Deriving Meaning from Chaos: The Mediating Role of the Sense of Coherence in the Serial Relationships among Fear of COVID-19, Indices of Psychological Distress, and Life Satisfaction
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
2.3. Procedure
2.4. Ethics
2.5. Data Analysis
3. Results
- Comprehensibility mediated the association between the fear of COVID-19 and hopelessness (β = 0.041, p < 0.001, 95% CI [0.01, 0.05]).
- Manageability mediated the association between the fear of COVID-19 and hopelessness (β = 0.039, p = 0.007, 95% CI [0.01, 0.05]).
- Meaningfulness mediated the association between the fear of COVID-19 and hopelessness (β = 0.040, p = 0.005, 96% CI [0.01, 0.05]).
- Comprehensibility mediated the association between the fear of COVID-19 and anxiety (β = 0.058, p < 0.001, 95% CI [0.04, 0.13]).
- Manageability mediated the association between the fear of COVID-19 and anxiety (β = 0.055, p < 0.001, 95% CI [0.04, 0.12]).
- Meaningfulness mediated the association between the fear of COVID-19 and anxiety (β = 0.029, p = 0.005, 95% CI [0.01, 0.07]).
- Comprehensibility mediated the association between the fear of COVID-19 and hopelessness, which in turn was associated with higher levels of life satisfaction (β = 0.041, p < 0.001, 95% CI [−0.04, −0.01]).
- Manageability mediated the association between the fear of COVID-19 and hopelessness, which in turn was associated with higher levels of life satisfaction (β = 0.039, p = 0.006, 95% CI [−0.03, −0.01]).
- Meaningfulness mediated the association between the fear of COVID-19 and hopelessness, which in turn was associated with higher levels of life satisfaction (β = 0.040, p = 0.005, 95% CI [−0.03, −0.01]).
- Comprehensibility mediated the association between the fear of COVID-19 and anxiety, which in turn was associated with higher levels of life satisfaction (β = 0.058, p = 0.002, 95% CI [−0.02, −0.004]).
- Manageability mediated the association between the fear of COVID-19 and anxiety, which in turn was associated with higher levels of life satisfaction (β = 0.055, p = 0.002, 95% CI [−0.02, −0.003]).
- Meaningfulness mediated the association between the fear of COVID-19 and anxiety, which in turn was associated with higher levels of life satisfaction (β = 0.029, p = 0.004, 95% CI [−0.01, −0.001]).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wirkner, J.; Christiansen, H.; Knaevelsrud, C.; Lüken, U.; Wurm, S.; Schneider, S.; Brakemeier, E.-L. Mental Health in Times of the COVID-19 Pandemic. Eur. Psychol. 2021, 26, 310–322. [Google Scholar] [CrossRef]
- Kumar, A.; Nayar, K.R. COVID 19 and its mental health consequences. J. Ment. Health 2021, 30, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Dymecka, J.; Gerymski, R.; Machnik-Czerwik, A. How does stress affect life satisfaction during the COVID-19 pandemic? Moderated mediation analysis of sense of coherence and fear of coronavirus. Psychol. Health Med. 2022, 27, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Daly, M.; Robinson, E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J. Psychiatr. Res. 2021, 136, 603–609. [Google Scholar] [CrossRef] [PubMed]
