 32.53 |
| 6 | 2 | 3 | 1 | 33.49 |
| 7 | 3 | 1 | 3 | 33.75 |
| 8 | 3 | 2 | 1 | 40.44 |
| 9 | 3 | 3 | 2 | 36.05 |
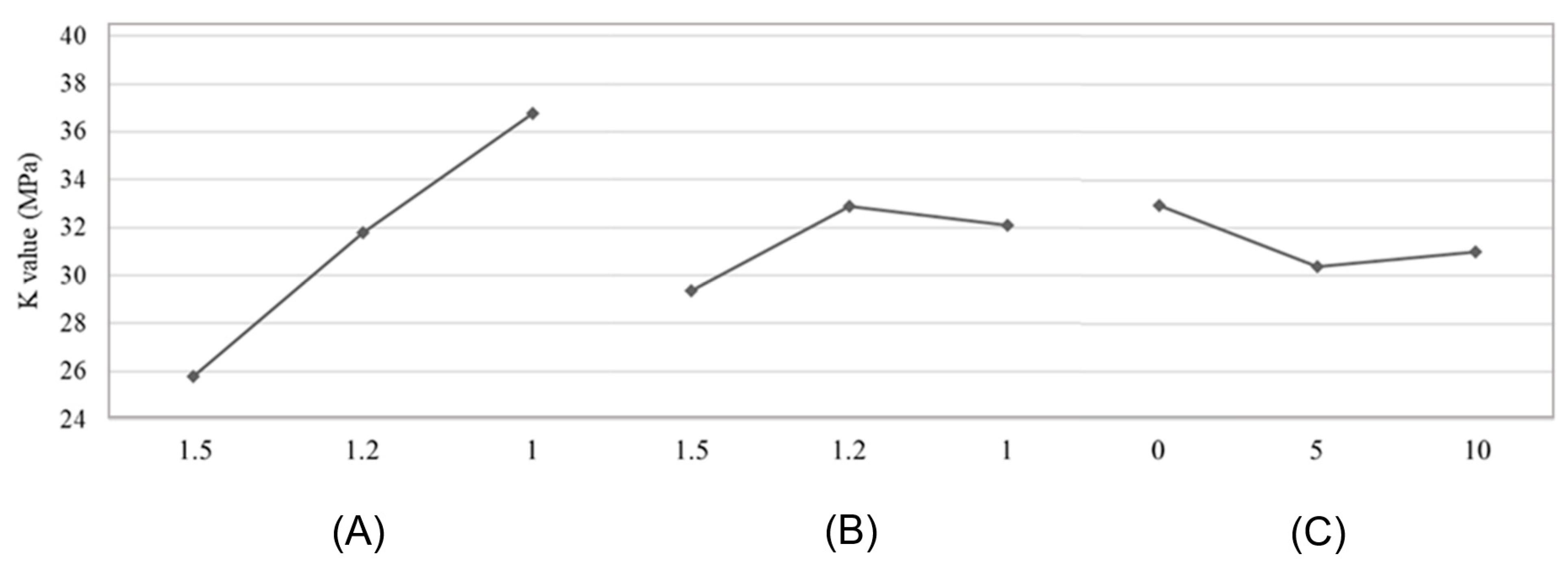
| Kj1 | 25.79 | 29.34 | 32.94 | |
| Kj2 | 31.80 | 32.89 | 30.38 | |
| Kj3 | 36.75 | 32.11 | 31.02 | |
| Range Rj | 10.96 | 3.54 | 2.56 | |
| Ranking | A > B > C | |||
| Optimal level | A1 | B1 | C2 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohd Mukhtar, N.Q.; Shuib, S.; Anuar, M.A.; Mohd Miswan, M.F.; Mohd Anuar, M.A. Design Optimisation of Bi-Cruciate Retaining Total Knee Arthroplasty (TKA) Prosthesis via Taguchi Methods. Mathematics 2023, 11, 312. https://doi.org/10.3390/math11020312
Mohd Mukhtar NQ, Shuib S, Anuar MA, Mohd Miswan MF, Mohd Anuar MA. Design Optimisation of Bi-Cruciate Retaining Total Knee Arthroplasty (TKA) Prosthesis via Taguchi Methods. Mathematics. 2023; 11(2):312. https://doi.org/10.3390/math11020312
Chicago/Turabian StyleMohd Mukhtar, Natrisya Qistina, Solehuddin Shuib, Muhamad Azhan Anuar, Mohd Fairudz Mohd Miswan, and Mohd Afzan Mohd Anuar. 2023. "Design Optimisation of Bi-Cruciate Retaining Total Knee Arthroplasty (TKA) Prosthesis via Taguchi Methods" Mathematics 11, no. 2: 312. https://doi.org/10.3390/math11020312
APA StyleMohd Mukhtar, N. Q., Shuib, S., Anuar, M. A., Mohd Miswan, M. F., & Mohd Anuar, M. A. (2023). Design Optimisation of Bi-Cruciate Retaining Total Knee Arthroplasty (TKA) Prosthesis via Taguchi Methods. Mathematics, 11(2), 312. https://doi.org/10.3390/math11020312






