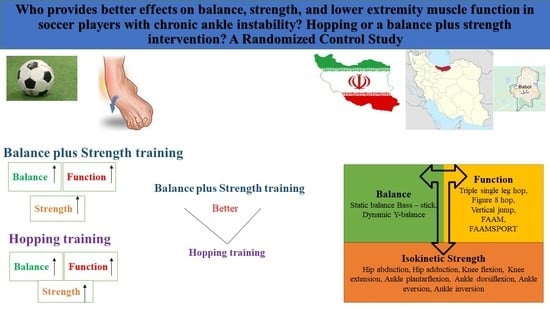
What Does Provide Better Effects on Balance, Strength, and Lower Extremity Muscle Function in Professional Male Soccer Players with Chronic Ankle Instability? Hopping or a Balance Plus Strength Intervention? A Randomized Control Study
Abstract
:1. Introduction
2. Materials and Methods
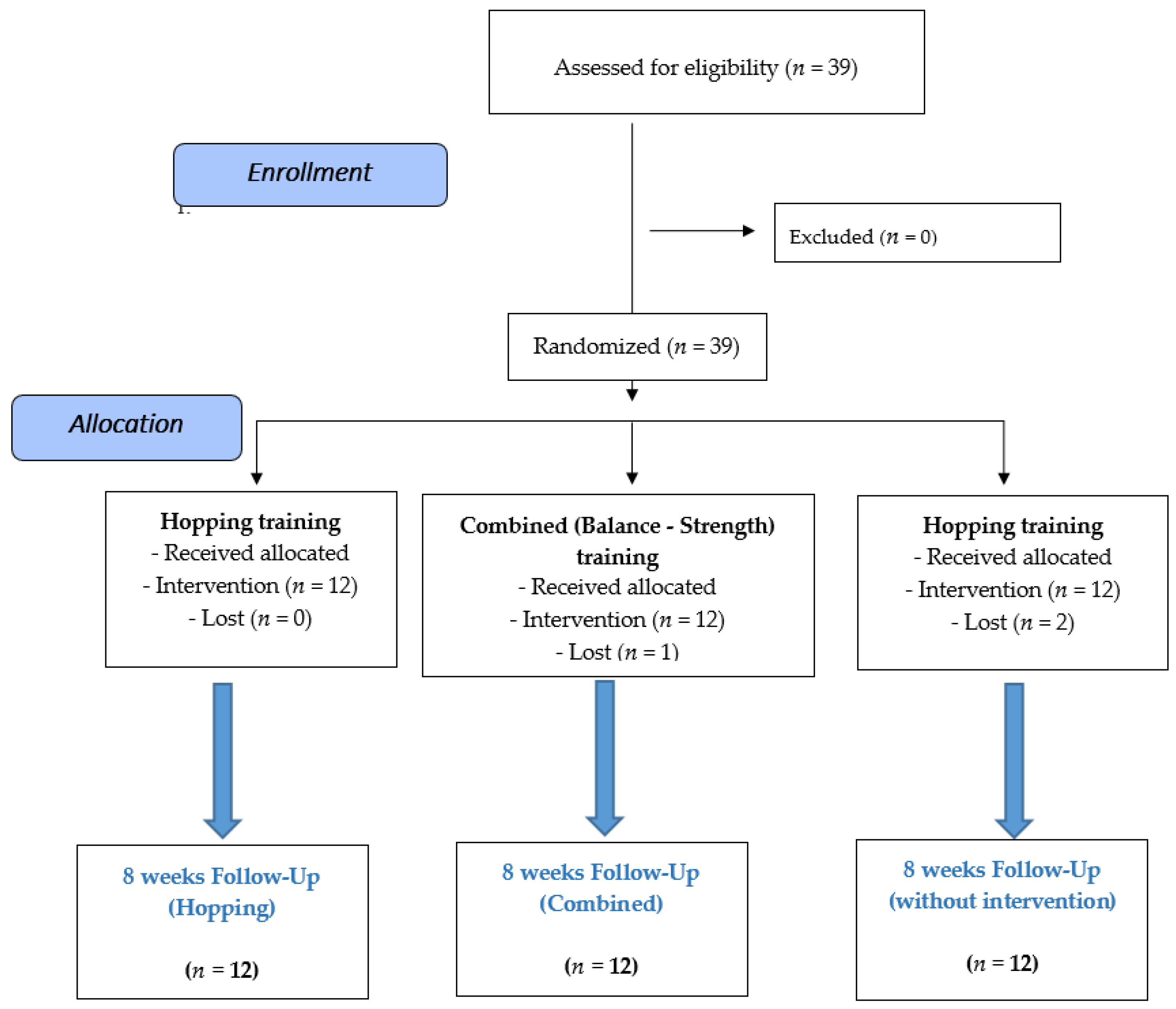
2.1. Design
2.2. Participants
2.3. Sample Size
2.4. Randomization
2.5. Procedures
2.5.1. Assessment of Dynamic Balance
2.5.2. Isometric Tests
Assessment of Isometric Hip Abductor Strength
Assessment of Isometric Hip Adductor Strength
Assessment of Isometric Knee Flexor Strength
Assessment of Isometric Knee Extensor Strength
Assessment of Isometric Ankle Plantarflexion and Dorsiflexion Strength
Assessment of Isometric Ankle Inversion and Eversion Strength
2.5.3. Assessment of Triple Hop
2.5.4. Assessment of Figure 8 Hop
2.5.5. Assessment of Vertical Jump
2.6. Interventions
2.6.1. Balance plus Strength Protocol
2.6.2. Hopping Protocol
2.6.3. Statistical Analysis
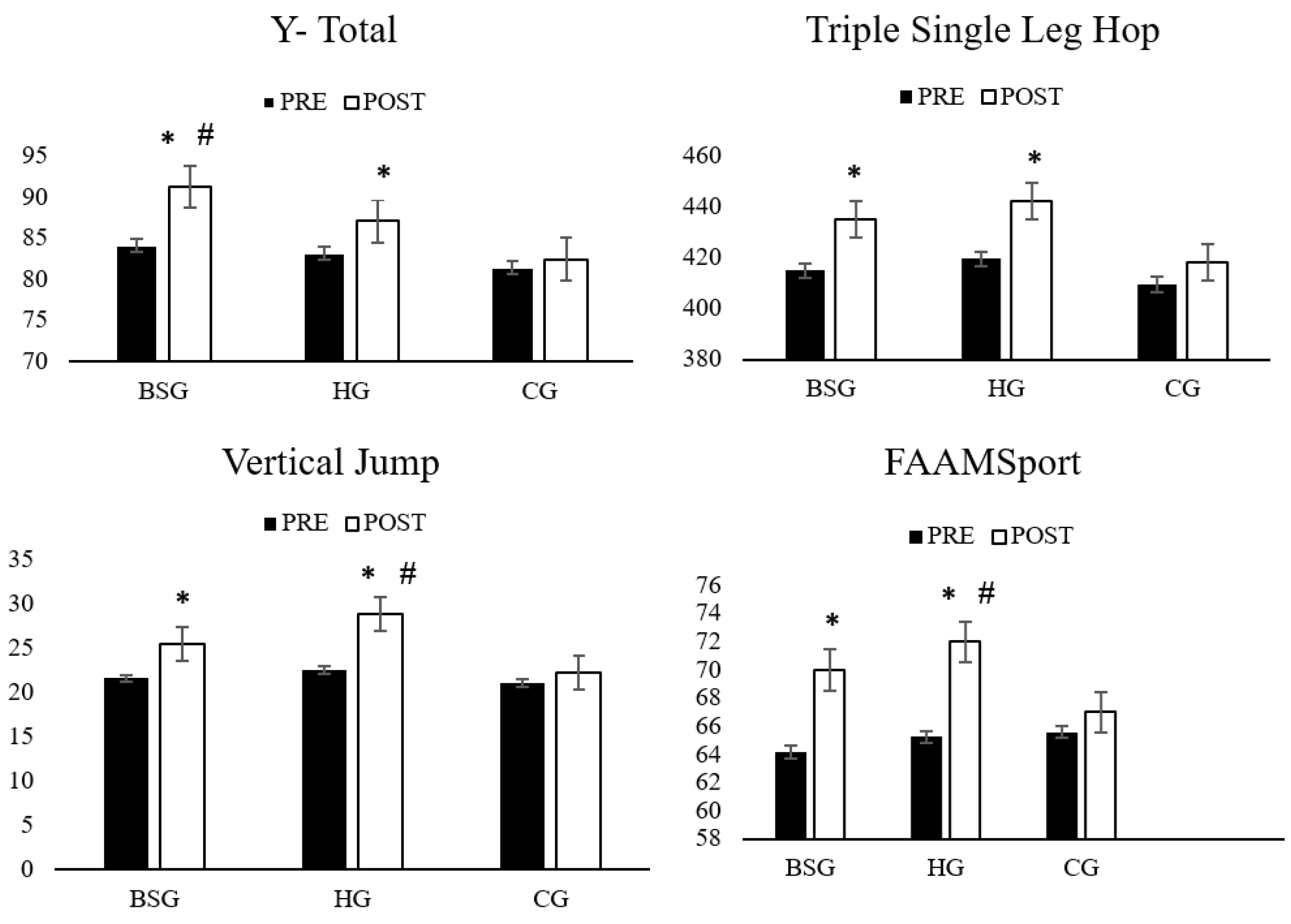
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hertel, J.; Corbett, R.O. An updated model of chronic ankle instability. J. Athl. Train. 2019, 54, 572–588. [Google Scholar] [CrossRef] [PubMed]
- Hale, S.A.; Fergus, A.; Axmacher, R.; Kiser, K. Bilateral improvements in lower extremity function after unilateral balance training in individuals with chronic ankle instability. J. Athl. Train. 2014, 49, 181–191. [Google Scholar] [CrossRef] [PubMed]
- Hubbard, T.J.; Wikstrom, E.A. Ankle sprain: Pathophysiology, predisposing factors, and management strategies. Open Access J. Sports Med. 2010, 1, 115. [Google Scholar] [CrossRef] [PubMed]
- Silva, D.C.F.; Santos, R.; Vilas-Boas, J.P.; Macedo, R.; Montes, A.M.; Sousa, A.S.P. Different cleat models do not influence side hop test performance of soccer players with and without chronic ankle instability. J. Hum. Kinet. 2019, 70, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Schiftan, G.S.; Ross, L.A.; Hahne, A.J. The effectiveness of proprioceptive training in preventing ankle sprains in sporting populations: A systematic review and meta-analysis. J. Sci. Med. Sport 2015, 18, 238–244. [Google Scholar] [CrossRef]
- Lee, A.J.; Lin, W.-H. The influence of gender and somatotype on single-leg upright standing postural stability in children. J. Appl. Biomech. 2007, 23, 173–179. [Google Scholar] [CrossRef]
- Kachouri, H.; Borji, R.; Baccouch, R.; Laatar, R.; Rebai, H.; Sahli, S. The effect of a combined strength and proprioceptive training on muscle strength and postural balance in boys with intellectual disability: An exploratory study. Res. Dev. Disabil. 2016, 53, 367–376. [Google Scholar] [CrossRef]
- Gribble, P.; Hertel, J.; Denegar, C.R.; Buckley, W.E. The effects of fatigue and chronic ankle instability on dynamic postural control. J. Athl. Train. 2004, 39, 321–329. [Google Scholar]
