Applying Discrete Event Simulation to Reduce Patient Wait Times and Crowding: The Case of a Specialist Outpatient Clinic with Dual Practice System
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Operational Characteristics and Patient Flow
2.2.1. Time-Motion Study (TMS)
- Observation 1 involved the recording of the time taken for public patient registration processes at the QMS counter, revenue counters, and O&G clinic counter over five working days. Due to fast processing times and multiple patients checking in concurrently at QMS and revenue counters, we randomly sampled patients at different time intervals during the TMS.
- Observation 2 involved the recording of the time taken for clinic processes for public and private patients at the O&G clinic counter, vital sign measurement station, laboratory, consultation rooms, and nurses’ station as well as registration and appointment processes at the private patient counter over five working days. Patients’ medical record number was recorded at the O&G clinic counter.
2.2.2. Time Required for Case Review and Management
2.3. Data Management
2.4. Simulation
2.4.1. Model Validation
2.4.2. Simulation Experiment with Scenarios
2.5. Statistical Analysis
3. Results
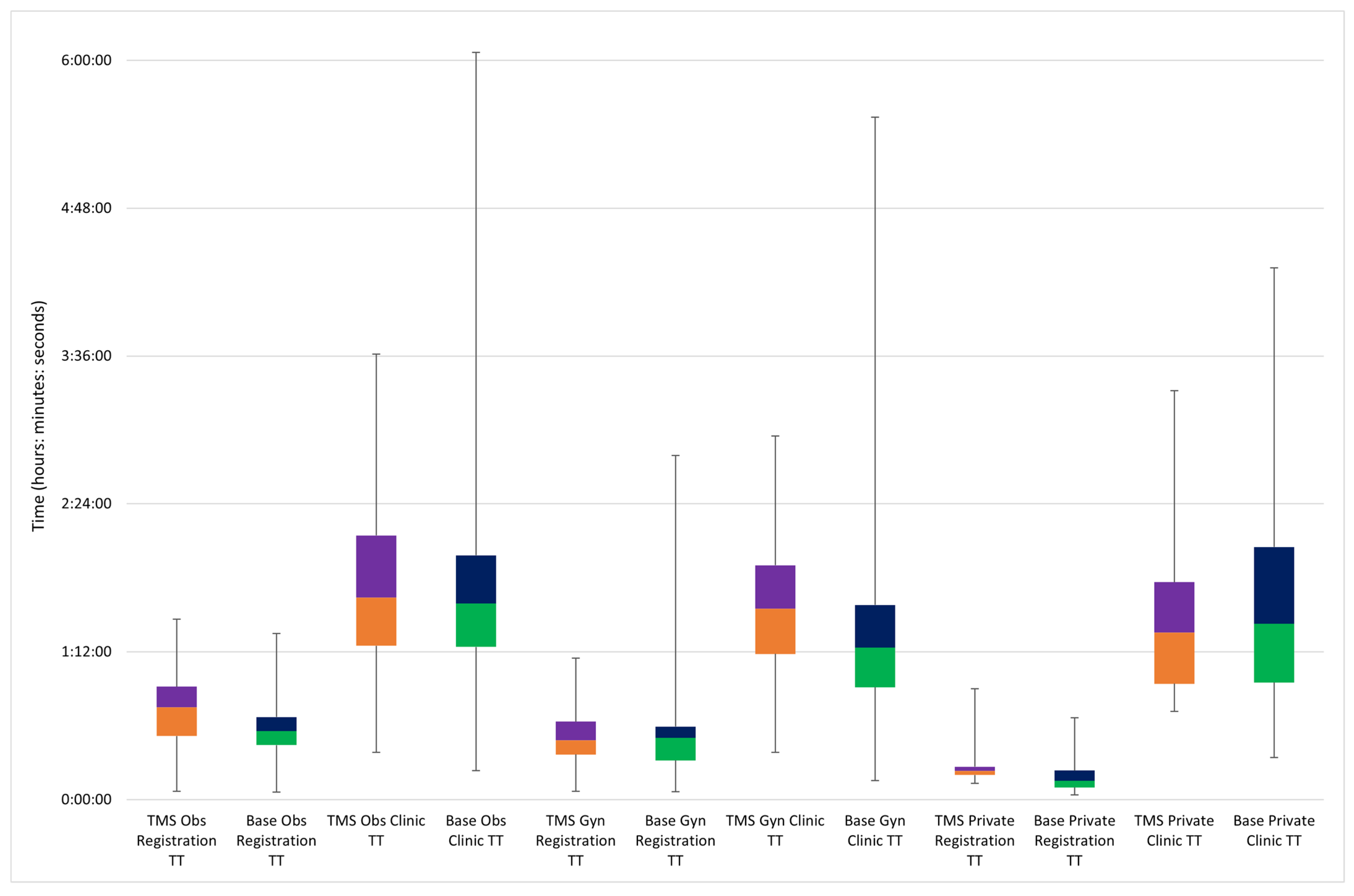
3.1. TMS Process Times and Turnaround Times
3.2. Model Validation
3.3. Effects of Scenarios on Overall TT and Number of Patients Waiting at the Clinic
4. Discussion
Implications for Research, Policy, and Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rannan-Eliya, R.P.; Anuranga, C.; Manual, A.; Sararaks, S.; Jailani, A.S.; Hamid, A.J.; Razif, I.M.; Tan, E.H.; Darzi, A. Improving Health Care Coverage, Equity, And Financial Protection Through A Hybrid System: Malaysia’s Experience. Health Aff. 2016, 35, 838–846. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health Malaysia. Guidelines for Implementation of Fee Order (Medical) (Full Paying Patient) 2007; Ministry of Health Malaysia: Putrajaya, Malaysia, 2015. [Google Scholar]
- Ferrinho, P.; Van Lerberghe, W.; Fronteira, I.; Hipólito, F.; Biscaia, A. Dual practice in the health sector: Review of the evidence. Hum. Resour. Health 2004, 2, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hipgrave, D.B.; Hort, K. Dual practice by doctors working in South and East Asia: A review of its origins, scope and impact, and the options for regulation. Health Policy Plan. 2014, 29, 703–716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McPake, B.; Russo, G.; Hipgrave, D.; Hort, K.; Campbell, J. Implications of dual practice for universal health coverage. Bull. World Health Organ. 2016, 94, 142–146. [Google Scholar] [CrossRef]
- Socha, K.Z.; Bech, M. Physician dual practice: A review of literature. Health Policy 2011, 102, 1–7. [Google Scholar] [CrossRef]
- Domenighetti, G.; Vineis, P.; De Pietro, C.; Tomada, A. Ability to pay and equity in access to Italian and British National Health Services. Eur. J. Public Health 2010, 20, 500–503. [Google Scholar] [CrossRef] [Green Version]
