Evolutionary Game Analysis of Healthcare Information Construction and Sharing Decisions Considering Synergy Benefits
Abstract
1. Introduction
- (1)
- What decisions will general hospitals and medical institutions make regarding information construction?
- (2)
- What are the main factors influencing the decisions of general hospitals and primary healthcare institutions?
- (3)
- How will these influencing factors affect the evolutionary paths of general hospitals and primary healthcare institutions?
2. Literature Review
2.1. Coordination between Different Healthcare Institutions
2.2. Service Coordination for Innovation and Information Synergy
3. Evolutionary Game Model
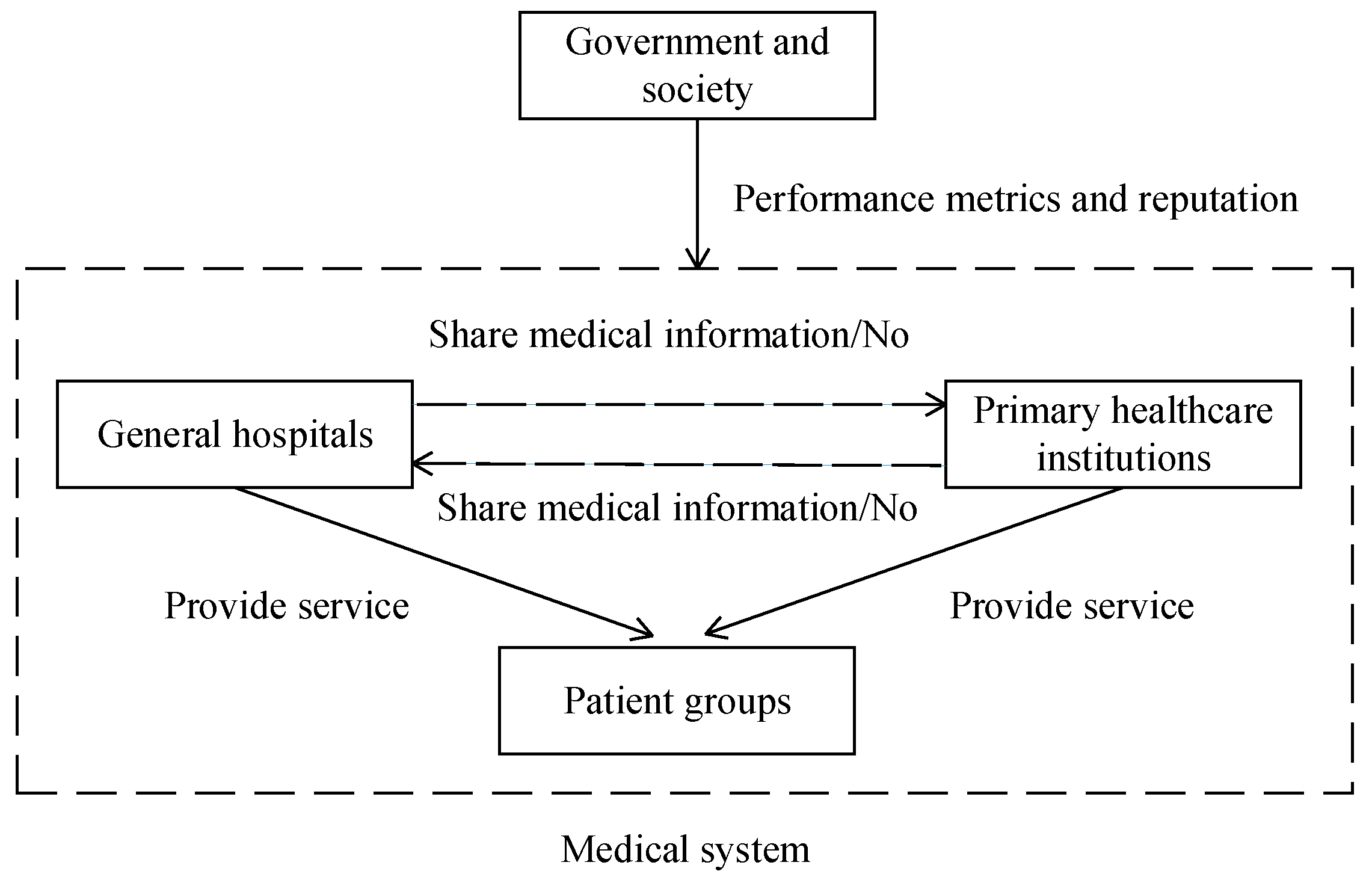
3.1. Model Description and Assumptions
3.2. Model Analysis
- (1)
- When , , and at least one of or holds (Case 1), the healthcare system will eventually evolve to .
- (2)
- When , , and at least one of or holds (Case 2), the healthcare system will eventually evolve to .
