The Impact of Do-Not-Resuscitate Order in the Emergency Department on Respiratory Failure after ICU Admission
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Study Participants
2.3. Measurements
2.4. Data Analysis
2.5. Propensity Score Matching (PSM)
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

Appendix B
| With DNR n = 1536 | Without DNR n = 16532 | p-Value | |
|---|---|---|---|
| Age | 71.71 ± 14.6 | 66.45 ± 15.7 | < 0.001 |
| Male sex | 948(61.7) | 10,554(63.8) | 0.098 |
| Chronic ischemia heart disease | 168(10.9) | 2314(14.2) | < 0.001 |
| Cerebrovascular disease | 223(14.5) | 2487(15) | 0.581 |
| Chronic obstructive pulmonary disease | 247(16.1) | 3115(18.8) | 0.008 |
| Liver cirrhosis | 147(9.6) | 1756(10.6) | 0.199 |
| Chronic kidney disease | 339(22.1) | 3241(19.6) | 0.020 |
| Malignancy | 380(24.7) | 2220(13.4) | < 0.001 |
| Main diagnosis | < 0.001 | ||
| Disease of the respiratory system | 589(38.3) | 6078(36.8) | |
| Disease of the nervous system | 310(20.2)) | 1980(12.0) | |
| Disease of the circulatory system | 340(22.1) | 4536(27.4) | |
| Disease of the digestive system | 107(7.0) | 1697(10.3) | |
| Other metabolic problems | 190(12.4) | 2241(13.6) |
| Variable | OR | 95% CI of OR |
|---|---|---|
| Age | 1.0 | 1.02–1.03 |
| Male sex | 1.0 | 0.87–1.09 |
| Chronic ischemia heart disease | 0.7 | 0.63–0.88 |
| Cerebrovascular disease | 1.2 | 1.00–1.37 |
| Chronic obstructive pulmonary disease | 0.8 | 0.65–0.87 |
| Liver cirrhosis | 1.1 | 0.87–1.27 |
| Chronic kidney disease | 1.2 | 1.06–1.38 |
| Malignancy | 2.3 | 2.03–2.63 |
References
- Burns, J.P.; Truog, R.D. The DNR Order after 40 Years. N. Engl. J. Med. 2016, 375, 504–506. [Google Scholar] [CrossRef] [PubMed]
- Walsh, E.C.; Brovman, E.Y.; Bader, A.M.; Urman, R.D. Do-Not-Resuscitate Status Is Associated With Increased Mortality But Not Morbidity. Anesth. Analg. 2017, 125, 1484–1493. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.B.; Bunch O’Neill, L. Do not resuscitate does not mean do not treat: How palliative care and other modalities can help facilitate communication about goals of care in advanced illness. Mt. Sinai J. Med. 2008, 75, 460–465. [Google Scholar] [CrossRef] [PubMed]
- Baek, M.S.; Koh, Y.; Hong, S.-B.; Lim, C.-M.; Huh, J.W. Effect of Timing of Do-Not-Resuscitate Orders on the Clinical Outcome of Critically Ill Patients. Korean J. Crit. Care Med. 2016, 31, 229–235. [Google Scholar] [CrossRef]
