Post-Work Recovery from Fatigue and Sleep Episodes among Nurses Who Are Engaged in 16-Hour Night Shifts: A Prospective Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Operational Terms
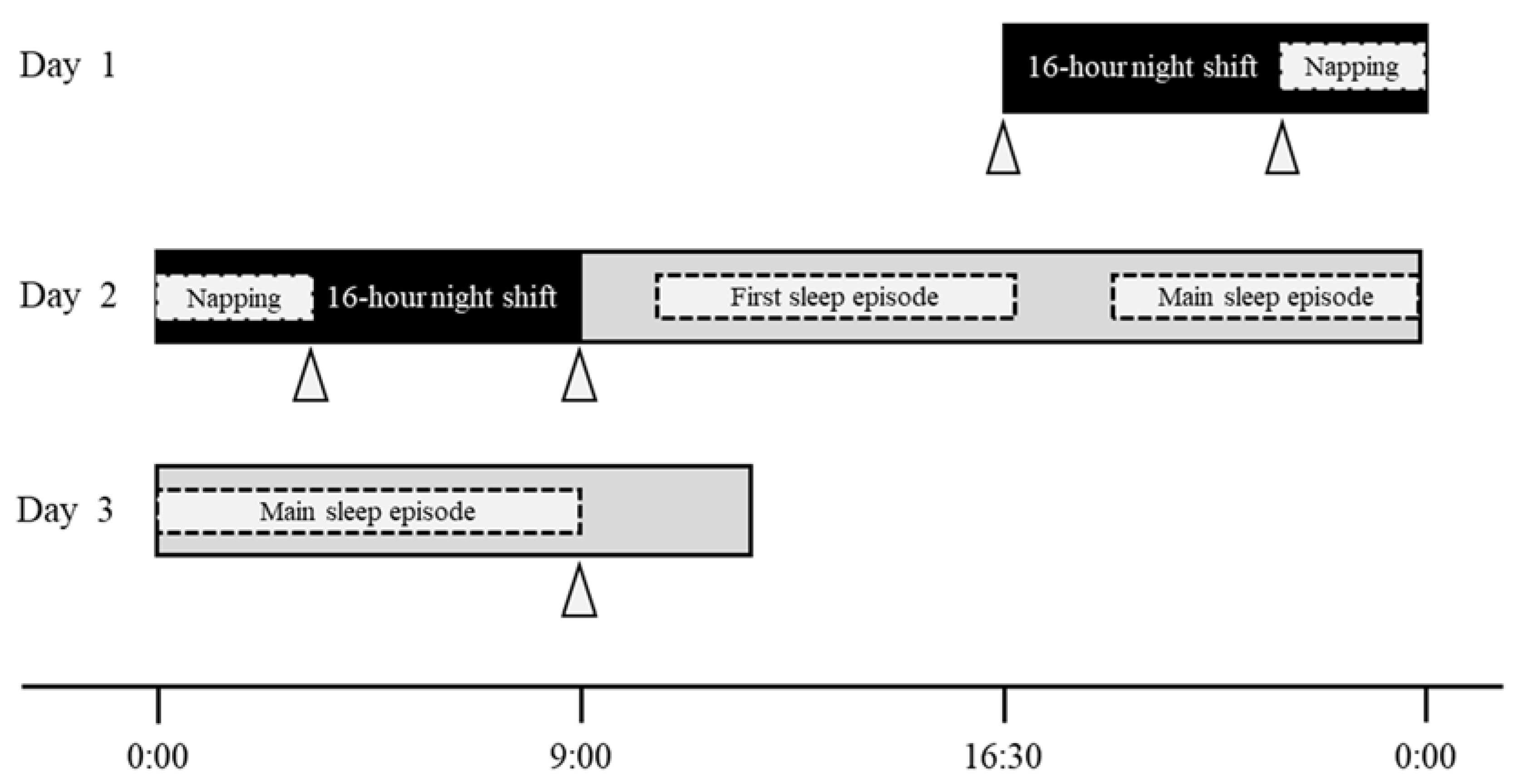
- 16 h night shift: a night shift from 16:30 to 09:00 the next day in a two-shift system (Figure 1).
- Night-shift napping: a short sleep taken during the night shift.
- First sleep episode: the first sleep episode after the night shift, excluding the main sleep episode.
- Main sleep episode: the longest sleep episode between the period after a night shift and the morning of the day after this shift.
2.2. Study Design and Participants
2.3. Outcome Measures
2.3.1. Demographic Data
2.3.2. Fatigue
2.3.3. Sleep and Napping
Activity/Sleep
Questionnaire for Night-Shift Napping and Sleep Diary for after the Night Shift
Analytical Methods for Sleeping and Napping Data
- (1)
- TIB (min): the time at which the posture involved lying.