- (3)
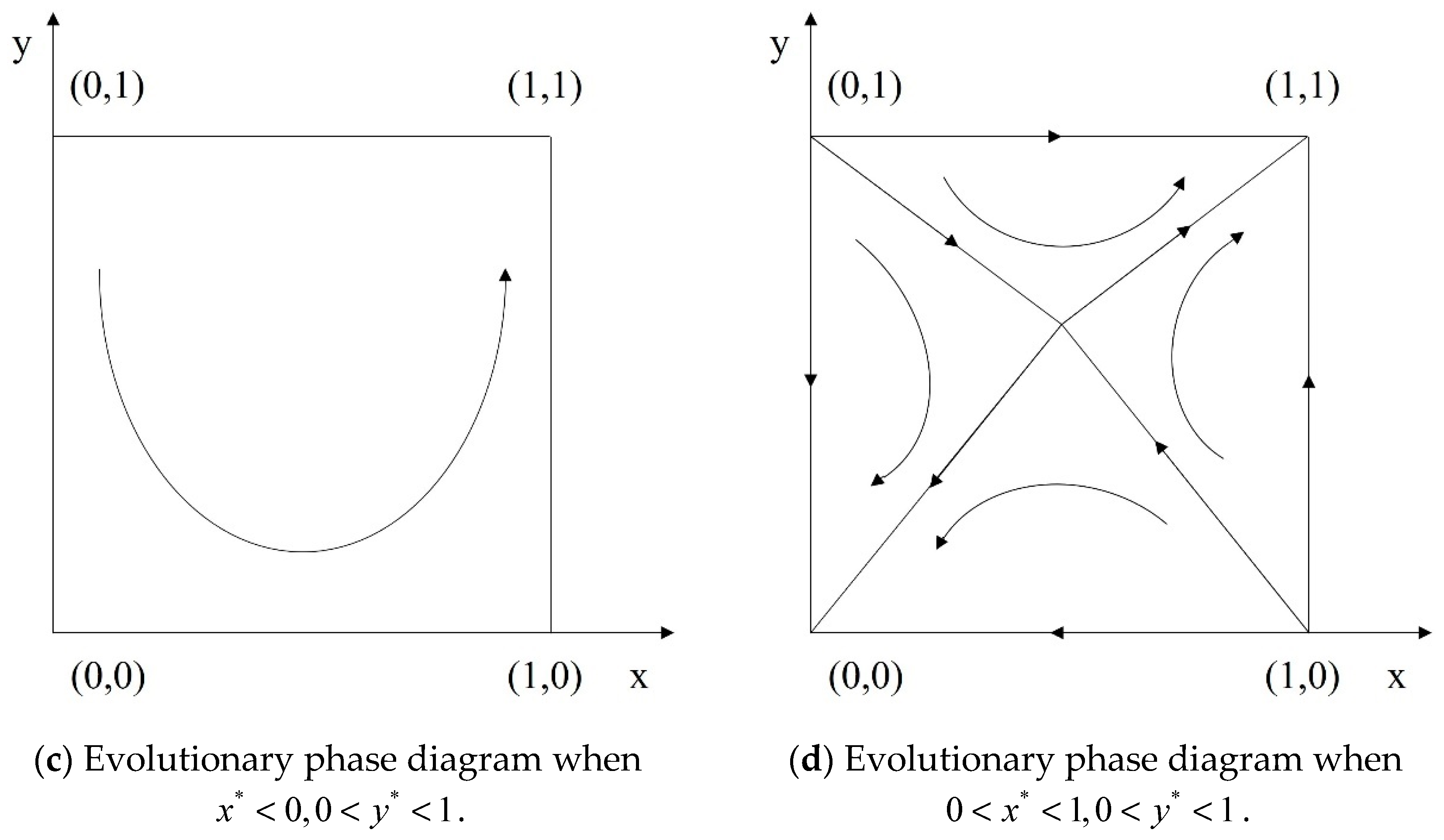
- When , , , and holds (Case 3), the healthcare system will eventually evolve to or .
- (4)
- When and holds or and holds (Case 4), the healthcare system will eventually evolve to or .
