Diagnostic Utility of Hysteroscopic Biopsy in Cases of Suspected Lobular Endocervical Glandular Hyperplasia and Comparison with Cervical Conization
Abstract
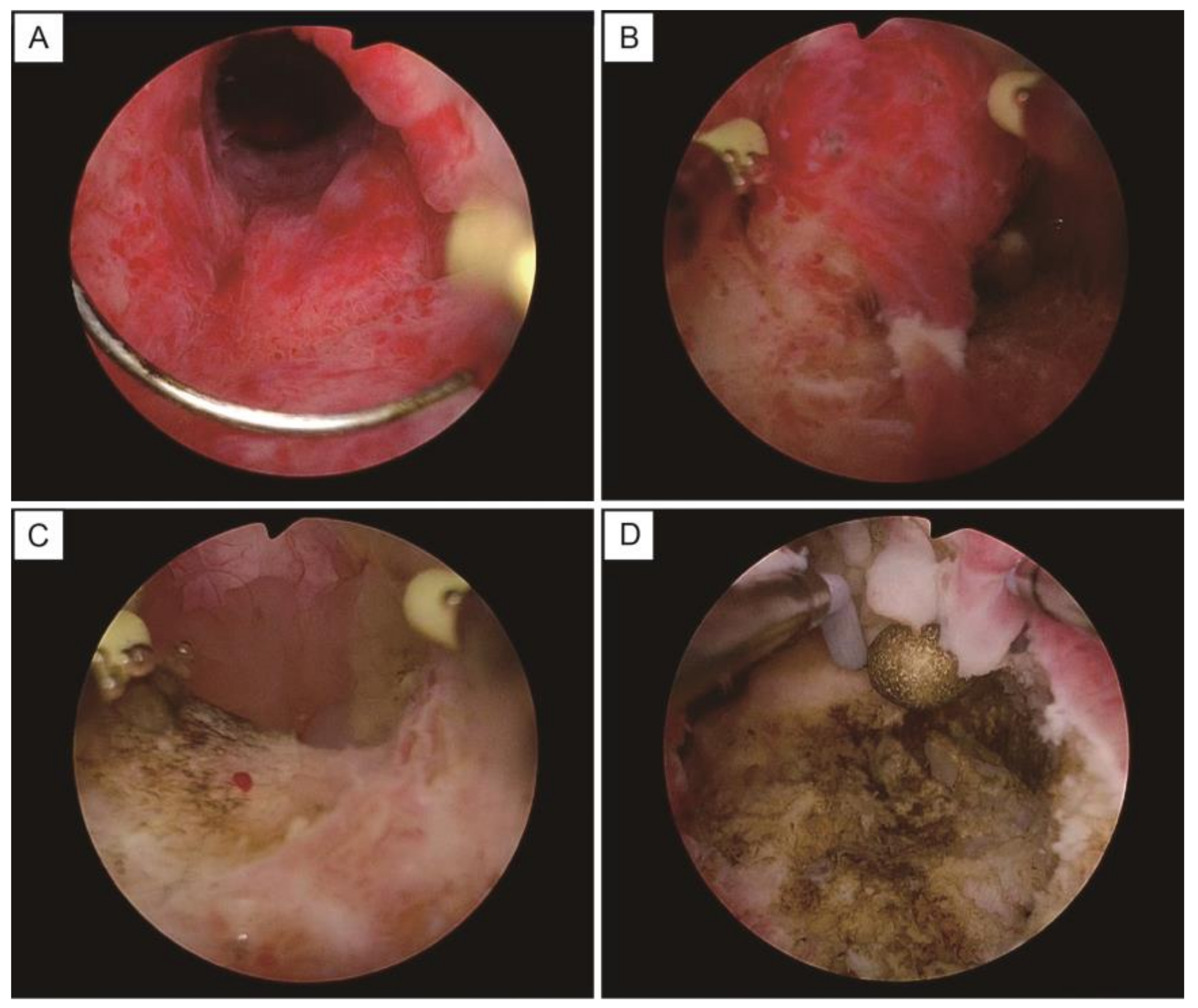
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mikami, Y.; McCluggage, W.G. Endocervical glandular lesions exhibiting gastric differentiation: An emerging spectrum of benign, premalignant, and malignant lesions. Adv. Anat. Pathol. 2013, 20, 227–237. [Google Scholar] [CrossRef] [PubMed]
- Nucci, M.R.; Clement, P.B.; Young, R.H. Lobular endocervical glandular hyperplasia, not otherwise specified: A clinicopathologic analysis of thirteen cases of a distinctive pseudoneoplastic lesion and comparison with fourteen cases of adenoma malignum. Am. J. Surg. Pathol. 1999, 23, 886–891. [Google Scholar] [CrossRef] [PubMed]
- Mikami, Y.; Kiyokawa, T.; Hata, S.; Fujiwara, K.; Moriya, T.; Sasano, H.; Manabe, T.; Akahira, J.; Ito, K.; Tase, T.; et al. Gastrointestinal immunophenotype in adenocarcinomas of the uterine cervix and related glandular lesions: A possible link between lobular endocervical glandular hyperplasia/pyloric gland metaplasia and ‘adenoma malignum’. Mod. Pathol. 2004, 17, 962–972. [Google Scholar] [CrossRef] [PubMed]
- Takatsu, A.; Miyamoto, T.; Fuseya, C.; Suzuki, A.; Kashima, H.; Horiuchi, A.; Ishii, K.; Shiozawa, T. Clonality analysis suggests that STK11 gene mutations are involved in progression of lobular endocervical glandular hyperplasia (LEGH) to minimal deviation adenocarcinoma (MDA). Virchows Arch. 2013, 462, 645–651. [Google Scholar] [CrossRef]
- Mikami, Y.; Hata, S.; Fujiwara, K.; Imajo, Y.; Kohno, I.; Manabe, T. Florid endocervical glandular hyperplasia with intestinal and pyloric gland metaplasia: Worrisome benign mimic of “adenoma malignum”. Gynecol. Oncol. 1999, 74, 504–511. [Google Scholar] [CrossRef]
- Mikami, Y.; Hata, S.; Melamed, J.; Fujiwara, K.; Manabe, T. Lobular endocervical glandular hyperplasia is a metaplastic process with a pyloric gland phenotype. Histopathology 2001, 39, 364–372. [Google Scholar] [CrossRef]
- Miyamoto, T.; Kobara, H.; Shiozawa, T. Biology and management of lobular endocervical glandular hyperplasia. J. Obstet. Gynaecol. Res. 2022, 48, 3056–3067. [Google Scholar] [CrossRef]
- Yamada, Y.; Kobara, H.; Shinagawa, M.; Ono, M.; Takeuchi, H.; Ida, K.; Miyamoto, T.; Shiozawa, T. Effectiveness of hysteroscopic transcervical resection in the diagnosis of lobular endocervical glandular hyperplasia: A case report. Jap. J. Gynecoloc. Obstet. Endosc. 2021, 37, 211–215. [Google Scholar] [CrossRef]
