1. Introduction
Factors such as resource efficiency, the hospital’s financial situation, and the needs of the staff play an important role in hospitals, which belong to the service industry and have complex processes. Operating rooms play a large role in hospital budgets, as they contain sensitive and expensive equipment, and they have been shown to constitute up to 40% of hospital expenses and account for two-thirds of hospital income [
1]. In these units, where surgeons perform various lifesaving medical interventions, human life is critical.
Scheduling activities determine the order and time in which jobs are performed. The capacity of resources must be taken into account when determining the start and completion times of these activities. The effective use of limited resources in operating rooms comes to the fore. When scheduling operating room activities, hospitals should allocate resources [
2].
There are many studies in the literature related to operating room scheduling. Ozkarahan [
3] looked at increasing the quality of service provided in healthcare institutions with increasing demands and developed a scheduling model that met the needs of hospitals to a great extent. Arenas et al. [
4] studied a hospital in Spain, aiming at reducing patient waiting time, while at the same time balancing resources in a hospital. Blake and Donald’s [
5] study emphasized the seriousness of operating room cost in hospitals, while Blake and Carter [
6] addressed the issue of resource allocation in hospitals, using the goal programming method in their study to keep service costs constant so that they could set goals for the hospital to balance their expenses with the care that they provide.
Kharraja et al. [
7] pointed out that, in the schedules created for operating rooms in hospitals, strategies should be directed toward increasing profitability. Wullink et al. [
8] studied the rate at which the operating rooms could respond to emergency situations by assessing the situations in which emergency cases occurred. Paoletti and Marty [
9] evaluated stochastic situations with the Monte Carlo simulation model. Lamiriet et al. [
10] considered uncertain situations for operating room planning. Beliën et al. [
11] pointed to the inefficiencies of resource use in the operating room with a comprehensive case study. Zhang et al. [
12] emphasized minimizing the costs associated with the length of stay of hospital patients.
A few of the main purposes of scheduling activities are to deliver a job on time to the customer, both keeping overtime in the operating room to a minimum and reducing idle times in order to ensure efficient use. When these goals are specifically intended for hospitals, a scheduled procedure in the operating room must be performed on the specified day and at the specified time. Thus, the satisfaction of the patients, referred to as customers, can be met at the highest level. At the same time, the effectiveness of resources is ensured by avoiding idleness and overtime in operating rooms and resources [
13].
Fei et al. [
14] wanted to balance the use of both hospital surgery rooms and recovery rooms. At the same time, they aimed to minimize overtime hours and balance costs. They analyzed and compared the monthly schedule of a hospital with its actual schedule. Tànfani and Testi [
15] aimed to offer a solution to the desired goals of administration and surgeons during the process of scheduling appointments for an operating room. Banditori et al. [
16] sought solutions to problems arising from high waiting times for patients on the waiting lists and the inability to homogenous distribution of hospital resources. Cappanera et al. [
17] aimed to better balance the workload of surgeons in operating room schedules, distribute resources more efficiently and fairly, and plan more systematically. Eren et al. [
18] designed an application to address the problem associated with operating room scheduling. They developed a mathematical model for this application and realized their aims. Xiang [
19] modeled the objectives of operating room schedules using ant colony optimization and Pareto sets. Abedini et al. [
20] in their work addressed the problem of balancing resources between operating room units.
When the above literature was evaluated in detail, it was found that it emphasized that operating room usage should be the most productive, both in terms of time and resources. In this study, a model is proposed for the problems associated with operating room scheduling using integrated goal programming and constraint programming methods and datasets from a state hospital. In schedules created with the integrated goal programming and constraint programming methods, it was attempted to minimize deviations for these purposes, and a flexible model was established.
