Numerical Modeling of Face Shield Protection against a Sneeze
Abstract
:1. Introduction
2. Materials and Methods
2.1. Validation
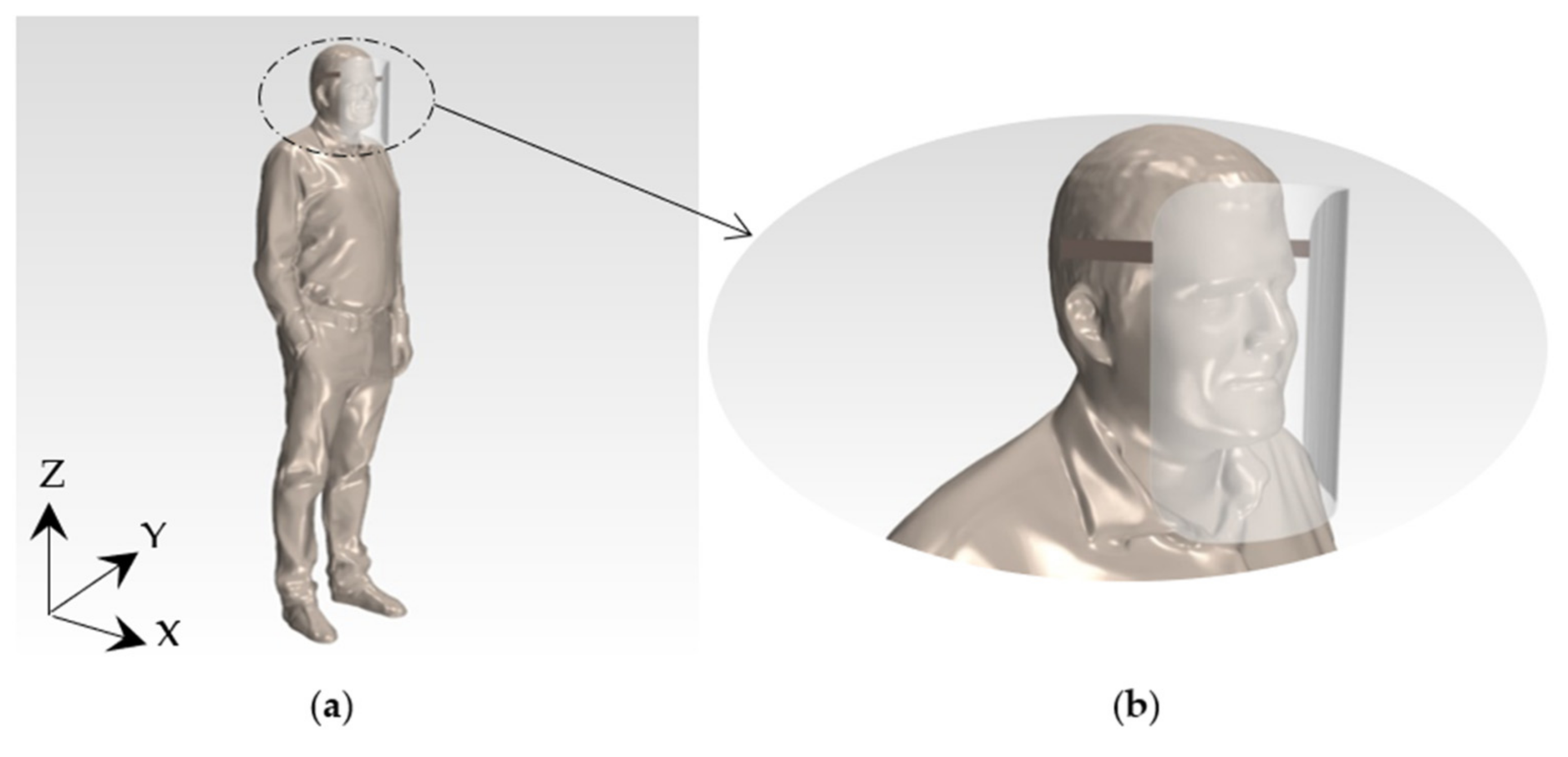
2.2. Computational Domain and Initial Conditions
2.3. Numerical Setup
3. Results
3.1. Effect of Relative Humidity and Environment Temperature in the Droplets’ Evaporation
3.2. Wind Analysis on the Path of the Droplets and a Social Distance Check
3.3. Consequences of People’s Height Difference in Protecting Themselves
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Saunders-Hastings, P.R.; Krewski, D. Reviewing the History of Pandemic Influenza: Understanding Patterns of Emergence and Transmission. Pathogens 2016, 5, 66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verma, S.; Dhanak, M.; Frankenfield, J. Visualizing droplet dispersal for face shields and masks with exhalation valves. Phys. Fluids 2020, 32, 91701. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Kato, S.; Yang, J. Study on transport characteristics of saliva droplets produced by coughing in a calm indoor environment. Build. Environ. 2006, 41, 1691–1702. [Google Scholar] [CrossRef]
- Wang, B.; Wu, H.; Wan, X. Transport and fate of human expiratory droplets-A modeling approach. Phys. Fluids 2020, 32, 083307. [Google Scholar] [CrossRef]
- Redrow, J.; Mao, S.; Celik, I.; Posada, J.A.; Feng, Z. Modeling the evaporation and dispersion of airborne sputum droplets expelled from a human cough. Build. Environ. 2011, 46, 2042–2051. [Google Scholar] [CrossRef]
- Li, X.; Shang, Y.; Yan, Y.; Yang, L.; Tu, J. Modelling of evaporation of cough droplets in inhomogeneous humidity fields using the multi-component Eulerian-Lagrangian approach. Build. Environ. 2018, 128, 68–76. [Google Scholar] [CrossRef]
- Wei, J.; Li, Y. Enhanced spread of expiratory droplets by turbulence in a cough jet. Build. Environ. 2015, 93, 86–96. [Google Scholar] [CrossRef]
- Morawska, L. Droplet fate in indoor environments, or can we prevent the spread of infection? Indoor Air 2006, 16, 335–347. [Google Scholar] [CrossRef] [Green Version]
- Xie, X.; Li, Y.; Chwang, A.T.Y.; Ho, P.L.; Seto, E.H. How far droplets can move in indoor environments -revisiting the Wells evaporation-falling curve. Indoor Air 2007, 17, 211–225. [Google Scholar] [CrossRef]