- (2)
- Sleep latency (SL; min): the interval between changing posture from standing to lying and the start of the sleep episode.
- (3)
- Total sleep time (TST; min): using the start and end of TIB, we calculated the sum of the periods in which participants were judged to have fallen asleep.
- (4)
- Sleep efficiency (SE; %): percentage of TST for TIB.
- (5)
- Wake after sleep onset (WASO; min): the amount of time spent awake during the interval between sleep onset and offset.
- (6)
- Bed-out time (BOT; min): the interval between the last sleep onset and the change in posture from lying to standing.
2.3.4. Burnout
2.3.5. Resilience
2.3.6. Coping Profile
2.3.7. Work Engagement
2.4. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
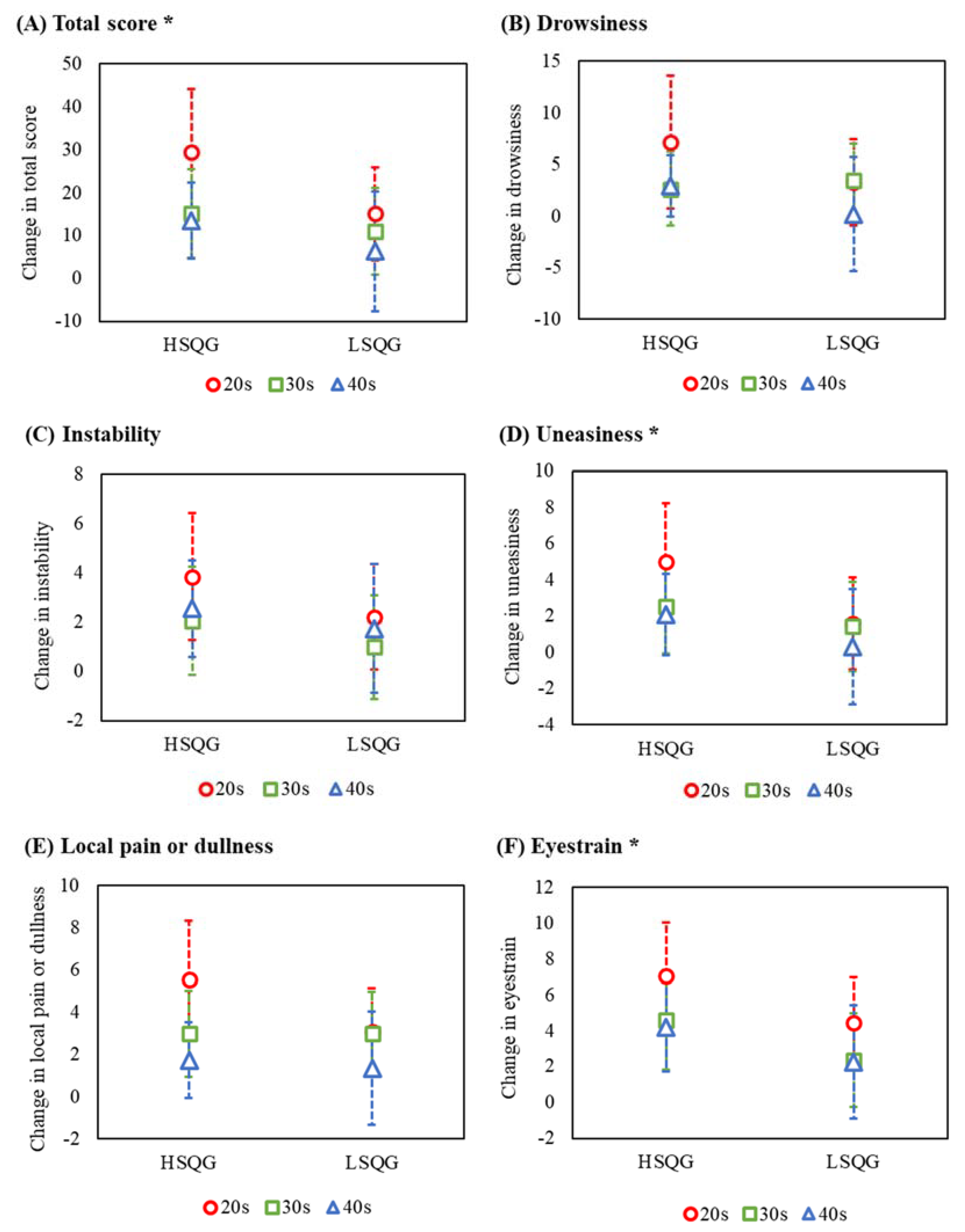
3.2. Fatigue by Age Group
3.3. Sleep Episodes and Napping by Age Group
3.4. Relationship between Post-Work Recovery from Fatigue, Sleep Episodes, and Age
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gifkins, J.; Johnston, A.; Loudoun, R.; Troth, A. Fatigue and recovery in shiftworking nurses: A scoping literature review. Int. J. Nurs. Stud. 2020, 112, 103710. [Google Scholar] [CrossRef] [PubMed]
- Fang, J.; Qiu, C.; Xu, H.; You, G. A model for predicting acute and chronic fatigue in Chinese nurses. J. Adv. Nurs. 2013, 69, 546–558. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Shao, Y.; Xing, Z.; Li, Y.; Wang, S.; Zhang, M.; Ying, J.; Shi, Y.; Sun, J. Napping on night-shifts among nursing staff: A mixed-methods systematic review. J. Adv. Nurs. 2019, 75, 291–312. [Google Scholar] [CrossRef] [PubMed]
- Querstret, D.; O’Brien, K.; Skene, D.J.; Maben, J. Improving fatigue risk management in healthcare: A scoping review of sleep-related/fatigue-management interventions for nurses and midwives (reprint). Int. J. Nurs. Stud. 2020, 112, 103745. [Google Scholar] [CrossRef] [PubMed]
- Sagherian, K.; Steege, L.M.; Cobb, S.J.; Cho, H. Insomnia, fatigue and psychosocial well-being during COVID-19 pandemic: A cross-sectional survey of hospital nursing staff in the United States. J. Clin. Nurs. 2020, in press. [Google Scholar] [CrossRef]
- Dall’Ora, C.; Ball, J.; Recio-Saucedo, A.; Griffiths, P. Characteristics of shift work and their impact on employee performance and wellbeing: A literature review. Int. J. Nurs. Stud. 2016, 57, 12–27. [Google Scholar] [CrossRef]
- Samaha, E.; Lal, S.; Samaha, N.; Wyndham, J. Psychological, lifestyle and coping contributors to chronic fatigue in shift-worker nurses. J. Adv. Nurs. 2007, 59, 221–232. [Google Scholar] [CrossRef]
- Winwood, P.C.; Winefield, A.H.; Lushington, K. Work-related fatigue and recovery: The contribution of age, domestic responsibilities and shiftwork. J. Adv. Nurs. 2006, 56, 438–449. [Google Scholar] [CrossRef]