- Padmanabhanunni, A.; Pretorius, T.B. When coping resources fail: The health-sustaining and moderating role of fortitude in the relationship between COVID-19-related worries and psychological distress. Afr. Saf. Promot. 2020, 18, 28–47. [Google Scholar]
- García-Fernández, L.; Romero-Ferreiro, V.; López-Roldán, P.D.; Padilla, S.; Calero-Sierra, I.; Monzó-García, M.; Pérez-Martín, J.; Rodriguez-Jimenez, R. Mental health impact of COVID-19 pandemic on Spanish healthcare workers. Psychol. Med. 2020, 52, 195–197. [Google Scholar] [CrossRef]
- Baker, C.N.; Peele, H.; Daniels, M.; Saybe, M.; Whalen, K.; Overstreet, S. Trauma-Informed Schools Learning Collaborative The New Orleans The experience of COVID-19 and its impact on teachers’ mental health, coping, and teaching. School Psych. Rev. 2021, 50, 491–504. [Google Scholar] [CrossRef]
- Barni, D.; Danioni, F.; Canzi, E.; Ferrari, L.; Ranieri, S.; Lanz, M.; Iafrate, R.; Regalia, C.; Rosnati, R. Facing the COVID-19 Pandemic: The Role of Sense of Coherence. Front. Psychol. 2020, 11, 578440. [Google Scholar] [CrossRef]
- Super, S.; Pijpker, R.; Polhuis, K. The relationship between individual, social and national coping resources and mental health during the COVID-19 pandemic in the Netherlands. Health Psychol. Rep. 2021, 9, 186–192. [Google Scholar] [CrossRef]
- Antonovsky, A. The salutogenic model as a theory to guide health promotion. Health Promot. Int. 1996, 11, 11–18. [Google Scholar] [CrossRef]
- Antonovsky, A. Unraveling the Mystery of Health: How People Manage Stress and Stay Well; Jossey-Bass: San Francisco, CA, USA, 1987. [Google Scholar]
- Schäfer, S.K.; Becker, N.; King, L.; Horsch, A.; Michael, T. The relationship between sense of coherence and post-traumatic stress: A meta-analysis. Eur. J. Psychotraumatology 2019, 10, 1562839. [Google Scholar] [CrossRef] [PubMed]
- Veronese, G.; Dhaouadi, Y.; Afana, A. Rethinking sense of coherence: Perceptions of comprehensibility, manageability, and meaningfulness in a group of Palestinian health care providers operating in the West Bank and Israel. Transcult Psychiatry 2021, 58, 38–51. [Google Scholar] [CrossRef]
- Braun-Lewensohn, O. Coping Resources and Stress Reactions Among Three Cultural Groups One Year After a Natural Disaster. Clin. Soc. Work J. 2013, 42, 366–374. [Google Scholar] [CrossRef]
- Mana, A.; Bauer, G.F.; Meier Magistretti, C.; Sardu, C.; Juvinyà-Canal, D.; Hardy, L.J.; Catz, O.; Tušl, M.; Sagy, S. Order out of chaos: Sense of coherence and the mediating role of coping resources in explaining mental health during COVID-19 in 7 countries. SSM Ment. Health 2021, 1, 100001. [Google Scholar] [CrossRef]
- Schäfer, S.K.; Sopp, M.R.; Schanz, C.G.; Staginnus, M.; Göritz, A.S.; Michael, T. Impact of COVID-19 on public mental health and the buffering effect of a sense of coherence. Psychother. Psychosom. 2020, 89, 386–392. [Google Scholar] [CrossRef]