- Chillón, S.A.; Ugarte-Anero, A.; Aramendia, I.; Fernandez-Gamiz, U.; Zulueta, E. Numerical Modeling of the Spread of Cough Saliva Droplets in a Calm Confined Space. Mathematics 2021, 9, 574. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef]
- Feng, Y.; Marchal, T.; Sperry, T.; Yi, H. Influence of wind and relative humidity on the social distancing effectiveness to prevent COVID-19 airborne transmission: A numerical study. J. Aerosol Sci. 2020, 147, 105585. [Google Scholar] [CrossRef]
- Li, H.; Leong, F.Y.; Xu, G.; Ge, Z.; Kang, C.W.; Lim, K.H. Dispersion of evaporating cough droplets in tropical outdoor environment. Phys. Fluids 2020, 32, 113301. [Google Scholar] [CrossRef]
- Dbouk, T.; Drikakis, D. On coughing and airborne droplet transmission to humans. Phys. Fluids 2020, 32, 053310. [Google Scholar] [CrossRef]
- Sen, N. Transmission and evaporation of cough droplets in an elevator: Numerical simulations of some possible scenarios. Phys. Fluids 2021, 33, 033311. [Google Scholar] [CrossRef]
- Akhtar, J.; Garcia, A.L.; Saenz, L.; Kuravi, S.; Shu, F.; Kota, K. Can face masks offer protection from airborne sneeze and cough droplets in close-up, face-to-face human interactions? —A quantitative study. Phys. Fluids 2020, 32, 127112. [Google Scholar] [CrossRef]
- Arumuru, V.; Pasa, J.; Samantaray, S.S.; Surendrasingh Varma, V. Breathing, virus transmission, and social distancing—An experimental visualization study. AIP Adv. 2021, 11, 045205. [Google Scholar] [CrossRef]
- Salimnia, H.; Meyer, M.P.; Mitchell, R.; Fairfax, M.R.; Gundel, A.; Guru, N.; Chopra, T. A laboratory model demonstrating the protective effects of surgical masks, face shields, and a combination of both in a speaking simulation. Am. J. Infect. Control 2021, 49, 409–415. [Google Scholar] [CrossRef]
- Akagi, F.; Haraga, I.; Inage, S.; Akiyoshi, K. Effect of sneezing on the flow around a face shield. Phys. Fluids 2020, 32, 127105. [Google Scholar] [CrossRef]
- Wendling, J.; Fabacher, T.; Pébaÿ, P.; Cosperec, I.; Rochoy, M. Experimental Efficacy of the Face Shield and the Mask against Emitted and Potentially Received Particles. Int. J. Environ. Res. Public Health 2021, 18, 1942. [Google Scholar] [CrossRef]
