The Preliminary Efficacy of a Program to Facilitate Benefit Finding for People with Mental Illness: A Pilot Randomized Controlled Trial in Japan
Abstract
1. Introduction
2. Materials and Methods
2.1. Program Development to Facilitate Benefit Finding: “To Live Lively”
2.2. Preliminary Pre–Post Study
2.3. Participants and Randomization
2.4. Procedures
2.5. Measures
2.5.1. Benefit Finding Questionnaire (BFQ)
2.5.2. Recovery Assessment Scale (RAS)
2.5.3. World Health Organization (WHO)-5 Well-Being Index
2.5.4. Behavior and Symptom Identification Scale (BASIS-32)
2.6. Statistical Analysis
2.7. Ethical Considerations and Clinical Trial Register
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Skar-Fröding, R.; Clausen, H.; Šaltytė Benth, J.; Ruud, T.; Slade, M.; Heiervang, K.S. Associations between personal recovery and service user-rated versus clinician-rated clinical recovery, a cross-sectional study. BMC Psychiatry 2022, 22, 42. [Google Scholar] [CrossRef]
- van Weeghel, J.; van Zelst, C.; Boertien, D.; Hasson-Ohayon, I. Conceptualizations, assessments, and implications of personal recovery in mental illness: A scoping review of systematic reviews and meta-analyses. Psychiatr. Rehabil. J. 2019, 42, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Wood, L.; Alsawy, S. Recovery in Psychosis from a Service User Perspective: A Systematic Review and Thematic Synthesis of Current Qualitative Evidence. Community Ment. Health J. 2018, 54, 793–804. [Google Scholar] [CrossRef] [PubMed]
- Lechner, S.C. Benefit-Finding. In The Oxford Handbook of Positive Psychology, 3rd ed.; Snyder, C.R., Lopez, S.J., Edwards, L.M., Eds.; Oxford University Press: Oxford, UK, 2020; pp. 907–918. [Google Scholar]
- Gallagher, S.; O’Sullivan, L.; Hughes, Z.; O’Connell, B.H. Building Resources in Caregivers: Feasibility of a Brief Writing Intervention to Increase Benefit Finding in Caregivers. Appl. Psychol. Health Well-Being 2020, 12, 513–531. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhang, L.; Cao, Y.; Xia, W.; Zhang, L. The relationship between coping styles and benefit finding of Chinese cancer patients: The mediating role of distress. Eur. J. Oncol. Nurs. Off. J. Eur. Oncol. Nurs. Soc. 2018, 34, 15–20. [Google Scholar] [CrossRef]
- Zhu, P.; Chen, C.; Liu, X.; Gu, W.; Shang, X. Factors associated with benefit finding and mental health of patients with cancer: A systematic review. Support. Care Cancer 2022, 30, 6483–6496. [Google Scholar] [CrossRef]
- Chiba, R.; Miyamoto, Y.; Funakoshi, A. Characteristics of Benefit-finding in People with Mental Illness. J. Jpn. Acad. Nurs. Sci. 2010, 30, 32–40. [Google Scholar] [CrossRef][Green Version]
- Anthony, W.A. Recovery from mental illness: The guiding vision of the mental health service system in the 1990s. Psychosoc. Rehabil. J. 1993, 16, 11–23. [Google Scholar] [CrossRef]