- Sterne, M. The True State of South Africa’s Schools. Mail and Guardian. 3 October 2021. Available online: https://mg.co.za/education/2021-10-03-the-true-state-of-our-schools/ (accessed on 15 July 2022).
- OECD. Results from Talis 2019; 2019. Available online: https://www.oecd.org/education/talis/ (accessed on 15 July 2022).
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The fear of COVID-19 scale: Development and initial validation. Int. J. Ment. Health Addict. 2020, 20, 1537–1545. [Google Scholar] [CrossRef] [Green Version]
- Spielberger, C.D. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1988. [Google Scholar]
- Beck, A.T.; Weissman, A.; Lester, D.; Trexler, L. The measurement of pessimism: The hopelessness scale. J. Consult. Clin. Psychol. 1974, 42, 861–865. [Google Scholar] [CrossRef] [PubMed]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The satisfaction with life scale. J. Pers. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Perz, C.A.; Lang, B.A.; Harrington, R. Validation of the Fear of COVID-19 Scale in a US College Sample. Int. J. Ment. Health Addict. 2020, 20, 273–283. [Google Scholar] [CrossRef]
- Pretorius, T.B.; Padmanabhanunni, A.; Stiegler, N.; Bouchard, J.P. Validation de l’Échelle de la Peur de la COVID-19 en Afrique du Sud: Trois analyses complémentaires. Ann. Med. Psychol. 2021, 179, 940–946. [Google Scholar] [CrossRef]
- Zsido, A.N.; Teleki, S.A.; Csokasi, K.; Rozsa, S.; Bandi, S.A. Development of the short version of the spielberger state—Trait anxiety inventory. Psychiatry Res. 2020, 291, 113223. [Google Scholar] [CrossRef]
- Pretorius, T.; Padmanabhanunni, A. A looming mental health pandemic in the time of COVID-19? Role of fortitude in the interrelationship between loneliness, anxiety, and life satisfaction among young adults. S. Afr. J. Psychol. 2021, 51, 256–268. [Google Scholar] [CrossRef]
- Alicia Edith, H.-d.-l.-T.; Cecilia, M.-S.; Fabiola, G.-B. Evidence for the Factorial Validity of the Beck Hopelessness Scale in Spanish with Clinical and non-Clinical Samples. Acta Colomb. Psicol. 2020, 23, 148. [Google Scholar] [CrossRef]
- Kocalevent, R.-D.; Finck, C.; Pérez-Trujillo, M.; Sautier, L.; Zill, J.; Hinz, A. Standardization of the Beck Hopelessness Scale in the general population. J. Ment. Health 2017, 26, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, M.; Mittelmark, M. The sense of coherence and its measurement. In The handbook of Salutogenesis; Mittelmark, M., Sagy, S., Bauer, G., Pelikan, J., Lindstrom, B., Espnes, G., Eds.; Springer Open: Cham, Switzerland, 2017; pp. 97–103. [Google Scholar]
- Yun, Y.H.; Rhee, Y.E.; Kang, E.; Sim, J.-A. The Satisfaction with Life Scale and the Subjective Well-Being Inventory in the General Korean Population: Psychometric Properties and Normative Data. Int. J. Environ. Res. Public Health 2019, 16, 1538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nooripour, R.; Hosseinian, S.; Ghanbari, N.; Haghighat, S.; Matacotta, J.J.; Gasparri, M.L. Validation of the Persian version of the satisfaction with life scale (SWLS) in Iranian women with breast Cancer. Curr. Psychol. 2021. [Google Scholar] [CrossRef]