4. Discussion
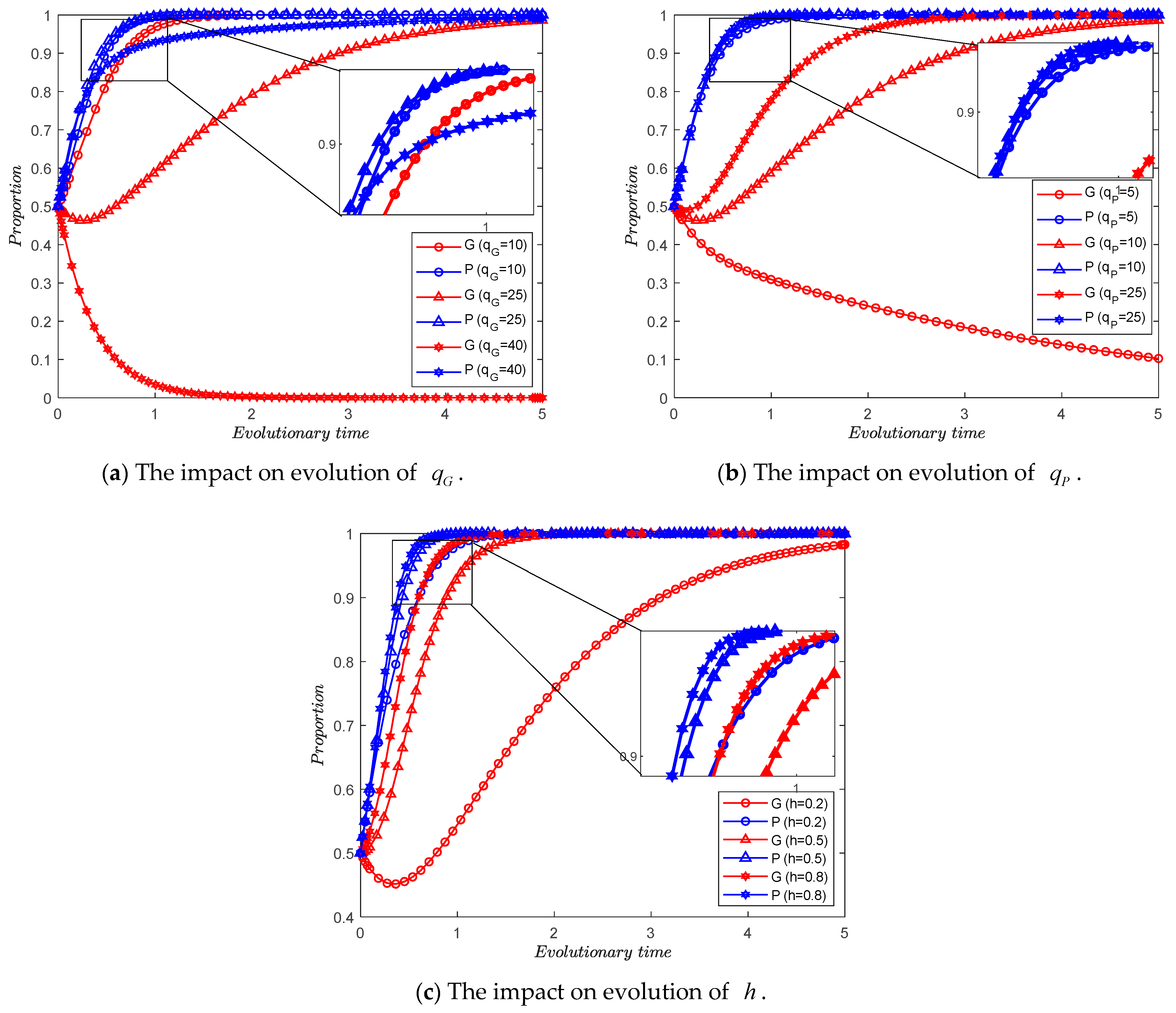
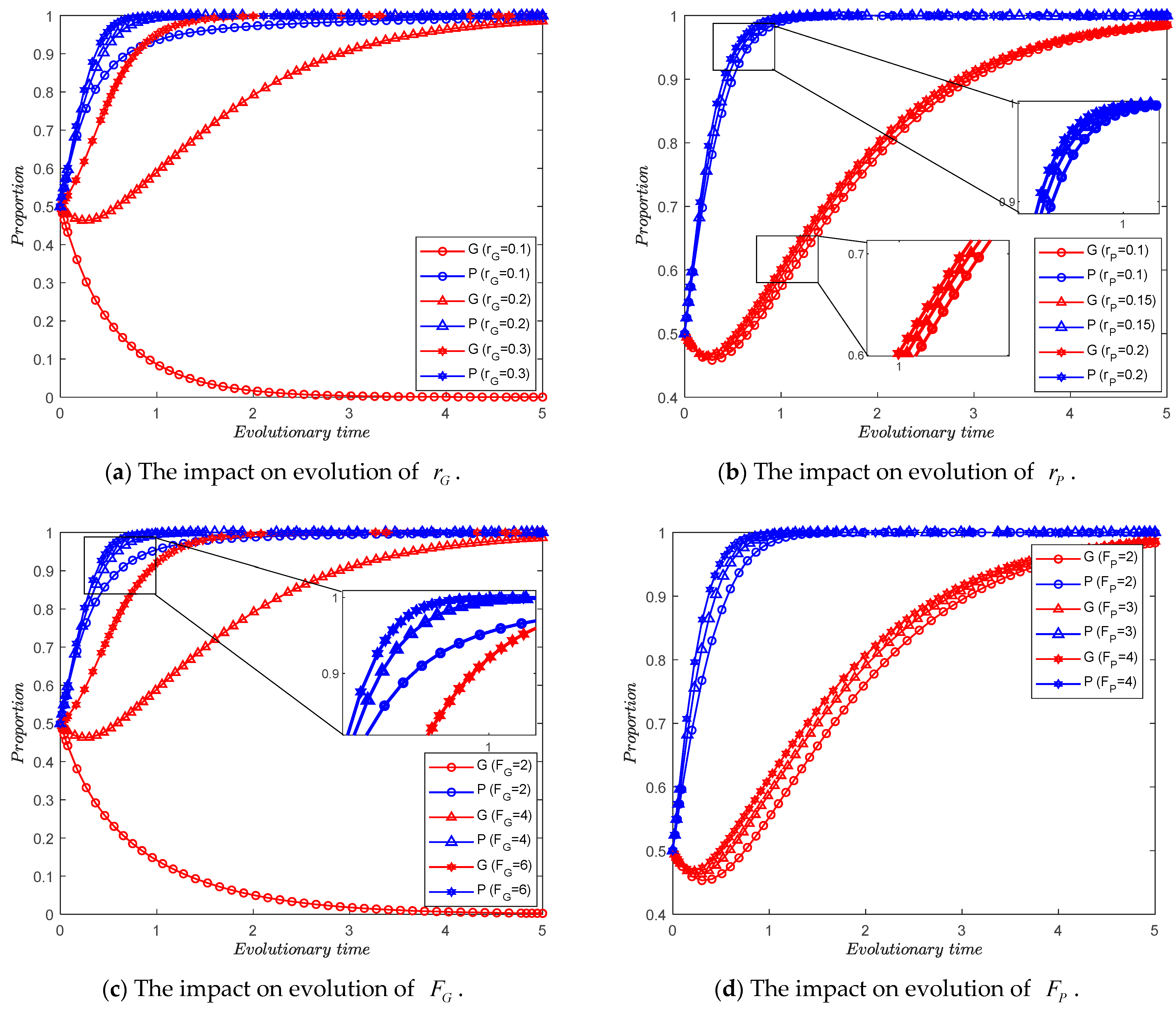
4.1. The Impact of the Volume of Information and the Degree of Recognition
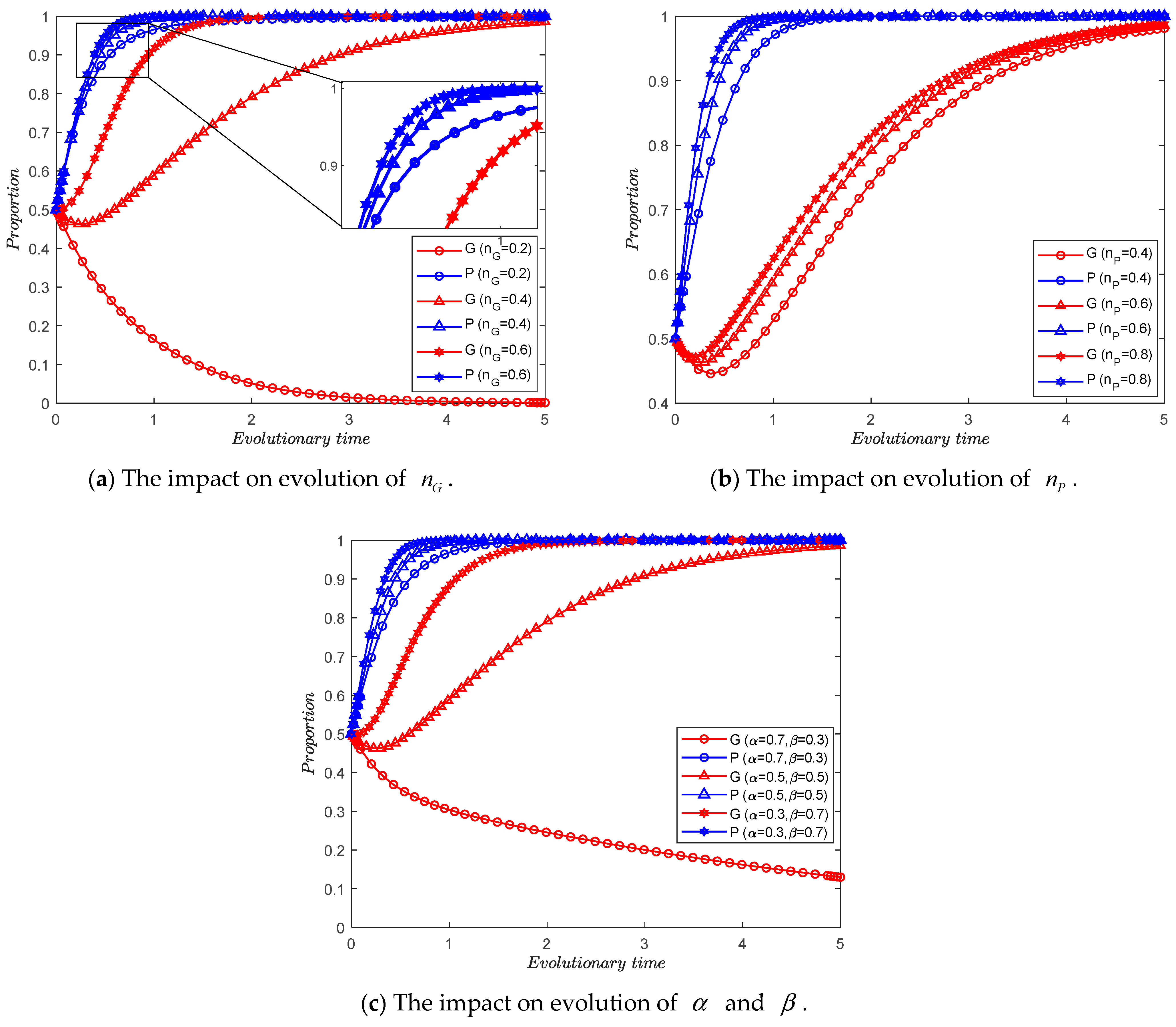
4.2. The Impact of the Benefits of Information Synergy
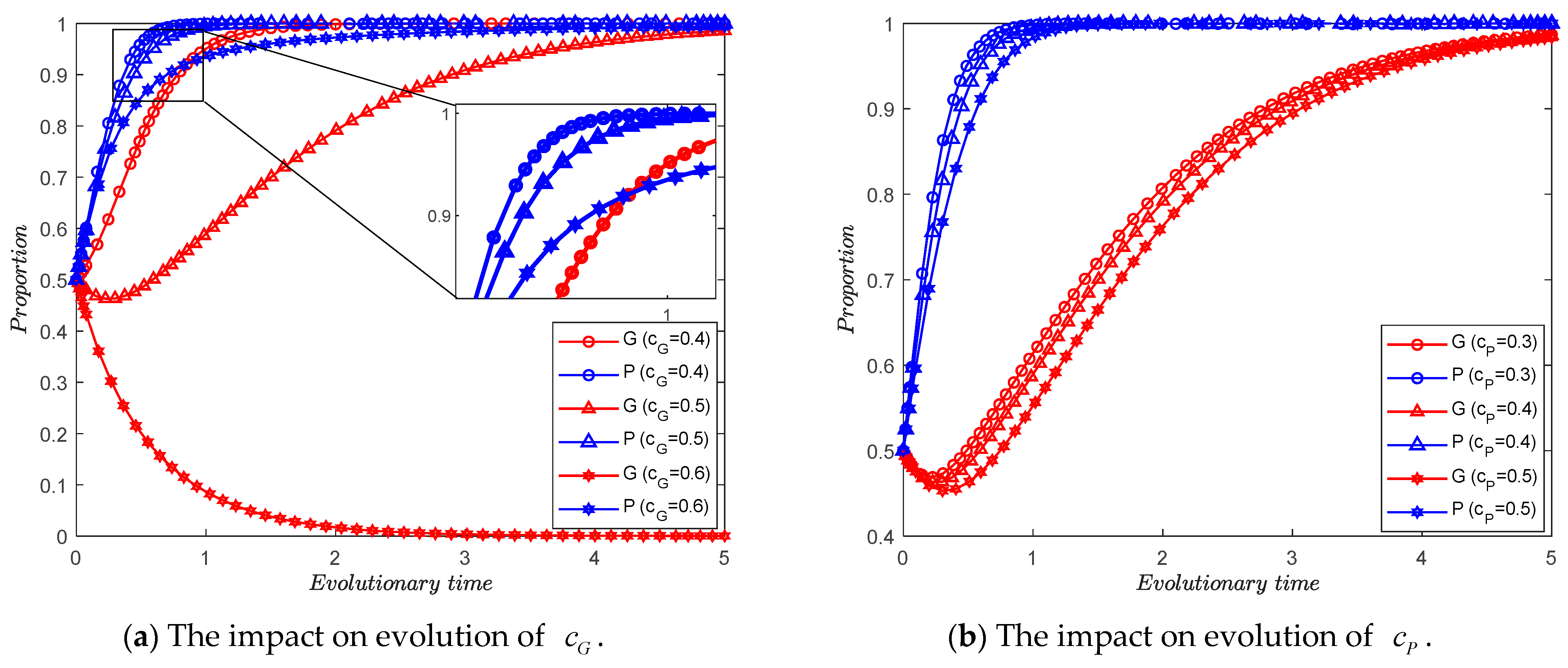
4.3. The Impact of the Cost of Information Construction
4.4. The Impact of the Societal and Government Incentives
5. Discussion and Managerial Implications
5.1. Benefits of Medical Information Synergy
5.2. Incentives for Information Synergy Behavior
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Núñez-Merino, M.; Maqueira-Marín, J.M.; Moyano-Fuentes, J.; Castaño-Moraga, C.A. Product development process for a new healthcare service in the Industry 4.0 context: An action research approach. Prod. Plan. Control 2024, 1–20. [Google Scholar] [CrossRef]
- Bardhan, I.R.; Thouin, M.F. Health information technology and its impact on the quality and cost of healthcare delivery. Decis. Support Syst. 2013, 55, 438–449. [Google Scholar] [CrossRef]
- Niu, B.; Xu, H.; Dai, Z. Check Only Once? Health Information Exchange between Competing Private Hospitals. Omega 2022, 107, 102556. [Google Scholar] [CrossRef]
- Li, Z.-P.; Wang, J.-J.; Chang, A.-C.; Shi, J. Capacity reallocation via sinking high-quality resource in a hierarchical healthcare system. Ann. Oper. Res. 2021, 300, 97–135. [Google Scholar] [CrossRef]
- Adida, E.; Bravo, F. Contracts for Healthcare Referral Services: Coordination via Outcome-Based Penalty Contracts. Manag. Sci. 2019, 65, 1322–1341. [Google Scholar] [CrossRef]
- Dong, C.; Liu, J.; Mi, J. Information-Driven Integrated Healthcare: An Analysis of the Cooperation Strategy of County Medical Community Based on Multi-Subject Simulation. Healthcare 2023, 11, 2019. [Google Scholar] [CrossRef]
- Wang, J.-J.; Li, Z.-P.; Shi, J.; Chang, A.-C. Hospital referral and capacity strategies in the two-tier healthcare systems. Omega 2020, 100, 102229. [Google Scholar] [CrossRef]
- Adida, E.; Mamani, H.; Nassiri, S. Bundled Payment vs. Fee-for-Service: Impact of Payment Scheme on Performance. Manag. Sci. 2017, 63, 1606–1624. [Google Scholar] [CrossRef]