Looking at studies from different application fields in the literature (e.g., References [
21,
22,
23,
24,
25,
26,
27]), the goal programming method allows decision-makers to simultaneously realize different goals [
28,
29]. The most important features that distinguish constraint programming from mathematical programming include mathematical constraints or constraints that can be of a logical or symbolic type [
30,
31,
32]. The integrated goal programming and constraint programming methods, which are used in the solution process, are effective solution tools for researchers. Each objective set in the integrated goal programming and constraint programming methods is defined as a constraint and minimizes deviations from these objectives. A solution can always be obtained using these methods. However, the resulting decision-makers must be satisfied [
33]. The constraint programming method can include mathematical constraints, as well as constraints that can be logical or symbolic. Constraint programming problems have structures that contain the definition set, constraints, and purpose of the decision variables, are identified with an appropriate language, and are solved via polynomial. Mathematical modelling is used for the solution of the problem [
34]. However, due to the nature of the problem, the integrated goal programming and constraint programming models were developed, as it was desired to simultaneously perform more than one purpose. These methods were integrated with each other in the study.
In the operating room scheduling problem, the aim is to assign operations to the operating rooms in the appropriate time intervals. For this, block times have been defined within one working day, and restrictions have been made for assigning the same expertise to each block. Only the assignment of operations is taken into account, while the ranking of operations is not taken into consideration. This situation is also mentioned in the assumptions. The problem is solved by using the integrated goal programming and constraint programming models.
The study consists of three parts. The first part is the introduction, where scheduling activities are discussed in general, information about operating room scheduling is given, and the importance of this scheduling style is mentioned. Information about the method used in the solution process is also given. In the second part, we discuss a case study. In the third part, the implementation results are examined. The results are also interpreted in general, and suggestions are made for future studies.
2. Method
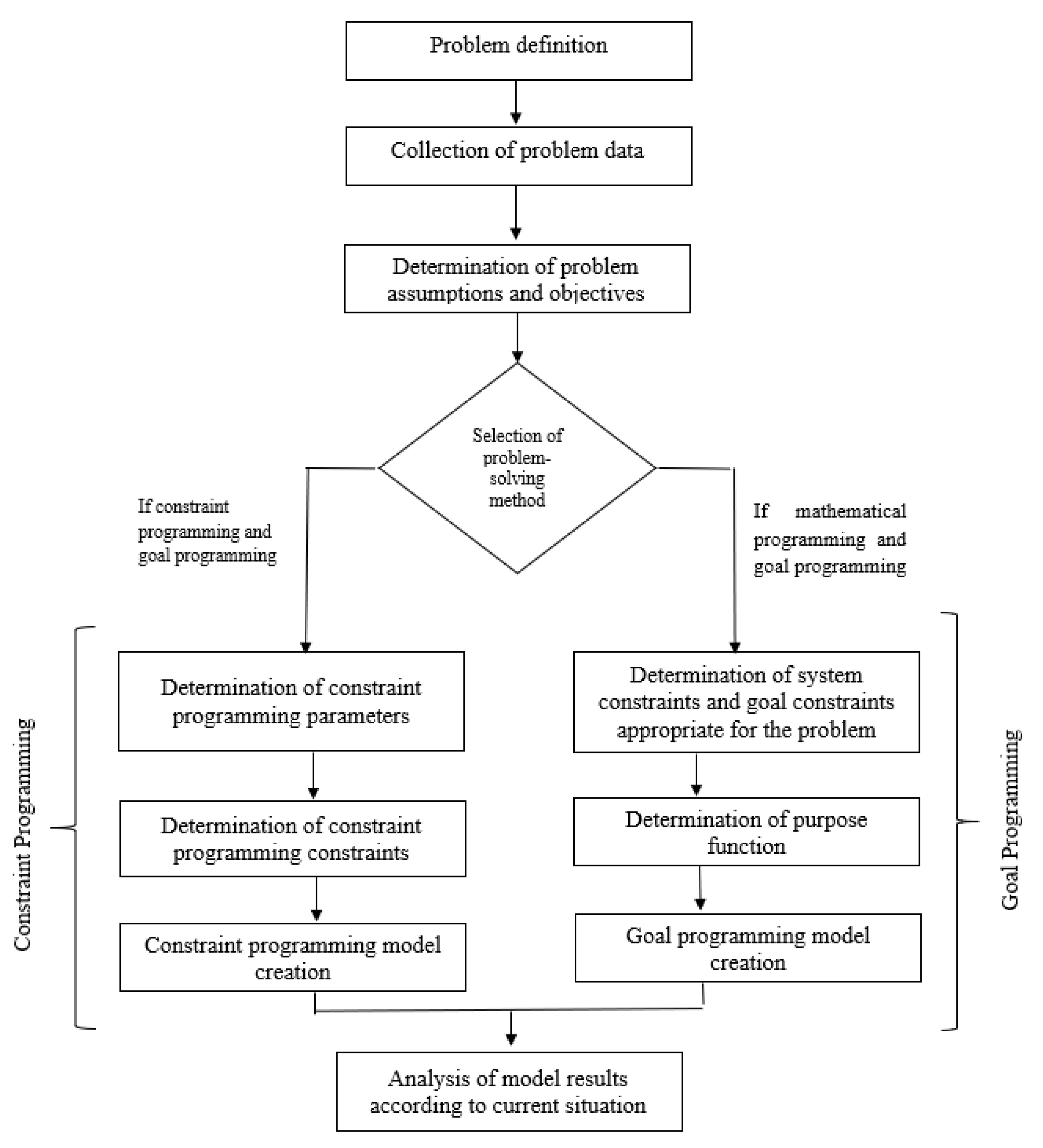
This study considers some situations that can be encountered in real life, using data from a state hospital. Increasing quality of service with the planned schedule in operating rooms, which are shown to be among the most important units of health institutions, is the main aim of this study. The flowchart of the study is shown in
Figure 1 and briefly summarizes the study.
