Patient-Reported Experiences and Satisfaction with Rural Outreach Clinics in New South Wales, Australia: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
Measures
2.2. Preparing the Data for Analyses
2.3. Statistical Analyses
2.4. Ethical Information
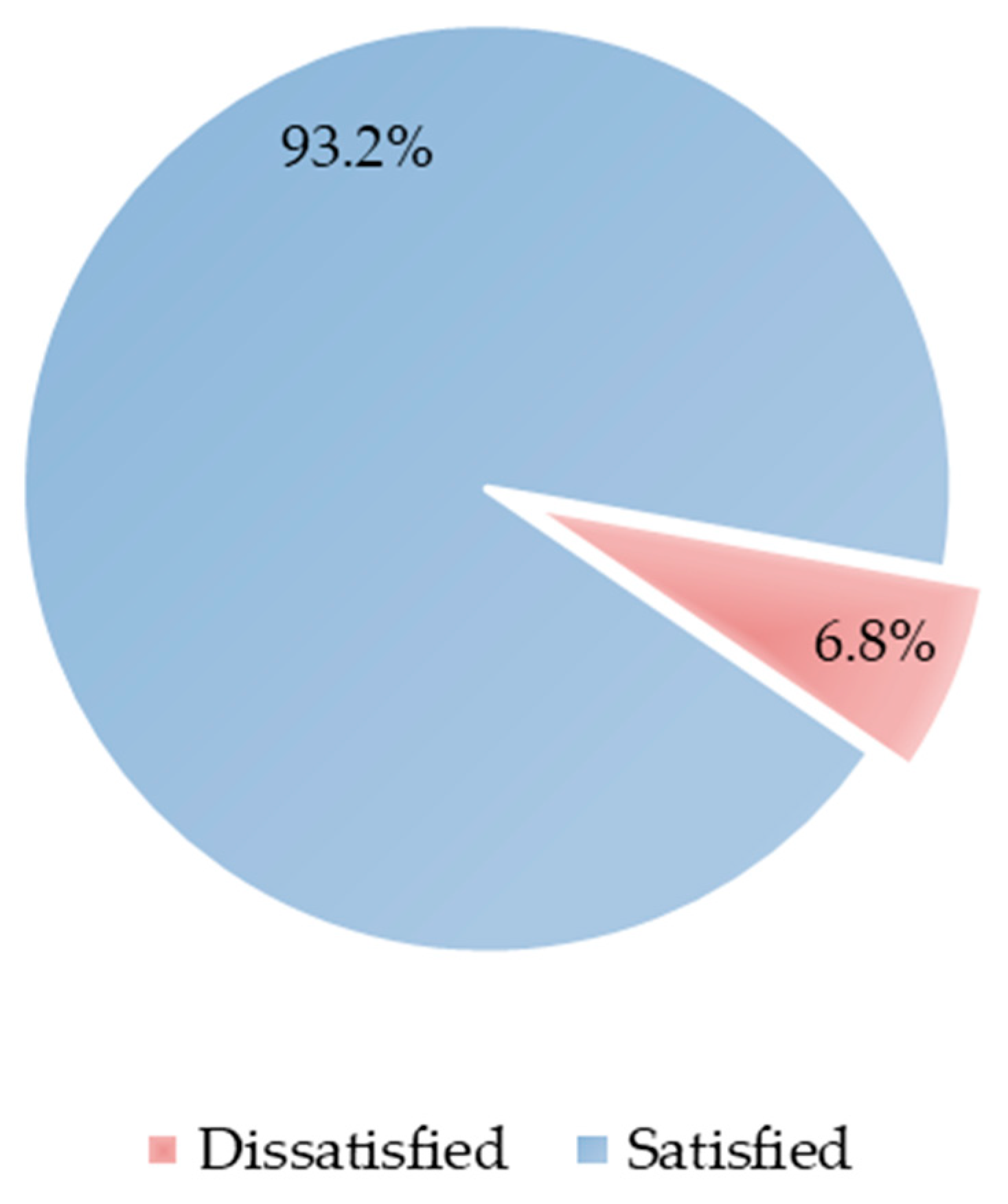
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Delaney, L.J. Patient-centred care as an approach to improving health care in Australia. Collegian 2018, 25, 119–123. [Google Scholar] [CrossRef]
- Santana, M.-J.; Manalili, K.; Zelinsky, S.; Brien, S.; Gibbons, E.; King, J.; Frank, L.; Wallström, S.; Fairie, P.; Leeb, K. Improving the quality of person-centred healthcare from the patient perspective: Development of person-centred quality indicators. BMJ Open 2020, 10, e037323. [Google Scholar] [CrossRef] [PubMed]
- ACSQHC. Patient-Centred Care: Improving Quality and Safety through Partnerships with Patients and Consumers; 0987061712; Australian Commission on Safety and Quality in Health Care: Sydney, NSW, Australia, 2011.