- Takatsu, A.; Shiozawa, T.; Miyamoto, T.; Kurosawa, K.; Kashima, H.; Yamada, T.; Kaku, T.; Mikami, Y.; Kiyokawa, T.; Tsuda, H.; et al. Preoperative differential diagnosis of minimal deviation adenocarcinoma and lobular endocervical glandular hyperplasia of the uterine cervix: A multicenter study of clinicopathology and magnetic resonance imaging findings. Int. J. Gynecol. Cancer 2011, 21, 1287–1296. [Google Scholar] [CrossRef]
- Stoehr, A.; Nann, D.; Staebler, A.; Oberlechner, E.; Brucker, S.Y.; Bachmann, C. Difficulties in diagnosis of a minimal deviation adenocarcinoma of uterine cervix diagnosed postoperatively: Brief communication and literature review. Arch. Gynecol. Obstet. 2019, 300, 1029–1043. [Google Scholar] [CrossRef]
- Ishii, K.; Kumagai, T.; Tozuka, M.; Ota, H.; Katsuyama, T.; Kurihara, M.; Shiozawa, T.; Noguchi, H. A new diagnostic method for adenoma malignum and related lesions: Latex agglutination test with a new monoclonal antibody, HIK1083. Clin. Chim. Acta 2001, 312, 231–233. [Google Scholar] [CrossRef]
- Ida, K.; Yamanoi, K.; Asaka, S.; Takeuchi, H.; Miyamoto, T.; Shiozawa, T.; Nakayama, J. alphaGlcNAc and its catalyst alpha4GnT are diagnostic and prognostic markers in uterine cervical tumor, gastric type. Sci. Rep. 2019, 9, 13043. [Google Scholar] [CrossRef]
- Kyrgiou, M.; Athanasiou, A.; Paraskevaidi, M.; Mitra, A.; Kalliala, I.; Martin-Hirsch, P.; Arbyn, M.; Bennett, P.; Paraskevaidis, E. Adverse obstetric outcomes after local treatment for cervical preinvasive and early invasive disease according to cone depth: Systematic review and meta-analysis. BMJ 2016, 354, i3633. [Google Scholar] [CrossRef]
- Bevis, K.S.; Biggio, J.R. Cervical conization and the risk of preterm delivery. Am. J. Obstet. Gynecol. 2011, 205, 19–27. [Google Scholar] [CrossRef]
- Baldauf, J.J.; Dreyfus, M.; Ritter, J.; Meyer, P.; Philippe, E. Risk of cervical stenosis after large loop excision or laser conization. Obstet. Gynecol. 1996, 88, 933–938. [Google Scholar] [CrossRef]
- Tanaka, Y.; Ueda, Y.; Kakuda, M.; Kubota, S.; Matsuzaki, S.; Iwamiya, T.; Okazawa, A.; Matsuzaki, S.; Hashimoto, K.; Kobayashi, E.; et al. Predictors for recurrent/persistent high-grade intraepithelial lesions and cervical stenosis after therapeutic conization: A retrospective analysis of 522 cases. Int. J. Clin. Oncol. 2017, 22, 921–926. [Google Scholar] [CrossRef]
- Berghella, V.; Pereira, L.; Gariepy, A.; Simonazzi, G. Prior cone biopsy: Prediction of preterm birth by cervical ultrasound. Am. J. Obstet. Gynecol. 2004, 191, 1393–1397. [Google Scholar] [CrossRef]
- Acharya, G.; Kjeldberg, I.; Hansen, S.M.; Sorheim, N.; Jacobsen, B.K.; Maltau, J.M. Pregnancy outcome after loop electrosurgical excision procedure for the management of cervical intraepithelial neoplasia. Arch. Gynecol. Obstet. 2005, 272, 109–112. [Google Scholar] [CrossRef]