- Rifat, A.; Berman, P.; Hsiao, W.; Myers, E.; Yap, W.A. Malaysia Health Systems Research Volume 1 Contextual Analysis of the Malaysian Health System; Ministry of Health Malaysia: Putrajaya, Malaysia; Harvard T.H. Chan School of Public Health: Boston, MA, USA, 2016. [Google Scholar]
- Institute for Health Systems Research (IHSR). National Health and Morbidity Survey (NHMS) 2019: Volume II: Healthcare Demand; Institute for Health Systems Research (IHSR), National Institutes of Health, Ministry of Health Malaysia: Shah Alam, Malaysia, 2020. [Google Scholar]
- Anderson, R.T.; Camacho, F.T.; Balkrishnan, R. Willing to wait?: The influence of patient wait time on satisfaction with primary care. BMC Health Serv. Res. 2007, 7, 31. [Google Scholar] [CrossRef] [Green Version]
- Johannessen, K.A.; Alexandersen, N. Improving accessibility for outpatients in specialist clinics: Reducing long waiting times and waiting lists with a simple analytic approach. BMC Health Serv. Res. 2018, 18, 827. [Google Scholar] [CrossRef]
- McIntyre, D.; Chow, C.K. Waiting Time as an Indicator for Health Services Under Strain: A Narrative Review. Inquiry 2020, 57, 46958020910305. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Lin, Q.; Zhao, P.; Zhang, Q.; Xu, K.; Chen, H.; Hu, C.J.; Stuntz, M.; Li, H.; Liu, Y. Reducing waiting time and raising outpatient satisfaction in a Chinese public tertiary general hospital-an interrupted time series study. BMC Public Health 2017, 17, 668. [Google Scholar] [CrossRef] [Green Version]
- Marshall, D.A.; Burgos-Liz, L.; IJzerman, M.J.; Osgood, N.D.; Padula, W.V.; Higashi, M.K.; Wong, P.K.; Pasupathy, K.S.; Crown, W. Applying dynamic simulation modeling methods in health care delivery research-the SIMULATE checklist: Report of the ISPOR simulation modeling emerging good practices task force. Value Health 2015, 18, 5–16. [Google Scholar] [CrossRef] [Green Version]
- Jacobson, S.H.; Hall, S.N.; Swisher, J.R. Discrete-Event Simulation of Health care Systems. In Patient Flow: Reducing Delay in Healthcare Delivery, 2nd ed.; Hall, R., Ed.; Springer: Boston, MA, USA, 2013; pp. 273–309. [Google Scholar]
- Bradley, B.D.; Jung, T.; Tandon-Verma, A.; Khoury, B.; Chan, T.C.Y.; Cheng, Y.-L. Operations research in global health: A scoping review with a focus on the themes of health equity and impact. Health Res. Policy Syst. 2017, 15, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, X. Application of discrete event simulation in health care: A systematic review. BMC Health Serv. Res. 2018, 18, 687. [Google Scholar] [CrossRef]
- Karnon, J.; Stahl, J.; Brennan, A.; Caro, J.J.; Mar, J.; Möller, J. Modeling using discrete event simulation: A report of the ISPOR-SMDM Modeling Good Research Practices Task Force–4. Med. Decis. Mak. 2012, 32, 701–711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Günal, M.M.; Pidd, M. Discrete event simulation for performance modelling in health care: A review of the literature. J. Simul. 2010, 4, 42–51. [Google Scholar] [CrossRef]