- Smith, B.I.; Docherty, C.L.; Simon, J.; Klossner, J.; Schrader, J. Ankle strength and force sense after a progressive, 6-week strength-training program in people with functional ankle instability. J. Athl. Train. 2012, 47, 282–288. [Google Scholar] [CrossRef]
- Minoonejad, H.; Ardakani, M.K.; Rajabi, R.; Wikstrom, E.A.; Sharifnezhad, A. Hop stabilization training improves neuromuscular control in college basketball players with chronic ankle instability: A randomized controlled trial. J. Sport Rehabil. 2019, 28, 576–583. [Google Scholar] [CrossRef]
- Ardakani, M.K.; Wikstrom, E.A.; Minoonejad, H.; Rajabi, R.; Sharifnezhad, A. Hop-stabilization training and landing biomechanics in athletes with chronic ankle instability: A randomized controlled trial. J. Athl. Train. 2019, 54, 1296–1303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taube, W.; Kullmann, N.; Leukel, C.; Kurz, O.; Amtage, F.; Gollhofer, A. Differential reflex adaptations following sensorimotor and strength training in young elite athletes. Endoscopy 2007, 28, 999–1005. [Google Scholar] [CrossRef] [PubMed]
- Hertel, J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J. Athl. Train. 2002, 37, 364–375. [Google Scholar] [PubMed]
- Martin, R.L.; Irrgang, J.J.; Burdett, R.G.; Conti, S.F.; Van Swearingen, J.M. Evidence of validity for the foot and ankle ability measure (FAAM). Foot Ankle Int. 2005, 26, 968–983. [Google Scholar] [CrossRef] [PubMed]
- Hiller, C.E.; Refshauge, K.M.; Bundy, A.C.; Herbert, R.D.; Kilbreath, S.L. The cumberland ankle instability tool: A report of validity and reliability testing. Arch. Phys. Med. Rehabil. 2006, 87, 1235–1241. [Google Scholar] [CrossRef]
- Hiller, C.E.; Kilbreath, S.L.; Refshauge, K.M. Chronic ankle instability: Evolution of the model. J. Athl. Train. 2011, 46, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Prajapati, B.; Dunne, M.; Armstrong, R. Sample size estimation and statistical power analyses. Optom. Today 2010, 16, 10–18. [Google Scholar]
- Gorji, S.M.; Samakosh, H.M.N.; Watt, P.; Marchetti, P.H.; Oliveira, R. Pain neuroscience education and motor control exercises versus core stability exercises on pain, disability, and balance in women with chronic low back pain. Int. J. Environ. Res. Public Health 2022, 19, 2694. [Google Scholar] [CrossRef]
- Chan, K.W.; Ding, B.C.; Mroczek, K.J. Acute and chronic lateral ankle instability in the athlete. Bull. NYU Hosp. Jt. Dis. 2011, 69, 17. [Google Scholar]
- Bulow, A.; Anderson, J.E.; Leiter, J.R.; MacDonald, P.B.; Peeler, J. The modified star excursion balance and y-balance test results differ when assessing physically active healthy adolescent females. Int. J. Sports Phys. Ther. 2019, 14, 192–203. [Google Scholar] [CrossRef]