- Pretorius, T.B.; Padmanabhanunni, A. Assessing the cognitive component of subjective well-being: Revisiting the satisfaction with life scale with classical test theory and item response theory. Afr. J. Psychol. Assess. 2022, 4, 9. [Google Scholar] [CrossRef]
- Martínez-Lorca, M.; Martínez-Lorca, A.; Criado-Álvarez, J.J.; Armesilla, M.D.C.; Latorre, J.M. The fear of COVID-19 scale: Validation in spanish university students. Psychiatry Res. 2020, 293, 113350. [Google Scholar] [CrossRef]
- Soraci, P.; Ferrari, A.; Abbiati, F.A.; Del Fante, E.; De Pace, R.; Urso, A.; Griffiths, M.D. Validation and Psychometric Evaluation of the Italian Version of the Fear of COVID-19 Scale. Int. J. Ment. Health Addict. 2020, 20, 1913–1922. [Google Scholar] [CrossRef]
- Winter, T.; Riordan, B.C.; Pakpour, A.H.; Griffiths, M.D.; Mason, A.; Poulgrain, J.W.; Scarf, D. Evaluation of the English version of the Fear of COVID-19 Scale and its relationship with behavior change and political beliefs. Int. J. Ment. Health Addict. 2020. [Google Scholar] [CrossRef]
- Yang, H.-J.; Ahn, J.-H.; Lee, J.; Lee, W.K.; Lee, J.; Kim, Y. Measuring Anxiety in Patients With Early-Stage Parkinson’s Disease: Rasch Analysis of the State-Trait Anxiety Inventory. Front. Neurol 2019, 10, 49. [Google Scholar] [CrossRef] [PubMed]
- Peracchia, S.; Presaghi, F.; Curcio, G. Pathologic Use of Video Games and Motivation: Can the Gaming Motivation Scale (GAMS) Predict Depression and Trait Anxiety? Int. J. Environ. Res. Public Health 2019, 16, 1008. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giner-Bartolome, C.; Mallorquí-Bagué, N.; Tolosa-Sola, I.; Steward, T.; Jimenez-Murcia, S.; Granero, R.; Fernandez-Aranda, F. Non-suicidal Self-Injury in Eating Disordered Patients: Associations with Heart Rate Variability and State-Trait Anxiety. Front. Psychol. 2017, 8, 1163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kliem, S.; Lohmann, A.; Mößle, T.; Brähler, E. Psychometric properties and measurement invariance of the Beck hopelessness scale (BHS): Results from a German representative population sample. BMC Psychiatry 2018, 18, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Yesilcinar, I.; Yanik, D.; Akbulut, S. Relationship between hopelessness and self-esteem of pregnant women: A cross-sectional study in South Eastern Turkey. Fresenius. Environ. Bull. 2020, 29, 3102–3109. [Google Scholar]
- İzci, F.; Erdogan, Z.İ.; İlgün, A.S.; Çelebi, E.; Alço, G.; Kocaman, N.; Ordu, Ç.; Öztürk, A.; Duymaz, T.; Pilavcı, K.N. Impact of personality traits, anxiety, depression and hopelessness levels on quality of life in the patients with breast cancer. Eur. J. Breast Health 2018, 14, 105. [Google Scholar] [CrossRef] [Green Version]
- Lorenzo-Seva, U.; Calderon, C.; Ferrando, P.J.; del Mar Muñoz, M.; Beato, C.; Ghanem, I.; Castelo, B.; Carmona-Bayonas, A.; Hernández, R.; Jiménez-Fonseca, P. Psychometric properties and factorial analysis of invariance of the satisfaction with life scale (SWLS) in cancer patients. Qual. Life Res. 2019, 28, 1255–1264. [Google Scholar] [CrossRef] [Green Version]