- Wang, Z.; Zhou, W.; Zheng, Z. Encouraging preventive services in primary care through payment schemes. Comput. Ind. Eng. 2022, 171, 108485. [Google Scholar] [CrossRef]
- Ghamat, S.; Zaric, G.S.; Pun, H. Care-coordination: Gain-sharing agreements in bundled payment models. Prod. Oper. Manag. 2021, 30, 1457–1474. [Google Scholar] [CrossRef]
- Lan, Y.; Chandrasekaran, A.; Goradia, D.; Walker, D. Collaboration Structures in Integrated Healthcare Delivery Systems: An Exploratory Study of Accountable Care Organizations. Manuf. Serv. Oper. Manag. 2022, 24, 1796–1820. [Google Scholar] [CrossRef]
- Bravo, F.; Levi, R.; Perakis, G.; Romero, G. Care coordination for healthcare referrals under a shared-savings program. Prod. Oper. Manag. 2023, 32, 189–206. [Google Scholar] [CrossRef]
- Teymourifar, A.; Kaya, O.; Ozturk, G. Contracting models for pricing and capacity decisions in healthcare systems. Omega 2021, 100, 102232. [Google Scholar] [CrossRef]
- Cao, X.; Rajagopalan, S.; Tong, C. Impact of vertical integration in a referral-based healthcare system. Omega 2024, 123, 102998. [Google Scholar] [CrossRef]
- Tiwari, M.; Bryde, D.J.; Stavropoulou, F.; Dubey, R.; Kumari, S.; Foropon, C. Modelling supply chain Visibility, digital Technologies, environmental dynamism and healthcare supply chain Resilience: An organization information processing theory perspective. Transp. Res. Part E Logist. Transp. Rev. 2024, 188, 103613. [Google Scholar] [CrossRef]
- Liu, W.; Chai, R.; Cao, X.; Fang, X.; Yang, Y. Promoting product idea contribution of heterogeneous users for product improvement in online innovation communities. Int. J. Prod. Res. 2022, 61, 3599–3620. [Google Scholar] [CrossRef]
- Andritsos, D.A.; Tang, C.S. Incentive Programs for Reducing Readmissions when Patient Care is Co-Produced. Prod. Oper. Manag. 2018, 27, 999–1020. [Google Scholar] [CrossRef]
- Yan, L.; Yan, X.; Tan, Y.; Sun, S.X. Shared minds: How patients use collaborative information sharing via social media platforms. Prod. Oper. Manag. 2019, 28, 9–26. [Google Scholar] [CrossRef]