- Chen, W.; Liu, Y.; Wang, C.; Wise, S.M. Convergence analysis of a fully discrete finite difference scheme for the Cahn-Hilliard-Hele-Shaw equation. Math. Comput. 2016, 85, 2231–2257. [Google Scholar] [CrossRef] [Green Version]
- Feng, X.; Prohl, A. Error analysis of a mixed finite element method for the Cahn-Hilliard equation. Numer Math 2004, 99, 47–84. [Google Scholar] [CrossRef] [Green Version]
- Yan, Y.; Chen, W.; Wang, C.; Wise, S.M. A Second-Order Energy Stable BDF Numerical Scheme for the Cahn-Hilliard Equation. Commun. Comput. Phys. 2018, 23. [Google Scholar] [CrossRef] [Green Version]
- Diegel, A.; Wang, C.; Wang, X.; Wise, S. Convergence analysis and error estimates for a second order accurate finite element method for the Cahn–Hilliard–Navier–Stokes system. Numer Math 2017, 137, 495–534. [Google Scholar] [CrossRef]
- Hamey, P.Y. The Evaporation of Airborne Droplets. Master’s Thesis, Cranfield Institute of Technology, Bedfordshire, UK, 1982. [Google Scholar]
- Carpenter, G.H. The Secretion, Components, and Properties of Saliva. Annu. Rev. Food Sci. Technol. 2013, 4, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Nicas, M.; Nazaroff, W.W.; Hubbard, A. Toward Understanding the Risk of Secondary Airborne Infection: Emission of Respirable Pathogens. J. Occup. Environ. Hyg. 2005, 2, 143–154. [Google Scholar] [CrossRef]
- Busco, G.; Yang, R.; Seo, J.; Hassan, Y.A. Sneezing and asymptomatic virus transmission. Phys. Fluids 2020, 32, 073309. [Google Scholar] [CrossRef] [PubMed]
- Kukkonen, J.; Vesala, T.; Kulmala, M. The interdependence of evaporation and settling for airborne freely falling droplets. J. Aerosol Sci. 1989, 20, 749–763. [Google Scholar] [CrossRef]
- Menter, F.R. Two-equation eddy-viscosity turbulence models for engineering applications. AIAA J. 1994, 32, 1598–1605. [Google Scholar] [CrossRef] [Green Version]
- Xie, X.; Li, Y.; Sun, H.; Liu, L. Exhaled droplets due to talking and coughing. J. R. Soc. Interface 2009, 6, S703–S714. [Google Scholar] [CrossRef] [Green Version]
- Karunarathne, S.; Tokheim, L. Comparison of the influence of drag models in CFD simulation of particle mixing and segregation in a rotating cylinder. Linköping Electron. Conf. Proc. 2017, 138, 151–156. [Google Scholar] [CrossRef] [Green Version]
- Siemens STAR CCM+ Version 14.02. Available online: http://mdx.plm.automation.siemens.com/ (accessed on 15 March 2021).