- Błażek, M.; Kaźmierczak, M.; Besta, T. Sense of Purpose in Life and Escape from Self as the Predictors of Quality of Life in Clinical Samples. J. Relig. Health 2015, 54, 517–523. [Google Scholar] [CrossRef] [Green Version]
- Ruiz, F.J.; Suárez-Falcón, J.C.; Flórez, C.L.; Odriozola-González, P.; Tovar, D.; López-González, S.; Baeza-Martín, R. Validity of the Satisfaction with Life Scale in Colombia and factorial equivalence with Spanish data. Rev. Latinoam Psicol. 2019, 51, 58–65. [Google Scholar] [CrossRef] [Green Version]
- Shoba, S. Lessons from Lockdown: South Africa’s Education System is Just Another Covid-19 Statistic. Daily Maverick. 18 July 2021. Available online: https://www.dailymaverick.co.za/article/2021-07-18-lessons-from-lockdown-south-africas-education-system-is-just-another-covid-19-statistic/ (accessed on 18 July 2022).
- Padmanabhanunni, A.; Pretorius, T. “I Teach, Therefore I Am”: The Serial Relationship between Perceived Vulnerability to Disease, Fear of COVID-19, Teacher Identification and Teacher Satisfaction. Int. J. Environ. Res. Public Health 2021, 18, 13243. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984. [Google Scholar]
- Kalisch, R.; Müller, M.B.; Tüscher, O. A conceptual framework for the neurobiological study of resilience. Behav. Brain Sci. 2015, 38, e92. [Google Scholar] [CrossRef] [PubMed]
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Fear of COVID-19 | — | ||||||
| 2. Anxiety | 0.33 *** | — | |||||
| 3. Hopelessness | 0.25 *** | 0.62 *** | — | ||||
| 4. Comprehensibility | −0.16 ** | −0.59 *** | −0.48 *** | — | |||
| 5. Manageability | −0.23 *** | −0.57 *** | −0.47 *** | 0.71 *** | — | ||
| 6. Meaningfulness | −0.14 ** | −0.45 *** | −0.45 *** | 0.43 *** | 0.42 *** | — | |
| 7. Life satisfaction | −0.11 * | −0.52 *** | −0.62 *** | 0.45 *** | 0.42 *** | 0.40 *** | — |
| Mean | 20.9 | 44.9 | 5.7 | 20.8 | 15.3 | 19.8 | 21.9 |
| SD | 7.1 | 10.3 | 4.9 | 5.4 | 4.4 | 4.1 | 7.3 |
| Alpha | 0.91 | 0.91 | 0.89 | 0.69 | 0.59 | 0.52 | 0.90 |
| Omega | 0.91 | 0.91 | 0.89 | 0.71 | 0.60 | 0.53 | 0.90 |
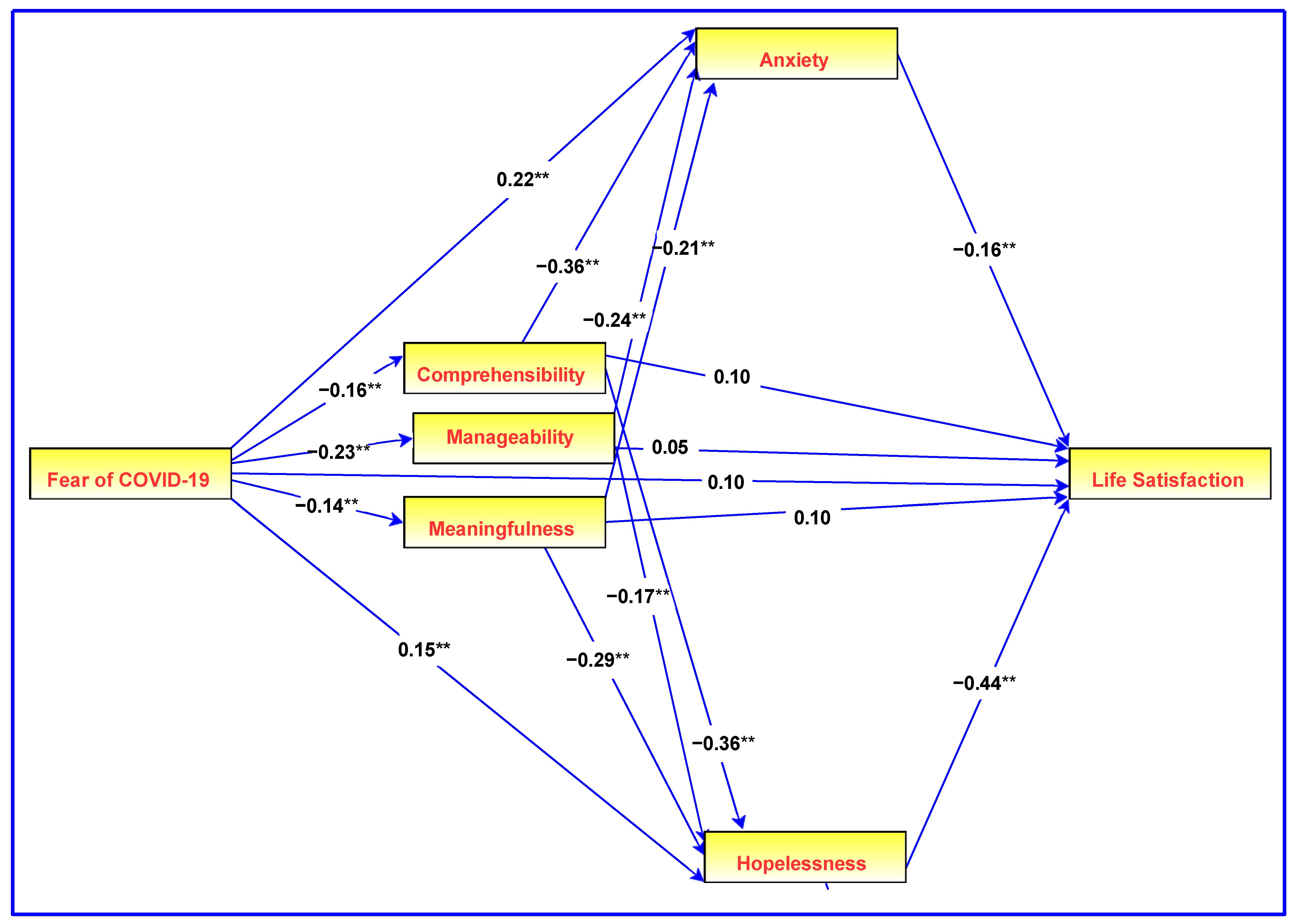
| Effect | Beta | SE | β | 95% CI | p |
|---|---|---|---|---|---|
| Fear of COVID-19 → Hopelessness | 0.097 | 0.032 | 0.150 | [0.070, 0.230] | 0.002 |
| Fear of COVID-19 → Anxiety | 0.289 | 0.062 | 0.220 | [0.148, 0.294] | 0.001 |
| Fear of COVID-19 → Meaningfulness | −0.079 | 0.029 | −0.137 | [−0.212, −0.048] | 0.009 |
| Fear of COVID-19 → Manageability | −0.144 | 0.032 | −0.231 | [−0.314, −0.147] | 0.001 |
| Fear of COVID-19 → Comprehensibility | −0.125 | 0.038 | −0.164 | [−0.248, −0.082] | 0.001 |
| Fear of COVID-19 → Life satisfaction | 0.090 | 0.051 | 0.096 | [0.005, 0.182] | 0.082 |
| Hopelessness → Life satisfaction | −0.640 | 0.082 | −0.439 | [−0.526, −0.345] | 0.001 |
| Anxiety → Life satisfaction | −0.113 | 0.045 | −0.157 | [−0.262, −0.052] | 0.006 |
| Meaningfulness → Hopelessness | −0.324 | 0.061 | −0.291 | [−0.378, −0.194] | 0.001 |