- Zheng, Y.; Zhou, B.; Bai, C.; Cai, Q. Differential game model of the cross-organizational cooperative r&d of general purpose technologies under two-way collaboration. Chin. J. Manag. Sci. 2023, 31, 255–265. [Google Scholar]
- Tang, Q.; Wang, C.; Feng, T. Research on the Group Innovation Information-Sharing Strategy of the Industry–University–Research Innovation Alliance Based on an Evolutionary Game. Mathematics 2023, 11, 4161. [Google Scholar] [CrossRef]
- Liu, Z.; Zhang, D.J.; Zhang, F. Information Sharing on Retail Platforms. Manuf. Serv. Oper. Manag. 2021, 23, 606–619. [Google Scholar] [CrossRef]
- Tan, Y.; Huang, X.; Li, W. Does blockchain-based traceability system guarantee information authenticity? An evolutionary game approach. Int. J. Prod. Econ. 2023, 264, 108974. [Google Scholar] [CrossRef]
- Li, K.; Liang, C. Exploring the promotion of blockchain adoption in the healthcare industry through government subsidies. Kybernetes, 2023; ahead-of-print. [Google Scholar] [CrossRef]
- Sun, M.; Chai, Q.; Ng, C.T. Managing the quality-speed tradeoff in blockchain-supported healthcare diagnostic services. Omega Int. J. Manag. Sci. 2023, 120, 102911. [Google Scholar] [CrossRef]
- Wang, G.; Li, J.; Hopp, W.J.; Fazzalari, F.L.; Bolling, S.F. Using Patient-Specific Quality Information to Unlock Hidden Healthcare Capabilities. Manuf. Serv. Oper. Manag. 2019, 21, 582–601. [Google Scholar] [CrossRef]
- Atasoy, H.; Chen, P.-Y.; Ganju, K. The Spillover Effects of Health IT Investments on Regional Healthcare Costs. Manag. Sci. 2018, 64, 2515–2534. [Google Scholar] [CrossRef]
- Gao, Y.; Zhu, Z.; Yang, J. An Evolutionary Game Analysis of Stakeholders’ Decision-Making Behavior in Medical Data Sharing. Mathematics 2023, 11, 2921. [Google Scholar] [CrossRef]
- Merrill, J.A.; Deegan, M.; Wilson, R.V.; Kaushal, R.; Fredericks, K. A system dynamics evaluation model: Implementation of health information exchange for public health reporting. J. Am. Med. Inform. Assoc. 2013, 20, e131–e138. [Google Scholar] [CrossRef]