There are various study requirements, such as the presence of equipment and devices that must be available in each operating room. Under various constraints, the assignments of these operations must be done in a systematic manner. Because there are many external factors, the operating room contains much uncertainty in its structure. For this reason, some assumptions are made in operating room scheduling. These assumptions are as follows:
The number of operations to be performed at the hospital is certain and emergency situations are not considered.
There are enough staff members and all the needed resources to perform the operations.
The average duration of each operation was calculated from past data from similar operations previously performed at the hospital. The duration of these operations includes preparation and cleaning times.
According to the decision of the hospital management committee, working hours at the hospital are 08:00–17:00, and there is one hour between 12:00 and 13:00 for lunch included in these working hours.
Surgeries are not held on weekends. For this reason, operating rooms are kept closed during this time.
Only the assignment status of the operations is taken into account on a working day.
With the operating room schedules established under these assumptions, the following are aimed:
Minimizing the cost of operating room units in the hospital;
balanced distribution of resources to prevent overtime and less use;
block scheduling;
ensuring patient and staff satisfaction is at the highest level; and
increasing hospital efficiency by getting the highest performance levels from the working staff.
The schedules formed in operating rooms, which are required to be professionally planned in line with these aims, highlight the effectiveness of the units. The data used in the study were taken from a state hospital: the number of operations, the number and capacity of existing operating rooms, the number of experts, and the operating times including preparation and cleaning times, which were prepared by using historical data.
Table 1 shows the operations of specialties and the operating times of these operations.
According to this, considering the capacities of the operating rooms, it is desired to minimize the use of overtime and less use. At the same time, a flexible model was created to allow block scheduling. Three different scenarios are considered in the study, considering three different situations. There are 120 operations planned in this hospital, which has six specialties. There are eight operating rooms for assignment of these operations. In the model, there are 10 time zones for assignments. Each time zone represents a four-hour working time. In total, it is thought that two time zones equal with one day.
2.1. Creating Surgical Schedule in Operating Rooms with the Goal Programming Method
Within the framework of the above assumptions and objectives, the model was coded and solved with IBM ILOG CPLEX [
35]. The goal programming model is given as follows.