- Liang, Z.; Xu, M.; Liu, G.; Zhou, Y.; Howard, P. Patient-centred care and patient autonomy: Doctors’ views in Chinese hospitals. BMC Med. Ethics 2022, 23, 38. [Google Scholar] [CrossRef] [PubMed]
- Santana, M.-J.; Ahmed, S.; Lorenzetti, D.; Jolley, R.J.; Manalili, K.; Zelinsky, S.; Quan, H.; Lu, M. Measuring patient-centred system performance: A scoping review of patient-centred care quality indicators. BMJ Open 2019, 9, e023596. [Google Scholar] [CrossRef]
- AHPEQS. Why Implement AHPEQS. Available online: https://www.safetyandquality.gov.au/our-work/indicators-measurement-and-reporting/patient-experience/implementers/why-implement-ahpeqs (accessed on 6 December 2021).
- Bhanu, P. Patient satisfaction. J. Cutan. Aesthet. Surg. 2010, 3, 151–155. [Google Scholar]
- Martínez-López-de-Castro, N.; Álvarez-Payero, M.; Martín-Vila, A.; Samartín-Ucha, M.; Iglesias-Neiro, P.; Gayoso-Rey, M.; Feijoo-Meléndez, D.; Casanova-Martínez, C.; Fariña-Conde, M.; Piñeiro-Corrales, G. Factors associated with patient satisfaction in an outpatient hospital pharmacy. Eur. J. Hosp. Pharm. 2018, 25, 183–188. [Google Scholar] [CrossRef] [Green Version]
- Zawisza, K.; Galas, A.; Tobiasz-Adamczyk, B. Factors associated with patient satisfaction with health care among Polish older people: Results from the polish part of the COURAGE in Europe. Public Health 2020, 179, 169–177. [Google Scholar] [CrossRef]
- Junewicz, A.; Youngner, S.J. Patient-Satisfaction Surveys on a Scale of 0 to 10: Improving Health Care, or Leading It Astray? Hastings Cent. Rep. 2015, 45, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Chandra, S.; Ward, P.; Mohammadnezhad, M. Factors associated with patient satisfaction in outpatient department of suva sub-divisional health center, fiji, 2018: A mixed method study. Front. Public Health 2019, 7, 183. [Google Scholar] [CrossRef] [PubMed]
- Batbaatar, E.; Dorjdagva, J.; Luvsannyam, A.; Savino, M.M.; Amenta, P. Determinants of patient satisfaction: A systematic review. Perspect. Public Health 2017, 137, 89–101. [Google Scholar] [CrossRef]
- Anhang Price, R.; Elliott, M.N.; Zaslavsky, A.M.; Hays, R.D.; Lehrman, W.G.; Rybowski, L.; Edgman-Levitan, S.; Cleary, P.D. Examining the role of patient experience surveys in measuring health care quality. Med. Care Res. Rev. 2014, 71, 522–554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schoenfelder, T.; Klewer, J.; Kugler, J. Analysis of factors associated with patient satisfaction in ophthalmology: The influence of demographic data, visit characteristics and perceptions of received care. Ophthalmic Physiol. Opt. 2011, 31, 580–587. [Google Scholar] [CrossRef] [PubMed]
- UN. Department of Economic and Social Affairs, Population Division. World Urbanization Prospects; The 2017 Revision, Highlights (ST/ESA/SER. A/352); UN: New York, NY, USA, 2017. [Google Scholar]
- Cyr, M.E.; Etchin, A.G.; Guthrie, B.J.; Benneyan, J.C. Access to specialty healthcare in urban versus rural US populations: A systematic literature review. BMC Health Serv. Res. 2019, 19, 974. [Google Scholar] [CrossRef] [PubMed]
- Hart, J.T. The inverse care law. Lancet 1971, 297, 405–412. [Google Scholar] [CrossRef] [Green Version]
- Ohta, R.; Sato, M.; Kitayuguchi, J.; Maeno, T.; Sano, C. Potential help-seeking behaviors associated with better self-rated health among rural older patients: A cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 9116. [Google Scholar] [CrossRef]