- Liu, S.; Li, Y.; Triantis, K.P.; Xue, H.; Wang, Y. The Diffusion of Discrete Event Simulation Approaches in Health Care Management in the Past Four Decades: A Comprehensive Review. MDM Policy Pract. 2020, 5, 2381468320915242. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Heng, B.H.; Teow, K.L. Analysis of Factors Causing Long Patient Waiting Time and Clinic Overtime in Outpatient Clinics. J. Med. Syst. 2012, 36, 707–713. [Google Scholar] [CrossRef]
- Griffin, J.; Xia, S.; Peng, S.; Keskinocak, P. Improving patient flow in an obstetric unit. Health Care Manag. Sci. 2012, 15, 1–14. [Google Scholar] [CrossRef]
- Young, N.; Taetgmeyer, M.; Zulaika, G.; Aol, G.; Desai, M.; Ter Kuile, F.; Langley, I. Integrating HIV, syphilis, malaria and anaemia point-of-care testing (POCT) for antenatal care at dispensaries in western Kenya: Discrete-event simulation modelling of operational impact. BMC Public Health 2019, 19, 1629. [Google Scholar] [CrossRef]
- Viana, J.; Simonsen, T.B.; Dahl, F.A.; Flo, K. A hybrid discrete event agent based overdue pregnancy outpatient clinic simulation model. In Proceedings of the 2018 Winter Simulation Conference, Gothenburg, Sweden, 9–12 December 2018; pp. 1488–1499. [Google Scholar]
- Mohiuddin, S.; Gardiner, R.; Crofts, M.; Muir, P.; Steer, J.; Turner, J.; Wheeler, H.; Hollingworth, W.; Horner, P.J. Modelling patient flows and resource use within a sexual health clinic through discrete event simulation to inform service redesign. BMJ Open 2020, 10, e037084. [Google Scholar] [CrossRef]
- Tellis, R.; Starobinets, O.; Prokle, M.; Raghavan, U.N.; Hall, C.; Chugh, T.; Koker, E.; Chaduvula, S.C.; Wald, C.; Flacke, S. Identifying Areas for Operational Improvement and Growth in IR Workflow Using Workflow Modeling, Simulation, and Optimization Techniques. J. Digit. Imaging 2020, 34, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Peres, I.T.; Hamacher, S.; Oliveira, F.L.C.; Barbosa, S.D.J.; Viegas, F. Simulation of Appointment Scheduling Policies: A Study in a Bariatric Clinic. Obes. Surg. 2019, 29, 2824–2830. [Google Scholar] [CrossRef]
- Douglas, J.M.; Jonathan, F.B.; Koenig, K.M. Designing and scheduling a multi-disciplinary integrated practice unit for patient-centred care. Health Syst. (Basingstoke) 2019, 9, 293–316. [Google Scholar] [CrossRef]
- Ahmadi-Javid, A.; Jalali, Z.; Klassen, K.J. Outpatient appointment systems in healthcare: A review of optimization studies. Eur. J. Oper. Res. 2017, 258, 3–34. [Google Scholar] [CrossRef]
- Cayirli, T.; Veral, E. Outpatient scheduling in health care: A review of literature. Prod. Oper. Manag. 2003, 12, 519–549. [Google Scholar] [CrossRef]
- Gupta, D.; Denton, B. Appointment scheduling in health care: Challenges and opportunities. IIE Trans. 2008, 40, 800–819. [Google Scholar] [CrossRef]