- Centini, G.; Troia, L.; Lazzeri, L.; Petraglia, F.; Luisi, S. Modern operative hysteroscopy. Minerva Ginecol. 2016, 68, 126–132. [Google Scholar]
- Keizer, A.L.; Jacobs, B.L.; Thurkow, A.L.; de Lange, M.E.; Radder, C.M.; van Kesteren, P.J.M.; Hanstede, M.M.F.; Huirne, J.A.F.; Hehenkamp, W.J.K. The effect of transcervical resection of submucous fibroids on menstrual blood loss: A prospective cohort study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2022, 274, 128–135. [Google Scholar] [CrossRef]
- Preutthipan, S.; Herabutya, Y. Hysteroscopic polypectomy in 240 premenopausal and postmenopausal women. Fertil. Steril. 2005, 83, 705–709. [Google Scholar] [CrossRef] [PubMed]
- Moore, J.F.; Carugno, J. Hysteroscopy; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Kobara, H.; Miyamoto, T.; Otsuki, T.; Ohya, A.; Shiozawa, T. Worsening cytology and lesion enlargement are useful indicators for malignant transformation of lobular endocervical glandular hyperplasia during follow-up: A case report. Gynecol. Oncol. Rep. 2020, 32, 100571. [Google Scholar] [CrossRef] [PubMed]
- Okuyama, R.; Hashimoto, H.; Miura, T.; Sugita, M.; Arai, M.; Tsunoda, H.; Sasajima, Y.; Horiuchi, H. Two cases of adenocarcinoma in situ arising in lobular endocervical glandular hyperplasia indicating localization of mucin on the cluster surface as an early cytological finding of malignant transformation. Diagn. Cytopathol. 2017, 45, 842–847. [Google Scholar] [CrossRef] [PubMed]
- Ando, H.; Miyamoto, T.; Kashima, H.; Takatsu, A.; Ishii, K.; Fujinaga, Y.; Shiozawa, T. Usefulness of a management protocol for patients with cervical multicystic lesions: A retrospective analysis of 94 cases and the significance of GNAS mutation. J. Obstet. Gynaecol. Res. 2016, 42, 1588–1598. [Google Scholar] [CrossRef]
- Wiik, J.; Kärrberg, C.; Nilsson, S.; Strander, B.; Jacobsson, B.; Sengpiel, V. Associations between cervical intraepithelial neoplasia during pregnancy, previous excisional treatment, cone-length and preterm delivery: A register-based study from western Sweden. BMC Med. 2022, 20, 61. [Google Scholar] [CrossRef]
- Vieira, M.A.; de Araujo, R.L.C.; da Cunha Andrade, C.E.M.; Schmidt, R.L.; Filho, A.L.; Reis, R.D. A randomized clinical trial of a new anti-cervical stenosis device after conization by loop electrosurgical excision. PLoS ONE 2021, 16, e0242067. [Google Scholar] [CrossRef]
- Grund, D.; Kohler, C.; Krauel, H.; Schneider, A. A new approach to preserve fertility by using a coated nitinol stent in a patient with recurrent cervical stenosis. Fertil. Steril. 2007, 87, 1212.e13–1212.e16. [Google Scholar] [CrossRef]