- Al Shammari, S.; Alhaidar, S.; Alotaibi, M.; Alanazi, A.; Al Shammari, W.; Alanazi, A.; Alsahabi, H.; Altammami, A.; Thaher, T. Help-seeking behavior among adults in Riyadh, Saudi Arabia—A crosssectional study. Altern. Integr. Med. 2016, 5. [Google Scholar]
- Orlando, J.F.; Beard, M.; Kumar, S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS ONE 2019, 14, e0221848. [Google Scholar] [CrossRef] [Green Version]
- East, L.; Targett, D.; Yeates, H.; Ryan, E.; Quiddington, L.; Woods, C. Nurse and patient satisfaction with intentional rounding in a rural Australian setting. J. Clin. Nurs. 2020, 29, 1365–1371. [Google Scholar] [CrossRef]
- Donato, R.; Scotton, R. The Australian health care system. In Economics and Australian Health Policy; Routledge: London, UK, 2020; pp. 20–39. [Google Scholar]
- Malik, A.; Lenzen, M.; McAlister, S.; McGain, F. The carbon footprint of Australian health care. Lancet Planet. Health 2018, 2, e27–e35. [Google Scholar] [CrossRef] [Green Version]
- Nolan-Isles, D.; Macniven, R.; Hunter, K.; Gwynn, J.; Lincoln, M.; Moir, R.; Dimitropoulos, Y.; Taylor, D.; Agius, T.; Finlayson, H. Enablers and barriers to accessing healthcare services for Aboriginal people in New South Wales, Australia. Int. J. Environ. Res. Public Health 2021, 18, 3014. [Google Scholar] [CrossRef] [PubMed]
- AIHW. Rural & Remote Health. Available online: https://www.aihw.gov.au/reports/rural-remote-australians/rural-remote-health/contents/access-to-health-care (accessed on 12 December 2021).
- AIHW. Coordination of Health Care: Experiences of Barriers to Accessing Health Services among Patients Aged 45 and Over; Australian Institute of Health and Welfare, Australian Government: Canberra, Australia, 2020.
- Ifediora, C.O.; Rogers, G.D. Levels and predictors of patient satisfaction with doctor home-visit services in Australia. Fam. Pract. 2017, 34, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Adams, L.; Lester, S.; Hoon, E.; van Der Haak, H.; Proudman, C.; Hall, C.; Whittle, S.; Proudman, S.; Hill, C.L. Patient satisfaction and acceptability with telehealth at specialist medical outpatient clinics during the COVID-19 pandemic in Australia. Intern. Med. J. 2021, 51, 1028–1037. [Google Scholar] [CrossRef] [PubMed]
- Cameron, I. Outreach Health Services Fill the Gaps. Available online: https://insightplus.mja.com.au/2016/2/outreach-health-services-fill-gaps/ (accessed on 21 October 2021).
- AIHW. Profile of Indigenous Australians. Available online: https://www.aihw.gov.au/reports/australias-health/profile-of-indigenous-australians (accessed on 12 July 2022).
- Gruen, R.L.; Weeramanthri, T.S.; Bailie, R.S. Outreach and improved access to specialist services for indigenous people in remote Australia: The requirements for sustainability. J. Epidemiol. Community Health 2002, 56, 517–521. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, B.G.; Stoelwinder, J.U.; McGrail, M.R. Specialist outreach services in regional and remote Australia: Key drivers and policy implications. Med. J. Aust. 2017, 207, 98–99. [Google Scholar] [CrossRef] [PubMed]
- Keane, S.; Smith, T.; Lincoln, M.; Wagner, S.; Lowe, S. The rural allied health workforce study (RAHWS): Background, rationale and questionnaire development. Rural. Remote Health 2008, 8, 1–12. [Google Scholar] [CrossRef]
- Smith, J.G.; Plover, C.M.; McChesney, M.C.; Lake, E.T. Isolated, small, and large hospitals have fewer nursing resources than urban hospitals: Implications for rural health policy. Public Health Nurs. 2019, 36, 469–477. [Google Scholar] [CrossRef]
- AIHW. Australia’s Health 2016; Australian Institute of Health and Welfare (AIHW): Canberra, Australia, 2016.