- Japan Federation of Medical Workers’ Unions. Night Shift Survey Report 2020. (In Japanese). Available online: http://irouren.or.jp/research/324e9714869db7acc3f8b80e6c3206459a902144.pdf (accessed on 28 June 2021).
- Oriyama, S.; Miyakoshi, Y.; Rahman, M.M. The effects of a 120-minute nap on sleepiness, fatigue, and performance during 16-hour night shifts: A pilot study. J. Occup. Health 2019, 61, 368–377. [Google Scholar] [CrossRef]
- Ruggiero, J.S.; Redeker, N.S. Effects of napping on sleepiness and sleep-related performance deficits in night-shift workers: A systematic review. Biol. Res. Nurs. 2014, 16, 134–142. [Google Scholar] [CrossRef]
- Kagamiyama, H.; Sumi, N.; Yoshida, Y.; Sugimura, N.; Nemoto, F.; Yano, R. Association between sleep and fatigue in nurses who are engaged in 16 h night shifts in Japan: Assessment using actigraphy. Jpn. J. Nurs. Sci. 2019, 16, 373–384. [Google Scholar] [CrossRef] [PubMed]
- Silva-Costa, A.; Rotenberg, L.; Griep, R.H.; Fischer, F.M. Relationship between sleeping on the night shift and recovery from work among nursing workers—The influence of domestic work. J. Adv. Nurs. 2011, 67, 972–981. [Google Scholar] [CrossRef] [PubMed]
- Japanese Nursing Association. Guidelines on Night Shift and Shift Work for Nurses; Japanese Nursing Association: Tokyo, Japan, 2013; pp. 92–94. (In Japanese) [Google Scholar]
- Han, Y.; Lee, J.; Cho, H.H.; Kim, M.R. Sleep disorders and menopause. J. Menopausal Med. 2019, 25, 172. [Google Scholar] [CrossRef] [PubMed]
- Gava, G.; Orsili, I.; Alvisi, S.; Mancini, I.; Seracchioli, R.; Meriggiola, M.C. Cognition, mood and sleep in menopausal transition: The role of menopause hormone therapy. Medicina 2019, 55, 668. [Google Scholar] [CrossRef] [PubMed]
- Carrier, J.; Semba, K.; Deurveilher, S.; Drogos, L.; Cyr-Cronier, J.; Lord, C.; Sekerovick, Z. Sex differences in age-related changes in the sleep-wake cycle. Front. Neuroendocrinol. 2017, 47, 66–85. [Google Scholar] [CrossRef] [PubMed]
- Hollandera, L.E.; Freeman, E.W.; Sammela, M.D.; Berlina, J.A.; Grisso, J.A.; Battistini, M. Sleep quality, estradiol levels, and behavioral factors in late reproductive age women. Obstet. Gynecol. 2001, 98, 391–397. [Google Scholar] [CrossRef]
- Kravitz, H.M.; Janssen, I.; Santoro, N.; Bromberger, J.T.; Schocken, M.; Everson-Rose, S.A.; Karavolos, K.; Powell, L.H. Relationship of day-to-day reproductive hormone levels to sleep in midlife women. Arch. Intern. Med. 2005, 165, 2370–2376. [Google Scholar] [CrossRef]