- Ho, C.K. Modeling airborne pathogen transport and transmission risks of SARS-CoV-2. Appl. Math. Model. 2021, 95, 297–319. [Google Scholar] [CrossRef]
- Jayaweera, M.; Perera, H.; Gunawardana, B.; Manatunge, J. Transmission of COVID-19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environ. Res. 2020, 188, 109819. [Google Scholar] [CrossRef]
- SARS-CoV-2 Variants of Concern and Variants under Investigation in England. Public Health Engl. 2021, 71.
- Sheikh, A.; McMenamin, J.; Taylor, B.; Robertson, C. SARS-CoV-2 Delta VOC in Scotland: Demographics, risk of hospital admission, and vaccine effectiveness. Lancet 2021, 397, 2461–2462. [Google Scholar] [CrossRef]
- Crawford, C.; Vanoli, E.; Decorde, B.; Lancelot, M.; Duprat, C.; Josserand, C.; Jilesen, J.; Bouadma, L.; Timsit, J.O. Modeling of aerosol transmission of airborne pathogens in ICU rooms of COVID-19 patients with acute respiratory failure. Sci. Rep. 2021, 11, 1–12. [Google Scholar] [CrossRef]
- Adhikari, U.; Chabrelie, A.; Weir, M.; Boehnke, K.; McKenzie, E.; Ikner, L.; Wang, M.; Wang, Q.; Young, K.; Haas, C.N.; et al. A Case Study Evaluating the Risk of Infection from Middle Eastern Respiratory Syndrome Coronavirus (MERS-CoV) in a Hospital Setting Through Bioaerosols. Risk Anal. 2019, 39, 2608–2624. [Google Scholar] [CrossRef] [PubMed] [Green Version]



 ) indicates the mouth of the individual that has the virus and sneezes: (a) The mesh in the domain when the mouths were at the same height; (b) The mesh in the domain when the mouths were at different heights (20 cm difference).
) indicates the mouth of the individual that has the virus and sneezes: (a) The mesh in the domain when the mouths were at the same height; (b) The mesh in the domain when the mouths were at different heights (20 cm difference).
 ) indicates the mouth of the individual that has the virus and sneezes: (a) The mesh in the domain when the mouths were at the same height; (b) The mesh in the domain when the mouths were at different heights (20 cm difference).
) indicates the mouth of the individual that has the virus and sneezes: (a) The mesh in the domain when the mouths were at the same height; (b) The mesh in the domain when the mouths were at different heights (20 cm difference).






| Dimension | Value |
|---|---|
| Height | 250 mm |
| Length | 196 mm |
| Area | 660 mm2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ugarte-Anero, A.; Fernandez-Gamiz, U.; Aramendia, I.; Zulueta, E.; Lopez-Guede, J.M. Numerical Modeling of Face Shield Protection against a Sneeze. Mathematics 2021, 9, 1582. https://doi.org/10.3390/math9131582
Ugarte-Anero A, Fernandez-Gamiz U, Aramendia I, Zulueta E, Lopez-Guede JM. Numerical Modeling of Face Shield Protection against a Sneeze. Mathematics. 2021; 9(13):1582. https://doi.org/10.3390/math9131582
Chicago/Turabian StyleUgarte-Anero, Ainara, Unai Fernandez-Gamiz, Iñigo Aramendia, Ekaitz Zulueta, and Jose Manuel Lopez-Guede. 2021. "Numerical Modeling of Face Shield Protection against a Sneeze" Mathematics 9, no. 13: 1582. https://doi.org/10.3390/math9131582