- Eftekhari, S.; Yaraghi, N.; Gopal, R.D.; Ramesh, R. Impact of Health Information Exchange Adoption on Referral Patterns. Manag. Sci. 2023, 69, 1615–1638. [Google Scholar] [CrossRef]
- Yang, S.; Wang, H.; Lin, X. Dynamic decision of health information exchange under different hospital relationships: A differential game approach. J. Ind. Manag. Optim. 2023, 19, 6634–6663. [Google Scholar] [CrossRef]
- Kang, K.; Tan, B.Q. Carbon emission reduction investment in sustainable supply chains under cap-and-trade regulation: An evolutionary game-theoretical perspective. Expert Syst. Appl. 2023, 227, 120335. [Google Scholar] [CrossRef]
- Liu, P.; Deng, Q.; Jiang, C. Evolutionary game analysis on collaborative logistics diffusion considering diminishing marginal utility under dynamic productivity. Int. J. Syst. Sci. Oper. Logist. 2024, 11, 2339388. [Google Scholar] [CrossRef]
- Xia, P.; Liu, Z.; Qing, Q. An evolutionary game analysis of vehicle recall supervision considering the impact of public opinion. J. Oper. Res. Soc. 2022, 74, 1640–1653. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, H.; Gu, X. A Two-Stage Evolutionary Game Model for Collaborative Emergency Management Between Local Governments and Enterprises. Int. J. Disaster Risk Sci. 2023, 14, 1029–1043. [Google Scholar] [CrossRef]
- Fan, W.; Wu, X.; He, Q. Digitalization drives green transformation of supply chains: A two-stage evolutionary game analysis. Ann. Oper. Res. 2024, 1–20. [Google Scholar] [CrossRef]
- Chen, Y.; Ding, S.; Zheng, H.; Zhang, Y.; Yang, S. Exploring diffusion strategies for mHealth promotion using evolutionary game model. Appl. Math. Comput. 2018, 336, 148–161. [Google Scholar] [CrossRef]
- Zhu, C.; Zhou, L.; Zhang, X.; Walsh, C.A. Tripartite Evolutionary Game and Simulation Analysis of Healthcare Fraud Supervision under the Government Reward and Punishment Mechanism. Healthcare 2023, 11, 1972. [Google Scholar] [CrossRef]
- Friedman, D. Evolutionary Games in Economics. Econometrica 1991, 59, 637–666. [Google Scholar] [CrossRef]
- Friedman, D. On economic applications of evolutionary game theory. J. Evol. Econ. 1998, 8, 15–43. [Google Scholar] [CrossRef]