- Kubo, T.; Tachi, N.; Takeyama, H.; Ebara, T.; Inoue, T.; Takanishi, T.; Arakomo, Y.; Murasaki, G.I.; Itani, T. Characteristic patterns of fatigue feelings on four simulated consecutive night shifts by “Jikaku-sho Shirabe”. Sangyo Eiseigaku Zasshi 2008, 50, 133–144. (In Japanese) [Google Scholar] [CrossRef]
- Matsuo, M.; Masuda, F.; Sumi, Y.; Takahashi, M.; Yamada, N.; Hasegawa-Ohira, M.; Fujiwara, K.; Kanemura, T.; Kadotani, H. Comparisons of portable sleep monitors of different modalities: Potential as naturalistic sleep recorders. Front. Neurol. 2016, 7, 110. [Google Scholar] [CrossRef]
- Nakazaki, K.; Kitamura, S.; Motomura, Y.; Hida, A.; Kamei, Y.; Miura, N.; Mishima, K. Validity of an algorithm for determining sleep/wake states using a new actigraph. J. Physiol. Anthropol. 2014, 33, 31. [Google Scholar] [CrossRef]
- Sumi, N.; Yoshida, Y.; Sugimura, N.; Yano, R. Investigation of the burnout stages experienced by nurses working in hospitals and related factors. Open J. Nurs. 2018, 8, 257–271. [Google Scholar] [CrossRef][Green Version]
- Kubo, M. The factorial and construct validity of the Japanese Burnout Scale among service workers. Shinrigaku Kenkyu 2014, 85, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Ihara, H.; Ogata, H.; Inuzuka, A.; Ohta, N.; Nagai, T.; Mizuno, M. Development and psychometric validation of the Resilience Scale for nurses. Jpn. J. Gen. Hosp. Psychiatry 2010, 22, 210–220. [Google Scholar] [CrossRef]
- Kageyama, T.; Kobayashi, T.; Kawashima, M.; Kanamaru, Y. Development of the Brief Scales for Coping Profile (BSCP) for Workers: Basic Information about its Reliability and Validity Takayuki. Sangyo Eiseigaku Zasshi 2004, 46, 103–114. (In Japanese) [Google Scholar] [CrossRef] [PubMed]
- Shimazu, A.; Schaufeli, W.B.; Kosugi, S.; Suzuki, A.; Nashiwa, H.; Kato, A.; Sakamoto, H.; Irimajiri, H.; Amano, S.; Hirohata, R.; et al. Work engagement in Japan: Validation of the Japanese version of the Utrecht work engagement scale. Appl. Psychol. 2008, 57, 510–523. [Google Scholar] [CrossRef]
- Brzozowski, S.L.; Cho, H.; Arsenault Knudsen, É.N.; Steege, L.M. Predicting nurse fatigue from measures of work demands. Appl. Ergon. 2021, 92, 103337. [Google Scholar] [CrossRef]
- Moser, D.K.; Lee, K.S.; Wu, J.R.; Mudd-Martin, G.; Jaarsma, T.; Huang, T.Y.; Fan, X.Z.; Strömberg, A.; Lennie, T.A.; Riegel, B. Identification of symptom clusters among patients with heart failure: An international observational study. Int. J. Nurs. Stud. 2014, 51, 1366–1372. [Google Scholar] [CrossRef]
- Van Lancker, A.; Beeckman, D.; Verhaeghe, S.; Van Den Noortgate, N.; Van Hecke, A. Symptom clustering in hospitalised older palliative cancer patients: A cross-sectional study. Int. J. Nurs. Stud. 2016, 61, 72–81. [Google Scholar] [CrossRef]