- ABS. Australian Social Trends March 2011 Health Services: Use and Patient Experience; Australian Bureau of Statistics: Canberra, Australia, 2011.
- O’Sullivan, B. Rural Outreach by Specialist Doctors in Australia. Ph.D. Thesis, Monash University, Melbourne, Australia, 2016. [Google Scholar]
- O’Sullivan, B.G.; Joyce, C.M.; McGrail, M.R. Rural outreach by specialist doctors in Australia: A national cross-sectional study of supply and distribution. Hum. Resour. Health 2014, 12, 50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galdas, P.M.; Cheater, F.; Marshall, P. Men and health help-seeking behaviour: Literature review. J. Adv. Nurs. 2005, 49, 616–623. [Google Scholar] [CrossRef] [PubMed]
- NSWGovernment. Your Experience Matters. Available online: https://www.snswlhd.health.nsw.gov.au/patients-visitors/your-experience-matters (accessed on 14 July 2022).
- RDN, N. Outreach. Available online: https://www.nswrdn.com.au/ (accessed on 31 August 2021).
- Renzi, C.; Abeni, D.; Picardi, A.; Agostini, E.; Melchi, C.; Pasquini, P.; Puddu, P.; Braga, M. Factors associated with patient satisfaction with care among dermatological outpatients. Br. J. Dermatol. 2001, 145, 617–623. [Google Scholar] [CrossRef]
- Agresti, A.; Kateri, M. Categorical Data Analysis; Springer: Berlin/Heidelberg, Germany, 2011. [Google Scholar]
- Islam, M.I.; Yunus, F.M.; Isha, S.N.; Kabir, E.; Khanam, R.; Martiniuk, A. The gap between perceived mental health needs and actual service utilization in Australian adolescents. Sci. Rep. 2022, 12, 5430. [Google Scholar] [CrossRef] [PubMed]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons: Hoboken, NJ, USA, 2013; Volume 398. [Google Scholar]
- Jones, A.M. Models for Health Care; University of York, Centre for Health Economics: York, UK, 2010. [Google Scholar]
- Murray, L.; Nguyen, H.; Lee, Y.-F.; Remmenga, M.D.; Smith, D.W. Variance Inflation Factors in Regression Models with Dummy Variables. 2012. Available online: https://newprairiepress.org/agstatconference/2012/proceedings/12/ (accessed on 14 July 2022).
- StataCorp. Stata Survey Data Reference Manual Release 17. 2021. Available online: https://www.stata.com/manuals/svy.pdf (accessed on 14 July 2022).
- Beck, R.S.; Daughtridge, R.; Sloane, P.D. Physician-patient communication in the primary care office: A systematic review. J. Am. Board Fam. Pract. 2002, 15, 25–38. [Google Scholar] [PubMed]
- DiMatteo, M.R.; Hays, R. The significance of patients’ perceptions of physician conduct. J. Community Health 1980, 6, 18–34. [Google Scholar] [CrossRef] [PubMed]
- Hayran, O.; Özer, O. Organizational health literacy as a determinant of patient satisfaction. Public Health 2018, 163, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Tisano, B.K.; Nakonezny, P.A.; Gross, B.S.; Martinez, J.R.; Wells, J.E. Depression and non-modifiable patient factors associated with patient satisfaction in an academic orthopaedic outpatient clinic: Is it more than a provider issue? Clin. Orthop. Relat. Res. 2019, 477, 2653. [Google Scholar] [CrossRef]
- OECD. OECD Reviews of Health Care Quality: Australia 2015: Raising Standards; OECD: Paris, France, 2015. [Google Scholar]
- Harris, A.; Robinson, G. The Aboriginal Mental Health Worker Program: The challenge of supporting Aboriginal involvement in mental health care in the remote community context. Aust. e-J. Adv. Ment. Health 2007, 6, 15–25. [Google Scholar] [CrossRef]
- Kosky, R.J.; Dundas, P. Death by hanging: Implications for prevention of an important method of youth suicide. Aust. N. Z. J. Psychiatry 2000, 34, 836–841. [Google Scholar] [CrossRef]
- Parker, R. Australia’s Aboriginal population and mental health. J. Nerv. Ment. Dis. 2010, 198, 3–7. [Google Scholar] [CrossRef]
- ABS. Patient Experiences in Australia: Summary of Findings, 2016–17 Data Cubes. ABS cat. no. 4839.0. Available online: http://www.abs.gov.au/AUSSTATS/[email protected]/DetailsPage/4839.02016-17?OpenDocument (accessed on 6 December 2021).