- Rad, Z.M.; Norasteh, A.A. The effect of a six-week core stability exercises on balance, strength, and endurance in female students with trunk defects. Phys. Treat. Specif. Phys. Ther. J. 2020, 10, 231–238. [Google Scholar] [CrossRef]
- Burcal, C.J.; Chung, S.; Johnston, M.L.; Rosen, A.B. Does the method of administration affect reliability of the foot and ankle ability measure? J. Sport Rehabil. 2020, 29, 1038–1041. [Google Scholar] [CrossRef]
- McBeth, J.M.; Earl-Boehm, J.E.; Cobb, S.C.; Huddleston, W.E. Hip muscle activity during 3 side-lying hip-strengthening exercises in distance runners. J. Athl. Train. 2012, 47, 15–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daloia, L.M.T.; Figueiredo, M.M.L.; Martinez, E.Z.; Mattiello-Sverzut, A.C. Isometric muscle strength in children and adolescents using Handheld dynamometry: Reliability and normative data for the Brazilian population. Braz. J. Phys. Ther. 2018, 22, 474–483. [Google Scholar] [CrossRef] [PubMed]
- Swearingen, J.; Lawrence, E.; Stevens, J.; Jackson, C.; Waggy, C.; Davis, D.S. Correlation of single leg vertical jump, single leg hop for distance, and single leg hop for time. Phys. Ther. Sport 2011, 12, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Tveter, A.T.; Holm, I. Influence of thigh muscle strength and balance on hop length in one-legged hopping in children aged 7–12 years. Gait Posture 2010, 32, 259–262. [Google Scholar] [CrossRef]
- Caffrey, E.; Docherty, C.L.; Schrader, J.; Klossnner, J. The ability of 4 single-limb hopping tests to detect functional performance deficits in individuals with functional ankle instability. J. Orthop. Sports Phys. Ther. 2009, 39, 799–806. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155. [Google Scholar] [CrossRef]
- Huang, P.-Y.; Jankaew, A.; Lin, C.-F. Effects of plyometric and balance training on neuromuscular control of recreational athletes with functional ankle instability: A randomized controlled laboratory study. Int. J. Environ. Res. Public Health 2021, 18, 5269. [Google Scholar] [CrossRef]
- Hall, E.A.; Chomistek, A.K.; Kingma, J.J.; Docherty, C.L. Balance-and strength-training protocols to improve chronic ankle instability deficits, part I: Assessing clinical outcome measures. J. Athl. Train 2018, 53, 568–577. [Google Scholar] [CrossRef]
- Ford, K.; Nguyen, A.-D.; Dischiavi, S.; Hegedus, E.; Zuk, E.; Taylor, J. An evidence-based review of hip-focused neuromuscular exercise interventions to address dynamic lower extremity valgus. Open Access J. Sports Med. 2015, 6, 291–303. [Google Scholar] [CrossRef] [PubMed]
- Mok, N.W.; Yeung, E.W.; Cho, J.C.; Hui, S.C.; Liu, K.C.; Pang, C.H. Core muscle activity during suspension exercises. J. Sci. Med. Sport 2015, 18, 189–194. [Google Scholar] [CrossRef]
- Gordon, A.T.; Ambegaonkar, J.P.; Caswell, S.V. Relationships between core strength, hip external rotator muscle strength, and star excursion balance test performance in female lacrosse players. Int. J. Sports Phys. Ther. 2013, 8, 97–104. [Google Scholar] [PubMed]