- Patel, K.; Sinvani, L.; Patel, V.; Kozikowski, A.; Smilios, C.; Akerman, M.; Kiszko, K.; Maiti, S.; Hajizadeh, N.; Wolf-Klein, G.; et al. Do-Not-Resuscitate Orders in Older Adults During Hospitalization: A Propensity Score-Matched Analysis. J. Am. Geriatr. Soc. 2018, 66, 924–929. [Google Scholar] [CrossRef] [PubMed]
- Beach, M.C.; Morrison, R.S. The effect of do-not-resuscitate orders on physician decision-making. J. Am. Geriatr. Soc. 2002, 50, 2057–2061. [Google Scholar] [CrossRef] [PubMed]
- Bedell, S.E.; Pelle, D.; Maher, P.L.; Cleary, P.D. Do-not-resuscitate orders for critically ill patients in the hospital. How are they used and what is their impact? JAMA 1986, 256, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, L.; Anstey, M.; Feng, M.; Toledano, R.; Kogan, S.; Howell, M.D.; Clardy, P.; Celi, L.; Talmor, D.; Novack, V. Quantifying the Mortality Impact of Do-Not-Resuscitate Orders in the ICU. Crit. Care Med. 2017, 45, 1019–1027. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.T.; Chuang, Y.C.; Tsai, Y.J.; Ko, W.J.; Yu, C.J. High Mortality in Severe Sepsis and Septic Shock Patients with Do-Not-Resuscitate Orders in East Asia. PLoS ONE 2016, 11, e0159501. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, E.; Arai, J.; Kojima, S.; Norisue, Y.; Suzuki, T.; Homma, Y.; Takahashi, O.; Obunai, K.; Watanabe, H. Early DNR Order and Long-Term Prognosis Among Patients Hospitalized for Acute Heart Failure: Single-Center Cohort Study in Japan. Int. J. Gen. Med. 2020, 13, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.C.; Fang, Y.T.; Chen, H.C.; Lin, C.Y.; Chang, Y.P.; Chen, Y.M.; Huang, C.H.; Huang, K.T.; Chang, H.C.; Su, M.C.; et al. Effect of do-not-resuscitate orders on patients with sepsis in the medical intensive care unit: A retrospective, observational and propensity score-matched study in a tertiary referral hospital in Taiwan. BMJ Open 2019, 9, e029041. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Overbeck, M.C. Airway Management of Respiratory Failure. Emerg. Med. Clin. N. Am. 2016, 34, 97–127. [Google Scholar] [CrossRef] [PubMed]
- Cardenas, H.C.; Carson, R.T.; Hanemann, M.; Louviere, J.J.; Whittington, D. Who should get the scarce ICU bed? The US public’s view on triage in the time of COVID-19. Emerg. Med. J. 2022, 39, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Saha, D.; Moreno, C.; Csete, M.; Perez, E.K.; Cubeddu, L.; Farcy, D.; Henry, S.; Glazer, Z.; Moreno-Walton, L.A.; Goldszer, R.C. Outcomes of Patients Who Have Do Not Resuscitate Status prior to Being Admitted to an Intensive Care Unit. Scientifica 2016, 2016, 1513946. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shao, S.C.; Chan, Y.Y.; Kao Yang, Y.H.; Lin, S.J.; Hung, M.J.; Chien, R.N.; Lai, C.C.; Lai, E.C. The Chang Gung Research Database-A multi-institutional electronic medical records database for real-world epidemiological studies in Taiwan. Pharmacoepidemiol. Drug Saf. 2019, 28, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Krell, R.W.; Girotti, M.E.; Dimick, J.B. Extended length of stay after surgery: Complications, inefficient practice, or sick patients? JAMA Surg. 2014, 149, 815–820. [Google Scholar] [CrossRef] [Green Version]
- Li, C.J.; Law, Y.Y.; Lin, Y.R.; Chen, C.C.; Lin, X.H.; Chuang, P.C. Impact of Using a Non-Rebreathing Mask in Patients With Respiratory Failure. Am. J. Med. Sci. 2021, 361, 436–444. [Google Scholar] [CrossRef]
- Wenger, N.S.; Pearson, M.L.; Desmond, K.A.; Brook, R.H.; Kahn, K.L. Outcomes of patients with do-not-resuscitate orders. Toward an understanding of what do-not-resuscitate orders mean and how they affect patients. Arch. Intern. Med. 1995, 155, 2063–2068. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.L.; Sosnov, J.; Lessard, D.; Goldberg, R.J. Impact of do-not-resuscitation orders on quality of care performance measures in patients hospitalized with acute heart failure. Am. Heart J. 2008, 156, 78–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meert, A.P.; Wittnebel, S.; Holbrechts, S.; Toffart, A.C.; Lafitte, J.J.; Piagnerelli, M.; Lemaitre, F.; Peyrony, O.; Calvel, L.; Lemaitre, J.; et al. Critically ill cancer patient’s resuscitation: A Belgian/French societies’ consensus conference. Intensive Care Med. 2021, 47, 1063–1077. [Google Scholar] [CrossRef] [PubMed]


| With DNR n = 1510 | Without DNR n = 6040 | p-Value | |
|---|---|---|---|
| Age | 71.53 ± 14.6 | 71.71 ± 14.10 | 0.660 |
| Male sex | 930(61.6) | 3699(61.2) | 0.804 |
| Chronic ischemia heart disease | 168(11.1) | 626(10.4) | 0.388 |
| Cerebrovascular disease | 223(14.8) | 908(15) | 0.796 |
| Chronic obstructive pulmonary disease | 247(16.4) | 970(16.1) | 0.778 |
| Liver cirrhosis | 143(9.5) | 551(9.1) | 0.676 |
| Chronic kidney disease | 337(22.3) | 1285(21.3) | 0.377 |
| Malignancy | 354(23.4) | 1381(22.9) | 0.632 |
| Main diagnosis | 0.834 | ||
| Disease of the respiratory system | 581(38.5) | 2411(39.9) | |
| Disease of the nervous system | 293(19.4) | 1136(18.8) | |
| Disease of the circulatory system | 340(22.5) | 1353(22.4) | |
| Disease of the digestive system | 107(7.1) | 430(7.1) | |
| Other metabolic problems | 189(12.5) | 710(11.8) |
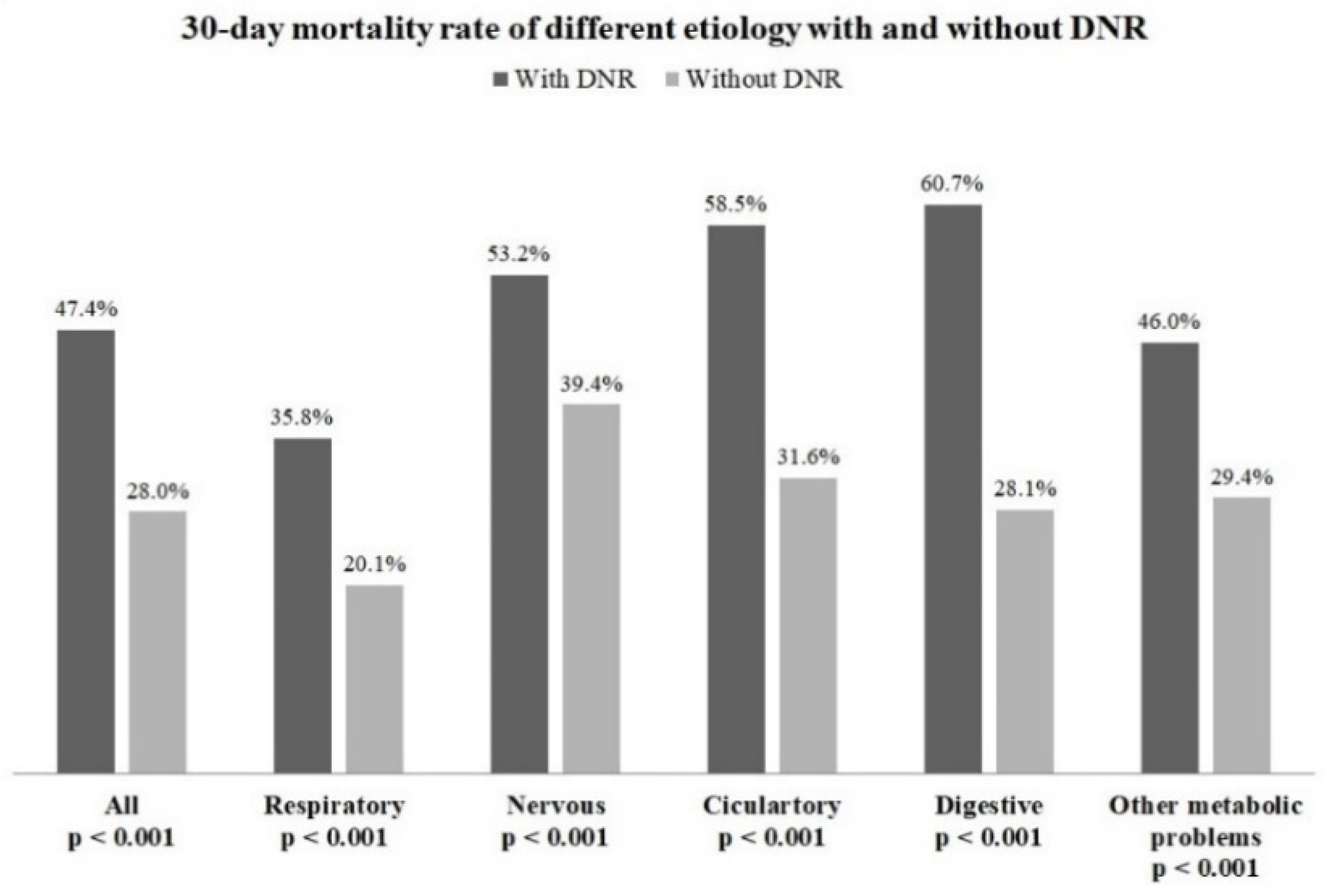
| Diagnosis | aHR | 95% CI of HR |