- Zhou, C.; Lan, Y.; Zhao, R.; Zhang, G. Incentive schemes for readmissions reduction in coordinating reverse referral healthcare services. Comput. Ind. Eng. 2023, 176, 108938. [Google Scholar] [CrossRef]
- Thrasher, E.H.; Craighead, C.W.; Byrd, T.A. An empirical investigation of integration in healthcare alliance networks. Decis. Support Syst. 2010, 50, 116–127. [Google Scholar] [CrossRef]
- Demirezen, E.M.; Kumar, S.; Sen, A. Sustainability of Healthcare Information Exchanges: A Game-Theoretic Approach. Inf. Syst. Res. 2016, 27, 240–258. [Google Scholar] [CrossRef]
- Shabbar, R.; Sayama, H. Health information exchange network under collaboration, cooperation, and competition: A game-theoretic approach. Health Care Manag. Sci. 2023, 26, 516–532. [Google Scholar] [CrossRef]
- Choi, S.J.; Chen, M.; Tan, X. Assessing the impact of health information exchange on hospital data breach risk. Int. J. Med. Inform. 2023, 177, 105149. [Google Scholar] [CrossRef]

| Parameters | Descriptions |
|---|---|
| The size of the medical information database () | |
| Reputation coefficient () | |
| Direct benefits coefficient () | |
| Synergy benefits coefficient () | |
| Information construction cost coefficient () | |
| Punishment for inadequate information construction () | |
| The degree of information recognition from primary healthcare institutions | |
| , | The elasticity coefficients of information synergy () |
| The elasticity coefficients of the information construction cost () |
| Primary Healthcare Institutions | |||
| General hospitals | |||
| Case 1 | |||||||||
| Scenario (1) | Scenario (2) | Scenario (3) | |||||||
| DetJ | TrJ | Stability | DetJ | TrJ | Stability | DetJ | TrJ | Stability | |
| + | − | ESS | + | − | ESS | + | − | ESS | |
| − | Uncertain | Saddle Point | + | + | Instability | − | Uncertain | Saddle Point | |
| + | + | Instability | − | Uncertain | Saddle Point | − | Uncertain | Saddle Point | |
| − | Uncertain | Saddle Point | − | Uncertain | Saddle Point | + | + | Instability | |
| − | 0 | Saddle Point | + | 0 | Saddle Point | + | 0 | Saddle Point | |