- Ben Kibler, W.; Press, J.; Sciascia, A. The role of core stability in athletic function. Sports Med. 2006, 36, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Munn, J.; Sullivan, S.J.; Schneiders, A. Evidence of sensorimotor deficits in functional ankle instability: A systematic review with meta-analysis. J. Sci. Med. Sport 2010, 13, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Holm, I.; Tveter, A.T.; Fredriksen, P.M.; Vøllestad, N. A normative sample of gait and hopping on one leg parameters in children 7–12 years of age. Gait Posture 2009, 29, 317–321. [Google Scholar] [CrossRef]
- Myer, G.D.; Ford, K.R.; Brent, J.L.; Hewett, T.E. The effects of plyometric vs. dynamic stabilization and balance training on power, balance, and landing force in female athletes. J. Stren. Cond. Res. 2006, 20, 345. [Google Scholar]
- Kramer, A.; Kümmel, J.; Gollhofer, A.; Armbrecht, G.; Ritzmann, R.; Belavy, D.; Felsenberg, D.; Gruber, M. Plyometrics can preserve peak power during 2 months of physical inactivity: An RCT including a one-year follow-up. Front. Physiol. 2018, 9, 633. [Google Scholar] [CrossRef]
- Ullrich, B.; Pelzer, T.; Pfeiffer, M. Neuromuscular effects to 6 weeks of loaded countermovement jumping with traditional and daily undulating periodization. J. Strength Cond. Res. 2018, 32, 660–674. [Google Scholar] [CrossRef]
- Noyes, F.R.; Barber-Westin, S.D.; Smith, S.T.T.; Campbell, T. A training program to improve neuromuscular and performance indices in female high school soccer players. J. Strength Cond. Res. 2013, 27, 340–351. [Google Scholar] [CrossRef]
- Hewett, T.E.; Stroupe, A.L.; Nance, T.A.; Noyes, F.R. Plyometric training in female athletes: Decreased impact forces and increased hamstring torques. Am. J. Sports Med. 1996, 24, 765–773. [Google Scholar] [CrossRef] [PubMed]
- Noyes, F.R.; Barber-Westin, S.D.; Smith, S.T.; Campbell, T.; Garrison, T.T. A Training program to improve neuromuscular and performance indices in female high school basketball players. J. Strength Cond. Res. 2012, 26, 709–719. [Google Scholar] [CrossRef] [PubMed]
- Barber-Westin, S.D.; Hermeto, A.A.; Noyes, F.R. A six-week neuromuscular training program for competitive junior tennis players. J. Strength Cond. Res. 2010, 24, 2372–2382. [Google Scholar] [CrossRef] [PubMed]
- Noyes, F.R.; Barber-Westin, S.D.; Smith, S.T.; Campbell, T. A Training program to improve neuromuscular indices in female high school volleyball players. J. Strength Cond. Res. 2011, 25, 2151–2160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Markovic, G.; Mikulic, P. Neuro-musculoskeletal and performance adaptations to lower-extremity plyometric training. Sports Med. 2010, 40, 859–895. [Google Scholar] [CrossRef] [PubMed]