- Qiu, X.; Zhang, K.; Zhang, Y.; Sun, L. Benefit Finding and Related Factors of Patients with Early-Stage Cancer in China. Int. J. Environ. Res. Public Health 2022, 19, 4284. [Google Scholar] [CrossRef]
- Liu, Z.; Doege, D.; Thong, M.S.Y.; Koch-Gallenkamp, L.; Bertram, H.; Eberle, A.; Holleczek, B.; Nennecke, A.; Waldmann, A.; Zeißig, S.R.; et al. Distress mediates the relationship between cognitive appraisal of medical care and benefit finding/posttraumatic growth in long-term cancer survivors. Cancer 2021, 127, 3680–3690. [Google Scholar] [CrossRef]
- Vitale, S.R.; Schneider, H.; Gardner, L.; Alessandri, M.; Marker, C. Challenging Behavior and Parental Depression: The Effects of Everyday Stressors and Benefit Finding for Parents of Children with Autism Spectrum Disorder. J. Autism Dev. Disord. 2022; in press. [Google Scholar] [CrossRef] [PubMed]
- Chiba, R.; Miyamoto, Y.; Kawakami, N.; Harada, N. Effectiveness of a program to facilitate recovery for people with long-term mental illness in Japan. Nurs. Health Sci. 2014, 16, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Chiba, R.; Yamazaki, Y.; Miyamoto, Y.; Funakoshi, A. Related Changes in Personal Recovery, Benefit Finding, and Sense of Coherence among People with Chronic Mental Illness: A Two-Wave Study. J. Psychol. 2021, 155, 292–308. [Google Scholar] [CrossRef] [PubMed]
- Prikken, S.; Raymaekers, K.; Lemiere, J.; Vercruysse, T.; Uyttebroeck, A.; Luyckx, K. Worries and Benefit Finding in Cancer Survivors and Parents: A Longitudinal Study. J. Pediatr. Psychol. 2021, 47, 641–651. [Google Scholar] [CrossRef]
- Cheng, S.T.; Lau, R.W.; Mak, E.P.; Ng, N.S.; Lam, L.C. Benefit-finding intervention for Alzheimer caregivers: Conceptual framework, implementation issues, and preliminary efficacy. Gerontologist 2014, 54, 1049–1058. [Google Scholar] [CrossRef]
- Antoni, M.H.; Ironson, G.; Schneiderman, N. Cognitive-Behavioral Stress Management Workbook; Oxford University Press: Oxford, UK, 2007. [Google Scholar]
- Penedo, F.J.; Molton, I.; Dahn, J.R.; Shen, B.J.; Kinsinger, D.; Traeger, L.; Siegel, S.; Schneiderman, N.; Antoni, M. A randomized clinical trial of group-based cognitive-behavioral stress management in localized prostate cancer: Development of stress management skills improves quality of life and benefit finding. Ann. Behav. Med. 2006, 31, 261–270. [Google Scholar] [CrossRef]
- Zhang, M.M.; Chen, J.J.; Zhang, T.; Wang, Q.L.; Li, H.P. Feasibility and effect of a guided self-disclosure intervention designed to facilitate benefit finding in breast cancer patients: A pilot study. Eur. J. Oncol. Nurs. 2021, 50, 101879. [Google Scholar] [CrossRef]
- Chiba, R.; Miyamoto, Y.; Harada, N. Psychological transformation by an intervention to facilitate benefit finding among people with chronic mental illness in Japan. Perspect. Psychiatr. Care 2016, 52, 139–144. [Google Scholar] [CrossRef]