| Manageability → Hopelessness | −0.173 | 0.071 | −0.168 | [−0.279, −0.060] | 0.010 |
| Comprehensibility → Hopelessness | −0.211 | 0.055 | −0.249 | [−0.358, −0.141] | 0.001 |
| Meaningfulness → Anxiety | −0.474 | 0.111 | −0.209 | [−0.290, −0.129] | 0.001 |
| Manageability → Anxiety | −0.503 | 0.134 | −0.239 | [−0.344, −0.136] | 0.001 |
| Comprehensibility → Anxiety | −0.614 | 0.106 | −0.355 | [−0.452, −0.260] | 0.001 |
| Meaningfulness → Life satisfaction | 0.149 | 0.089 | 0.092 | [0.002, 0.183] | 0.092 |
| Manageability → Life satisfaction | 0.079 | 0.115 | 0.052 | [−0.069, 0.179] | 0.493 |
| Comprehensibility → Life satisfaction | 0.127 | 0.103 | 0.103 | [−0.034, 0.240] | 0.208 |
| Effect | Beta | SE | β | 95% CI | p |
|---|---|---|---|---|---|
| Fear of COVID-19 → Comprehensibility → Hopelessness 1 | 0.026 | 0.011 | 0.041 | [0.012, 0.050] | 0.000 |
| Fear of COVID-19 → Manageability → Hopelessness 2 | 0.025 | 0.012 | 0.039 | [0.009, 0.049] | 0.007 |
| Fear of COVID-19 → Meaningfulness → Hopelessness 3 | 0.026 | 0.011 | 0.040 | [0.010, 0.045] | 0.005 |
| Fear of COVID-19 → Comprehensibility → Anxiety 4 | 0.077 | 0.028 | 0.058 | [0.039, 0.134] | 0.000 |
| Fear of COVID-19 → Manageability → Anxiety 5 | 0.073 | 0.024 | 0.055 | [0.039, 0.123] | 0.000 |
| Fear of COVID-19 → Meaningfulness → Anxiety 6 | 0.038 | 0.017 | 0.029 | [0.014, 0.069] | 0.005 |
| Fear of COVID-19 → Comprehensibility → Hopelessness → Life satisfaction 7 | −0.017 | 0.008 | 0.041 | [−0.035, −0.007] | 0.000 |
| Fear of COVID-19 → Manageability → Hopelessness → Life satisfaction 8 | −0.016 | 0.008 | 0.039 | [−0.033, −0.006] | 0.006 |
| Fear of COVID-19 → Meaningfulness → Hopelessness → Life satisfaction 9 | −0.016 | 0.007 | 0.040 | [−0.031, −0.006] | 0.005 |
| Fear of COVID-19 → Comprehensibility → Anxiety → Life satisfaction 10 | −0.009 | 0.004 | 0.058 | [−0.021, −0.004] | 0.002 |
| Fear of COVID-19 → Manageability → Anxiety → Life satisfaction 11 | −0.008 | 0.005 | 0.055 | [−0.019, −0.003] | 0.002 |
| Fear of COVID-19 → Meaningfulness → Anxiety → Life satisfaction 12 | −0.004 | 0.003 | 0.029 | [−0.010, −0.001] | 0.004 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pretorius, T.B.; Padmanabhanunni, A. Deriving Meaning from Chaos: The Mediating Role of the Sense of Coherence in the Serial Relationships among Fear of COVID-19, Indices of Psychological Distress, and Life Satisfaction. Healthcare 2022, 10, 2276. https://doi.org/10.3390/healthcare10112276
Pretorius TB, Padmanabhanunni A. Deriving Meaning from Chaos: The Mediating Role of the Sense of Coherence in the Serial Relationships among Fear of COVID-19, Indices of Psychological Distress, and Life Satisfaction. Healthcare. 2022; 10(11):2276. https://doi.org/10.3390/healthcare10112276
Chicago/Turabian StylePretorius, Tyrone B., and Anita Padmanabhanunni. 2022. "Deriving Meaning from Chaos: The Mediating Role of the Sense of Coherence in the Serial Relationships among Fear of COVID-19, Indices of Psychological Distress, and Life Satisfaction" Healthcare 10, no. 11: 2276. https://doi.org/10.3390/healthcare10112276