- Butler, R.J.; Crowell III, H.P.; Davis, I.M. Lower extremity stiffness: Implications for performance and injury. Clin. Biomech. 2003, 18, 511–517. [Google Scholar] [CrossRef]
- McKeon, P.O.; Hertel, J. Systematic review of postural control and lateral ankle instability, part I: Can deficits be detected with instrumented testing? J. Athl. Train. 2008, 43, 293–304. [Google Scholar] [CrossRef]
- Webster, K.A.; Gribble, P.A. Functional rehabilitation interventions for chronic ankle instability: A systematic review. J. Sport Rehabil. 2010, 19, 98–114. [Google Scholar] [CrossRef]
- Carcia, C.R.; Martin, R.L.; Drouin, J.M. Validity of the foot and ankle ability measure in athletes with chronic ankle instability. J. Athl. Train. 2008, 43, 179–183. [Google Scholar] [CrossRef]
- Teixeira, J.; Forte, P.; Ferraz, R.; Leal, M.; Ribeiro, J.; Silva, A.; Barbosa, T.; Monteiro, A. Monitoring accumulated training and match load in football: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 3906. [Google Scholar] [CrossRef]
- Miguel, M.; Oliveira, R.; Loureiro, N.; García-Rubio, J.; Ibáñez, S. Load measures in training/match monitoring in soccer: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 2721. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, R.; Francisco, R.; Fernandes, R.; Martins, A.; Nobari, H.; Clemente, F.M.; Brito, J.P. In-season body composition effects in professional women soccer players. Int. J. Environ. Res. Public Health 2021, 18, 12023. [Google Scholar] [CrossRef] [PubMed]
- Kotzamanidis, C.; Chatzopoulos, D.; Michailidis, C.; Papaiakovou, G.; Patikas, D. The effect of a combined high-intensity strength and speed training program on the running and jumping ability of soccer players. J. Strength Cond. Res. 2005, 19, 369–375. [Google Scholar] [CrossRef] [PubMed]



| Exercise | Period of Training at the Week | |||||||
|---|---|---|---|---|---|---|---|---|
| 1–2 Weeks | 3–4 Weeks | 5–6 Weeks | 7–8 Weeks | |||||
| Set | R/S | Set | R/S | Set | R/S | Set | R/S | |
| Bridge to plank (s) | 3 | 20 | 3 | 25 | 4 | 30 | 5 | 30 |
| 60-degree trunk flexion (s) | 3 | 20 | 3 | 25 | 4 | 30 | 5 | 30 |
| Scissor movement (R) | 3 | 10 | 3 | 15 | 4 | 15 | 5 | 15 |
| Working with resistance band a (R) | 3 | 10 | 3 | 15 | 4 | 15 | 5 | 15 |
| Movement by wall b (R) | 3 | 10 | 3 | 15 | 4 | 15 | 5 | 15 |
| Single leg squat | 3 | 10 | 3 | 15 | 4 | 15 | 5 | 15 |
| Standing on one foot (s) | 3 | 8 | 3 | 12 | 4 | 15 | 5 | 15 |
| Working with a wobble board c (S) | 3 | 8 | 3 | 12 | 4 | 15 | 5 | 15 |
| Squat Jump (R) | 3 | 8 | 3 | 12 | 4 | 15 | 5 | 15 |
| Tuck jump (R) | 3 | 8 | 3 | 12 | 4 | 15 | 5 | 15 |
| Longitudinal jump (R) | 3 | 8 | 3 | 12 | 4 | 15 | 5 | 15 |
| Lateral jump (R) | 3 | 8 | 3 | 12 | 4 | 15 | 5 | 15 |
| Weeks | Number of Hops | Type of Exercise | Set × Repetition |
|---|---|---|---|
| 1 | 70 | Side hop with two legs (hands-free) | 3 × 10 |