- SAS Institute Inc. Cubic Clustering Criterion. In SAS® Enterprise Miner™ 14.3: Reference Help; SAS Institute Inc.: Cary, NC, USA, 2017; pp. 113–149. [Google Scholar]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 26, 863. [Google Scholar] [CrossRef]
- Bjorvatn, B.; Dale, S.; Hogstad-Erikstein, R.; Fiske, E.; Pallesen, S.; Waage, S. Self-reported sleep and health among Norwegian hospital nurses in intensive care units. Nurs. Crit. Care 2012, 17, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Chaiard, J.; Deeluea, J.; Suksatit, B.; Songkham, W.; Inta, N.; Stone, T.E. Sleep disturbances and related factors among nurses. Nurs. Health Sci. 2019, 21, 470–478. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, J.S. Correlates of fatigue in critical care nurses. Res. Nurs. Health 2003, 26, 434–444. [Google Scholar] [CrossRef] [PubMed]
- Shao, M.F.; Chou, Y.C.; Yeh, M.Y.; Tzeng, W.C. Sleep quality and quality of life in female shift-working nurses. J. Adv. Nurs. 2010, 66, 1565–1572. [Google Scholar] [CrossRef]
- Centofanti, S.A.; Dorrian, J.; Hilditch, C.J.; Banks, S. Do night naps impact driving performance and daytime recovery sleep? Accid. Anal. Prev. 2017, 99, 416–421. [Google Scholar] [CrossRef]
- Rizza, S.; Luzi, A.; Mavilio, M.; Ballanti, M.; Massimi, A.; Porzio, O.; Magrini, A.; Hannemann, J.; Menghini, R.; Lehrke, M.; et al. Alterations in Rev-ERBα/BMAL1 ratio and glycated hemoglobin in rotating shift workers: The EuRhythDia study. Acta Diabetol. 2021, 58, 1111–1117. [Google Scholar] [CrossRef]
- Sun, Q.; Ji, X.; Zhou, W.; Liu, J. Sleep problems in shift nurses: A brief review and recommendations at both individual and institutional levels. J. Nurs. Manag. 2019, 27, 10–18. [Google Scholar] [CrossRef]
- Horrocks, N.; Pounder, R.; RCP Working Group. Working the night shift: Preparation, survival and recovery--a guide for junior doctors. Clin. Med. 2006, 6, 61–67. [Google Scholar] [CrossRef]
- McCulloch, M.; Ferguson, T.; Pine Street Foundation. Sleep: An Evolutionary Imperative. Are You Getting Enough? Available online: https://pinestreetfoundation.org/sleep-an-evolutionary-imperative-are-you-getting-enough/ (accessed on 4 June 2022).
- Shochat, T. Impact of lifestyle and technology developments on sleep. Nat. Sci. Sleep 2012, 4, 19–31. [Google Scholar] [CrossRef]
- Heath, G.; Coates, A.; Sargent, C.; Dorrian, J. Sleep Duration and Chronic Fatigue Are Differently Associated with the Dietary Profile of Shift Workers. Nutrients 2016, 8, 771. [Google Scholar] [CrossRef]
- Sadeghniiat-Haghighi, K.; Aminian, O.; Pouryaghoub, G.; Yazdi, Z. Efficacy and hypnotic effects of melatonin in shift-work nurses: Double-blind, placebo-controlled crossover trial. J. Circadian Rhythm. 2008, 6, 10. [Google Scholar] [CrossRef] [PubMed]