- Ramos, C.; Costa, P.A.; Rudnicki, T.; Marôco, A.L.; Leal, I.; Guimarães, R.; Fougo, J.L.; Tedeschi, R.G. The effectiveness of a group intervention to facilitate posttraumatic growth among women with breast cancer. Psychooncology 2018, 27, 258–264. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. A clinical approach to post-traumatic growth. In Positive Psychology in Practice.; Linley, P.A., Joseph, S., Eds.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2004; pp. 405–419. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Chiba, R.; Funakoshi, A.; Yamazaki, Y.; Miyamoto, Y. The Benefit Finding Questionnaire (BFQ): Scale Development, Validation, and Its Psychometric Properties Among People with Mental Illness. Healthcare 2020, 8, 303. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, P.W.; Salzer, M.; Ralph, R.O.; Sangster, Y.; Keck, L. Examining the factor structure of the recovery assessment scale. Schizophr. Bull. 2004, 30, 1035–1041. [Google Scholar] [CrossRef] [PubMed]
- Chiba, R.; Miyamoto, Y.; Kawakami, N. Reliability and validity of the Japanese version of the Recovery Assessment Scale (RAS) for people with chronic mental illness: Scale development. Int. J. Nurs. Stud. 2010, 47, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef]
- Awata, S.; Bech, P.; Yoshida, S.; Hirai, M.; Suzuki, S.; Yamashita, M.; Ohara, A.; Hinokio, Y.; Matsuoka, H.; Oka, Y. Reliability and validity of the Japanese version of the World Health Organization-Five Well-Being Index in the context of detecting depression in diabetic patients. Psychiatry Clin. Neurosci. 2007, 61, 112–119. [Google Scholar] [CrossRef]
- Eisen, S.V.; Leff, H.S.; Schaefer, E. Implementing outcome systems: Lessons from a test of the BASIS-32 and the SF-36. J. Behav. Health Serv. Res. 1999, 26, 18–27. [Google Scholar] [CrossRef]
- Setoya, Y.; Tachimori, H.; Ito, H.; Naganuma, Y.; Kurita, H. Seishinka nyuuin kanja ni okeru koudou oyobi shoujyou sokutei shakudo BASIS-32 nihongoban no yuuyousei [Utility of the Japanese version of the BASIS-32 in inpatients in psychiatric hospitals]. Jpn. J. Clin. Psychiatr. 2002, 31, 571–575. (In Japanese) [Google Scholar]
- Brydges, C.R. Effect Size Guidelines, Sample Size Calculations, and Statistical Power in Gerontology. Innov. Aging 2019, 3, igz036. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef]
- Wang, S.; Zhou, Y.; Li, L.; Kent, S. Benefit finding: Understanding the impact and public health factors among COVID-19 patients in China. Br. J. Nurs. 2022, 31, 222–228. [Google Scholar] [CrossRef]
- Cheng, S.T.; Chan, W.C.; Lam, L.C. Are Care-Recipient Outcomes Attributable to Improved Caregiver Well-Being? A Cluster-Randomized Controlled Trial of Benefit-Finding Intervention. Am. J. Geriatr. Psychiatry 2022, 30, 903–913. [Google Scholar] [CrossRef] [PubMed]