- Sun, Y.; Raghavan, U.N.; Vaze, V.; Hall, C.S.; Doyle, P.; Richard, S.S.; Wald, C. Stochastic programming for outpatient scheduling with flexible inpatient exam accommodation. Health Care Manag. Sci. 2021, 24, 460–481. [Google Scholar] [CrossRef] [PubMed]
- Viana, J.; Simonsen, T.B.; Faraas, H.E.; Schmidt, N.; Dahl, F.A.; Flo, K. Capacity and patient flow planning in post-term pregnancy outpatient clinics: A computer simulation modelling study. BMC Health Serv. Res. 2020, 20, 117. [Google Scholar] [CrossRef] [Green Version]
- Jin, X.; Sivakumar, A.; Lim, S. A simulation based analysis on reducing patient waiting time for consultation in an outpatient eye clinic. In Proceedings of the 2013 Winter Simulation Conference, Washington, DC, USA, 8–11 December 2013; pp. 2192–2203. [Google Scholar]
- Kern, C.; König, A.; Fu, D.J.; Schworm, B.; Wolf, A.; Priglinger, S.; Kortuem, K.U. Big data simulations for capacity improvement in a general ophthalmology clinic. Graefes Arch. Clin. Exp. Ophthalmol. 2021, 259, 1289–1296. [Google Scholar] [CrossRef]
- Pan, C.; Zhang, D.; Kon, A.W.; Wai, C.S.; Ang, W.B. Patient flow improvement for an ophthalmic specialist outpatient clinic with aid of discrete event simulation and design of experiment. Health Care Manag. Sci. 2015, 18, 137–155. [Google Scholar] [CrossRef]
- Vieira, B.; Demirtas, D.; van de Kamer, J.B.; Hans, E.W.; van Harten, W. Improving workflow control in radiotherapy using discrete-event simulation. BMC Med. Inform. Decis. Mak. 2019, 19, 199. [Google Scholar] [CrossRef] [Green Version]
- Lim, M.E.; Worster, A.; Goeree, R.; Tarride, J.-É. Simulating an emergency department: The importance of modeling the interactions between physicians and delegates in a discrete event simulation. BMC Med. Inform. Decis. Mak. 2013, 13, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fialho, A.S.; Oliveira, M.D.; Sá, A.B. Using discrete event simulation to compare the performance of family health unit and primary health care centre organizational models in Portugal. BMC Health Serv. Res. 2011, 11, 274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saidani, M.; Kim, H.; Kim, J. Designing optimal COVID-19 testing stations locally: A discrete event simulation model applied on a university campus. PLoS ONE 2021, 16, e0253869. [Google Scholar] [CrossRef]
- Monks, T.; Currie, C.S.M.; Onggo, B.S.; Robinson, S.; Kunc, M.; Taylor, S.J.E. Strengthening the reporting of empirical simulation studies: Introducing the STRESS guidelines. J. Simul. 2019, 13, 55–67. [Google Scholar] [CrossRef]