- Jansen, F.W.; Vredevoogd, C.B.; van Ulzen, K.; Hermans, J.; Trimbos, J.B.; Trimbos-Kemper, T.C. Complications of hysteroscopy: A prospective, multicenter study. Obstet. Gynecol. 2000, 96, 266–270. [Google Scholar] [CrossRef]
- Elahmedawy, H.; Snook, N.J. Complications of operative hysteroscopy: An anaesthetist’s perspective. BJA Educ. 2021, 21, 240–242. [Google Scholar] [CrossRef]
- Aas-Eng, M.K.; Langebrekke, A.; Hudelist, G. Complications in operative hysteroscopy—Is prevention possible? Acta Obstet. Gynecol. Scand. 2017, 96, 1399–1403. [Google Scholar] [CrossRef]


| Case | Age | GP | Gastric Mucin | Cervical Cytology | Pathology after Biopsy | Hysterectomy after Biopy | Surgery | Pathology after Hysterectomy |
|---|---|---|---|---|---|---|---|---|
| 1 | 44 | G0 | N/A | LSIL | gastric-type lesion | Y | TLH | nabothian cyst |
| 2 | 45 | G4P4 | positive | NILM | LEGH | Y | TLH | LEGH |
| 3 | 33 | G0 | N/A | AGC-FN | gastric-type mucinous carcinoma | Y | LRH | gastric-type mucinous carcinoma, pT2a2 |
| 4 | 31 | G0 | negative | NILM | nabothian cyst | N | ||
| 5 | 50 | G3P3 | negative | NILM | nabothian cyst | N | ||
| 6 | 37 | G1P0 | positive | NILM | gastric-type lesion | Y | TLH | LEGH |
| 7 | 48 | G1P1 | N/A | AGC-FN | nabothian cyst | N | ||
| 8 | 48 | G2P2 | negative | NILM | no lesions | Y (request by the patient) | TLH | nabothian cyst |
| 9 | 59 | G4P3 | negative | NILM | nabothian cyst | N | ||
| 10 | 49 | G1P1 | N/A | NILM | nabothian cyst | Y (due to hypermenorrhea) | TLH | nabothian cyst |
| 11 | 44 | G2P2 | negative | NILM | no lesions | N | ||
| 12 | 48 | G4P1 | N/A | AGC-NOS | LEGH | Y | TLH | LEGH |
| 13 | 49 | G0 | N/A | AGC-NOS | no lesions | N |
| Case | Age | GP | Gastric Mucin | Cervical Cytology | Pathology after Biopsy | Hysterectomy after Biopsy | Surgery | Pathology after Hysterectomy |
|---|---|---|---|---|---|---|---|---|
| 1 | 37 | G0 | N/A | NILM | no lesion | N | ||
| 2 | 40 | G0 | N/A | NILM | no lesion | N | ||
| 3 | 55 | G6P3 | N/A | NILM | nabothian cyst | N | ||
| 4 | 41 | G2P2 | N/A | NILM | nabothian cyst | N | ||
| 5 | 59 | G1P1 | N/A | AGC | nabothian cyst | N | ||
| 6 | 35 | G1P1 | N/A | NILM | no lesion | N | ||
| 7 | 33 | G0 | N/A | NILM | nabothian cyst | Y (due to hypermenorrhea) | TAH | nabothian cyst |
| 8 | 69 | G1P0 | N/A | AGC | no lesion | N | ||
| 9 | 31 | G0 | N/A | AGC | MDA | Y | mRH | MDA |
| 10 | 48 | G1P0 | N/A | AGC | MDA | Y | RH | LEGH |
| 11 | 46 | G1P1 | N/A | AGC | LEGH | Y | TLH | LEGH, AIS |
| 12 | 46 | G2P1 | N/A | AGC | microglandular hyperplasia | N | ||
| 13 | 81 | G4P3 | N/A | adenocarcinoma | nabothian cyst | N | ||
| 14 | 44 | G0 | N/A | AGC-NOS | no lesion | Y | TLH | LEGH |
| 15 | 55 | G4P3 | N/A | NILM | LEGH | Y | TAH | mucinous carcinoma |
| 16 | 45 | G0 | N/A | NILM | microglandular hyperplasia | N | ||