Notation of model-forming expressions:
| |
| |
| |
| : time of operation i, including cleaning and preparation times | |
| Used daily time of operating room j in the kth time zone | |
| the set from s experts that prefers to be assigned to the time zone | |
| M: A large number | |
Deviation variables:
| amount of negative deviation to the total available time from operating room j in kth time zone; | |
| amount of positive deviation to the total available time from operating room j in kth time zone; | |
| amount of negative deviation from a balanced distribution of time zones in operating room j; | |
| amount of positive deviation from a balanced distribution of time zones in operating room j; | |
| amount of negative deviation from the preferred time zone by experts s; | |
| amount of positive deviation from the preferred time zone by experts s; | |
| amount of negative deviation from assigned experts in operating room j; | |
| amount of positive deviation from assigned experts in operating room j. | |
Constraint 1 states that each operation is assigned to the whole operating room and time zones only once. Constraint 2 ensures that at most six different specialties are able to work in all operating rooms at any time zone. Thus, operations can be carried out with the same equipment and technical personnel in the time zone. Constraints 3 and 4 always ensure that each time zone and each specialty be assigned to all operating rooms six times at most. Thus, in different time zones, different experts can be in balanced distribution in all operating rooms. It is possible to prevent the accumulation of an expert in only one operating room. Constraint 5 makes it possible to assign an expert in all operating rooms throughout the entire time zone. Thus, in the operating room separated by the same expert, operations can be carried out without any waiting or interruption due to equipment and technical personnel changes throughout the whole week.
Constraint 6 aims to minimize operating room overtime and less use of the operating room. It ensures to minimize deviations between reachable time and working time in this goal. The purpose function of this goal is as follows:
Goal Constraint 7 aims to distribute all operations in all operating rooms in a balanced manner. The right side is set to six because, in the problem with the 10 time zones, it is required to assign an average of six time zones to each operating room. Negative and positive deviations are minimized by using this constraint. The purpose function of this goal is as follows:
Goal Constraint 8 aims to perform the operations of a specialist surgeon in each operating room at the desired time zones. When the constraint is run, it is equal to zero by nothing the time zones in which we do not want to be assigned. In this goal constraint, deviation in the positive direction is minimized. Thus, attempts are made to prevent assignment to undesired time zones. The purpose function of this goal is as follows:
Goal Constraint 9 is aimed at allocation each operating room for different specialties during the week. Thus, a specialist is working all the time during the week. In this goal constraint, deviation in the positive direction is minimized. The purpose function of this goal is as follows:
With this mathematical model, three different scenarios were developed. Block scheduling was considered for 120 operations. Block schedules are enacted according to the logic of working certain specialties into specific time zones. The created scenarios are as follows:
Scenario 1. Block scheduling was worked into this model. In order to prevent overtime and less use, same-expertise operations are assigned to the same time zones. In this scenario, in the objective function, deviation in the negative and positive directions related to using operating room capacity/duration constraint is minimized. In the constraints, Equations (1)–(4) and (6) are used. Table 2 shows the solution results. Scenario 2. In this scenario, block scheduling was performed. Specialists were given the opportunity to choose certain times. According to experts who want to create this scenario, it is thought that the possibility of making a choice is beneficial for surgeons to prepare their own schedules. In this scenario, an orthopedic surgeon is needed to work in each operating room at the time period from 8:00 to 12:00. In mathematical modeling, the orthopedic surgeon’s undesirable time zones are outlined. The right side is equal to zero, and deviation in the positive direction in this goal was minimized. This was made to prevent assignment in undesirable time zones.