| Forward and backward hop (hands-free) | 2 × 10 | ||
| Forward hop with two legs (hands-free) | 2 × 10 | ||
| 2 | 90 | Side hop with two legs (hands-on chest) | 2 × 15 |
| Forward and backward hop (hands-free) | 2 × 10 | ||
| Forward hop with two legs (hands-free) | 2 × 10 | ||
| Side hop with one leg (hands-free) | 5 × 4 | ||
| 3 | 100 | Side hop with one leg (hands-on chest) | 3 × 10 |
| Forward and backward hop with one leg (hands-free) | 2 × 10 | ||
| Forward hop with two legs (hands-on chest) | 2 × 10 | ||
| Zigzag hop with two legs (hands-free) | 2 × 10 | ||
| 4 | 110 | Side hop with one leg (hands behind) | 2 × 10 |
| Forward and backward hop with one leg (hands-on chest) | 2 × 10 | ||
| Forward hop with on leg (hands-free) | 2 × 10 | ||
| Zigzag hop with one leg (hands-free) | 2 × 10 | ||
| Square hop with two legs (hands-free) | 2 × 10 | ||
| 5–6 | 120 | Side hop with one leg (hands behind) | 2 × 10 |
| Forward hop with on leg (hands behind) | 2 × 10 | ||
| Forward and backward hop with one leg (hands behind) | 2 × 10 | ||
| Zigzag hop with one leg (hands-on chest) | 2 × 10 | ||
| Square hop with one leg (hands-free) | 2 × 10 | ||
| Figure 8 hop with two legs (hands-free) | 2 × 10 | ||
| 7–8 | 130 | Side hop with one leg (hands behind) | 3 × 10 |
| Forward hop with on leg (hands behind) | 2 × 10 | ||
| Forward and backward hop with one leg (hands behind) | 2 × 10 | ||
| Zigzag hop with one leg (hands behind) | 2 × 10 | ||
| Square hop with one leg (hands-on chest) | 2 × 10 | ||
| Figure 8 hop with one leg (hands-free) | 2 × 10 |
| Variables | BSG (n = 12) | HG (n = 12) | CG (n = 12) | p-Value |
|---|---|---|---|---|
| Age [years] | 21.08 ± 1.78 | 20.83 ± 1.80 | 20.58 ± 1.37 | 0.76 |
| Body weight [kg] | 76.41 ± 9.21 | 75.41 ± 9.62 | 71.83 ± 7.60 | 0.42 |
| Body height [cm] | 177.58 ± 7.15 | 176.58 ± 5.59 | 178.58 ± 2.88 | 0.60 |
| BMI [kg·m−2] | 24.20 ± 0.71 | 24.18 ± 0.71 | 21.13 ± 0.13 | 0.15 |
| Dominant leg length [cm] | 100.41 ± 5.93 | 101.16 ± 3.95 | 98.50 ± 3.20 | 0.34 |
| Activity history [years] | 6.16 ± 2.62 | 6.08 ± 2.67 | 6.25 ± 2.37 | 0.98 |
| Groups | Pre Test (Mean ± SD) | Post Test (Mean ± SD) | Pre vs. Post Performance Change (%) | Pre vs. Post ES (CI, 95%) |
|---|---|---|---|---|
| Static balance Bass–stick (s) | ||||
| BSG | 9.33 ± 1.85 | 15.18 ± 2.64 c | ↑ 62.70 | 2.56 (1.50 to 3.63) *** |
| HG | 10.07 ± 2.24 | 11.22 ± 2.13 | ↑ 11.42 | 0.52 (−0.24 to 1.39) * |
| CG | 8.85 ± 1.57 | 8.97 ± 1.73 | ↑1.35 | 0.07 (−0.74 to 0.86) |
| Y balance–Anterior (cm) | ||||
| BSG | 82.35 ± 6.18 | 88.56 ± 5.21 | ↑ 7.54 | 1.08 (0.70 to 2.53) *** |
| HG | 82.41 ± 6.30 | 83.76 ± 5.64 | ↑ 1.63 | 0.22 (−0.57 to 1.03) * |
| CG | 78.20 ± 6.23 | 78.97 ± 3.11 | ↑ 0.98 | 0.09 (−0.65 to 0.96) |
| Y balance–Posteromedial (cm) | ||||
| BSG | 87.42 ± 6.63 | 95.71 ± 4.21 c | ↑ 9.48 | 1.49 (0.65 to 2.47) *** |