- Lenin, R.B.; Lowery, C.L.; Hitt, W.C.; Manning, N.A.; Lowery, P.; Eswaran, H. Optimizing appointment template and number of staff of an OB/GYN clinic–micro and macro simulation analyses. BMC Health Serv. Res. 2015, 15, 387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deo, S.; Topp, S.M.; Garcia, A.; Soldner, M.; Yagci Sokat, K.; Chipukuma, J.; Wamulume, C.S.; Reid, S.E.; Swann, J. Modeling the Impact of Integrating HIV and Outpatient Health Services on Patient Waiting Times in an Urban Health Clinic in Zambia. PLoS ONE 2012, 7, e35479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santibáñez, P.; Chow, V.S.; French, J.; Puterman, M.L.; Tyldesley, S. Reducing patient wait times and improving resource utilization at British Columbia Cancer Agency’s ambulatory care unit through simulation. Health Care Manag. Sci. 2009, 12, 392–407. [Google Scholar] [CrossRef]
- Rohleder, T.R.; Lewkonia, P.; Bischak, D.P.; Duffy, P.; Hendijani, R. Using simulation modeling to improve patient flow at an outpatient orthopedic clinic. Health Care Manag. Sci. 2011, 14, 135–145. [Google Scholar] [CrossRef]
- Morley, C.; Unwin, M.; Peterson, G.M.; Stankovich, J.; Kinsman, L. Emergency department crowding: A systematic review of causes, consequences and solutions. PLoS ONE 2018, 13, e0203316. [Google Scholar] [CrossRef]
- Bao, Y.; Fan, G.; Zou, D.; Wang, T.; Xue, D. Patient experience with outpatient encounters at public hospitals in Shanghai: Examining different aspects of physician services and implications of overcrowding. PLoS ONE 2017, 12, e0171684. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Kline, J.A.; Jackson, B.E.; Robinson, R.D.; Sullivan, M.; Holmes, M.; Watson, K.A.; Cowden, C.D.; Phillips, J.L.; Schrader, C.D.; et al. The role of patient perception of crowding in the determination of real-time patient satisfaction at Emergency Department. Int. J. Qual. Health Care 2017, 29, 722–727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Comas, M.; Castells, X.; Hoffmeister, L.; Román, R.; Cots, F.; Mar, J.; Gutiérrez-Moreno, S.; Espallargues, M. Discrete-event simulation applied to analysis of waiting lists. evaluation of a prioritization system for cataract surgery. Value Health 2008, 11, 1203–1213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abera, G.G.; Alemayehu, Y.K.; Herrin, J. Public-on-private dual practice among physicians in public hospitals of Tigray National Regional State, North Ethiopia: Perspectives of physicians, patients and managers. BMC Health Serv. Res. 2017, 17, 713. [Google Scholar] [CrossRef] [Green Version]
- Kiwanuka, S.N.; Rutebemberwa, E.; Nalwadda, C.; Okui, O.; Ssengooba, F.; Kinengyere, A.A.; Pariyo, G.W. Interventions to manage dual practice among health workers. Cochrane Database Syst. Rev. 2011, 7, CD008405. [Google Scholar] [CrossRef]



| Simulation | Arrival Pattern | QMS Registration Start Time | Consultation Start Time | Maximum Number of Public Patient Arrival in Every 30-min Slot | Last Public Patient Time Slot | Private Patients’ Start Time | Maximum Number of Private Patient Arrival in Every 30-min Slot |
|---|---|---|---|---|---|---|---|
| Base case | Random | TMS (7:00 a.m.) | TMS (~9:00 a.m.) | TMS (22) | ~12:00 p.m. | TMS (11:30 a.m.) | TMS (9) |
| Scenario 1 | Even | TMS (7:00 a.m.) | TMS (~9:00 a.m.) | TMS (22) | ~12:00 p.m. | TMS (11:30 a.m.) | TMS (9) |