In this scenario, the objective function was primarily to minimize deviation in the positive direction in the time-preference constraints of surgeons with certain specialties, deviation in the positive and negative direction in the constraint on the balanced distribution of operating rooms, and deviation in the positive and negative direction at the constraint on using operating room capacity/duration. In the constraints, Equations (1)–(4) and (6)–(8) were used. Table 3 shows the solution results. Scenario 3. This scenario studies an expertise in the same operating room for the entire week. With this scenario, the same expertise was assigned throughout the whole time zone of an operating room. Thus, operations of the same expertise could be performed without changing equipment and technical personnel.
In this scenario, the objective function was primarily to minimize deviation in the positive direction of the constraint of operating rooms belonging to the same specialty, and deviation in the positive and negative direction in the constraint of using operating room capacity/duration. In the constraints, Equations (1)–(6) and (9) were used. Table 4 shows the solution results. 2.2. Creating a Surgical Schedule in Operating Rooms with Constraint Programming
The specified goals and assumptions under the heading goal programming method were also valid during this solution phase. According to the obtained data, operating room capacities and resource utilization were considered (see
Table 1). In this phase, three scenarios were created by considering different situations that were modeled by constraint programming. The time zone and operating room index were converted into single indices, and 80 (= 8 × 10) operating room time periods were named. Within the framework of these assumptions and objectives, every model was coded and resolved with the CP optimizer program.
Notation of model-forming expressions
Decision variables and parameters:
| |
| |
| |
| |
| : operation time i, including cleaning and preparation times | |
| Daily use time of operating room j | |
| set from experts s, who prefer to be assigned to the time zone | |
| M: A large number | |
Deviation variables:
| amount of negative deviation to the total available time from operating room time j; | |
| amount of positive deviation to the total available time from operating room time j; | |
| amount of negative deviation from the preferred time zone by experts s; | |
| amount of negative deviation from the preferred time zone by experts s; | |
| amount of negative deviation from assigned experts in operating room time j; | |
| amount of positive deviation from assigned experts in operating room time j. | |
Constraint 10 states that each operation is assigned to the whole operating room and the time zones only once, with operating-time boundaries to which the i operation can be assigned. Constraint 11 ensures that we have, at most, six different specialties in all operating rooms at any time zone. Thus, operations can be carried out with the same equipment and technical personnel in the time zone. An index, such as k, is added at the constraint. While this index specifies the bounds of the number of operations for the relevant expertise in index i in block scheduling, the number of the remaining operations in index k is retained. The constraint for the number of operations of each expertise is written, the number of operations of the previous expertise is also subtracted at each time, and the remaining number of operations is collected in index k. Constraints 12–14 could assign an expert in all operating rooms throughout the entire time zone. Thus, in operating rooms separated by the same expert, operations could be carried out without any wait or interruption due to equipment and technical personnel changes throughout the whole week. Constraint 12, if operation i is assigned within operating room time j, has this value stored in the decision variable with the corresponding i and j index values. In Constraints 13 and 14, operations are grouped according to their expertise and then blocked with the t-index according to the operating-time group. Thus, an expertise is only assigned to the operating room time group on a column basis.
Constraint 15 aims to minimize operating room overtime and less use of the operating room. It ensures to minimize deviations between reachable time and working time in this goal. The purpose function of this goal is as follows:
Goal Constraint 16 aims at performing a specialist surgeon’s operations in each operating room at the desired time zones. When the constraint is run, it is equal to zero by outlining the time zones during which one does not want to be assigned. The c index is expressed as a set of specializations that have preferences. In this goal constraint, deviation in the positive direction is minimized. Thus, attempts are made to prevent assignment to undesired time zones. The purpose function of this goal is as follows:
Goal Constraint 17 is aimed at allocating each operating room to different specialties during the week. Thus, a specialist works all the time during the week. In this goal constraint, deviation in the positive direction is minimized. The purpose function of this goal is as follows:
With this mathematical model, three different scenarios were developed. Block scheduling was considered for 120 operations. Block schedules act according to the logic of working certain specialties into specific time zones. These created scenarios are as follows:
Scenario 4. In this scenario, block scheduling was worked into this model. In this model, there was an attempt to balance operating room use. In order to prevent overtime and less use, same-expertise operations were assigned to the same time zones. In this scenario, the objective function was to minimize deviation in the negative and positive directions related to using operating room capacity/duration constraint. In the constraints, Equations (10), (11) and (15) were used. Table 5 shows the solution results. Scenario 5. In this scenario, block scheduling was performed. Specialists were given the opportunity to choose certain times. In this created scenario, an orthopedic surgeon wanted to work in each operating room between 8:00 and 12:00. At the same time, it ensures that overall expertise distribution is balanced. In the model, the orthopedic surgeon’s undesirable time zones are written. The right side is equal to zero, and deviation in the positive direction in this goal was minimized. It was made to prevent assignment to undesirable time zones.