- Yoon, I.Y.; Song, B.G. Role of morning melatonin administration and attenuation of sunlight exposure in improving adaptation of night-shift workers. Chronobiol. Int. 2002, 19, 903–913. [Google Scholar] [CrossRef] [PubMed]
- Fang, R.; Li, X. A regular yoga intervention for staff nurse sleep quality and work stress: A randomised controlled trial. J. Clin. Nurs. 2015, 24, 3374–3379. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Trinkoff, A.M.; Geiger-Brown, J. Factors associated with work-related fatigue and recovery in hospital nurses working 12-hour shifts. Workplace Health Saf. 2014, 62, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Min, A.; Min, H.; Hong, H.C. Work schedule characteristics and fatigue among rotating shift nurses in hospital setting: An integrative review. J. Nurs. Manag. 2019, 27, 884–895. [Google Scholar] [CrossRef] [PubMed]
- Min, A.; Hong, H.C.; Son, S.; Lee, T. Sleep, fatigue and alertness during working hours among rotating-shift nurses in Korea: An observational study. J. Nurs. Manag. 2021, 29, 2647–2657. [Google Scholar] [CrossRef]
| Variable | Total (n = 62) | 20s (n = 20) | 30s (n = 22) | 40s (n = 20) | p-Value |
|---|---|---|---|---|---|
 | |||||
| Age (years): mean (SD) | 34.5 (7.6) | 26.4 (2.1) | 33.2 (2.7) | 44.1 (2.5) | <0.001 a |
 | |||||
| Years of nursing experience (years): mean (SD) | 11.0 (7.1) | 4.3 (2.0) | 11.1 (3.3) | 17.4 (7.3) | <0.001 a |
| BMI (kg/m2): mean (SD) | 21.6 (3.4) | 20.8 (2.3) | 21.3 (2.6) | 22.6 (4.7) | 0.616 a |
| Sex (female): N (%) | 60 (96.8) | 19 (95.0) | 21 (95.5) | 20 (100.0) | 0.999 d |
| Married (yes): N (%) | 16 (25.8) | 4 (20.0) | 8 (36.4) | 4 (20.0) | 0.371 c |
| Child rearing (yes): N (%) | 13 (21.0) | 1 (5.0) | 6 (27.3) | 6 (30.0) | 0.096 d |
| Taking nap before night shift (yes): N (%) | 18 (29.0) | 3 (15.0) | 8 (36.4) | 7 (35.0) | 0.243 c |
| Napping during night shift (yes): N (%) | 52 (83.9) | 17 (85.0) | 16 (72.7) | 19 (95.0) | 0.197 c |
 | |||||
| Resting time during night shift (min): mean (SD) | 132.5 (49.3) | 135.9 (28.1) | 153.0 (62.3) | 105.8 (33.1) | 0.002a |
 | |||||
| Cumulative steps during night shift (steps): mean (SD) | 9848.3 (2827.5) | 11,189.2 (2580.6) | 9200.7 (3258.7) | 9219.9 (2116.1) | 0.033b |
| Frequency of drinking (yes): N (%) | |||||
| Rarely drinking | 22 (35.5) | 5 (25.0) | 10 (45.4) | 7 (35.0) | 0.433 d |
| Drinking every day | 3 (4.8) | 1 (70.0) | 0 (0.0) | 2 (10.0) | |
| Other | 37 (59.7) | 14 (5.0) | 12 (54.6) | 11 (55.0) | |
| Frequency of caffeine intake (yes): N (%) | |||||
| Rarely drinking | 8 (12.9) | 3 (15.0) | 3 (13.6) | 2 (10.0) | 0.002d |
| Drinking every day | 26 (41.9) | 3 (15.0) | 8 (36.4) | 15 (75.0) | |