| HG | 86.59 ± 4.37 | 92.27 ± 4.67 a | ↑ 6.55 | 1.25 (0.15 to 1.84) *** |
| CG | 87.81 ± 2.78 | 88.63 ± 2.81 | ↑ 0.93 | 0.29 (−0.58 to 1.03) * |
| Y balance–Posterolateral (cm) | ||||
| BSG | 82.54 ± 4.33 | 89.69 ± 4.01 a | ↑ 8.66 | 1.71 (1.09 to 3.05) *** |
| HG | 80.69 ± 8.09 | 85.16 ± 6.20 a | ↑ 5.53 | 0.62 (−0.19 to 1.45) ** |
| CG | 78.19 ± 3.79 | 79.75 ± 5.46 | ↑ 1.99 | 0.33 (−0.49 to 1.12) * |
| Y balance–total (cm) | ||||
| BSG | 84.10 ± 3.19 | 91.32 ± 2.33 c | ↑ 8.58 | 2.58 (1.28 to 3.31) *** |
| HG | 83.23 ± 4.90 | 87.07 ± 4.23 a | ↑ 4.61 | 0.83 (0.18 to 1.87) ** |
| CG | 81.40 ± 1.33 | 82.45 ± 1.85 | ↑ 1.28 | 0.65 (−0.52 to 1.09) ** |
| Triple single leg hop (cm) | ||||
| BSG | 414.99 ± 8.40 | 434.98 ± 12.67 b | ↑ 1.28 | 1.85 (1.22 to 3.22) *** |
| HG | 419.63 ± 14.49 | 442.22 ± 13.56 b,d | ↑ 5.38 | 1.60 (1.03 to 2.97) *** |
| CG | 409.44 ± 15.31 | 418.15 ± 18.95 | ↑ 2.12 | 0.50 (−0.33 to 1.33) * |
| Figure 8 hop (s) | ||||
| BSG | 9.00 ± 0.89 | 7.64 ± 0.34 b,d | ↓ 15.11 | 2.01 (−0.93 to 0.68) *** |
| HG | 9.11 ± 1.11 | 7.03 ± 0.61 c,f | ↓ 22.83 | 2.32 (7−3.82 to–1.63) *** |
| CG | 9.76 ± 0.70 | 8.88 ± 1.02 | ↓ 9.01 | 1 (−1.66 to–0.79) *** |
| Vertical jump (cm) | ||||
| BSG | 21.55 ± 2.21 | 25.46 ± 1.93 b,d,h | ↑ 18.14 | 1.88 (1.61 to 3.78) *** |
| HG | 22.57 ± 1.40 | 28.89 ± 1.71 c,f | ↑ 28.00 | 4.04 (2.01 to 4.38) *** |
| CG | 21.04 ± 3.22 | 22.19 ± 3.20 | ↑ 5.46 | 0.35 (−0.34 to 1.28) * |
| FAAM | ||||
| BSG | 76.16 ± 3.35 | 82.33 ± 3.89 a,d | ↑ 8.10 | 1.69 (0.80 to 2.66) *** |
| HG | 76.25 ± 5.04 | 83.16 ± 3.88 b | ↑ 9.06 | 1.53 (0.95 to 2.86) *** |
| CG | 75.41 ± 4.05 | 77.16 ± 3.48 | ↑ 2.32 | 0.46 (−0.40 to 1.21) * |
| FAAMSPORT | ||||
| BSG | 64.16 ± 1.52 | 70.00 ± 16.51 c,d,i | ↑ 9.10 | 0.49 (−0.33 to 1.30) * |
| HG | 65.25 ± 2.34 | 72.00 ± 8.59 c | ↑ 10.34 | 1.07 (0.24 to 1.95) *** |
| CG | 65.58 ± 2.06 | 67.00 ± 4.60 | ↑ 2.16 | 0.39 (−0.42 to 1.20) * |
| Groups | Pre Test (Mean ± SD) | Post Test (Mean ± SD) | Pre vs. Post Performance Change (%) | Pre vs. Post ES (95% CI) |
|---|---|---|---|---|
| Hip abduction (Kg) | ||||
| BSG | 11.75 ± 1.74 | 14.79 ± 0.82 c,j,f | ↑ 25.87 | 2.23 (0.98 to 2.90) *** |
| HG | 12.57 ± 1.87 | 13.58 ± 1.99 | ↑ 8.03 | 0.52 (−0.27 to 1.35) * |
| CG | 11.73 ± 1.03 | 11.91 ± 0.97 | ↑ 1.53 | 0.17 (−0.68 to 0.92) |
| Hip adduction (Kg) | ||||
| BSG | 10.51 ± 1.25 | 13.19 ± 1.36 c,j,f | ↑ 25.49 | 2.05 (1.22 to 3.23) *** |
| HG | 10.46 ± 1.66 | 12.14 ± 1.02 b | ↑ 16.06 | 1.21 (0.58 to 2.37) *** |
| CG | 10.67 ± 0.93 | 10.83 ± 0.88 | ↑ 1.49 | 0.17 (−0.68 to 0.92) |
| Knee flexion (Kg) | ||||
| BSG | 11.49 ± 0.72 | 13.56 ± 0.82 c,j,f | ↑ 18.01 | 2.68 (1.32 to 3.37) *** |
| HG | 11.79 ± 1.27 | 13.61 ± 1.43 c,f | ↑ 15.43 | 1.34 (0.69 to 2.52) *** |
| CG | 11.36 ± 0.77 | 11.58 ± 0.76 | ↑ 1.93 | 0.28 (−0.59 to 1.01) * |
| Knee extension (Kg) | ||||
| BSG | 11.82 ± 1.56 | 12.56 ± 1.42 d | ↑ 6.26 | 2.50 (−0.17 to 1.47) *** |