In this scenario, the objective function was primarily to minimize deviation in the positive direction of the time-preference constraints of surgeons with certain specialties, and deviation in the positive and negative direction of the constraint of using operating room capacity/duration. In the constraints, Equations (10), (11), (15) and (16) were used. Table 6 shows the solution results. Scenario 6. This scenario studies a type of expertise in the same operating room for the entire week. In this scenario, which is more desirable to realize in real life, the same type of expertise was assigned throughout the whole time zone of an operating room. Thus, operations of the same expertise could be performed without changing equipment and technical personnel.
In this scenario, the objective function is primarily to minimize deviation in the positive direction of the constraint of operating rooms belonging to the same specialty, and deviation in the positive and negative direction of the constraint of using operating room capacity/duration. In the constraints, Equations (10)–(15) and (17) are used. Table 7 shows the solution results. 3. Results
In this study, the integrated-goal programming and constraint programming methods were used in the operating room scheduling processes by using data from a state hospital. Both methods have decision variables, an objective function, and restrictive equations.
Table 8 summarizes the current situation and scenarios.
Table 8 shows the success rates of both methods, modeled with integrated goal programming and constraint programming, in these scenarios. Looking at the detailed schedules, Scenarios 1 and 4 have all operations assigned through the goal programming method. The 11 time zones in the operating rooms have a full-capacity utilization rate. Thus, in some time zones, operating rooms are closed and prevented from idly waiting. Surgeons’ working hours are also programmed during working hours without overtime. Costs caused by overtime were avoided, and surgeons’ satisfaction was increased. In constraint programming, simplicity is provided in the modeling processes. In constraint programming, only the seventh operating room does not work on the third day between 08:00 and 12:00. All patient operations on the waiting list are carried out. This increased the level of patient satisfaction. However, in the 20 time zones, capacity was below the desired utilization level. However, according to the solution results, the utilization rates of the operating rooms were decreased. This situation is likely to result in costs that arise from operating room waiting times. Scenarios 2 and 5: all operations were assigned with the goal programming method. All operating room utilization rates were intended to use full capacity, but it seems that overtime was done in 17 time zones. In this case, surgeon satisfaction levels may be reduced and, at the same time, the desired surgery efficiency may be affected. It could also cause overtime costs to increase. In constraint programming, there is a capacity utilization rate at the desired level in operating rooms. In this method, overtime was only observed in two time zones, and all waiting-list patient operations were performed. The level of satisfaction of both surgeons and patients increased without overtime. In addition, overtime costs were avoided. The orthopedic surgeon wanting to work during the desired time intervals was achieved in both methods. Scenarios 3 and 6: the operating rates of operating rooms were close to 100% and worked without overtime in goal programming. Overtime was observed in operating rooms where the orthopedic surgeon appointed the constraint program. This suggests that the model is difficult to distribute over time. According to the results of the two methods, the schedule showed that the total utilization rates were very close to each other.