- Clever, S.L.; Jin, L.; Levinson, W.; Meltzer, D.O. Does doctor–patient communication affect patient satisfaction with hospital care? Results of an analysis with a novel instrumental variable. Health Serv. Res. 2008, 43, 1505–1519. [Google Scholar] [CrossRef] [Green Version]
- Biglu, M.-H.; Nateq, F.; Ghojazadeh, M.; Asgharzadeh, A. Communication skills of physicians and patients’ satisfaction. Mater. Socio-Med. 2017, 29, 192. [Google Scholar] [CrossRef] [Green Version]
- Carlsen, B.; Aakvik, A. Patient involvement in clinical decision making: The effect of GP attitude on patient satisfaction. Health Expect. 2006, 9, 148–157. [Google Scholar] [CrossRef] [Green Version]
- Vahdat, S.; Hamzehgardeshi, L.; Hessam, S.; Hamzehgardeshi, Z. Patient involvement in health care decision making: A review. Iran. Red Crescent Med. J. 2014, 16, e12454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yashadhana, A.; Fields, T.; Blitner, G.; Stanley, R.; Zwi, A.B. Trust, culture and communication: Determinants of eye health and care among Indigenous people with diabetes in Australia. BMJ Glob. Health 2020, 5, e001999. [Google Scholar] [CrossRef] [PubMed]
- Skyring, T.A.; Mansfield, K.J.; Mullan, J.R. Factors Affecting Satisfaction with the Decision-Making Process and Decision Regret for Men with a New Diagnosis of Prostate Cancer. Am. J. Men’s Health 2021, 15, 15579883211026812. [Google Scholar] [CrossRef] [PubMed]
- Moslehpour, M.; Shalehah, A.; Rahman, F.F.; Lin, K.-H. The Effect of Physician Communication on Inpatient Satisfaction. Healthcare 2022, 10, 463. [Google Scholar] [CrossRef] [PubMed]
- Trant, A.A.; Szekely, B.; Mougalian, S.S.; DiGiovanna, M.P.; Sanft, T.; Hofstatter, E.; Silber, A.; Adelson, K.B.; Chagpar, A.; Killelea, B. The impact of communication style on patient satisfaction. Breast Cancer Res. Treat. 2019, 176, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Chia, Y.Y.P.; Ekladious, A. Australian public hospital inpatient satisfaction related to early patient involvement and shared decision-making in discharge planning. Intern. Med. J. 2021, 51, 891–895. [Google Scholar] [CrossRef] [PubMed]
- Doyle, C.; Lennox, L.; Bell, D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013, 3, e001570. [Google Scholar] [CrossRef] [PubMed]
| n (%) | 95% CI | |
|---|---|---|
| Age (Mean = 58.6, SD = ±20.50) | ||
| Adults (18–64 years) | 106 (51.2) | 0.45–0.58 |
| Children (≤17 years) | 9 (4.4) | 0.02–0.08 |
| Older adult (≥65 years) | 92 (44.4) | 0.38–0.51 |
| Gender | ||
| Male | 104 (50.2) | 0.43–0.57 |
| Female | 103 (49.8) | 0.42–0.56 |
| Country of birth | ||
| Australia | 187 (90.3) | 0.85–0.93 |
| Overseas | 20 (9.7) | 0.06–0.14 |
| Indigeneity | ||
| Non-Indigenous | 132 (63.8) | 0.56–0.71 |
| Indigenous | 75 (36.2) | 0.29–0.43 |
| Health professionals visited 1 | ||
| Medical | 169 (81.6) | 0.75–0.86 |
| Non-Medical | 38 (18.4) | 0.14–0.24 |
| Mode of consultation | ||
| In-person | 189 (91.3) | 0.86–0.95 |
| Telephone or Online | 18 (8.7) | 0.05–0.13 |
| Type of transport | ||
| Private | 148 (71.5) | 0.65–0.78 |
| Public | 35 (16.9) | 0.12–0.22 |
| No transport or Walk | 24 (11.6) | 0.07–0.16 |
| Travel time | ||