|---|---|---|
| All * | 1.9 | 1.70–2.03 |
| Disease of the respiratory system | 2.0 | 1.71–2.36 |
| Disease of the nervous system | 1.4 | 1.19–1.72 |
| Disease of the circulatory system | 2.0 | 1.68–2.36 |
| Disease of the digestive system | 2.7 | 2.00–3.69 |
| Other metabolic problems | 1.7 | 1.30–2.16 |
| Variable | HR | 95% CI of HR |
|---|---|---|
| Age | 1.0 | 0.99–1.00 |
| Male sex | 1.0 | 0.84–1.14 |
| Chronic ischemia heart disease | 1.2 | 0.96–1.60 |
| Cerebrovascular disease | 2.7 | 2.11–3.41 |
| Chronic obstructive pulmonary disease | 0.8 | 0.62–1.02 |
| Liver cirrhosis | 1.7 | 1.29–2.14 |
| Chronic kidney disease | 1.3 | 1.12–1.59 |
| Malignancy | 1.4 | 1.16–1.65 |
| Main diagnosis | ||
| Disease of the respiratory system | 1.0 | |
| Disease of the nervous system | 1.5 | 1.22–1.88 |
| Disease of the circulatory system | 1.3 | 0.10–1.65 |
| Disease of the digestive system | 1.4 | 1.03–1.95 |
| Other metabolic problems | 1.3 | 1.01–1.69 |
| Variable | OR | 95% CI of HR |
|---|---|---|
| Age | 1 | 0.999–1.009 |
| Male sex | 1.1 | 0.92–1.21 |
| Chronic ischemia heart disease | 0.7 | 0.59–0.95 |
| Cerebrovascular disease | 0.9 | 0.72–1.17 |
| Chronic obstructive pulmonary disease | 0.8 | 0.64–0.92 |
| Liver cirrhosis | 1 | 0.77–1.33 |
| Chronic kidney disease | 1.5 | 1.25–1.72 |
| Malignancy | 1.7 | 1.43–1.98 |
| Do-not-resuscitate | 1.2 | 1.02–1.44 |
| Main diagnosis | ||
| Disease of the respiratory system | 1 | |
| Disease of the nervous system | 1.4 | 1.15–1.66 |
| Disease of the circulatory system | 0.9 | 0.69–1.07 |
| Disease of the digestive system | 0.8 | 0.59–1.08 |
| Other metabolic problems | 0.8 | 0.67–1.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, T.-Y.; Wang, P.-M.; Chuang, P.-C.; Lin, Y.-R.; Syue, Y.-J.; Tsai, T.-C.; Li, C.-J. The Impact of Do-Not-Resuscitate Order in the Emergency Department on Respiratory Failure after ICU Admission. Healthcare 2022, 10, 434. https://doi.org/10.3390/healthcare10030434
Hsu T-Y, Wang P-M, Chuang P-C, Lin Y-R, Syue Y-J, Tsai T-C, Li C-J. The Impact of Do-Not-Resuscitate Order in the Emergency Department on Respiratory Failure after ICU Admission. Healthcare. 2022; 10(3):434. https://doi.org/10.3390/healthcare10030434
Chicago/Turabian StyleHsu, Ting-Yu, Pei-Ming Wang, Po-Chun Chuang, Yan-Ren Lin, Yuan-Jhen Syue, Tsung-Cheng Tsai, and Chao-Jui Li. 2022. "The Impact of Do-Not-Resuscitate Order in the Emergency Department on Respiratory Failure after ICU Admission" Healthcare 10, no. 3: 434. https://doi.org/10.3390/healthcare10030434