Looking at
Table 8, it can be seen that the obtained results are directed towards the efficiency that hospital managers want to obtain from operating rooms. Results were achieved with very little deviation. The established mathematical models were run for 3000 s. Concerning model deviations, in the results of Scenarios 1and 4, there were no deviations that would cause overtime in the goal programming results. In the case of constraint programming, a deviation of over 60 min was observed. In the results of Scenarios 2 and 5, there were 255 min of overtime in the goal programming method, and 70 min of overtime in the constraint programming method. In Scenarios 3 and 6, there was no overtime in the goal programming method. In the constraint programming method, 125 min overtime occurred. Deviation values indicate the overtime time intervals in the operating rooms. The reason for overtime in these scenarios was due to special constraints in the models. When hospital administrators provide opportunities such as special preference for surgeons and the separation of special operations of operating rooms, it can be seen that overtime occurred in the model. However, when the results are examined, the best results are obtained in the time constraint. Overtime work is done in operating rooms as little as possible, and the desired constraints and other purposes are provided. In the model, there was no deviation in other purpose constraints in the objective function. In addition, the number of decision variables in the constraint programming method was less than the number of decision variables in the goal programming model. This facilitated the establishment and resolution of the model. The results show that the operating rooms in the hospital were used as effectively as possible. In other words, it is understood that overtime rates, waiting periods, and the unnecessary use of resources in hospitals could be reduced. Reducing these conditions increases operating room efficiency. Operations can be carried out in the current time, which is separated by decreased waiting and postponements. Resources can be effectively used. At the same time, these results allow the study to be reprogrammable. In this case, it is possible to maximize the number of patients who can be treated with idle block times. Thus, it is possible to increase the obtained performance and efficiency from operating rooms. The fact that the study is open to development in this respect shows that it may have a fundamental nature. The fact that this study is adaptable according to the hospital structure emphasizes the preferable feature of hospital managers. The purpose of reducing the desired costs of operating rooms and increasing their efficiency is the overlap of the obtained results from this study. In the literature [
36,
37,
38], the main purpose of operating rooms is to reduce costs. These costs are mostly due to overtime and waiting. In order to reduce these costs, researchers benefit from different methods. Thus, they obtain high-quality and efficient programs with the methods they use in operating room scheduling processes [
39]. The aim of this study was to prevent confusion and possible problems caused by the mixed performance of hospital operations. In other words, with the assignment of different types of operations in succession to the same operating room, it is desired to increase efficiency from the equipment and surgical team. In these results, these situations are prevented. At the same time, the impact of these situations is reduced and performance is improved, allowing for a more robust and flexible start-up program.
In the current case, since schedules are manually prepared, not all operations could be transferred to the schedules, which led to an increase in patient waiting times. With these created schedules, all operations were assigned. Even though the created schedules had an overtime status in the time zones, the operating rooms were used with full capacity. In the current case, the utilization of operating rooms was not effective because the assignment of operations could not be done in a balanced way.
4. Discussion and Conclusion
The inability of surgeons to promptly enter operations, which is one of the problems experienced in hospitals today, causes both the inability to effectively use existing hospital capacity, and the decrease of offered service quality to patients. In this study, a flexible model proposal is presented with integrated goal programming and constraint programming methods. It aims to increase patient/staff satisfaction by ensuring the efficient use of hospital resources. Three different scenarios were created for the purposes of hospital managers. According to these scenarios, the established models were run for 3000 s. According to the appropriate solutions, obtained as a result of 3000 s, scenario charts were created. In the first scenario, on the basis of the block-scheduling strategy, the aim was the balanced distribution of operations in operating rooms and the effective use of operating rooms. In the second scenario, in addition to these goals, an objective for the orthopedic surgeon to only work during morning hours was determined, and the balanced distribution of operations in the time zones was desired. In the third scenario, it was desirable that an operating room be divided into only one specialty during all time zones. All these scenarios are modeled by the integrated-goal programming and constraint programming methods. Then, the method results were compared and analyzed according to the current situation.