| HG | 11.45 ± 1.55 | 13.58 ± 0.91 c,f | ↑ 21.57 | 1.67 (0.75 to 2.59) *** |
| CG | 11.17 ± 0.79 | 11.38 ± 0.38 | ↑ 1.88 | 0.33 (−0.62 to 0.99) * |
| Ankle plantarflexion (Kg) | ||||
| BSG | 8.93 ± 1.07 | 11.30 ± 1.07 c,d,j | ↑ 26.53 | 2.21 (1.46 to 3.58) *** |
| HG | 9.24 ± 1.23 | 11.90 ± 1.23 c,f | ↑ 27.13 | 2.16 (1.29 to 3.33) *** |
| CG | 9.36 ± 0.79 | 9.66 ± 0.71 | ↑ 3.20 | 0.33 (−0.51 to 1.10) * |
| Ankle dorsiflexion (Kg) | ||||
| BSG | 8.20 ± 0.73 | 10.91 ± 1.18 c,d | ↑ 33.04 | 2.76 (10.91 to 8.2) *** |
| HG | 8.71 ± 0.73 | 11.41 ± 1.28 c,f | ↑ 24.69 | 2.59 (11.41 to 8.71) *** |
| CG | 9.15 ± 0.68 | 9.42 ± 0.66 | ↑ 2.95 | 0.40 (9.42 to 9.15) * |
| Ankle eversion (Kg) | ||||
| BSG | 4.69 ± 0.47 | 6.09 ± 0.72 c,f | ↑ 29.85 | 2.30 (0.91 to 2.80) *** |
| HG | 4.95 ± 0.52 | 5.48 ± 0.71 | ↑ 10.70 | 0.85 (0.04 to 1.72) ** |
| CG | 4.70 ± 0.48 | 4.87 ± 0.51 | ↑ 3.61 | 0.34 (−0.53 to 1.08) * |
| Ankle inversion (Kg) | ||||
| BSG | 5.53 ± 0.54 | 7.45 ± 0.51 c,f,h | ↑ 34.71 | 3.65 (2.55 to 5.20) *** |
| HG | 5.32 ± 0.74 | 6.49 ± 0.75 c,d | ↑ 21.99 | 1.57 (0.85 to 2.73) *** |
| CG | 5.52 ± 0.63 | 5.69 ± 0.72 | ↑ 3.07 | 0.25 (−0.57 to 1.04) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohammadi Nia Samakosh, H.; Brito, J.P.; Shojaedin, S.S.; Hadadnezhad, M.; Oliveira, R. What Does Provide Better Effects on Balance, Strength, and Lower Extremity Muscle Function in Professional Male Soccer Players with Chronic Ankle Instability? Hopping or a Balance Plus Strength Intervention? A Randomized Control Study. Healthcare 2022, 10, 1822. https://doi.org/10.3390/healthcare10101822
Mohammadi Nia Samakosh H, Brito JP, Shojaedin SS, Hadadnezhad M, Oliveira R. What Does Provide Better Effects on Balance, Strength, and Lower Extremity Muscle Function in Professional Male Soccer Players with Chronic Ankle Instability? Hopping or a Balance Plus Strength Intervention? A Randomized Control Study. Healthcare. 2022; 10(10):1822. https://doi.org/10.3390/healthcare10101822
Chicago/Turabian StyleMohammadi Nia Samakosh, Hadi, João Paulo Brito, Seyed Sadredin Shojaedin, Malihe Hadadnezhad, and Rafael Oliveira. 2022. "What Does Provide Better Effects on Balance, Strength, and Lower Extremity Muscle Function in Professional Male Soccer Players with Chronic Ankle Instability? Hopping or a Balance Plus Strength Intervention? A Randomized Control Study" Healthcare 10, no. 10: 1822. https://doi.org/10.3390/healthcare10101822
APA StyleMohammadi Nia Samakosh, H., Brito, J. P., Shojaedin, S. S., Hadadnezhad, M., & Oliveira, R. (2022). What Does Provide Better Effects on Balance, Strength, and Lower Extremity Muscle Function in Professional Male Soccer Players with Chronic Ankle Instability? Hopping or a Balance Plus Strength Intervention? A Randomized Control Study. Healthcare, 10(10), 1822. https://doi.org/10.3390/healthcare10101822