| Case 2 | |||||||||
| Scenario (4) | Scenario (5) | Scenario (6) | |||||||
| DetJ | TrJ | Stability | DetJ | TrJ | Stability | DetJ | TrJ | Stability | |
| + | + | Instability | − | Uncertain | Saddle Point | − | Uncertain | Saddle Point | |
| − | Uncertain | Saddle Point | + | + | Instability | − | Uncertain | Saddle Point | |
| + | − | ESS | + | − | ESS | + | − | ESS | |
| − | Uncertain | Saddle Point | − | Uncertain | Saddle Point | + | + | Instability | |
| − | 0 | Saddle Point | + | 0 | Saddle Point | + | 0 | Saddle Point | |
| Case 3 | Case 4 | ||||||||
| Scenario (7) | Scenario (8) | Scenario (9) | |||||||
| DetJ | TrJ | Stability | DetJ | TrJ | Stability | DetJ | TrJ | Stability | |
| + | − | ESS | − | Uncertain | Saddle Point | − | Uncertain | Saddle Point | |
| + | + | Instability | + | + | Instability | + | − | ESS | |
| + | − | ESS | − | Uncertain | Saddle Point | − | Uncertain | Saddle Point | |
| + | + | Instability | + | − | ESS | + | + | Instability | |
| − | 0 | Saddle Point | − | 0 | Saddle Point | − | 0 | Saddle Point | |
| Parameters | |||||||
| Values | 0.2 | 0.15 | 25 | 10 | 0.5 | 0.4 | 0.6 |
| Parameters | |||||||
| Values | 0.5 | 0.5 | 1 | 0.5 | 0.4 | 4 | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, S.; Wang, H. Evolutionary Game Analysis of Healthcare Information Construction and Sharing Decisions Considering Synergy Benefits. Mathematics 2024, 12, 2751. https://doi.org/10.3390/math12172751
Yang S, Wang H. Evolutionary Game Analysis of Healthcare Information Construction and Sharing Decisions Considering Synergy Benefits. Mathematics. 2024; 12(17):2751. https://doi.org/10.3390/math12172751
Chicago/Turabian StyleYang, Sen, and Haiyan Wang. 2024. "Evolutionary Game Analysis of Healthcare Information Construction and Sharing Decisions Considering Synergy Benefits" Mathematics 12, no. 17: 2751. https://doi.org/10.3390/math12172751
APA StyleYang, S., & Wang, H. (2024). Evolutionary Game Analysis of Healthcare Information Construction and Sharing Decisions Considering Synergy Benefits. Mathematics, 12(17), 2751. https://doi.org/10.3390/math12172751