| Other | 28 (45.2) | 14 (70.0) | 11 (50.0) | 3 (15.0) | |
| Burnout: mean (SD) | |||||
| Emotional exhaustion | 3.5 (1.0) | 3.9 (0.7) | 3.5 (1.1) | 3.2 (1.0) | 0.101 b |
| Decline in personal accomplishment | 3.8 (0.6) | 3.9 (0.5) | 3.8 (0.5) | 3.7 (0.7) | 0.697 a |
| Depersonalization | 2.3 (1.0) | 2.6 (0.9) | 2.2 (0.9) | 2.1 (0.9) | 0.133 a |
| Resilience: mean (SD) |  | ||||
| Total score | 71.6 (10.5) | 68.0 (13.1) | 70.4 (9.4) | 76.5 (6.5) | 0.029b |
| Positivity in nursing | 24.7 (6.0) | 24.4 (6.7) | 23.3 (6.9) | 26.5 (3.7) | 0.275 a |
 | |||||
| Interpersonal skills | 16.9 (2.8) | 15.8 (3.3) | 16.8 (2.7) | 18.1 (1.9) | 0.025a |
| Having an anchor in one’s personal life | 20.5 (3.1) | 19.3 (3.9) | 21.1 (2.6) | 21.0 (2.4) | 0.105 b |
 | |||||
| Response to novelty | 9.5 (3.0) | 8.5 (3.0) | 9.1 (2.5) | 11.0 (3.3) | 0.026b |
| Coping profile: mean (SD) |  | ||||
| Active solution | 9.2 (1.8) | 8.6 (1.1) | 9.0 (1.9) | 10.3 (1.9) | 0.010a |
| Avoidance and suppression | 6.5 (2.1) | 7.4 (2.3) | 6.2 (2.1) | 6.0 (1.7) | 0.129 a |
| Changing mood | 8.4 (2.4) | 9.1 (1.9) | 8.2 (2.3) | 7.9 (2.8) | 0.233 b |
| Changing a point of view | 7.5 (2.0) | 7.0 (1.8) | 7.5 (2.2) | 7.9 (2.1) | 0.279 a |
| Seeking help for a solution | 8.9 (2.1) | 8.1 (1.9) | 9.3 (1.8) | 9.2 (2.5) | 0.123 a |
| Emotional expression involving others | 4.6 (1.3) | 5.0 (1.1) | 4.5 (1.5) | 4.4 (1.1) | 0.183 a |
| Work engagement: mean (SD) | |||||
| Vigor | 6.1 (3.2) | 5.1 (2.6) | 6.5 (3.6) | 6.7 (3.0) | 0.228 b |
| Dedication | 7.4 (3.3) | 6.7 (3.0) | 7.7 (3.8) | 8.0 (2.9) | 0.422 a |
| Absorption | 5.4 (3.0) | 4.5 (3.0) | 5.3 (3.4) | 6.5 (2.5) | 0.127 a |
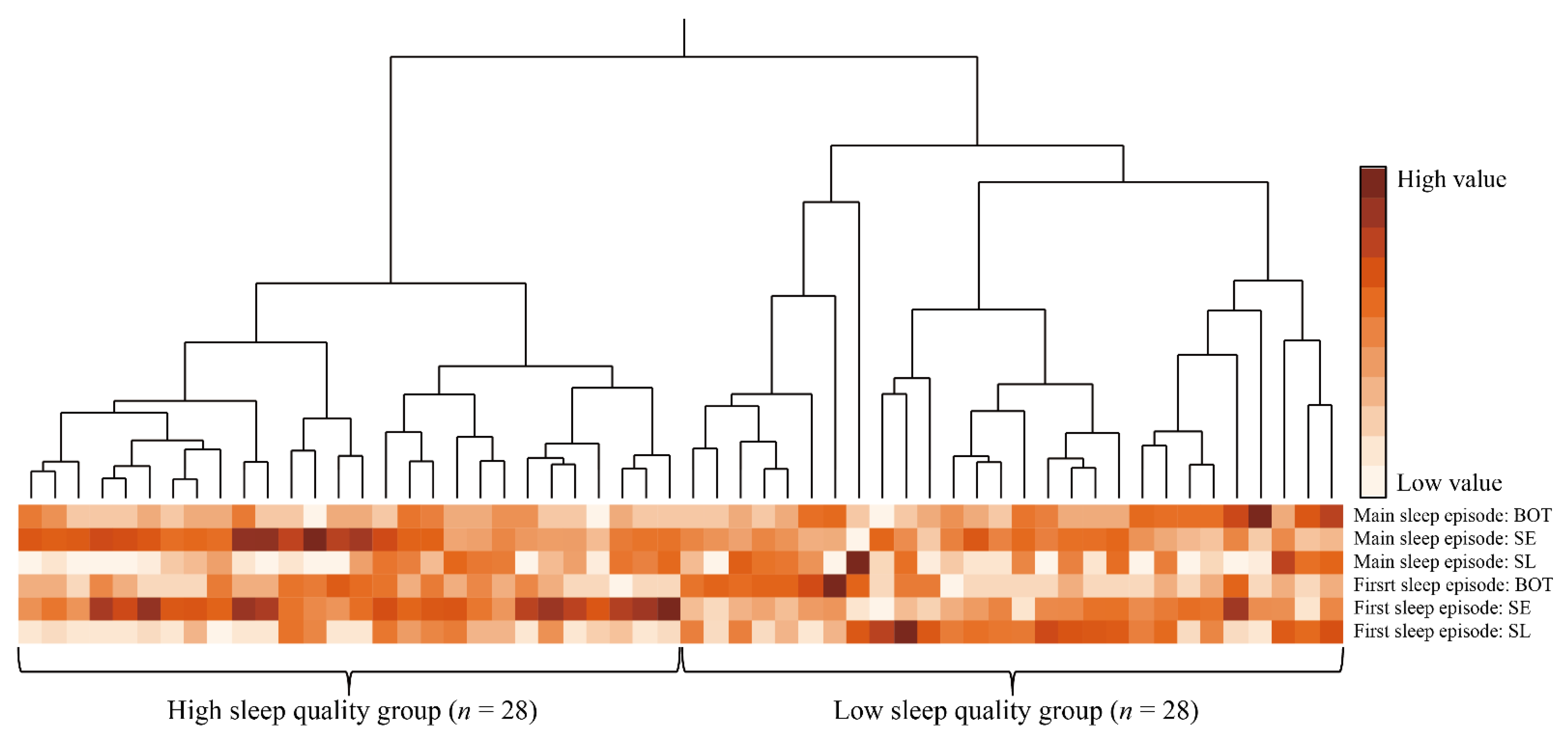
| Variable | HSQG (n = 28) | LSQG (n = 28) | Test Statistic | Effect Size | p-Value |
|---|---|---|---|---|---|
| First sleep episode: cluster mean (SD) | |||||
| SL (min) | 9.9 (8.2) | 30.7 (21.3) | - | - | |
| SE (%) | 82.4 (8.8) | 63.9 (13.0) | - | - | |
| BOT (min) | 7.1 (3.6) | 9.4 (7.8) | - | - | |
| Main sleep episode: cluster mean (SD) | |||||
| SL (min) | 16.9 (14.9) | 28.0 (33.8) | - | - | |
| SE (%) | 80.4 (10.0) | 68.8 (10.1) | - | - | |
| BOT (min) | 5.9 (3.2) | 12.2 (11.2) | - | - | |
| Age group: N (%) | |||||
| 20s | 8 (28.6) | 11 (39.3) | 1.42 | 0.16 | 0.492 c |
| 30s | 9 (32.1) | 10 (35.7) | |||
| 40s | 11 (39.3) | 7 (25.0) | |||
| Years of nursing experience (years): mean (SD) | 10.7 (6.9) | 10.4 (7.4) | 0.01 | 0.00 | 0.922 a |
| BMI (kg/m2): mean (SD) | 21.2 (3.3) | 21.6 (3.0) | 0.17 | 0.02 | 0.682 a |
| Sex (female): N (%) | 27 (96.4) | 27 (96.4) | 0.00 | 0.00 | 0.999 c |
| Married (yes): N (%) | 9 (32.1) | 4 (14.3) | 2.50 | 0.21 | 0.114 c |