- Miao, M.; Zheng, L.; Wen, J.; Jin, S.; Gan, Y. Coping with coronavirus disease 2019: Relationships between coping strategies, benefit finding and well-being. Stress Health 2022, 38, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Wepf, H.; Joseph, S.; Leu, A. Pathways to Mental Well-Being in Young Carers: The Role of Benefit Finding, Coping, Helplessness, and Caring Tasks. J. Youth Adolesc. 2021, 50, 1911–1924. [Google Scholar] [CrossRef] [PubMed]
- Levin, R.L.; Rawana, J.S. Exploring two models of emotion regulation: How strategy use, abilities, and flexibility relate to well-being and mental illness. Anxiety Stress Coping 2021, 1–14. [Google Scholar] [CrossRef]

| Total (n = 24) | Intervention (n = 15) | Control (n = 9) | ||||
|---|---|---|---|---|---|---|
| Characteristic | n/Mean | %/SD | n/Mean | %/SD | n/Mean | %/SD |
| Gender (male), n (%) | 11 | (45.8) | 9 | (60.0) | 2 | (22.2) |
| Age (years), Mean (SD) | 42.5 | (13.4) | 39.0 | (11.6) | 48.3 | (14.7) |
| Range | 22–72 | 22–56 | 22–72 | |||
| Duration of mental illness (years), Mean (SD) | 16.3 | (9.9) | 15.0 | (6.5) | 18.4 | (14.1) |
| Range | 3–44 | 5–26 | 3–44 | |||
| Diagnosis, n (%) | ||||||
| Schizophrenia | 15 | (62.5) | 10 | (66.7) | 5 | (55.6) |
| Depression | 6 | (25.0) | 3 | (20.0) | 3 | (33.3) |
| Bipolar disorder | 2 | (8.3) | 1 | (6.7) | 1 | (11.1) |
| Other | 1 | (4.2) | 1 | (6.7) | 0 | (0.0) |
| Experience of hospitalization for psychiatric wards (Yes), n (%) | 6 | (25.0) | 4 | (26.7) | 7 | (77.8) |
| Duration of hospitalization for psychiatric wards (months), Mean (SD) | 32.7 | (96.5) | 10.3 | (10.3) | 70.1 | (155.1) |
| Range | 0–481 | 0–30 | 0–481 | |||
| Recipient of Mental disability certificate (Yes), n (%) | 23 | (95.8) | 14 | (93.3) | 9 | (100.0) |
| Recipient of Disability pension (Yes), n (%) | 12 | (50.0) | 8 | (53.3) | 4 | (44.4) |
| Recipient of Livelihood protection (Yes), n (%) | 10 | (41.7) | 7 | (46.7) | 3 | (33.3) |
| Services in use (multiple answers), n (%) | ||||||
| Employment support (Yes) | 18 | (75.0) | 14 | (93.4) | 4 | (44.4) |
| Community activity support center (Yes) | 4 | (16.7) | 3 | (20.0) | 1 | (11.1) |
| Home-visit nursing (Yes) | 6 | (25.0) | 4 | (26.7) | 2 | (22.2) |
| Psychiatric day care center (Yes) | 4 | (16.7) | 2 | (13.3) | 2 | (22.2) |
| Self-help group (Yes) | 3 | (12.5) | 1 | (6.7) | 2 | (22.2) |
| Experience as a peer (Yes), n (%) | 8 | (33.3) | 4 | (26.7) | 4 | (44.4) |
| Intervention (n = 15) | Control (n = 9) | Test of Difference | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | (SD) | Mean Change (SD) from T1 | Mean | (SD) | Mean Change (SD) from T1 | T2-T1 | T3-T1 | |||||||||||
| Instruments and subscales (range) | T1 | T2 | T3 | T1 | T2 | T3 | t | df | Effect Size (d) | t | df | Effect Size (d) | ||||||
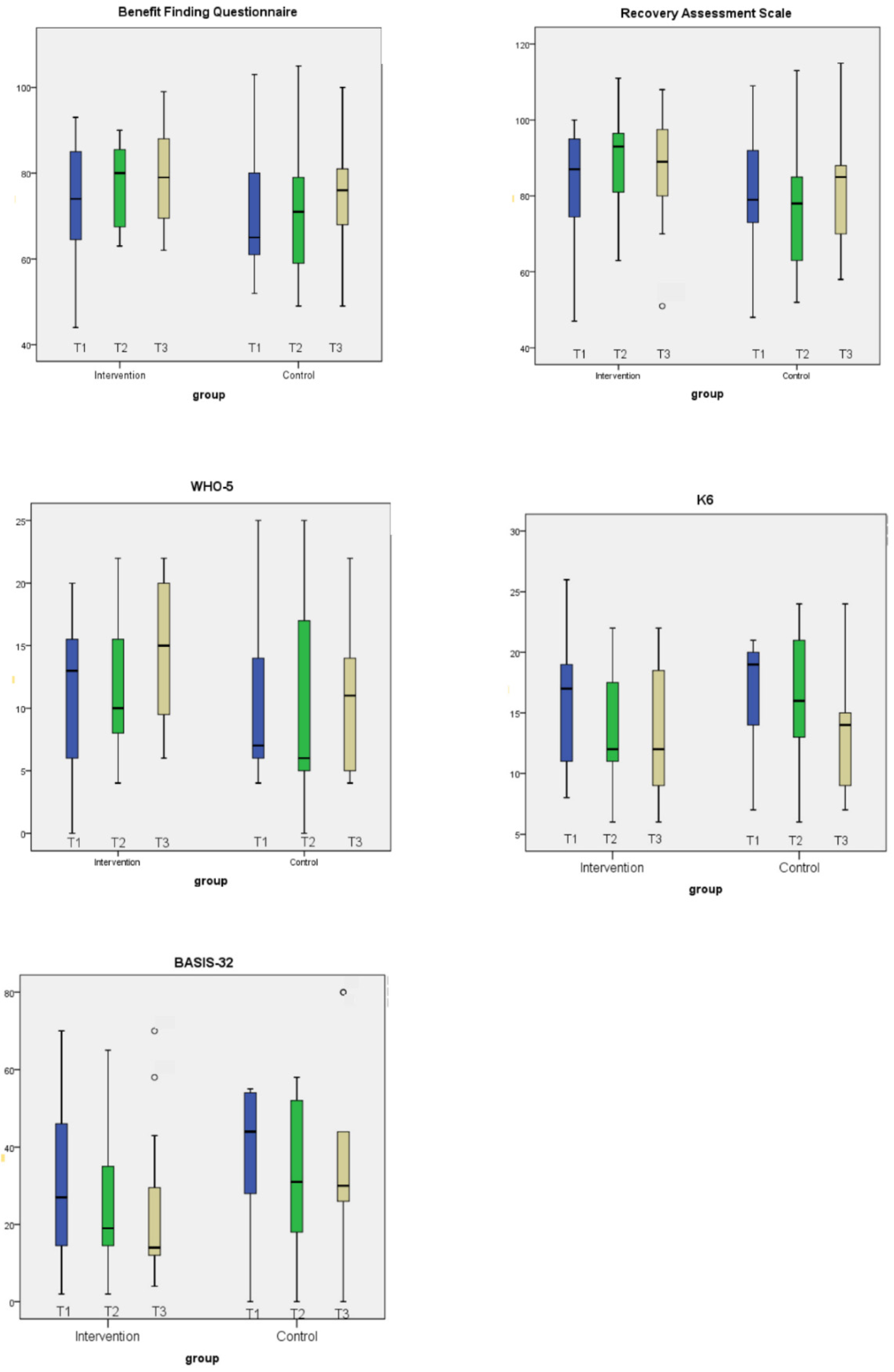