| 17 | 42 | G1P1 | N/A | AGC-NOS | nabothian cyst, microglandular hyperplasia | N | ||
| 18 | 44 | G2P1 | N/A | NILM | microglandular hyperplasia | Y | TLH | LEGH |
| 19 | 46 | G0 | N/A | AGC | MDA | Y | RH | LEGH |
| 20 | 37 | G0 | N/A | NILM | atypical glands | N | ||
| 21 | 56 | G4P3 | N/A | AGC | endocervical adenocarcinoma, usual type | Y | TLH | no lesion |
| 22 | 52 | G3P2 | N/A | ASC-US | CIN 1, nabothian cyst | N | ||
| 23 | 51 | G2P2 | N/A | NILM | no lesion | N |
| Total Hysterectomy | ||||
|---|---|---|---|---|
| LEGH or Greater Lesion | Nabothian Cyst No Lesion | Total | ||
| Hysteroscopic Biopsy | LEGH or greater lesion | 4 | 1 | 5 |
| nabothian cyst no lesion | 0 | 2 | 2 | |
| Total | 4 | 3 | 7 | |
| Total Hysterectomy | ||||
|---|---|---|---|---|
| LEGH or Greater Lesion | Nabothian Cyst No Lesion | Total | ||
| Conization | LEGH or greater lesion | 6 | 1 | 7 |
| nabothian cyst no lesion | 1 | 1 | 2 | |
| Total | 7 | 2 | 9 | |
| Hysteroscpopy (n = 13) | Conization (n = 23) | p Value | |
|---|---|---|---|
| mean age (year) | 45 ± 8 | 48 ± 12 | 0.49 |
| operative time (minute) | 23 ± 12 | 35 ± 20 | 0.06 |
| total blood loss (mL) | small amounts (not countable) | 43 ± 70 | |
| postoperative hospital stay (day) | 1.1 ± 0.2 | 1.6 ± 1.4 | 0.22 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shiro, R.; Kotani, Y.; Ohta, M.; Sato, H.; Kashima, Y.; Murakami, K.; Kawasaki, K.; Nakai, H.; Matsumura, N. Diagnostic Utility of Hysteroscopic Biopsy in Cases of Suspected Lobular Endocervical Glandular Hyperplasia and Comparison with Cervical Conization. Healthcare 2023, 11, 1619. https://doi.org/10.3390/healthcare11111619
Shiro R, Kotani Y, Ohta M, Sato H, Kashima Y, Murakami K, Kawasaki K, Nakai H, Matsumura N. Diagnostic Utility of Hysteroscopic Biopsy in Cases of Suspected Lobular Endocervical Glandular Hyperplasia and Comparison with Cervical Conization. Healthcare. 2023; 11(11):1619. https://doi.org/10.3390/healthcare11111619
Chicago/Turabian StyleShiro, Reona, Yasushi Kotani, Mamiko Ohta, Hanako Sato, Yoko Kashima, Kosuke Murakami, Kaoru Kawasaki, Hidekatsu Nakai, and Noriomi Matsumura. 2023. "Diagnostic Utility of Hysteroscopic Biopsy in Cases of Suspected Lobular Endocervical Glandular Hyperplasia and Comparison with Cervical Conization" Healthcare 11, no. 11: 1619. https://doi.org/10.3390/healthcare11111619
APA StyleShiro, R., Kotani, Y., Ohta, M., Sato, H., Kashima, Y., Murakami, K., Kawasaki, K., Nakai, H., & Matsumura, N. (2023). Diagnostic Utility of Hysteroscopic Biopsy in Cases of Suspected Lobular Endocervical Glandular Hyperplasia and Comparison with Cervical Conization. Healthcare, 11(11), 1619. https://doi.org/10.3390/healthcare11111619