| Child rearing (yes): N (%) | 8 (28.6) | 2 (7.1) | 4.38 | 0.28 | 0.036c |
| Napping during night shift (yes): N (%) | 23 (82.1) | 23 (82.1) | 0.00 | 0.00 | 0.999 c |
| Resting time during night shift (min): mean (SD) | 138.8 (62.5) | 123.3 (32.3) | 1.60 | 0.21 | 0.206 a |
| Cumulative steps during night shift (steps): mean (SD) | 9954.5 (2695.1) | 9812.1 (3044.8) | 0.19 | 0.05 | 0.854 b |
| Frequency of drinking (yes): N (%) | |||||
| Rarely drinking | 10 (35.7) | 9 (32.1) | 0.50 | 0.09 | 0.831 d |
| Drinking every day | 2 (7.2) | 1 (3.6) | |||
| Other | 16 (57.1) | 18 (64.3) | |||
| Frequency of caffeine intake (yes): N (%) | |||||
| Rarely drinking | 5 (17.9) | 3 (10.7) | 0.88 | 0.13 | 0.673 d |
| Drinking every day | 11 (39.3) | 10 (35.7) | |||
| Other | 12 (42.8) | 15 (53.6) | |||
| Start of TIB in first sleep episode: N (%) | |||||
| AM in the day after the night shift | 13 (46.4) | 14 (50.0) | 0.07 | 0.04 | 0.789 c |
| PM in the day after the night shift | 15 (53.6) | 14 (50.0) | |||
| Start of TIB in main sleep episode: N (%) | . | ||||
| Before midnight | 10 (43.5) | 8 (40.0) | 0.05 | 0.03 | 0.818 c |
| After midnight | 13 (56.5) | 12 (60.0) | |||
| Work engagement: Mean (SD) | |||||
| Vigor | 6.6 (3.6) | 5.6 (2.7) | 1.14 | 0.31 | 0.261 b |
| Dedication | 8.1 (3.8) | 6.8 (2.8) | 4.11 | 0.39 | 0.043a |
| Absorption | 5.8 (3.3) | 4.9 (2.7) | 1.49 | 0.30 | 0.222 a |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Konya, I.; Watanabe, K.; Shishido, I.; Sugimura, N.; Matsushita, Y.; Yamaguchi, S.; Yano, R. Post-Work Recovery from Fatigue and Sleep Episodes among Nurses Who Are Engaged in 16-Hour Night Shifts: A Prospective Observational Study. Healthcare 2022, 10, 1089. https://doi.org/10.3390/healthcare10061089
Konya I, Watanabe K, Shishido I, Sugimura N, Matsushita Y, Yamaguchi S, Yano R. Post-Work Recovery from Fatigue and Sleep Episodes among Nurses Who Are Engaged in 16-Hour Night Shifts: A Prospective Observational Study. Healthcare. 2022; 10(6):1089. https://doi.org/10.3390/healthcare10061089
Chicago/Turabian StyleKonya, Issei, Kazuhiro Watanabe, Inaho Shishido, Naotaka Sugimura, Yuta Matsushita, Shinya Yamaguchi, and Rika Yano. 2022. "Post-Work Recovery from Fatigue and Sleep Episodes among Nurses Who Are Engaged in 16-Hour Night Shifts: A Prospective Observational Study" Healthcare 10, no. 6: 1089. https://doi.org/10.3390/healthcare10061089
APA StyleKonya, I., Watanabe, K., Shishido, I., Sugimura, N., Matsushita, Y., Yamaguchi, S., & Yano, R. (2022). Post-Work Recovery from Fatigue and Sleep Episodes among Nurses Who Are Engaged in 16-Hour Night Shifts: A Prospective Observational Study. Healthcare, 10(6), 1089. https://doi.org/10.3390/healthcare10061089