| Scenario 2 | Even | TMS (7:00 a.m.) | 8:15 a.m. | TMS (22) | ~12:00 p.m. | TMS (11:30 a.m.) | TMS (9) |
| Scenario 3 | Even | 7:30 a.m. | 8:15 a.m. | 10 | 12:00 p.m. | 1:30 p.m. | 2 |
| Scenario 4 | Even | 7:30 a.m. | TMS (~9:00 a.m.) | 10 | 12:00 p.m. | 1:30 p.m. | 2 |
| Scenario 5 | Even | 8:00 a.m. | TMS (~9:00 a.m.) | 7 | 3:00 p.m. | TMS (11:30 a.m.) | TMS (9) |
| Scenario 6 | Even | 8:00 a.m. | TMS (~9:00 a.m.) | 10 | 12:30 p.m. | 1:30 p.m. | 2 |
| Scenario 7 | Even | 8:00 a.m. | TMS (~9:00 a.m.) | 10 | 12:30 p.m. | 11:00 a.m. | 2 |
| Median (Q1–Q3) Time (Hours: Min) | |||
|---|---|---|---|
| Observation 1 | Public (n = 338) | Private (n = 32) | |
| Obs (n = 191) | Gyn (n = 147) | ||
| Registration TT a, b | 00:45 (00:31–00:55) | 00:29 (00:22–00:38) | 00:14 (00:12–00:16) |
| Registration and payment b | - | - | 00:04 (00:02–00:07) |
| Observation 2 | Public (n = 357) | Private (n = 32) | |
| Obs (n = 180) | Gyn (n = 177) | ||
| Clinic TT a | 01:39 (01:15–02:08) | 01:33 (01:11–01:54) | 01:06 (00:43–01:33) |
| Vital sign measurement | 00:02 (00:01–00:03) | 00:02 (00:01–00:04) | 00:01 (00:01–00:01) |
| Laboratory c | 00:04 (00:03–00:06) | - | 00:03 (00:02–00:04) |
| Consultation d | 00:13 (00:10–00:20) | 00:10 (00:07–00:17) | 00:17 (00:13–00:21) |
| Appointment setting | 00:02 (00:01–00:04) | 00:02 (00:01–00:04) | 00:02 (00:01–00:05) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fun, W.H.; Tan, E.H.; Khalid, R.; Sararaks, S.; Tang, K.F.; Ab Rahim, I.; Md. Sharif, S.; Jawahir, S.; Sibert, R.M.Y.; Nawawi, M.K.M. Applying Discrete Event Simulation to Reduce Patient Wait Times and Crowding: The Case of a Specialist Outpatient Clinic with Dual Practice System. Healthcare 2022, 10, 189. https://doi.org/10.3390/healthcare10020189
Fun WH, Tan EH, Khalid R, Sararaks S, Tang KF, Ab Rahim I, Md. Sharif S, Jawahir S, Sibert RMY, Nawawi MKM. Applying Discrete Event Simulation to Reduce Patient Wait Times and Crowding: The Case of a Specialist Outpatient Clinic with Dual Practice System. Healthcare. 2022; 10(2):189. https://doi.org/10.3390/healthcare10020189
Chicago/Turabian StyleFun, Weng Hong, Ee Hong Tan, Ruzelan Khalid, Sondi Sararaks, Kar Foong Tang, Iqbal Ab Rahim, Shakirah Md. Sharif, Suhana Jawahir, Raoul Muhammad Yusof Sibert, and Mohd Kamal Mohd Nawawi. 2022. "Applying Discrete Event Simulation to Reduce Patient Wait Times and Crowding: The Case of a Specialist Outpatient Clinic with Dual Practice System" Healthcare 10, no. 2: 189. https://doi.org/10.3390/healthcare10020189
APA StyleFun, W. H., Tan, E. H., Khalid, R., Sararaks, S., Tang, K. F., Ab Rahim, I., Md. Sharif, S., Jawahir, S., Sibert, R. M. Y., & Nawawi, M. K. M. (2022). Applying Discrete Event Simulation to Reduce Patient Wait Times and Crowding: The Case of a Specialist Outpatient Clinic with Dual Practice System. Healthcare, 10(2), 189. https://doi.org/10.3390/healthcare10020189