| <20 min | 117 (56.5) | 0.49–0.63 |
| ≥20 min | 90 (43.5) | 0.36–0.50 |
| Frequency of visits 2 | ||
| Twice or more | 156 (75.4) | 0.69–0.8 1 |
| Once | 51 (24.6) | 0.19–0.31 |
| Behaviour of Health Professionals | ||
| Not respectful | 23 (11.1) | 0.08–0.16 |
| Respectful | 184 (88.9) | 0.83–0.92 |
| Dissatisfied | Satisfied | Pearson χ2 (p-Value) | |
|---|---|---|---|
| n (%) | n (%) | ||
| Age (Mean = 58.6, SD = ±20.50) | 4.21 (0.121) | ||
| Adults (18–64 years) | 5 (4.7) | 101 (95.3) | |
| Children (≤17 years) | 2 (22.2) | 7 (77.8) | |
| Older adult (≥65 years) | 7 (7.61) | 85 (92.4) | |
| Gender | 0.32 (0.567) | ||
| Male | 6 (5.8) | 98 (94.2) | |
| Female | 8 (7.8) | 95 (92.2) | |
| Country of birth | 0.11 (0.741) | ||
| Australia | 13 (6.9) | 174 (93.1) | |
| Overseas | 1 (5.0) | 19 (95.0) | |
| Indigeneity | 0.38 (0.537) | ||
| Non-Indigenous | 10 (7.6) | 122 (92.4) | |
| Indigenous | 4 (5.3) | 71 (94.7) | |
| Health professionals visited | 0.09 (0.759) | ||
| Medical | 11 (6.5) | 158 (93.5) | |
| Non-Medical | 3 (7.9) | 35 (92.1) | |
| Mode of consultation | 3.06 (0.080) | ||
| In-person | 11 (5.8) | 178 (94.2) | |
| Telephone or Online | 3 (16.7) | 15 (83.3) | |
| Type of transport | 7.79 (0.020 *) | ||
| Private | 6 (4.1) | 142 (95.9) | |
| Public | 6 (17.1) | 29 (82.9) | |
| No transport or Walk | 2 (8.3) | 22 (91.7) | |
| Travel time | 0.36 (0.544) | ||
| <20 min | 9 (7.7) | 108 (92.3) | |
| ≥20 min | 5 (5.6) | 85 (94.4) | |
| Frequency of visits | 5.20 (0.023 *) | ||
| Twice or more | 7 (4.5) | 149 (95.5) | |
| Once | 7 (13.7) | 44 (86.3) | |
| Behaviour of Health Professional | 69.18 (<0.001 ***) | ||
| Not respectful | 11 (47.8) | 12 (52.2) | |
| Respectful | 3 (1.6) | 181 (98.4) |
| aOR | 95% CI | VIF | |
|---|---|---|---|
| Vehicle used (Ref. Private) | 1.07 | ||
| Public | 0.11 *** | 0.08–0.17 | |
| No transport or Walk | 0.12 | 0.00–15.95 | |
| Frequency of visits (Ref. Twice or more) | 1.07 | ||
| Once | 0.25 | 0.03–2.10 | |
| Behaviour of Health professionals (Ref. Not respectful) | 1.00 | ||
| Respectful | 159.41 ** | 28.78–883.25 | |
| Model statistics | |||
| McKelvey and Zavoina’s R2 | 0.578 | ||
| Goodness-of-fit test | 7.18 | ||
| Link test | 7.68 ** | ||
| Mean VIF | 1.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Islam, M.I.; O’Neill, C.; Kolur, H.; Bagnulo, S.; Colbran, R.; Martiniuk, A. Patient-Reported Experiences and Satisfaction with Rural Outreach Clinics in New South Wales, Australia: A Cross-Sectional Study. Healthcare 2022, 10, 1391. https://doi.org/10.3390/healthcare10081391
Islam MI, O’Neill C, Kolur H, Bagnulo S, Colbran R, Martiniuk A. Patient-Reported Experiences and Satisfaction with Rural Outreach Clinics in New South Wales, Australia: A Cross-Sectional Study. Healthcare. 2022; 10(8):1391. https://doi.org/10.3390/healthcare10081391
Chicago/Turabian StyleIslam, Md Irteja, Claire O’Neill, Hibah Kolur, Sharif Bagnulo, Richard Colbran, and Alexandra Martiniuk. 2022. "Patient-Reported Experiences and Satisfaction with Rural Outreach Clinics in New South Wales, Australia: A Cross-Sectional Study" Healthcare 10, no. 8: 1391. https://doi.org/10.3390/healthcare10081391