| Benefit Finding Questionnaire (21–105) | 72.9 | (14.2) | 4.9 | (16.4) | 6.6 | (15.8) | 71.2 | (15.9) | 1.1 | (5.9) | 3.9 | (9.1) | 0.8 | 19 | 0.28 | 0.5 | 22 | 0.20 |
| Changes in sense of values and way of thinking (13–65) | 45.6 | (10.8) | 3.1 | (11.7) | 3.8 | (11.0) | 44.1 | (11.6) | 0.3 | (3.4) | 3.3 | (7.7) | 0.9 | 18 | 0.29 | 0.1 | 22 | 0.05 |
| Changes in relationships with others (8–40) | 27.3 | (4.5) | 1.8 | (5.6) | 2.8 | (6.0) | 27.1 | (5.0) | 0.8 | (3.0) | 0.6 | (3.8) | 0.5 | 22 | 0.21 | 1.0 | 22 | 0.42 |
|
Recovery Assessment Scale (24–120) | 83.0 | (15.6) | 5.9 | (13.2) | 3.8 | (11.5) | 80.0 | (21.6) | −0.3 | (8.7) | 2.2 | (14.2) | 1.3 | 22 | 0.53 | 0.3 | 22 | 0.13 |
| Goal/success orientation and hope (9–45) | 32.3 | (7.9) | 1.3 | (6.0) | 1.9 | (5.1) | 30.8 | (7.5) | −0.1 | (4.8) | 1.7 | (6.5) | 0.6 | 22 | 0.26 | 0.1 | 22 | 0.05 |
| Reliance on others (4–20) | 14.5 | (3.5) | 0.7 | (1.8) | −0.7 | (2.1) | 14.4 | (3.9) | 0.0 | (1.6) | −0.6 | (2.6) | 0.9 | 22 | 0.38 | −0.1 | 22 | 0.05 |
| Personal confidence (5–25) | 15.1 | (4.0) | 2.1 | (4.7) | 1.5 | (3.2) | 13.4 | (5.6) | 1.0 | (3.0) | 2.4 | (4.2) | 0.7 | 22 | 0.22 | −0.6 | 22 | 0.27 |
| No domination by symptoms (2–10) | 6.9 | (1.8) | 0.5 | (1.5) | 0.6 | (1.5) | 7.4 | (1.9) | −0.6 | (1.2) | −0.8 | (2.1) | 1.8 | 22 | 0.74 | 1.8 | 22 | 0.79 |
| Willingness to ask for help (4–20) | 14.2 | (2.3) | 1.3 | (2.5) | 0.5 | (2.5) | 13.9 | (3.9) | −0.7 | (2.2) | −0.6 | (2.2) | 1.9 | 22 | 0.80 | 1.0 | 22 | 0.42 |
| WHO-5 Well-Being Index (0–25) | 11.1 | (6.1) | 1.0 | (5.2) | 3.4 | (6.1) | 11.0 | (7.7) | −0.7 | (9.2) | 0.1 | (3.6) | 0.6 | 22 | 0.24 | 1.5 | 22 | 0.62 |
| BASIS-32 (0–128) | 31.2 | (20.5) | -5.1 | (21.1) | -8.1 | (20.5) | 37.0 | (21.4) | −4.1 | (10.0) | 0.7 | (19.3) | −0.1 | 22 | 0.05 | -1.0 | 22 | 0.44 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiba, R.; Funakoshi, A.; Miyamoto, Y. The Preliminary Efficacy of a Program to Facilitate Benefit Finding for People with Mental Illness: A Pilot Randomized Controlled Trial in Japan. Healthcare 2022, 10, 1491. https://doi.org/10.3390/healthcare10081491
Chiba R, Funakoshi A, Miyamoto Y. The Preliminary Efficacy of a Program to Facilitate Benefit Finding for People with Mental Illness: A Pilot Randomized Controlled Trial in Japan. Healthcare. 2022; 10(8):1491. https://doi.org/10.3390/healthcare10081491
Chicago/Turabian StyleChiba, Rie, Akiko Funakoshi, and Yuki Miyamoto. 2022. "The Preliminary Efficacy of a Program to Facilitate Benefit Finding for People with Mental Illness: A Pilot Randomized Controlled Trial in Japan" Healthcare 10, no. 8: 1491. https://doi.org/10.3390/healthcare10081491
APA StyleChiba, R., Funakoshi, A., & Miyamoto, Y. (2022). The Preliminary Efficacy of a Program to Facilitate Benefit Finding for People with Mental Illness: A Pilot Randomized Controlled Trial in Japan. Healthcare, 10(8), 1491. https://doi.org/10.3390/healthcare10081491