When creating the model, we tried to create weekly schedules, together with the time-zone index, without complicating the problem structure. In the scenarios, utilization rates were a measure of how effectively operating room capacity was being used. This shows that the methods help to make the process systematic. According to the current situation, schedule efficiency was increased with the created models, and the best possible utilization of the operating room was achieved. It is aimed that this study will be an example for future studies. With the integration of constraint programming and goal programming, it has contributed to the literature by increasing schedule effectiveness. With this integration, scenarios were created for different desired goals from other work.
When other studies in the literature are examined, it is seen that operating room scheduling studies have frequently been discussed by the researchers in the last forty years [
39]. Studies [
39,
40,
41,
42] indicate that operating room planning is affected by personnel and equipment-based factors. Therefore, multiple objectives cannot be taken into consideration in planning and scheduling. In this context, problems can be solved by developing strategies for solution techniques. Researchers use various solution methods in operating room scheduling problems [
43,
44,
45]. Each method has its own advantage. These methods are also determined according to the problem type. In this study, unlike other studies, the integrated goal programming and constraint programming methods, which are effective for the simultaneous realization of the desired objectives, were used. This integration allows flexibility in the objectives and enables to produce solutions to real-life problems [
33]. At the same time, in this study, the realization of situations encountered in real-life scenarios differentiates the process from other studies. In fact, multiple real-life problems could be considered at the same time with this scenario. In this case, a systematic structure was developed to solve problems encountered in hospitals. In addition, the integrated goal programming and constraint programming methods enable the solution process to be suitable for real life by operationally strengthening the study. Because the work allows flexibility, it is easy to create a new start-up program at times when reprogramming is needed. The discussed multipurpose problem was solved for the single purpose of modelling. The objectives to be carried out in the solution process were combined with the goal programming method, and the problem was modelled using the constraint programming method. With the systematic structure established, the model can quickly be reviewed without major and complex changes. In this context, this study comes to the fore in the literature. In this study, the flexibility and advantages of goal programming and constraint programming were utilized. The constraint programming method facilitates writing logical constraints in the modelling process. At the same time, decision variables can take values in different structures besides numerical variables. In the solution processes, the constraint programming method allows decision-makers to establish models with fewer decision variables. Decision makers can use the search algorithms defined in the modelling phase. Considering the advantages of the constraint programming method, the basic constraint programming model is proposed in the problem solution. The operating room scheduling problem mainly deals with which operation should be assigned to which operating room. In this problem, the decision variable structure is a 0–1 logic structure. If the operation is assigned to the operating room, it takes the value of 1; if it is not assigned, it takes 0. Different solution approaches were developed by researchers for the scheduling problems involving this 0–1 variable structure. The constraint programming method also allows to model variables in the 0–1 structure as an integer [
46]. The constraint programming method has a structure that can work more efficiently with relatively few variables in the modelling. With this feature, constraint programming provides better performance by reducing the domain. This problem is translated from a 0–1 structure into an integer structure by taking advantage of the modelling power of constraint programming [
46].
At the same time, in the literature, researchers mostly focus on an open-planning strategy as they facilitate the solution process. However, this situation causes operations with the same expertise in operating rooms to be assigned to different operating rooms at different times. This necessitates the permanent displacement of equipment used during operations in operating rooms. Most of the time, due to these displacements, equipment damage or patient/surgeon waiting times increase. In this context, all these reasons exponentially cause negative consequences to hospital managers. Considering all this, a block-scheduling strategy was adopted in this study to avoid negative results, and to ensure patient/surgeon satisfaction in the hospital. When block-scheduling studies [
11,
15,
16,
20,
47,
48,
49] in the literature are examined, it is understood that they want to avoid these negative results.
In future studies, the inclusion of different constraints could be considered with regard to the special circumstances of surgeons’ working conditions. Depending on each surgeon’s preferences, prioritization and assignments can be made using multicriteria decision-making methods in operations. Various situations could be considered, such as the fact that special circumstances related to the staff are reflected in the constraints.